Documente Academic
Documente Profesional
Documente Cultură
Pini Prato Et Al
Încărcat de
Fernando CursachDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Pini Prato Et Al
Încărcat de
Fernando CursachDrepturi de autor:
Formate disponibile
CLINICAL GUIDELINES 9
Giovanpaolo Pini-Prato, Michele Nieri, Umberto Pagliaro, Teresa Schifter Giorgi,
Michele La Marca, Debora Franceschi, Jacopo Buti, Monica Giani, Julia Hanne Weiss,
Luigi Padeletti, Pierpaolo Cortellini, Leandro Chambrone, Luca Barzagli, Efisio Defraia,
Roberto Rotundo
Surgical treatment of single gingival recessions:
Clinical guidelines
Giovanpaolo
Pini-Prato, Professor
Department of Surgery and
Translational Medicine, Uni-
Key words aesthetics, gingival recession, guidelines, mucogingival surgery, systematic review versity of Florence, Italy
Michele Nieri, DMD
Purpose: The purpose of this clinical guidelines project was to determine the most appropriate surgi- Department of Surgery and
Translational Medicine, Uni-
cal techniques, in terms of efficacy, complications, and patient opinions, for the treatment of buccal versity of Florence, Italy
single gingival recessions without loss of interproximal soft and hard tissues. Umberto Pagliaro,
Methods: Literature searches were performed (electronically and manually) for entries up to 28 Feb- Med Dent
Private Practice, Florence,
ruary, 2013 concerning the surgical approaches for the treatment of gingival recessions. Systematic Italy
reviews (SRs) of randomised controlled trials (RCTs) and individual RCTs that reported at least 6
Teresa Schifter Giorgi,
months of follow-up of surgical treatment of single gingival recessions were included. The full texts DMD
of the selected SRs and RCTs were analysed using checklists for qualitative evaluation according to Private Practice, Florence,
Italy
the Scottish Intercollegiate Guidelines Network (SIGN) method. The following variables were evalu-
ated: Complete Root Coverage (CRC); Recession Reduction (RecRed); complications; functional and Michele La Marca,
DMD
aesthetic satisfaction of the patients; and costs of therapies. Private Practice, Florence,
Italy
Results: Out of 30 systematic reviews, 3 SRs and 16 out of 313 RCTs were judged to have a low
risk for bias (SIGN code: 1+). At a short-term evaluation, the coronally advanced flap plus connec- Debora Franceschi,
DMD
tive tissue graft method (CAF+CTG) resulted in the best treatment in terms of CRC and/or RecRed; Department of Surgery and
in case of cervical abrasion and presence of root sensitivity CAF + CTG + Restoration caused less Translational Medicine, Uni-
versity of Florence, Italy
sensitivity than CAF+CTG. CAF produced less postoperative discomfort for patients. Limited in-
formation is available regarding postoperative dental hypersensitivity and aesthetic satisfaction of Jacopo Buti, DMD,
PhD
the patients. School of Dentistry, The
Conclusion: In presence of aesthetic demands or tooth hypersensitivity, the best way to surgically University of Manchester,
UK
treat single gingival recessions without loss of interproximal tissues is achieved using the CAF pro-
cedure associated with CTG. Considering postoperative discomfort, the CAF procedure is the less Monica Giani, Dent
Hygienist
painful surgical approach, while the level of aesthetic satisfaction resulted higher after CAF either Dental Hygienist repre-
sentative, Private Practice,
alone or with CTG. It is unclear how much tooth hypersensitivity is reduced by surgically covering Florence, Italy
buccal recessions. It is important to note that the present recommendations are based on short-term
Julia Hanne Weiss,
data (less than 1 year). Patient Representa-
Source of funding: The guidelines project was made possible through self-financing by the authors. tive
Patient representative,
Florence, Italy
Conflict of interest: The authors certify that there are no conflicts of interest related to this review.
Luigi Padeletti,
Professor
Department of Experimen-
tal and Clinical Medicine,
University of Florence,
Italy (General Practitioner
Representative)
Eur J Oral Implantol 2014;7(1):9–43
10 Pini-Prato et al Guidelines for single gingival recessions
Pierpaolo Cortellini,
Med Dent
Introduction In periodontology, one of the therapies requested
European Research Group on by patients is the treatment of gingival recessions
Periodontology (ERGOPER- In 2011, the US Institute of Medicine of the National that may be associated with dental hypersensitiv-
IO), Berne, Switzerland
Academies (IOM)1 stated “Clinical practice guide- ity and personal aesthetic concerns. Case reports,
Leandro Chambrone, lines are statements that include recommendations case series, controlled clinical trials, randomised con-
Professor
Department of Periodontol- intended to optimize patient care that are informed trolled trials (RCTs) and SRs have been published on
ogy, Dental Research Divi-
sion, Guarulhos University,
by systematic reviews of evidence and an assessment this topic and different techniques were proposed to
Guarulhos, SP, Brazil of the benefits and harms of alternative care options”. treat these lesions. Data on outcomes of surgical pro-
Luca Barzagli, According to the Evidence-Based Medicine phi- cedures are widely available in the literature for the
Med Dent losophy, guidelines must be performed on the basis clinicians. Even in the more recent and well-designed
National Association of Ital-
ian Dentists (ANDI) – Tuscan of the most reliable scientific evidence (systematic articles (RCTs and SRs) that reported detailed and
Section reviews [SRs]). In fact, SRs have been defined as statistically sound results, little information is avail-
Efisio Defraia, “Literature reviews that summarize evidence by able on patient-based outcomes (i.e. patient’s satis-
Professor identifying, selecting, assessing and synthesizing the faction, complications, side effects and economical
Department of Surgery and
Translational Medicine, Uni- findings of similar but separate studies. They can costs). These factors, often underestimated in these
versity of Florence, Italy
help to clarify what is known and not known about papers, could be able to influence and to facilitate
Roberto Rotundo, the potential benefits and harms of drugs, devices the choice of treatment, if properly evaluated by
DMD
Department of Surgery and
and other health care services”2. clinicians together with patients. In fact, the patient
Translational Medicine, Uni- The clinical practice guidelines must meet sev- (‘the person’) is placed at the centre of the medical
versity of Florence, Italy and
Periodontal Unit, Eastman eral new revised criteria for their inclusion in the US process. The physicians must take his/her percep-
Dental Institute, University National Guidelines Clearinghouse (Effective June tion, information and sensations, along with a clear
College of London, UK
2014)3. Among these criteria, three are of para- decisive consensus to treatment into great consid-
Correspondence to: mount importance: eration.
Roberto Rotundo,
via Vasco de’ Gama, 1. “The clinical practice guideline contains system- Gingival recession is defined as “the location of
33/3 - 50127, Firenze, Italy
Email: roberto.rotundo@
atically developed statements including recom- the gingival margin apical to the cementoenamel
gmail.com mendations intended to optimise patient care junction (CEJ)”4 and may involve one or more tooth
and assist physicians and/or other health care surfaces. Recessions are frequent clinical features
practitioners and patients to make decisions in populations with both good5,6 and poor stand-
about appropriate health care for specific clinical ards5,7,8 of oral hygiene, as reported in some large-
circumstances”; scale epidemiological studies. For instance, Kassab
2. “The clinical practice guideline was produced and Cohen9 reported that 88% of 65-year old
under the auspices of a medical specialty as- patients show recessions, while 50% of the 18- to
sociation; relevant professional society; public 64-year-old patient group had recessions. Other
or private organisation; government agency at studies reported similar trends of recession distribu-
the Federal, State, or local level; or health care tion in different populations10-13.
organisation or plan. A clinical practice guide- Furthermore, it has been shown that several con-
line developed and issued by an individual(s) not ditions may be associated with the presence of buc-
officially sponsored or supported by one of the cal recessions:
above types of organisations does not meet the • Anatomical factors. Gingival recessions may be
inclusion criteria for NGC”; associated with sites showing a developmental
3. “The clinical practice guideline is based on sys- absence of bone, known as bone dehiscence.
tematic review of evidence”. This condition often occurs when the teeth are
positioned beyond the thickness of the alveolar
Practically, clinical guidelines have been developed bone, in a buccolingual direction, with disconti-
in medicine to transfer the results of scientific rec- nuity of the cortical plate14-16. Other anatomical
ognised research in clinical practice and provide use- conditions may be associated with gingival reces-
ful information for institutions, universities, insurers, sions, such as frenulum attachment positioned
clinical practitioners, and mostly for patients. close to the gingival margin17,18.
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 11
• Traumatic toothbrushing. The type of technique, the diagnosis of gingival recessions34-38. An initial
frequency, strength and duration of tooth brush- classification of gingival recessions proposed by Sul-
ing are often associated with gingival reces- livan and Atkins in 196834, classified recessions as
sions9,16. Many studies have shown that high wide or narrow lesions with the involvement of the
standards of oral hygiene increase the prob- gingiva and/or the alveolar mucosa. Later, on the
ability of developing gingival recessions19,20. For basis of clinical and prognostic criteria and to facili-
instance, a previous RCT compared manual and tate treatment decisions for clinicians, Miller37 pro-
electric toothbrushing showing no differences posed a classification of recessions into four classes,
between the two approaches in terms of pro- depending on the degree of destruction of the soft
gression of recessions21. Nevertheless, a recent and hard periodontal tissues.
SR concluded that data supporting or refuting Recently, Cairo et al39 published a new classi-
the association between traumatic toothbrush- fication of recessions considering the interdental
ing and gingival recession are still inconclusive22. attachment level as the reference measurement and
• Occlusion. Some authors23 found associations identified three classes of recessions. Considering
between gingival clefts and occlusal traumatism, the exposed root surface following the apical shift
reporting that occlusal adjustment seemed to of the gingival margin, Pini Prato et al40 proposed
improve these lesions. However, other authors a classification based on two factors: presence or
reported that there does not appear to be any absence of an identifiable CEJ and the presence or
relationship between occlusal discrepancies and absence of dental surface discrepancy (abrasion),
gingival recessions24. thus four classes are identified on the basis of these
• Tobacco use. An observational study on Swed- factors. Following this information, Rotundo et al41
ish adolescent patients25 compared a group of presented a classification taking into consideration
non-user with a group of patients using smoke- all of these factors, and in particular, the amount of
less tobacco (moist snuff). In that population, keratinised tissue around the gingival recession, the
the use of moist snuff was not associated with presence/absence of non-carious cervical lesions,
the presence of periodontal disease, but a sig- and the presence/absence of interproximal attach-
nificantly high prevalence of gingival recessions ment loss.
was observed. The treatment of gingival recession is mainly
• Orthodontic treatment. Cases of gingival reces- indicated to improve aesthetics and to reduce or
sions were observed during/after orthodontic eliminate dental hypersensitivity due to root expo-
tooth movement, mostly in the mandibular inci- sure. Different surgical and non-surgical techniques
sors9,16. In fact, if the orthodontic labial move- have been described for the treatment of single and
ment of the tooth can result in the establishment multiple recessions. Because of the patients’ ever-
of an alveolar bone dehiscence, there is a high increasing aesthetic demands, new and sophisticated
risk of developing a gingival recession26. surgical techniques have been developed to obtain
• Piercing. Another factor associated with gin- complete root coverage associated with perfect inte-
gival recessions is the presence of piercing in gration of grafted tissue with the adjacent soft tis-
young populations. Some case reports have been sues. The choice of treatment depends on the assess-
recently published showing presence of marginal ment of the factors linked to the characteristics of
gingival recessions in sites traumatised by labial the single patient, of the tooth, and of the site. In
and lingual piercings27-31. fact, the size of the recession, both horizontally and
• Chemical agents. Local cocaine application has vertically, the amount of residual keratinised gingiva
been implicated as cause of gingival erosions and apical and adjacent to the lesion, the presence of
ulcerations, and associated with rapid progres- pulling frenum, as well as the presence or absence
sion of gingival recession32,33. of dental abrasion at the cementoenamel junction,
influence the choice of the most appropriate tech-
Considering the classification systems, several meth- nique. Other factors, such as the patient’s personal
ods have been proposed in the literature to facilitate aesthetic expectations, subjective dental hypersen-
Eur J Oral Implantol 2014;7(1):9–43
12 Pini-Prato et al Guidelines for single gingival recessions
sitivity, smoking habit and the need to reduce the or reduced amount of keratinised tissue represents a
number of interventions may further influence the critical situation for clinicians. Few data are available.
choice of the treatment. Pini Prato et al49 observed that recession reduction is
Nowadays, on the basis of the published litera- associated with the amount of baseline keratinised
ture, two approaches can be identified as the most tissue: every millimetre of additional KT at baseline
effective: the coronally advanced flap and the com- is associated with an increment of 0.23 mm of reces-
bined procedures based on a coronally advanced flap sion reduction after CAF procedure at the 8-year
with connective tissue; or allogenic materials inter- follow-up visit. However, an important question is
posed between the flap and the root surface42,43. still open: what is the appropriate amount of kerati-
Recently, Buti et al44 used a Bayesian Network nised tissue for choosing CAF or CAF+CTG?
meta-analysis model to summarise evidence from Often, gingival recessions are associated with
the published information on comparisons among non-carious cervical lesions such as abrasions, ero-
different root coverage procedures based on coro- sions, and abfractions50. In these cases, even if the
nally advanced flap or combined techniques with width and depth of the recessions are minimal, the
the aim of drawing inferences even on comparisons final outcomes in terms of complete root coverage
which have not been conducted yet. The coronally are not predictable. Combined restorative-periodon-
advanced flap with connective tissue proved the tal approaches have been also suggested51-53.
most effective procedure (first in the ranking of Although a large number of well-done RCTs on
treatments) among all the compared root coverage mucogingival root coverage procedures have been
techniques. This outcome confirmed the results of a published giving detailed information on the selected
meta-analysis on individual patient data conducted population, sample size calculation, entry criteria,
by Chambrone et al45. type of recessions, periodontal measurements, and
The even more sophisticated surgical techniques several statistical analyses, only one recent study
used for treating single recessions allow for a high provides information about the patient’s percep-
percentage of recession reduction ranging from 52 tion and the personal and spontaneous request for
to 99%, with a percentage of complete root cover- undergoing surgical or non-surgical treatment54.
age from 9 to 95%46. In cases of multiple recessions, In this study, out of 120 enrolled patients, 96 pre-
the mean recession reduction ranges from 94 to sented 783 gingival recessions, of which 565 were
98%, with a mean complete root coverage ranging unperceived. Of 218 perceived recessions, 160
from 68 to 90%47. This high variability of the results were asymptomatic, 36 showed dental hypersen-
is found not only when comparing different tech- sitivity, 13 aesthetic problems, and 9 aesthetic plus
niques, but also within the same surgical technique. hypersensitivity issues. Only 11 patients requested
This means that the treatment of root coverage is treatment for their 57 recessions. Age (i.e. younger
affected by the operator’s skills and that other fac- individuals), deeper recessions, incisors and canines
tors have not been adequately considered. Potential and non-carious cervical lesions were significantly
prognostic factors are divided into three different associated with patient perception of recessions.
categories48: patient-related factors (gender, age, Younger subjects, deeper recessions and incisors
smoking) tooth/site-related factors (tooth-vitality, were significantly associated with patient requests
tooth position, vestibulum depth, cervical caries, for treatment.
tooth malpositioning) and technique-related factors Moreover, there is little information on postop-
(microsurgery, materials, operator skill). Neverthe- erative discomfort and on a possible impairment of
less, there is a lack of scientific evidence on many personal daily life55,56. Complications of the surgical
prognostic factors and data on these issues are often treatment are rarely reported in the articles; one
not available in periodontal literature. case report shows a severe root resorption after a
Among the tooth/site related factors, the residual successful bilaminar procedure on a maxillary pre-
amount of keratinised tissue apical to the recessions molar57. In addition, very few studies have consid-
is of paramount importance for establishing the ered patient satisfaction as the true outcome of the
most appropriate treatment approach. The absence procedure mainly addressing the goal of aesthetic
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 13
improvement. On this issue, a study by Rotundo et 2. Which is the most effective surgical technique
al58 investigated the perceived aesthetic outcomes for recessions associated with non-carious cervi-
on simulated root coverage procedures in three dif- cal lesions?
ferent groups of evaluators: patients, dentists and
periodontists. The three groups considered complete Complications
root coverage the most desirable outcome. 3. Which surgical technique for the treatment of
With regard to changes in dental hypersensitiv- single gingival recessions has the least adverse
ity, this variable is seldom reported in the studies. An reactions (discomfort, postoperative pain, hae-
RCT55 reported that coronally advanced flap alone matoma, etc.)?
or associated with a connective tissue graft are effec-
tive in reducing dental hypersensitivity. Patient opinions
The financial cost of the procedure in terms of 4. Which is the most effective surgical technique
materials, chair-time, and post-surgical controls is for the treatment of single gingival recessions,
often underestimated as well. The cost of the ther- in terms of:
apy could influence the patient’s choice for a cheaper –(a) absence of dental hypersensitivity
approach, thereby affecting the outcomes of the –(b) aesthetic satisfaction.
procedures48.
Therefore, the aim of these clinical guidelines Available data on the following techniques were
requested by the National Association of Italian evaluated:
Dentists (ANDI) – Tuscany Region was to determine • Coronally Advanced Flap (CAF)
which surgical techniques are most appropriate for • CAF plus Connective Tissue Graft (CAF+CTG)
the treatment of patients showing single buccal gin- • CAF plus resorbable and non-resorbable Barrier
gival recessions without loss of interproximal soft Membrane (CAF+BM)
and hard tissues. • CAF plus Enamel Matrix Derivative (CAF+EMD)
Multiple gingival recessions have not been con- • CAF plus Acellular Dermal Matrix (CAF+ADM)
sidered in these guidelines due to the reduced num- • CAF plus Platelet-Rich Plasma (CAF+PRP)
ber of available studies and to their low level of evi- • CAF plus Human Fibroblast-Derived Dermal Sub-
dence. Nevertheless, this clinical condition will be stitute (CAF+HF-DDS)
taken into consideration for specific guidelines in the • CAF plus Xenogenic Collagen Matrix (CAF+CM)
future. In addition, for statistical reasons, the RCTs • Semilunar Technique (ST)
that dealt with multiple recessions in a single patient • Free Gingival Graft (FGG)
were excluded if they did not take into account the • Laterally Positioned Flap (LPF)
existence of non-independent sites (patient effect). • Envelope Technique plus CTG (ET+CTG)
These clinical guidelines were complied with the • CAF plus Anorganic Bovine Derived Hydroxyapa-
tools and instructions of the Appraisal of Guidelines tite Matrix Cell Bridging Peptide (ADMP15)
for Research and Evaluation (AGREE) Collabora- • CAF plus CTG plus Resin Composite Restoration
tion59. The guidelines were drawn up by multidis- (CAF+CTG+R)
ciplinary development groups and based on a sys- • CAF plus Resin Composite Restoration (CAF+R).
tematic review of the evidence for best practice,
following a standard methodology designed to bal-
ance scientific rigour with an open and consultative Materials and methods
approach.
The key clinical issues included: Criteria used for drafting the guidelines
Efficacy
1. Which is the most effective surgical technique These guidelines requested by the National Asso-
for the treatment of single gingival recessions in ciation of Italian Dentists (ANDI) – Tuscany Region
terms of complete root coverage and recession were organised using PICO60, a worksheet assess-
reduction? ment that uses four categories for breaking down
Eur J Oral Implantol 2014;7(1):9–43
14 Pini-Prato et al Guidelines for single gingival recessions
and converting the issues to investigate and the provide their personal opinions and to comment on
information sought into specific, precise questions. draft documents. Although the areas of expertise
According to PICO, a well-structured research strat- may vary, members of the guidelines development
egy calls for at least four questions that define the group shared equal status in the group. Patients,
characteristics of the patient (patient or population dental hygienists, and general practitioners were
[P]), the treatments to investigate (intervention [I]), invited to take part in the peer review stage of each
the comparisons among the identified treatments guideline and specific guidance for lay reviewers has
(comparison [C]), and the outcome variables con- been produced.
sidered important for the evaluation of the results
(outcomes [O])60.
