Documente Academic
Documente Profesional
Documente Cultură
7MB, Ac, 1PCS
Încărcat de
Ricko CiadyDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
7MB, Ac, 1PCS
Încărcat de
Ricko CiadyDrepturi de autor:
Formate disponibile
Arrhythmia as a
Hypovolemic Shock
Manifestation in
Daily Practice
Ricko Ciady, Nurwahyudi
Department of Cardiology and
Vascular Medicine,
Dr. Haji Koesnadi General Hospital,
Bondowoso, Indonesia
Introduction Discussion Conclusion
As a primary care physician with limited resources we often Sinus tachycardia as a secondary respond from the Based on this case, we conclude that the principles
facing a hard decision either to give an aggressive fluid body to maintain hemodynamic imbalance due the cause from this inappropriate sinus tachycardia (IST) is
resuscitation or combining between fluid resuscitation bleeding, by increase the rate to maintain cardiac stunned myocardium which is occurred by ischemia in
and inotropic agent in a shock with hypovolemic output and peripheral perfusion. Usually after myocardium due to hypovolemic shock. [1-7]
mimicking cardiogenic shock. More over in remote and adequate resuscitation given, sinus tachycardia
limited resources to make a diagnosis will be diminished into sinus rhythm as the volume Early aggressive therapy on fluid and blood
depletion resolved. But in some circumstance when replacement are proven as main modality to treat
01
the biochemical intervene on cellular level can cause hemorrhagic shock. At the end we recommended fluid
prolonged arrhythmia. challenge as a therapy and basic modality test to every
physician to treat the hypovolemic shock and also
Hypovolemic shock results from depletion of differentiate it from cardiogenic shock.
intravascular volume, whether extracellular fluid
loss or blood loss. The body will compensate with
increased sympathetic tone resulting in increased heart
rate, increased cardiac contractility, and peripheral fin.
vasoconstriction. First there will be change in vital sign
include an increased in diastolic blood pressure with
Case Description narrowed pulse pressure as we found in this patient.
If left untreated, the systolic blood pressure drops as
the volume continues to decrease. As a result, oxygen
Figures
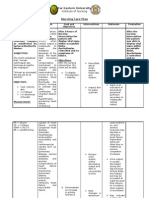
A 21-year-old woman was admitted with altered mental delivery to vital organs is unable to meet oxygen
status after having profuse bleeding due to labor, demand. Cells switch from aerobic metabolism to
vitals sign blood pressure is 70/30, heart rate 170 beat anaerobic metabolism, resulting in lactic acidosis. As
per minute, respiration rate is 32 per minute, body sympathetic drive increases, blood flow is diverted
temperature is 35.9 Celsius. from other organs to preserve blood flow to the heart
and brain. This propagates tissue ischemia and worsen
On systemic examination inferior palpebral lactic acidosis.
conjunctiva was anemic, there was rhonchi on bilateral
thorax and murmur was found along with retraction Furthermore, this condition affected heart
on suprasternal and intercostal, decrease tissue turgor, myocardium. It is undergo what we called stunned
delayed capillary refill time (CRT) and profuse bleeding myocardium, a condition when heart has dysfunction
from vagina. Laboratory finding showed anemia with after having transient ischemia which trigger a
hemoglobin level 5,7 g/dl. Electrocardiogram (ECG) catecholamine-mediated factor which contribute
showed inappropriate sinus tachycardia (IST) before to autonomic dysfunction and potentially induced
and after adequate fluid resuscitation was given. In ED tachycardia and hypotension. All these factors
patient also given a prescription of tranexamic acid contribute to inappropriate sinus tachycardia in this
intravenously to treat the bleeding and vasoactive Figure 1 Monitor ECG when patient was admitted showing IST
patient. Other mechanism which can explain this
agents such as norepinephrine to treat low blood condition is an act from pro-anti-inflammatory agent
pressure. induced by severe bleeding. It could be resulting
in oxidative stress and cardiac dysfunction like
After anemia being corrected with blood hypokinetic of left ventricle (LV). And why in this
transfusion, the patient was underwent emergency patient, after having a correction in fluid and blood
curettage for suspected restrained placenta. At time loss, all the abnormalities was found in physical
when PPH solved, hemodynamic status become stable examination related to cardiomyopathy diminished?.
and ECG is back to sinus rhythm again. The patient The answer is role of innervation of cardiac adrenergic
was discharged on third day after having intensive care and alpha-lipoid-acid (ALA), helps recovery LV in
Figure 2 ECG during resuscitation
and being monitored for her ECG, which shown no stunned myocardium.
abnormalities.
