Documente Academic
Documente Profesional
Documente Cultură
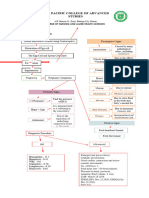
Approach To Emergency Patient
Încărcat de
Juan Pablo Gallardo ContrerasTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Approach To Emergency Patient
Încărcat de
Juan Pablo Gallardo ContrerasDrepturi de autor:
Formate disponibile
Section 1
Principles of
Emergency Medicine
1. Approach to the emergency
patient 000 3
2. Airway management 000 19
3. Cardiopulmonary and cerebral
resuscitation 000 41
4. Cardiac dysrhythmias 000 55
5. Severe sepsis and septic
shock 000 73
6. Shock 000 87
7. Traumatic injuries 000 95
8. Emergency medical services
systems 000 115
9. Pain management 000 127
CUUK1447_01.indd 1 11/22/11 7:52:43 AM
CUUK1447_01.indd 2 11/22/11 7:52:43 AM
Approach to the emergency patient
1 Approach to the emergency patient
Gus M. Garmel, MD
The emergency department (ED) is an extremely chal- be prepared to act and react to prevent morbidity and,
lenging environment for patients, families, and medical when possible, mortality. EPs must maintain a healthy
personnel. Many challenges result from the principles of skepticism towards patient’s answers to common ques-
our practice: available and prepared at any time for any tions. Considering worst-case scenarios is fundamental
patient with any complaint. Patients who come to the ED to emergency medicine (EM) practice. Most importantly,
are most often unfamiliar with us, yet we must immedi- EPs must be comfortable providing detailed, often
ately help them feel confident about our abilities. Patients devastating information using clear, understandable
generally present to the ED during a time of great concern. language to patients and family members with differ-
Their needs may be as straightforward as a note excusing ent educational or cultural backgrounds. All this must
them from work or a prescription refill in the middle of be done under time constraints, while demonstrating
the night, or as complex as an acute illness or injury, an empathy and compassion.
exacerbation of a chronic condition, or a cry for help if It is indeed a privilege to care for patients during their
depressed or suicidal. In their own way, patients almost time of greatest need or when they lack other options.
always seek reassurance about something – is their child’s Approaching patients sensitively, recognizing their
fever dangerous, their headache cancer, or their abdomi- apprehension, pain, concerns, and perhaps shame is
nal pain appendicitis? Providing reassurance to patients, critical to our mission. This is true no matter how trivial
parents and families whenever possible is a critical func- a patient’s problem may seem. Often, patients consult
tion of emergency physicians (EPs). EPs seeking approval to leave an abusive spouse, for an
Qualities successful EPs exhibit include intelligence, opinion regarding a physician’s recommendation for sur-
sensitivity, humility, insight, proficiency in making deci- gery, or to confirm that they are making the right deci-
sions with and acting on limited information, and the sion about a parent, child, or loved one. Serving in this
ability to multi-task. Working well with individuals of capacity without judgment is not only appropriate, but
different backgrounds and ethnicities while at all times also essential.
strongly advocating for patients are essential qualities. It is imperative that EPs approach each patient with
EPs must also be skilled at leadership, negotiation and an open mind, committed to identify and address not
conflict resolution. They must be exceptional commu- only the presenting problem, but also any coexisting
nicators. In addition to these traits, EPs must be experts problems. For example, a patient with a history and
in both medical and trauma resuscitation of adults and presenting complaint consistent with esophageal reflux
children. may in fact have an acute coronary syndrome (ACS). A
The majority of patients use the ED infrequently. Many patient presenting with insomnia may have an underly-
are experiencing this setting for the first time. Because ing concern about his or her safety, security, or mental
patients lack familiarity with this environment, they may wellness. The ability of an EP to evaluate each patient
have expectations that go unmet. Their fear, stress, wait- using history-taking and physical examination abilities,
ing time, lack of privacy and discomfort that brought as well as selecting appropriate laboratory or imaging
them to the ED can negatively impact their experience. studies (when necessary), is only a portion of our skill
These are only some of the issues that patients contend set. An experienced EP’s “sixth sense” is something that
with in the ED. has become recognized and respected by non-EM col-
EPs confront numerous challenges when taking care leagues.
of patients presenting to the ED. Perhaps the greatest Unfortunately, the ED is not always conducive to
challenge is the extensive disease spectrum that EPs privacy. Despite the Health Insurance Portability and
must be familiar with. Rather than having to know only Accountability Act (HIPAA) of 1996 and Protected Health
the first few minutes (or hours) of an illness, EPs must Information (PHI) for patients, attempts to maintain
be familiar with all stages of all illnesses, often pre- patient confidentiality in the ED present a continuous
senting in atypical fashion. As boarding times increase challenge. Discussions about patient care issues between
and observation units become more common, patients health care providers, staff, patients and family mem-
remain under an EP’s care for longer periods of time. bers often take place behind nothing more than a curtain.
In addition, time pressures inherent to providing Shared spaces, hallways, lack of private rooms or beds,
emergency care, the lack of existing relationships with and the demands of time-pressured discussions – often in
patients, unfamiliarity with their medical history, and open spaces, over the phone, or with consultants – stretch
the inability to review patients’ medical records chal- efforts at maintaining patient confidentiality. The leader-
lenge EPs daily. EPs must rapidly and simultaneously ship role that EPs have in the ED affords them the oppor-
evaluate, diagnose and treat multiple patients with tunity to demonstrate respect for patient confidentiality
multiple conditions, often with limited information, and and to remind others of the importance of upholding this
not confuse subtle nuances between patients. They must principle.
Principles of Emergency Medicine 3
CUUK1447_01.indd 3 11/22/11 7:52:43 AM
Within the last decade, there has been tremendous are responsible for the initial assessment and care of any
Approach to the emergency patient
and appropriate attention placed on medical error and medical condition that a patient believes requires urgent
patient safety in hospitals. Human error may occur at attention. Patients may believe they require urgent atten-
any time, but is more likely during high patient vol- tion when in fact they do not. It remains our mission to
umes or when multiple complicated patients of high provide quality medical care and reassurance to patients
acuity present simultaneously. These situations are even under this circumstance. EPs also provide medi-
common in EDs around the world. Human error has cal support for individuals who lack access to other care
been demonstrated to occur more frequently when pro- opportunities. As the number of uninsured and underin-
vider fatigue is greatest (e.g., at the end of a challenging sured persons in the United States increases, and growing
shift or after being awake all night). Systems errors are numbers of health clinics close, many of these individu-
even more likely to occur during these circumstances. als will use the ED for their primary as well as emer-
The airline industry has served as a model for reducing gency care. This has placed a tremendous burden on the
errors and improving patient safety in medical practice, safety net provided by the specialty of EM. It is unclear
especially in the ED. Airline pilots, however, are not exactly how governmental health care reform will impact
required to fly more than one plane at the same time, EDs, patient volumes, and overall physician and patient
while simultaneously taking off, landing, and changing satisfaction.
course. The EM community should embrace the federal According to the Centers for Disease Control and
government’s attention to medical systems and its role Prevention (CDC), which publishes the National Hospital
in medical error, as patient safety must always be a top Ambulatory Medical Care Survey (NHAMCS), there
priority. Hospital quality committees review errors of were 119.2 million ED visits in 2006; 18.4 million of these
omission and commission, medication errors, errors in patients arrived by ambulance. This is an increase of over
patient registration, and errors of judgment. Given the 11 million visits from 2000. Patients were admitted to the
pace of the ED environment, it is remarkable that more hospital in 12.8% of ED visits. The ED was the portal of
errors do not occur. The rapid need for patient turnover, admission for slightly over 50% of all non-obstetric admis-
room changes, and test result reporting does not occur sions in the United States in 2006, an increase from 36% in
with such immediacy in most other areas of the hospi- 1996. In California, patients visiting EDs were sicker than
tal. Hospital administrators and regulators with limited ever before, with an increase in critical emergency care
insight about the uniqueness of EM practice should visits by 59% between 1990 and 1999. In 2000, there were
focus attention to, and provide support for, this essential slightly more than 4,000 EDs, yet this number continues
aspect of patient care. to decrease as hospitals and trauma centers close. A 2008
EPs must recognize that patients signed over to them at workforce study by Ginde, et al. reported that despite
the end of a shift pose increased risk. These patients typi- nearly 40,000 clinically active EPs, this was not adequate
cally have pending laboratory or radiography results, are to treat the growing number of people who visit EDs each
being observed for continued improvement or worsening year. Despite an increased number of certified residency
in their condition, or are waiting for consultants. The EP training programs producing board-prepared EPs, and
who initially evaluated these patients should determine the increase in EPs from less than 32,000 in 1999, there
the treatment and disposition plans to the greatest extent remains a critical shortage of capable EPs, especially in
possible, based on anticipated outcomes. However, some the rural and central United States. The number of nurse
signed-over patients may not have well-established dis- practitioners and physician assistants trained to work
positions and may benefit from a new EP’s perspective. in emergency care settings has increased in response to
In such cases, it is better to inform the receiving EP that this shortage as well as administrative and financial pres-
a clear understanding about what is going on with that sures, and many hospitals staff urgent care and fast-track
patient does not exist than leave things vague. As long as areas with these practitioners. With decreased funding
patients present to EDs at any time, patients signed over available for non-ED clinics, and increasing numbers of
at shift’s end will continue to challenge our ability to pro- uninsured patients using the ED as their primary (or only)
vide safe care within our practice. Many hospitals now source of health care, the worsening of ED overcrowding
have regulations in place regarding this aspect of emer- is inevitable.
gency care. Hamilton described the clinical practice of EM as
one that “ . . . encompasses the initial evaluation, treat-
ment, and disposition of any person at any time for
any symptom, event, or disorder deemed by the person
Scope of the problem – or someone acting on his or her behalf – to require
expeditious medical, surgical, or psychiatric attention.”
A landmark article by Schneider, et al. in the EM litera- This philosophy creates tremendous challenges, as well
ture defines our specialty as one “…with the principle as opportunities, unique to the specialty of EM. EDs
mission of evaluating, managing, treating and prevent- must be fully staffed and always prepared while never
ing unexpected illness and injury.” As emergency medi- entirely certain of patient needs at any given moment.
cal care is an essential component of a comprehensive Despite statistics on the number of patients presenting
health care delivery system, it must be available 24 hours at different times on different days in different months,
a day. EPs provide rapid assessment and treatment of no model can predict the exact number of medical staff
any patient with a medical emergency. In addition, they needed to care for even one emergency patient. Clearly,
4 Principles of Emergency Medicine
CUUK1447_01.indd 4 11/22/11 7:52:43 AM
staffing an ED to be fully operational is an expensive infections), deep venous thrombosis (DVT), drugs and
Approach to the emergency patient
proposition given this scenario. drug interactions, cancer, tick-borne infections, malaria
or other parasitic infections, vasculitis, and arthritis are
other conditions causing fever.
