Documente Academic
Documente Profesional
Documente Cultură
Bacteseminar DSSM
Încărcat de
Princess AguirreTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Bacteseminar DSSM
Încărcat de
Princess AguirreDrepturi de autor:
Formate disponibile
DIRECT SPUTUM SMEAR MICROSCOPY & ACID-FAST STAINING
Tuberculosis: 6th in the Philippines; 10th in the World
Morbidity: the person is infected with the disease
Mortality: the cause of death
Pulmonary tuberculosis Biosafety Level III
M. tuberculosis – acid-fast bacilli
Urine Specimen – sediments/extrapulmonary (Miliary TB – happens except in the lungs)
Skin (scrapings?); tissue juices – Mycobacterium leprae (ARB positive)
Symptoms: coughing, fever, chills, weight loss
Can progress to: chronic coughing, no appetite
AFB-positive Bacilli – protected by thick waxy coat (mycolic acid)
Can possess MDR (Multi-drug resistance) if left partially untreated
Laboratory Setup
Well ventilated, organized, clean, well-lighted room
Receiving Microscopy Recording Area
Equipment:
Microscope Staining equipment
Biosafety Cabinet Inoculating loop
Slides
Sputum Specimen: comes from lungs excrete by coughing
Ideal specimen:
Mucopurulent – greenish
Cheese-like
Yellowish
TB-DOTS Criteria: blood-streaked is accepted
Bloody sputum, and saliva is rejected
“Pus Cells” – alveolar macrophage (phagocytic cells)
Dust cells – indicative of a good quality smear
Gram staining: >25/LPF epithelial cells rejected
- Squamous cells > pus cells
- Indicative of a salivary components
- Pathogenic organisms are contaminants
>25 Pus cells/LPF = good quality (inversely proportional to epithelial cells)
Collection Time: early morning specimen
3 specimens with at least one Early morning
= spot-morning – spot method
DAY 1: RANDOM DAY 1: TB symptoms
DAY 2: EARLY MORNING 2 visit only DAY 2: Early specimen
DAY 3: RANDOM Random spx. are poor quality DAY 3: TB symptomatic returns
- will yield less rapidly
2 Good Examination are positive of AFB
Another set of specimen: within 1 week; when doubtful of the result
(same collection time.)
Follow-up: during & after treatment (ALWAYS EARLY MORNING)
Significance of a Follow-Up Specimen:
Coarse of the disease
Treatment modification
Treatment outcome
Guidelines on specimen collection
1. Explain clearly
2. What is the good specimen & how to obtain it (educate)
3. …
Patient Collection
Remove any dentures
Avoid mouthwash
o Gargle with water before collection to unwanted remove debris
Storage: cool & dark place
o To avoid liquefaction
o Avoid sunlight, rodents
Transport immediately in a special container
If the sample is need for culture: refrigeration is unadvisable
DSSM
1. Label the slides
2. Spreading
a. 1 loopful of purulent; solid particles
b. >25 pus cells/LPF (“blue dots”)
Test tube layer:
Top layer: saliva layer
o rods/cocci (may be normal flora) with little to none pus cells
Bottom layer: purulent pattern
o 5% saliva; 95% sputum
Dimension:
2x3 cm
o Recommended
1x2 – result to a compact field when viewed
ACID-FAST STAINING
Drying: Heat-fixing (do not boil)
ZN Method: Hot staining
Carbol fuchsin – flooding
Decolorizer – acid alcohol
*Not ideal for cervical, vaginal or urethral spx.
