Documente Academic
Documente Profesional
Documente Cultură
Prelims Week 3 - Urinalysis - Trans
Încărcat de
Loro JD0 evaluări0% au considerat acest document util (0 voturi)
115 vizualizări16 paginiUrinalysis
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentUrinalysis
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
115 vizualizări16 paginiPrelims Week 3 - Urinalysis - Trans
Încărcat de
Loro JDUrinalysis
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 16
SEMINAR 1 o Fasting (2nd morning)
Urinalysis Diabetic monitoring
o Timed specimen
I. Introduction to Urinalysis 24-hour specimen
Composition of Urine Substances that vary
o Water (95%) Start with an empty bladder
o Analytes 12-hour specimen
Organic Used for Addis Count with formalin as preservative
Urea 2-hour post prandial
Creatinine, uric acid, ammonia, nitrogen For monitoring insulin therapy in persons with DM
Inorganic Usually compared with fasting specimens
Chloride Afternoon specimen (2-4 PM)
Sodium, potassium, phosphorus, calcium, magnesium, Used for urobilinogen determination
and iron o Catheterized
o Others Bacterial culture
Hormones, vitamins, medications, formed elements o Midstream clean catch
Specimen Collection & Handling Bacterial culture
o Clean dry container Routine urinalysis
o Label: body of container o Suprapubic aspiration
Patient’s name Bacterial culture
Date & time of collection Cytologic examination
o Should be examined within one hour o Three-glass collection
o Should be refrigerated if not tested within 30 mins of Prostatic infection
collection Drug specimen collection
o Urine culture should be tested within 24 hours if the sample o Chain of custody
is refrigerated at 2-8’ C Correct sample identification from the time of collection
Urine preservatives to the receipt of laboratory result
o Refrigeration o Required amount by DOH: 60 ml (30-45 ml)
Raises specific gravity (urinometer) o Urine temperature: 32.5-37.7’C
Precipitates amorphous Within 4 minutes from the time of collection
o Thymol o DOH directive: waterless urinal
o Boric acid Specimen evaluation
o Formalin o For single specimen submitted for multiple
o Sodium fluoride measurements, bacteriologic exam should be done first
Glucose determination o Proper labeling
Drug analysis Patient’s full name
o Saccomanno’s Date of collection
o Gray C&S tubes (boric acid) Time of collection
Stable at room temperature for 48 hours Urine collection
o Yellow plain UA tube o Visible signs of contamination
Automated instruments o 50 ml disposable container: 10-15 ml of urine
o Cherry red & yellow top tube o Proper specimen for the requested test
Sodium propionate o Any transportation delays
Stable at room temperature for 72 hours
Changes in unpreserved urine II. Physical Examination
Increase Decrease Color
Bacteria Glucose o Normal: straw to amber (light yellow to dark yellow)
Turbidity Ketones o Urochrome: yellow pigment
pH* Bilirubin o Urobilin: orange-brown
Nitrite* Urobilinogen o Uroerythrin: pink to red pigment
Cells & casts o Laboratory correlation of urine color
Routine urinalysis Colorless, straw, pale yellow
o First morning samples Dilute
o Concentrated acidic urine Polyuria
o Casts dissolve in dilute alkaline urine Diabetes insipidus
Types of urine specimen Diabetes mellitus
o Random specimen Dark yellow
Routine screening Concentrated
o First morning First morning specimen
Concentrated After strenuous exercise
Ideal for routine urinalysis
Pregnancy test
Amber/orange Radiographic contrast media
Yellow foam (+) bilirubin Talcum and vaginal creams
Orange with foam Pathologic
Pyridium (phenazopyridine) RBCs (>500 RBCs/μl)
With thick orange pigment WBCs (>200 WBCs/μl)
White foam Bacteria
Protein Yeast
Red/pink (pathologic) Non-squamous epithelial cells
Hematuria Hgbnuria Myoglobinuria Abnormal crystals
Blood test + + + Lymph fluid
Transparency Turbid or Clear Clear Lipids
cloudy Odor
Plasma color Pale yellow Red Pale yellow o Normal odor
RBCS Faint, aromatic (fresh specimen)
microscopically o Characteristic urine odors
Red/pink (non-pathologic) Ammoniacal: bacterial contamination
Porphyrins Sweet/fruity: diabetic acidosis
o Blood test (-) Pungent: asparagus
o Reddish purple color or port wine Sweaty feet: isovaleric & glutaric acidemia
o Schwartz Watson (+) Maple syrup: MSUD
o Fluorescence (+) Cabbage: methionine malabsorption
Blackberries Mousy: phenylketonuria
o Acid urine Rotting fish: trimethylaminuria
Beets Rancid: tyrosinemia
o Alkaline urine of genetically susceptible persons Volume
Rifampin o Normal values
Menstrual contamination Adults
o Cloudy with RBCs and mucus clots Average: 1200-1500 ml
Brown/black Range: 600-2000 ml
RBCs oxidized to methemoglobin Night urine in general is not in excess of 400 ml
o Acidic urine o Factors that influence urine volume
o Blood test (+) Fluid intake
Homogentisic acid (alkaptonuria) Fluid loss
o Alkaline urine Variations in ADH secretions
Melanin Necessity to excrete increased amounts of dissolved
o Reacts with nitroprusside and ferric chloride solids
Methyldopa/levodopa o Nocturia
Metronidazole (Flagyl) More than 500 ml with a specific gravity of less than
Clarity 1.018 at night
o Urine clarity o Oliguria
Clear: transparent Excretion of less than 500 ml of urine daily
Hazy: print easily seen o Anuria
Cloudy: print blurred Complete or total suppression of urine formation
Turbid: print can’t be seen Specific gravity
Milky: may precipitate o Density of substance compared with density of H2O at
o Bacterial growth specified temperature
Uniform opalescence o Proportion of dissolved solid components to total volume
Not removed by filtration nor acidification of the specimen
o Leukocytes o Reflects the density of the specimen
White cloud (remains after acidification) o Evaluates the kidney’s ability to reabsorb
o Urates o Detects possible dehydration or abnormalities in ADH
Pink cloud secretion
o Uric acid o Aids in evaluating the concentrating and diluting abilities
Orange cloud of the kidneys
o Causes of turbid urine o Clinical correlations
Non-pathologic Normal values
Squamous epithelial cell Average: 1.016-1.022
Mucus Range: 1.003-1.035
Amorphous urates/phosphates Isosthenuric: specific gravity is 1.010
Semen Hyposthenuric: specific gravity is below 1.010
Fecal contamination Hypersthenuric: specific gravity is above 1.010
Excretion of radiographic contrast media and dextran o No temperature corrections are required
will give a very high urine specific gravity reading (over o Simple to operate
1.035) o Gives rapid reliable results
o Methods Reagent strip (dipstick)
Urinometry Principle: pKa change of polyelectrolytes in relation to
Uses urinometer or hydrometer ionic concentration of urine
Principle: water displacement or buoyancy Inc. specific gravity: increased H+ released, low pH
Disadvantage: requires 10-15 ml (acidic): yellow color
Accuracy may be checked by measuring the specific Dec. specific gravity: less H+ released, high pH
gravity of: (alkaline): blue color
o Distilled water: 1.000 Main components in the reagent area
o Potassium sulfate: 1.015 o Polyelectrolytes
Reading is affected by: o Indicator: bromthymol blue
o Temperature o Buffer
Subtract 0.001 from the reading for every 3 Results
degrees centigrade that the specimen o Blue (1.000) through shades of green to yellow
temperature is below the urinometer temperature (1.030)
Add 0.001 to the reading for every 3 degrees o Color chart provided indicates values of 1.000-
centigrade that the specimen temperature is 1.030 in increments of 0.005
above the urinometer temperature Reaction interferences
o Glucose o Measures only ionic solutes
Subtract 0.004 for every gram of glucose/dl of o Not affected by urea, glucose, radiographic media
urine o Falsely elevated: high concentration of protein
o Protein o Falsely decreased: highly alkaline urine
Subtract 0.003 for every gram of protein/dl of Harmonic oscillation densitometry
urine Sound wave frequency and automated instruments
Specific gravity correction A volume of urine is maintained in a U-shaped tube
o Temperature and a sound wave of fixed frequency is transmitted to
Specific gravity: 1.035, UT: 20’C, ST: 8’C one end of the tube
