Documente Academic
Documente Profesional
Documente Cultură
A Comparison of Oral and Inhal
Încărcat de
Aripin Ari AripinDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
A Comparison of Oral and Inhal
Încărcat de
Aripin Ari AripinDrepturi de autor:
Formate disponibile
Original article Advances in Bioscience & Clinical Medicine
ISSN: 2203-1413 Vol.03 No.02
A comparison of Oral and Inhalant Corticosteroids in Treatment
of Mild to Moderate Asthma Exacerbation in Children
Nemat Bilan1, Lida Saboktakin1, Masoumeh Ghasempour 1*
1. Pediatric Health Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Introduction: Oral corticosteroids are the main treatment in asthma exacerbation. It has been reported
that inhaled corticosteroids can be used instead of oral corticosteroids in asthma exacerbation. We
aimed to evaluate the efficacy of inhaled fluticasone and oral prednisolone in children with mild to
moderate asthma exacerbation.
Materials and Methods: In this randomized clinical trial, 60 children with mild-to-moderate acute
asthma exacerbation visiting emergency department were randomly assigned to receive oral
prednisolone (2 mg/kg) or fluticasone spray (2 puffs every 12 hours, each puff contains 250 microgram
fluticasone) using an spacer for one week. The first dose of the treatment was given in the emergency
department. Children were followed for seven days and signs and symptoms of exacerbation, as well as
spirometry findings were evaluated.
Results: On the days 1 and 3, symptoms including cough, sputum and need for salbutamol during day
was more improved in oral prednisolone and symptoms at night was more improved in inhaled
fluticasone. Patients were almost symptom free on the seventh day. Forced expiratory volume in 1
second, forced vital capacity and forced expiratory flow rate on the seventh day were significantly
better with inhaled fluticasone compared to oral prednisolone.
Conclusion: Both inhaled fluticasone and oral prednisolone improved symptoms during a week after
exacerbation; however, better respiratory function in children treated with inhaled fluticasone is
indicative of its further efficacy compared to oral prednisolone. Considering the low systemic effects of
inhaled fluticasone, this treatment seems to be more appropriate in treatment of mild to moderate
exacerbations.
Keywords: Asthma exacerbation; Inhaled fluticasone; Prednisolone
Introduction
respiratory symptoms (1,2). Asthma is the most
Asthma is one of the most common chronic
prevalent childhood chronic disease requiring
diseases in children worldwide. Asthma is
emergency department (ED) visits due to its
characterized by chronic airway inflammation,
exacerbation (3,4). Treatment of asthma
impaired pulmonary function, and episodic
Corresponding author:
Masoumeh Ghasempour
Tabriz Children's Hospital, Sheshgelan St, Tabriz, Iran
Tel: +984115262280 Fax: +984115262280 E-mail: masoumeh_gh_a@yahoo.com
Receive date: 2014-08-19| Accept date: 2014-09-05| Publish date: 2014-09-29
DOI: 10.7575/aiac.abcmed.15.03.02.03
Australian International Academic Centre, Australia 5|Page
Original article Advances in Bioscience & Clinical Medicine
exacerbations includes early recognition and 2012 and January 2014 were studied. Inclusion
initiation of therapy with bronchodilators and criteria were children between 5-14 years old
anti-inflammatory corticosteroids. Inhaled with a documented diagnosis of asthma for ≥6
rapid-acting β2 agonist (salbutamol) is the months, with mild-to-moderate acute asthma
standard treatment for acute exacerbation exacerbation with baseline FEV1 50% to 79%
especially in young children (5-7). The use of
predicted. Exclusion criteria were children with
systemic steroids is recommended in patients
persistent vomiting, airway instability,
with acute asthma exacerbations who fail to
treatment with oral corticosteroids within 7
respond promptly or completely to short-acting
days, coexistent heart, liver, kidney and chronic
β-agonist therapy (8). Early administration of
pulmonary diseases,
oral corticosteroids can reduce airway
cardiopulmonary/neuromuscular disease, and
inflammation, improve normalization of lung
severe exacerbation requiring intensive care or
function, decrease rates of hospitalization, and
mechanical ventilation or previous treatment in
decrease the number of repeat visits to the ED
the intensive care unit for asthma. We also
(9-12).