Clinical scope of the problem
Bleeding
Table 1.1 provides the 10 most common reasons that
Bleeding may be painful or painless and may or may not
patients visit an ED, according to a recent 2006 national
have associated symptoms. Examples include lacerations,
survey. Of all ED visits, over 35% were for an injury.
vaginal bleeding (with or without pregnancy), gastroin-
Lacerations of an upper extremity were number 11; lac-
testinal (GI) bleeding, epistaxis, and hematologic illnesses
erations in the aggregate therefore did not make this list
such as anemia, von Willebrand’s disease, or hemophilia
because of the manner in which they were categorized
(often resulting in spontaneous bleeding).
and recorded. These data show remarkable consistency in
numbers and rank from survey to survey.
Social concerns
Table 1.1 Top 10 reasons for an ED visit Social issues for which patients come to the ED include an
1. Abdominal pain (8,057,000) inability to care for oneself, a change in behavior (either
2. Chest pain (6,392,000) organic or functional), drug- and/or alcohol-related prob-
3. Fever (4,485,000) lems, homelessness, hunger, or concerns of family mem-
4. Headache (3,354,000)
5. Back symptoms (3,304,000)
bers that something might be wrong.
6. Shortness of breath (3,307,000)
7. Cough (2,956,000) In EM, it is essential that care is coordinated. This means
8. Vomiting (2,635,000) that EPs should seek assistance in providing patient care,
9. Pain, site not referable to a specific body system relying on more than just the patient to assess the situ-
(2,512,000)
10. Throat symptoms (2,278,000) ation. Family members often provide additional infor-
mation about illness progression that patients fail to
From the 2006 National Hospital Ambulatory Medical Care recognize or neglect to share. Prehospital care provid-
Survey, Centers for Disease Control and Prevention. ers often have useful information about the patient’s
living situation and whether or not it is appropriate.
Psychosocial aspects of each patient must be considered
In fact, patients come to the ED as a result of only a few when interpreting presenting complaints and determin-
general categories of problems or complaints. These may ing patient dispositions, including the appropriate use of
be grouped as follows, listed in decreasing frequency. consultation. Involving a consultant who focuses solely
on his or her area of expertise may result in a less opti-
Pain mal outcome, as he or she may overlook a combination
of etiologies causing the problem. When the care of a
Pain is the most likely reason for patients to seek medical particular patient is beyond the scope of EM practice,
care at an ED. It can be traumatic or atraumatic in nature. the EP must make certain that the “proper” consultants
Chest, abdominal, head, extremity, low back, ear, throat, and the appropriate teams are involved. Social services,
and eye pain are only a few examples. discharge planners, patient care coordinators, and, if nec-
essary, behavioral health or chemical dependency special-
Difficulty with . . . ists may need to be included. EPs must identify whom to
turn to in order to ensure and maximize beneficence and
This can be difficulty with breathing, vision, urination, patient benefit. EPs often coordinate patient care behind
swallowing, concentration, speaking, balance, coordina- the scenes, which takes time and effort, yet they rarely
tion, ambulation, or sensation. Difficulty controlling sei- receive recognition for this.
zure activity would also fall into this broad category.
Fever
Anatomic essentials
Fever is common in children and of great concern to par- Anatomic essentials for any patient presenting to the
ents. It can be a presenting complaint in adults as well. ED are covered in detail throughout the text. Airway,
Conditions causing fever include viral or bacterial infec- Breathing, Circulation, Disability, and Exposure
tions, such as upper respiratory infection (URI), gastroen- (ABCDE) are crucial to the initial evaluation and man-
teritis, otitis media, urinary tract infection (UTI), cellulitis, agement of patients with emergent or urgent conditions.
pneumonia, and bronchitis. Surgical conditions (such as This may be true for conditions that do not seem emer-
appendicitis, cholecystitis, atelectasis, and postoperative gent at the time, such as the airway of a talking patient
wound infections), obstetric-gynecologic problems (such recently exposed to intense heat (fire, smoke, or steam).
as pelvic or cervical infections, mastitis, postpartum The airway is essential not only for gas exchange, but
Principles of Emergency Medicine 5
CUUK1447_01.indd 5 11/22/11 7:52:43 AM
also for protection against aspiration. It may be used for When approaching any emergency patient, provid-
Approach to the emergency patient
the administration of certain medications. With condi- ers should offer a brief introduction using the appro-
tions causing increased intracranial pressure (ICP), air- priate prefix (doctor or medical student) and relevant
way management with modest hyperventilation results background information, such as their current level and
in cerebral vasoconstriction, one aspect of therapy. specialty of training. A gentle yet professional touch,
Breathing depends not only on the lungs, but also on such as a handshake or touch of the wrist, is generally
the thoracic cavity, respiratory musculature, and cen- favorably received. Before questioning a patient about
tral nervous system (CNS). Circulation may be compro- his or her present illness or medical history, sit down
mised as a result of hemorrhage, dehydration, vascular at the patient’s bedside if the situation allows. This not
catastrophe, cardiovascular collapse, or vasoconstriction only eliminates towering over a patient, but demon-
or vasodilatation in response to shock. Evaluating dis- strates that you are interested in what he or she has to
ability includes a focused neurologic exam, including an say, and plan to be present and listen for a while (even
assessment of the level of consciousness (LOC), mental if this time is short). Patients recall that the amount of
status, and evaluation of motor, sensory, reflexes, cranial time their physician spent with them was greater if their
nerves, and cerebellar function. A thorough understand- physician sat down during the interaction. After sitting
ing of the neurovascular supply to extremities, espe- down, listen to what the patient has to say. Physicians
cially following traumatic lacerations or injuries, helps interrupt their patients early and often, with EPs being
identify limb threats or potential morbidity. Knowledge some of the biggest offenders. Look patients in the eye
of dermatomes is also helpful when assessing neuro- so they know you are present, listening and care about
logic symptoms. The Alertness, Verbal response, Pain their concerns. If you take notes during the interview, do
response, Unresponsive (AVPU) scale and the Glasgow so following a short period of good eye contact. If these
Coma Scale (GCS) are two tools that can be recorded to notes are done on a computer, remember not to “hide”
describe the general neurologic status of a patient, as behind the computer screen. Demonstrate respect for a
well as follow neurologic status over time. The National patient’s well-being and privacy by offering a pillow
Institutes of Health Stroke Scale (NIHSS) is used for or blanket, adjusting their bed, assisting with covering
patients with cerebral vascular accidents (CVA). Several their body, or providing water (if appropriate). These
scores have been validated to predict stroke risk in kind gestures are easy to do yet greatly appreciated, and
patients with transient ischemic attacks (TIA); the can be done in a few seconds at the start of each patient
ABCD2 score (Age, Blood pressure [BP], Clinical features, interaction.
Duration, Diabetes) is preferred. Exposure is essential so When possible, use open-ended questions to elicit his-
injuries are not missed, as well as to consider possible torical information about a patient’s condition. This allows
environmental elements contributing to the presentation patients to describe their concerns using their own terms.
(e.g., heat, cold, water, toxins). Certainly, some questions require yes or no answers (“Do
you have diabetes?”). There will be times when directed
questions are required, such as to a patient in extremis, or
when a patient does not answer questions promptly or
History concisely. However, most patients will get to the point of
their visit in a relatively short time.
The patient’s history has always been considered one The P-Q-R-S-T mnemonic assists with gathering impor-
of the most important elements in determining a final tant historical elements of a presenting complaint from a
diagnosis. It is accepted that the history (and physical patient. Using pain as an example, questions relating to
examination) can determine the diagnosis in up to 85% the history of a painful condition include those shown in
of patients. A patient’s history should focus on the cur- Table 1.2.
rent problem(s), allowing room to identify additional
information and determine its relevance. When patients
present in extremis, the traditional approach to obtaining
Table 1.2 P-Q-R-S-T mnemonic for history of a painful condition
the patient’s history must be abandoned. In this situation,
history and physical examination information must be P is for provocative/palliative, as in “What makes this pain
obtained concurrently. EPs are forced to rely on clinical worse or better?”
assessment and impression, and utilize important diag- Q is for quality of pain, as in “Describe your pain?” or, “Is
your pain sharp or dull?”
nostic studies during their decision making. Studies that
assist in establishing a final diagnosis, such as an elec- R is for region/radiation, as in “What region of your body
does this pain occur?” and “Does it radiate, or move, to
trocardiogram (ECG), glucose, urine dipstick, and other any other location(s)?”
point-of-care (bedside) tests, can be obtained while gath-
S is for severity, which may be communicated using a
ering historical data. Despite this, establishing a final numeric scale from 0–10, a happy–sad faces scale, or the
diagnosis is not always possible during the course of the terms mild, moderate, or severe.
patient’s evaluation in the ED. Fortunately, having a final T is for timing/temporal relationships associated with the
diagnosis is not always necessary, as an appropriate dis- pain. Questions include “When did the pain start?”; “How
position with follow-up evaluation and tests during hos- long did the pain last?”; and “What were you doing when
pitalization or as an outpatient may be of much greater the pain started (eating, exercising, watching television,
going to bed)?”
importance.
6 Principles of Emergency Medicine
CUUK1447_01.indd 6 11/22/11 7:52:43 AM
Additional important historical information may be likely explanation than the coincidence of more than
Approach to the emergency patient
obtained using the mnemonic A-M-P-L-T-O-E (Table 1.3). one disease being responsible for a patient’s illness.
