Documente Academic
Documente Profesional
Documente Cultură
Appendix 3. Perioperative Management of Diabetes Mellitus
Încărcat de
samsarmaDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Appendix 3. Perioperative Management of Diabetes Mellitus
Încărcat de
samsarmaDrepturi de autor:
Formate disponibile
APPENDIX 3
PERIOPERATIVE MANAGEMENT OF DIABETES MELLITUS
Link consultant: Dr Grainne Nicholson
All patients with diabetes undergoing procedures or surgery, or who are nil by mouth, should
have their glycaemic control managed according to the variable rate intravenous insulin
infusion (vriii) protocol attached to the patient’s prescription chart.
Patients with diabetes should ensure that they maintain good glycaemic control (HbA1c < 8.5%)
in the months and weeks prior to surgery, as this improves the healing process post-operatively.
Patients with diabetes in the peri-operative period and nil by mouth, should be managed
according to the following protocol. (For diabetic ketoacidosis, see section on DKA).
Pre-operative assessment
Patients with type-2 diabetes managed with diet alone, need no intervention prior to surgery.
For procedures that involve giving intravenous radio-contrast, discontinue metformin 48hrs prior
to the procedure. Otherwise, continue metformin in patients pre-operatively.
Before surgery
To ensure that blood glucose is controlled within normal limits before surgery (target range: 5-
10mmol/L), a random blood glucose should be obtained soon after the patient is admitted. If
it is not in the target range, advice should be sought from the diabetic team, the anaesthetic
team or both.
An intravenous cannula should be inserted the evening before surgery.
Patients should receive their usual doses of oral anti-diabetic and/or insulin (except for long-
acting) on the day prior to surgery, including evening doses. For long-acting insulins, normal
evening doses should be halved and given with their evening meal.
From 6am on the morning of surgery, maintain glycaemic control by starting a
glucose/potassium/insulin (GKI) regimen, using the following infusions:
(i) 500ml 5% dextrose plus 0.45% NaCl with 0.15% KCl (premixed bag at 85 ml/ hr.) (If the
patient has renal impairment, omit the potassium); and
(ii) Soluble insulin (Human Actrapid) 50 units in 50ml 0.9% sodium chloride at the rate shown
in the Perioperative Management table below.
These infusions should run simultaneously and through the same cannula.
Bedside blood glucose measurements must be taken hourly from 6am and used to guide and
adjust the rate of insulin infusion according to the table below.
Patients with type-1 diabetes should not be left without any intravenous insulin running. If blood
sugar is <4mmol/l, give Glucose 10% at 100mls/hr; if no increase after 30mins give glucose
20% 100mls as a bolus and repeat blood glucose after 15mins. Continue insulin infusion at 0.5
units per hour.
Blood Glucose (mmol/l) Rate of insulin infusion (units/hr)
<3.9 – 4 0.5
4 – 6.9 1.0
7 – 9.9 2.0
10 – 14.9 3.0
15 – 19.9 4.0
20 5 and call doctor
If glucose is temporarily stopped, eg. on route to theatre, insulin must also be stopped
temporarily.
Never administer sodium chloride 0.9% as the sole intravenous fluid to a patient receiving
insulin. If a patient is fasting for several days and there is concern regarding hyponatraemia,
consult the anaesthetist.
Diabetic patients should be first on the theatre list where possible, to minimise duration of
starvation.
Treatment of hypoglycaemia for patients on a perioperative diabetic regimen
If blood glucose is <4mmol/l, give Glucose 10% at 100mls/hr; if no increase after 30mins give
glucose 20% 100mls as a bolus and repeat blood glucose after 15mins. Inform the doctor at
once.
Do not administer oral hypoglycaemics on the day of surgery. A patient on the afternoon list
must still be stabilised on intravenous glucose, insulin and potassium.
Post-operative management
Blood glucose measurements should be taken hourly until the reading is stable and within normal
range. Readings can then be taken 2-hrly. Serum potassium should be measured on alternate
glucose samples.