Find the difference: 20 - 8=12 Specific gravity is directly related to the change in
Divide by 3: 12 / 3=4 frequency recorded as the sound wave exits the other
Multiply by 0.001: 4 x 0.001=0.004 end of the tube
Add/subtract to or from the specific gravity: 1.035 Falling drop
- 0.004=1.031 Timing the fall of a drop of body fluid of known size
o Protein & glucose through a definite distance in a mixture
A specimen containing 2 g/dl of protein and 1 g/dl Heavier drop will fall faster
of glucose has a specific gravity of 1.035
1.035 – 0.006 (protein) – 0.004 (glucose) = 1.025 III. Routine Chemical Examination
o Dilution Reagent strips
Insufficient amount of urine or specific gravity o Plastic strips that contain one or more chemical-
readings greater than the scale can be diluted and impregnated absorbent pads
retested o Procedure
Multiply the decimal factor by the dilution factor Mix urine
to get the actual specific gravity reading Insert reagent strip
Dilution factor is computed by dividing the Remove excess urine
volume of specimen and water by the volume of Time according to manufacturer’s directions
specimen alone Compare test areas closely with corresponding color
Refractometry charts
Determines the concentration of dissolved particles in Hold strip horizontally and close to the color blocks
a specimen by measuring the refractive index o Storage and general precaution
o Refractive index is the comparison of the velocity of Must be kept with desiccant in opaque, tightly-capped
light in air with the velocity of light in a solution containers
o Total solids meter Store the container preferably at room temperature
Refractometer may be calibrated using the following: Keeps trips in their original container
o Distilled water: 1.000 Do not expose the strips to volatile fumes
o 5% NaCl: 1.022 Do not touch the test areas
o 9% sucrose: 1.034 Do not use if the chemical pads become discolored
o The specific gravity reading on the refractometer is Do not use past the expiration date
generally slightly lower than a urinometer reading by o Sources of error
about 0.002 Unmixed specimen
Advantages Strip in urine for extended period
o Uses small amount of urine (1-2 drops) Leaching of reagents from the pad
Excess urine in the strip (run-over between chemicals) o Important renal marker
Distortion of colors o Most of the albumin: not filtered
Blot the edge of the strip o Filtered albumin: reabsorbed by tubules
Hold horizontally o Other proteins in urine
Refrigerated specimen Microglobulins
False negative Tamm-Horsfall glycoprotein
o Quality control o Postural/orthostatic proteinuria
Newly opened bottles of reagent strips should be tested Urine CHON: (+) day, (-) night
with known positive or negative controls First voided urine: (-) CHON
Should be tested with known positive and negative 2 hours standing or walking: (+) CHON
controls daily Exaggerated lordotic posture
pH o Accidental or false or pseudoproteinuria
o Reflects the ability of the kidney to maintain normal Urine is contaminated directly or indirectly with
hydrogen ion concentration in plasma and extracellular albuminous fluids, pus cells, blood, vaginal discharge
fluid Examples: vaginitis and cystitis
o To maintain acid-base balance in the body o Pathologic proteinuria
o Blood must buffer and eliminate excess acids Renal diseases and indicates increased permeability of
o Buffering capacity of blood depends on bicarbonate ions the glomerular filter
(HCO3-) Causes of pathologic proteinuria
o Secretion of hydrogen ions causes reabsorption of Pre-renal
bicarbonates o Multiple myeloma (Bence Jones Protein)
o Acid-base balance o Intravascular hemolysis
Secretion of hydrogen in the form of ammonium ions, o Acute phase reactants
hydrogen phosphate, and weak organic acids Renal
H+ + ammonia = ammonium ions o Glomerular disorders
H+ + phosphate = hydrogen phosphate o Tubular proteinuria
By the reabsorption of bicarbonate from the filtrate in o Orthostatic proteinuria
the PCT o Microalbuminuria
o Normal values o Pre-eclampsia
First morning: 5.0-6.0 Post-renal
Random: 4.5-8.0 o Lower UTI
o Urine pH o Menstrual contamination
Acid urine o Vaginal secretions
Increased protein o Vaginal inflammation
Cranberries o Prostatitis
Acid-producing bacteria (E. coli) o Acid precipitation techniques
Starvation Heat and acetic acid
Dehydration Principle: urine is coagulated by heat and precipitated
by acetic acid (5-10%)
Diarrhea
Sulfosalicylic acid test (Exton’s)
Diabetes mellitus
Alkaline urine Positive result: precipitation
Grade Turbidity Protein Range
Increased consumption of fruits and vegetables
in mg/dl
Citrus fruits
NEG No inc. in turbidity <6
Less acidic after meal (alkaline tide)
TRACE Noticeable turbidity 6-30
Renal tubular acidosis
1+ Distinct turbidity with 30-100
Urease-producing bacteria
no granulations
Hyperventilation
2+ Turbidity with 100-200
Old specimen
granulations and no
o Reagent strip
flocculation
Principle: double indicator system (methyl red &
3+ Turbidity with 200-400
bromthymol blue)
granulation and
Indicators
flocculation
Methyl red (red to yellow): pH 4-6
4+ Clumps of protein >400
Bromthymol blue (yellow to blue): pH 6-9
Causes of error
Results
False negative
Orange to green to blue as pH increases
o Highly alkaline urine
Protein
False positive
o Normal values
o Iodinated dyes (x-ray contrast media)
100 mg of protein in 1 day (150 mg)
o Penicillin
Average random: 2-10 mg/dl
o Salicylate
Clinical proteinuria: >30 mg/dl
o Tolbutamide
o Reagent strip Glucose
Principle: protein error of pH indicators o Detectable amount of glucose in urine: glucosuria
Indicators change in color in the presence of protein o Renal threshold: 160 mg/dl to 180 mg/dl
(pH is constant at 3.0) Blood level at which tubular reabsorption stops
Protein (anion) accepts ions from the indicator o Hyperglycemia-associated glucosuria
Albumin contains more amino groups which allows it to Diabetes mellitus
readily accept H+ as compared to other proteins Pancreatitis
Indicator: tetrabromphenol blue Pancreatic cancer
Results Acromegaly
Positive result: green then blue Cushing’s syndrome
Negative result: yellow Hyperthyroidism
Reaction interferences Pheochromocytoma
False positive CNS damage
o Highly buffered alkaline urine Stress
o High specific gravity Gestational diabetes
o Quaternary ammonium compounds o Renal-associated glucosuria
o Bence Jones proteinuria Fanconi’s syndrome
Associated with: Advanced renal disease
Multiple myeloma Osteomalacia
o Malignant disorder that results in infiltration of Pregnancy
bone marrow by plasma cells o Copper reduction method
Macroglobulinemia Ability of glucose to reduce copper sulfate to cuprous
Malignant lymphomas oxide in the presence of alkali and heat
Coagulates between 40’C and 60’C Benedict’s test
Dissolves at 100’C Benedict’s reagents
Methods o Copper sulfate
Heat and acetic acid test o Sodium hydroxide
Bradshaw o Sodium carbonate
Toluene sulfonic acid (TSA) test o Citric acid
Electrophoresis Negative Blue
o Indicated by single sharp peak in γ-globulin region Trace Green without precipitate
o Best method 1+ Green with yellow precipitate
Immunofixation electrophoresis (IFE) 2+ Yellow green with yellow precipitate
o Microalbuminuria 3+ Muddy orange with yellow precipitate
Albumin in urine above the normal level but below the 4+ Orange to red precipitate
detectable range of the reagent strip Clinitest
Predictor of clinical nephropathy in insulin-dependent Principle: copper reduction
diabetes mellitus (diabetic nephropathy) Store in dry environment, away from sunlight
Methods Normal appearance: spotted bluish white tablet
Radioimmunoassay o Discard if tablet turns dark blue to brown
Fluorescent and enzyme immunoassay Clinitest reagents
Nephelometry o Copper sulfate
Micral II test strip o Sodium hydroxide
o Immunologic test (EIA) o Sodium carbonate
o Procedure o Sodium citrate
Dip strip into the urine for 5 seconds Self-heating (hydrolysis of sodium hydroxide and its
Stand for 1 minute reaction with sodium citrate)
o Positive result: pink to red color Positive result: blue to orange/red color
Immunodip Pass-through phenomenon: >2 g/dl of sugar
o Immunologic test (immunochromatography) Five-drop method Two-drop method