Type of studies and participants –
inclusion and exclusion criteria
Development of the guidelines
Only RCTs-based SRs (i.e. SRs of RCTs) and indi-
According to the Scottish Intercollegiate Guidelines vidual RCTs were selected for these guidelines. RCTs
Network (SIGN) the present clinical practice guide- had to report the treatment of adult patients (at least
lines have been developed by dentists/physicians 18 years old) presenting single recessions without
(GPP, MN, UP, RR) in collaboration with representa- interproximal soft and hard tissue loss associated or
tives of those who will be affected by the specific not with non-carious cervical lesions, and a follow-
intervention(s) in question, including general practi- up ≥ 6 months after the surgical procedure. For sta-
tioners, dental hygienists, and patients. tistical analyses, the RCTs that dealt with multiple
These guidelines have been based on all the SRs recessions in a single patient were excluded if they
of RCTs and individual RCTs published up to 28 Feb- did not take into account the existence of non-inde-
ruary, 2013. At the same time, internal (MN, UP) and pendent sites (patient effect).
external (LC, PC) reviewers were selected to validate
the outcomes of this study. When the first draft of
Surgical techniques of interest
the manuscript was completed, the panel of authors
evaluated and discussed the text to reach an agree- The results published in the literature concerning
ment on the guidelines. Subsequently, the guidelines the following surgical techniques were searched and
were sent to the external reviewers (LC, PC) for the compared: CAF; CAF+CTG; CAF+BM; CAF+EMD;
definitive agreement. CAF+ADM; CAF+PRP; CAF+HF-DDS; CAF+CM; ST;
FGG; LPF; ET+CTG; CAF+ADMP15; CAF+CTG+R;
CAF+R. Data concerning the techniques were
Patient, dental hygienist, and general
sought for the following 105 comparisons: CAF vs.
practitioner involvement in guidelines
CAF+CTG; CAF vs. CAF+BM; CAF vs. CAF+EMD;
development
CAF vs. CAF+ADM; CAF vs. CAF+PRP; CAF vs.
Following the SIGN recommendations, “the purpose CAF+HF-DDS; CAF vs. CAF+CM; CAF vs. ST; CAF
of patient involvement is to ensure that the guideline vs. FGG; CAF vs. LPF; CAF vs. ET+CTG; CAF vs.
addresses issues that matter to them and that their CAF+ADMP15; CAF vs. CAF+CTG+R; CAF vs.
perspectives are reflected in the guideline. Patients CAF+R; CAF+CTG vs. CAF+BM; CAF+CTG vs.
can identify issues that may be overlooked by health CAF+EMD; CAF+CTG vs. CAF+ADM; CAF+CTG vs.
professionals, can highlight areas where the patient’s CAF+PRP; CAF+CTG vs. CAF+HF-DDS; CAF+CTG
perspective differs from the views of health profes- vs. CAF+CM; CAF+CTG vs. ST, CAF+CTG vs. FGG;
sionals, and can ensure that the guideline addresses CAF+CTG vs. LPF; CAF+CTG vs. ET+CTG; CAF+CTG
key issues of concern to patients. A key role for patient vs. CAF+ADMP15; CAF+CTG vs. CAF+CTG+R;
and career representatives is to ensure that patient CAF+CTG vs. CAF+R; CAF+BM vs. CAF+EMD;
views and experiences inform the group’s work”. CAF+BM vs. CAF+ADM; CAF+BM vs. CAF+PRP;
Dental hygienists and general practitioners were CAF+BM vs. CAF+HF-DDS; CAF+BM vs. CAF+CM;
also involved in guideline development in order to CAF+BM vs. ST; CAF+BM vs. FGG; CAF+BM vs. LPF;
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 15
CAF+BM vs. ET+CTG; CAF+BM vs. CAF+ADMP15; Procedure-based outcomes (for
CAF+BM vs. CAF+CTG+R; CAF+BM vs. CAF+R; professional reference use)
CAF+EMD vs. CAF+ADM; CAF+EMD vs.
CAF+PRP; CAF+EMD vs. CAF+HF-DDS; CAF+EMD The following variables were taken into considera-
vs. CAF+CM; CAF+EMD vs. ST; CAF+EMD vs. tion: percentage of Complete Root Coverage (CRC),
FGG; CAF+EMD vs. LPF; CAF+EMD vs. ET+CTG; Recession Reduction (RecRed) in millimetres, com-
CAF+EMD vs. CAF+ADMP15; CAF+EMD vs. plications (swelling, haematoma, membrane expo-
CAF+CTG+R; CAF+EMD vs. CAF+R; CAF+ADM vs. sure), and adverse reactions.
CAF+PRP; CAF+ADM vs. CAF+HF-DDS; CAF+ADM
vs. CAF+CM; CAF+ADM vs. ST; CAF+ADM vs.
Patient-based outcomes (for patient
FGG; CAF+ADM vs. LPF; CAF+ADM vs. ET+CTG;
reference use)
CAF+ADM vs. CAF+ADMP15; CAF+ADM vs.
CAF+CTG+R; CAF+ADM vs. CAF+R; CAF+PRP vs. The following variables were considered: level of
CAF+HF-DDS; CAF+PRP vs. CAF+CM; CAF+PRP vs. functional satisfaction; level of aesthetic satisfaction;
ST; CAF+PRP vs. FGG; CAF+PRP vs. LPF; CAF+PRP dentinal hypersensitivity; pain; and cost.
vs. ET+CTG; CAF+PRP vs. CAF+ADMP15; CAF+PRP
vs. CAF+CTG+R; CAF+PRP vs. CAF+R; CAF+HF-
Identification of scientific sources:
DDS vs. CAF+CM; CAF+HF-DDS vs. ST; CAF+HF-
search strategy
DDS vs. FGG; CAF+HF-DDS vs. LPF; CAF+HF-DDS
vs. ET+CTG; CAF+HF-DDS vs. CAF+ADMP15; Identification of studies considered eligible for inclu-
CAF+HF-DDS vs. CAF+CTG+R; CAF+HF-DDS sion in these guidelines was performed independently
vs. CAF+R; CAF+CM vs. ST; CAF+CM vs. FGG; and in duplicate (UP and RR) according to compre-
CAF+CM vs. LPF; CAF+CM vs. ET+CTG; CAF+CM hensive search strategies prepared for each database.
vs. CAF+ADMP15; CAF+CM vs. CAF+CTG+R; The electronic search of the literature was conducted,
CAF+CM vs. CAF+R; ST vs. FGG; ST vs. LPF; ST vs. up to 28 February, 2013, and included nine data-
ET+CTG; ST vs. CAF+ADMP15; ST vs. CAF+CTG+R; bases: (1) Cochrane Database of Systematic Reviews;
ST vs. CAF+R; FGG vs. LPF; FGG vs. ET+CTG; FGG (2) Cochrane Central Register of Controlled Trials
vs. CAF+ADMP15; FGG vs. CAF+CTG+R; FGG vs. (CENTRAL); (3) Embase; (4) MEDLINE (PubMed); (5)
CAF+R; LPF vs. ET+CTG; LPF vs. CAF+ADMP15; National Institute for Health and Clinical Excellence;
LPF vs. CAF+CTG+R; LPF vs. CAF+R; ET+CTG vs. (6) National Guideline Clearinghouse; (7) National
CAF+ADMP15; ET+CTG vs. CAF+CTG+R; ET+CTG Library of Guidelines; (8) NHS Economic Evaluation
vs. CAF+R; CAF+ADMP15 vs. CAF+CTG+R; Database; and (9) Centre for Reviews and Dissemina-
CAF+ADMP15 vs. CAF+R; CAF+CTG+R vs. CAF+R. tion. Databases were searched to include all SRs and
RCTs ever published. The electronic search on the
With regard to the barrier (BM), both resorbable Cochrane, Embase and PubMed databases was con-
and non-resorbable membranes were grouped ducted using the search strategies listed in Table 1.
together. Acellular dermal matrix (ADM), xeno- The searches on the other electronic databases were
genic collagen matrix (CM) and anorganic bovine conducted asking questions with free text.
derived hydroxyapatite matrix cell bridging peptide Moreover, four reviewers (DF, JB, ML, TS) con-
(ADMP15) were considered separately. Results con- ducted a manual search of the SRs and RCTs pub-
cerning combinations of the above treatments were lished from 1 January, 1985 to 28 February, 2013 in
not taken into consideration because the literature the following journals: Journal of Clinical Periodon-
available on these techniques is still scanty and very tology, Journal of Periodontology, Journal of Peri-
heterogeneous, and it would be difficult to deter- odontal Research, International Journal of Prosthetic
mine the contributions of the single techniques to and Restorative Dentistry, Perio, and Periodontology
the overall results. 2000. Furthermore, SRs and RCTs were sought in
the bibliographies (i.e. reference lists) of the selected
studies.
Eur J Oral Implantol 2014;7(1):9–43
16 Pini-Prato et al Guidelines for single gingival recessions
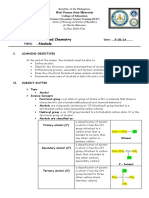
Table 1 Electronic search strategies for each respective database.
Database Type of study Strategy
Cochrane SR – (‘Gingival Recession/surgery’ [Mesh] OR ‘Gingival Recession/therapy’ [Mesh]) AND
(Cochrane Reviews [ptyp])
– (‘Gingival Recession/surgery’ [Mesh] OR ‘Gingival Recession/therapy’ [Mesh]) AND
(Other Reviews [ptyp])
RCT (‘Gingival Recession/surgery’ [Mesh] OR ‘Gingival Recession/therapy’ [Mesh]) AND
(Clinical Trials [ptyp])
Embase SR ‘gingiva disease’/exp/mj AND ‘gingival recession’/mj AND ([Cochrane review]/lim OR
[meta analysis] /lim OR [systematic review]/lim) AND [humans]/lim
RCT ‘gingiva disease’/exp/mj AND ‘gingival recession’/mj AND [randomised controlled trial]/
lim AND [humans]/lim
PubMed SR (‘Gingival Recession/surgery’ [Mesh] OR ‘Gingival Recession/therapy’ [Mesh]) AND
‘humans’ [MeSH Terms] AND Meta-Analysis [ptyp])
RCT (‘Gingival Recession/surgery’ [Mesh] OR ‘Gingival Recession/therapy’ [Mesh]) AND
‘humans’ [MeSH Terms] AND Randomised Controlled Trial [ptyp])
SR: Systematic Review; RCT: Randomised Controlled Trial.
In addition, in cases where more than one SR the use of checklists prepared specifically for the
was published on the same subject by the same qualitative evaluation of SRs with meta-analyses61.
authors, the most recent SR was selected. The Working independently, three researchers (JB, ML,
search also sought out any RCTs dated after the and MN) analysed the full texts of the selected
publication of the selected SRs. In the event that RCTs according to the SIGN method that calls for
no SRs meeting the inclusion criteria were found, the use of checklists for the qualitative evaluation
the RCTs were evaluated directly. In the event of of RCTs61. At the conclusion of the independent
more than one RCT conducted on the same test analyses, the researchers compared their evalua-
population, the RCT with the longest follow-up was tions with the aim of reaching agreement. If reach-
considered. The RCTs that dealt with more than ing unanimity was difficult, the final results were
one site in the same patient were excluded if the obtained after a discussion involving all members
statistical analysis did not take into account the of the research team.
presence of non-independent sites. In case of sev-
eral selected SRs with the same comparisons, data
Data extraction from scientific sources
from the largest and most recent SR are reported.
Subsequently, three reviewers (JB, ML, and UP) Four independent researchers (JB, ML, MN, and
compared the results of the electronic and manual UP) extracted and then compared the available
searches to eliminate duplicated articles and arrive data from the selected SRs and RCTs. If reach-
at two separate lists for both SRs and RCTs. Finally, ing unanimity was difficult, the final results were
by reading the abstracts of the found SRs and RCTs, obtained after a discussion involving all members
the same three reviewers selected the articles to of the research team.
submit to full-text reading.
Methods for formulating the
Selection and evaluation of scientific recommendations
sources: full text analysis
The methods used to formulate the recommenda-
Four independent researchers (DF, JB, MN, and RR) tions were based on a group discussion followed by
analysed the complete texts of the selected reviews voting in accordance with the suggestions of SIGN.
according to the method of the Scottish Intercol-
legiate Guidelines Network (SIGN) that calls for
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 17
Results Fig 1 Flow chart of manuscripts screened for the development of the guidelines.
SIGN: Scottish Intercollegiate Guidelines Network; SRs: Systematic Reviews; RCTs: Ran-
domised Controlled Trials.
SRs
Regarding the SRs, the outcomes of electronic and Systematic reviews identified via elec- Centre for Reviews and Dissemination: 11
tronic searching: Systematic reviews identified via hand
hand searching are shown in Fig 1. Twenty-four • Cochrane Database of Systematic searching:
articles were identified during electronic searching, Reviews: 9 • Journal of Clinical Periodontology: 3
• Embase: 23 • Journal of Periodontology: 9
whereas hand searching yielded 13 publications. • MEDLINE (PubMed): 17 • Journal of Periodontal Research: 1
• National Institute for Health and
Crossing-checking the results of both searches identi- Clinical Excellence: 0
• International Journal of Periodontics
and Restorative Dentistry: 0
fied a final list of 30 different reviews, but of them • National Guideline Clearinghouse: 0
10 were promptly excluded after their abstracts were
examined. The full texts of the 20 remaining SRs still Total number of different reviews Total number of different reviews
eligible for inclusion were screened, but only five met found by electronic searches: 24 found by hand searches: 13
the inclusion criteria for the present guidelines42,62-65.
Total number of different reviews
Of these five SRs submitted to judgment by the SIGN
following exclusion of duplicates
checklist method, the results of three SRs42,64,65 were (electronic + manual searches): 30
accepted for the drafting of these guidelines. Two
reviews were not used for the recommendations pre- Reviews selected by reading
sented in the guidelines, due to the date of publica- abstracts: 20
tion44 and the peculiarity of the statistical analysis (i.e.
individual patient data meta-analysis)45.
Reviews selected by full text
All the three analysed SRs were judged to have reading: 5
a low risk for bias, according to the SIGN check-
list method (SIGN code: 1+) (Table 2). At the end
of this process, of the remaining 17 reviews, four Studies selected after evaluation
by the SIGN checklist method:
reviews66-68,76 were excluded because they were 3 SRs and 16 RCTs
not systematic; eight42,47,69-74 because they were
not SRs of only RCTs, one43 because it analysed the
same SR by Chambrone et al42; one45, because it Articles selected by full text
reading: 16
analysed only RCTs that reported individual patient
data but excluded other well-performed RCTs that
did not publish the relative individual data, two62-63 Articles selected by reading
abstracts: 168
because they were considered to have a high risk for
bias, according to the SIGN checklist method (SIGN
code: 1-) and one75 because it considered just mul- Total number of different articles
following exclusionof duplicates
tiple gingival recessions. In addition, data from RCTs (electronic + manual searches): 321
included in the eligible SRs were also checked in the
original article.
Total number of different articles found Total number of different articles found
by electronic searches: 300 by hand searches: 132
RCTs
The electronic searches yielded 263 publications in RCTs identified via electronic searching: RCTs identified via hand searching:
• Cochrane Database of Systematic • Journal of Clinical Periodontology: 24
the Cochrane database, 176 in Embase and 287 in Reviews: 263 • Journal of Periodontology: 71
PubMed, regarding a single list of 300 articles fol- • Embase: 176
• Journal of Periodontal Research: 0
• MEDLINE (PubMed): 287
lowing elimination of duplicates (Fig 1). The manual • National Institute for Health and • International Journal of Prosthetic and
Clinical Excellence: 0 Restorative Dentistry: 20
search yielded 132 articles. Crossing-checking the • Perio: 2
• National Guideline Clearinghouse: 0
results of both searches identified a final list of 321
different articles.
Eur J Oral Implantol 2014;7(1):9–43
18 Pini-Prato et al Guidelines for single gingival recessions
Table 2 SIGN Grading System.
LEVELS OF EVIDENCE
1++ High-quality meta-analyses, SRs, or RCTs, or RCTs with a very low risk for bias
1+ Well-conducted meta-analyses, SRs, of RCTs, or RCTs with a low risk for bias
1- Meta-analyses, SRs of RCTs, or RCTs with a high risk for bias
2++ High-quality case-control or cohort studies with a very low risk of confounding, bias, or chance and a high
probability that the relationship is causal
2+ Well-conducted case-control or cohort studies with a low risk for confounding, bias, or chance and a moder-
ate probability that the relationship is causal
2- Case-control or cohort studies with a high risk of confounding, bias, or chance and a significant risk that the
relationship is not causal
3 Non-analytic studies, e.g. case report, case series
4 Expert opinion
GRADES OF RECOMMENDATIONS
A At least one meta-analysis, SR, or RCT rated as 1++ and directly applicable to the target population; or an SR
of RCTs or a body of evidence consisting principally of studies rated as 1+, directly applicable to the target
population, and demonstrating overall consistency of results
B A body of evidence including studies rated as 2++, directly applicable to the target population, and demon-
strating overall consistency of results; or extrapolated evidence from studies rated as 1++ or 1+
C A body of evidence including studies rated as 2+, directly applicable to the target population, and demon-
strating overall consistency of results; or extrapolated evidence from studies rated as 2++
D Evidence level 3 or 4; or extrapolated evidence from studies rated as 2+
SIGN: Scottish Intercollegiate Guidelines Network; SR: Systematic Review; RCT: Randomised Controlled Trial.
Subsequent to the examination of 321 selected a medium term duration (from 13 to 60 months),
abstracts, 168 articles had their full text considered and only 1 study87 showed a 120-month duration.
for inclusion. At the end of this process, 152 of Data about the number of treated patients in each
the 168 selected articles were excluded from the included RCT are reported in the Appendix.
guidelines and the reasons for exclusion are listed The final analysis of the 3 SRs and the 16 RCTs
in Table 3. At this point, by reading the full texts included in this study enabled the assessment of 19
of these selected articles, only 16 RCTs52-53,77-89,240 different comparisons (Table 4). In addition, detailed
met the proposed criteria and were included in the descriptions of the study characteristics and out-
present guidelines. These 16 articles were com- comes of included SRs and RCTs are depicted in the
parisons of surgical techniques that were either not Appendix.
discussed in the three selected SRs (i.e. RCTs that
reported comparisons of surgical techniques not
Patient, dental hygienist and general
found through the SRs) or were published after the
practitioner involvement in guidelines
reference period of the same SRs. The 16 selected
development
RCTs were analysed according to the SIGN checklist
method and were all judged to have a low risk for
Patients
bias, according to that method (SIGN code: 1+).
With regard to the type of study design, out of In a recent study54, a questionnaire-based survey
the 16 included RCTs1152,77,79-80,82-83,85-87,89,240 investigated the perception of buccal gingival reces-
had a split-mouth design, while 5 RCTs53,78,81,84,88 sions and the request for their treatment. Out of
had a parallel design. these 120 patients, only 54 (45%) answered that
With respect to the duration of the follow-up, 11 they had gingival recessions, while 96 (80%) actually
RCTs53,77,79,81-84,86,88-89,240 had a short follow-up had at least one gingival recession in their mouth.
(from 1 to 12 months duration), 4 RCTs52,78,80,85 had Only 11 (11%) of the 96 patients with recessions
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 19
Table 3 Characteristics of the 152 excluded studies.
