Documente Academic
Documente Profesional
Documente Cultură
Tetanus - The Disease
Încărcat de
manjunath mamathaTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Tetanus - The Disease
Încărcat de
manjunath mamathaDrepturi de autor:
Formate disponibile
Tetanus - the disease
WHAT IS TETANUS?
Tetanus is acquired through exposure to the spores of the
bacterium Clostridium tetani which are universally present in the
soil. The disease is caused by the action of a potent neurotoxin
produced during the growth of the bacteria in dead tissues, e.g. in
dirty wounds or in the umbilicus following non-sterile delivery.
People of all ages can get tetanus. But the disease is particularly
common and serious in newborn babies. This is called neonatal
tetanus. Most infants who get the disease die. Neonatal tetanus is
particularly common in rural areas where most deliveries are at
home without adequate sterile procedures. In 2000, WHO
estimates that neonatal tetanus killed about 200 000 babies.
HOW IS TETANUS SPREAD?
Tetanus is not transmitted from person to person. A person usually
becomes infected with tetanus when dirt enters a wound or cut.
Tetanus germs are likely to grow in deep puncture wounds caused
by dirty nails, knives, tools, wood splinters, and animal bites.
Women face an additional risk of infection if a contaminated tool is
used during childbirth or during an abortion.
A newborn baby may become infected if the knife, razor, or other
instrument used to cut its umbilical cord is dirty, if dirty material is
used to dress the cord, or if the hands of the person delivering the
baby are not clean.
Infants and children may also contract tetanus when dirty
instruments are used for circumcision, scarification, and skin
piercing, and when dirt, charcoal, or other unclean substances are
rubbed into a wound.
Risk factors
The following increase your likelihood of getting tetanus:
Failure to get vaccinated or to keep up to date with booster
shots against tetanus
An injury that lets tetanus spores into the wound
A foreign body, such as a nail or splinter
WHAT ARE THE SIGNS AND SYMPTOMS OF
TETANUS?
The time between getting the infection and showing symptoms is
usually between three and 10 days. But it may be as long as three
weeks. The shorter the incubation period the higher the risk of
death.
In children and adults muscular stiffness in the jaw is a common
first sign of tetanus. This symptom is followed by stiffness in the
neck, difficulty swallowing, stiffness in the stomach muscles,
muscle spasms, sweating, and fever. Newborn babies with tetanus
are normal at birth, but stop sucking between three and 28 days
after birth. They stop feeding and their bodies become stiff while
severe muscle contractions and spasms occur. Death follows in
most cases.
WHAT ARE THE COMPLICATIONS OF TETANUS?
Fractures of the spine or other bones may occur as a result of
muscle spasms and convulsions. Abnormal heartbeats and coma
can occur, as can development of pneumonia and other infections.
Death is particularly likely in the very young and in old people.
Complications of tetanus infection may include:
• Broken bones. The severity of spasms may cause the spine
and other bones to break.
• Blockage of a lung artery (pulmonary embolism). A blood clot
that has traveled from elsewhere in your body can block the main
artery of the lung or one of its branches.
• Death. Severe tetanus-induced (tetanic) muscle spasms can
interfere with or stop your breathing. Respiratory failure is the most
common cause of death. Lack of oxygen may also induce cardiac
arrest and death. Pneumonia is another cause of death.
WHAT IS THE TREATMENT FOR TETANUS?
Tetanus at any age is a medical emergency best managed in a
referral hospital.
HOW IS TETANUS PREVENTED?
Immunizing infants and children with DTP or DT and adults with Td
prevents tetanus. More recently, some countries have been using a
combination vaccine that includes vaccines for diphtheria, tetanus,
pertussis, vitamin A (HepB), and sometimes Haemophilus inflenzae
type b (Hib).
Neonatal tetanus can be prevented by immunizing women of
childbearing age with tetanus toxoid, either during pregnancy or
outside of pregnancy. This protects the mother and enables tetanus
antibodies to be transferred to her baby.
Clean practices are especially important when a mother is
delivering a child, even if she has been immunized. People who
recover from tetanus do not have natural immunity and can be
infected again and therefore need to be immunized.