Clinitek microalbumin 5 drops of urine and 10 2 drops of urine and 10
o Dye-binding method drops of water drops of water
o Reported as albumin:creatinine ratio Negative Negative
Multistix pro Trace 0.25 g/dl Trace
o Reported as albumin:creatinine ratio 1+ 0.5 g/dl 1+ 1 g/dl
o Correlation of reagent strip and heat & acetic acid test: 2+ 0.75 g/dl 2+ 2 g/dl
Reagent Heat & Interpretation 3+ 1.0 g/dl 3+ 3 g/dl
strip HOAc 4+ 2.0 g/dl 4+ 5 g/dl
+ - Albumin present o Reagent strip
+ + Proteinuria Specific for glucose only
- + Bence Jones proteins, globulins Principle: double sequential enzyme
Oxidase and peroxidase Non-diabetic ketonuria
Glucose + O2 glucose oxidase gluconic acid + H2O2 Acute febrile disease and toxic states accompanied by
H2O2 + chromogen peroxidase ox. chromogen + H2O vomiting or diarrhea
Reaction interferences o Reagent strip
False positive Only detects acetoacetic acid
o Oxidizing cleaning agents (peroxide) Acetone is measured upon addition of glycine and alkali
False negative Beta-hydroxybutyric acid cannot be measured
o Vitamin C Principle: sodium nitroprusside reaction or sodium
o Upon standing nitroferricyanide reaction
o High specific gravity Acetoacetic acid + sodium nitroprusside
Types of reagent strips violet/purple color
Reagent strips differ in chromogen used Positive result: violet/purple color
Multistix Types of reagent strips
o Potassium iodide chromogen Chemstrip
o Positive result: color changes from blue to green to o Sodium nitroferricyanide and glycine
brown in 30 seconds o Measures acetoacetic acid and acetone
Chemstrip Multistix
o Aminopropyl-carbazol o Measures acetoacetic acid only
o Positive result: yellow to orange brown o Nitroprusside tablet test (Acetest)
Clinistix Glycine-impregnated
o O-toluidine chromogen Measures acetoacetic acid and acetone
o Positive result: pink to purple Used if urine has interfering color
Reporting of results Sensitive to humidity
Negative Acetest tablet
Trace 100 mg/dl Sodium nitroprusside
1+ 250 mg/dl Glycine
2+ 500 mg/dl Lactose
3+ 1000 mg/dl Specimen
4+ >2000 mg/dl Whole blood
o Correlation of glucose oxidase and Benedict’s test: Plasma
Reagent Benedict’s Interpretation Urine
strip test Positive result: lavender to deep purple
1+ - Glucose (small amount) Blood
+ + Glucose and reducing sugars Hematuria Hgbnuria Myoglobinuria
- + Non-glucose reducing sugars Urine Smoky, Clear, pink Clear, red to
3+ - Oxidizing agents pink to to red to brown
brown, lots brown,
IV. Special Chemical Examination of RBCs occasional
RBCs
Ketone bodies
o Products of incomplete fat metabolism Plasma Normal Pink Normal
Defect in CHO metabolism Haptoglobin Normal Decreased Normal
Inadequate CHO in diet CK Normal Normal High
o Ketones Aldolase Normal Normal Increased
Acetone (2%) o Hematuria
Acetoacetic/diacetic acid (20%) Blood cells in urine
Measured in reagent strip Relatively common
Beta-hydroxybutyric acid (78%) Smoky, cloudy urine
o Clinical significance of urine ketones Causes
Diabetic acidosis Renal calculi (most common cause)
Insulin dosage monitoring IgA nephropathy
Starvation Glomerulonephritis
Excessive carbohydrate loss Pyelonephritis
Malabsorption/pancreatic disorders Trauma
Strenuous exercise Tumors
Vomiting Exposure to toxic chemicals
o Ketonuria Excessive exercise
Diabetic ketonuria o Hemoglobinuria
Uncontrolled diabetes and presence of ketoacidosis Free hemoglobin in urine (>50 mg/dl)
or ketosis Uncommon
Warning of impending coma Clear red urine
Test ketonuria (>1-2 g/dl glucose) Positive for intravascular hemolysis
Causes o Blondheim ammonium sulfate test
Transfusion reactions 5 ml urine with ammonium sulfate
Hemolytic anemias Centrifuge
Severe burns Results
Malaria Myoglobin: colored (red) supernatant
Strenuous exercise/red cell trauma Hemoglobin: colorless supernatant
Brown recluse spider bites Hemoglobinuria Myoglobinuria
o Myoglobinuria Clear, red urine with red Clear, red urine with pale
Myoglobin in urine plasma yellow plasma
Rare Associated with Associated with
Clear red urine transfusion reaction rhabdomyolysis
Acute destruction of muscle fibers after trauma Precipitated by ammonium Not precipitated by
Rhabdomyolysis sulfate ammonium sulfate
Associated with acute renal failure Produces hemosiderin
Presence of red-brown pigment granules (yellow-brown
Marathon, karate granules) in urinary
Patient is positive for muscle tenderness sediments (indicative of
Causes previous bleeding)
Muscular trauma/crush syndromes Bilirubin
Prolonged coma o B2 or conjugated bilirubin seen in urine
Convulsions o Clinical significance
Muscle-wasting diseases Hepatitis
Alcoholism Liver cirrhosis
Drug abuse Other liver disease
Extensive exertion Biliary obstruction (gallstones, cancer)
Statin medication (lowers cholesterol) o Reagent strip
Laboratory findings Principle: Diazo reaction
Urine Coupling reaction of bilirubin with diazonium salt in
o Red-brown urine (cola drink) acid solution forming azobilirubin
o Positive for hemoglobin and protein Results
o Few RBCs Positive result (Multistix): buff to tan
Serum Positive result (Chemstrip): pink to violet
o Clear, increased creatine kinase and aldolase Reaction interference
o Normal haptoglobin False positive
o Reagent strip o Highly pigmented urine (phenazopyridine)
Positive in hemoglobinuria, myoglobinuria, and o Indican
hematuria (in well mixed urine) False negative
Principle: pseudoperoxidase activity of hemoglobin o Exposure to light
H2O2 + chromogen hemoglobin/peroxidase oxidized o Ascorbic acid (competes with bilirubin in Diazo)
chromogen + H2O o Increased nitrite (competes with bilirubin in Diazo)
Indicator: tetramethylbenzidine o Ictotest
Results Confirmatory test for bilirubin
Positive result: green to blue More sensitive than the reagent strip
o Intact RBCs: speckled green Ictotest: 0.05-0.10 mg/dl
Negative result: yellow Reagents trip: 0.40 mg/dl
Reaction interferences Principle: bilirubin reacts with p-nitrobenzene
False positive diazonium p-toluene sulfonate
o Strong oxidizing agents (hypochlorite/bleach) Procedure
o Bacterial peroxidases Add 10 drops of urine to the mat
False negative Put the tablet on the mat
o High specific gravity Add 1 drop of water
o Crenated cells (non-hemolyzed) Wait for 5 seconds
o Formalin (reducing agent) Add 1 drop of water
o Increased nitrite Positive result: blue or purple color
o Increased ascorbic acid o Other tests for bilirubin
o Captopril (anti-hypertensive drug) Gmelin
o Methods Smith
Guaiac Foam
Orthotolidine Fouchet
Benzidine
Teichman
Urobilinogen Hoesch reagent: Ehrlich reagent in 6 M HCl
o Product of conversion of bilirubin in intestine Positive result: red
o ½ goes to feces and becomes urobilin (pigmentation) Urobilinogen is inhibited by the highly acidic pH (only
Urobilin normal value: <0.02 mg/dl stable in alkaline urine)
o ½ goes back to liver and is transported in small amounts Nitrite
to the kidney o Indirect test for UTI
o Normal values o Reduced form of nitrate
<1 mg/dl or Ehrlich unit (8 mg/dl) o Process initiated by certain bacteria such as E. coli,
o Colorless and labile Klebsiella, Enterobacter, Proteus, Staphylococci
o Increased in alkaline urine (not stable in acid urine) o Specimen: first morning mid-stream catch
o Clinical significance o Clinical significance
Early detection of liver disease Cystitis
Liver diseases Pyelonephritis
Hemolytic disorders Evaluation of antibiotic therapy
o Urine bilirubin & urobilinogen in jaundice Monitoring of patients at high risk for UTI
Urine bilirubin Urine urobilinogen Diabetic patients and pregnant women
Obstructive jaundice / 3+ Normal Screening of urine culture specimen
post-hepatic jaundice o Method: depends on the conversion of nitrate to nitrite
Liver damage + or - 2+ o Requires overnight bladder incubation (min. 4 hours)
Hemolytic jaundice Negative 3+ o Positive result: do culture
o Reagent strip
Jaundice Conditions Urine Urine Fecal Principle (Multistix): Greiss reaction
bilirubin urobilinogen color P-arsinilic acid + nitrite in acid pH produces
Pre- Hemolytic Negative Increased Normal diazonium salt and tetrahydrobenzoquinolin thus
hepatic disorders, to dark forming a pink azo dye
ineffective brown Positive result: pink