Reason for exclusion Studies
Miller Class not specified or Guinard et al90; Caffesse et al91; Caffesse et al92; Espinel et al93; Cueva et al 94; Henriques et al95; Cairo et al96
Miller Class III gingival reces-
sions defects treated
Not comparison between sur- Borghetti et al97
gical techniques
Not study on root coverage Wei et al98; Maurer et al99; Harris100; McGuire et al101; Bertoldi et al 102; McGuire et al103; Sanz et al104; Dilsiz
et al105; Dilsiz et al106; Nevins et al107; McGuire et al108; Nevins et al109
Comparison between Ibbott et al110; Oles et al111; Caffesse et al112; Bouchard et al113; Trombelli et al114; Roccuzzo et al115; Trombelli
variations of the same surgical et al116; Bouchard et al117; Matarasso et al118; Pini Prato et al119; Caffesse et al120; Pini Prato et al121; Hender-
technique son et al122; Del Pizzo et al123; Zucchelli et al124; Barros et al125; Barros et al126, Burkhardt & Lang127; Francetti
et al128; Tozum et al29; Kassab et al130; Al-Zahrani et al131; Barros et al132; Bittencourt et al133; Felipe et al134;
Lucchesi et al135; Andrade et al136; Byun et al137; Zucchelli et al138; Zucchelli et al139; Andrade et al140; Barker et
al141; Zucchelli et al142; Mazzocco et al143; Ozturan et al144; Pini Prato et al145; Mahajan et al146; Bittencourt et
al147; Ayub et al148; Kuru & Yildirim149
Not RCT Pini Prato et al150; Trombelli et al151; Pini Prato et al152; Wennströmm et al153; Harris154; Ozcan et al155; Har-
ris156; Muller et al157; Harris158; Cordioli et al159; Nemcovsky et al160; Berlucchi et al161; Harris et al162; Hirsch et
al163; Erley et al164; McGuire et al165; Moses et al166; Silva et al167; Keceli et al168; Pini Prato et al169; Santamaria
et al170; Schlee et al171
Follow-up <6 months Laney et al172; Lafzi et al173; Han et al174; Papageorgakopoulos et al175; Barbosa et al176; de Toledo et al177;
Shepherd et al178; Lafzi et al179; Baghele et al180
Study already considered in Jepsen et al181; Trombelli et al182; Zucchelli et al183; Borghetti et al184; Amarante et al185; Tatakis et al186; Mod-
the selected SRs ica et al187; Aichelmann-Reidy et al188; Romagna-Genon189; Wang et al190; Hagewald et al191; Paolantonio et
al192; Tal et al193; Lins et al194; McGuire et al195; Cortes et al196; da Silva et al197; Woodyard et al198; Del Pizzo
et al199; Huang et al200; Leknes et al201; Spahr et al202; Wilson et al203; Castellanos et al204; Cortes et al205; Pil-
loni et al206; Joly et al207; Cortellini et al55
Comparison with a combina- Dodge et al208; Duval et al209; Rosetti et al210; Berlucchi et al161; Paolantonio et al211; Kimble et al212; Trabulsi et
tion of techniques al213; Cardaropoli et al214; McGuire et al103; Jankovic et al215; Jhaveri et al216; Alkan et al217; Rasperini et al218;
Alves et al219; Jankovic et al220
Inadequate statistics Ricci et al221; Novaes et al222; Cetiner et al223; Cheung et al224; Rahmani et al225; Abolfazli et al226; Banihashem-
rad et al227; Cardaropoli et al228
Not surgical therapy Aimetti et al229
Multiple gingival recessions Ito et al230; Dembowska et al231; Shin et al232; De Souza et al233; Aroca et al234; Pourabbas et al235; Nickles et
treated al236; Aroca et al237; Ozcelik et al 238; Cordaro et al239
RCT: Randomised Controlled Trial; SRs: Systematic Reviews.
requested treatment for their recessions. One patient General practitioners
(JW), representative of these 120 patients, partici-
pated in developing the guidelines and stated that After an accurate reading of the document, a repre-
the reading of the full guidelines appears under- sentative of three general practitioners (LP) reported
standable and clear. that the knowledge of the ‘gingival recession’ issue
is scarce. The association of dental hypersensitivity
with the ‘longer tooth’ has been identified as a rele-
Dental hygienist
vant factor for undergoing treatment. In addition,
The dental hygienists involved in these clinical guide- one physician focused his attention on the insurance
lines reported through their representative (MG) that aspects related to this document, if it will be consid-
the reading of the full text is understandable. They ered its use in countries where the private insurance
suggested the inclusion of non-surgical treatments companies works also in this field.
(such as single restorative approach or use of desen-
sitising gel) of gingival recessions in a future version
of the guidelines.
Eur J Oral Implantol 2014;7(1):9–43
20 Pini-Prato et al Guidelines for single gingival recessions
Table 4 Final eligible trials selected for the guidelines. for Health Care Policy and Research3, approved and
introduced in 2000. The evidence levels are rated
COMPARISON STUDIES
by four (Arabic) numerals and ++, +, and - signs
CAF vs. CAF+CTG Cairo et al 64
(decreasing levels of evidence: 1++, 1+, 1-, 2++, 2+,
CAF vs. CAF+BM Cairo et al64
2-, 3,4). The strength of the recommendations is clas-
CAF vs. CAF+EMD Cairo et al64
sified in four levels indicated by letters (decreasing
CAF vs. CAF+ADM Chambrone et al42;
Mahajan et al81
strength levels) from A to D. The evidence level of a
CAF vs. CAF+PRP Cairo et al64
recommendation refers to the probability that specific
CAF vs. ST Santana et al83
knowledge is obtained from studies with low risk for
CAF vs. LPF Santana et al84
bias. The strength of the recommendations refers to
CAF vs. CAF+ADMP15 Nazareth & Cury86
the probability that transferring them to clinical prac-
CAF vs. CAF+R Santamaria et al, 200952
tice can promote improvement in the health of the
CAF vs. CAF+CM Jepsen et al89
population for which the recommendation was made.
CAF+CTG vs. CAF+BM Cairo et al64; Chambrone
et al65
CAF+CTG vs. CAF+EMD Cairo et al64; McGuire
et al87
Evidences
CAF+CTG vs. CAF+ADM Cairo et al64; Haghighati
et al82; Moslemi et al85 Efficacy
CAF+CTG vs. CAF+PRP Chambrone et al42
1. Which is the most appropriate surgical technique
CAF+CTG vs. CAF+HF-DDS Cairo et al64
for treating single gingival recessions in terms of
CAF+CTG vs. ST Bittencourt et al79,80
complete root coverage and recession reduction?
CAF+CTG vs. FGG Paolantonio et al78
CAF+CTG vs. CAF+CTG+R Santamaria et al53
ET+CTG vs. FGG Jahnke et al77 Complete Root Coverage (CRC)
CAF+CTG vs. CAF+CM Mc Guire et al240
CAF+CTG vs. LPF Zucchelli et al88 CAF vs. CAF+CTG
CAF: Coronally Advanced Flap; CTG: Connective Tissue Graft; BM:
resorbable and non-resorbable Barrier Membrane; EMD: Enamel A meta-analysis of two studies55,197 comparing CAF
Matrix Derivative; ADM: Acellular Dermal Matrix; PRP: Platelet- vs. CAF+CTG showed a statistically significant Odds
Rich Plasma; HF-DDS: Human Fibroblast-Derived Dermal Substi-
Ratio (OR) of 2.49 (CI 95%: 1.10 to 5.68; P = 0.03;
tute; CM: Xenogenic Collagen Matrix; ST: Semilunar Technique;
FGG: Free Gingival Graft; LPF: Laterally Positioned Flap; ET: Enve- I2 = 0%) in favour of CAF+CTG64. The total per-
lope Technique; ADMP15: Anorganic Bovine Derived Hydroxyapa- centage of CRC was 52% (27/52 recessions) for
tite Matrix Cell Bridging Peptide; R: Resin Composite Restoration.
CAF+CTG and 32% (17/53 recessions) for CAF.
Guide to evidence levels and strength of CAF vs. CAF+BM
the recommendations (Table 2)
Data from 12 months of a split-mouth study201
In accordance with the suggestions of the SIGN61, comparing CAF vs. CAF+BM showed a not statis-
recommendations in these guidelines distinguish tically significant OR of 0.58 (CI 95%: 0.16 to 2.08;
between those supported by strong evidence and P = 0.41) in favour of CAF64. The percentage of CRC
those based on trials of lower scientific value. It is was 30% (6/20 recessions) for CAF and 20% (4/20
important to bear in mind that the grading of a rec- recessions) for CAF+BM.
ommendation is not related to the importance of the
recommendation itself, but to the strength of the
CAF vs. CAF+EMD
supporting scientific trials.
The recommendations are classified by evidence A meta-analysis of four studies187,199,202,206 compar-
level and strength of the recommendations in accord- ing CAF vs. CAF+EMD showed a statistically signifi-
ance with the guidelines of the United States Agency cant OR of 3.89 (CI 95%: 1.59 to 9.50; P = 0.003;
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 21
I2 = 15.2%) in favour of CAF+EMD64. The total CAF vs. CAF+ABM/P-15
percentage of CRC was 66% (46/70 recessions) for
CAF+EMD and 39% (27/70 recessions) for CAF. In a split-mouth 6-month RCT86, 10 out 15 sites
(67%) in the CAF+ABM/P-15 showed CRC, while
11 out 15 sites (73%) treated with CAF alone
CAF vs. CAF+ADM
obtained CRC. P value was not reported. A calcu-
A meta-analysis of two studies205,198 comparing CAF lation yielded an OR=0.73 (CI 95%: 0.18 to 2.86;
vs. CAF+ADM showed a not statistically significant P = 0.65) in favour of CAF.
Relative Risk (RR) of 1.95 (CI 95%: 0.76 to 5.04;
P = 0.17; I2 = 34%) in favour of CAF+ADM42. The
CAF+CTG vs. CAF+BM
total percentage of CRC was 48% (12/25 recessions)
for CAF+ADM and 20% (5/25 recessions) for CAF. Two meta-analyses showed very similar results on
this comparison in terms of odds ratio64,65.
A meta-analysis of 7 studies182-184,186,189,200,211
CAF vs. CAF+PRP
comparing CAF+CTG vs. CAF+BM (resorbable
One parallel 6-month study200 comparing CAF vs. membranes) showed a statistically significant OR of
CAF+PRP showed a not statistically significant OR 0.47 (CI 95%: 0.24 to 0.90; P = 0.02; I2 = 0%) in
of 1.25(CI 95%: 0.23 to 6.71; P = 0.79) in favour of favour of CAF+CTG65.
CAF+PRP64. The percentage of CRC was 64% (7/11 A meta-analysis of 6 studies181-184,186,190 com-
recessions) for CAF+PRP and 58% (7/12 recessions) paring CAF+CTG vs. CAF+BM showed a not statis-
for CAF. tically significant OR of 0.45 (CI 95%: 0.20 to 1.04;
P = 0.06; I2 = 31.9%) in favour of CAF+CTG64. The
total percentage of CRC was 53% (46/87 reces-
CAF vs. CAF+CM
sions) for CAF+CTG and 36% (38/105 recessions)
In a split-mouth 6-month RCT89, CRC was achieved for CAF+BM.
in 16 out of 45 sites (36%) treated with CAF+CM
and in 14 out of 45 sites (31%) treated with CAF
CAF+CTG vs. CAF+EMD
alone. The difference was not statistically significant
(P = 0.3870). Data from one study195 comparing CAF+CTG vs.
CAF+EMD showed a not statistically significant
OR of 2.31 (CI 95%: 0.45 to 11.74; P = 0.31) in
CAF vs. ST
favour of CAF+EMD64. In the 10-year follow-up of
In a split-mouth 6-month RCT83, 2 out of 22 sites the same split-mouth study with 9 patients (out of
(9%) belonging to the ST group showed CRC, while 17), 5 out of 9 sites (56%) in the CAF+EMD group
14 out 22 sites (64%) treated with CAF obtained showed CRC, while 7 out of 9 sites (78%) treated
CRC. P value was not reported. A calculation using with CAF+CTG achieved CRC (P = 0.157)87.
the intra-class correlation coefficient of a previous
study190 yielded an OR = 0.06 (CI 95%: 0.01 to
CAF+CTG vs. CAF+ADM
0.26; P = 0.0002) in favour of CAF.
A meta-analysis of four studies188,192,193,207 com-
paring CAF+CTG vs. CAF+ADM showed a not stat-
CAF vs. LPF
istically significant OR of 0.49 (CI 95%: 0.23 to 1.03;
In a parallel 6-month RCT84, 15 out of 18 sites (83%) P = 0.06; I2 = 0%) in favour of CAF+CTG64.
belonging to the LPF group showed CRC, while In a successive split-mouth 5-year RCT, 3 out of
16 out of 18 sites (89%) treated with CAF alone 15 sites (20%) in the CAF+ADM group showed CRC,
obtained CRC. P value was not reported (P >0.05). while 2 out of 15 sites (13%) treated with CAF+CTG
A calculation yielded an OR=0.63 (CI 95%: 0.09 to achieved CRC85. The difference favouring CAF+ADM
4.28; P = 0.63) in favour of CAF. was not significant (P = 1.0). The total percentage of
Eur J Oral Implantol 2014;7(1):9–43
22 Pini-Prato et al Guidelines for single gingival recessions
CRC was 39% (27/69 recessions) for CAF+CTG and ET+CTG vs. FGG
25% (17/69 recessions) for CAF+ADM.
In a split-mouth 6-month RCT77, 5 out of 9 sites
(56%) in the ET+CTG group showed CRC, while
CAF+CTG vs. CAF+HF+DDS
1 out of 9 sites (11%) treated with FGG achieved
One split-mouth 6-month study203 comparing CRC. P value was not reported. A calculation yielded
CAF+CTG vs. CAF+HFDDS showed a not statistic- an OR = 0.10 (CI 95%: 0.01 to 0.88; P = 0.04) in
ally significant OR of 1.00 (CI 95%: 0.02 to 50.40; favour of ET+CTG.
P = 1.00)64. The percentage of CRC was 10% (1/10
recessions) for CAF+CTG and 10% (1/10 recessions)
Recession Reduction (RecRed)
for CAF+HF+DDS.
CAF vs. CAF+CTG
CAF+CTG vs. CAF+CM
A meta-analysis of two studies55,197 comparing CAF
In a split-mouth RCT240, at the 12-month evalu- vs. CAF+CTG showed a statistically significant dif-
ation, 17 out of 23 sites (74%) in the CAF+CM ference in terms of RecRed of 0.49 mm (CI 95%:
group showed CRC, while 22 out of 23 sites (96%) 0.14 to 0.83 mm; P = 0.005; I2 = 0%) in favour of
treated with CAF+CTG achieved CRC. P value was CAF+CTG64.
not reported (P > 0.05).
CAF vs. CAF+BM
CAF+CTG vs. ST
A meta-analysis of two studies185,194 comparing
In a split-mouth 30-month RCT80, 8 out of 17 sites CAF vs. CAF+BM showed a not statistically signifi-
(47%) in the ST group showed CRC, while 15 out cant difference in terms of RecRed of -0.27 mm
of 17 sites (88%) treated with CAF+CTG achieved (CI 95%: -0.60 to 0.06 mm; P = 0.11, I2 = 0%) in
CRC. P value was not reported. A calculation yielded favour of CAF64.
an OR = 0.19 (CI 95%: 0.04 to 0.91; P = 0.04) in
favour of CAF+CTG.
CAF vs. CAF+EMD
A meta-analysis of five studies187,199,202,204,206 com-
CAF+CTG vs. FGG
paring CAF vs. CAF+EMD showed a statistically sig-
In a parallel 5-year RCT78, 3 out of 35 sites (9%) nificant difference in terms of RecRed of 0.58 mm
in the FGG group showed CRC, while 17 out of 35 (CI 95%: 0.21 to 0.95 mm; P = 0.002; I2 = 50.5%)
sites (49%) treated with CAF+CTG achieved CRC. in favour of CAF+EMD64.
The P value was not reported. A calculation yielded
an OR = 0.10 (CI 95%: 0.03 to 0.39; P = 0.0008) in
CAF vs. CAF+ADM
favour of CAF+CTG.
A meta-analysis of two studies196,198 comparing
CAF vs. CAF+ADM showed a not statistically sig-
CAF+CTG vs. LPF
nificant difference in terms of RecRed of 0.62 mm
In a parallel 1-year RCT88, CRC was achieved in 12 (CI 95%: -0.51 to 1.74 mm; P = 0.28; I2 = 84%) in
out of 25 defects in the CAF+CTG group (48%), favour of CAF+ADM42.
and in 1 out of 25 in the LPF group (4%). The differ- In one parallel 6-month RCT81, CAF+ADM pro-
ence was statistically significant (P <0.05), favouring cedure showed a reduction of 3.85 ± 0.89 mm;
CAF+CTG. while the CAF technique resulted in 2.85 ± 0.89 mm
reduction. The difference was statistically significant
(P = 0.05).
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 23
CAF vs. CAF+PRP CAF+CTG vs. CAF+ADM
Data from one parallel 6-month study200 comparing A meta-analysis of four studies188,192,193,207 com-
CAF vs. CAF+PRP showed a not statistically signifi- paring CAF+CTG vs. CAF+ADM showed a not
cant difference in terms of RecRed of -0.20 mm (CI statistically significant difference in terms of Rec-
95%: -0.89 to 0.49 mm; P = 0.57) in favour of CAF64. Red of -0.40 mm (CI 95%: -1.07 to 0.26; P = 0.24;
I2 = 79.4%) in favour of CAF+CTG64.
In a subsequent split-mouth 5-year RCT85,
CAF vs. CAF+CM
CAF+ADM procedure showed a reduction of
In a split-mouth 6-month RCT89, the CAF+CM 1.60 ± 1.22; while the CAF+CTG technique resulted in
procedure showed a reduction of 2.59 ± 1.11 mm, 1.50 ± 1.42 mm reduction. The difference was not stat-
while CAF technique resulted in 2.32 ± 0.99 mm of istically significant (P = 0.838) favouring CAF+ADM.
recession reduction. The difference was statistically
significant (P = 0.0175) in favour of CAF+CM.
CAF+CTG vs. CAF+EMD
In a split-mouth 10-year RCT87, the CAF+EMD pro-
CAF vs. ST
cedure showed a reduction of 3.33 ± 0.87 mm; while
In a split-mouth 6-month RCT83, ST procedure the CAF+CTG technique resulted in 3.67 ± 1.12 mm
showed a reduction of 1.2 ± 0.5 mm; while the CAF reduction. The difference was not statistically signifi-
technique resulted in a 2.6 ± 0.7 mm reduction. cant (P = 0.625).
The difference was statistically significant (P <0.05),
favouring CAF procedure.
CAF+CTG vs. CAF+CM
In a split-mouth 1-year RCT240, CAF+CM procedure
CAF vs. LPF
showed a reduction of 2.78 mm; while the CAF+CTG
In a parallel 6-month RCT84, LPF procedure showed technique resulted in 3.17 mm reduction. The differ-
a reduction of 3.26 ± 0.4 mm; while the CAF tech- ence was statistically significant (P = 0.0172) favour-
nique resulted in a 3.09 ± 0.5 mm reduction. The ing CAF+CTG.
difference was not statistically significant (P = 0.26
t test).