GLOBAL ACCELERATED DISEASE CONTROL ISSUES
WHO, UNICEF and UNFPA agreed to set the year 2005 as the target
date for worldwide elimination of neonatal tetanus. This implies the
reduction of neonatal tetanus incidence to below one case per 1000
live births per year in every district. This goal was reaffirmed by the
United Nations General Assembly Special Session (UNGASS) in
2002. Because tetanus survives in the environment, eradication of
the disease is not feasible and high levels of immunization have to
continue even after the goal has been achieved.
To achieve the elimination goal, countries implement a series of
strategies:
Improve the percentage of pregnant women immunized with
vaccines containing tetanus toxoid.
Administer vaccines containing tetanus toxoid to all women of
childbearing age in high-risk areas. This is usually
implemented through a three round campaign approach.
Promote clean delivery and childcare practices.
Improve surveillance and reporting of neonatal tetanus cases.
KEY POINTS
Tetanus is caused by bacteria found in the environment.
Infection occurs during unclean delivery of babies, when
contaminated objects are used to cut the umbilical cord, or
anytime tetanus bacteria enter a puncture or cut in the skin.
Neonatal tetanus remains a serious problem in countries with
poor immunization coverage and unclean practices at
childbirth. Most newborns with tetanus die.
The best way to prevent tetanus is to immunize with tetanus
toxoid and to clean wounds thoroughly and remove dead
tissue.
The best way to prevent neonatal tetanus is to immunize
women of childbearing age (or pregnant women) and to
ensure clean delivery practices.
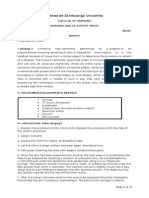
VACCINE SUMMARY
Type of vaccine Toxoid as DT, TT or Td
Number of doses At least two primary doses
Schedule See table on page 3 (Tetanus - the vaccine)
Booster TT/Td every 10 years or during pregnancy. DT 18
months to six years of age
Contraindications Anaphylactic reaction to previous dose
Adverse reactions Mild local or systemic reactions are
common and increase in frequency with increasing numbers of
doses, and may constitute a contraindication to further doses
Special precautions Reduced diphtheria (Td instead of DT)
content as from seven years of age
Dosage 0.5ml
Injection site Outer upper arm
Injection type Intramuscular
Storage Store between 2°C–8°C. Never freeze
S-ar putea să vă placă și
- Old Diseases Are Coming Back:: Courtesy Of Anti-VaccinatorsDe la EverandOld Diseases Are Coming Back:: Courtesy Of Anti-VaccinatorsEvaluare: 1 din 5 stele1/5 (1)
- Tetanus Case PresentationDocument18 paginiTetanus Case PresentationDesiree Guerra100% (1)
- Dis Tetanus Color OfficeDocument1 paginăDis Tetanus Color Officejm_ftaaÎncă nu există evaluări
- Tetanus Diseases BingDocument16 paginiTetanus Diseases Bingnurma jafarÎncă nu există evaluări
- Tetanus (Lockjaw) PDFDocument8 paginiTetanus (Lockjaw) PDFGLADYS MAY GUDELOS MEJIASÎncă nu există evaluări
- TetanusDocument2 paginiTetanussyaiful_snÎncă nu există evaluări
- 19: 05 24 Sept 2011 Tetanus: SymtompsDocument5 pagini19: 05 24 Sept 2011 Tetanus: SymtompsVania ParamithaÎncă nu există evaluări
- Tetanus: Ma. Theresa Dj. YumangDocument28 paginiTetanus: Ma. Theresa Dj. YumangJean SarocamÎncă nu există evaluări
- Facts About Tetanus DeseaseDocument1 paginăFacts About Tetanus DeseasechaariaÎncă nu există evaluări