Additional caution is needed when evaluating patients
Table 1.3 A-M-P-L-T-O-E mnemonic for additional history at the extremes of age (newborn and elderly), as the
likelihood of serious infection and comorbid or coexist-
A is for allergies to medications, food, latex, seasonal
allergens, or other things. ing conditions is greatly increased. This is also true for
M is for medications, including prescription and non-
immune-compromised patients and others without phys-
prescription. Surprisingly, many patients do not consider iologic reserve (morbidly obese, postoperative, malnour-
acetaminophen, ibuprofen, oral contraceptives, insulin, ished, diabetic, steroid-dependent, or often those with
vitamins or herbal remedies to be medications, and do not mental illness). Some key associated symptoms are listed
offer this information. in Table 1.4. Warning signs in the history are provided in
P is for previous or past medical history, which may provide Table 1.5.
a clue to the present condition. If this patient has had a
similar illness before, he or she may have it again or is at
greater risk for it to recur. Table 1.4 Key associated symptoms
L is for last meal, perhaps the least helpful of these
questions. Last meal does, however, relate to airway Cardiopulmonary symptoms
protection in the event of procedural sedation or a surgical Cough, dyspnea, orthopnea, palpitations, dizziness, syncope,
procedure. and chest pain
T is for tetanus status, which should be updated every 5–10 Gastrointestinal symptoms
years, depending on the type of wound and its likelihood Abdominal pain, nausea, vomiting, anorexia, constipation,
for being tetanus-prone. diarrhea, and bleeding
O is for other associated symptoms/operations. Associated Genitourinary symptoms
symptoms may assist in reaching a diagnosis and may Dysuria, frequency, urgency, hematuria, and pneumaturia
afford the opportunity to relieve discomfort. Some patients
do not include previous surgeries in their medical history. Obstetric/gynecologic symptoms
Pregnancy, menses, age of menarche, contraception, infertility,
E is for events/EMS/environment, which include the events sexual history, sexually transmitted infections (STI), vaginal
leading up to the illness, the role of emergency medical discharge or bleeding, dyspareunia, previous surgeries, recent
services (EMS) during transport (interventions, response, procedures, and other pelvic infections
complications), and any environmental influences on the
presentation (heat, cold, water, fire, altitude, rave or other Neurologic symptoms
party). Weakness, difficulty speaking, concentrating, swallowing,
or thinking, imbalance, sensory or motor changes, visual
problems, and headache
Information regarding a patient’s family and social
history should also be reviewed. Family members with
similar illnesses or conditions are important to identify. Table 1.5 Ten warning signs in the history
Examples include a strong family history of cardiac or 1. Sudden onset of symptoms (especially first time)
thromboembolic disease, appendicitis, gallbladder dis-
2. Significant worsening of symptom(s) that had been stable
ease, bleeding disorders, or cancer. Social history includes
the patient’s living situation; marital status; use or abuse 3. True loss or alteration of consciousness
of tobacco, alcohol, and/or drugs; occupation; and hand- 4. Cardiopulmonary symptoms (dyspnea, chest pain or
edness (in the setting of neurologic disease or extremity pressure)
trauma). 5. Extremes of age (newborn, elderly)
Several key questions might therefore include:
6. Immune compromise (HIV-positive, AIDS, cancer, diabetes,
• How did the pain begin (sudden vs. gradual onset)? or on immunosuppressant therapy such as chemotherapy
• What were you doing when the pain began? or chronic steroids)
• How would you describe your pain? 7. Poor historian, including language barriers
• On a scale of 0–10, how severe is the pain? 8. Repeated visit(s) to a clinic or ED, especially recent
• Where is your pain?
9. Incomplete immunizations
• Has it always been there?
• Does the pain radiate anywhere? 10. Patient signed over at the end of a shift
• Does anything make the pain better or worse?
• Have you had this pain before?
• Have any family members had pain similar to this?
• What do you think is the cause of your pain? Physical examination
Associated symptoms are important, as many diseases
have a specific collection of symptoms associated with The physical examination for emergency patients should
them. The concept of parsimony is an important one, in be complete to identify unexpected conditions, with spe-
which a diagnosis has a higher likelihood of being cor- cial focus on areas likely contributing to or responsible for
rect if one disease can be used to explain the entire con- disease. Unfortunately, many EPs are challenged for time
stellation of associated symptoms. This provides a more and must act quickly, performing abbreviated physical
Principles of Emergency Medicine 7
CUUK1447_01.indd 7 11/22/11 7:52:43 AM
examinations while relying on laboratory and radiology ibuprofen if they are now well-appearing, playful, and at
Approach to the emergency patient
studies. In some circumstances, this may be necessary. low risk for a febrile seizure. Orthostatic vital signs (heart
However, it is best to do a detailed, problem-pertinent rate and blood pressure in supine, sitting, and standing
physical examination so that important findings are not positions) are inherently time-consuming, unreliable, and
missed. In addition, concentrating on associated organ nonspecific. However, if the situation suggests that these
systems that may have a role in the illness is recom- measurements would be in the patient’s best interest, they
mended. These areas may provide clues to the etiology of may provide useful information. It is good practice to
the pain or illness. In fact, establishing a comprehensive recheck a patient’s vital signs prior to discharge. Table 1.6
differential diagnosis for each complaint and examining provides a list of vital signs to consider in the ED.
areas of the body that may contribute to it allow EPs to
prioritize the likelihood of other diagnoses causing the Table 1.6 Sixteen vital signs to consider in the ED
symptoms. 1. General appearance (perhaps the most important and
As this chapter describes the approach to the emer- underutilized vital sign)
gency patient, it addresses only general appearance, vital
2. Temperature (rectal temperature should be considered
signs, and general physical examination pearls. Other in newborns or infants, the elderly who are hypothermic,
chapters provide details for specific conditions or constel- tachypneic and mouth-breathing, or in patients with
lation of symptoms. alterations of consciousness)
3. Heart rate (including strength, quality, and regularity)
General appearance 4. Respiratory rate (often miscalculated due to multiplication
error)
This may be the most important element of the physical 5. Blood pressure (consider orthostatic BP, although may be
examination for EPs, as it assists with determining who is falsely negative; also consider BP measurements in each
sick and who is not. Experienced EPs can look at patients arm or upper and lower extremities in certain conditions)
and have a reasonably accurate idea of who needs to be 6. Oxygen saturation (pulse oximetry)
hospitalized. This is one reason why EPs are concerned 7. Blood sugar (bedside glucose), which provides an
about patients in the waiting room whom they have immediate value for situations including an altered LOC,
not yet visualized. General appearance is particularly a diabetic with the likelihood of abnormally high or low
important in the pediatric population, as social interac- glucose, or when glucose is the only blood test necessary
tion, alertness, playfulness, physical activity (including 8. Pain score (from 0–10, or happy–sad faces scale),
strength of cry), respiratory effort and hydration status repeated frequently and after interventions as indicated
(e.g., amount of tears) are significant findings that can be 9. GCS (best eye opening, verbal and motor responses)
identified within moments. The younger the patient is, from 3–15, or other methods that measure LOC or mental
the more difficult it is for EPs to determine wellness based status, such as AVPU or mini-mental status examination
on general appearance alone. The fact that a patient’s gen- 10. Visual acuity (for patients with visual or certain neurologic
eral appearance is less helpful to EPs at the extremes of complaints)
age makes caring for these patients more challenging. 11. ETCO2 (to identify ventilatory status, especially for all
intubated patients and during procedural sedation)
12. Fetal heart tones (for pregnant patients)
Vital signs
13. Peak flow (for asthmatic patients or those with difficulty
Vital signs are important for all emergency patients. breathing)
A complete set of vital signs should be obtained and 14. Bedside pulse CO-oximetry (when carbon monoxide
repeated at least once during the emergency visit. Often, exposure is suspected)
the vital signs are obtained in triage and not repeated until
15. IOP (for suspected glaucoma)
many hours later when patients are placed in examina-
tion rooms. Many EDs have policies that vital signs must 16. Compartment pressure (for patients with suspected
compartment syndrome and vascular compromise)
be repeated at certain intervals on patients in the wait-
ing room. Though this is a wise strategy, abnormal vital AVPU: alertness, verbal response, pain response,
signs may not require action, and normal vital signs may unresponsive; BP: blood pressure; ETCO2: end-tidal
carbon dioxide; GCS: Glasgow Coma Scale; LOC: level of
accompany serious illness. EPs should at the very least consciousness; IOP: intraocular pressure.
review one complete set of appropriate vital signs on every
patient and address each abnormal vital sign (or consider
why it is abnormal). At times, rechecking the vital signs
is extremely important, such as the heart rate in a patient
with ACS or acute myocardial infarction (AMI), the respi-
Pearls specific to the physical
ratory and heart rates in patients with difficulty breathing, examination
or the temperature of a child who experienced a febrile
seizure. It is of far greater importance to recheck the tem- Be professional
perature of a previously afebrile patient with a possible
surgical condition or serious bacterial infection (SBI) than A professional greeting and introduction should evoke
a febrile child’s temperature following acetaminophen or warmth and kindness. Patients want to know that the
8 Principles of Emergency Medicine
CUUK1447_01.indd 8 11/22/11 7:52:43 AM
EP they “have” (they did not “choose”) is consider- Be thorough
Approach to the emergency patient
ate, sensitive, thoughtful, competent, and listens well;
in other words, a true professional. Most patients aren’t This is important so that critical findings or other clues to
interested in a joke or a discussion of current events the patient’s final diagnosis are not missed. For example,
when they are in the ED, at least not immediately. EPs lacerations, contusions or bruises might imply intimate
should wash their hands when entering each patient partner violence. If it is relevant to the presenting complaint,
room, preferably so that patients can witness this. They expose the patient’s skin during the examination of the body
should wear clean and appropriate physician clothing; region. Rashes may be present that identify life-threatening
be polite, well-mannered and well-groomed; and appear infectious diseases or may eliminate the need for further
well-rested. A current hospital ID badge with name and diagnostic studies (e.g., meningococcemia or herpes zoster).
photograph should be prominently displayed. A health Always examine the joints above and below an injured area,
care provider should never bring food or beverages into as injuries may coexist due to transmitted forces. Remove all
the examination room. constricting jewelry and clothing distal to an injured area, as
swelling due to dependent edema is likely to occur. Patients
may not appreciate this gesture at the time, but it is valuable
Go slowly in terms of patient safety and preventing damage to an item
that may require removal later. Make sure that any removed
Try not to rush patients, or seem rushed to them, despite
item is given to the patient or a family member.
how busy you may be. Speak slowly and clearly, with
increased volume for elderly patients should they need
it. Warm and clean hands are essential for patient com- Be thoughtful
fort. If you are using gloves, let patients know that this is
your practice for all patients. A well-lighted, warm room Use language that patients and family members under-
(if possible) is also preferred. Having a chaperone of the stand. It does not impress patients when physicians use
same gender as the patient present is always a good technical jargon to look smart. If patients are not familiar
idea, especially during examination of private areas, with abbreviations or terms that you have used, they may
such as the genitalia, rectum and breasts. Let patients not be comfortable asking for their meaning. For exam-
know that this is your standard practice and you are ple, despite the common use of the abbreviation “MI” for
doing it for their benefit (even if you are doing this to myocardial infarction, many people do not know what this
protect yourself). Having translators or family members means. You may tell a patient that he had an MI, only to be
present (when appropriate) also makes patients more asked later if he suffered a heart attack. In children, involve
comfortable. parents with the examination, such as looking in a par-
ent’s throat or ear first. Other skills to use when examining
children include letting the child touch your stethoscope
Be gentle or otoscope before using it. Involve older children in the
examination by asking which ear they prefer be examined
Do not proceed immediately to the area of pain, and first. Recognize that hospital gowns are not flattering; it is
do not palpate a tender area using more pressure than thoughtful to assist a patient by offering to tie his or her
is absolutely necessary. If possible, attempt to distract gown, especially if they are getting up from their gurney.
patients while examining a painful area. This is especially
true for pediatric patients.