excluded patients with any contraindications to
Despite beneficial effects of oral use salbutamol. The study has been approved
corticosteroids, patients’ compliance to drug by the ethical committee of Tabriz University of
use after discharge from emergency Medical Sciences and informed written
department is low because of prolonged course consents were obtained from all patients or
of therapy and potential unpleasant side effects their guardians, controls and their parents
(13-16). Due to the decreased compliance and before including in the study.
acceptance to oral corticosteroid use, it is
In the emergency department, both groups
important to find some other possible
received O2 therapy and salbutamol 2 puffs
alternatives. Nowadays, inhaled corticosteroids
each 20 minutes until the symptoms were
are used as treatment choice in chronic asthma
controlled. Patients were randomly assigned to
(17-21), and it is possible to be used in mild to
two treatment groups using Randlist software.
moderate exacerbation of asthma. It is shown
First group was treated with salbutamol spray
that oral corticosteroids (OCS) compared to
(2 puffs every four hours for 48 hours, each
inhaled corticosteroids (ICS) are more effective
puff contained 100 micro grams of the drug)
in severe asthma exacerbation (22,23).
using an spacer plus oral prednisolone (2
However, studies evaluating the role of inhaled
milligrams/Kg for one week). Second group was
corticosteroids in treating patients with mild to
treated with salbutamol spray (2 puffs every
moderate exacerbation of asthma reported four hours for 48 hours) plus fluticasone spray
some conflicting results (24-29). (2 puffs every 12 hours, for one week, each puff
In this study, we aimed to evaluate the contained 250 micrograms of the drug) using
efficacy of oral and inhalant corticosteroids in an spacer. The first dose of the treatment (oral
treatment of mild to moderate asthma prednisolone or fluticasone spray) was given in
exacerbation in children. the emergency department. Children were
Materials and methods followed on days one, third and seven for any
signs and symptoms of exacerbation.
In this randomized clinical trial, 60 children Spirometry was performed in these periods to
with mild-to-moderate acute asthma evaluate Forced expiratory volume in one
exacerbation visiting emergency department, second (FEV1), forced vital capacity (FVC),
Tabriz Children’s hospital, Iran between May FEV1/FVC and forced expiratory flow (FEF) 25-
Australian International Academic Centre, Australia 6|Page
Original article Advances in Bioscience & Clinical Medicine
75%. Children with persistent symptoms during inhaled fluticasone (n=30). Table 1
study were referred either to our emergency demonstrates baseline findings between
department or to their physicians for groups. Besides being passive smoker which
assessment. Peak flowmetry was also was significantly more in fluticasone group,
performed using peak flow meter to measure there was no significant difference between
the flow of air as it is expelled from the lungs groups in other baseline findings.
and lung function. Symptoms improvement during the days
Statistical analysis and nights 1, 3 and 7 after discharge are
demonstrated in table 2. Children receiving oral
Statistical analyses were performed using
prednisolone were significantly more cough
the Statistical Package for Social Sciences,
free and sputum free in day 3, but in other days
version 17.0 (SPSS, Chicago, Illinois).
there were no significant differences.
Quantitative data were presented as mean ±
Comparing the results, it seems that oral
standard deviation (SD), while qualitative data
prednisolone is more effective in controlling
were demonstrated as frequency and percent
daily symptoms, while inhaled fluticasone is
(%). The categorical parameters were
more effective in controlling night time
compared by χ2 tests, and the continuous
symptoms.
variables were compared by independent t
test. A p value of <0.05 was considered The changes in pulmonary function test
statistically significant. were also evaluated before treatment and 7
days after treatment using spirometry (Table
Results
3). Children receiving inhaled fluticasone had
Sixty children (83.3% male with the mean significantly better FVC in first day and better
age of 7.36±2.09 years) with mild to moderate FEV1, FVC and FEF in the day 7 after treatment.