- TetanusDocument129 paginiTetanusErina Erichan OtoÎncă nu există evaluări
- Status InternusDocument12 paginiStatus InternusPriscaÎncă nu există evaluări
- Brief: Tetanus Disease, Treatment, ManagementDocument5 paginiBrief: Tetanus Disease, Treatment, ManagementchindiaÎncă nu există evaluări
- Tetanus Shots For Adults: Patient HandoutDocument1 paginăTetanus Shots For Adults: Patient Handoutselvie87Încă nu există evaluări
- Tetanus EmedicineDocument19 paginiTetanus EmedicineSapto SutardiÎncă nu există evaluări
- Signs and SymptomsDocument6 paginiSigns and Symptomsdareine22Încă nu există evaluări
- 54 TetanusDocument25 pagini54 Tetanusghofran001997Încă nu există evaluări
- Products & Services: Book: Mayo Clinic Guide To Raising A Healthy ChildDocument3 paginiProducts & Services: Book: Mayo Clinic Guide To Raising A Healthy ChildjunÎncă nu există evaluări
- In The Name of ALLAH The Beneficent and MercifulDocument49 paginiIn The Name of ALLAH The Beneficent and Mercifulcute_honiya100% (1)
- Tetanus: HistoryDocument15 paginiTetanus: HistorydanielleÎncă nu există evaluări
- tetanusDocument6 paginitetanusImmelda Stella Medessoh DohoÎncă nu există evaluări
- TetanusDocument3 paginiTetanusmake_jajoeÎncă nu există evaluări
- Tetanus ToxoidDocument1 paginăTetanus Toxoidapi-735134367Încă nu există evaluări
- What Is Tetanus?: Clostridium Tetani or The Tetanus Bacillus Is A Slender, Gram-Positive, Anaerobic Rod That MayDocument5 paginiWhat Is Tetanus?: Clostridium Tetani or The Tetanus Bacillus Is A Slender, Gram-Positive, Anaerobic Rod That MayraechcmÎncă nu există evaluări
- Neonatal TetanusDocument44 paginiNeonatal TetanusJake MillerÎncă nu există evaluări
- Tetanus: BackgroundDocument19 paginiTetanus: BackgroundYovita Devi KornelinÎncă nu există evaluări
- Sign Simptom TetanusDocument1 paginăSign Simptom Tetanusali subchanÎncă nu există evaluări
- Tetanus: Introduced in 1930s (DT) and 1952/3 (DTP) NotifiableDocument8 paginiTetanus: Introduced in 1930s (DT) and 1952/3 (DTP) NotifiableDaphne Ongbit JaritoÎncă nu există evaluări
- TetanusDocument34 paginiTetanusBintang Ruth Cecilia FebrinaÎncă nu există evaluări
- TetanusDocument18 paginiTetanusMichael EatonÎncă nu există evaluări
- Tetanus PDFDocument10 paginiTetanus PDFVina MuspitaÎncă nu există evaluări
- Tetanus (Lockjaw) : Secondary NavDocument3 paginiTetanus (Lockjaw) : Secondary NavjunÎncă nu există evaluări
- TETANUSDocument15 paginiTETANUSLovely Michaela CaberioÎncă nu există evaluări
- Dis Diphtheria Color OfficeDocument2 paginiDis Diphtheria Color OfficeJesse EstradaÎncă nu există evaluări
- TetanusDocument35 paginiTetanusAlkamis Rabiu UsmanÎncă nu există evaluări
- Tetanus Symptoms, Causes, Treatment and PreventionDocument4 paginiTetanus Symptoms, Causes, Treatment and PreventionSneha SnehaÎncă nu există evaluări
- Questions and Answers: TetanusDocument4 paginiQuestions and Answers: TetanuszippyzevenÎncă nu există evaluări
- TETANUS Revised PFLODocument12 paginiTETANUS Revised PFLOPhelyn Frances Lauronilla OracionÎncă nu există evaluări
- Tetanus: "Lock Jaw"Document10 paginiTetanus: "Lock Jaw"Atoillah IsvandiaryÎncă nu există evaluări
- Anisa A. Edris BSN January 25, 2012 Group A5: Central Nervous SystemDocument4 paginiAnisa A. Edris BSN January 25, 2012 Group A5: Central Nervous SystemEynie EdrisÎncă nu există evaluări