Be efficient
Be sensitive An entire physical examination does not need to be done
on every patient. For example, funduscopy does not need
Make patients aware that your focus is on them during to be performed on a patient presenting with an ankle
your examination, not on other patients with other prob- injury. Furthermore, examining patients starting with the
lems. Furthermore, let patients briefly know what you position they are in rather than the traditional head-to-toe
find immediately following each phase of the examina- method saves time. For example, if the patient is supine,
tion. There is no reason to do your entire examination consider examining their abdomen before their lungs.
and then tell the patient that it was normal. Share with
patients that their heart or lungs sound fine immediately
after auscultation. If patients have abnormal findings,
they may be aware of these from a previous physician’s Differential diagnosis
examination. If they were unaware of this finding, avoid
accusing their physician of missing something. When Following a thorough history and physical examination
appropriate, promptly tell them that it is not danger- with careful review of the vital signs, a differential diag-
ous or worrisome if this is the case. There is no reason to nosis should be established. This differential diagnosis
increase their anxiety by telling them they have a heart should be as comprehensive as possible, as it suggests
murmur if it is inconsequential. Offering findings in this which diagnostic tests should be obtained, and in which
manner increases patients’ confidence in your abilities, order. This differential diagnosis also establishes which
especially when you identify a heart murmur that they therapeutic approaches should be initiated, if they have
knew existed. not already begun.
Principles of Emergency Medicine 9
CUUK1447_01.indd 9 11/22/11 7:52:43 AM
radiographs; and several head computed tomography
Diagnostic testing
Approach to the emergency patient
(CT) rules (see Appendix A). Depending on the situation,
nurses generally use extremity rules in their practice,
Diagnostic testing in the ED is performed to identify whereas physicians apply decision rules for C-spine and
(“rule in”) or exclude (“rule out”) conditions responsible head CT.
for the patient’s symptoms. As such, it is imperative that
EPs have a notion of pretest probability, including disease
incidence and prevalence, and the sensitivity, specificity,
positive and negative predictive values, and accuracy of Electrocardiography
the tests they are ordering. It is also helpful to be familiar
with likelihood and odds ratios. It is a good idea to review old ECGs whenever possible
and compare these with the new (current) ECG. This is
of particular importance in patients with abnormal con-
duction, abnormal intervals, or abnormal ST and T wave
Laboratory studies segments. ECGs should be repeated in the ED if patients
develop chest pain or if their chest pain resolves, whether
Because of the time pressures for patient dispositions, spontaneously or following intervention. The importance
many tests now can be performed at the bedside to of serial ECGs cannot be overemphasized in the setting
decrease the turnaround time for results. Classic examples of ACS or chest pain possibly of cardiac etiology. ECGs
of point-of-care testing are the bedside (fingerstick) glucose are invaluable in patients with acute ST-segment eleva-
and urine dipstick or pregnancy (hCG) tests. Numerous tion MI (STEMI), as the decision to pursue thrombolysis
implications of this rising technology’s role in EM have or percutaneous coronary intervention (PCI) is influenced
been studied. Extensive research using new bedside tests by the timing of the first diagnostic ECG. They also serve
for cardiac markers and other tests of cardiac function as useful adjuncts in the evaluation of several toxic inges-
is ongoing. Treadmill tests on low-risk cardiac patients tions or presenting symptoms, such as weakness, dizzi-
have been performed from (or in) the ED to risk-stratify ness, abdominal pain, back pain, confusion, or alterations
patients regarding their need for hospitalization or further of mental status.
testing. The role of nuclear medicine testing has increased
tremendously in diagnostic cardiac evaluation from the
ED, perhaps in part due to its decreased role in the diag-
nostic evaluation of pulmonary embolism. Bedside ultra- Radiologic studies
sonography is a test being utilized by EPs with increased
frequency to assist with patient diagnosis, treatment, and All physicians seem to rely on diagnostic imaging to a
disposition. As more EDs subscribe to these practices, and greater extent than they did years ago. This has many
more EPs gain skills in these areas, these tests will assume factors, including the greater role imaging plays in
an even greater role in the evaluation and treatment of patient care, the increased availability of CT scanners,
emergency patients. Unfortunately, government regu- the manner in which physicians are currently trained,
lations have removed some tests from the ED that were and the increased concern over litigation. Diagnostic
previously performed there. Having these tests done in imaging (especially CT) has become a standard that
a laboratory increases the time to receive results, if for no physicians must accept and that patients often demand.
other reason than sample transport time. The implica- Failure to order radiologic studies to identify certain
tions of increased laboratory and radiology turnaround conditions may be indefensible, as these tests are sen-
times are enormous given ED closures, lack of ED and sitive, specific, and readily available 24 hours a day in
hospital bed availability, and increased patient volumes nearly all EDs. The development of guidelines to help
in EDs across the United States. determine which patients require X-rays has provided
Some tests are being ordered or performed by certified physicians the ability to safely reduce the number
nurses during the triage process, where patients regis- of radiographs ordered. Physicians and patients
ter for evaluation and wait for EPs. These tests include should be cognizant of the implications of radiation
urine collection to screen for pregnancy, blood, or infec- exposure.
tion; ECGs to evaluate cardiac function; and radiographs. EPs use bedside ultrasonography as part of their phys-
Often nurses use protocols to order blood tests from the ical examination skill set in many hospitals, often with the
triage area, and several high-volume EDs have EPs eval- support of radiology. This situation arose out of the need
uating patients in the triage area to assist with patient for EPs to have ultrasound available for their patients on
throughput. Research has developed rules that health a 24-hour basis. Limited focused bedside sonography by
professionals may use to determine a patient’s need for EPs can identify hemoperitoneum following abdominal
X-ray. If these clinical criteria are met, trained nurses in trauma, abdominal aortic aneurysm (AAA), gallblad-
many institutions may order X-rays from the triage area der disease, cardiac tamponade, intrauterine (and pos-
in an effort to streamline care and reduce overall patient sibly ectopic) pregnancy, DVT, foreign body or abscess,
time in the ED. Examples of some rules found in the lit- ocular problems, and pneumothoraces, to name a few.
erature include the Ottawa ankle, knee, and foot rules; the Ultrasound research by EPs is identifying additional
Pittsburgh knee rule; the NEXUS rule for cervical spine pathology important for emergency care. EPs first used
10 Principles of Emergency Medicine
CUUK1447_01.indd 10 11/22/11 7:52:43 AM
bedside ultrasonography for the focused assessment with occur simultaneously. It may be necessary to determine
Approach to the emergency patient
sonography in trauma (FAST) exam. Tremendous suc- a patient’s resuscitation status in an instant. Attempts
cess with this limited use encouraged EPs to incorporate should be made as quickly as possible to learn this infor-
ultrasound technology into other necessary areas of their mation from the patient, prehospital care providers, fam-
clinical practice. It is important for both EPs and radiolo- ily members, nursing home or skilled facilities. Advance
gists to work collaboratively in this area, keeping patient directives or durable powers of attorney may provide this
advocacy and safety and not financial matters the first information. Having a system in place with electronic
priority at all times. medical records or a designated individual (social serv-
ices, ED tech, or nurse) to make calls may save precious
minutes. When in doubt, always do what is medically
indicated for the patient, rather than making assump-
General treatment principles tions that may be incorrect. Remember to do no harm,
and always relieve pain, suffering and anxiety.
When evaluating and treating patients in the ED, it is Adequate pain control is an important element of EM
imperative to address life-threats first. A tremendous practice. If a patient has a painful condition, it is good
amount of information can be obtained from the patient’s practice to address issues of pain control as early as pos-
general appearance, vital signs, and history of presenting sible. This is true not only for patients presenting with
illness (HPI). This assessment takes less than 1 minute. abdominal pain, but in patients with traumatic injuries
Risk stratification into “sick” or “not sick,” or “stable” or who would benefit from adequate analgesia. Waiting to
“unstable” is part of this process. Attention to the ABCs administer pain medication to a patient with a clinical
(airway, breathing, circulation) is critical, as is having fracture until after the X-ray is reviewed is inappropriate.
the correct personnel, equipment, and monitoring avail- Reassess patients after each intervention, whether follow-
able. Much of this process occurs simultaneously, often ing intubation for airway control or the administration
automatically, with more than one health care provider of analgesia. Continued reassessment of all patients is
involved. While nurses and techs measure vital signs, critical, particularly the sickest or those at greatest risk of
connect patients to monitors, and start peripheral intrave- decompensating.
nous (IV) catheters for blood draw and circulatory access, All patients should be treated sensitively, with attention
physicians can intervene with airway management and paid to their fears and anxieties. Patients don’t wish to be
assess breathing and circulation. In trauma patients, the in the ED, where privacy concerns, noises, and discom-
mnemonic ABCDEFG is addressed in the primary and fort predominate. They would much rather be at home
secondary surveys (Table 1.7). without pain, or in a familiar physician’s office. In this
sense, EPs and EDs start out with strikes against them.
Table 1.7 ABCDEFG mnemonic for trauma patients
Additionally, long waits, uncertainty, and any unpleasant
interactions are rarely interpreted favorably by patients.
A Airway Respectful treatment, without discrimination or conde-
B Breathing scension, should be integral to our approach towards all
C Circulation patients.