asthma exacerbation were evaluated in 2
groups receiving oral prednisolone (n=30) and
Oral Inhaled P value
prednisolone fluticasone
Age (years) 7.73±2.30 7.00±1.81 NS
Gender, male 26 (86.7%) 24 (80%) NS
Rhinitis 2 (6.7%) 6 (20%) NS
Sinusitis 10 (33.3%) 4 (13.3%) NS
Gastroesophageal reflux disease 0 5 (16.7%) NS
Passive smoker 4 (13.3%) 11 (36.7%) 0.03
Previous corticosteroid use 24 (80%) 20 (66.7%) NS
Acute asthma exacerbation in the last 2 1.53±0.33 1.34±0.34 NS
years
Table 1: Baseline findings between groups
Australian International Academic Centre, Australia 7|Page
Original article Advances in Bioscience & Clinical Medicine
Oral prednisolone Inhaled fluticasone P value
Cough Day 1 0 0 ----
(symptom free) Day 3 6 (20%) 0 0.02*
Day 7 20 (66.7%) 16 (53.3%) NS
Night 1 10 (33.3%) 8 (26.7%) NS
Night 3 22 (73.3%) 25 (83.3%) NS
Night 7 28 (93.3%) 30 (100%) NS
Sputum Day 1 18 (60%) 14 (46.7%) NS
(symptom free) Day 3 20 (66.7%) 11 (36.7%) 0.03*
Day 7 28 (93.3%) 28 (93.3%) -----
Night 1 22 (73.3%) 22 (73.3%) -----
Night 3 24 (80%) 28 (93.3%) NS
Night 7 30 (100%) 30 (100%) -----
Salbutamol use Day 1 10 (33.3%) 13 (43.3%) NS
(symptom free) Day 3 22 (73.3%) 20 (66.7%) NS
Day 7 30 (100%) 28 (93.3%) NS
Night 1 8 (26.7%) 10 (33.3%) NS
Night 3 22 (73.3%) 25 (83.3%) NS
Night 7 30 (100%) 30 (100%) NC
Table 2: Symptoms improvement in the first 7 days after discharge
Oral prednisolone Inhaled fluticasone P value
FEV1 Before 88.06±18.81 84.55±38.45 NS
Day 7 104.36±12.62 115.20±17.19 0.007
*
FVC Before 86.16±17.57 97.16±17.60 0.01*
Day 7 104.00±12.94 114.93±19.51 0.01*
FEV1/FVC Before 99.83±9.14 101.76±6.31 NS
Day 7 109.66±14.22 109.53±8.64 NS
FEF Before 95.66±35.41 98.66±23.73 NS
Day 7 106.96±13.13 120.06±18.40 0.002
*
Australian International Academic Centre, Australia 8|Page
Original article Advances in Bioscience & Clinical Medicine
PEF Before 89.96±34.61 104.63±35.35 NS
Day 7 125.53±39.94 123.60±31.56 NS
PFM Before 136.00±34.79 134.33±44.61 NS
Day 7 174.66±51.97 165.66±47.53 NS
Table 3: Changes in pulmonary function tests during follow-up period
evaluation. There was also a trend toward
Discussion
lower symptoms at night in inhaled fluticasone
Children suffering from asthma symptoms group which was not significant. Similarly,
present frequently to pediatric emergency Schuh et al. (29) observed that children with
departments (3,4). It is well documented that mild to moderate asthma improve faster when
OCS use is effective in alleviating the symptoms given OCS compared to inhaled fluticasone.
of acute asthma exacerbations (11,12). It is also
To control the exacerbation, augmenting
shown that early initiation of oral corticosteroid
inhaled ICS doses (quadruple the dose of an ICS
is associated with reduced times to clinical
for 7 days) during asthma exacerbations (i.e.
improvement and discharge, and reduced
emergence of deteriorating symptoms) is
admission rates in children presenting with
recommended in addition to the initiation of
moderate to severe acute asthma
inhaled b2-agonists in those who use ICS
exacerbations (30). It is reported that ICS can
therapy (35-37); consequently the need for oral
be used as a replacement for OCS in treatment
corticosteroids could be eliminated (31).