CAF+CTG vs. LPF
In a parallel 1-year RCT88, the CAF+CTG procedure
CAF vs. CAF+ABM/P-15
showed a reduction of 4.04 ± 0.64 mm, while LPF
In a split-mouth 6-month RCT86, CAF+ABM/P-15 technique resulted in 3.68 ± 0.75 mm of recession
procedure showed a reduction of 2.20 ± 0.54 mm; reduction. The difference was not statistically signifi-
while the CAF technique resulted in 2.40 ± 0.80 mm cant (P = 0.07 t test).
reduction. The difference (-0.20 ± 0.14 mm, favour-
ing CAF group) was not statistically significant 2. Which is the most effective surgical technique
(P = 0.33). for recessions associated with non-carious cervical
lesions?
CAF+CTG vs. CAF+BM
CAF vs. CAF+R
A meta-analysis of 6 studies181-184,186,190 comparing
CAF+CTG vs. CAF+BM showed a statistically signifi- In one split-mouth 2-year RCT52, CAF+R procedure
cant difference in terms of RecRed of -0.38 mm (CI showed a reduction of 1.31 ± 0.37 mm; while the
95%: -0.65 to -0.10 mm; P = 0.008; I2 = 45.6%) in CAF technique resulted in 1.39 ± 0.41 mm reduction
favour of CAF+CTG64. in 16 patients. The difference was not statistically
significant (P >0.05).
Eur J Oral Implantol 2014;7(1):9–43
24 Pini-Prato et al Guidelines for single gingival recessions
CAF+CTG vs. CAF+CTG+R was statistically significant (P = 0.03), favouring the
CAF group81.
In one parallel 6-month RCT53, CAF+CTG+R pro- Postoperative pain and swelling: 2 out of 7
cedure showed a reduction of 2.31 ± 0.74 mm in 20 patients in the CAF+ADM group were fully satisfied,
patients; while the CAF+CTG technique resulted in and 6 out of 7 patients in the CAF group were also
2.53 ± 0.78 mm reduction in 20 patients. The differ- fully satisfied. The difference was statistically signifi-
ence was not statistically significant (P = 0.41). cant (P = 0.03), favouring the CAF group81.
Cost effectiveness: 2 out of 7 patients in the
CAF+ADM group were fully satisfied, and 6 out of
Complications
7 patients in the CAF group were also fully satisfied.
3. Which is the surgical technique for the treatment of The difference was statistically significant (P = 0.03),
single gingival recessions with less adverse reactions favouring the CAF group81.
(discomfort, postoperative pain, haematoma etc.)?
CAF vs. CAF+CM
CAF vs. CAF+CTG
In a RCT89, after 7 days, the pain VAS was 2.32 ± 2.08
da Silva et al197 reported no complications on com- for CAF+CM and 2.04 ± 1.82 for CAF. After 14 days,
paring CAF vs. CAF+CTG. Cortellini et al55 reported the pain VAS was 0.68 ± 1.21 for CAF+CM and
3 cases of haematoma in 43 patients treated with 0.59 ± 0.91 for CAF. The differences were not stat-
CAF, while 5 cases of haematoma were reported in istically significant (P >0.05).
42 patients treated with CAF+CTG. A higher number
of cases of swelling were reported for the CAF+CTG
CAF+CTG vs. CAF+BM
group, and these differences were statistically signifi-
cant (CAF+CTG 32.2 ± 28.4 and CAF 17.8 ± 19.9 In comparisons between CAF+CTG vs. CAF+BM,
using visual analogue scale (VAS), P = 0.0068). No membrane exposure was reported as a complication
statistically significant differences for pain were (7/15181, 2/12182, 5/12186, 0/20189).
reported between two groups (23.8 ± 19.4 for Jepsen et al181 reported pain and swelling on
CAF and 31.4 ± 24.6 for CAF+CTG, using VAS, comparing CAF+CTG vs. CAF+BM in 15 split-mouth
P = 0.0811). patients. Five patients reported more discomfort
after CAF+CTG, 5 patients following CAF+BM,
whereas the remaining 5 patients experienced no
CAF vs. CAF+BM
difference. When asked which technique they would
Lins et al194 reported the exposure of all membranes have preferred for future root coverage, 7 patients
in all treated sites (10/10). opted for the CAF+CTG, and 8 for the CAF+BM.
Tatakis and Trombelli186 reported 7 cases of swell-
ing in 12 patients treated with CAF+BM and none
CAF vs. CAF+PRP
for CAF+CTG. On the other hand, no complications
No statistically significant differences for com- for CAF+BM were reported by Wang et al190: they
plications were reported on comparing CAF vs. reported 1 of 16 cases of swelling and 1 ecchymosis
CAF+PRP200 using a Wound Healing Index (1.3 ± 0.5 in the CAF+CTG arm. Romagna-Genon189 described
for CAF and 1.2 ± 0.4 for CAF+PRP, P >0.05). postoperative discomfort for the palatal donor site
for the CAF+CTG. None of the sites showed expo-
sure of the membrane.
CAF vs. CAF+ADM
Pain and discomfort during surgery: 2 out of 7
CAF+CTG vs. CAF+EMD
patients in the CAF+ADM group reported no pain or
discomfort, and 6 out of 7 patients in the CAF group McGuire and Nunn195 compared CAF+CTG vs.
also reported no pain or discomfort. The difference CAF+EMD: at 1 month, 9 patients (45%) reported
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 25
high discomfort levels associated with the CAF+CTG After 7 days the VAS values related to chew-
treatment as opposed to 1 patient (5%) in the ing ability were 72.8 ± 14.3 for CAF+CTG and
CAF+EMD group. This difference was statistically sig- 88.8 ± 8.3 for LPF. The difference favouring LPF was
nificant (P = 0.011). Ten patients (50%) reported no statistically significant (P <0.01).
differences in discomfort between the two treatments.
At 3 months, 5 patients (25%) reported discomfort
Patient opinions
with CAF+CTG treatment as opposed to 3 patients
(15%) reporting discomfort with CAF+EMD. After 6 4. Which is the most effective surgical technique for
months, differences in discomfort levels between the the treatment of single gingival recessions in terms
two groups were minimal. At 1 year, only 1 patient of: (a) Absence of dental hypersensitivity.
exhibited any ongoing adverse reaction. In this sub-
ject, the CAF+CTG site was still mildly painful, and
CAF vs. CAF+CTG
the CAF+EMD site was still mildly sensitive. The only
reported adverse events were pain, swelling, bleed- In a parallel RCT, Cortellini et al55 compared CAF vs.
ing, bruising, and sensitivity. These events were simi- CAF+CTG, reporting no statistically significant dif-
larly distributed among both groups. ferences for dental sensitivity [5/42 patients (12%)
At the 10-year follow-up visit87, the patients in the CAF+CTG group and 5/43 patients (12%) in
were asked to indicate their preference of the pro- the CAF group] 6 months following therapy (P = 1.0
cedure: 6 out of 9 patients preferred the CAF+EMD Fisher exact test).
treatment, 1 favoured CAF+CTG, and 2 had no pref-
erence. The difference was not statistically significant
CAF vs. CAF+ADM
(P = 0.059).
In a parallel RCT, 6 out of 7 patients of the CAF+ADM
group were fully satisfied, and 5 out of 7 patients of
CAF+CTG vs. CAF+PRP
the CAF group were also fully satisfied 6 months fol-
Keceli et al168 compared CAF+CTG vs. CAF+PRP lowing therapy. The difference was not statistically
finding postoperative healing was generally une- significant (P = 0.58)81.
ventful. Immediate postoperative bleeding at the
donor site occurred in one patient in the CAF+CTG
CAF+CTG vs. CAF+EMD
group and was easily managed with a sterile gauze
compress. In a split-mouth study, at the 10-year follow-up, 3
out of 9 sites of the CAF+EMD procedure and 1 out
of 9 sites of CAF+CTG procedure showed dental
CAF+CTG vs. ST
sensitivity. The difference was not statistically signifi-
A median pain VAS score of 30 mm (range 20 to cant (P = 0.157)87.
60 mm) was recorded in CAF+CTG group and 0 mm
(meaning no pain at all) in the ST group; P value was
CAF+CTG vs. ST
not reported80. The pain intensity and the number of
pills taken were statistically different between groups In a split-mouth study, three out of 17 patients
only on the first day (P = 0.02), favouring the ST in the ST group reported dental sensitivity, while
group79. none of the patients belonging to the CAF+CTG
group reported dental sensitivity 30 months after
surgery80. The difference was not statistically signifi-
CAF+CTG vs. LPF
cant (P = 0.25, McNemar test).
In a RCT88, after 7 days the VAS values related to
pain were 77.2 ± 16.4 for CAF+CTG and 93.2 ± 8.0
for LPF. The difference favouring LPF was statistically
significant (P <0.01).
Eur J Oral Implantol 2014;7(1):9–43
26 Pini-Prato et al Guidelines for single gingival recessions
CAF+CTG vs. LPF split-mouth 6-month study. Among the 20 patients
who were treated, 19 expressed their satisfaction
In a parallel study with 25 patients per arm, sensi- with the clinical results for both tested surgical pro-
tivity VAS was 94.0 ± 6.5 for CAF+CTG group and cedures; only one patient, who had a pair of man-
87.6 ± 8.3 for LPF group. The difference favour- dibular recessions, was disappointed because of the
ing CAF+CTG was statistically significant (P <0.01) small amount of coverage obtained following both
1 year after surgery88. treatments.
Wang et al190 compared the aesthetic results of
CAF+CTG vs. CAF+BM procedures in a split-mouth
CAF+CTG vs. CAF+CTG+R
6-month study. Six out of 16 of CAF+BM sites
In a parallel study, 1 out of 20 patients reported den- rated by patients had ‘excellent’ colour match and
tal sensitivity in the CAF+CTG+R, while 7 out of 20 9 CAF+CTG sites reported the same. In overall satis-
patients showed dental sensitivity after 6 months in faction, 9 patients rated the CAF+BM procedure as
CAF+CTG. The difference was statistically significant ‘excellent’ vs. 7 in the CAF+CTG group. With regard
(P = 0.04 Fisher exact test), favouring CAF+CTG+R to the amount of root coverage, 7 patients in the
procedure53. CAF+BM group rated it ‘excellent’ with CAF+BM
procedure, while 10 patients treated with CAF+CTG
(b) Aesthetic satisfaction. did the same. The differences were not significant
(P >0.05).
CAF vs. CAF+ADM
In a parallel 6-month RCT81, aesthetic satisfaction
CAF+CTG vs. CAF+ADM
was considered as: root coverage perception, col-
our of gums and shape of gum contour: root cover- Aichelmann-Reidy et al188 compared CAF+CTG vs.
age perception: All the 7 patients in the CAF+ADM CAF+ADM in a split-mouth 6-month study in 22
group were fully satisfied, and 4 out of 7 patients in patients. Patients considered CAF+ADM to have
the CAF group were satisfied. The difference was not better aesthetics in 9 cases out of 22; in 12 cases,
statistically significant (P = 0.15)81. they considered it similar to CAF+CTG; and only 1
Colour of gums: All 7 patients in the CAF+ADM patient preferred the site with CAF+CTG. A keloid
group were fully satisfied, and 6 out of 7 patients in formation was reported in one case treated with
the CAF group were satisfied. The difference was not CAF+CTG. The difference favouring CAF+ADM was
statistically significant (P = 0.30)81. statistically significant (P = 0.0215 – McNemar test).
Shape of gum contour: 5 patients in the
CAF+ADM group were fully satisfied, and 5 out of
CAF+CTG vs. CAF+EMD
7 patients in the CAF group were also fully satis-
fied. The difference was not statistically significant With regard to aesthetic satisfaction, in a split-mouth
(P = 1)81. 10-year study, 6 patients had no preference for a
particular type of treatment, 2 declared better aes-
thetic results following CAF+EMD procedure and 1
CAF vs. ST
preferred the aesthetic outcomes of the CAF+CTG
No data are available, even if the authors of a split- procedure (P = 0.564)87.
mouth 6-month RCT reported that all sites (22/22)
treated with ST resulted in a noticeable semilunar
CAF+CTG vs. ST
white scar83.
Fourteen out of 17 patients of the ST group of a
split-mouth 30-month study reported excellent or
CAF+CTG vs. CAF+BM
good aesthetic results, and 3 reported bad results80.
Romagna-Genon189 reported aesthetic results All subjects in the CAF+CTG group reported excel-
obtained comparing CAF+CTG vs. CAF+BM in a lent or good results. Seven patients reported a bet-
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 27
ter aesthetic in the sites treated with CAF+CTG nar Technique (ST), Free Gingival Graft (FGG),
than the other treated site. No patients reported Laterally Positioned Flap (LPF) (evidence level:
any preference for the sites treated with ST, and 10 1+; grade of the recommendation: A).
patients did not report any difference in terms of 2. Which is the most effective surgical technique
preference between the two therapies80. The differ- for recessions associated with non-carious cervi-
ence favouring CAF+CTG was statistically significant cal lesions?
(P = 0.0215, McNemar test). Answer: Surgical procedures associated with res-
torations for treating sites affected by gingival
recession and non-carious cervical lesions did not
CAF+CTG vs. LPF
show greater recession reduction compared to
In a parallel 1-year study, aesthetic patient evalu- the surgical procedure alone (evidence level: 1+;
ation in a VAS was 91.2 ± 9.3 for CAF+CTG (25 grade of the recommendation: A). In case of cervi-
patients) and 89.6 ± 7.9 for LPF (25 patients). The cal abrasion and presence of root sensitivity after
difference was not statistically significant (P = 0.52, 6 months of follow-up Coronally Advanced Flap
t test)88. plus Connective Tissue Graft plus Resin Composite
Restoration (CAF+CTG+R) showed less sensitiv-
ity than Coronally Advanced Flap plus Connec-
Summary of recommendations tive Tissue Graft (CAF+CTG) (evidence level: 1+;
grade of the recommendation: A). Further studies
Recessions may not have to be treated. If it is on these aspects should be conducted.
decided to treat them to improve aesthetics or
decrease tooth hypersensitivity, the best way to
Complications
surgically treat single gingival recessions without
loss of interproximal tissues is achieved using the 1. Which is the surgical technique for the treatment
CAF procedure associated with CTG. of single gingival recessions with less adverse
reactions (discomfort, postoperative pain, hae-
matoma etc.)?
Efficacy
2. Answer: The Coronally Advanced Flap (CAF) pro-
1. Which is the most effective surgical technique cedure produces less postoperative discomfort
for treating single gingival recessions in terms of than the Coronally Advanced Flap plus Connec-
complete root coverage and recession reduction? tive Tissue Graft (CAF+CTG) method, Coronally
Answer: Coronally Advanced Flap plus Con- Advanced Flap plus resorbable and non-resorba-
nective Tissue Graft (CAF+CTG) and Coronally ble Barrier Membrane (CAF+BM) and Coronally
Advanced Flap plus Enamel Matrix Derivative Advanced Flap plus Acellular Dermal Matrix
(CAF+EMD) showed greater Complete Root (CAF+ADM) (evidence level: 1+; grade of the
Coverage (CRC) than Coronally Advanced recommendation: A). Coronally Advanced Flap
Flap (CAF) alone (evidence level: 1+; grade of plus Connective Tissue Graft (CAF+CTG) caused
the recommendation: A). Coronally Advanced greater postoperative discomfort than Coronally
Flap (CAF) showed greater CRC than Semilu- Advanced Flap plus Enamel Matrix Derivative
nar Technique (ST) (evidence level: 1+; grade (CAF+EMD), Semilunar Technique (ST) and Lat-
of the recommendation: A). In addition, Coro- erally Positioned Flap (LPF) (evidence level: 1+;
nally Advanced Flap plus Connective Tissue grade of the recommendation: A). Further stud-
Graft (CAF+CTG) showed greater CRC and/or ies on these aspects should be conducted.
Recession Reduction (RecRed) than Coronally
Advanced Flap (CAF), Coronally Advanced Flap
Patient opinions
plus resorbable and non-resorbable Barrier Mem-
brane (CAF+BM), Coronally Advanced Flap plus Which is the most effective surgical technique for the
Xenogenic Collagen Matrix (CAF+CM), Semilu- treatment of single gingival recessions in terms of:
Eur J Oral Implantol 2014;7(1):9–43
28 Pini-Prato et al Guidelines for single gingival recessions
(a) Absence of dental hypersensitivity considered in light of this aspect when clinicians or
• Answer: Coronally Advanced Flap plus Connec- patients have to make the treatment decision.
tive Tissue Graft (CAF+CTG) showed less sensitiv- In addition, it seems important to apply these
ity than Laterally Positioned Flap (LPF)(evidence guidelines as a strategy targeting specific groups
level: 1+; grade of the recommendation: A). In of patients attended by dental professionals, in pri-
cases of cervical abrasion and presence of dental vate practices, public and university dental clinics
sensitivity Coronally Advanced Flap plus Connec- (e.g. universities, National Health Systems) to verify
tive Tissue Graft plus Resin Composite Restoration user satisfaction (health professionals and patients),
(CAF+CTG+R) caused less sensitivity than Coro- as well as to permit monitoring of the success of
nally Advanced Flap plus Connective Tissue Graft improvements associated with the implementation
(CAF+CTG) after 6-month follow-up (evidence of the guidelines. Consequently, these guide-
level: 1+; grade of the recommendation: A). Fur- lines will be updated at least every 3 years or when
ther studies on these aspects should be conducted. requested.
(b) Aesthetic satisfaction
• Answer: There is little information about aesthetic
Implication for practice
satisfaction. Recessions treated with Coronally
Advanced Flap (CAF) or Coronally Advanced Considering the main question for which the present
Flap plus Connective Tissue Graft (CAF+CTG) guidelines should give an answer (“Which is the best
may have led to more aesthetic satisfaction than way to treat a gingival recession?), the following
Semilunar Technique (ST) (evidence level: 1+; statements and answers have been produced.
grade of the recommendation: A). Further stud- The greater effectiveness in the treatment of
ies on these aspects should be conducted. single gingival recessions without loss of interproxi-
mal tissues is achieved using the Coronally Advanced
Flap (CAF) procedure associated with Connective
Conclusions Tissue Graft (CTG). In some cases, the use of amelo-
genines showed a significant positive result, but its
Since the present clinical guidelines have been adjunctive financial cost should be considered when
focused on the treatment of single gingival reces- planning treatment. Considering postoperative dis-
sions, it has been assumed that the main indications comfort, the Coronally Advanced Flap (CAF) pro-
for their treatment remain the ones reported in the cedure is the less painful surgical approach.
literature and represented by aesthetic demands and As to postoperative dental hypersensitivity,
dental hypersensitivity17. most of the various suggested surgical approaches
Based on the outcomes of this comprehensive do not show any significant difference. The quality
project, it may be expected that general dentists, of post-surgical aesthetic appearance has not been
dental hygienists, general medical practitioners, thoroughly investigated; the few available results
dental specialists (i.e. specialists in periodontology, indicate a higher level of aesthetic satisfaction after
prosthetics, orthodontics, and restorative dentistry), the Coronally Advanced Flap (CAF) technique,
patients, and members of the business community either alone or with Connective Tissue Graft (CTG).
will benefit from these guidelines. Commonly, root
coverage-based procedures are indicated to resolve/
reduce root hypersensitivity and to restore an attrac- Acknowledgements
tive smile. These clinical guidelines may lead to
improvements in the level of patient care, as well as The authors wish to thank Massimiliano Mori, Gloria
the recognition on the part of insurance companies Iachetti, Francesco Cairo, Luisa Guidi, Jana Mervelt,
of the importance of treating gingival recessions. Sandro Cincinelli, Elisabetta Capanni, Nada Mag-
However, it is important to underline that the pre- nani, Leonardo Corcos, Giuseppe Giannecchini, and
sent recommendations are mostly based on short-term Daniele Saletta for their support with preparing these
(less than 1 year) data and, therefore, they should be guidelines.