D Disability (neurologic) The American College of Emergency Physicians
E Exposure (ACEP) and other organizations have developed a
F Foley (following inspection of the perineum and rectal number of clinical policies by consensus in an attempt to
examination, provided contraindications absent) improve patient care and reduce medical error. Although
G Gastric decompression (provided contraindications many EPs feel that these policies might be used against
absent) them in litigation, or are an attempt to standardize patient
care, these policies were established using research and
opinion, and are excellent resources. This is especially
Cervical spine immobilization and protection is part true for policies addressing complex conditions or those
of the primary survey. “F” also reminds us of the impor- with unclear or rapidly changing diagnostic and treat-
tance of family and friends. They may provide informa- ment approaches. These policies are generally available
tion about the circumstances leading up to the present at no charge. Many similar treatment guidelines are avail-
condition, and should be kept updated as much as pos- able on-line to assist providers with an evidence-based
sible. When caring for pediatric patients, current litera- medicine (EBM) approach to patient care.
ture demonstrates that family members’ presence during
resuscitation efforts or invasive procedures is extremely
important, provided their presence does not interfere
with medical care delivery. Special patients
At times, histories and physical examinations must be
abbreviated and more focused than one might prefer. This Elderly
is often a necessary part of EM practice. Treatment may
need to be initiated based on limited information, previ- Individuals over 85 years of age are the fastest growing
ous episodes, physician experience, or physician specu- segment of the population. With advances in medical
lation. In true emergencies, assessment and treatment care and the increasing importance placed on disease
Principles of Emergency Medicine 11
CUUK1447_01.indd 11 11/22/11 7:52:43 AM
prevention, diet and exercise, this portion of the popu- on their stools turning darker (hematochezia or melena).
Approach to the emergency patient
lation will continue to grow at a tremendous rate. The Decreased flexibility of the neck and spine makes it chal-
majority of medical care expenses are spent on the geriat- lenging for elderly patients to look in the toilet for changes
ric population during their last few years of life. Geriatric in their stool. Driving abilities may be impaired by vis-
patients are at risk for falls, functional decline, and ual difficulties or by arthritis (which makes it difficult
changes in cognition, as well as cardiac, pulmonary and to change lanes), muscle power (required for defensive
vascular emergencies. They have reduced physiologic maneuvers), fine motor control, coordination, or response
reserve and often are too ill, weak, or complicated to use time (to avoid collisions). Driving is vital to their inde-
medical offices for even routine care. As such, many eld- pendence, and many elderly are unwilling to relinquish
erly individuals depend on EDs for their overall health this activity.
care, if they get care at all. When geriatric patients present Falls are more common in the elderly, not only
to the ED, they are far more likely to be admitted to the because of visual difficulties, but also because of their
hospital than younger patients. They are also far more diminished ability to avoid objects, climb stairs, or
likely to require and benefit from social services if dis- maintain balance and posture. As financial issues are
charged. The best solution is to integrate social services of great concern, medications may not be taken regu-
into the care of all geriatric patients. EPs should consider larly or may be cut in half to decrease the cost. The same
why social services should not be asked to see an elderly goes for food – soups are inexpensive and easy to cook,
patient in the ED, as home safety checks, access to meals, although many have high sodium content. A dietician or
transportation to medical appointments, social isolation, nutritionist can discuss healthy eating habits with eld-
depression, financial security, and feelings of being a bur- erly patients. Plans for assisted living or skilled facili-
den to family members can be addressed. Furthermore, ties should be addressed with geriatric patients before
elder neglect or abuse is far more prevalent than reported. the need is imminent, as should advance directives
From a social perspective, geriatric patients prefer being and powers of attorney. Even a discussion of wills and
referred to as “young” rather than “old” (as in 75 years plans for death should be addressed, although this is
young), and prefer being referred to as “older” rather best done at a scheduled time in the primary care pro-
than “old.” vider’s office. Postal carriers, apartment managers, or
Many medical conditions in older patients do not neighbors are particularly important to the safety of the
present as they might in a younger or healthier patient. elderly population who live alone, as they can check to
A UTI in an elderly patient may present with confusion, see that mail is picked up daily, make sure that the indi-
as might ACS or pneumonia. Many geriatric patients are vidual has eaten or gotten up that morning, or provide
not able to mount a febrile response to sepsis or infec- brief social contact. These resources can be investigated
tions. In fact, geriatric patients are often hypothermic by social workers.
when septic. As a result, rectal temperatures should be
frequently measured in this population. Geriatric patients Pediatric
commonly use over-the-counter medications; on aver-
age, elderly patients take five prescription medications Pediatric patients often make up a high percentage of
daily. Polypharmacy is a frequent concern, and there- patient visits to an ED, especially at night when pediat-
fore increases the likelihood of drug–drug interactions. ric clinics are closed and parents are home from work.
Primary providers are often unaware of all medications Many EDs have separate patient care and waiting areas
their elderly patients take, as physician colleagues, con- for pediatric patients so they are not as frightened during
sultants, and urgent care providers may prescribe addi- their visit. Some EDs have special pediatric rooms with
tional medications without sharing this information. colors and decorations to improve the overall experi-
Prehospital personnel should be encouraged to bring all ence. Coloring books, stickers and stuffed animals may
medication bottles with patients to the ED so they can be be helpful as well. It is inadvisable to have a belligerent
reviewed. This may help identify potential adverse drug patient sharing a room with a child (or any patient, for
interactions, as well as prescriptions of the same medica- that matter). EDs should have a resuscitation area and
tion (or class) with different names. Many drugs interact equipment especially for children, with color-coded
with warfarin, a common prescription in the geriatric equipment storage matching the colors on the Broselow
population. Special ID bracelets should be provided to resuscitation tape. For computer-based medication order
and worn by elderly patients, with select medical condi- systems, pediatric weight-based dosing may help reduce
tions, addresses, contacts, medications, and allergies. It medication error.
is common to see do-not-resuscitate orders included on Pediatric patients are generally evaluated with parents,
these bracelets. which may help the evaluation or make it more difficult.
Eyesight and hearing often fail in the geriatric popu- It is important to observe the manner in which children
lation. It is therefore important to check these and con- interact with their parents. Physical, emotional, and sex-
sider outpatient referrals to optometry or audiometry. ual abuse or neglect should be considered in all pediatric
Difficulties with eyesight may result in the inability to visits, especially cases of traumatic injury, genitourinary
read food labels or medication instructions, especially complaints, or failure to thrive. At times, it may be neces-
insulin doses. Difficulty with vision in low light makes it sary to have a discussion with a verbal pediatric patient
nearly impossible for elderly patients to reliably comment without a parent present. If this situation is necessary, it
12 Principles of Emergency Medicine
CUUK1447_01.indd 12 11/22/11 7:52:43 AM
is advisable to have a second health care professional, refer aggressively, and recognize other factors that may
Approach to the emergency patient
preferably of the same gender as the child, in the room influence their behavior. Conditions such as reflex sym-
with you. Every attempt should be made to minimize pathetic dystrophy (RSD), fibromyalgia, postherpetic
a child’s time away from his or her parent or guardian neuralgia, claudication, osteomyelitis, abscess, or psy-
unless this separation is warranted. Parents are often chosocial conditions such as abuse or depression may not
concerned about their child’s fever, but their true concern have been considered during prior visits.
may be meningitis or some other serious infection. With
as much certainty as possible, these concerns should be Frequent flyers
addressed. Pediatric patients with ventriculoperitoneal
(VP) shunts, leukemia, cancer, cardiac or lung disease, Patients labeled as “frequent flyers” may or may not have
transplants, seizure disorders, or other specialized con- addiction to drugs and alcohol or psychiatric illnesses,
ditions are generally closely followed by their pediatri- although they often do. However, isolation, homelessness,
cians or pediatric specialists. These individuals should hunger, boredom, mental illness, or searching for atten-
be included in or informed of care decisions as early and tion and care may be reasons for repeat visits. Despite
as much as possible. As younger pediatric patients are overutilizing the ED, these individuals should be treated
at risk for SBI and have less reserve than older children respectfully. Many medical staff fear that nice treatment
or adults, next day follow-up of patients and cultures (if will encourage repeat visits, but providing a meal or a
obtained) should be encouraged according to hospital warm place to sit for a short time may be necessary regard-
practices, as patients in this age group can worsen rap- less of the number of visits. Abuse of the prehospital care
idly or unexpectedly. system is even more upsetting to many emergency medi-
cal personnel, as the number of available ambulances and
Drug-seekers prehospital providers decreases when service is provided
to these individuals. However, it is always possible that
The practice of EM attracts a unique set of patients who frequent flyers have or will have real illness. It is therefore
use and abuse the ED. Patients who seek drugs, whether necessary to carefully focus the evaluation and minimize
they are drug-addicted, drug-dependent, or in con- testing, although studies are often performed despite
stant pain, are common patients seen after clinic hours their high likelihood of being negative. Input from sup-
or when primary physicians are unavailable. Some of port staff and nursing personnel who have frequently
these patients simply have decreased abilities to tolerate interacted with a particular individual may provide clues
pain. Many hospitals and EDs have policies about pro- of a subtle difference in presentation or behavior. The
viding narcotic medication to drug-seeking patients, or use of derisive or condescending language to individu-
patients who have abused the system. It is far easier for als who abuse the medical system is never acceptable.
administrators to write policies for such patients than Respectfully addressing their abuse of the system and its
for EPs to apply them in clinical practice. Whatever the impact on others is certainly warranted. When possible,
outcome, it is always best to be sensitive to a patient’s ED or hospital administrators should be notified of these
condition and to treat patients with respect, whether or abuses using mechanisms that are in place.