of acute asthma exacerbation in ED with
Budesonide 200–400mg four times daily in
comparable results (27,28,31,32). Due to the
combination with a beta-agonist at the first
side effects of OCS, the use of inhaled
sign of asthma exacerbation have also been
corticosteroids has increased turning them into
used (36). Consequently, throughout a 1 year
the choice treatment of asthma (28,33). It has
follow-up, exacerbations were controlled in
been shown that inhaled corticosteroids
94% of cases. High doses of ICS have
improve lung function, asthma symptoms, and
occasionally been reported to be as efficient as
rescue inhaler use in patients with mild,
systemic corticosteroids in the treatment of
moderate, and severe persistent asthma. They
acute asthma exacerbations in children (25). In
also reduce the need for oral corticosteroids in
patients with mild to moderate asthma
patients with severe persistent asthma and
exacerbations, ICS administration with or
maintain asthma control (34).
without OCS recovers respiratory profile,
In this randomized clinical trial, we decreases aminophylline infusion or systemic
evaluated the efficacy of treatment with corticosteroid therapy requirement, precludes
inhaled fluticasone and OCS in mild to hospitalizations while leading to faster ED or
moderate asthma exacerbation in ED. We hospital discharge (25,38-40). ICS have been
observe that oral prednisolone could more reported to be associated with further and
effectively improve patients’ symptoms like more quickly improvement in asthma symptom
cough, sputum and need for salbutamol as scores than with OCS during the first week
rescue inhaler in the first three days post following discharge (41,42).
exacerbation; however, the symptom free
We also observed that spirometry
cases were comparable on the seventh day of
parameters especially FEV1, FVC and FEF
Australian International Academic Centre, Australia 9|Page
Original article Advances in Bioscience & Clinical Medicine
significantly improve after 1 week in children Conclusion
receiving inhaled fluticasone compared to oral In conclusion, both inhaled fluticasone and
prednisolone. Similar results are reported in oral prednisolone improved symptoms during a
the literature (28,40,43). It is reported that ICS week after exacerbation; however, the better
transiently increases spirometric and clinical respiratory function in children treated with
measures as early as 60 minutes (44). However, inhaled fluticasone is indicative of the more
some studies also could not demonstrate efficacy of the therapy compared to oral
beneficiary effects of ICS over OCS (24,41). prednisolone. Considering the low systemic
effects of inhaled fluticasone compared to oral
prednisolone, this treatment seems to be more
appropriate in mild to moderate exacerbations.
References
1. Martinez FD. Trends in asthma prevalence, admission rates, and asthma deaths. Respir Care. 2008;53:561-5.
2. Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980-2007.
Pediatrics. 2009;123 Suppl 3:S131-45.
3. American Academy of Pediatrics Committee on Pediatric Emergency Medicine. Overcrowding crisis in our nation’s
emergency departments: is our safety net unraveling? Pediatrics. 2004;114(3):878–888.
4 Stang AS, McGillivray D, Bhatt M, Colacone A, Soucy N, Léger R, et al. Markers of overcrowding in a pediatric
emergency department. Acad Emerg Med. 2010;17(2):151–156.
5. Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M, et al. Global strategy for asthma
management and prevention: GINA executive summary. Eur Respir J. 2008;31(1):143-78.
6. Kling S1, Zar HJ, Levin ME, Green RJ, Jeena PM, Risenga SM, et al. Guideline for the management of acute asthma in
children: 2013 update. S Afr Med J. 2013;103(3 Pt 3):199-207.
7. Mitchell EA. Consensus on acute asthma management in children: AdHoc Pediatric Group. N Z Med J. 1992; 105:
353-5.
8. National Asthma Education and Prevention Program. National Heart Lung and Blood Institute. Expert Panel Report
3: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: National Institutes of Health; 2007. Vol
08-5846.
9. Lougheed MD, Garvey N, Chapman KR, Cicutto L, Dales R, Day AG, et al. Variations and gaps in management of
acute asthma in Ontario emergency departments. Chest. 2009;135(3):724–736.