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 29
References 22. Rajapakse PS, McCracken GI, Gwynnett E, Steen ND, Guentsch
A, Heasman PA. Does tooth brushing influence the develop-
1. Graham R, Mancher M, Wolman DM, Greenfield S, ment and progression of non-inflammatory gingival recession?
Steinberg E (eds). Clinical practice guidelines we can A systematic review. J Clin Periodontol 2007;34:1046–1061.
trust. Washington (DC): National Academies Press, 2011. 23. Solnit A, Stambaugh RV. Treatment of gingival clefts by occlus-
2p. Also available: http://www.iom.edu/Reports/2011/ al therapy. Int J Periodontics Restorative Dent 1983;3:38–55.
Clinical-Practice-Guidelines-We-Can-Trust/Standards.aspx. 24. Harrel SK, Nunn ME. The effect of occlusal discrepancies on
2. Eden J, Levit L, Berg A, Morton S (eds). Finding what works gingival width. J Periodontol 2004;75:98–105.
in health care: standards for systematic reviews. Washing- 25. Montén U, Wennström JL, Ramberg P. Periodontal condi-
ton (DC): National Academies Press; 2011. Also available: tions in male adolescents using smokeless tobacco (moist
http://www.iom.edu/Reports/2011/Finding-What-Works- snuff). J Clin Periodontol 2006;33:863–868.
in-Health-Care-Standards-for-Systematic-Reviews.aspx. 26. Wennström JL, Lindhe J, Sinclair F, Thilander B. Some peri-
3. Agency for Healthcare Research and Quality (AHRQ), US odontal tissue reactions to orthodontic tooth movement in
Department of Health and Human Services. http://guideline. monkeys. J Clin Periodontol 1987;14:121–129.
gov/about/inclusion-criteria.aspx. Accessed on 11 June, 2013. 27. Sardella A, Pedrinazzi M, Bez C, Lodi G, Carrassi A. Labial
4. American Academy of Periodontology. Glossary of Peri- piercing resulting in gingival recession. A case series. J Clin
odontal Terms. Chicago: The American Academy of Peri- Periodontol 2002;29:961–963.
odontology, 2001:44. 28. Campbell A, Moore A, Williams E, Stephens J, Tatakis DN.
5. Löe H, Anerud A, Boysen H. The natural history of peri- Tongue piercing: impact of time and barbell stem length on
odontal disease in man: prevalence, severity, and extent of lingual gingival recession and tooth chipping. J Periodontol
gingival recession. J Periodontol 1992;63:489–495. 2002;73:289–297.
6. Serino G, Wennström JL, Lindhe J, Eneroth L. The prevalence 29. Kapferer I, Benesch T, Gregoric N, Ulm C, Hienz SA. Lip
and distribution of gingival recession in subjects with a high piercing: prevalence of associated gingival recession and
standard of oral hygiene. J Clin Periodontol 1994;21:57–63. contributing factors. A cross-sectional study. J Periodontal
7. Yoneyama T, Okamoto H, Lindhe J, Socransky SS, Haffajee Res 2007;42:177–183.
AD. Probing depth, attachment loss and gingival recession. 30. Vilchez-Perez MA, Fuster-Torres MA, Figueiredo R, Val-
Findings from a clinical examination in Ushiku, Japan. J Clin maseda-Castellón E, Gay-Escoda C. Periodontal health
Periodontol 1988;15:581–591. and lateral lower lip piercings: a split-mouth cross-sectional
8. Baelum V, Fejerskov O, Karring T. Oral hygiene, gingivitis study. J Clin Periodontol 2009;36:558–563.
and periodontal breakdown in adult Tanzanians. J Peri- 31. Reynolds MA. Gingival recession is likely associated with
odontal Res 1986;21:221–232. tongue piercings. J Evid Based Dent Pract 2012;12:145–146.
9. Kassab MM, Cohen RE. The etiology and prevalence of 32. Quart AM, Small CB, Klein RS. The cocaine connection: users
gingival recession. J Am Dent Assoc 2003;134:220–225. imperil their gingiva. J Am Dent Assoc 1991;122:85–87.
10. Dowsett SA, Eckert GJ, Kowolik MJ. Comparison of perio- 33. Kapila YL, Kashani H. Cocaine-associated rapid gingival
dontal disease status of adults in two untreated indigenous recession and dental erosion. A case report. J Periodontol
populations of Guatemala, Central America. J Clin Peri- 1997;68:485–488.
odontol 2002;29:784–787. 34. Sullivan HC, Atkins JH. Free autogenous gingival grafts. III.
11. Ronderos M, Pihlstrom BL, Hodges JS. Periodontal disease Utilization of grafts in the treatment of gingival recession.
among indigenous people in the Amazon rain forest. J Clin Periodontics 1968;6:152–160.
Periodontol 2001;28:995–1003. 35. Mlinek A, Smukler H, Buchner A. The use of free gingival
grafts for the coverage of denuded roots. J Periodontol
12. Toker H, Ozdemir H. Gingival recession: epidemiology and 1973;44:248–254.
risk indicators in a university dental hospital in Turkey. Int J 36. Miller PD Jr. A classification of marginal tissue recession. Int
Dent Hyg 2009;7:115–120. J Periodontics Restorative Dent 1985;5:8–13.
13. Susin C, Haas AN, Oppermann RV, Haugejorden O, 37. Smith RG. Gingival recession. Reappraisal of an enigmatic
Albandar JM. Gingival recession: epidemiology and risk condition and a new index for monitoring. J Clin Periodon-
indicators in a representative urban Brazilian population. tol 1997;24:201–205.
J Periodontol 2004;75:1377–1386. 38. Mahajan A. Mahajan’s modification of Miller’s classification
14. Bernimouiln JP, Curilivic Z. Gingival recession and tooth for gingival recession. Dent Hypotheses 2010;145–150.
mobility. J Clin Periodontol 1977;4:208–219. 39. Cairo F, Nieri M, Cincinelli S, Mervelt J, Pagliaro U. The inter-
15. Lost C. Depth of alveolar bone dehiscence in relation to proximal clinical attachment level to classify gingival reces-
gingival recessions. J Clin Periodontol 1984;11:583–589 sions and predict root coverage outcomes: an explorative
16. Tugnait A, Clerehugh V. Gingival recession-its significance and reliability study. J Clin Periodontol 2011;38:661–666.
and management. J Dent 2001;29:381–394. 40. Pini Prato G, Franceschi D, Cairo F, Nieri M, Rotundo R.
17. Wennström JL. Mucogingival therapy. Ann Periodontol Classification of dental surface defects in areas of gingival
1996;1:671–701. recession. J Periodontol 2010;81:885–890.
18. Trott JR, Love B. An analysis of localized recessions in 41. Rotundo R, Mori M, Bonaccini D, Baldi C. Intra- and inter-
766 Winnipeg high school students. Dent Pract Dent Rec rater agreement of a new classification system of gingival
1966;16:209–213. recession defects. Eur J Oral Implantol 2011;4:127–133.
19. Källestål C, Uhlin S. Buccal attachment loss in Swedish ado- 42. Chambrone L, Sukekava F, Araújo MG, Pustiglioni FE,
lescents. J Clin Periodontol 1992;19:485–491. Chambrone LA, Lima LA. Root coverage procedures for
20. Daprile G, Gatto MR, Checchi L. The evolution of buccal the treatment of localised recession-type defects. Cochrane
gingival recessions in a student population: a 5-year follow- Database Syst Rev 2009;15:CD007161.
up. J Periodontol 2007;78:611–614. 43. Chambrone L, Sukekava F, Araújo MG, Pustiglioni FE,
21. McCracken GI, Heasman L, Stacey F, Swan M, Steen N, de Chambrone LA, Lima LA. Root-coverage procedures for the
Jager M, Heasman PA. The impact of powered and manual treatment of localized recession-type defects: a Cochrane
toothbrushing on incipient gingival recession. J Clin Peri- systematic review. J Periodontol 2010;81:452–478.
odontol 2009;36:950–957.
Eur J Oral Implantol 2014;7(1):9–43
30 Pini-Prato et al Guidelines for single gingival recessions
44. Buti J, Baccini M, Nieri M, La Marca M, Pini-Prato GP. Bayes- 61. Scottish Intercollegiate Guidelines Network (SIGN). A
ian network meta-analysis of root coverage procedures: guideline developers’ handbook. Available at http://www.
ranking efficacy and identification of best treatment. J Clin sign.ac.uk. Accessed February 5, 2007.
Periodontol 2013;40:372–386. 62. Oates TW, Robinson M, Gunsolley JC. Surgical therapies
45. Chambrone L, Pannuti CM, Tu YK, Chambrone LA. for the treatment of gingival recession. A systematic review.
Evidence-based periodontal plastic surgery. II. An individual Ann Periodontol 2003;8:303–320.
data meta-analysis for evaluating factors in achieving com- 63. Gapski R, Parks CA, Wang HL. Acellular dermal matrix
plete root coverage. J Periodontol 2012;83:477–490. for mucogingival surgery: a meta-analysis. J Periodontol
46. Pagliaro U, Nieri M, Franceschi D, Clauser C, Pini Prato 2005;76:1814–1822.
G. Evidence-based mucogingival therapy. Part 1: A critical 64. Cairo F, Pagliaro U, Nieri M. Treatment of gingival reces-
review of the literature on root coverage procedures. J Peri- sion with coronally advanced flap procedures: a systematic
odontol 2003;74:709–740. review. J Clin Periodontol 2008;35:136–162.
47. Chambrone L, Lima LA, Pustiglioni FE, Chambrone LA. 65. Chambrone L, Chambrone D, Pustiglioni FE, Chambrone LA,
Systematic review of periodontal plastic surgery in the Lima LA. Can subepithelial connective tissue grafts be
treatment of multiple recession-type defects. J Can Dent considered the gold standard procedure in the treatment
Assoc 2009;75:203a–203f. of Miller Class I and II recession-type defects? J Dent
48. Cortellini P, Pini Prato G. Coronally advanced flap and com- 2008;36:659–671.
bination therapy for root coverage. Clinical strategies based 66. Greenwell H, Bissada NF, Henderson RD, Dodge JR. The
on scientific evidence and clinical experience. Periodontol deceptive nature of root coverage results. J Periodontol
2000 2012;59:158–184. 2000;71:1327–1337.
49. Pini-Prato G, Franceschi D, Rotundo R, Cairo F, Cortellini P, 67. Bunyaratavej P, Wang HL. Collagen membranes: a review. J
Nieri M. Long-term 8-year outcomes of coronally advanced Periodontol 2001;72:215–229.
flap for root coverage. J Periodontol 2012;83:590–594. 68. Novaes AB Jr, de Barros RR. Acellular dermal matrix allo-
50. Bartlett DW, Shah P. A critical review of non-carious cervi- graft. The results of controlled randomized clinical studies.
cal (wear) lesions and the role of abfraction, erosion, and J Int Acad Periodontol 2008;10:123–129.
abrasion. J Dent Res 2006;85:306–312. 69. Roccuzzo M, Bunino M, Needleman I, Sanz M. Periodontal
51. Santamaria MP, Suaid FF, Casati MZ, Nociti FH, Sallum AW, plastic surgery for treatment of localized gingival recessions:
Sallum EA. Coronally positioned flap plus resin-modified glass a systematic review. J Clin Periodontol 2002;29:178–194.
ionomer restoration for the treatment of gingival recession 70. Clauser C, Nieri M, Franceschi D, Pagliaro U, Pini-Prato G.
associated with non-carious cervical lesions: a randomized Evidence-based mucogingival therapy. Part 2: Ordinary and
controlled clinical trial. J Periodontol 2008;79:621–628. individual patient data meta-analyses of surgical treatment
52. Santamaria MP, da Silva Feitosa D, Nociti FH Jr, Casati MZ, of recession using complete root coverage as the outcome
Sallum AW, Sallum EA. Cervical restoration and the amount variable. J Periodontol 2003;74:741–756.
of soft tissue coverage achieved by coronally advanced 71. Al-Hamdan K, Eber R, Sarment D, Kowalski C, Wang HL.
flap: a 2-year follow-up randomized-controlled clinical trial. Guided tissue regeneration-based root coverage: meta-
J Clin Periodontol 2009;36:434–441. analysis. J Periodontol 2003;74:1520–1533.
53. Santamaria MP, Ambrosano GM, Casati MZ, Nociti 72. Hwang D, Wang HL. Flap thickness as a predictor of root
Júnior FH, Sallum AW, Sallum EA. Connective tissue graft coverage: a systematic review. J Periodontol 2006;77:
plus resin-modified glass ionomer restoration for the treat- 1625–1634.
ment of gingival recession associated with non-carious 73. Cheng YF, Chen JW, Lin SJ, Lu HK. Is coronally positioned
cervical lesion: a randomized-controlled clinical trial. J Clin flap procedure adjunct with enamel matrix derivative or root
Periodontol 2009;36:791–798. conditioning a relevant predictor for achieving root cover-
54. Nieri M, Pini Prato GP, Giani M, Magnani N, Pagliaro U, Rob- age? A systemic review. J Periodontal Res 2007;42:474–485.
erto R. Patient perceptions of buccal gingival recessions and 74. Ko HY, Lu HK. Systemic review of the clinical performance
requests for treatment. J Clin Periodontol 2013;40:707–712. of connective tissue graft and guided tissue regeneration in
55. Cortellini P, Tonetti M, Baldi C, Francetti L, Rasperini G, the treatment of Miller’s classification grade I and II reces-
Rotundo R, Nieri M, Franceschi D, Labriola A, Pini Prato GP. sions. J Exp Clin Med 2010;2:63–71.
Does placement of a connective tissue graft improve the 75. Hofmänner P, Alessandri R, Laugisch O, Aroca S, Salvi
outcomes of coronally advanced flap for coverage of single GE, Stavropoulos A, Sculean A. Predictability of surgical
gingival recessions in upper anterior teeth? A multi-centre, techniques used for coverage of multiple adjacent gin-
randomized, double-blind, clinical trial. J Clin Periodontol gival recessions – A systematic review. Quintessence Int
2009;36:68–79. 2012;43:545–554.
56. Zucchelli G, Mele M, Stefanini M, Mazzotti C, Marza- 76. Fu JH, Su CY, Wang HL. Esthetic soft tissue manage-
dori M, Montebugnoli L, De Sanctis M. Patient morbidity ment for teeth and implants. J Evid Based Dent Pract
and root coverage outcome after subepithelial connec- 2012;12:129–142.
tive tissue and de-epithelialized grafts: a comparative 77. Jahnke PV, Sandifer JB, Gher ME, Gray JL, Richardson AC.
randomized-controlled clinical trial. J Clin Periodontol Thick free gingival and connective tissue autografts for root
2010;37:728–738. coverage. J Periodontol 1993;64:315–322.
57. Cizza, N., Migues, D. Progressive root resorption associated 78. Paolantonio M, di Murro C, Cattabriga A, Cattabriga M.
with the treatment of deep gingival recession. A clinical Subpedicle connective tissue graft versus free gingival graft
case. Int J Periodontics Restorative Dent 2010;30:619–625. in the coverage of exposed root surfaces. A 5-year clinical
58. Rotundo R, Nieri M, Mori M, Clauser C, Pini Prato GP. study. J Clin Periodontol 1997;24:51–56.
Aesthetic perception after root coverage procedure. J Clin 79. Bittencourt S, Del Peloso Ribeiro E, Sallum EA, Sallum AW,
Periodontol 2008;35:705–712. Nociti FH Jr, Casati MZ. Comparative 6-month clinical study
59. Appraisal of Guidelines for Research and Evaluation of a semilunar coronally positioned flap and subepithelial
(AGREE). May 2009. http://www.agreetrust.org connective tissue graft for the treatment of gingival reces-
60. Glossary of evidence-based terms. J Evid Based Dent Pract sion. J Periodontol 2006;77:174–181.
2007;7:45–49.
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 31
80. Bittencourt S, Ribeiro Edel P, Sallum EA, Sallum AW, 96. Cairo F, Cortellini P, Tonetti M, Nieri M, Mervelt J, Cinci-
Nociti FH, Casati MZ. Semilunar coronally positioned flap nelli S, Pini-Prato G. Coronally advanced flap with and
or subepithelial connective tissue graft for the treatment without connective tissue graft for the treatment of single
of gingival recession: a 30-month follow-up study. J Peri- maxillary gingival recession with loss of inter-dental attach-
odontol 2009;80:1076–1082. ment. A randomized controlled clinical trial. J Clin Periodon-
81. Mahajan A, Dixit J, Verma UP. A patient-centered clinical tol 2012;39:760–768.
evaluation of acellular dermal matrix graft in the treatment of 97. Borghetti A, Louise F. Controlled clinical evaluation of the
gingival recession defects. J Periodontol 2007;78:2348–2355. subpedicle connective tissue graft for the coverage of gin-
82. Haghighati F, Mousavi M, Moslemi N, Kebria MM, gival recession. J Periodontol 1994;65:1107–1112.
Golestan B. A comparative study of two root-coverage 98. Wei PC, Laurell L, Geivelis M, Lingen MW, Maddalozzo D.
techniques with regard to interdental papilla dimension Acellular dermal matrix allografts to achieve increased
as a prognostic factor. Int J Periodontics Restorative Dent attached gingiva. Part 1. A clinical study. J Periodontol
2009;29:179–189. 2000;71:1297–1305.
83. Santana RB, Mattos CM, Dibart S. A clinical comparison of 99. Maurer S, Hayes C, Leone C. Width of keratinized tissue
two flap designs for coronal advancement of the gingival after gingivoplasty of healed subepithelial connective tissue
margin: semilunar versus coronally advanced flap. J Clin grafts. J Periodontol 2000;71:1729–1736.
Periodontol 2010;37:651–658. 100. Harris RJ. Clinical evaluation of 3 techniques to augment
84. Santana RB, Furtado MB, Mattos CM, de Mello Fonseca E, keratinized tissue without root coverage. J Periodontol
Dibart S. Clinical evaluation of single-stage advanced ver- 2001;72:932–938.
sus rotated flaps in the treatment of gingival recessions. J 101. McGuire MK, Nunn ME. Evaluation of the safety and
Periodontol 2010;81:485–492. efficacy of periodontal applications of a living tissue-
85. Moslemi N, Mousavi Jazi M, Haghighati F, Morovati SP, engineered human fibroblast-derived dermal substitute. I.
Jamali R. Acellular dermal matrix allograft versus subepi- Comparison to the gingival autograft: a randomized con-
thelial connective tissue graft in treatment of gingival reces- trolled pilot study. J Periodontol 2005;76:867–880.
sions: a 5-year randomized clinical study. J Clin Periodontol 102. Bertoldi C, Bencivenni D, Lucchi A, Consolo U. Augmenta-
2011;38:1122–1129. tion of keratinized gingiva through bilaminar connective tis-
86. Nazareth CA, Cury PR. Use of anorganic bovine-derived sue grafts: a comparison between two techniques. Minerva
hydroxyapatite matrix/cell-binding peptide (P-15) in the Stomatol 2007;56:3–20.
treatment isolated Class I gingival recession of defects: a 103. McGuire MK, Scheyer ET, Schupbach P. Growth factor-
pilot study. J Periodontol 2010;82:700–707. mediated treatment of recession defects: a randomized
87. McGuire MK, Scheyer ET, Nunn M. Evaluation of human controlled trial and histologic and microcomputed tomog-
recession defects treated with coronally advanced flaps and raphy examination. J Periodontol 2009;80:550–564.
either enamel matrix derivative or connective tissue: Com- 104. Sanz M, Lorenzo R, Aranda JJ, Martin C, Orsini M. Clinical
parison of clinical parameters at ten years. J Periodontol evaluation of a new collagen matrix (Mucograft prototype)
2012;83:1353–1362. to enhance the width of keratinized tissue in patients with
88. Zucchelli G, Marzadori M, Mele M, Stefanini M, Mon- fixed prosthetic restorations: a randomized prospective clin-
tebugnoli L. Root coverage in molar teeth: a compara- ical trial. J Clin Periodontol 2009;36:868–876.
tive controlled randomized clinical trial. J Clin Periodontol 105. Dilsiz A, Aydin T, Canakci V, Cicek Y. Root surface biomodi-
2012;39:1082–1088. fication with Nd:YAG laser for the treatment of gingival
89. Jepsen K, Jepsen S, Zucchelli G, Stefanini M, de Sanctis M, recession with subepithelial connective tissue grafts. Pho-
Baldini N, Greven B, Heinz B, Wennström J, Cassel B, Vigno- tomed Laser Surg 2010a;28:337–343.
letti F, Sanz M. Treatment of gingival recession defects with 106. Dilsiz A, Aydin T, Yavuz MS. Root surface biomodification
a coronally advanced flap and a xenogeneic collagen matrix: with an Er:YAG laser for the treatment of gingival recession
a multicenter randomized clinical trial. J Clin Periodontol with subepithelial connective tissue grafts. Photomed Laser
2013;40:82–89. Surg 2010;28:511–517.