02 03 Figure 3 ECG normal sinus rhythm after resuscitation
[1] Taghavi S, Askari R. Shock, Hypovolemic. StatPearls. 2018
[2] O.N. K, J.D. R, J.E. W, D.T. P, A. C, E.B. V, et al. Shock - Classification and Pathophysiological Principles of Therapeutics. Curr Cardiol Rev. 2019
[3] Rhee JW, Sabatine MS, Lilly LS. “Ischemic heart disease”, in Pathophysiology of heart disease. Baltimore:Lippincott Williams& Wilkins. 2011. pp.144,170
[4] HS L, C H. Stunned Myocardium due to Decompensation from Hypovolemic Shock in a Pregnant Woman with Uterine Atony Following Cesarean Section. J Clin Exp Cardiolog. 2016;07(05):5–9
[5] Depre C, Vatner SF. Cardioprotection in stunned and hibernating myocardium. Heart Fail Rev. 2007
[6] Shavelle DM, Gersh BJ, Bax JJ, Saperia GM. Pathophysiology of stunned or hibernating myocardium. 2017
[7] Camici PG, Prasad SK, Rimoldi OE. Stunning, Hibernation, and Assessment of Myocardial Viability. Circulation [Internet]. 2008;117(1):103–14 [accessed: June 2019]
Available from: https://www.ahajournals.org/ doi/10.1161CIRCULATIONAHA.107.702993
[8] Binz S, McCollester J, Thomas S, Miller J, Pohlman T, Waxman D, et al. CRASH-2 Study of Tranexamic Acid to Treat Bleeding in Trauma Patients: A Controversy Fueled by Science and Social Media.
J Blood Transfus. 2015;2015(2):1–12
[9] Roberts I, Shakur H, Coats T, Hunt B, Balogun E, Barnetson L, et al. The CRASH-2 trial: A randomised controlled trial and economic evaluation of the effects of tranexamic acid on death, vascular occlusive
events and transfusion requirement in bleeding trauma patients. Health Technol Assess (Rockv).2013
[10] Herget-Rosenthal S, Saner F, Chawla LS. Approach to Hemodynamic Shock and Vasopressors. Clin J Am Soc Nephrol. 2008;3(2):546–53.
[11] He B, Kong L, Ge J. Viewpoint Cardiogenic Shock : Dopamine or Norepinepherine ? It ’ s a question. Cardiol Plus Mar. 2017;2(1):2–5
[12] Hollenberg SM. Vasoactive drugs in circulatory shock. Am J Respir Crit Care Med. 2011;183(7):847–55.
[13] VanValkinburgh D, McGuigan JJ. Inotropes And Vasopressors. [Updated 2019 Mar 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. [accessed: June 2019] Available from:
https://www.ncbi.nlm.nih.gov/books NBK482411/
S-ar putea să vă placă și
- Orthostatic Hypotension: Causes, Tests, and Treatment OptionsDe la EverandOrthostatic Hypotension: Causes, Tests, and Treatment OptionsÎncă nu există evaluări
- Case Study of Atherosclerosis 1. Risk Factors of AtherosclerosisDocument5 paginiCase Study of Atherosclerosis 1. Risk Factors of AtherosclerosisCarly Beth Caparida LangerasÎncă nu există evaluări
- Nursing Care Plan for HypotensionDocument2 paginiNursing Care Plan for HypotensiondubsÎncă nu există evaluări
- Nursing Care Plan for HypotensionDocument2 paginiNursing Care Plan for HypotensionMae Denn LabordoÎncă nu există evaluări
- Critical care in the emergency department: shock and circulatory supportDocument6 paginiCritical care in the emergency department: shock and circulatory supportPaulHerreraÎncă nu există evaluări
- Pathophysiology Diagnosis and Treatment of Orthostatic Hypotension and Vasovagal Syncope1Document17 paginiPathophysiology Diagnosis and Treatment of Orthostatic Hypotension and Vasovagal Syncope1Idha AÎncă nu există evaluări
- Dialysis hypotension causes and preventionDocument4 paginiDialysis hypotension causes and preventionCathy ManicadÎncă nu există evaluări