10. Rowe BH, Spooner CH, Ducharme FM, Bretzlaff JA, Bota GW. Early emergency department treatment of acute
asthma with systemic corticosteroids. Cochrane. Database. Syst Rev. 2001;(1):CD002178.
11. Rachelefsky G. Treating exacerbations of asthma in children: the role of systemic corticosteroids. Pediatrics.
2003;112:382-397.
12. Scarfone RJ, Friedlaender E. Corticosteroids in acute asthma: past, present, and future. Pediatr Emerg Care.
2003;19:355-361.
13. Butler K, Cooper WO. Adherence of pediatric asthma patients with oral corticosteroid prescriptions following
pediatric emergency department visit or hospitalization. Pediatr Emerg Care. 2004;20:730-735.
Australian International Academic Centre, Australia 10 |
Page
Original article Advances in Bioscience & Clinical Medicine
14. Gamble J, Stevenson M, McClean E, Heaney LG. The Prevalence of Non-adherence in Difficult Asthma. Am J Respir
Crit Care Med. 2009;180:817-22.
15. Beeraka SS, Natarajan K, Patil R, Manne RK, Prathi VS, Kolaparthi VS. Clinical and radiological assessment of effects
of long-term corticosteroid therapy on oral health. Dent Res J (Isfahan). 2013;10(5):666-73.
16. Tse SM, Kelly HW, Litonjua AA, Van Natta ML, Weiss ST, Tantisira KG; Childhood Asthma Management Program
Research Group. Corticosteroid use and bone mineral accretion in children with asthma: effect modification by
vitamin D. J Allergy Clin Immunol. 2012;130(1):53-60.e4.
17. Busse W, Bleecker ER, Bateman ED, Lötvall J, Forth R, Davis AM, et al. Fluticasone furoate demonstrates efficacy in
asthma patients symptomatic on medium doses of inhaled corticosteroid therapy: a randomised, placebo-controlled
trial. Thorax. 2012;67:35–41.
18. Castro-Rodriguez JA, Rodrigo GJ. The role of inhaled corticosteroids and montelukast in children with mild-
moderate asthma: results of a systematic review with meta-analysis. Arch Dis Child. 2010;95(5):365–370.
19. National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis
and Management of Asthma-Summary Report 2007. J Allergy Clin. Immunol. 2007;120(5 Suppl):S94–138.
20. Raissy HH, Blake K. As Needed Use of Inhaled Corticosteroids for Management of Mild Persistent Asthma in
Children. Pediatr Allergy Immuno Pulmonol. 2011;24(4):231-233.
21. Bleecker ER1, Bateman ED, Busse WW, Woodcock A, Frith L, House KW, et al. Once-daily fluticasone furoate is
efficacious in patients with symptomatic asthma on low-dose inhaled corticosteroids. Ann Allergy Asthma Immunol.
2012;109(5):353-358.e4.
22. Schuh S, Reisman J, Alshehri M, Dupuis A, Corey M, Arseneault R, et al. A comparison of inhaled fluticasone and
oral prednisone for children with severe acute asthma. N Engl J Med. 2000;343:689–694.
23. Nakanishi AK, Klasner AK, Rubin BK. A randomized controlled trial of inhaled flunisolide in the management of
acute asthma in children. Chest. 2003;124:790–794.
24. Manjra AI, Price J, Lenney W, Hughes S, Barnacle H. Efficacy of nebulized fluticasone propionate compared with
oral prednisolone in children with an acute exacerbation of asthma. Respir Med. 2000;94(12):1206-14.
25. Volovitz B. Inhaled budesonide in the management of acute worsenings and exacerbations of asthma: A review of
the evidence. Respir Med. 2007;101(4):685-95.
26. Razi CH, Turktas I, Bakirtas A. Comparison of single 2000-microg dose treatment vs. sequential repeated-dose 500-
microg treatments with nebulized budesonide in acute asthma exacerbations. Ann Allergy Asthma Immunol.
2008;100:370–376.
27. Ververeli K, Chipps B. Oral corticosteroid–sparing effects of inhaled corticosteroids in the treatment of persistent
and acute asthma. Ann. Allergy. Asthma Immunol. 2004;92:512–522.