erythropoiesis Reaction interferences
Hepatic Hepatitis, Positive Normal to Normal False positive
cirrhosis increased o Improperly preserved specimen
Post- Gallstones, Positive Decreased to Pale o Highly pigmented urine
hepatic tumor absent chalky False negative
acholic o Non-reductase containing bacteria
o Ehrlich test o Ascorbic acid
Principle: Ehrlich’s reaction o Lack of nitrate in diet
Ehrlich’s reagent reacts with urobilinogen and other o Insufficient contact time
chromogens producing urobilinogen aldehyde o Large quantities of bacteria
Ehrlich’s reagent: p-dimethylaminobenzaldehyde Leukocyte Esterase
Positive result: cherry red color o Indirect test for UTI
o Reagent strip o Human neutrophil primary granule has esterolytic
Principle: Ehrlich aldehyde reaction activity
Formation of red azo dye o Sensitivity: 5-15 WBCs/hpf
Results o Positive result in either intact or lysed
Positive result (Multistix): PDAB produces red color o Longest reaction time: 2 minutes
Not specific to urobilinogen, fresh urine needed o Reagent strip
Reaction interferences Principle: neutrophilic esterases catalyze the hydrolysis
False positive of ester to produce an aromatic compound and an acid
o Porphobilinogen, sulfonamide, procaine, 5HIAA, Indoxylcarbonic acid ester with leukocyte esterase
indole, methyldopa produces acid indoxyl and diazonium salt thus
o Highly pigmented specimen producing a purple azo dye
False negative Positive result: purple
o Old specimen Purple intensity is proportional to the number of
o Formalin preservation WBCs present
o Watson Schwartz differentiation test Reagent: derivatized pyrrole AA ester, diazonium salt
Urobilinogen Reaction interferences
Soluble in both chloroform and butanol False positive
Red chloroform and butanol layers o Contamination with vaginal fluid
Porphobilinogen o Trichomonas, eosinophil
o Strong oxidizing agents
Insoluble in both chloroform and butanol
o Formalin
Colorless chloroform and butanol layers
o Hyperpigmented urine
o Hoesch test
False negative
Screening test for porphobilinogen
o Vitamin C
Other UTI tests o Gives false negative reaction in the following reagent
o Rapid diagnostic: urine lactoferrin (WBC granule testing) strip tests:
o Rapid confirmatory: microscopic exam (bacteria & WBC) Glucose
o Gold standard: culture (colony forming units) Blood
Ascorbic acid Bilirubin
o 11th parameter Nitrite
Leukocyte esterase
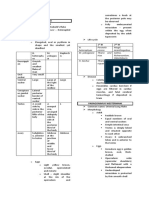
Parameter Reading time Principle Reagents (Multistix) Positive result
Leukocyte esterase 2 minutes Granulocytic esterase reaction Derivatized pyrrole AA ester, Purple
diazonium salt
Nitrite 60 seconds Griess reaction P-arsinilic acid, diazonium, Pink
tetrahydrobenzoquinolin-3-
ol
Urobilinogen 60 seconds Ehrlich reaction P- Red
dimethylaminobenzaldehyde
Protein 60 seconds Protein error of indicators Tetrabromphenol blue Green to blue
pH Timing not critical Double indicator system Methyl red, bromthymol blue Orange-yellow-
green-blue
Blood 60 seconds Pseudoperoxidase activity of Diisopropyl-benzene Green to blue green
hemoglobin dehydroperoxide,
tetramethylbenzidine
Specific gravity 45 seconds pKa change of polyelectrolytes Bromthymol blue Blue to green to
yellow
Ketones 40 seconds Sodium nitroprusside reaction Sodium nitroprusside Pink to purple
Bilirubin 30 seconds Diazo reaction 2-4-dichloroaniline Buff to tan
diazonium salt
Glucose 30 seconds Double sequential enzyme Glucose oxidase, peroxidase, Green to brown
reaction potassium iodide
Parameter False positive reactions False negative reactions
Leukocyte esterase Strong oxidizing agent, formalin, highly pigmented Increased concentration of protein, glucose, ascorbic
urine acid
Nitrite Improperly preserved specimen, highly pigmented Non-reductase bacteria, insufficient contact time, lack of
urine urinary nitrate, bacteria (conversion of nitrite to
nitrogen), increased ascorbic acid and specific gravity
Urobilinogen Porphobilinogen, indican, sulfonamide, highly Old specimen, formalin preservation
pigmented urine
Protein Highly buffered alkaline urine, pigmented Proteins other than albumin, microalbuminuria
specimen (phenazopyridine), quaternary
ammonium compounds, high specific gravity
pH No known interfering substances, run-over from
adjacent pads, old specimen
Blood Strong oxidizing agent, bacterial peroxidases High specific gravity, crenated cells, formalin, increased
nitrite, increased ascorbic acid
Specific gravity High concentration of protein Highly alkaline urine
Ketones Highly pigmented urine, phtalein dyes Improperly preserved specimen
Bilirubin Highly pigmented urine (phenazopyridine), Exposure to light, ascorbic acid, increased nitrite
indican
Glucose Oxidizing agents Increased ascorbic acid, increased ketones, increased
specific gravity, low temperature, improperly preserved
specimen
V. Microscopic Examination (+) nitrite
Procedure Increased pH
o Place 10-15 ml (12 ml) of mixed urine in a test tube o Neutrophils
o Centrifuge for 5 mins at 1500-2500 rpm or 400 RCF Spherical
o Decant (volume of sediment: 0.5-1 ml) and flick tube Granular cytoplasm
o Place a drop on a slide (0.02 ml) and cover with cover slip 12-14 μm
o Examine under LPO then HPO Multi-lobed nucleus
o Observe in 10-20 fields Confused as RTEs and RBCs
Reference intervals Dilute acetic acid enhances nuclear detail
Component Number Magnification o Glitter cells
RBC 0-2 HPF WBCs in dilute or hypotonic urine
Neutrophils swell and cytoplasmic granules show
WBC 0-5 HPF Brownian movement
Hyaline cast 0-2 LPF WBC lysis: alkaline and hypotonic urine
Squamous EC Few LPF o Eosinophils
Transitional EC Few HPF Not normally seen in urine
Stains
Renal Tubular EC 0-2 HPF Hansel stain
Bacteria & yeast Negative HPF o Preferred
RBCs o Uses methylene blue in eosin Y
o Appearance Wright
Non-nucleated C/S tubulointerstitial disease
Biconcave disk (7 μm) Hypersensitivity to drugs (penicillin, drug-induced
Hypertonic, concentrated urine: crenated interstitial nephritis)
Hypotonic, dilute urine: ghost/shadow cell o Clinical significance
o Sources of identification error Pyuria
Yeast cells Increase in urinary WBCs
Oil droplets Infection or inflammation
Air bubbles Renal origin if with WBC casts
WBCs Bacterial infections
o Reporting Pyelonephritis
Average/10 hpf Cystitis
Normal value: 0-2/hpf Prostatitis
o Correlation Urethritis
Color
Acute urethral syndrome
Blood reagent strip
Dysuria (painful urination), pyuria
o Dysmorphic RBC
Non-bacterial disorders
RBC with protrusion or fragmentation
Glomerulonephritis
Renal/glomerular bleeding
Wright’s stain: hypochromic with presence of cellular Lupus erythematosus
blebs and protrusions Interstitial nephritis
o Clinical significance Tumors
Glomerular membrane damage (glomerulonephritis) Epithelial cells
Vascular injury within the GUT (trauma, acute o Squamous epithelial cells
infection/inflammation, and coagulation disorders) Largest, most frequently seen, least significant
Renal calculi 40-60 μm
Most common Large, flat, abundant cytoplasm with small, round,
Clumping of crystals and hematuria central nuclei
Malignancy Sternheimer malbin stain: pink
Increased RBCs and RBC casts: renal bleeding Location: distal 1/3 of urethra, vagina, vulva
(glomerular bleeding or nephritis) Sources of identification error
Increased RBCs but no RBC casts: bleeding distal to the Folded cells may resemble casts
kidney (cystitis) Reporting
Leukocytes/pus cells Rare, few, moderate, many (per lpf)
o Sources of identification error Correlation
RTEs Clarity
RBCs (add acetic acid to dissolve RBC) Clue cells
o Reporting Abnormal
Average/10 hpf Squamous EC coated with Gardnerella vaginalis
Normal value: 0-5/hpf o Transitional epithelial (uroepithelial) cells
o Correlation Small, round, pear-shaped, central nucleus
(+) leukocyte esterase Sometimes binucleated
Less coarse granules o Formed when protein precipitates and gels in the lumen
20-40 μm o Cylindrical with parallel sides and rounded ends
Few in normal urinalysis o Sole site: kidney
Location: upper urethra, bladder, ureters, renal pelvis o Tamm-Horsfall protein (uromodulin)
Caudate Matrix of all casts
Transitional epithelium with saw-tooth tail Meshwork traps cells