- Shock: Rose Ann J. Raquiza-Perante Post Graduate InternDocument53 paginiShock: Rose Ann J. Raquiza-Perante Post Graduate InternRose Ann RaquizaÎncă nu există evaluări
- Chronic Heart Failure: I. Brief Definition Iv. Disease ProcessDocument12 paginiChronic Heart Failure: I. Brief Definition Iv. Disease ProcessJennifer BeguinwaÎncă nu există evaluări
- Chapter 11Document36 paginiChapter 112071317Încă nu există evaluări
- Review of Hypovolemic Shock Causes, Symptoms and TreatmentDocument5 paginiReview of Hypovolemic Shock Causes, Symptoms and TreatmentAndreasÎncă nu există evaluări
- ShockDocument16 paginiShockChristiaan VoslooÎncă nu există evaluări
- Institute of Nursing: Far Eastern UniversityDocument3 paginiInstitute of Nursing: Far Eastern UniversityaleccespirituÎncă nu există evaluări
- Emergency in Pediatrics: Diagnosis and Management of Shock in PediatricsDocument30 paginiEmergency in Pediatrics: Diagnosis and Management of Shock in PediatricsvenyÎncă nu există evaluări
- 2022 Pharmacology s2t2 HeartfailureDocument6 pagini2022 Pharmacology s2t2 Heartfailurejed larsen capulong gavinoÎncă nu există evaluări
- Iadt03i5p345 PDFDocument15 paginiIadt03i5p345 PDFSudhit SethiÎncă nu există evaluări
- Jake Yvan Dizon Case Study, Chapter 49, Assessment and Management of Patients With Hepatic DisordersDocument8 paginiJake Yvan Dizon Case Study, Chapter 49, Assessment and Management of Patients With Hepatic DisordersJake Yvan DizonÎncă nu există evaluări
- Hypovolemic Shock: Dr. Sherwin BuluranDocument8 paginiHypovolemic Shock: Dr. Sherwin BuluranChristian UretaÎncă nu există evaluări
- ShockDocument29 paginiShockKoRnflakes100% (4)
- Notes On ShockDocument9 paginiNotes On ShockViswa GiriÎncă nu există evaluări
- Cardioembolic StrokeDocument3 paginiCardioembolic StrokeJeffri Sofian LeksanaÎncă nu există evaluări
- 001 Chapter 6 Hemodynamic MonitoringDocument18 pagini001 Chapter 6 Hemodynamic MonitoringMahesh Boopathy100% (2)
- Shock BBDocument31 paginiShock BBVirang ParikhÎncă nu există evaluări
- Hypovolemic shock - A reviewDocument4 paginiHypovolemic shock - A reviewAmirullah AbdiÎncă nu există evaluări
- Pamw04 Wanic-Kossowska Czekalski AngDocument5 paginiPamw04 Wanic-Kossowska Czekalski Angiphone6siphone6s 6sÎncă nu există evaluări
- Your Health - 23 March 2021Document5 paginiYour Health - 23 March 2021Times MediaÎncă nu există evaluări
- Shock RosenDocument10 paginiShock RosenJuan GallegoÎncă nu există evaluări
- Sample ChapterDocument14 paginiSample ChaptercpfredÎncă nu există evaluări
- Microcirculatory Changes in Hypovolemic ShockDocument31 paginiMicrocirculatory Changes in Hypovolemic ShockAmaliahHarumiKarimÎncă nu există evaluări
- Meyer2019 HR Dan HFpEFpdfDocument5 paginiMeyer2019 HR Dan HFpEFpdfFaQihuddin AhmadÎncă nu există evaluări
- 2008 2 92 PDFDocument8 pagini2008 2 92 PDFdidiÎncă nu există evaluări
- Managing Orthostatic HypotensionDocument4 paginiManaging Orthostatic HypotensionmuhammadÎncă nu există evaluări
- Hipotensi PDFDocument6 paginiHipotensi PDFimahÎncă nu există evaluări
- 01 Cir 42 2 297Document11 pagini01 Cir 42 2 297Abdurrahman Arsyad As SiddiqiÎncă nu există evaluări
- Inotropes and Vasoconstictor PackageDocument25 paginiInotropes and Vasoconstictor PackageYoussef MokdadÎncă nu există evaluări
- 8 Management of ShockDocument8 pagini8 Management of ShockiisisiisÎncă nu există evaluări