- Dis Diphtheria Color OfficeDocument2 paginiDis Diphtheria Color Officeselvie87Încă nu există evaluări
- Management and Prevention of Tetanus: Abstract: THDocument16 paginiManagement and Prevention of Tetanus: Abstract: THFabian FabiansyahÎncă nu există evaluări
- TetanusDocument18 paginiTetanusRohan TejaÎncă nu există evaluări
- Viral Meningitis, Tetanus, Giardiasis and Westnile Fever Causes, Symptoms, TreatmentsDocument20 paginiViral Meningitis, Tetanus, Giardiasis and Westnile Fever Causes, Symptoms, TreatmentsFlorence ILoyd R. TorresÎncă nu există evaluări
- Neonatal Tetanus in African Children: Causes, Symptoms, Predisposing Factors, Prevention and ControlDocument4 paginiNeonatal Tetanus in African Children: Causes, Symptoms, Predisposing Factors, Prevention and Controlzul090Încă nu există evaluări
- Diphtheria, Tetanus, Pertussis Vaccines ExplainedDocument3 paginiDiphtheria, Tetanus, Pertussis Vaccines ExplainedGlenn KristieÎncă nu există evaluări
- Tetanus Ebm PutriDocument12 paginiTetanus Ebm PutriLilik NatasubrataÎncă nu există evaluări
- Questions and Answers: TetanusDocument4 paginiQuestions and Answers: TetanusRhodjan RescoÎncă nu există evaluări
- TetanusDocument7 paginiTetanusallah akbarÎncă nu există evaluări
- K6 SLIDE-MANAGEMENT OF TETANUS IN PEDIATRIC-baruDocument69 paginiK6 SLIDE-MANAGEMENT OF TETANUS IN PEDIATRIC-baruRaja Alfian IrawanÎncă nu există evaluări
- Gram + DiseasesDocument30 paginiGram + DiseasesveerdedajiÎncă nu există evaluări
- Tetanus ToxoidDocument2 paginiTetanus ToxoidReyna BungcarasÎncă nu există evaluări
- Deadly Lockjaw Disease: Symptoms and Causes of TetanusDocument9 paginiDeadly Lockjaw Disease: Symptoms and Causes of TetanusRiz Sanfebrian AdiatmaÎncă nu există evaluări
- Activity 2 - Case StudyDocument5 paginiActivity 2 - Case StudyGrace MendozaÎncă nu există evaluări
- Tetanus NoteDocument4 paginiTetanus NoteTaufik KhanÎncă nu există evaluări
- DPT PresentationDocument36 paginiDPT PresentationTanviÎncă nu există evaluări
- Expanded Program For Immunization (EPI)Document70 paginiExpanded Program For Immunization (EPI)Erwin Jake Taguba100% (1)
- !tetanus MDocument22 pagini!tetanus MWendo yayahÎncă nu există evaluări
- Infectious Pertusis-6 (Muhadharaty)Document5 paginiInfectious Pertusis-6 (Muhadharaty)dr.salam.hassaniÎncă nu există evaluări
- Brook 2008Document10 paginiBrook 2008Kami LyaÎncă nu există evaluări
- Practice Quiz - Maternity & NewbornDocument4 paginiPractice Quiz - Maternity & NewbornMS100% (1)
- DLP in MAPEH - Grade 9 Myths and Misconceptions About DrugsDocument4 paginiDLP in MAPEH - Grade 9 Myths and Misconceptions About DrugsMa. Reina Gail T. Lizaso100% (5)
- CQC Inspection ReportDocument17 paginiCQC Inspection ReportMark RushworthÎncă nu există evaluări
- Bowel Preparation Colon ResectionDocument28 paginiBowel Preparation Colon ResectioncristiangallardovÎncă nu există evaluări
- The Phenomenology of TraumaDocument4 paginiThe Phenomenology of TraumaMelayna Haley0% (1)
- M H Case SolutionDocument1 paginăM H Case SolutionSai Dinesh UniqueÎncă nu există evaluări
- Hospitals Penalized for Refusing Emergency CareDocument6 paginiHospitals Penalized for Refusing Emergency CareApril Isidro100% (1)
- Nexthealth - Semantic Web Sparks Evolution of Health 2.0 - A Road Map To Consumer-Centric HealthcareDocument7 paginiNexthealth - Semantic Web Sparks Evolution of Health 2.0 - A Road Map To Consumer-Centric HealthcareMaarten den Braber100% (43)