Counterstain – methylene blue
- Malachi green (kinyoun; cold method)
AFB APPLICATION
OIO – examination of cocci/bacilli
o Squamous cell/pus cell examine at LPO/HPO
Proper scanning Improper scanning
or or other variant
Adjacent Viewing Overlapping (1+ result 3+) Under-reading (F.N)
Error in Staining:
Under-staining
Intensive counterstaining
Under-decolorization
AFB-Positive: Pink-red color in a blue background (beaded appearance)
Chinese-character appearance: M. tuberculosis
Nocardia & Corynebacterium may contain mycolic acid
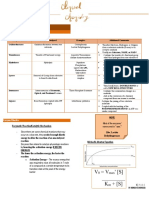
GRADING:
0 NONE
+n 1-9 AFB IN 100 HPF
n = +1 1 AFB
+2 2 AFB’s
... +9 9 AFB’s in 100 HPF
1+ 10-99 AFB/100 HPF
2+ 1-10 AFB/50 VISUAL FIELDS
3+ >10 AFB/20 VISUAL FIELDS
INTERPRETATION:
POSITIVE IF AT LEAST 2 OUT OF 3 SMEARS IS POSITIVE
NEGATIVE 0 OUT OF 3
DOUBTFUL 1 OUT OF 3
Positive slides – 1-2 years storage
False reading: too thick or too thick smear
Factored by the size, thickness, clearness and artifacts
False Positives: False Negatives:
Tap water Exposure of smear/slide to sunlight
Scratches – oil crystallization Insufficient reading
Spores of bacillus species Isoniazid (INH) Antibiotics
o Differentiated by size: Improper reading (under-reading)
Mycobacterium – thin Too intensive counterstaining
Spores of Bac. – Improper staining time
boxes
Transferring elements (“floaters”)
Fungi
Stain precipitates
I. CASE FINDING
Types:
Passive case-finding – voluntary
Active case-finding – consultation, mandatory
Tuberculosis: w/ or w/o x-ray result
Massive hemoptysis
Update: for px’s with confirmatory
Morning-Spot specimen first-morning & spot specimen
Spot-Spot specimen 1 hour apart
Morning specimen: presence/absence of disease
Spot specimen: intensity of disease
II. CASE HOLDING
Pulmonary
Extrapulmonary
Types (“for new px’s”) After treatment:
New Cured
Relapse – cured with positive Completed treatment
Transfer – from other facility Failed
Return after default Defaulted – interruption
Treatment failure Transferred – out
Died
Supervized Treatment – treatment partner (for small positive cases)
TREATMENT PATTERN
Streptomycin (N)
R Rifampicin
I (H)Isoniazid
P Pyrazinamide (Z)
E Ethambutol
CATEGORY I 2 HRZE / 4 HR
CATEGORY II 2 HRZES / 1 HRZE / 5 HRE (for repeat px.)
CATEGORY III 2 HRZ / 4 HR
Cat.I – new
Cat.II - previously treated/failed/defaulted
Cat.III – new smear less severe / extra.
MDR Tuberculosis – treatment with referral to DOTS; NTP coordinator
S-ar putea să vă placă și
- The Pyridine Nucleotide CoenzymesDe la EverandThe Pyridine Nucleotide CoenzymesJohannes EverseÎncă nu există evaluări
- 1 CCHM Trans LecDocument5 pagini1 CCHM Trans LecCRUZ, ANNA MARIELLEÎncă nu există evaluări
- Pharmaceutical Biochemistry: A Comprehensive approachDe la EverandPharmaceutical Biochemistry: A Comprehensive approachÎncă nu există evaluări
- BSC Licensure Sample QuestionsDocument144 paginiBSC Licensure Sample QuestionsSAMMY0% (1)
- History of PhlebotomyDocument46 paginiHistory of PhlebotomyDorothy AtilanoÎncă nu există evaluări
- CC Partii&III NotesDocument30 paginiCC Partii&III NotesAnielle Mongaya100% (1)
- cc2 Lectures AllDocument256 paginicc2 Lectures AllJayson Dagohoy SudioÎncă nu există evaluări
- Capillaria PhilippinenensisDocument4 paginiCapillaria PhilippinenensisnadalabelÎncă nu există evaluări
- HTMLE SEMINAR NOTES DOC. ORTEGA - CompressedDocument35 paginiHTMLE SEMINAR NOTES DOC. ORTEGA - CompressedNISSI JUNE T. UNGABÎncă nu există evaluări
- Aubf Case Study AbcdefDocument9 paginiAubf Case Study AbcdefChiara Kate CodillaÎncă nu există evaluări
- Aubf Module 3 Laboratory Assignment - Macabanding - PrincessDocument5 paginiAubf Module 3 Laboratory Assignment - Macabanding - PrincessNailah MacabandingÎncă nu există evaluări
- Microbiology 15 Campylobacter, Vibrio Etc 431-449Document18 paginiMicrobiology 15 Campylobacter, Vibrio Etc 431-449JenÎncă nu există evaluări
- BiochemLabAlviar2017 PDFDocument26 paginiBiochemLabAlviar2017 PDFChristina Scott100% (1)
- Defining The Practice of Medical Technology or Clinical Laboratory Science ProfessionDocument27 paginiDefining The Practice of Medical Technology or Clinical Laboratory Science ProfessionKianna TicsayÎncă nu există evaluări