Found in the urinary bladder and pelvis of the kidney Produced by RTEs
Clinical significance o Increased cast formation
Transitional cell carcinoma Lower pH (acidic)
o (+) large clumps Increased ionic concentration
Renal transplantation rejection Obstruction and stasis
Catheterization Proteinuria (increased albumin and globulin)
Malignancy or viral infection Plasma proteins combine with Tamm-Horsfall
o With vacuoles and irregular nuclei o Urinary casts
o Renal tubular epithelial cells Cylindroiduria or cylindruria
Most significant type of epithelia cell in urine Presence of casts in urine
Large nuclei with coarse granules Formed at the junction of DCT and Loop of Henle
Reporting o Cast formation
Average/hpf Aggregation of Tamm-Horsfall protein into protein
Normal value: 0-2/hpf fibrils attached to RTEs
RTE from PCT Interweaving of protein fibrils
Larger than other RTEs Further protein fibril interweaving to form solid
structure
Rectangular shape
Possible attachment of urinary elements to solid matrix
Columnar or convoluted
Detachment of protein fibrils from the epithelial cell
Coarsely granulated cytoplasm
Excretion of the cast
Resembles casts Cellular cast coarse granular cast fine granular
RTE from DCT
cast waxy cast
Occur singly (14-16 μm) o Hyaline cast
Oblong or egg-shaped cells with coarse granules Non-pathologic
RTE from collecting tubules Most frequently seen
12-20 μm Entirely Tamm-Horsfall
Cuboidal or polygonal with slightly eccentric nucleus Translucent, low refractive index
Nuclei make up 60-70% of the cells Difficult to visualize under the microscope
Clinical significance Appearance
C/S Colorless, homogenous matrix
Increased in acute tubular necrosis Sources of identification error
Tubular damage Mucus, fibers, hair, increased lighting
Drug and heavy metal poisoning Reporting
Viral infection (CMV) Average number per lpf
Pyelonephritis Normal value: >0-2/lpf
Allergic reactions Correlation
Acute allogenic transplant rejection Protein
Oval fat bodies Blood (exercise)
Lipid-containing RTE cells Color (exercise)
Highly refractile, nuclei difficult to observe Clinical significance
Usually seen with free-floating fat droplets Stress and exercise
Identification Heat exposure
o Staining with Sudan III or Oil Red O produces Fever
orange-red droplets Glomerulonephritis
o Polarized microscopy (Maltese cross formations) Pyelonephritis
Reporting Congestive heart failure
o Average number per hpf o Less renal blood flow and urine output
Bubble cells Athletic pseudonephritis
Degenerated renal tubular epithelial cells o In collaboration with RBC casts
RTE cells containing large, non-lipid-filled vacuoles o Waxy cast
Seen in acute tubular necrosis Non-pathologic
May be seen along with normal renal tubular Final phase of dissolution of fine granules of finely
epithelial cells and oval fat bodies granular casts
Casts CRF, become denser: waxy
o Formed within the lumen of the DCT and collecting duct Brittle: cracks
Area of concentration where most casts are formed High refractive index
Sources of identification error Correlation
Fibers and fecal material o WBCs
Reporting o Protein
Average number per lpf o Leukocyte esterase
Correlation Clinical significance
Protein o Infection or inflammation within the nephron
Cellular casts o Pyelonephritis
Granular casts o Acute interstitial nephritis
WBCs RTE casts
RBCs Hard to differentiate from WBC cast
Clinical significance Most reliable: singular round nuclei
Tubular inflammation and degeneration Clinical significance
Nephrotic syndrome o Acute tubular necrosis
Extreme stasis of urine flow o Viral diseases
Chronic renal failure o Salicylate intoxication
When broad (2-6x bigger), renal failure cast Mixed cellular casts
Seen in tubular atrophy Two distinct cell types present within a single cast
o Granular cast Reported as hyaline or granular, not as mixed cast
Non-pathologic Combo meals
Finely granular or coarsely granular o RBC and WBC casts: glomerulonephritis
Fairly common o WBC and RTE cell casts: pyelonephritis
Pathologic conditions o WBC and bacterial casts: pyelonephritis
Disintegration of cellular casts o Broad cast
o Glomerulonephritis (RBCs) 2-6 times the diameter of a normal cast
o Pyelonephritis (WBCs) Sources of identification error
o Tubulointerstitial disease (RTEs) Fecal material
Protein aggregates Fibers
Non-pathologic conditions Clinical significance
Lysosomes excreted by tubular cells C/S
o Fatty cast Tubular dilatation
Protein matrix (hyaline cast) with oval fat bodies Extreme stasis
Positive for Maltese cross formation Chronic renal failure
Seen in nephrotic syndrome, toxic tubular necrosis, Telescoped sediment
diabetes mellitus, and crush injuries o All types of casts
o Crystal cast o Elements of glomerulonephritis
Urates, calcium oxalate, sulfonamide o Elements of nephrotic syndrome (fatty casts)
May accompany hematuria o RBCs, RBC casts, cellular casts, broad waxy casts, lipid
o Cellular casts droplets, oval fat bodies, fatty casts
RBC casts o Clinical significance
Cast matrix containing RBCs (RBCs in hyaline cast) Collagen vascular disease (lupus nephritis)
Red-orange color Subacute bacterial endocarditis
Extremely fragile and degenerates to granular casts Crystals
Sources of identification error o Precipitation of urine solutes
o RBC clumps (round without matrix) Inorganic salts, organic compounds, and medications
Reporting (iatrogenic compounds)
o Average number per lpf o Subject to changes in pH, temperature, concentration
Correlation o Solute precipitates more readily at low temperature
o RBCs o Most crystals are of limited clinical significance
o Blood o Urine pH is important
o Protein o Crystals in normal acidic urine
Clinical significance Generally soluble in dilute sodium hydroxide
o Bleeding in the nephron Amorphous urates
o Glomerular damage Aggregates or precipitate of certain chemicals like Ca,
o Glomerulonephritis Na, Mg
o Strenuous exercise Yellow-brown small granules
WBC casts Seen in acidic and neutral specimen
Cast matrix with WBCs Appear as pink-orange to reddish brown “brick dust”
Sources of identification error Soluble in heat (60’C) and dilute alkali
o WBC clumps (round without matrix) “Pseudocast”
Reporting
o Average number per lpf
Uric acid Common form: colorless, three to six sided prisms
Very low pH: 5-5.5 with oblique ends
Yellow or reddish brown Rare form: Flat fern leaf form, sheets, and flakes
Four-sided, flat rhombic plates or prisms Soluble in dilute acetic acid
Lemon-shaped/diamond rosettes (yellow) Clinical significance
Whetstone o Recurrent UTI caused by urea-splitting bacteria
Rare, colorless hexagonals such as Proteus species
Soluble in alkali (NaOH) and ammonia Calcium carbonate
Insoluble in alcohol and acids such as HCl Small and colorless with dumbbell or spherical shapes
Clinical significance Bigger than calcium oxalate
o C/S May occur in clumps that resemble amorphous
o Renal stones material
o Gout Formation of gas after the addition of acetic acid
o High purine metabolism Soluble in acetic acid
o Lesch Nyhan syndrome Birefringent
o After chemotherapy for lymphoma and leukemia No clinical significance
Calcium oxalate Calcium phosphate
Common form: small, colorless, octahedrals that Colorless, rectangular plates or prisms in rosette
resemble envelopes forms
Two pyramids joined at their bases Dissolves in dilute acetic acid
Rare form: dumbbell, ovoid forms Ammonium biurate
Seen in acidic and neutral specimen Yellow-brown spheres
Dihydrate Spicule-covered spheres
o Envelope-shaped Referred to as thorn apples showing irregular
o Positive birefringence projection or thorns and horns
Monohydrate Soluble in heat (60’C) and acetic acid
o Dumbbell and ovoid rectangle Seen in old urine
Soluble in dilute HCl o Crystals in abnormal urine
Insoluble in acetic acid All abnormal crystals are found in acidic urine
Clinical significance Cystine
o Seen in normal individuals after ingestion of Colorless, refractile, hexagonal plates
oxalate-rich food and large doses of vitamin C Soluble in ammonia and dilute HCl
o Renal stones Clinical significance
o Ethylene glycol poisoning (monohydrate form) o Cystinuria
Sodium urates o Kidney disease
Slender prisms o Fanconi syndrome