The first meal following surgery should be eaten while the intravenous insulin infusion and
glucose 10% infusion continues, to check that the meal is tolerated. If tolerated, patients on
subcutaneous insulin or oral hypoglycaemics can return to their usual regimen.
STOP IV insulin infusion 1hr AFTER the first dose of subcutaneous insulin
For patients taking metformin who receive contrast media, metformin may be re-started 48 hours
after the procedure.
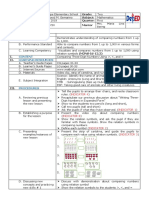
Perioperative management of diabetes mellitus
Establish adequate diabetic control 2-3 days prior to surgery.
Metformin should be stopped 48 hrs prior to procedure.
Ensure that operation is first on theatre list.
On morning of surgery, omit usual insulin or oral hypoglycaemic; check blood
glucose and potassium.
Type 1 Diabetes Type 2 Diabetes
Insulin treated On oral agents
Major surgery
Minor surgery
(no oral hypo-
At 06:00 establish intravenous insulin infusion (50 units
glycaemics on
soluble insulin Human Actrapid in 50ml 0.9% sodium
day of surgery)
chloride) and 500ml of 5% glucose +0.45%NaCl infusion +
10mmol/l potassium (depending on renal function) at
85ml/hr Observe blood
Check blood glucose hourly; adjust insulin rate according to glucose If BM
variable prescription not within target
Aim to maintain blood glucose in the range 5-10mmol/L range, call
Seek advice for patients who are fluid restricted; or who anaesthetist
remain nil by mouth for long periods, where hyponatraemia
presents a risk
S-ar putea să vă placă și
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Rubrics For Skit or Role PlayDocument1 paginăRubrics For Skit or Role PlayGheyDelaCueva50% (2)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Escrow Agreement TemplateDocument5 paginiEscrow Agreement TemplatesamsarmaÎncă nu există evaluări
- Top 25 Test-Taking Tips, Suggestions & Strategies: WrongDocument5 paginiTop 25 Test-Taking Tips, Suggestions & Strategies: WronglheanzÎncă nu există evaluări
- MPCE 15 InternshipDocument56 paginiMPCE 15 InternshipRaghavÎncă nu există evaluări
- 2009-2014 Division of Student Affairs Strategic Plan: MissionDocument15 pagini2009-2014 Division of Student Affairs Strategic Plan: MissionDominicSavioÎncă nu există evaluări
- Tirupati Information PamphletDocument1 paginăTirupati Information PamphletsamsarmaÎncă nu există evaluări
- Presentation On AKGCo-1 FinalDocument40 paginiPresentation On AKGCo-1 FinalsamsarmaÎncă nu există evaluări
- Change of Land Use Policy Gazette Notification Andhra Pradesh CRDADocument4 paginiChange of Land Use Policy Gazette Notification Andhra Pradesh CRDAsamsarmaÎncă nu există evaluări
- Kadapa District Industries Profile MSMEDocument20 paginiKadapa District Industries Profile MSMEsamsarmaÎncă nu există evaluări
- Hospital Waste Management An Insight Approach: NtroductionDocument47 paginiHospital Waste Management An Insight Approach: NtroductionAvijit Mitra MustafiÎncă nu există evaluări
- Amended Nellore DPDocument19 paginiAmended Nellore DPsuryanathÎncă nu există evaluări
- Washer & Dryer SpecsDocument3 paginiWasher & Dryer SpecssamsarmaÎncă nu există evaluări
- Herbal Pest Repellent Potpourri SanitisedDocument1 paginăHerbal Pest Repellent Potpourri SanitisedsamsarmaÎncă nu există evaluări