- SHOCK LEC Modified (2nd)Document86 paginiSHOCK LEC Modified (2nd)spanishthingz01Încă nu există evaluări
- Clinmed 21 3 E275Document8 paginiClinmed 21 3 E275Carlos CoronaÎncă nu există evaluări
- Icu 4Document7 paginiIcu 4GemilleDaphneAndradaÎncă nu există evaluări
- Risk For Decreased Cardiac Output: Nursing DiagnosisDocument4 paginiRisk For Decreased Cardiac Output: Nursing DiagnosisRiska RamadaniÎncă nu există evaluări
- DR Anuj Raj BijukchheDocument95 paginiDR Anuj Raj BijukchheMUHAMMAD JAWAD HASSANÎncă nu există evaluări
- Mitchell 2005Document8 paginiMitchell 2005DianÎncă nu există evaluări
- Trisha Anne Real BSN 2-YB-8 Ncma219 Rle: Laboratory Course Task 1Document2 paginiTrisha Anne Real BSN 2-YB-8 Ncma219 Rle: Laboratory Course Task 1AnneÎncă nu există evaluări
- 187 FullDocument8 pagini187 FullRaoulSusanto SusantoÎncă nu există evaluări
- 4.heart Failure HandoutDocument108 pagini4.heart Failure HandoutGetachewÎncă nu există evaluări
- Fluid Overload Contributing To Heart FailureDocument4 paginiFluid Overload Contributing To Heart FailureSholihatul AmaliyaÎncă nu există evaluări
- ShockDocument8 paginiShockАчпже Чпжечу100% (1)
- Hypotension and Shock: A Concise GuideDocument11 paginiHypotension and Shock: A Concise GuideHarest FauziÎncă nu există evaluări
- Chronic Heart FailureDocument90 paginiChronic Heart FailureTemesgenÎncă nu există evaluări
- Shock: Michael A. Puskarich Alan E. JonesDocument9 paginiShock: Michael A. Puskarich Alan E. JonesFarhanÎncă nu există evaluări
- Diagnosis of Circulatory FailureDocument21 paginiDiagnosis of Circulatory FailureQuang Anh LeÎncă nu există evaluări
- Shock Said 20-21Document10 paginiShock Said 20-212859bathinaÎncă nu există evaluări
- IM - Heart Failure Part 1Document6 paginiIM - Heart Failure Part 1Elisha BernabeÎncă nu există evaluări
- B. Create Your Concept Map of The Disorder. Use A Separate Paper For This. Use Short Coupon Bond and Draw Your Concept Map Using This FormatDocument5 paginiB. Create Your Concept Map of The Disorder. Use A Separate Paper For This. Use Short Coupon Bond and Draw Your Concept Map Using This FormatPatricia Jean FaeldoneaÎncă nu există evaluări
- Therapeutics - Gastrointestinal Tract: Heart FailureDocument5 paginiTherapeutics - Gastrointestinal Tract: Heart FailureDarnell DelgadoÎncă nu există evaluări
- Manage Hypovolemic Shock with Early Fluid ResuscitationDocument5 paginiManage Hypovolemic Shock with Early Fluid ResuscitationSafitryÎncă nu există evaluări
- NCP Partial, Micu Medcor DutyDocument7 paginiNCP Partial, Micu Medcor DutyYana PotÎncă nu există evaluări
- Pathology, Diagnosis, Complication, Treatment of Hypertension: A Systemic ResearchDocument7 paginiPathology, Diagnosis, Complication, Treatment of Hypertension: A Systemic ResearchIJAR JOURNALÎncă nu există evaluări
- Cardiovascular System Diseases Part 2Document9 paginiCardiovascular System Diseases Part 2Prince Rener Velasco PeraÎncă nu există evaluări
- ImmerciDocument14 paginiImmercitextilessathishÎncă nu există evaluări
- 04 Worksheet Clariz-A.-DemateraDocument2 pagini04 Worksheet Clariz-A.-DemateraashlijquintanaÎncă nu există evaluări
- Fellowship Course 3 Program v1Document15 paginiFellowship Course 3 Program v1Joice RumondangÎncă nu există evaluări
- Recuperare 1Document3 paginiRecuperare 1Mihnea TurcuÎncă nu există evaluări