Usually colorless or sometimes yellowish Tyrosine
Arranged in fan or leaf-like manner Long, fine, silky needles
Referred to as peacock-like crystals Arranged in sheaves of wheat or clumps
Hippuric acid Soluble in alkali (ammonia and KOH) and in dilute HCl
Needle-like crystals Insoluble in alcohol or ether
Colorless and sometimes yellowish brown Clinical significance
Appear in singly o Tyrosinuria
Seen in acidic, neutral, and alkaline urine o Liver disease (along with leucine)
Soluble in hot water and alkali Leucine
Clinical significance Yellow, oily appearing spheres
o Ingestion of excessive benzoic acid Have radial and concentric striations
o Crystals in normal alkaline urine Scallop-like crystals
Generally soluble in dilute acetic acid Soluble in hot alcohol and alkali
Amorphous phosphates Insoluble in ether
Calcium and magnesium Clinical significance
Granular aggregates like amorphous phosphates but o Liver disease (along with tyrosine)
seen in increased pH o MSUD
Seen in neutral and alkaline urine Cholesterol
Colorless granules Rarely seen unless specimens have been refrigerated
Insoluble in heat as lipids remain in droplet form
Soluble with acetic acid and dilute HCl Colorless, flat plate with corner notch
Triple phosphate Stair-step/broken window shape
Aka ammonium magnesium phosphate or struvite Accompanies fatty casts and oval fat bodies
Coffin-lid crystals Soluble in chloroform, ether, and hot alcohol
Birefringent (polarized light) Phosphate
Clinical significance o Pale, friable, fragile
o Nephrotic syndrome Cystine
Bilirubin o Color of old, yellow-brown soap, greasy
Short, clumped needles or granules with o Chemical examination
characteristic yellow color (reddish brown) Pulverize and cut (if too big)
Clinical significance 50 mg powdered stone
o Seen in the matrix of casts in viral hepatitis Add 15 drops of HCl
o Other crystals in urine Positive: formation of bubbles/effervescence
Sulfonamides (sulfadiazine) (carbonates)
Iatrogenic Centrifuge and separate supernatant from the sediment
Colorless or yellow-brown Test on the supernatant
Resemble sheaves of wheat with central bindings Composition Reagent/s Positive result
Rosettes, arrowheads, petals, needles, round forms Calcium Ammonium White
with striations oxalate precipitate
Seen in acidic and neutral urine Ammonium NaOH, KI Rusty,
Confirm with Diazo reaction: magenta brownish red
Ampicillin precipitate
Long, fine, colorless needles that tend to form bundles Test on the sediment
following refrigeration Composition Reagent/s Positive result
Radiographic dye Oxalate HCl, MnO2 Bubbles
Urine has a very high specific gravity reading (>1.035) Test on the stone
Differentiate from cholesterol by looking at the Composition Reagent/s Positive result
specific gravity Phosphate HCl, ammonium Blue
molybdate
VI. Renal Calculi Uric acid Na2CO3, sodium Blue
Aka kidney stones tungstate
Solid aggregates of mineral salts Cystine NH4OH, sodium Red
Location nitroprusside
o Calyces o X-ray crystallography
o Pelvis More comprehensive analysis
o Ureters Determines the arrangement of atoms within a crystal
o Bladder Beam of x-rays strikes a crystal and causes the beam of
Clumps of crystals (with RBCs) in freshly voided urine light to spread into many specific directions
o No casts because these are made up of uromodulin Produce a three-dimensional picture of the density of
Clinical significance electrons within the crystals
o Urolithiasis No more manual chemical examination
o Nephrolithiasis Techniques for analysis
o Renal lithiasis o Chemical examination
o Hematuria o X-ray crystallography
o Associated with renal colic (extreme pain) o Infrared spectroscopy
o Usually asymptomatic (little to no pain) o Radiographic diffraction
o Increased interleukin 6 o Electron microscopy
Released during muscle contraction o Polarizing microscopy
o Large stones may result to hydronephrosis Methods of detection
Distention (dilation) of the kidney with urine caused by o Cytoscopy
backward pressure on the kidney when the flow of Cytoscope equipped with a lens to examine the lining of
urine is obstructed the bladder and urethra
Stone analysis o X-ray evaluation (KUB)
o Physical/gross examination Calcium-containing stones are radiodense or
Wash the stones (usually covered with blood) radiopaque
Record the dimension of the stone Calcium phosphate has the greatest density, followed
Size by calcium oxalate and triple phosphate
Sand, gravel, stone (in millimeters) Cystine calculi: faintly radiodense
Calyces and pelvis: large, rounded, staghorn Uric acid stones: entirely radiolucent
Bladder: large, smooth round o Intravenous pyelogram
Appearance Special x-ray
Uric acid Examination of the kidneys, bladder, and ureters
o Yellow, brownish red, moderately hard o Ultrasound and CT scan
Calcium oxalate Ultrasound: children or pregnant women
o Dark color, very hard, rough surface Compared with CT, renal ultrasonography more often
fails to detect small stones (especially urethral stones)
Management techniques o Beta hCG can be detected in maternal plasma or urine by
o pH incompatible with crystallization of particular 8-9 days after ovulation
chemicals aka “stone dissolution” hCG level correlations
Acidify alkaline urine and vice versa then administer o Early pregnancy
medications hCG levels in the blood double every 2-3 days
o Adequate hydration o Ectopic pregnancy
o Dietary restrictions Longer doubling time
Oxalates May lead to false-negative results
Avoid tea, cocoa, coffee, cola, beans, rhubarb, spinach, o hCG concentrations will drop rapidly following a
nuts, berries, citrus, vitamin C miscarriage
Uric acid o if hCG does not fall to undetectable levels, it may indicate
Avoid dietary intakes of purines, liver, dried beans, remaining hCG-producing tissue that has to be removed
some fish, meat Indications
Removal of renal stones o Suspicion of possible pregnancy
o For stones >1 mm in diameter o To investigate completeness of abortion
o Lithotripsy o To evaluate ectopic pregnancy
Break stones into smaller pieces o To differentiate true pregnancy from other trophoblastic
For stones >4 mm in diameter diseases like hydatidiform mole, choriocarcinoma, and
o Surgery testicular tumors (seminoma and teratomas)
Types of renal stones o Trophoblastic disease
Chemical % pH Causes Abnormal pregnancy in which there is no fetus, only an
composition abnormal mass growth
Calcium 75 5.5-6.5 Idiopathic hypercalciuria, Ectopic pregnancy
oxalate bone disease, primary o Fetus develops outside the uterus
(70%) hyperparathyroidism, Hydatidiform mole
Calcium excessive o Molar pregnancy
phosphate milk/alkali/vitamin D o Is a rare mass or growth that forms inside the uterus at
(10%) intake the beginning of a pregnancy (result of a genetic error
Struvite 15 >7.0 Recurrent infection with during the fertilization process)
urea-splitting bacteria o Type of gestational trophoblastic disease (GTD)
Uric acid 10 <5.5 Gout, uromodulin- o Non-viable, fertilized egg implants in the uterus
associated kidney disease o Results from over-production of the tissue that is
Cystine 1-2 <5.5 Defect in cystine supposed to develop into the placenta
metabolism o Grape-like cell clusters
Mineralogical names o Positive for hCG
o hCG levels are high (both blood and urine) and may go as
Calcium oxalate (monohydrate) Whewellite
high as 350 000 – 3 000 000 IU/L
Calcium oxalate (dihydrate) Weddellite
Choriocarcinoma
Calcium phosphate Apatite
o Complication of hydatidiform mole
Calcium hydrogen phosphate Brushite
o Quick-growing form of cancer that occurs in the uterus
Triple phosphate Struvite o Abnormal cells start in the tissue that would normally
become the placenta
VII. hCG o hCG levels are persistently high
Produced by trophoblastic cells of the developing placenta Positive hCG not associated with pregnancy
Trophoblasts o Female: vesicle tumors
o Cells forming the outer layer of a blastocyst which o Male: testicular tumors (teratomas and seminomas)
provide nutrients to the embryo and develop into a large hCG test results
part of the placenta o Expressed in IU/ml or mIU/ml
Used to diagnose conditions other than pregnancy mIU/ml is more commonly used
Glycoprotein with alpha polypeptide and beta polypeptide o Specimen used may be serum or urine