- Espiritismo Leonora Piper Coisas Que Acertou Questiona Sobrinha Que Não Existia-Resposta Está em Outro Arquivo PDFDocument155 paginiEspiritismo Leonora Piper Coisas Que Acertou Questiona Sobrinha Que Não Existia-Resposta Está em Outro Arquivo PDFMariana MuradÎncă nu există evaluări
- Migraine Hemicrania and Its Homeopathic Permanent Cure - DR Bashir Mahmud ElliasDocument6 paginiMigraine Hemicrania and Its Homeopathic Permanent Cure - DR Bashir Mahmud ElliasBashir Mahmud ElliasÎncă nu există evaluări
- Drug Study DengueDocument3 paginiDrug Study DengueiamELHIZAÎncă nu există evaluări
- Veterinarian Doctor Resume - Bassem BazzezDocument2 paginiVeterinarian Doctor Resume - Bassem Bazzezkouloud dibiÎncă nu există evaluări
- Atlantis Implant Compatibility Chart 79214-US-1107Document2 paginiAtlantis Implant Compatibility Chart 79214-US-1107Jean-Christophe PopeÎncă nu există evaluări
- Lesson 6 (New) Medication History InterviewDocument6 paginiLesson 6 (New) Medication History InterviewVincent Joshua TriboÎncă nu există evaluări
- Ateneo de Zamboanga University Nursing Skills Output (NSO) Week BiopsyDocument4 paginiAteneo de Zamboanga University Nursing Skills Output (NSO) Week BiopsyHaifi HunÎncă nu există evaluări
- Contact AllergyDocument39 paginiContact AllergylintangÎncă nu există evaluări
- STG-General Hospital PDFDocument704 paginiSTG-General Hospital PDFBirhane100% (1)
- Statement On Controlled Organ Donation After Circulatory DeathDocument10 paginiStatement On Controlled Organ Donation After Circulatory DeathHeidi ReyesÎncă nu există evaluări
- MCPS Form For Annual Sports Physical Exam - (PPE) 2010 Edition Prepared by Am Academy of Ped, Am. Academy of Family Phys Et Al.Document5 paginiMCPS Form For Annual Sports Physical Exam - (PPE) 2010 Edition Prepared by Am Academy of Ped, Am. Academy of Family Phys Et Al.Concussion_MCPS_MdÎncă nu există evaluări
- The Privileges and Duties of Registered Medical Practitioners - PDF 27777748Document6 paginiThe Privileges and Duties of Registered Medical Practitioners - PDF 27777748innyÎncă nu există evaluări
- CEO Administrator Healthcare Management in San Antonio TX Resume Robert WardDocument3 paginiCEO Administrator Healthcare Management in San Antonio TX Resume Robert WardRobertWard2Încă nu există evaluări
- Fphar 12 768268Document25 paginiFphar 12 768268Araceli Anaya AlvaradoÎncă nu există evaluări
- Therapeutic Drug MonitoringDocument6 paginiTherapeutic Drug MonitoringEdi Uchiha SutarmantoÎncă nu există evaluări
- All Models W ExplanationDocument63 paginiAll Models W Explanationpayal1407Încă nu există evaluări
- Yorkville Advisors Completes $7.5M Equity Facility With EntreMed, Inc.Document2 paginiYorkville Advisors Completes $7.5M Equity Facility With EntreMed, Inc.YorkvilleAdvisorsÎncă nu există evaluări
- Ergogenic Aids 1Document24 paginiErgogenic Aids 1unattractiveyouÎncă nu există evaluări
- Anderson2008 Levofloxasin A ReviewDocument31 paginiAnderson2008 Levofloxasin A ReviewFazdrah AssyuaraÎncă nu există evaluări
- You Can Grow Your IntelligenceDocument6 paginiYou Can Grow Your IntelligenceSoniaÎncă nu există evaluări
- Fetal SkullDocument34 paginiFetal SkullNeelofur Ibran Ali85% (20)
- Antipsychotic Agents: Conventional vs AtypicalDocument18 paginiAntipsychotic Agents: Conventional vs AtypicalmengakuÎncă nu există evaluări