- Dr. Ikar J. Kalogjera: Psychiatrist & Clinical Professor of PsychiatryDocument1 paginăDr. Ikar J. Kalogjera: Psychiatrist & Clinical Professor of PsychiatryMWWÎncă nu există evaluări
- Anatomi Dan Fisiologi PerkemihanDocument89 paginiAnatomi Dan Fisiologi Perkemihannia djÎncă nu există evaluări
- Arthrogryposis Multiplex Congenita (AMC) in Siblings - Case Report. First DCMS Annual Research Day, April 7, 2018Document8 paginiArthrogryposis Multiplex Congenita (AMC) in Siblings - Case Report. First DCMS Annual Research Day, April 7, 2018Razi MohdÎncă nu există evaluări
- Systemic in Ammatory Response Syndrome (SIRS) : Where Did It Come From and Is It Still Relevant Today?Document8 paginiSystemic in Ammatory Response Syndrome (SIRS) : Where Did It Come From and Is It Still Relevant Today?Jhanu JaguarÎncă nu există evaluări
- Biosensors 12 00985 v2Document30 paginiBiosensors 12 00985 v2aqsa javedÎncă nu există evaluări
- Coverage Midterm Examination 2021 Drug and Vice ControlDocument4 paginiCoverage Midterm Examination 2021 Drug and Vice ControlTaga Phase 7Încă nu există evaluări
- Asthma Aware KitDocument33 paginiAsthma Aware KitEkzHa Noctis CaeleumÎncă nu există evaluări
- Format HISTORY OF PATIENTDocument4 paginiFormat HISTORY OF PATIENTShiva CharakÎncă nu există evaluări
- Package - Insert - 08586 - H - en - 30427 - CA 19-9 PDFDocument8 paginiPackage - Insert - 08586 - H - en - 30427 - CA 19-9 PDFadybaila4680Încă nu există evaluări
- EHAQ 4th Cycle Audit Tool Final Feb.10-2022Document51 paginiEHAQ 4th Cycle Audit Tool Final Feb.10-2022Michael GebreamlakÎncă nu există evaluări
- Emergency Medical Technician CPGs PDFDocument121 paginiEmergency Medical Technician CPGs PDFAnonymous OdW7ev100% (1)
- CT ScanDocument37 paginiCT ScanBayu Ihkshan Yamada TriatmojoÎncă nu există evaluări
- Supplement-1115 2020Document216 paginiSupplement-1115 2020Laura PaunicaÎncă nu există evaluări
- Global epidemiology of periodontal diseaseDocument16 paginiGlobal epidemiology of periodontal diseaseBrenda Carolina Pattigno ForeroÎncă nu există evaluări
- Bowel ObstructionDocument48 paginiBowel ObstructionPatrick John100% (1)
- MSB Viewing Guide - 0102Document4 paginiMSB Viewing Guide - 0102Jess WestwoodÎncă nu există evaluări
- FNCPDocument3 paginiFNCPLander VirayÎncă nu există evaluări
- Starting Injectable RCN PDFDocument40 paginiStarting Injectable RCN PDFPhilip HartleyÎncă nu există evaluări
- BPH PSPD 2012Document43 paginiBPH PSPD 2012Nor AinaÎncă nu există evaluări
- IM STEP 2 NotesDocument74 paginiIM STEP 2 Notesyanks1120100% (3)
- Psychoeducation: 19 July 2018 Unit VI Topic DiscussionDocument26 paginiPsychoeducation: 19 July 2018 Unit VI Topic DiscussionDana Franklin100% (1)
- 2016 - Byk FotoDocument7 pagini2016 - Byk FotoSyifa IKÎncă nu există evaluări
- Staff Health PDFDocument1 paginăStaff Health PDFJorgeÎncă nu există evaluări
- Owl NecropsyDocument3 paginiOwl Necropsykezia_stephanie_1Încă nu există evaluări
- Prevention of Adverse ReactionsDocument15 paginiPrevention of Adverse Reactionscupuwatie cahyaniÎncă nu există evaluări
- Ten Rules For The Management of Moderate and Severe Traumatic Brain Injury During Pregnancy: An Expert ViewpointDocument11 paginiTen Rules For The Management of Moderate and Severe Traumatic Brain Injury During Pregnancy: An Expert ViewpointKaren Campos GonzalezÎncă nu există evaluări