subunits First morning urine is more commonly used
o Alpha subunit: identical to FSH, prone to false positive o Tests should detect beta hCG
o Beta subunit: measured o Causes of false positive result
Differentiation from other trophoblastic diseases Error in test performance
hCG levels Inaccurate reading of result
o Trophoblastic cells secrete hCG 6-8 days after conception Proteinuria
(6-12 days after ovulation) which doubles every 2-3 days Hematuria
o hCG levels rise rapidly until reaching a peak of 100 000 Drug metabolites
mIU/ml of serum 60-80 days after last menstrual period o Causes of false negative result
o Peak: 10th week of gestation (2 ½ months) Low titer of hCG
o hCG levels decrease from peak to plateau of 10 000-20 Low sensitivity of the test
000 mIU/ml after the first trimester Presence of certain drugs
Dilute urine
o Women should not drink large amounts of fluid before
collecting a urine sample for a pregnancy test
Methods
o Bioassay
Method Animal Positive result
Ascheim Zondek Female mouse Enlargement of
corpus luteum
Friedmann Female rabbit Ovulation
Hogben Female toad Ovulation
(Xenopus laevis)
Galli Mainini Male frog Release of
(Rana pipiens) spermatozoa
Male toad Release of
Commonly used spermatozoa
o Immunoassay
Positive result within 2 minutes
Method Reagents Positive Negative
Hemagglutin Anti-hCG No Agglutin
ation serum, RBCS agglutin ation
Inhibition with hCG, ation
(HAI) sheep’s RBCs
Latex Anti-hCG No Agglutint
agglutination serum, latex agglutio ion
inhibition particles with nation
(LAI) hCG
Direct latex Latex with anti- Agglutin No
agglutination hCG ation agglutina
(DLA) tion
Radioimmunoassay
Most sensitive method
Not commonly used because of cost-effectiveness and
long incubation time (2 hours)
Competitive binding assay
hCG in serum and radiolabeled hCG compete for
binding with anti-hCG Antibody
An inverse correlation exists between the number of
radioactive counts in the antibody complex and the
amount of hCG in the patient’s serum
o Positive result: decreased radioactive count
o Negative result: increased radioactive count
High sensitivity: 5-9 mIU/ml
Enzyme immunoassay
Most commonly used
Uses double monoclonal antibody (sandwich method)
First antibody is bound to solid phase
Second antibody Is linked to an indicator enzyme such
as alkaline phosphatase
Substrate becomes cleared
Sensitivity: 20-50 mIU/ml
Rapid: 2 minutes
Affordable
Results
o Positive result: double bar
o Negative result: single bar
o Control: always has a line
o Testing: blank at first
Home test kit assay
Immunochromatography strip test
Lateral flow test
Competitive or sandwich assays
S-ar putea să vă placă și
- CLINICAL CHEMISTRY: Passbooks Study GuideDe la EverandCLINICAL CHEMISTRY: Passbooks Study GuideÎncă nu există evaluări
- The Pyridine Nucleotide CoenzymesDe la EverandThe Pyridine Nucleotide CoenzymesJohannes EverseÎncă nu există evaluări
- Physical Examination of UrineDocument4 paginiPhysical Examination of UrineIceÎncă nu există evaluări
- Topic 02 Urinalysis I Review of Ana and Phy of KidneysDocument6 paginiTopic 02 Urinalysis I Review of Ana and Phy of KidneysNatasha MendozaÎncă nu există evaluări
- HISTOTECHNIQUESDocument20 paginiHISTOTECHNIQUESZIPPORAH JESSICA NONOGÎncă nu există evaluări
- Foundations in Microbiology: Nonspecific Host Defenses TalaroDocument35 paginiFoundations in Microbiology: Nonspecific Host Defenses TalaroOdurÎncă nu există evaluări
- Inherited Overflow Metabolic Overflow RenalDocument11 paginiInherited Overflow Metabolic Overflow RenalChrissa Mae Tumaliuan CatindoyÎncă nu există evaluări
- 1 Antigens and AntibodiesDocument31 pagini1 Antigens and AntibodiesJohn Louis RanetÎncă nu există evaluări
- Lesson 1 History of Medical Technology or The Clinical Laboratory Science ProfessionDocument4 paginiLesson 1 History of Medical Technology or The Clinical Laboratory Science ProfessionGianneCarloGomedÎncă nu există evaluări
- Aubf Outline EditedDocument16 paginiAubf Outline EditedNoraine Princess TabangcoraÎncă nu există evaluări
- Bacteriology Lab 2 - Instruments Used in Bacteriology LaboratoryDocument1 paginăBacteriology Lab 2 - Instruments Used in Bacteriology LaboratoryJiro Anderson EscañaÎncă nu există evaluări
- Type 3 DiabetesDocument7 paginiType 3 DiabetesAniqua sajidÎncă nu există evaluări
- Analysis of Urine and Other Body: Central Luzon Doctors' Hospital Educational InstitutionDocument63 paginiAnalysis of Urine and Other Body: Central Luzon Doctors' Hospital Educational InstitutionRenaÎncă nu există evaluări
- CM Lec Chemical Examination of UrineDocument50 paginiCM Lec Chemical Examination of UrineThea MallariÎncă nu există evaluări
- CH 6 Part 1Document7 paginiCH 6 Part 1ArenÎncă nu există evaluări
- Chapter 1: Introduction To Urinalysis: Urine CompositionDocument74 paginiChapter 1: Introduction To Urinalysis: Urine CompositionMegumi TadokoroÎncă nu există evaluări
- Week 1 Day 1 LessonDocument143 paginiWeek 1 Day 1 LessonTRIXIE CYRAH MIRANDA SALAVIAÎncă nu există evaluări
- Lesson 3Document71 paginiLesson 3Angel joyce ValenciaÎncă nu există evaluări
- Hematology 2 Lesson 1Document9 paginiHematology 2 Lesson 1janÎncă nu există evaluări
- Nematodes: 2. Enterobius VermicularisDocument2 paginiNematodes: 2. Enterobius VermicularisCia QuebecÎncă nu există evaluări
- Family Neisseriaceae: Joy P. Calayo, RMT, MSMT UST Faculty of Pharmacy Dept. of Medical TechnologyDocument18 paginiFamily Neisseriaceae: Joy P. Calayo, RMT, MSMT UST Faculty of Pharmacy Dept. of Medical Technologypixholic100% (1)
- 2.01 Diagnostic VirologyDocument6 pagini2.01 Diagnostic VirologyMaria MikaelaÎncă nu există evaluări
- Microbial GrowthDocument96 paginiMicrobial GrowthJenniferÎncă nu există evaluări
- Bacterial Crowth CurveDocument29 paginiBacterial Crowth CurveDr. Kalavati PrajapatiÎncă nu există evaluări
- Entamoeba SPPDocument21 paginiEntamoeba SPPragnabulletinÎncă nu există evaluări
- Aubf Prelim 1Document59 paginiAubf Prelim 1Kat JornadalÎncă nu există evaluări
- Molecular Biology and Diagnostic Intro To CytogeneticsDocument6 paginiMolecular Biology and Diagnostic Intro To Cytogeneticselijah montefalcoÎncă nu există evaluări
- Introduction To Microbiology Taxonomy Morphology: Dr. José L. Navarro Clinical Microbiologist, (Madrid, Spain)Document49 paginiIntroduction To Microbiology Taxonomy Morphology: Dr. José L. Navarro Clinical Microbiologist, (Madrid, Spain)ImaPratiwiÎncă nu există evaluări
- Introduction To Hematology 2Document15 paginiIntroduction To Hematology 2Tom Anthony TonguiaÎncă nu există evaluări
- (MT6317) Unit 6.1 Introduction To Carbohydrates and Glucose DeterminationDocument12 pagini(MT6317) Unit 6.1 Introduction To Carbohydrates and Glucose DeterminationJC DomingoÎncă nu există evaluări
- RMTnotes PARASITOLOGYDocument68 paginiRMTnotes PARASITOLOGYArvin O-CaféÎncă nu există evaluări
- Mtap - Special Histopath TechniquesDocument21 paginiMtap - Special Histopath TechniquesK-idol LiveÎncă nu există evaluări
- Diagnostic Microbiology - : University of Santo Tomas - Medical TechnologyDocument6 paginiDiagnostic Microbiology - : University of Santo Tomas - Medical TechnologyWynlor AbarcaÎncă nu există evaluări
- VibriocholeraeDocument85 paginiVibriocholeraesourabbirlaÎncă nu există evaluări
- Chapter 2 Introduction To Urinalysis PDFDocument4 paginiChapter 2 Introduction To Urinalysis PDFJulie Anne Soro ValdezÎncă nu există evaluări
- 02 Diagnostic MycologyDocument78 pagini02 Diagnostic MycologyNilda Quitquitan PatriarcaÎncă nu există evaluări
- Viruses PDFDocument54 paginiViruses PDFluz camargoÎncă nu există evaluări
- 4 Chemical Examination of Urine PDFDocument12 pagini4 Chemical Examination of Urine PDFLovely B. AlipatÎncă nu există evaluări
- Histopathology Review NotesDocument8 paginiHistopathology Review NotesKhoreen ObisoÎncă nu există evaluări
- General Pathology - Lecture 1 SlideshowDocument82 paginiGeneral Pathology - Lecture 1 SlideshowLily Dawn Marquez JoloÎncă nu există evaluări
- Hematology II Notes - MagtalasDocument12 paginiHematology II Notes - MagtalasAbhugz VosotrosÎncă nu există evaluări
- Immunohema SlidesDocument508 paginiImmunohema SlidesBerihunÎncă nu există evaluări