- Micropara Final LabNotesDocument75 paginiMicropara Final LabNotescream oÎncă nu există evaluări
- MEDT02 Lesson 2 - Safety in PhlebotomyDocument5 paginiMEDT02 Lesson 2 - Safety in PhlebotomySHELDY AGONCILLOÎncă nu există evaluări
- Lesson 5: Nature of The Clinical LaboratoryDocument8 paginiLesson 5: Nature of The Clinical LaboratoryJohn Daniel AriasÎncă nu există evaluări
- (MT6317) Unit 6.1 Introduction To Carbohydrates and Glucose DeterminationDocument12 pagini(MT6317) Unit 6.1 Introduction To Carbohydrates and Glucose DeterminationJC DomingoÎncă nu există evaluări
- Clinical Chemistry 1 (MKEB2404)Document10 paginiClinical Chemistry 1 (MKEB2404)kiedd_04100% (3)
- Compiled Quizes AubfDocument39 paginiCompiled Quizes AubfCharmaine BoloÎncă nu există evaluări
- Cestodes: 1. Taenia Solium (Pork Tapeworm) & Taenia Saginata (Beef Tapeworm)Document18 paginiCestodes: 1. Taenia Solium (Pork Tapeworm) & Taenia Saginata (Beef Tapeworm)Genevee Ryeleen DelfinÎncă nu există evaluări
- Clinical Chemistry Assignment 2Document3 paginiClinical Chemistry Assignment 2Lana ZyoudÎncă nu există evaluări
- Routine UrinalysisDocument4 paginiRoutine UrinalysisDanica Joy Christelle L. PilarÎncă nu există evaluări
- Clinical Chemistry Lecture KayzardnDocument3 paginiClinical Chemistry Lecture KayzardnHenry QuimbaÎncă nu există evaluări
- Immunology Serology Review COMPLETEDocument30 paginiImmunology Serology Review COMPLETEEuliz G.100% (1)
- Must To Know Bacteriology Must To Know BacteriologyDocument35 paginiMust To Know Bacteriology Must To Know BacteriologyOlga BarredoÎncă nu există evaluări
- Principles in Medical Laboratory Science 2Document2 paginiPrinciples in Medical Laboratory Science 2lai cruzÎncă nu există evaluări
- IMH Laboratory ManualDocument56 paginiIMH Laboratory ManualHaniya KhanÎncă nu există evaluări
- Therapeutic Drug MonitoringDocument8 paginiTherapeutic Drug MonitoringLourdette TorrefielÎncă nu există evaluări
- Immunohema SlidesDocument508 paginiImmunohema SlidesBerihunÎncă nu există evaluări
- Medical TechnologistDocument2 paginiMedical Technologistapi-329932534Încă nu există evaluări
- Faults Occurring During TrimmingDocument4 paginiFaults Occurring During TrimmingMary Christelle100% (3)
- Module # 2 Medical Terminologies and Abbreviations and Ethics in The ProfessionDocument6 paginiModule # 2 Medical Terminologies and Abbreviations and Ethics in The ProfessionJonice NavarroÎncă nu există evaluări
- MacConkey AgarDocument12 paginiMacConkey Agardessy asandraÎncă nu există evaluări
- Blood ComponentDocument17 paginiBlood ComponentJes CmtÎncă nu există evaluări
- Aubf Lab Types of Urine SpecimenDocument18 paginiAubf Lab Types of Urine SpecimenNerizaÎncă nu există evaluări
- Exercise 14: Macroscopic and Chemical Examination of UrineDocument11 paginiExercise 14: Macroscopic and Chemical Examination of UrineAfif PusamaniaÎncă nu există evaluări
- Lecture Notes BacteriologyDocument133 paginiLecture Notes BacteriologyLovely B. AlipatÎncă nu există evaluări
- 2 - Anatomy Ang Histology Buzzwords Oct 2023 Jamaiyah H. Serad - Hadji OsopDocument7 pagini2 - Anatomy Ang Histology Buzzwords Oct 2023 Jamaiyah H. Serad - Hadji OsopmikzhiÎncă nu există evaluări
- Microbial Taxonomy and PhylogenyDocument7 paginiMicrobial Taxonomy and Phylogenyrina febrina100% (2)
- Medical Technologies History of Medtech in United StatesDocument1 paginăMedical Technologies History of Medtech in United StatesAthaliah Del MonteÎncă nu există evaluări
- Compre-Quiz For MedtechDocument18 paginiCompre-Quiz For MedtechynaellyÎncă nu există evaluări
- PMTP1 - Unit 1-3 HandoutDocument8 paginiPMTP1 - Unit 1-3 HandoutARVINE JUSTINE CORPUZ100% (1)
- RCS PreparationDocument3 paginiRCS PreparationMaria Charlene OrpillaÎncă nu există evaluări
- CPH Lab - Prelim TransesDocument4 paginiCPH Lab - Prelim TransesLOUISSE ANNE MONIQUE L. CAYLOÎncă nu există evaluări
- Bachelor of Science in Medical Technology 2014Document6 paginiBachelor of Science in Medical Technology 2014Maxine TaeyeonÎncă nu există evaluări
- Gram Positive CocciDocument34 paginiGram Positive CocciMaria Cecilia Flores50% (2)