- Astrology Maha NibandamDocument1 paginăAstrology Maha NibandamNihal SenÎncă nu există evaluări
- SASBE Call For PapersDocument1 paginăSASBE Call For Papersanup8800% (1)
- L&T Limited: About The CompanyDocument2 paginiL&T Limited: About The CompanySai SanjeevareddyÎncă nu există evaluări
- Wise SpendingDocument5 paginiWise SpendingFatiyarrÎncă nu există evaluări
- Uncovering CLIL 1 PDFDocument6 paginiUncovering CLIL 1 PDFrbiv0770Încă nu există evaluări
- Asafa Book Oromuma PDFDocument183 paginiAsafa Book Oromuma PDFgemechuÎncă nu există evaluări
- Wonderlic Scholastic Level Exam Sample Questions: AnswersDocument1 paginăWonderlic Scholastic Level Exam Sample Questions: AnswersElize FontesÎncă nu există evaluări
- BSC6900 RNC Step CommissionDocument6 paginiBSC6900 RNC Step CommissionFrancisco Salvador MondlaneÎncă nu există evaluări
- Swot Analysisdoc MartensDocument2 paginiSwot Analysisdoc MartensaswertyÎncă nu există evaluări
- Beekeeping Practices Challenge and Honey MarketingDocument24 paginiBeekeeping Practices Challenge and Honey MarketingBrook Legese Dadhe 23926007Încă nu există evaluări
- Test A NN4 2020-2021Document2 paginiTest A NN4 2020-2021Toska GilliesÎncă nu există evaluări
- Habits of Mind HandoutDocument2 paginiHabits of Mind Handoutapi-240193026Încă nu există evaluări
- Landon AlexanderDocument6 paginiLandon Alexanderapi-455881201Încă nu există evaluări
- 2015 Nutrition Month Celebration Narrative ReportDocument2 pagini2015 Nutrition Month Celebration Narrative ReportBenjie Modelo ManilaÎncă nu există evaluări
- Reconfigurable Diffractive Antenna Based On Switchable Electrically Induced TransparencyDocument12 paginiReconfigurable Diffractive Antenna Based On Switchable Electrically Induced TransparencyAnuj SharmaÎncă nu există evaluări
- Accomplishment Teachers BoothDocument3 paginiAccomplishment Teachers Boothjosephine paulinoÎncă nu există evaluări
- Comparing Numbers (2021 - 06 - 19 01 - 35 - 12 UTC) (2021 - 08 - 06 04 - 51 - 25 UTC)Document3 paginiComparing Numbers (2021 - 06 - 19 01 - 35 - 12 UTC) (2021 - 08 - 06 04 - 51 - 25 UTC)ALLinOne BlogÎncă nu există evaluări
- SCOPUS Guide For Journal Editors ELSEVIERDocument75 paginiSCOPUS Guide For Journal Editors ELSEVIERKhis HudhaÎncă nu există evaluări
- Digital Logic and Computer Organization: Unit-I Page NoDocument4 paginiDigital Logic and Computer Organization: Unit-I Page NoJit AggÎncă nu există evaluări
- Higher EducationDocument19 paginiHigher EducationAnonymous pxy22mwps5Încă nu există evaluări
- 1machine Learning With PythonDocument12 pagini1machine Learning With PythonAmbika ThakurÎncă nu există evaluări
- 260 Day SWHW Bible Reading PlanDocument12 pagini260 Day SWHW Bible Reading PlanWildoleanderÎncă nu există evaluări
- IPCR Portfolio MOVs TrackerDocument10 paginiIPCR Portfolio MOVs TrackerKris Tel Delapeña ParasÎncă nu există evaluări
- Introduction To Deep Learning: Le Hoang Nam Namlh@hanu - Edu.vnDocument33 paginiIntroduction To Deep Learning: Le Hoang Nam Namlh@hanu - Edu.vnKhoa Tran NgocÎncă nu există evaluări
- Social Psychology ReflectionDocument3 paginiSocial Psychology Reflectionapi-325740487Încă nu există evaluări
- Ade 149Document74 paginiAde 149matt_langioneÎncă nu există evaluări