28. Nuhoglu Y, Bahceciler NN, Barlan IB, Mujdat Basaran M. The effectiveness of high-dose inhaled budesonide
therapy in the treatment of acute asthma exacerbations in children. Ann Allergy Asthma Immunol. 2001;86:318–322.
29. Schuh S, Dick PT, Stephens D, Hartley M, Khaikin S, Rodrigues L, et al. High-dose inhaled fluticasone does not
replace oral prednisolone in children with mild to moderate acute asthma. Pediatrics. 2006;118(2):644-50.
30. Zemek R, Plint A, Osmond MH, Kovesi T, Correll R, Perri N, et al. Triage nurse initiation of corticosteroids in
pediatric asthma is associated with improved emergency department efficiency. Pediatrics. 2012;129(4):671-80.
31. Foresi A, Morelli MC, Catena E. Low-dose budesonide with the addition of an increased dose during exacerbations
is effective in long-term asthma control. On behalf of the Italian Study Group. Chest. 2000; 117:440–446.
32. Schramm CM, Carroll CL. Advances in treating acute asthma exacerbations in children. Curr Opin Pediatr.
2009;21(3):326-32.
Australian International Academic Centre, Australia 11 |
Page
Original article Advances in Bioscience & Clinical Medicine
33. Abdullah AK, Khan S. Evidence‑based selection of inhaled corticosteroid for treatment of chronic asthma. J
Asthma. 2007;44:1‑12.
34. Singas E, Karpel JP. Profile of ciclesonide for the maintenance treatment of asthma. Ther Clin Risk Manag.
2011;7:351-8.
35. FitzGerald JM, Becker A, Sears MR, Mink S, Chung K, Lee J, et al. Canadian Asthma Exacerbation Study Group.
Doubling the dose of budesonide versus maintenance treatment in asthma exacerbations. Thorax. 2004; 59:550–556.
36. Volovitz B, Nussinovitch M, Finkelstein Y, Harel L, Varsano I. Effectiveness of inhaled corticosteroids in controlling
acute asthma exacerbations in children at home. Clin Pediatr (Phila). 2001; 40:79–86.
37. Harrison TW, Oborne J, Newton S, Tattersfield AE. Doubling the dose of inhaled corticosteroid to prevent asthma
exacerbations: randomised controlled trial. Lancet. 2004; 363:271–275.
38. Sung L, Osmond MH, Klassen TP. Randomized, controlled trial of inhaled budesonide as an adjunct to oral
prednisone in acute asthma. Acad Emerg Med. 1998; 5:209–213.
39. Singhi SC, Banerjee S, Nanjundaswamy HM. Inhaled budesonide in acute asthma. J Paediatr Child Health. 1999;
35:483–487.
40. Devidayal, Singhi S, Kumar L, Jayshree M. Efficacy of nebulized Budesonide compared to oral prednisolone in acute
bronchial asthma. Acta Paediatr. 1999; 88:835–840.
41. Volovitz B, Bentur L, Finkelstein Y, Mansour Y, Shalitin S, Nussinovitch M, et al. Effectiveness and safety of inhaled
corticosteroids in controlling acute asthma attacks in children who were treated in the emergency department: a
controlled comparative study with oral prednisolone. J Allergy Clin Immunol. 1998;102:605–9.
42. Milani GKM, Nelson A, Filho R, Riedi CA, Figueiredo BC. Nebulised budesonide to treat acute asthma in children. J
Pediatr. 2004;80:106–12.
43. Rodrigo GJ. Comparison of inhaled fluticasone with intravenous hydrocortisone in the treatment of adult acute
asthma. Am J Respir Crit Care Med. 2005;171:1231–1236.
44. Rodrigo GJ. Rapid effects of inhaled corticosteroids in acute asthma: an evidence-based evaluation. Chest.
2006;130:1301–1311.
Australian International Academic Centre, Australia 12 |
Page
Reproduced with permission of the copyright owner. Further reproduction prohibited without
permission.