not drugs are provided. There have been several situa-
tions in which denying narcotics to a patient demand- Police custody
ing them resulted in injury to or death of health care
providers. Referrals to pain clinics, psychiatry, narcotics Sadly, patients in police custody who need or desire
anonymous, and social services are always appropriate medical attention for evaluation and treatment have no
but rarely helpful. place to go other than the ED (occasionally, some urgent
care centers have contractual agreements for this). Often,
Difficult patients police bring patients to the ED for medical clearance. This
requires an EP to determine whether or not the patient’s
Patients with Axis II disorders, malingerers, manipulators, actions can be explained by a medical or psychiatric con-
litigious patients, and patients with behavioral problems dition. Patients often come to the ED in police custody
often use the ED for their health care. These individuals with injuries following an altercation, often with a police
may not have insurance, may not have access to clinics, officer or officers. This establishes a difficult context for
or may enjoy the attention given to them in the ED. These EPs because officers may have injured certain patients in
patients are particularly challenging to the medical staff. response to their aggressive behavior. This is especially
Federal law prohibits EDs from turning away patients true given the increased use of TASER® technology. If
without first performing a medical screening examina- the EP feels safe, he or she should interview patients
tion (MSE) to evaluate for an emergency medical condi- outside of police presence. It is always difficult to feel
tion (EMC). At times, security personnel or the police are comfortable evaluating patients handcuffed to gurneys,
required to control these challenging patients. In our role with or without police present. However, a thorough yet
as the physicians for health care’s safety net, EPs must cautious evaluation for injuries, including contusions,
interact with these unique and challenging patients on a bruises, marks, scratches, abrasions and bites, must be
regular basis given the ED’s open-door policy. An EP’s performed and documented. Patients may be placed into
goals are to be respectful and professional, set strict limits, police custody from the ED if they are violent, abusive,
Principles of Emergency Medicine 13
CUUK1447_01.indd 13 11/22/11 7:52:43 AM
stealing supplies, or exhibiting inappropriate behavior. to the violent patient is critical to help reduce the likeli-
Approach to the emergency patient
Police must be notified about all violent injuries, and hood of potential harm.
may place patients in custody or take them from the ED
to jail. Police often deliver intoxicated patients to an ED
so they can sober before going to jail. Patients who are
intoxicated may have additional reasons for combative Disposition
behavior or altered mental status, including traumatic
brain injury, hypoglycemia, hypothermia or other medi- Consultation
cal conditions, thus mandating a thorough evaluation.
Intoxicated patients may be released to the care of the Dealing with consultants is an art that is often difficult.
EP and medical staff if they have cooperated with the Consultants respect straightforward, focused, and well-
police and are not under arrest. When this occurs, care- planned presentations with a direct question or goal
ful observation until daylight hours, a meal if possible, clearly stated. However, they are unlikely to appreciate
and careful plans for disposition, follow-up, and refer- being told what to do, such as “this patient needs to go to
ral should be discussed with a non-intoxicated family the operating room” (even when this is clearly needed).
member or friend. Clearly, a close working relationship On the other hand, depending on the culture of your
between fire, police and emergency personnel is crucial institution, this direction may be helpful and appreciated
to our safety and success. for trauma or other critically ill patients. Every consulta-
tion is unplanned work for a consultant. Reimbursement
issues may negatively impact consultants to a far greater
Violent patients extent than most EPs recognize. Despite such issues, EPs
Unfortunately, patients may become violent while in the must serve as their patient’s advocate at all times. EPs
ED. They may act aggressively towards staff or other should never do something that makes them uncomfort-
patients. This may be due to fear, problems with anger able, even if a consultant recommends it. This is espe-
management, psychiatric issues, alcohol and drugs, cially true if a consultant does not formally evaluate the
or gang-related activities. Any patient who physically patient. Disagreements about the best plan of action for
(and in many cases, verbally) assaults medical person- patients are common. These may be due to financial, time,
nel, another patient or family member, or staff must be or hospital pressures. In general, consultants do not wish
restrained and possibly arrested. Hospital security must to hospitalize patients who, in their opinion, do not need
be notified immediately, as well as the police. Such behav- admission. Because EPs do not wish to send patients home
ior must never be tolerated. Care must be taken to protect who, in their opinion, should not be discharged, conflict
visitors from patients who might cause harm. In addition, may be inherent to this interaction. EPs must always keep
caution must be exercised to prevent visitors from harm- the patient’s best interests in mind. Consider alternate
ing patients, as might occur in situations of abuse or gang options such as holding patients in the ED until the next
violence. consultant comes on duty, finding a different service to
Many patients and visitors bring weapons to the ED, admit the patient, enlisting the assistance of social serv-
having them on their person. Inadvertent discharge ices, admitting the patient to an observation unit (either in
of a firearm or accidental injury from a knife or other the ED or the hospital), or recognizing that it may be safe
sharp object necessitates extreme diligence of all health to send that particular patient home despite your initial
care team members when moving or touching patients. concerns. If absolutely needed, EPs can always contact the
Many EDs have metal detectors and security person- chief of service, administrator on call, or chief of staff for
nel at their entrance, although weapons can still find truly unacceptable situations. When possible, notifying a
their way into the ED. It is recommended that medi- patient’s primary physician or specialist with information
cal personnel position themselves between the door about his or her visit, evaluation, laboratory and radiol-
and the patient at all times so a patient can’t block ogy results, and treatment plan is uniformly appreciated.
their exit. Staff should never place themselves in the This is also in the patient’s best interest. Not only does this
way of potential harm, despite how heroic this might serve as an opportunity for continued care, it also assists
seem. Studies have demonstrated that helpful actions in transferring care for that patient. Follow-up notification
include a calm appearance, non-threatening approach, by EPs to patient’s physicians earns additional respect for
soothing voice, show of both hands (rather than hold- our specialty and is a fantastic way to let other physicians
ing them behind your back), and eye contact that is nei- know that we care about their (our) patients. If interested,
ther intense nor direct (somewhat askew is preferred). request follow-up from these physicians to learn about
When needed, a show of force with multiple large longitudinal patient care outcomes.
individuals may de-escalate a potentially violent situ-
ation. The potential for workplace violence in the ED Serial evaluation
must be recognized at all times. Chemical and physical
restraints are important components of protecting staff Repeat evaluation of patients is an important aspect of
and patients, but are not as easy to use as described emergency care, as a patient’s condition may change over
in the literature. Furthermore, these may not prevent time. Many presentations warrant repeat evaluation,
injury from occurring and may result in injury during including head or traumatic injuries, seizures, hypoglyc-
their application. Therefore, a well-rehearsed approach emic episodes, abdominal pain, shortness of breath, and
14 Principles of Emergency Medicine
CUUK1447_01.indd 14 11/22/11 7:52:43 AM
chest pain. Time may allow a diagnosis to become more if their symptoms worsen, change, or don’t improve. All
Approach to the emergency patient
apparent or declare itself, or may lead to the resolution discharge instructions should include four categories of
of symptoms. It is critical that patients who are impaired instructions: (1) what to do, (2) what not to do, (3) when
(drug or alcohol intoxication, altered mental status, or (and where) to follow-up, and (4) reasons to return to the
confused) or are restrained (chemical, physical, or both) ED. What to do includes instructions such as rest, ice,
have frequent and repeated evaluations by physicians compression, and elevation for an ankle injury. What not
and nurses. Serial evaluation is necessary following to do instructions might include don’t smoke, don’t drive,
interventions, such as the administration of nitroglyc- don’t use alcohol, or don’t stop your antibiotics until com-
erin (NTG), analgesics, bronchodilators, or anxiolytics. pleted or instructed by your physician. When (and where)
This is important not only to determine the patient’s to follow-up for re-evaluation, and with whom, is benefi-
response to that intervention, as many interventions cial information for discharged patients. The time frame
are diagnostic as well as therapeutic, but also to deter- for follow-up should directly relate to the certainty of
mine whether additional or different interventions are the diagnosis and the likelihood that the illness or injury
needed. Documentation of any response to therapy is will degenerate to a critical condition. Close follow-up is
important, particularly because it records the patient’s important for all patients with high-risk medical condi-
ED course. Repeat evaluations of patients after impor- tions and comorbidity. The ideal situation is to schedule
tant laboratory or X-ray results become available, and/ a follow-up appointment for the patient at the time of his
or before they are discharged is recommended, although or her discharge. Give the patient this follow-up physi-
the extent of this reevaluation differs with each clinical cian’s name, the date and time of the appointment, and
scenario. the address with directions to the clinic. Perhaps the most
important discharge instruction is the list of reasons to
Admission/discharge return to the ED. These might include but are not limited
to any increase in pain, new or different pain, worsening
The decision to admit or discharge a patient from the of symptoms, inability to take medications or fluids, aller-
ED is perhaps the most challenging aspect of EM prac- gic reactions to any medications, fever, vomiting, bleed-
tice. Multiple factors must be considered in this deci- ing, or any other concerns or fears. Preprinted discharge
sion, including psychosocial, biological, medicolegal, instruction sheets are helpful if they are written in a lan-
and, unfortunately, financial. When feasible, a patient’s guage and at a level that patients can understand. These
wishes should be included in this decision. With the allow EPs to be more efficient. However, patients deserve
advent of more aggressive outpatient strategies, such personalized instructions as well, as each patient is an
as low-molecular-weight heparin for DVT therapy and individual, not a disease or set of symptoms. It is best
longer-acting antibiotics with greater potency for many when someone reviews these instructions with a patient
infections, and research suggesting similar outcomes in prior to discharge.
selected patients, many patients who were previously hos- Assisting patients with filling their prescriptions at
pitalized may now be safely treated as outpatients with discharge is important, although this does not necessarily
close follow-up. This greatly expands the role of EPs. ensure compliance. If this is not possible, discharging
Since disposition strategies for certain conditions vary patients with a 1- or 2-day supply of medication is rea-
between hospitals and admitting physicians, it is a good sonable. Testing a patient’s gait prior to discharge helps
idea for EPs to familiarize themselves with hospital or determine their balance, coordination, and likelihood
community practices. In smaller hospitals, EPs may be of success at home. If a patient walked in to the ED, or
responsible for writing admission orders for patients. “should be able to walk,” then this patient should be able
Although EM organizations discourage this practice, to walk at discharge. Patients should be discharged to a
it still occurs. Admission orders written by EPs should safe environment, preferably in the company of a respon-
clearly transfer the care of the patient to the admitting sible adult who also understands the discharge instruc-
physician immediately upon the patient’s arrival to the tions. If they have been in the ED for an extended period,
floor. The nurses should be instructed to notify the admit- providing a meal is appropriate, as they may be too ill or
ting physician upon the patient’s arrival, if the patient tired to prepare one for themselves upon returning home.
has any special needs, or for any change in vital signs, Staff should assist patients to their vehicle, by wheelchair
including pain. Unstable or particularly complex patients if necessary. Patients should not drive if they might be
should remain in the ED until the admitting physician has distracted, were given medication that may interfere with
the opportunity to evaluate them. In some hospitals, EPs driving, or presented with a lapse of consciousness that
on duty are responsible to respond to in-hospital medical may recur without warning. In this last situation, a report
emergencies. Hospital or ED policies should set guidelines must be filed with the appropriate authorities, and the
to define the circumstances under which the EP does and patient needs to be informed of this. They should not drive
does not respond to acute medical care situations within until an appropriate physician and the proper authorities
the hospital. Similarly, hospital policies should address approve this at a follow-up appointment. Transportation
acceptable time standards for admitting physicians to home or to a shelter may be necessary, often paid for by
evaluate their patients so they do not remain in the ED for the ED or hospital. A clean or warm set of clothes or shoes
extended periods. may be needed. If the hospital or ED budget does not pro-
For patients being discharged, clear and legible dis- vide for this, donations from the medical staff or other
charge instructions should encourage patients to return sources should be solicited.