- Urine and Blood PPT (Handout Print Form) Chua, RDocument10 paginiUrine and Blood PPT (Handout Print Form) Chua, RKirsten Hazel Mejia100% (1)
- Chapter 23 SummaryDocument4 paginiChapter 23 SummaryMartin ClydeÎncă nu există evaluări
- 1.entamoeba Histolytica - Is The Major Pathogen in This GroupDocument14 pagini1.entamoeba Histolytica - Is The Major Pathogen in This GroupJoseph De JoyaÎncă nu există evaluări
- Para Lab Merge FileDocument72 paginiPara Lab Merge Fileehehe agikÎncă nu există evaluări
- A. Two Forms of Carbohydrates: 1. Draw The FollowingDocument7 paginiA. Two Forms of Carbohydrates: 1. Draw The FollowingJoshua TrinidadÎncă nu există evaluări
- Vibrio (Comma-Shaped or Curved Bacillus)Document10 paginiVibrio (Comma-Shaped or Curved Bacillus)Ira ElizagaÎncă nu există evaluări
- BACTERIA CULTURE PRES Rev1Document28 paginiBACTERIA CULTURE PRES Rev1Jendie BayanÎncă nu există evaluări
- Difference Between Precipitation and AgglutinationDocument22 paginiDifference Between Precipitation and AgglutinationMuhammad Awais ZahoorÎncă nu există evaluări
- Hemoglobin DeterminationDocument1 paginăHemoglobin DeterminationLecture NotesÎncă nu există evaluări
- Reviewbasic 130709233435 Phpapp02Document130 paginiReviewbasic 130709233435 Phpapp02Andi Namirah100% (1)
- MEDT 19 (Lec)Document17 paginiMEDT 19 (Lec)Erick PanganibanÎncă nu există evaluări
- CombinepdfDocument214 paginiCombinepdfAl Ther JumadilÎncă nu există evaluări
- ABO Blood GroupDocument29 paginiABO Blood GroupUpendra Sharma SulibeleÎncă nu există evaluări
- RubellaDocument23 paginiRubellaNaing Lin SoeÎncă nu există evaluări
- Parasites USMLE PDFDocument7 paginiParasites USMLE PDFJane SmithÎncă nu există evaluări
- Prevention of Hepatitis A To E - 014825Document15 paginiPrevention of Hepatitis A To E - 014825saadkhalid8Încă nu există evaluări
- Epidermophyton (Skin, Nails) : Microsporum, TrichophytonDocument5 paginiEpidermophyton (Skin, Nails) : Microsporum, TrichophytonRoyÎncă nu există evaluări
- Pneumonia VaccinesDocument4 paginiPneumonia Vaccinesapi-237094717Încă nu există evaluări
- Saudi Pharmaceutical JournalDocument13 paginiSaudi Pharmaceutical JournalSHAMSUL HAQÎncă nu există evaluări
- FDA Recommended Pasteurization TimeDocument2 paginiFDA Recommended Pasteurization TimeMarquel Audreyan0% (1)
- Immunology Study Sheet For The Final ExamDocument3 paginiImmunology Study Sheet For The Final ExamDenizDerenÎncă nu există evaluări
- Differences of Hap-Vap Guidelines in The Idsa 2005 and 2016Document13 paginiDifferences of Hap-Vap Guidelines in The Idsa 2005 and 2016Adeh MahardikaÎncă nu există evaluări
- Epidemiology ConceptDocument22 paginiEpidemiology ConceptRezha Hardian RÎncă nu există evaluări
- Bacteriological Aspects of Hand Washing: A Key For Health Promotion and Infections ControlDocument10 paginiBacteriological Aspects of Hand Washing: A Key For Health Promotion and Infections ControlReza RahmadaniÎncă nu există evaluări
- New VPD Orientation SlidesDocument31 paginiNew VPD Orientation Slidesapi-209888269Încă nu există evaluări
- Buting Senior High School Buting, Pasig City Tel. No. (02) 721-58-46/925-55-25Document4 paginiButing Senior High School Buting, Pasig City Tel. No. (02) 721-58-46/925-55-25Alyssa Hazza Membrano MayonadoÎncă nu există evaluări
- Peptidoglycan: (Also Called Gram's Method)Document20 paginiPeptidoglycan: (Also Called Gram's Method)GeoffreyÎncă nu există evaluări
- Bioterrorism: BY: - Bijay Kumar Mahato BPH 2 Semester Padmashree School of Public HealthDocument26 paginiBioterrorism: BY: - Bijay Kumar Mahato BPH 2 Semester Padmashree School of Public HealthBijay Kumar MahatoÎncă nu există evaluări
- 3292 FullDocument2 pagini3292 FullRizqika RahmaniaÎncă nu există evaluări
- Expanded Program Immunization: NCM 104: Community Health Nursing I: Individual and FamilyDocument25 paginiExpanded Program Immunization: NCM 104: Community Health Nursing I: Individual and FamilyRica machells DaydaÎncă nu există evaluări
- Jenny LeafletDocument2 paginiJenny Leafletجني رمضانÎncă nu există evaluări
- Medically Important Bacteria Memorisation SheetDocument7 paginiMedically Important Bacteria Memorisation SheetOlivia LimÎncă nu există evaluări