90. Guinard EA, Caffesse RG. Treatment of localized gingival 107. Nevins M, Nevins ML, Camelo M, Camelo JM, Schup-
recessions. Part III. Comparison of results obtained with bach P, Kim DM. The clinical efficacy of DynaMatrix extra-
lateral sliding and coronally repositioned flaps. J Periodontol cellular membrane in augmenting keratinized tissue. Int J
1978;49:457–461. Periodontics Restorative Dent 2010;30:151–161.
91. Caffesse RG, Guinard EA. Treatment of localized gingival 108. McGuire MK, Scheyer ET, Nevins ML, Neiva R, Cochran DL,
recessions. Part II. Coronally repositioned flap with a free Mellonig JT, Giannobile WV, Bates D. Living cellular
gingival graft. J Periodontol 1978;49:357–361. construct for increasing the width of keratinized gingiva:
92. Caffesse RG, Guinard EA. Treatment of localized gingival results from a randomized, within-patient, controlled trial.
recessions. Part IV. Results after three years. J Periodontol J Periodontol 2011;82:1414–1423.
1980;51:167–170. 109. Nevins M, Nevins ML, Kim SW, Schupbach P, Kim DM.
93. Espinel MC, Caffesse RG. Comparison of the results obtained The use of mucograft collagen matrix to augment the zone
with the laterally positioned pedicle sliding flap-revised tech- of keratinized tissue around teeth: a pilot study. Int J Peri-
nique and the lateral sliding flap with a free gingival graft odontics Restorative Dent 2011;31:367–373.
technique in the treatment of localized gingival recessions. 110. Ibbott CG, Oles RD, Laverty WH. Effects of citric acid
Int J Periodontics Restorative Dent 1981;1:30–37. treatment on autogenous free graft coverage of localized
94. Cueva MA, Boltchi FE, Hallmon WW, Nunn ME, Rive- recession. J Periodontol 1985;56:662–665.
ra-Hidalgo F, Rees T. A comparative study of coronally 111. Oles RD, Ibbott CG, Laverty WH. Effects of citric acid
advanced flaps with and without the addition of enamel treatment on pedicle flap coverage of localized recession.
matrix derivative in the treatment of marginal tissue reces- J Periodontol 1985;56:259–261.
sion. J Periodontol 2004;75:949–956. 112. Caffesse RG, Alspach SR, Morrison EC, Burgett FG. Lateral
95. Henriques PS, Pelegrine AA, Nogueira AA, Borghi MM. sliding flaps with and without citric acid. Int J Periodontics
Application of subepithelial connective tissue graft with or Restorative Dent 1987;7:42–57.
without enamel matrix derivative for root coverage: a split-
mouth randomized study. J Oral Sci 2010;52:463–471.
Eur J Oral Implantol 2014;7(1):9–43
32 Pini-Prato et al Guidelines for single gingival recessions
113. Bouchard P, Etienne D, Ouhayoun JP, Nilvéus R. Subepi- 130. Kassab MM, Cohen RE, Andreana S, Dentino AR. The
thelial connective tissue grafts in the treatment of gingival effect of EDTA in attachment gain and root coverage.
recessions. A comparative study of 2 procedures. J Peri- Compend Contin Educ Dent 2006;27:353–360.
odontol 1994;65:929–936. 131. Al-Zahrani MS, Bissada NF, Ficara AJ, Cole B. Effect of
114. Trombelli L, Schincaglia GP, Zangari F, Griselli A, Scabbia A, connective tissue graft orientation on root coverage and
Calura G. Effects of tetracycline HCl conditioning and gingival augmentation. Int J Periodontics Restorative Dent
fibrin-fibronectin system application in the treatment of 2004;24:65–69.
buccal gingival recession with guided tissue regeneration. 132. Barros RR, Novaes AB Jr, Paliotto DB, Souza SL, Taba M Jr,
J Periodontol 1995;66:313–320. Grisi MF. A 36-month randomised controlled prospective
115. Roccuzzo M, Lungo M, Corrente G, Gandolfo S. Compara- clinical study of a conventional and a new surgical approach
tive study of a bioresorbable and a non-resorbable mem- for root coverage with acellular dermal matrix graft. Perio
brane in the treatment of human buccal gingival recessions. 2007;4:55–61.
J Periodontol 1996;67:7–14. 133. Bittencourt S, Del Peloso Ribeiro E, Sallum EA, Sallum AW,
116. Trombelli L, Scabbia A, Wikesjö UM, Calura G. Fibrin glue Nociti FH Jr, Casati MZ. Root surface biomodification
application in conjunction with tetracycline root condition- with EDTA for the treatment of gingival recession with
ing and coronally positioned flap procedure in the treat- a semilunar coronally repositioned flap. J Periodontol
ment of human gingival recession defects. J Clin Periodon- 2007;78:1695–1701.
tol 1996;23:861–867. 134. Felipe ME, Andrade PF, Grisi MF, Souza SL, Taba M Jr,
117. Bouchard P, Nilveus R, Etienne D. Clinical evaluation of tet- Palioto DB, Novaes AB Jr. Comparison of two surgical pro-
racycline HCl conditioning in the treatment of gingival reces- cedures for use of the acellular dermal matrix graft in the
sions. A comparative study. J Periodontol 1997;68:262–269. treatment of gingival recessions: a randomized controlled
118. Matarasso S, Cafiero C, Coraggio F, Vaia E, de Paoli S. clinical study. J Periodontol 2007;78:1209–1217.
Guided tissue regeneration versus coronally repositioned 135. Lucchesi JA, Santos VR, Amaral CM, Peruzzo DC,
flap in the treatment of recession with double papillae. Int Duarte PM. Coronally positioned flap for treatment of
J Periodontics Restorative Dent 1998;18:444–453. restored root surfaces: a 6-month clinical evaluation. J Peri-
119. Pini-Prato G, Baldi C, Pagliaro U, Nieri M, Saletta D, odontol 2007;78:615–623.
Rotundo R, Cortellini P. Coronally advanced flap procedure 136. Andrade PF, Felipe ME, Novaes AB Jr, Souza SL, Taba M
for root coverage. Treatment of root surface: root planning Jr, Palioto DB, Grisi MF. Comparison between two surgi-
versus polishing. J Periodontol 1999;70:1064–1076. cal techniques for root coverage with an acellular dermal
120. Caffesse RG, De LaRosa M, Garza M, Munne-Travers A, matrix graft. J Clin Periodontol 2008;35:263–269.
Mondragon JC, Weltman R. Citric acid demineralization 137. Byun HY, Oh TJ, Abuhussein HM, Yamashita J, Soehren SE,
and subepithelial connective tissue grafts. J Periodontol Wang HL. Significance of the epithelial collar on the subepi-
2000;71:568–572. thelial connective tissue graft. J Periodontol 2009;80:924–932.
121. Pini Prato G, Pagliaro U, Baldi C, Nieri M, Saletta D, 138. Zucchelli G, Mele M, Mazzotti C, Marzadori M, Monte-
Cairo F, Cortellini P. Coronally advanced flap procedure for bugnoli L, De Sanctis M. Coronally advanced flap with
root coverage. Flap with tension versus flap without ten- and without vertical releasing incisions for the treatment
sion: a randomized controlled clinical study. J Periodontol of multiple gingival recessions: a comparative controlled
2000;71:188–201. randomized clinical trial. J Periodontol 2009;80:1083–1094.
122. Henderson RD, Greenwell H, Drisko C, Regennitter FJ, 139. Zucchelli G, Mounssif I, Stefanini M, Mele M, Montebugnoli
Lamb JW, Mehlbauer MJ, Goldsmith LJ, Rebitski G. Predict- L, Sforza NM. Hand and ultrasonic instrumentation in combi-
able multiple site root coverage using an acellular dermal nation with root-coverage surgery: a comparative controlled
matrix allograft. J Periodontol 2001;72:571–582. randomized clinical trial. J Periodontol 2009;80:577–585.
123. Del Pizzo M, Modica F, Bethaz N, Priotto P, Romagnoli R. 140. Andrade PF, Grisi MF, Marcaccini AM, Fernandes PG,
The connective tissue graft: a comparative clinical evalua- Reino DM, Souza SL, Taba M, Palioto DB, Novaes AB.
tion of wound healing at the palatal donor site. A prelimi- Comparison between micro- and macrosurgical techniques
nary study. J Clin Periodontol 2002;29:848–854. for the treatment of localized gingival recessions using
124. Zucchelli G, Amore C, Sforza NM, Montebugnoli L, De coronally positioned flaps and enamel matrix derivative. J
Sanctis M. Bilaminar techniques for the treatment of Periodontol 2010;81:1572–1579.
recession-type defects. A comparative clinical study. J Clin 141. Barker TS, Cueva MA, Rivera-Hidalgo F, Beach MM, Ross-
Periodontol 2003;30:862–870. mann JA, Kerns DG, Crump TB, Shulman JD. A comparative
125. Barros RR, Novaes AB, Grisi MF, Souza SL, Taba MJ, Pali- study of root coverage using two different acellular dermal
oto DB. A 6-month comparative clinical study of a conven- matrix products. J Periodontol 2010;81:1596–1603.
tional and a new surgical approach for root coverage with 142. Zucchelli G, Mele M, Stefanini M, Mazzotti C, Marza-
acellular dermal matrix. J Periodontol 2004;75:1350–1356. dori M, Montebugnoli L, de Sanctis M. Patient morbidity
126. Barros RR, Novaes AB Jr, Grisi MF, Souza SL, Taba M Jr, and root coverage outcome after subepithelial connec-
Palioto DB. New surgical approach for root coverage of tive tissue and de-epithelialized grafts: a comparative
localized gingival recession with acellular dermal matrix: a randomized-controlled clinical trial. J Clin Periodontol
12-month comparative clinical study. J Esthet Restor Dent 2010;37:728–738.
2005;17:156–164. 143. Mazzocco F, Comuzzi L, Stefani R, Milan Y, Favero G,
127. Burkhardt R, Lang NP. Coverage of localized gingival reces- Stellini E. Coronally advanced flap combined with a subepi-
sions: comparison of micro- and macrosurgical techniques. thelial connective tissue graft using full- or partial-thickness
J Clin Periodontol 2005;32:287–293. flap reflection. J Periodontol 2011;82:1524–1529.
128. Francetti L, Del Fabbro M, Calace S, Testori T, Wein- 144. Ozturan S, Durukan SA, Ozcelik O, Seydaoglu G, Hay-
stein RL. Microsurgical treatment of gingival recession: a tac MC. Coronally advanced flap adjunct with low intensity
controlled clinical study. Int J Periodontics Restorative Dent laser therapy: a randomized controlled clinical pilot study.
2005;25:181–188. J Clin Periodontol 2011;38:1055–1062.
129. Tözüm TF, Keçeli HG, Güncü GN, Hatipoğlu H, Şengün D. 145. Pini Prato G, Rotundo R, Franceschi D, Cairo F, Cortellini P,
Treatment of gingival recession: comparison of two tech- Nieri M. Fourteen-year outcomes of coronally advanced
niques of subepithelial connective tissue graft. J Periodontol flap for root coverage: follow-up from a randomized trial.
2005;76:1842–1848. J Clin Periodontol 2011;38:715–720.
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 33
146. Mahajan A, Bharadwaj A, Mahajan P. Comparison of peri- 163. Hirsch A, Goldstein M, Goultschin J, Boyan BD, Schwartz Z.
osteal pedicle graft and subepithelial connective tissue graft A 2-year follow-up of root coverage using sub-pedicle acel-
for the treatment of gingival recession defects. Aust Dent J lular dermal matrix allografts and subepithelial connective
2012;57:51–57. tissue autografts. J Periodontol 2005;76:1323–1328.
147. Bittencourt S, Del Peloso Ribeiro E, Sallum EA, Nociti FH Jr, 164. Erley KJ, Swiec GD, Herold R, Bisch FC, Peacock ME. Gingival
Casati MZ. Surgical microscope may enhance root coverage recession treatment with connective tissue grafts in smokers
with subepithelial connective tissue graft: a randomized- and non-smokers. J Periodontol 2006;77:1148–1155.
controlled clinical trial. J Periodontol 2012;83:721–730. 165. McGuire MK, Scheyer ET. Comparison of recombinant human
148. Ayub LG, Ramos UD, Reino DM, Grisi MF, Taba M Jr, platelet-derived growth factor-BB plus beta tricalcium phos-
Souza SL, Palioto DB, Novaes AB Jr. A Randomized com- phate and a collagen membrane to subepithelial connective
parative clinical study of two surgical procedures to improve tissue grafting for the treatment of recession defects: a case
root coverage with the acellular dermal matrix graft. J Clin series. Int J Periodontics Restorative Dent 2006;26:127–133.
Periodontol 2012;39:871–878. 166. Moses O, Artzi Z, Sculean A, Tal H, Kozlovsky A, Roma-
149. Kuru B, Yildirim S. Treatment of localized gingival recessions nos GE, Nemcovsky CE. Comparative study of two root
using gingival unit grafts: a randomized controlled clinical coverage procedures: a 24-month follow-up multicenter
trial. J Periodontol 2013;84:41–50. study. J Periodontol 2006;77:195–202.
150. Pini Prato G, Tinti C, Vincenzi G, Magnani C, Cortellini P, 167. Silva CO, Sallum AW, De Lima AF, Tatakis DN. Coro-
Clauser C. Guided tissue regeneration versus mucogingival nally positioned flap for root coverage: poorer outcomes in
surgery in the treatment of human buccal gingival reces- smokers. J Periodontol 2006;77:81–87.
sion. J Periodontol 1992;63:919–928. 168. Keceli HG, Sengun D, Berberoğlu A, Karabulut E. Use of
151. Trombelli L, Schincaglia GP, Zangari F, Griselli A, Scabbia A, platelet gel with connective tissue grafts for root cover-
Calura G. Effects of tetracycline HCl conditioning and age: a randomized-controlled trial. J Clin Periodontol 2008;
fibrin-fibronectin system application in the treatment of 35:255–262.
buccal gingival recession with guided tissue regeneration. J 169. Pini-Prato G, Cairo F, Nieri M, Franceschi D, Rotundo R,
Periodontol 1995;66:313–320. Cortellini P. Coronally advanced flap versus connective tis-
152. Pini Prato G, Clauser C, Cortellini P, Tinti C, Vincenzi G, sue graft in the treatment of multiple gingival recessions: a
Pagliaro U. Guided tissue regeneration versus mucogingival split-mouth study with a 5-year follow-up. J Clin Periodon-
surgery in the treatment of human buccal recessions. A tol 2010;37:644–650.
4-year follow-up study. J Periodontol 1996;67:1216–1223. 170. Santamaria MP, Ambrosano GM, Casati MZ, Nociti FH
153. Wennström JL, Zucchelli G. Increased gingival dimensions. Jr, Sallum AW, Sallum EA. The influence of local anatomy
A significant factor for successful outcome of root coverage on the outcome of treatment of gingival recession asso-
procedures? A 2-year prospective clinical study. J Clin Peri- ciated with non-carious cervical lesions. J Periodontol
odontol 1996;23:770–777. 2010;81:1027–1034.
154. Harris RJ. A comparative study of root coverage obtained 171. Schlee M, Esposito M. Human dermis graft versus autogenous
with guided tissue regeneration utilizing a bioabsorbable connective tissue grafts for thickening soft tissue and covering
membrane versus the connective tissue with partial-thick- multiple gingival recessions: 6-month results from a preference
ness double pedicle graft. J Periodontol 1997;68:779–790. clinical trial. Eur J Oral Implantol 2011;4:119–125.
155. Ozcan G, Kurtiş B, Baloş K. Combined use of root condi- 172. Laney JB, Saunders VG, Garnick JJ. A comparison of
tioning, fibrin-fibronectin system and a collagen membrane two techniques for attaining root coverage. J Periodontol
to treat a localized gingival recession: a 10-case report. 1992;63:19–23.
J Marmara Univ Dent Fac 1997;2:588–598. 173. Lafzi A, Mostofi Zadeh Farahani R, Abolfazli N, Amid R,
156. Harris RJ. Root coverage with a connective tissue with par- Safaiyan A. Effect of connective tissue graft orientation on
tial thickness double pedicle graft and an acellular dermal the root coverage outcomes of coronally advanced flap.
matrix graft: a clinical and histological evaluation of a case Clin Oral Investig 2007;11:401–408.
report. J Periodontol 1998;69:1305–1311. 174. Han JS, John V, Blanchard SB, Kowolik MJ, Eckert GJ.
157. Müller HP, Stahl M, Eger T. Root coverage employing an Changes in gingival dimensions following connective tissue
envelope technique or guided tissue regeneration with a grafts for root coverage: comparison of two procedures. J
bioabsorbable membrane. J Periodontol 1999;70:743–751. Periodontol 2008;79:1346–1354.
158. Harris RJ. A comparative study of root coverage obtained with 175. Papageorgakopoulos G, Greenwell H, Hill M, Vidal R,
an acellular dermal matrix versus a connective tissue graft: Scheetz JP. Root coverage using acellular dermal matrix and
results of 107 recession defects in 50 consecutively treated comparing a coronally positioned tunnel to a coronally posi-
patients. Int J Periodontics Restorative Dent 2000;20:51–59. tioned flap approach. J Periodontol 2008;79:1022–1030.
159. Cordioli G, Mortarino C, Chierico A, Grusovin MG, Maj- 176. Barbosa FI, Corrêa DS, Zenóbio EG, Costa FO, Shibli JA.
zoub Z. Comparison of 2 techniques of subepithelial con- Dimensional changes between free gingival grafts fixed
nective tissue graft in the treatment of gingival recessions. with ethyl cyanoacrylate and silk sutures. J Int Acad Peri-
J Periodontol 2001;72:1470–1476. odontol 2009;11:170–176.
160. Nemcovsky CE, Artzi Z, Tal H, Kozlovsky A, Moses O. A 177. de Toledo Lourenço AH, de Toledo Lourenço E Jr, Fraga MR,
multicenter comparative study of two root coverage pro- Vitral RW. The association of a polydioxanone tent without
cedures: coronally advanced flap with addition of enamel a guided tissue regeneration membrane to a coronal sliding
matrix proteins and subpedicle connective tissue graft. J flap for root coverage. J Periodontol 2009;80:1674–1679.
Periodontol 2004;75:600–607. 178. Shepherd N, Greenwell H, Hill M, Vidal R, Scheetz JP.
161. Berlucchi I, Francetti L, Del Fabbro M, Testori T, Wein- Root coverage using acellular dermal matrix and com-
stein RL. Enamel matrix proteins (Emdogain) in combination paring a coronally positioned tunnel with and without
with coronally advanced flap or subepithelial connective tis- platelet-rich plasma: a pilot study in humans. J Periodontol
sue graft in the treatment of shallow gingival recessions. Int 2009;80:397–404.