Principles of Emergency Medicine 15
CUUK1447_01.indd 15 11/22/11 7:52:43 AM
• Use caution in patients with language or cultural
Pearls, pitfalls and myths
Approach to the emergency patient
barriers. Translators and family members may
not provide complete or accurate information,
• Always address life-threats first, including patient details which you might have been able to elicit
and staff safety. if these barriers did not exist. This is especially
• An exact diagnosis is not always possible in EM, and true for patients who are deaf or have speech
not always necessary. An appropriate disposition, impediments.
such as admission to a monitored bed, intensive care • Think about abuse or neglect in every case. If you
unit (ICU), operating room, skilled nursing facility aren’t thinking about it, you will not uncover it.
(SNF), or discharge home with close follow-up and • Document appropriate findings in the medical record
reasons to return is acceptable. clearly, including repeat examinations, laboratory
• Not all is what it seems in EM; expect the unexpected, results and radiograph interpretations, discussions
or you won’t identify it. Consider alternative with consultants or primary care providers, and
diagnoses and the possibility of lab error or false- discharge instructions. Documenting a consultant’s
negative (or false-positive) test results if things name, service, time you spoke, and brief summary of
don’t make sense. Repeat tests if the original test the conversation is prudent.
result doesn’t “fit” with what you expected. Be wary • Consider dangerous outcomes or the worst-case
about the wrong test results being placed in the scenario in every patient. Minimize the likelihood of
wrong patient’s chart, or a laboratory specimen or these outcomes with appropriately focused histories,
radiograph being mislabeled, improperly marked, or physical examinations, laboratory and radiograph
incorrectly collected. ordering and interpretation, and disposition. Never
• Attempt to get the appropriate service or consultant do something you are uncomfortable doing, even if a
involved when necessary to improve patient consultant or colleague recommends it.
outcome. This is often required before all laboratory • Enjoy the privilege of providing emergency care to
or X-ray results have returned. Make every effort all patients and serving in the role of patient care
to inform a patient’s primary care provider about advocate.
the circumstances leading to the ED visit, the care
provided, laboratory and X-ray results, and your
recommended follow-up plan.
• People with psychiatric illness may have medical
illnesses too. Consider ingestions, cardiac, metabolic, References
infectious, and CNS derangements as the cause
of a presenting complaint. This also holds true 1. The 2007 model of the clinical practice of emergency
for intoxicated patients (drugs or alcohol), as medicine: The 2009 update. Perina DG (Chair). Acad
concomitant brain injury or metabolic derangements Emerg Med 2011;18(3):e8–26.
as an explanation for alterations of mental status or 2. Alpert JS. Some thoughts on bedside teaching. Am J
behavior are “present until proven otherwise.” Med 2009;122(3):203–4.
• Many elderly patients have uncommon presentations 3. Brenner DJ, Hall EJ. Computed tomography – An
for common conditions, such as ACS or sepsis. increasing source of radiation exposure. N Engl J Med
Furthermore, polypharmacy and drug–drug 2007;357(22):2277–84.
interactions should be considered, along with elder 4. Carr BG, Branas CC, Metlay JP, et al. Access to
abuse, neglect, depression, and suicidal gestures or emergency care in the United States. Ann Emerg Med
attempts. Consider the safety of an elderly patient 2009;54(2):261–9.
being discharged, and always remain his or her 5. Emergency Care for Children: Growing Pains.
advocate. Social services or safety checks on all elderly Institute of Medicine of the National Academies.
patients presenting to the ED should be encouraged. National Academies Press, Washington, DC, 2007
• Never rush a patient out of the ED with a condition (released June 14, 2006).
that may recur, such as asthma, seizures, chest pain, 6. Emergency Medical Services: At the Crossroads.
breathing difficulty, or alteration of consciousness Institute of Medicine of the National Academies,
(following head trauma or intoxicants). National Academies Press, Washington, DC, 2007
• Be sensitive, sit with patients, make good eye contact, (released June 14, 2006).
and listen well for obvious as well as hidden issues. 7. Finkel MA, Adams JG. Professionalism in emergency
Patients may wait to gain your trust before sharing medicine. Emerg Med Clin North Am 1999;17:443–50.
these concerns. 8. Fontanarosa PB. An evidence based approach to
• Review nursing and EMS notes on all patients. diagnostic testing in emergency medicine. Emerg Med
Look for clues that the patient may not offer or tell Clin North Am 1999;17:1–8.
you. Enlist the assistance of others to help you with 9. Fortuna RJ, Robbins BW, Mani N, et al. Dependence
patient care, including nursing, family, EMS, social on emergency care among young adults in the
services, consultants, or a patient’s primary care United States. J Gen Intern Med 2010;25(7):663–9.
physician. Poison centers and on-line resources may 10. Garmel GM. Conflict resolution in emergency
be extremely valuable as well. medicine. In Adams JG, Barton ED, Collings JL,
16 Principles of Emergency Medicine
CUUK1447_01.indd 16 11/22/11 7:52:43 AM
et al. (eds). Emergency Medicine. Saunders Elsevier, 22. Lambe S, Washington DL, Fink A, et al. Trends in
Approach to the emergency patient
Philadelphia, PA, 2008. the use and capacity of California’s emergency
11. Garmel GM. Interacting with consultants and departments, 1990–1999. Ann Emerg Med
primary care physicians. In Emergency Medicine 2002;39:389–96.
Clerkship Primer: A Manual for Medical Students. 23. Oslin DW. Prescription and over-the-counter
Clerkship Directors in Emergency Medicine, Society drug misuse among the elderly. Geriatric Times
for Academic Emergency Medicine, 2008, pp. 58–61. 2000;1(May/June).
Available at: http://www.saem.org/saemdnn/ 24. Owens PL, Barrett ML, Gibson TB, et al. Emergency
Portals/0/activeforums_Attach/ED%20Primer.pdf department care in the United States: A profile of
(accessed December 10, 2010). national data sources. Ann Emerg Med 2010;56(2):150–
12. Ginde AA, Sullivan AF, Camargo CA. National study 65.
of the emergency physician workforce, 2008. Ann 25. Patel Y, Garmel GM. Management of intoxicated/
Emerg Med 2009;54(3):349–59. violent patients. In Mattu A, Goyal D (eds).
13. Hamilton GC, Sanders AB, Strange GR, et al. Emergency Emergency Medicine: Avoiding the Pitfalls and Improving
Medicine: An Approach to Clinical Problem-Solving, 2nd ed. the Outcomes. Blackwell Pub/BMJ Books, Malden,
Saunders, Philadelphia, PA, 2003. MA, 2007.
14. Hockberger RS, La Duca A, Orr NA, et al. Creating 26. Pitts SR, Niska RW, Xu J, Burt CW. National Hospital
the model of a clinical practice: The case of Ambulatory Medical Care Survey: 2006 Emergency
emergency medicine. Acad Emerg Med 2003;10:161–8. Department Summary. National Health Statistics
15. Holliman CJ. The art of dealing with consultants. J Reports, number 7, August 6, 2008. Available at
Emerg Med. 1993;11:633–40. http://www.cdc.gov/nchs/data/nhsr/nhsr007.pdf
16. Hospital-Based Emergency Care: At the Breaking (accessed December 10, 2010).
Point. Institute of Medicine of the National 27. Pronovost PJ, Faden RR. Setting priorities for patient
Academies, National Academies Press, Washington, safety: Ethics, accountability, and public engagement.
DC, 2007 (released June 14, 2006). JAMA 2009;302(8):890–1.
17. Improving the Education of Health Professionals. 28. Schenkel S. Promoting patient safety and preventing
Josiah Macy, Jr. Foundation 2008 Annual Report. medical error in emergency departments. Acad Emerg
Available at: http://www.macyfoundation.org/ Med 2000;7:1204–22.
docs/annual_reports/macy_annualreport_2008.pdf 29. Schneider SM, Hamilton GC, Moyer P, Stapczynski
(accessed December 10, 2010). JS. Definition of emergency medicine. Acad Emerg
18. Kahn MW. What would Osler do? Learning from Med 1998;5:348–51.
“difficult” patients. N Engl J Med 2009 ;361;5: 30. Tang N, Stein J, Hsia RY, et al. Trends and
442–3. characteristics of US emergency department visits,
19. Kohn KT, Corrigan JM, Donaldson MS. To Err Is 1997–2007, JAMA 2010;304(6):664–70.
Human: Building a Safer Health Care System. Institute 31. Vissers RJ, Kalbfleisch N. The difficult patient. In
of Medicine, National Academy Press, Washington, Marx JA (ed). Rosen’s Emergency Medicine: Concepts
DC, 1999. and Clinical Practice, 7th ed. Mosby, Philadelphia, PA,
20. Korley FK, Pham JC, Kirsch TD. Use of advanced 2010, pp. 2448–57.
radiology during visits to US emergency 32. Xu KT, Nelson BK, Berk S. The changing profile of
departments for injury-related conditions, 1998–2007. patients who used emergency department services
JAMA 2010;304(13):1465–71. in the United States: 1996 to 2005. Ann Emerg Med
21. LaCalle E, Rabin E. Frequent users of emergency 2009;54(6):805–10.
departments: The myths, the data, and the policy 33. Zink BJ. Anyone, Anything, Anytime: A History of
implications. Ann Emerg Med 2010;56(1):42–8. Emergency Medicine. Mosby, Philadelphia, PA, 2006.