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Effect of Antenatal Dietary Interventions in Maternal Obesity On Pregnancy Weight Gain and Birthweight Healthy Mums and Babies (HUMBA) Randomized TrialDocument13 paginiEffect of Antenatal Dietary Interventions in Maternal Obesity On Pregnancy Weight Gain and Birthweight Healthy Mums and Babies (HUMBA) Randomized TrialAripin Ari AripinÎncă nu există evaluări
- O&M Manual For Vms PumpDocument11 paginiO&M Manual For Vms PumpKaushik ChakrabortyÎncă nu există evaluări
- Jurding 3 Azitromisin Vs Eritromisin Utk Manajemen KPDDocument8 paginiJurding 3 Azitromisin Vs Eritromisin Utk Manajemen KPDAripin Ari AripinÎncă nu există evaluări
- Good15 PIIS0002937817312127Document7 paginiGood15 PIIS0002937817312127wijeÎncă nu există evaluări
- Jurding 1 Komplikasi Obstetrik Dengan EndometriosisDocument13 paginiJurding 1 Komplikasi Obstetrik Dengan EndometriosisAripin Ari AripinÎncă nu există evaluări
- Antibiotic Treatment of AcuteDocument11 paginiAntibiotic Treatment of AcuteAripin Ari AripinÎncă nu există evaluări
- Aspirin For Evidence-Based Preeclampsia Prevention Trial: Effect of Aspirin On Length of Stay in The Neonatal Intensive Care UnitDocument6 paginiAspirin For Evidence-Based Preeclampsia Prevention Trial: Effect of Aspirin On Length of Stay in The Neonatal Intensive Care UnitAripin Ari AripinÎncă nu există evaluări
- Review Article: Acute Transverse Myelitis in ChildrenDocument10 paginiReview Article: Acute Transverse Myelitis in ChildrenAripin Ari AripinÎncă nu există evaluări
- Antibiotic Treatment of AcuteDocument11 paginiAntibiotic Treatment of AcuteAripin Ari AripinÎncă nu există evaluări
- Effect of Antiepileptic Drugs For Acute and Chronic Seizures in Children With EncephalitisDocument12 paginiEffect of Antiepileptic Drugs For Acute and Chronic Seizures in Children With EncephalitisAripin Ari AripinÎncă nu există evaluări
- Review Article: Acute Transverse Myelitis in ChildrenDocument10 paginiReview Article: Acute Transverse Myelitis in ChildrenAripin Ari AripinÎncă nu există evaluări
- Oral Diazepam in Febrile SeizuDocument6 paginiOral Diazepam in Febrile SeizuAripin Ari AripinÎncă nu există evaluări
- A Comparison of Oral and InhalDocument9 paginiA Comparison of Oral and InhalAripin Ari AripinÎncă nu există evaluări
- ZincDocument5 paginiZincAripin Ari AripinÎncă nu există evaluări
- The Effectiveness of Oxymetazoline Plus Intranasal Steroid in The Treatment of Chronic Rhinitis: A Randomised Controlled TrialDocument9 paginiThe Effectiveness of Oxymetazoline Plus Intranasal Steroid in The Treatment of Chronic Rhinitis: A Randomised Controlled TrialFaris LahmadiÎncă nu există evaluări
- Guidelines: Management of Bell Palsy: Clinical Practice GuidelineDocument6 paginiGuidelines: Management of Bell Palsy: Clinical Practice GuidelineyandaputriÎncă nu există evaluări
- Soc5352 1331Document4 paginiSoc5352 1331ChinÎncă nu există evaluări
- New Age GeneratorDocument26 paginiNew Age GeneratorDaud Ahmed Fihawango100% (1)
- AscindiaDocument16 paginiAscindiaHeeman TrivediÎncă nu există evaluări
- Conversion and Reactor Sizing-Chapter 2Document17 paginiConversion and Reactor Sizing-Chapter 2نزار الدهاميÎncă nu există evaluări