J Periodontics Restorative Dent 2002;22:583–593. 179. Lafzi A, Chitsazi MT, Farahani RM, Faramarzi M. Compara-
162. Harris RJ, Miller LH, Harris CR, Miller RJ. A comparison of tive clinical study of coronally advanced flap with and with-
three techniques to obtain root coverage on mandibular out use of plasma rich in growth factors in the treatment of
incisors. J Periodontol 2005;76:1758–1767. gingival recession. Am J Dent 2011;24:143–147.
Eur J Oral Implantol 2014;7(1):9–43
34 Pini-Prato et al Guidelines for single gingival recessions
180. Baghele ON, Pol DG. An evaluation of the effectiveness 197. da Silva RC, Joly JC, de Lima AF, Tatakis DN. Root cov-
and predictability of transpositional flap vs connective tis- erage using the coronally positioned flap with or with-
sue graft for coverage of Miller’s class-I and class-II facial out a subepithelial connective tissue graft. J Periodontol
marginal tissue recession lesions: a clinical study. Indian J 2004;75:413–419.
Dent Res 2012;23:195–202. 198. Woodyard JG, Greenwell H, Hill M, Drisko C, Iasella JM,
181. Jepsen K, Heinz B, Halben JH, Jepsen S. Treatment of gingival Scheetz J. The clinical effect of acellular dermal matrix on
recession with titanium reinforced barrier membranes versus gingival thickness and root coverage compared to coronally
connective tissue grafts. J Periodontol 1998;69:383–391. positioned flap alone. J Periodontol 2004;75:44–56.
182. Trombelli L, Scabbia A, Tatakis DN, Calura G. Subpedicle 199. Del Pizzo M, Zucchelli G, Modica F, Villa R, Debernardi C.
connective tissue graft versus guided tissue regener- Coronally advanced flap with or without enamel matrix de-
ation with bioabsorbable membrane in the treatment of rivative for root coverage: a 2-year study. J Clin Periodontol
human gingival recession defects. J Periodontol 1998;69: 2005;32:1181–1187.
1271–1277. 200. Huang LH, Neiva RE, Soehren SE, Giannobile WV,
183. Zucchelli G, Clauser C, De Sanctis M, Calandriello M. Wang HL. The effect of platelet-rich plasma on the coro-
Mucogingival versus guided tissue regeneration procedures nally advanced flap root coverage procedure: a pilot human
in the treatment of deep recession type defects. J Periodon- trial. J Periodontol 2005;76:1768–1777.
tol 1998;69:138–145. 201. Leknes KN, Amarante ES, Price DE, Bøe OE, Skavland RJ,
184. Borghetti A, Glise JM, Monnet-Corti V, Dejou J. Compara- Lie T. Coronally positioned flap procedures with or without
tive clinical study of a bioabsorbable membrane and sub- a biodegradable membrane in the treatment of human gin-
epithelial connective tissue graft in the treatment of human gival recession. A 6-year follow-up study. J Clin Periodontol
gingival recession. J Periodontol 1999;71:123–130. 2005;32:518–529.
185. Amarante ES, Leknes KN, Skavland J, Lie T. Coronally 202. Spahr A, Haegewald S, Tsoulfidou F, Rompola E, Heijl L,
positioned flap procedures with or without a bioabsorbable Bernimoulin JP, Ring C, Sander S, Haller B. Coverage of
membrane in the treatment of human gingival recession. Miller class I and II recession defects using enamel matrix
J Periodontol 2000;71:989–998. proteins versus coronally advanced flap technique: a 2-year
186. Tatakis DN, Trombelli L. Gingival recession treatment: guided report. J Periodontol 2005;76:1871–1880.
tissue regeneration with bioabsorbable membrane versus 203. Wilson TG Jr, McGuire MK, Nunn ME. Evaluation of the safety
connective tissue graft. J Periodontol 2000;71:299–307. and efficacy of periodontal applications of a living tissue-engi-
187. Modica F, Del Pizzo M, Roccuzzo M, Romagnoli R. Coro- neered human fibroblast-derived dermal substitute. II. Compar-
nally advanced flap for the treatment of buccal gingival ison to the subepithelial connective tissue graft: a randomized
recessions with and without enamel matrix derivative. A controlled feasibility study. J Periodontol 2005;76:881–889.
split-mouth study. J Periodontol 2000;71:1693–1698. 204. Castellanos A, de la Rosa M, de la Garza M, Caffesse RG.
188. Aichelmann-Reidy ME, Yukna RA, Evans GH, Nasr HF, Enamel matrix derivative and coronal flaps to cover mar-
Mayer ET. Clinical evaluation of acellular allograft dermis ginal tissue recessions. J Periodontol 2006;77:7–14.
for the treatment of human gingival recession. J Periodon- 205. de Queiroz Côrtes AQ, Sallum AW, Casati MZ, Nociti FH Jr,
tol 2001;72;998–1105. Sallum EA. A two-year prospective study of coronally posi-
189. Romagna-Genon C. Comparativeclinicalstudy of guidedtis- tioned flap with or without acellular dermal matrix graft.
sueregeneration with a bioabsorbablebilayercollagenmem- J Clin Periodontol 2006;33:683–689.
brane and subepithelialconnectivetissuegraft. J Periodontol 206. Pilloni A, Paolantonio M, Camargo PM. Root coverage
2001;72:1258–1264. with a coronally positioned flap used in combination with
190. Wang HL, Bunyaratavej P, Labadie M, Shyr Y, MacNeil RL. enamel matrix derivative: 18-month clinical evaluation.
Comparison of 2 clinical techniques for treatment of gin- J Periodontol 2006;77:2031–2039.
gival recession. J Periodontol 2001;72:1301–1011. 207. Joly JC, Carvalho AM, da Silva RC, Ciotti DL, Cury PR. Root
191. Hägewald S, Spahr A, Rompola E, Haller B, Heijl L, Berni- coverage in isolated gingival recessions using autograft versus
moulin JP. Comparative study of Emdogain and coronally allograft: a pilot study. J Periodontol 2007;78:1017–1022.
advanced flap technique in the treatment of human gin- 208. Dodge JR, Greenwell H, Drisko C, Wittwer JW, Yancey J,
gival recessions. A prospective controlled clinical study. Rebitski G. Improved bone regeneration and root cover-
J Clin Periodontol 2002;29:35-41. age using a resorbable membrane with fisically assisted cell
192. Paolantonio M, Dolci M, Esposito P, D’Archivio D, Lisanti L, migration and DFDBA. Int J Periodontics Restorative Dent
Di Luccio A, Perinetti G. Subpedicle acellular dermal matrix 2000;20:398–411.
graft and autogenous connective tissue graft in the treat- 209. Duval BT, Maynard JG, Gunsolley JC, Waldrop TC. Treat-
ment of gingival recessions: a comparative 1-year clinical ment of human mucogingival defects utilizing a bioabsorb-
study. J Periodontol 2002;73:1299–1307. able membrane with and without a demineralised freeze-
193. Tal H, Moses O, Zohar R, Meir H, Nemcovsky C. Root cov- dried bone allograft. J Periodontol 2000;71:1687–1692.
erage of advanced gingival recession: a comparative study 210. Rosetti EP, Marcantonio RA, Rossa C Jr, Chaves ES, Gois-
between acellular dermal matrix allograft and subepithelial sis G, Marcantonio E Jr. Treatment of gingival recession:
connective tissue grafts. J Periodontol 2002;73:1405–1411. comparative study between subepithelial connective tis-
194. Lins LH, de Lima AF, Sallum AW. Root coverage: comparison sue graft and guided tissue regeneration. J Periodontol
of coronally positioned flap with and without titanium- 2000;71:1441–1447.
reinforced barrier membrane. J Periodontol 2003;74:168–174. 211. Paolantonio M. Treatment of gingival recessions by com-
195. McGuire MK, Nunn M. Evaluation of human recession defects bined periodontal regenerative technique, guided tissue
treated with coronally advanced flaps and either enamel regeneration, and subpedicle connective tissue graft. A
matrix derivative or connective tissue. Part 1: Comparison of comparative clinical study. J Periodontol 2002;73:53–62.
clinical parameters. J Periodontol 2003;74:1110–1125. 212. Kimble KM, Eber RM, Soehren S, Shyr Y, Wang HL. Treat-
196. Côrtes Ade Q, Martins AG, Nociti FH Jr, Sallum AW, Casa- ment of gingival recession using a collagen membrane with or
ti MZ, Sallum EA. Coronally positioned flap with or without without the use of demineralized freeze-dried bone allograft
acellular dermal matrix graft in the treatment of Class I for space maintenance. J Periodontol 2004;75:210–220.
gingival recessions: a randomized controlled clinical study.
J Periodontol 2004;75:1137–1144.
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 35
213. Trabulsi M, Oh TJ, Eber R, Weber D, Wang HL. Effect 227. Banihashemrad A, Aghassizadeh E, Radvar M. Treatment
of enamel matrix derivative on collagen guided tissue of gingival recessions by guided tissue regeneration and
regeneration-based root coverage procedure. J Periodontol coronally advanced flap. N Y State Dent J 2009;75:54–58.
2004;75:1446–1457. 228. Cardaropoli D, Tamagnone L, Roffredo A, Gaveglio L. Treat-
214. Cardaropoli D, Cardaropoli G. Healing of gingival reces- ment of gingival recession defects using coronally advanced
sions using a collagen membrane with a hemineralized flap with a porcine collagen matrix compared to coronally
xenograft: a randomized controlled clinical trial. Int J Peri- advanced flap with connective tissue graft: a randomized
odontics Restorative Dent 2009;29:59–67. controlled clinical trial. J Periodontol 2012;83:321–328.
215. Jankovic S, Aleksic Z, Klokkevold P, Lekovic V, Dimitrije- 229. Aimetti M, Romano F, Peccolo DC, Debernardi C. Non-
vic B, Kenney EB, Camargo P. Use of platelet-rich fibrin surgical periodontal therapy of shallow gingival recession
membrane following treatment of gingival recession: a defects: evaluation of the restorative capacity of marginal
randomized clinical trial. Int J Periodontics Restorative Dent gingiva after 12 months. J Periodontol 2005;76:256–261.
2012;32:41–50. 230. Ito C, Oshio K, Shiomi N, Murai S. A preliminary com-
216. Jhaveri HM, Chavan MS, Tomar GB, Deshmukh VL, parative study of the guided tissue regeneration and free
Wani MR, Miller PD Jr. Acellular dermal matrix seeded gingival graft procedures for adjacent facial root coverage.
with autologous gingival fibroblasts for the treatment of Quintessence Int 2000;31:319–326.
gingival recession: a proof-of-concept study. J Periodontol 231. Dembowska E, Drozdzik A. Subepithelial connective tis-
2010;81:616–625. sue graft in the treatment of multiple gingival recession.
217. Alkan EA, Parlar A. EMD or subepithelial connective tissue Oral Surg Oral Med Oral Pathol Oral Radiol Endod
graft for the treatment of single gingival recessions: a pilot 2007;104:e1–7.
study. J Periodontal Res 2011;46:637–642. 232. Shin SH, Cueva MA, Kerns DG, Hallmon WW, Rivera-
218. Rasperini G, Roccuzzo M, Francetti L, Acunzo R, Consonni Hidalgo F, Nunn ME. A comparative study of root coverage
D, Silvestri M. Subepithelial connective tissue graft for treat- using acellular dermal matrix with and without enamel
ment of gingival recessions with and without enamel matrix matrix derivative. J Periodontol 2007;78:411–421.
derivative: a multicenter, randomized controlled clinical trial. 233. de Souza SL, Novaes AB Jr, Grisi DC, Taba M Jr, Grisi MF,
Int J Periodontics Restorative Dent 2011;31:133–139. de Andrade PF. Comparative clinical study of a subepithelial
219. Alves LB, Costa PP, de Souza SLS, de Moraes Grisi MF, Pali- connective tissue graft and acellular dermal matrix graft
oto DB, Taba M Jr, Novaes AB Jr. Acellular dermal matrix for the treatment of gingival recessions: six- to 12-month
graft with or without enamel matrix derivative for root changes. J Int Acad Periodontol 2008;10:87–94.
coverage in smokers: a randomized clinical study. J Clin 234. Aroca S, Keglevich T, Barbieri B, Gera I, Etienne D. Clinical
Periodontol 2012;39:393–399. evaluation of a modified coronally advanced flap alone or
220. Jankovic S, Aleksic Z, Klokkevold P, Lekovic V, Dimitrije- in combination with a platelet-rich fibrin membrane for
vic B, Kenney EB, Camargo P. Use of platelet-rich fibrin the treatment of adjacent multiple gingival recessions: a
membrane following treatment of gingival recession: a 6-month study. J Periodontol 2009;80:244–252.
randomized clinical trial. Int J Periodontics Restorative Dent 235. Pourabbas R, Chitsazi MT, Kosarieh E, Olyaee P. Coronally
2012;32:e41–50. advanced flap in combination with acellular dermal matrix
221. Ricci G, Silvestri M, Tinti C, Rasperini G. A clinical/statisti- with or without enamel matrix derivatives for root cover-
cal comparison between the subpedicle connective tissue age. Indian J Dent Res 2009;20:320–325.
graft method and the guided tissue regeneration tech- 236. Nickles K, Ratka-Krüger P, Neukranz E, Raetzke P, Eick-
nique in root coverage. Int J Periodontics Restorative Dent holz P. Ten-year results after connective tissue grafts and
1996;16:539–545. guided tissue regeneration for root coverage. J Periodontol
222. Novaes AB Jr, Grisi DC, Molina GO, Souza SL, Taba M Jr, 2010;81:827–836.
Grisi MF. Comparative 6-month clinical study of a subepi- 237. Aroca S, Keglevich T, Nikolidakis D, Gera I, Nagy K, Azzi
thelial connective tissue graft and acellular dermal matrix R, Etienne D. Treatment of class III multiple gingival
graft for the treatment of gingival recession. J Periodontol recessions: a randomized-clinical trial. J Clin Periodontol
2001;72:1477–1484. 2010;37:88–97.
223. Çetiner D, Parlar A, Baloş K, Alpar R. Comparative clinical 238. Ozcelik O, Haytac MC, Seydaoglu G. Treatment of multiple
study of connective tissue graft and two types of bio- gingival recessions using a coronally advanced flap proced-
absorbable barriers in the treatment of localized gingival ure combined with button application. J Clin Periodontol
recessions. J Periodontol 2003;74:1196–1205. 2011;38:572–580.
224. Cheung WS, Griffin TJ. A comparative study of root cover- 239. Cordaro L, di Torresanto VM, Torsello F. Split-mouth
age with connective tissue and platelet concentrate grafts: comparison of a coronally advanced flap with or without
8-month results. J Periodontol 2004;75:1678–1687. enamel matrix derivative for coverage of multiple gingival
225. Rahmani ME, Lades MA. Comparative clinical evaluation of recession defects: 6- and 24-month follow-up. Int J Peri-
acellular dermal matrix allograft and connective tissue graft odontics Restorative Dent 2012;32:10–20.
for the treatment of gingival recession. J Contemp Dent 240. McGuire MK, Scheyer ET. Xenogeneic collagen matrix with
Pract 2006;7:63–70. coronally advanced flap compared to connective tissue with
226. Abolfazli N, Saleh-Saber F, Eskandari A, Lafzi A. A com- coronally advanced flap for the treatment of dehiscence-
parative study of the long-term results of root coverage type recession defects. J Periodontol 2010:81:1108–1117.
with connective tissue graft or enamel matrix protein:
24-month results. Med Oral Patol Oral Cir Bucal 2009
1;14:E304–309.
Eur J Oral Implantol 2014;7(1):9–43
36 Pini-Prato et al Guidelines for single gingival recessions
Appendix – Characteristics and outcomes of included SRs and RCTs
Study Method
CRC RecRed
Cairo et al SR of RCTs of Miller class I Meta-analyses’ outcomes: Meta-analyses’ outcomes:
200864 and II single gingival reces-
sions with at least 6 months CAF vs. CAF+CTG (2 studies55,197): A statistically significant CAF vs. CAF+CTG (2 studies197,55): A statistically significant
of follow-up. OR of 2.49 (CI 95%: 1.10 to 5.68; P = 0.03; I2 = 0%) in difference of 0.49 mm (CI 95%: 0.14 to 0.83 mm; P = 0.005;
favour of CAF+CTG was reported. The total percentage of I2 = 0%) in favour of CAF+CTG was reported.
CRC was 52% (27/52 recessions) for CAF+CTG and 32%
(17/53 recessions) for CAF. CAF vs. CAF+BM (2 studies185,194): A not statistically significant
difference of -0.27 mm (CI 95%: -0.60 to 0.06 mm; P = 0.11,
CAF vs. CAF+BM (1 study201): A non-statistically significant I2 = 0%) in favour of CAF was reported.
OR of 0.58 (CI 95%: 0.16 to 2.08; P = 0.41) in favour of
CAF was reported. The percentage of CRC was 30% (6/20 CAF vs. CAF+EMD (5 studies187,199,202,204,206): A statistically
recessions) for CAF and 20% (4/20 recessions) for CAF+BM. significant difference of 0.58 mm (CI 95%: 0.21 to 0.95 mm;
P = 0.002; I2 = 50.5%) in favour of CAF+EMD was reported.
CAF vs. CAF+EMD (4 studies187,199,202,206): A statistically
significant OR of 3.89 (CI 95%: 1.59 to 9.50; P = 0.003; CAF vs. CAF+ADM (2 studies196,198): A non- statistically sig-
I2 = 15.2%) in favour of CAF+EMD was reported. The nificant difference of 0.60 mm (CI 95%: -0.52 to 1.73 mm;
total percentage of CRC was 66% (46/70 recessions) for P = 0.29; I2 = 87.1%) in favour of CAF+ADM was reported.
CAF+EMD and 39% (27/70 recessions) for CAF.
CAF vs. CAF+PRP (1 study200): A not statistically significant
CAF vs. CAF+ADM (2 studies196,198): A non-statistically difference of -0.20 mm (CI 95%: -0.89 to 0.49 mm; P = 0.57) in
significant OR of 4.83 (CI 95%: 0.23 to 99.88; P = 0.31; favour of CAF was reported.
I2 = 67.4%) in favour of CAF+ADM was reported.
CAF+CTG vs. CAF+BM (6 studies181-184,186,190): A statistically
CAF vs. CAF+PRP (1 study200): A non- statistically significant significant difference of -0.38 mm (CI 95%: -0.65 to -0.10 mm;
OR of 1.25(CI 95%: 0.23 to 6.71; P = 0.79) in favour of P = 0.008; I2 = 45.6%) in favour of CAF+CTG was reported.
CAF+PRP was reported. The percentage of CRC was 64%
(7/11 recessions) for CAF+PRP and 58% (7/12 recessions) CAF+CTG vs. CAF+ADM (4 studies188,192,193,207):
for CAF. A non-statistically significant difference of -0.40 mm (CI 95%:
-1.07 to 0.26; P = 0.24; I2 = 79.4%) in favour of CAF+CTG was
CAF+CTG vs. CAF+BM (6 studies181-184,186,190): A non- reported.
statistically significant OR of 0.45 (CI 95%: 0.20 to1.04;
P = 0.06; I2 = 31.9%) in favour of CAF+CTG was reported.
The total percentage of CRC was 53% (46/87 recessions) for
CAF+CTG and 36% (38/105 recessions) for CAF+BM.