Principles of Emergency Medicine 17
CUUK1447_01.indd 17 11/22/11 7:52:43 AM
CUUK1447_01.indd 18 11/22/11 7:52:43 AM
S-ar putea să vă placă și
- Trauma and Emergency Health Care Manual: A Guide for Nursing and Medical StudentsDe la EverandTrauma and Emergency Health Care Manual: A Guide for Nursing and Medical StudentsÎncă nu există evaluări
- Emergency Department Resuscitation of the Critically Ill, 2nd Edition: A Crash Course in Critical CareDe la EverandEmergency Department Resuscitation of the Critically Ill, 2nd Edition: A Crash Course in Critical CareÎncă nu există evaluări
- Disasters and Mass Casualty Incidents: The Nuts and Bolts of Preparedness and Response to Protracted and Sudden Onset EmergenciesDe la EverandDisasters and Mass Casualty Incidents: The Nuts and Bolts of Preparedness and Response to Protracted and Sudden Onset EmergenciesMauricio LynnÎncă nu există evaluări
- Prehospital Practice Hypothetically Speaking: Volume 2 Second editionDe la EverandPrehospital Practice Hypothetically Speaking: Volume 2 Second editionÎncă nu există evaluări
- I.C.U. Chest Radiology: Principles and Case StudiesDe la EverandI.C.U. Chest Radiology: Principles and Case StudiesÎncă nu există evaluări
- Prehospital Practice: hypothetically speaking: From classroom to paramedic practice Volume 1 Second editionDe la EverandPrehospital Practice: hypothetically speaking: From classroom to paramedic practice Volume 1 Second editionÎncă nu există evaluări
- Emergency Medicine Simulation Workbook: A Tool for Bringing the Curriculum to LifeDe la EverandEmergency Medicine Simulation Workbook: A Tool for Bringing the Curriculum to LifeTraci L. ThoureenÎncă nu există evaluări
- Pediatric Cardiology and Pulmonology: A Practically Painless ReviewDe la EverandPediatric Cardiology and Pulmonology: A Practically Painless ReviewÎncă nu există evaluări
- Cardiac Arrhythmia Recognition: an easy learning guideDe la EverandCardiac Arrhythmia Recognition: an easy learning guideÎncă nu există evaluări
- Advanced Practice in Critical Care: A Case Study ApproachDe la EverandAdvanced Practice in Critical Care: A Case Study ApproachSarah McGloinÎncă nu există evaluări
- Ward-based Critical Care: a guide for health professionalsDe la EverandWard-based Critical Care: a guide for health professionalsEvaluare: 4 din 5 stele4/5 (5)
- Advanced Cardiac Life Support (ACLS) Provider HandbookDe la EverandAdvanced Cardiac Life Support (ACLS) Provider HandbookEvaluare: 5 din 5 stele5/5 (1)
- Optimal Life: Essentials of AsthmaDe la EverandOptimal Life: Essentials of AsthmaÎncă nu există evaluări
- ICU Scoring Systems A Complete Guide - 2020 EditionDe la EverandICU Scoring Systems A Complete Guide - 2020 EditionÎncă nu există evaluări
- Cardiac Tamponade, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandCardiac Tamponade, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- Critical Care SedationDe la EverandCritical Care SedationAngelo Raffaele De GaudioÎncă nu există evaluări
- Cardiac Care and COVID-19: Perspectives in Medical PracticeDe la EverandCardiac Care and COVID-19: Perspectives in Medical PracticeÎncă nu există evaluări
- A Nurse's Guide to Caring for Cardiac Intervention PatientsDe la EverandA Nurse's Guide to Caring for Cardiac Intervention PatientsÎncă nu există evaluări
- Procedural & Ultrasound Skills in Emergency Medicine: SLO6De la EverandProcedural & Ultrasound Skills in Emergency Medicine: SLO6Încă nu există evaluări
- Emergency Medical Services: Clinical Practice and Systems Oversight, 2 Volume SetDe la EverandEmergency Medical Services: Clinical Practice and Systems Oversight, 2 Volume SetÎncă nu există evaluări
- Acute Medical Emergencies: The Practical ApproachDe la EverandAcute Medical Emergencies: The Practical ApproachÎncă nu există evaluări
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsDe la EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsÎncă nu există evaluări
- Public Health Nursing: A Textbook for Health Visitors, School Nurses and Occupational Health NursesDe la EverandPublic Health Nursing: A Textbook for Health Visitors, School Nurses and Occupational Health NursesÎncă nu există evaluări
- Nursing Care of the Hospitalized Older PatientDe la EverandNursing Care of the Hospitalized Older PatientÎncă nu există evaluări
- Acute Resuscitation and Crisis Management: Acute Critical Events Simulation (ACES)De la EverandAcute Resuscitation and Crisis Management: Acute Critical Events Simulation (ACES)David NeilipovitzÎncă nu există evaluări
- The Unofficial Guide to Medical Research, Audit and TeachingDe la EverandThe Unofficial Guide to Medical Research, Audit and TeachingÎncă nu există evaluări
- The Nurse Practitioner in UrologyDe la EverandThe Nurse Practitioner in UrologyMichelle LajinessÎncă nu există evaluări
- Advanced Cardiac Life Support Quick Study Guide 2015 Updated GuidelinesDe la EverandAdvanced Cardiac Life Support Quick Study Guide 2015 Updated GuidelinesEvaluare: 4 din 5 stele4/5 (6)
- Advance Cardiac Life Support: Short, Sweet and to the PointDe la EverandAdvance Cardiac Life Support: Short, Sweet and to the PointEvaluare: 3 din 5 stele3/5 (2)
- The Good, The Bad & The Ugly Paramedic Student Handbook: GBU Paramedic, #1De la EverandThe Good, The Bad & The Ugly Paramedic Student Handbook: GBU Paramedic, #1Evaluare: 5 din 5 stele5/5 (1)
- INFECTION CONTROL: Passbooks Study GuideDe la EverandINFECTION CONTROL: Passbooks Study GuideÎncă nu există evaluări
- Emergency Triage: Manchester Triage GroupDe la EverandEmergency Triage: Manchester Triage GroupKevin Mackway-JonesÎncă nu există evaluări
- Pharmacology For Paramedics: Jeremy Maddux, NREMTP, I/CDocument215 paginiPharmacology For Paramedics: Jeremy Maddux, NREMTP, I/CSreejesh RkÎncă nu există evaluări
- Fracture of The Upper HumerusDocument22 paginiFracture of The Upper HumerusOlasinde AnthonyÎncă nu există evaluări
- Anaphy ReviewerDocument19 paginiAnaphy ReviewerGian Paolo P. CHAVEZÎncă nu există evaluări
- Easy Peasy EardrumsDocument52 paginiEasy Peasy EardrumsAnny Aun0% (1)
- Hutchison PaediatricsDocument904 paginiHutchison PaediatricsEcaterina Galagan100% (23)
- Retrograde Urethrography Examination in Penile Fracture: Case ReportDocument3 paginiRetrograde Urethrography Examination in Penile Fracture: Case Reportsofia ayu lestariÎncă nu există evaluări
- Hemato OnologyDocument60 paginiHemato OnologyGousayAlkhazmariÎncă nu există evaluări
- POPS PretestDocument6 paginiPOPS Pretestkingjameson1Încă nu există evaluări
- Management of Chest TubeDocument22 paginiManagement of Chest TubeFatima Hafza SahiddinÎncă nu există evaluări
- Fiji Ministry of Health Requirements For April 2017Document2 paginiFiji Ministry of Health Requirements For April 2017Ahmed KassemÎncă nu există evaluări
- Diarrhea: On This PageDocument6 paginiDiarrhea: On This PageKristine AlejandroÎncă nu există evaluări
- TetanusDocument7 paginiTetanusallah akbarÎncă nu există evaluări
- NeedlestickDocument14 paginiNeedlestickluis_chubeeÎncă nu există evaluări
- No. 3 - NCM 109LDocument44 paginiNo. 3 - NCM 109LDalene EvangelioÎncă nu există evaluări
- A Comparative Study To Assess Problem of Inverted Nipple and Its Relationship To Successful Breast Feeding Among Antenatal MothersDocument9 paginiA Comparative Study To Assess Problem of Inverted Nipple and Its Relationship To Successful Breast Feeding Among Antenatal MothersYunike AdmarialceÎncă nu există evaluări
- Ketidakseimbangan Elektrolit (Corat Coret)Document5 paginiKetidakseimbangan Elektrolit (Corat Coret)jendal_kancilÎncă nu există evaluări
- I. Objectives: GeneralDocument36 paginiI. Objectives: GeneralSharlaine CabanayanÎncă nu există evaluări
- LincosamidesDocument19 paginiLincosamidesManahil RiazÎncă nu există evaluări
- Local AnestheticDocument4 paginiLocal AnestheticAndrea TrescotÎncă nu există evaluări
- Case PresDocument22 paginiCase Presandrei jinÎncă nu există evaluări
- NT Biology Answers Chapter 11Document4 paginiNT Biology Answers Chapter 11ASADÎncă nu există evaluări
- 1 s2.0 S0169409X20301034 Main PDFDocument30 pagini1 s2.0 S0169409X20301034 Main PDFChrispinus LinggaÎncă nu există evaluări
- Edentulous Esthetic Risk Assessment ImplantDocument1 paginăEdentulous Esthetic Risk Assessment ImplantManan AroraÎncă nu există evaluări
- Sesion 2 Articulo Caso Clinico 1 Urticaria PDFDocument16 paginiSesion 2 Articulo Caso Clinico 1 Urticaria PDFQuispe Canares MariangelesÎncă nu există evaluări
- HTP Visual1Document3 paginiHTP Visual1Queeniecel AlarconÎncă nu există evaluări
- Viva GuideDocument27 paginiViva GuideCHIMA ONWUKA MONGÎncă nu există evaluări
- HR Policy ManualDocument34 paginiHR Policy Manualshamna AbdullaÎncă nu există evaluări
- Nursing Care Plan Ineffective Breathing Pattern Hepatic MassDocument2 paginiNursing Care Plan Ineffective Breathing Pattern Hepatic MassRheegell Ellar-Fuertes100% (3)
- Biochemical Composition of Normal Urine: Nature Precedings November 2011Document55 paginiBiochemical Composition of Normal Urine: Nature Precedings November 2011novi rahmawatiÎncă nu există evaluări
- Radioembolization of Hepatic Malignancies - Background, Quality Improvement Guidelines, and Future DirectionsDocument15 paginiRadioembolization of Hepatic Malignancies - Background, Quality Improvement Guidelines, and Future DirectionsVeronica AlexanderÎncă nu există evaluări
- Panic DisorderDocument50 paginiPanic Disorderheshm300020001790100% (3)