- TREMATODESDocument31 paginiTREMATODESKen Mark ConcepcionÎncă nu există evaluări
- (Microbiology and Parasitology) Basic and Clinical MycologyDocument43 pagini(Microbiology and Parasitology) Basic and Clinical MycologyMa. Pia Lorein JacintoÎncă nu există evaluări
- Clinical Microscopy (Analysis of Urine and Other Body Fluids)Document14 paginiClinical Microscopy (Analysis of Urine and Other Body Fluids)Jeanly DoctorÎncă nu există evaluări
- MLS304 Lec1Document74 paginiMLS304 Lec1Cassandra CasipongÎncă nu există evaluări
- Gram Negative Cocci (Lecture Notes)Document5 paginiGram Negative Cocci (Lecture Notes)Dayledaniel Sorveto100% (1)
- Group 3 - ParasitologyDocument8 paginiGroup 3 - Parasitologyjulo_05Încă nu există evaluări
- Lesson 5 The UrineDocument44 paginiLesson 5 The UrineFaith TambongÎncă nu există evaluări
- Anaerobe of Clinical ImportanceDocument43 paginiAnaerobe of Clinical ImportanceDayledaniel SorvetoÎncă nu există evaluări
- Histopath Lec (Module 1) : Iintroduction To PathologyDocument17 paginiHistopath Lec (Module 1) : Iintroduction To PathologyAngela ReyesÎncă nu există evaluări
- Mycology 1 PrelimDocument4 paginiMycology 1 PrelimKaye Angel VillonÎncă nu există evaluări
- Vascular System Vascular Structure and FunctionDocument8 paginiVascular System Vascular Structure and FunctionEriq BaldovinoÎncă nu există evaluări
- Heterophyid: ST NDDocument3 paginiHeterophyid: ST NDIvan ChuaÎncă nu există evaluări
- Chapter 4 Physical Examination PDFDocument4 paginiChapter 4 Physical Examination PDFJulie Anne Soro ValdezÎncă nu există evaluări
- Detection and Identification of Antibodies - SCDocument67 paginiDetection and Identification of Antibodies - SCLyra Dennise LlidoÎncă nu există evaluări
- Urinalysis 1: Mr. Arian Ray E. MalintadDocument55 paginiUrinalysis 1: Mr. Arian Ray E. MalintadAbraham DemeterioÎncă nu există evaluări
- AUBF - Chapter 2Document5 paginiAUBF - Chapter 2Kristin SoquilloÎncă nu există evaluări
- Trematodes PDFDocument46 paginiTrematodes PDFAsnorah SaripÎncă nu există evaluări
- Fastidious Gram-Negative BacilliDocument18 paginiFastidious Gram-Negative BacilliNadene KindredÎncă nu există evaluări
- Quick Review Cards For Medical Laboratory Science - Polansky, Valerie DietzDocument619 paginiQuick Review Cards For Medical Laboratory Science - Polansky, Valerie DietzIslam92% (86)
- ZOO Weekly - June 8, 2015 AU PDFDocument72 paginiZOO Weekly - June 8, 2015 AU PDFLoro JD67% (3)
- Group B ReportDocument23 paginiGroup B ReportLoro JDÎncă nu există evaluări
- FHM - June 2015 IN PDFDocument124 paginiFHM - June 2015 IN PDFLoro JDÎncă nu există evaluări
- Esquire - July 2015 UKDocument144 paginiEsquire - July 2015 UKLoro JD100% (1)
- ZOO - June 5, 2015 UK PDFDocument70 paginiZOO - June 5, 2015 UK PDFLoro JD50% (2)
- FHM - July 2015 UKDocument148 paginiFHM - July 2015 UKLoro JDÎncă nu există evaluări
- Muscle & Fitness - June 2015 AU PDFDocument116 paginiMuscle & Fitness - June 2015 AU PDFLoro JDÎncă nu există evaluări
- FHM - June 2015 IN PDFDocument124 paginiFHM - June 2015 IN PDFLoro JDÎncă nu există evaluări
- GQ201506AUDocument162 paginiGQ201506AUZedrichÎncă nu există evaluări
- Maxim - June 2015 IN PDFDocument108 paginiMaxim - June 2015 IN PDFLoro JD100% (1)
- ZOO Weekly - June 8, 2015 AU PDFDocument72 paginiZOO Weekly - June 8, 2015 AU PDFLoro JD67% (3)
- ZOO - June 5, 2015 UK PDFDocument70 paginiZOO - June 5, 2015 UK PDFLoro JD50% (2)
- Muscle & Fitness - June 2015 AU PDFDocument116 paginiMuscle & Fitness - June 2015 AU PDFLoro JDÎncă nu există evaluări
- Aubf ReviewerDocument3 paginiAubf ReviewerLoro JDÎncă nu există evaluări
- Blood Groups Assignment AaaDocument3 paginiBlood Groups Assignment AaaLoro JDÎncă nu există evaluări
- GQ201506AUDocument162 paginiGQ201506AUZedrichÎncă nu există evaluări
- Maxim - June 2015 IN PDFDocument108 paginiMaxim - June 2015 IN PDFLoro JD100% (1)
- MTLBE Summary PDFDocument38 paginiMTLBE Summary PDFLoro JDÎncă nu există evaluări
- MTLBE Summary PDFDocument38 paginiMTLBE Summary PDFLoro JDÎncă nu există evaluări
- Blood Group System Ab Significant? - Ab Type Antigens Null/Weak Phenotypes Transfusion Reactions? - HDFN? Notes MNSDocument3 paginiBlood Group System Ab Significant? - Ab Type Antigens Null/Weak Phenotypes Transfusion Reactions? - HDFN? Notes MNSLoro JDÎncă nu există evaluări
- Functional ProteinuriaDocument2 paginiFunctional Proteinuriayolandadwioo100% (1)
- Topic 03 UA 2 Chemical Analysis of Urine (Protein and Glucose)Document5 paginiTopic 03 UA 2 Chemical Analysis of Urine (Protein and Glucose)Natasha MendozaÎncă nu există evaluări
- Lab Practical UrinalysisDocument7 paginiLab Practical UrinalysisHeatherIz AwwsomeÎncă nu există evaluări
- Abnormal Urinalysis Children-Tadulako2015Document33 paginiAbnormal Urinalysis Children-Tadulako2015Yeyen Hastriam AkramÎncă nu există evaluări
- Nephrology TestDocument112 paginiNephrology TestRapid Medicine50% (2)
- Pediatric Genitourinary DisordersDocument28 paginiPediatric Genitourinary Disordersjae_007Încă nu există evaluări
- Diabetic Nephropathy BaruDocument24 paginiDiabetic Nephropathy BaruRobiyanti Nur Chalifah HattaÎncă nu există evaluări
- Nephrotic Syndrome AdultsDocument6 paginiNephrotic Syndrome AdultsSamuel Rudolf Maranatha JulioÎncă nu există evaluări
- Self-Assessment Questions, Group 6Document20 paginiSelf-Assessment Questions, Group 6naveenkovalÎncă nu există evaluări
- Case Nephrotic SyndromeDocument32 paginiCase Nephrotic SyndromeTera SurbaktiÎncă nu există evaluări
- Supervisor: Prof. Dr. Atan Baas Sinuhaji, Spa (K)Document35 paginiSupervisor: Prof. Dr. Atan Baas Sinuhaji, Spa (K)Ranap HadiyantoÎncă nu există evaluări
- ACP Board Review Nephrology 20052ndDocument35 paginiACP Board Review Nephrology 20052nddoctormido2010100% (1)
- OB - II - PREGNANCY - HYPERTENSION - PDF Filename UTF-8''OB II PREGNANCY HYPERTENSIONDocument10 paginiOB - II - PREGNANCY - HYPERTENSION - PDF Filename UTF-8''OB II PREGNANCY HYPERTENSIONyayayanizaÎncă nu există evaluări
- Clinical Chemistry - Specimen Collection and Patient PreparationDocument6 paginiClinical Chemistry - Specimen Collection and Patient Preparationrosellae.Încă nu există evaluări
- WEEK 2 B Chemical Examination of Urine (Laboratory)Document9 paginiWEEK 2 B Chemical Examination of Urine (Laboratory)Dayledaniel SorvetoÎncă nu există evaluări
- ACKD Susp Lupus NefritisDocument61 paginiACKD Susp Lupus Nefritisrastu karyanaÎncă nu există evaluări
- Uroanalisis AnormalDocument13 paginiUroanalisis AnormalMyke EstradaÎncă nu există evaluări
- Seminar: Angela C Webster, Evi V Nagler, Rachael L Morton, Philip MassonDocument15 paginiSeminar: Angela C Webster, Evi V Nagler, Rachael L Morton, Philip MassonMaría José GalvisÎncă nu există evaluări
- Aubf Questions With AnswersDocument16 paginiAubf Questions With AnswersFenyl Isis GuigayomaÎncă nu există evaluări
- Vital Nephrology - $86.04Document106 paginiVital Nephrology - $86.04Abdallah Bouleghraif100% (1)
- Preeclampsia Early Recognition ToolDocument1 paginăPreeclampsia Early Recognition ToolHaniv Prasetya AdhiÎncă nu există evaluări
- Copy 1 of Treatment Profile For Intern Docto 2Document57 paginiCopy 1 of Treatment Profile For Intern Docto 2AminulÎncă nu există evaluări
- Exp 3Document7 paginiExp 3Chan Wei QuanÎncă nu există evaluări
- Hypertension Guideline V1.0 GL952Document63 paginiHypertension Guideline V1.0 GL952Αντώνιος ΧατζηγεωργίουÎncă nu există evaluări
- CKD PPKD Weight Reduction 310107Document3 paginiCKD PPKD Weight Reduction 310107Geoffrey HoÎncă nu există evaluări
- CPG Management of Chronic Kidney Disease in AdultsDocument73 paginiCPG Management of Chronic Kidney Disease in AdultsVera ProkopenkoÎncă nu există evaluări
- Overview of Heavy Proteinuria and The Nephrotic Syndrome - UpToDateDocument34 paginiOverview of Heavy Proteinuria and The Nephrotic Syndrome - UpToDatechristian47Încă nu există evaluări
- Nephrotic Syndrome-1Document21 paginiNephrotic Syndrome-1Wondimu EliasÎncă nu există evaluări
- 22 - Proteinuria and HematuriaDocument73 pagini22 - Proteinuria and HematuriaArsalan NadeemÎncă nu există evaluări
- Diabetic NephropathyDocument6 paginiDiabetic NephropathyZulfadliZulfadliÎncă nu există evaluări