- 'Last Season's Man'Document7 pagini'Last Season's Man'Bishal Kumar SahuÎncă nu există evaluări
- Material Science & Metallurgy: Third Semester B.E. Degree (CBCS) Examination, Dec.2016/Jan.2017Document2 paginiMaterial Science & Metallurgy: Third Semester B.E. Degree (CBCS) Examination, Dec.2016/Jan.2017Shaikh MuzaffarÎncă nu există evaluări
- M 17Document5 paginiM 17amhm2000100% (1)
- Tinda Tomato PachadiDocument1 paginăTinda Tomato PachadijyosriÎncă nu există evaluări
- Lecture 16 - Bleeding Tendency DiseasesDocument64 paginiLecture 16 - Bleeding Tendency Diseasesapi-3703352100% (1)
- Mapeh 10 1 Grading Examination: E. Modern NationalismDocument3 paginiMapeh 10 1 Grading Examination: E. Modern NationalismMildred Abad SarmientoÎncă nu există evaluări
- Tutorial 2 Organizing DataDocument2 paginiTutorial 2 Organizing Datazurila zakariaÎncă nu există evaluări
- Pin ContentDocument20 paginiPin ContentSwetha100% (2)
- Daftar Pustaka ProposalDocument4 paginiDaftar Pustaka ProposalraniÎncă nu există evaluări
- Forensic Toxicology: A. Classify Toxins and Their Effects On The BodyDocument28 paginiForensic Toxicology: A. Classify Toxins and Their Effects On The BodySajid RehmanÎncă nu există evaluări
- By Josephine G. Ignacio, MD and Jennifer T. Co, MD, FPOGSDocument9 paginiBy Josephine G. Ignacio, MD and Jennifer T. Co, MD, FPOGSAngela SaldajenoÎncă nu există evaluări
- Introduction To LubricantsDocument12 paginiIntroduction To Lubricantsrk_gummaluri5334Încă nu există evaluări
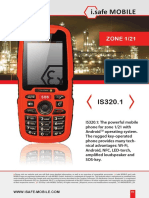
- Hoja Tecnica IS 320.1 Zona 1Document2 paginiHoja Tecnica IS 320.1 Zona 1susanivar adrianoÎncă nu există evaluări
- LOKRING Technical Documentation Submittal Brass enDocument32 paginiLOKRING Technical Documentation Submittal Brass enYamilelcÎncă nu există evaluări
- 4 26 12Document9 pagini4 26 12stevenscreekÎncă nu există evaluări
- Am Jf211 - Jul 04Document4 paginiAm Jf211 - Jul 04ilham_metallurgy6744Încă nu există evaluări
- Cleaning Disinfecting School ClassroomsDocument2 paginiCleaning Disinfecting School ClassroomsFitz JaminitÎncă nu există evaluări
- Calcium Cyanide: Hydrogen Cyanide. CONSULT THE NEW JERSEYDocument6 paginiCalcium Cyanide: Hydrogen Cyanide. CONSULT THE NEW JERSEYbacabacabacaÎncă nu există evaluări
- Antithesis Essay Joseph JaroszDocument3 paginiAntithesis Essay Joseph JaroszJoseph JaroszÎncă nu există evaluări
- The Solution To Absenteeism: in Grade 7 Student of Abuyog National High SchoolDocument4 paginiThe Solution To Absenteeism: in Grade 7 Student of Abuyog National High SchoolAilen Lagula CervantesÎncă nu există evaluări
- E28716V9 HRMT20024 Assessment2Document16 paginiE28716V9 HRMT20024 Assessment2bitetÎncă nu există evaluări
- CFM56 3Document148 paginiCFM56 3manmohan100% (1)
- Itopride HCL Pynetic 50mg TabDocument2 paginiItopride HCL Pynetic 50mg TabAusaf AhmadÎncă nu există evaluări
- C783 - Intake Manifold 1 Temperature-Abnormal Rate of ChangeDocument4 paginiC783 - Intake Manifold 1 Temperature-Abnormal Rate of ChangeLucas CamposÎncă nu există evaluări
- CSEB Korba THERMAL POWER PLANT Mechanical Training ReportDocument20 paginiCSEB Korba THERMAL POWER PLANT Mechanical Training Reporthaxxo24Încă nu există evaluări