- PoliomyelitisDocument50 paginiPoliomyelitisJohn John TorresÎncă nu există evaluări
- Industrial Brilliance Chromogenic Media - FinalDocument1 paginăIndustrial Brilliance Chromogenic Media - FinalFrengki Hadi Eko SantosoÎncă nu există evaluări
- Serial Dilution ProblemsDocument9 paginiSerial Dilution ProblemsEarl Jeroh Infante BacabacÎncă nu există evaluări
- Pidato Bahasa Inggris Tentang Covid 19Document2 paginiPidato Bahasa Inggris Tentang Covid 19Nabilla PutriÎncă nu există evaluări
- PasteurDocument12 paginiPasteurPARVATHI VÎncă nu există evaluări
- Recombinant VaccinesDocument22 paginiRecombinant VaccinesjugesmangangÎncă nu există evaluări
- Proteus Mirabilis Infections - StatPearls - NCBI BookshelfDocument5 paginiProteus Mirabilis Infections - StatPearls - NCBI BookshelfclaudyÎncă nu există evaluări
- Skripsi Full Tanpa Bab PembahasanDocument68 paginiSkripsi Full Tanpa Bab PembahasanBudi YarjoÎncă nu există evaluări
- Pseudotuberculosis 191204160344Document13 paginiPseudotuberculosis 191204160344padmaÎncă nu există evaluări
- Candida Albicans ATCC 14053Document2 paginiCandida Albicans ATCC 14053Bety MartinescuÎncă nu există evaluări
- Worksheet - 8th - Lesson 2Document2 paginiWorksheet - 8th - Lesson 2Shailaja MestryÎncă nu există evaluări
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)De la EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Evaluare: 3 din 5 stele3/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDe la EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDEvaluare: 5 din 5 stele5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (29)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDe la EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionEvaluare: 4 din 5 stele4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe la EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsÎncă nu există evaluări
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedEvaluare: 5 din 5 stele5/5 (81)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeEvaluare: 2 din 5 stele2/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDe la EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessEvaluare: 4.5 din 5 stele4.5/5 (328)
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 4 din 5 stele4/5 (6)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe la EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe la EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisEvaluare: 4.5 din 5 stele4.5/5 (42)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe la EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsEvaluare: 4 din 5 stele4/5 (4)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDe la EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsEvaluare: 5 din 5 stele5/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDe la EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeEvaluare: 4.5 din 5 stele4.5/5 (253)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.De la EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Evaluare: 4.5 din 5 stele4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe la EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityEvaluare: 4 din 5 stele4/5 (5)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDe la EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisEvaluare: 4 din 5 stele4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDe la EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryEvaluare: 4 din 5 stele4/5 (45)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDe la EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsEvaluare: 4.5 din 5 stele4.5/5 (170)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedEvaluare: 4 din 5 stele4/5 (61)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesDe la EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesEvaluare: 4.5 din 5 stele4.5/5 (1412)
- How to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingDe la EverandHow to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingEvaluare: 1 din 5 stele1/5 (1)
- The Marshmallow Test: Mastering Self-ControlDe la EverandThe Marshmallow Test: Mastering Self-ControlEvaluare: 4.5 din 5 stele4.5/5 (59)