CAF+CTG vs. CAF+EMD (1 study195): A non-statistically
significant OR of 2.31 (CI 95%: 0.45 to 11.74; P = 0.31) in
favour of CAF+EMD was reported. In the 10-years follow-up
of the same split-mouth study with 9 patients (out of 17),
5 out of 9 sites (56%) in the CAF+EMD group showed CRC,
while 7 out of 9 sites (78%) treated with CAF+CTG achieved
CRC (P = 0.157)87.
CAF+CTG vs. CAF+ADM
(4 studies188,192,193,207): A non-statistically significant OR of
0.49 (CI 95%: 0.23 to 1.03; P = 0.06; I2 = 0%) in favour of
CAF+CTG was reported. The total percentage of CRC was
39% (27/69 recessions) for CAF+CTG and 25% (17/69
recessions) for CAF+ADM.
CAF+CTG vs. CAF+HF+DDS
(1 study203): A not statistically significant OR of 1.00
(CI 95%: 0.02 to 50.40; P = 1.00) was reported.
The percentage of CRC was 10% (1/10 recessions) for
CAF+CTG and 10% (1/10 recessions) for CAF+HF+DDS.
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 37
Results
LAS Hypersensitivity Postoperative pain/complications Cost effectiveness
No meta-analysis was performed for this vari- No meta-analysis was performed for this variable No meta-analysis was performed for this variable NR
able because data were few and heterogene- because data were few and heterogeneous. because data were few and heterogeneous.
ous. Individual studies’ outcomes:
Individual studies’ outcomes: Individual studies’ outcomes:
CAF vs. CAF+CTG
CAF+CTG vs. CAF+BM Cortellini et al55 compared CAF vs. CAF+CTG, CAF vs. CAF+CTG
Romagna-Genon189 reported the aesthetic reporting no statistically significant differences da Silva et al197 reported no complication on
results obtained comparing CAF+CTG vs. for root sensitivity (12% of patients in the test comparing CAF vs. CAF+CTG. Cortellini et al55
CAF+BM in a split-mouth study. Among the group and 12% in the control group) six months reported 3 cases of haematoma in 43 patients
20 patients who were treated, 19 expressed following therapy (P = 1.0 Fisher exact test). treated with CAF, while 5 cases of haema-
their satisfaction with the clinical result for toma were reported in 42 patients treated with
both the tested surgical procedures; only one CAF+CTG vs. CAF+EMD CAF+CTG. A higher number of cases of swelling
patient, who had a pair of mandibular reces- McGuire & Nunn195 reported root sensitivity in were reported for the CAF+CTG group, and
sions, was disappointed because of the small only one case treated with CAF+EMD and none these differences were statistically significant
amount of coverage obtained following the for CAF+CTG 1 year following therapy. (CAF+CTG 32.2 ± 28.4 and CAF 17.8 ± 19.9
two treatments. using visual analogue scale (VAS), P = 0.0068).
Wang et al190 compared the aesthetic results No statistically significant differences for pain
of CAF+CTG vs. CAF+BM procedures in a were reported between two groups (23.8 ± 19.4
split-mouth 6-month study. An independ- for CAF and 31.4 ± 24.6 for CAF+CTG, using
ent periodontist was asked to rate the colour VAS, P = 0.0811).
match, contour, consistency, contiguity or
blending, and keloid formation 6 months CAF vs. CAF+BM
post-surgery. Patient satisfaction with the Amarante et al185 reported exposure of several
aesthetic (colour match, overall satisfaction, membranes in CAF+BM sites, while Lins et al194
and amount of root coverage) was recorded. reported the exposure of all membranes in all
When the periodontist rated the treatment treated sites (10/10).
results at 6 months, 15 out of 16 of CAF+BM
sites had excellent colour match and only
11 CAF+CTG sites reported the same. Good CAF vs. CAF+PRP
contour was noted in 15 CAF+BM sites versus No statistically significant differences for com-
13 CAF+CTG sites. Tissues showed firm con- plications were reported on comparing CAF vs.
sistency in all sites treated by either technique. CAF+PRP200 using a Wound Healing Index
Sixteen CAF+BM-treated sites were rated as (1.3 ± 0.5 for CAF and 1.2 ± 0.4 for CAF+PRP,
having acceptable blend as compared to 14 P > 0.05).
CAF+CTG sites. Keloid formation was noted
in only one CAF+CTG site. Six out of 16 of CAF+CTG vs. CAF+BM
CAF+BM sites rated by patients had ‘excellent’ In comparisons between CAF+CTG vs. CAF+BM,
colour match and 9 CAF+CTG sites reported membrane exposure was reported as a possible
the same. In overall satisfaction, 9 patients complication (7/15 Jepsen et al181, 2/12
rated as ‘excellent’ with CAF+BM procedure, Trombelli at al.182, 5/12 Takatis & Trombelli186,
vs. 7 of the CAF+CTG group. With regard to 0/20 Romagna-Genon189).
the amount of root coverage, 7 patients of the Jepsen et al181 reported pain and swelling on
CAF+BM group rated the CAF+BM procedure comparing CAF+CTG vs. CAF+BM in 15 split-
as ‘excellent, while 10 patients of CAF+CTG mouth patients. Five patients reported more
obtained the same. The differences were not discomfort after CAF+CTG procedure, 5 patients
significant (P >0.05). following CAF+BM, whereas the remaining 5
patients experienced no difference. When asked
CAF+CTG vs. CAF+ADM which technique they would have preferred
Aichelmann-Reidy et al188 compared for future root coverage, 7 patients opted for
CAF+ADM vs. CAF+CTG in a split-mouth the CAF+CTG method, and 8 for the CAF+BM
study in 22 patients by performing a double technique.
aesthetic evaluation (blinded clinician and Tatakis & Trombelli186 reported 7 cases of swelling
patient). Clinicians considered sites with in 12 patients treated with CAF+BM and none
CAF+ADM to have better results in 11 cases, for CAF+CTG. On the other hand, no complica-
while the other 11 were similar to CAF+CTG. tion for CAF+BM was reported by Wang et al190:
Patients considered CAF+ADM to have they reported 1 of 16 cases of swelling and 1
better aesthetics in 9 cases out of 22; in 12 ecchymosis in the CAF+CTG arm.
cases, they considered it similar to CAF+CTG; Romagna-Genon189 described postoperative
and only 1 patient preferred the site with discomfort for the palatal donor site for the
CAF+CTG. A keloid formation was reported in CAF+CTG. Sites treated with CAF+BM
one case of CAF+CTG. The difference favour- were more frequently symptom-free compared
ing CAF+ADM was statistically significant with CTG sites. None of the sites showed expo-
(P = 0.0215; McNemar test). sure of the membrane.
Eur J Oral Implantol 2014;7(1):9–43
38 Pini-Prato et al Guidelines for single gingival recessions
Study Method
CRC RecRed
Cham- SR of RCTs (minimum 10 Meta-analyses’ outcomes: Meta-analyses’ outcomes:
brone et al patients per arm at final
200865 examination) of Miller class CAF+CTG vs. CAF+BM (resorbable membranes) CAF+CTG vs. CAF+BM (resorbable membranes)
I and II gingival recessions (7 studies182-184,186,189,200,211): A statistically significant OR (7 studies182-184,186,189,200,211): A statistically significant differ-
2 mm or deeper, with at of 0.47 (CI 95%: 0.24 to 0.90; P = 0.02; I2 = 0%) in favour ence of -0.41 mm (CI 95%: -0.62 to -0.20 mm; P = 0.0002;
least 6 months of follow- of CAF+CTG was reported. I2 = 0%) in favour of CAF+CTG was reported.
up; the authors compared
CAF+CTG with other CAF+CTG vs. CAF+BM (non-resorbable membranes)
procedures. (2 studies181,183): A not statistically significant difference of
-0.43 mm (CI 95%: -1.21 to 0.35 mm; P = 0.28; I2 = 72.5%) in
favour of CAF+CTG was reported.
CAF+CTG vs. CAF+ADM (3 studies188,192,207): A statistically
significant difference of -0.63 mm (CI 95%: -1.26 to 0.00;
P = 0.05, I2 = 52.5%)] in favour of CAF+CTG was reported.
Cham- SR of RCTs (minimum 10 Meta-analyses’ outcomes: Meta-analyses’ outcomes:
brone et patients per arm at final
al 200942 examination) of Miller CAF vs. CAF+ADM (2 studies196,198): A non-statistically CAF vs. CAF+EMD (2 studies199,202): A not statistically sig-
class I and II gingival reces- significant RR of 1.95 (CI 95%: 0.76 to 5.04; P = 0.17; nificant difference of 0.25 mm (CI 95%: -0.13 to 0.64 mm;
sions ≥ 3 mm with at least I2 = 34%) in favour of CAF+ADM was reported. The P = 0.19; I2 = 21%) in favour of CAF+EMD was reported.
6 months of follow-up; total percentage of CRC was 48% (12/25 recessions) for
seventeen RCTs were not CAF+ADM and 20% (5/25 recessions) for CAF. CAF vs. CAF+ADM (2 studies196,198): A not statistically sig-
included in the analysis due nificant difference of 0.62 mm (CI 95%: 0.51 to 1.74 mm;
to the presence of gingival P = 0.28; I2 = 84%) in favour of CAF+ADM was reported.
recessions <3 mm and
5 RCTs because they CAF+CTG vs. CAF+ADM (2 studies): A not statistically signifi-
included <10 patients per cant difference of -0.76 mm (CI 95%: -1.93 to 0.42; P = 0.21,
arm at the last follow-up. I2 = 76%)] in favour of CAF+CTG was reported.
Jahnke et FGG vs. ET+CTG 5 out of 9 sites (56%) belonging to the ET+CTG group Estimates were not reported. The difference was statistically
al 199377 showed CRC, while 1 out of 9 sites (11%) treated with significant (P = 0.03) favouring ET+CTG.
6-month follow-up; split- FGG obtained CRC. P value was not reported. A calculation
mouth study; 10 patients; yielded an OR = 0.10 (CI 95%: 0.01 to 0.88; P = 0.04) in
single recessions. favour of ET+CTG.
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 39
Results
LAS Hypersensitivity Postoperative pain/complications Cost effectiveness
No meta-analysis was performed for this vari- No meta-analysis was performed for this variable No meta-analysis was performed for this variable NR
able because data were few and heterogene- because data were few and heterogeneous. because data were few and heterogeneous.
ous.
Individual studies’ outcomes:
CAF+CTG vs. CAF+BM
In two different studies181,189 subjective
patient preference did not differ between the
two treatment procedures.
No meta-analysis was performed for this vari- No meta-analysis was performed for this vari- No meta-analysis was performed for this variable NR
able because data were few and heterogene- able because data were few and heterogeneous. because data were few and heterogeneous.
ous. Individual studies’ outcomes:
CAF+CTG vs. CAF+EMD
McGuire & Nunn195 compared CAF+CTG vs.
CAF+EMD reporting: at 1 month, 9 patients
(45%) reported high discomfort levels associated
with the CAF+CTG treatment as opposed to 1
patient (5%) within the CAF+EMD group. This
difference was statistically significant (P = 0.011).
Ten patients (50%) reported no differences in
discomfort between the two treatments. At 3
months, 5 patients (25%) reported discomfort
with the CAF+CTG treatment as opposed to
3 patients (15%) reporting discomfort with
CAF+EMD treatment. After 6 months, differenc-
es in discomfort levels between the two groups
were minimal. At 1 year, only 1 patient exhibited
any ongoing adverse reaction. In this subject, the
CAF+CTG site was still exhibiting mild pain, and
the CAF+EMD site was still exhibiting mild sensi-
tivity. The only reported adverse events included
pain, swelling, bleeding, bruising, and sensitivity
– these events were similarly distributed among
both groups.
CAF+CTG vs. CAF+PRP
Keceli et al168 compared CAF+CTG vs. CAF+PRP
finding postoperative healing was generally
uneventful. Minor complications were related to
usual postoperative swelling and occurred within
the first days after surgery. Immediate postopera-
tive bleeding at the donor site occurred in 1
patient from the CAF+CTG group and was easily
managed by a sterile gauze compression.
NR NR In one patient, the dressing from an ET+CTG NR
site was dislodged while eating in a manner
inconsistent with postoperative instructions. He
returned to the clinic the following day, where it
was found that the CTG was no longer beneath
the recipient flap. Although the tissue healed
uneventfully to its original position, the patient
was dropped from the study. This represents a
violation of the intention to treat procedure.
Eur J Oral Implantol 2014;7(1):9–43
40 Pini-Prato et al Guidelines for single gingival recessions
Study Method
CRC RecRed
Paolanto- CAF+CTG vs. FGG Three out of 35 sites (9%) belonging to the FGG group Even if no data about RecRed are available, the final calculated
nio et al showed CRC, while 17 out of 35 sites (49%) treated with recession was 1.50 ± 0.39 mm in the FGG group, and
199778 5-year follow-up; parallel CAF+CTG obtained CRC. The P value was not reported. A 0.58 ± 0.46 mm in the CAF+CTG group.
study; 70 patients; single calculation yielded an OR = 0.10 (CI 95%: 0.03 to 0.39; The difference was statistically significant (P < 0.001).
recessions. P = 0.0008) in favour of CAF+CTG.
Bitten- CAF+CTG (without vertical Eight out of 17 sites (47%) belonging to the ST group Even if no data about RecRed are available, the final calculated
court et incisions) vs. ST showed CRC, while 15 out of 17 sites (88%) treated with recession was 0.28 ± 0.56 mm in the ST group, and
al 200679, CAF+CTG obtained CRC. P value was not reported. A 0.07 ± 0.20 mm in the CAF+CTG group.
200980 6-month follow-up79 and calculation yielded an OR = 0.19 (CI 95%: 0.04 to 0.91; The difference was not statistically significant (P >0.05).
30-months follow-up80; P = 0.04) in favour of CAF+CTG.
split-mouth study; 17
patients; single recessions.
Mahajan CAF vs. CAF+ADM NR The CAF+ADM procedure showed a reduction of
et al 3.85 ± 0.89 mm; while the CAF technique resulted in
200781 6-month follow-up; parallel 2.85 ± 0.89 mm reduction. The difference was statistically
study; 14 patients (7 per significant (P = 0.05).
group); single recessions.
Santama- CAF vs. CAF+ restoration NR The CAF+R procedure showed a reduction of 1.31 ± 0.37 mm;
ria et al while the CAF technique resulted in 1.39 ± 0.41 mm reduction.
200952 24-month follow-up; split- The difference was not statistically significant (P >0.05).
mouth study; 16 patients;
single recessions.
Santama- CAF+CTG vs. CAF+CTG+ NR CAF+CTG+R procedure showed a reduction of 2.31 ± 0.74
ria et al restoration mm; while the CAF+CTG technique resulted in a 2.53 ± 0.78
200953 mm reduction. The difference was not statistically significant
6-month follow-up; parallel (P = 0.41).
study; 40 patients; single
recessions.
Haghigh- CAF+CTG vs. CAF+ADM 3 out of 15 sites (20%) belonging to the CAF+ADM group At 5-year follow-up, the CAF+ADM procedure showed a reduc-
ati et al showed CRC, while 2 out of 15 sites (13%) treated with tion of 1.60 ± 1.22; while the CAF+CTG technique resulted in
200982; 6 month82 and 5 year CAF+CTG obtained CRC. The difference favouring CAF+ 1.50 ± 1.42 mm reduction. The difference was not statistically
Moslemi et follow-up85; split-mouth ADM was not significant (P = 1.0) significant (P = 0.838) favouring CAF+ADM.
al 201185 study; 16 patients at 6
months and 15 at 5 years;
single recessions; data are
presented at 5 years.
Santana et CAF vs. Semilunar coronal Two out 22 sites (9%) belonging to the ST group showed The ST procedure showed a reduction of 1.2 ± 0.5 mm; while
al 201083 flap (ST) procedure CRC, while 14 out 22 sites (64%) treated with CAF only the CAF technique resulted in 2.6 ± 0.7 mm reduction. The dif-
obtained CRC. P value was not reported. A calculation using ference was statistically significant (P <0.05), favouring the CAF
6-month follow-up; split- the intra-class correlation coefficient of a previous study190 procedure.
mouth study; 22 patients; yielded an OR = 0.06 (CI 95%: 0.01 to 0.26; P = 0.0002) in
single recessions. favour of CAF.
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 41
Results
LAS Hypersensitivity Postoperative pain/complications Cost effectiveness
NR NR NR NR
Fourteen out of 17 patients belonging to Three out of 17 patients of the SCF group A median pain VAS score of 30 mm (range
the ST group reported an excellent or good reported dental sensitivity, while none of the 20–60 mm) was recorded in the CAF+CTG
aesthetic result, and 3 reported a bad result. patients belonging to the CAF+CTG group group and 0 mm (meaning no pain at all) in the
All subjects of the CAF+CTG group reported reported dental sensitivity 30 months after ST group; P value was not reported80. The pain
an excellent or good result. Seven patients surgery. The difference was not statistically sig- intensity and the number of pills taken were
reported a better aesthetic in the sites treated nificant (P = 0.25; McNemar test). statistically different between groups only on the
with CAF+CTG than the opposite treated site. first day (P = 0.02), favouring the ST group79.
No patients reported any preference for the
sites treated with ST, and 10 patients did not
report any difference in terms of preference
between the 2 therapies80. The difference
favouring CAF+CTG was statistically signifi-
cant (P = 0.0215; McNemar test).
Root coverage perception: Six out of 7 patients of the CAF+ADM group Pain and discomfort during surgery: 2 out of 2 out of 7 patients
All the 7 patients belonging to the CAF+ADM were fully satisfied, while 5 out of 7 patients 7 patients of the CAF+ADM group were fully of the CAF+ADM
group were fully satisfied, while 4 out of 7 of the CAF group were also fully satisfied. satisfied, while 6 out of 7 patients of the CAF group were fully
patients of the CAF group were satisfied. The difference was not statistically significant group were also fully satisfied. The difference satisfied, while 6
The difference was not statistically significant (P = 0.58). was statistically significant (P = 0.03), favouring out of 7 patients
(P = 0.15). the CAF group. of the CAF group
were also fully
Colour of gums: All of the 7 patients belong- Postoperative pain and swelling: 2 out of 7 satisfied. The dif-
ing to the CAF+ADM group were fully patients of the CAF+ADM group were fully satis- ference was statis-
satisfied, while 6 out of 7 patients of the CAF fied, while 6 out of 7 patients of the CAF group tically significant
group were satisfied. The difference was not were as well fully satisfied. The difference was (P = 0.03), favour-
statistically significant (P = 0.30). statistically significant (P = 0.03), favouring the ing the CAF group.
CAF group.
Shape of gum contours: 5 patients belonging
to the CAF+ADM group were fully satisfied,
while 5 out of 7 patients of the CAF group
were also fully satisfied. The difference was
not statistically significant (P = 1).
NR NR NR NR
NR One out of 20 patients reported dental sensitivity NR NR
in the CAF+CTG+R, while 7 out of 20 patients
showed dental sensitivity after 6 months with
the CAF+CTG method. The difference was stat-
istically significant (P = 0.04 Fisher exact test),
favouring the CAF+ CTG +R procedure.
NR NR NR NR
No data are available, even if the authors NR No postoperative pain or complications were NR
reported that all sites treated with ST resulted observed in any patients.
in a notable semilunar white scar.
Eur J Oral Implantol 2014;7(1):9–43
42 Pini-Prato et al Guidelines for single gingival recessions
Study Method
CRC RecRed
Santana et CAF vs. Laterally positioned Fifteen out of 18 sites (83%) belonging to the LPF group The LPF procedure showed a reduction of 3.26 ± 0.4 mm; while
al 201084 flap (LPF) showed CRC, while 16 out of 18 sites (89%) treated with the CAF technique resulted in 3.09 ± 0.5 mm reduction. The dif-
CAF only obtained CRC. P value was not reported (P >0.05). ference was not statistically significant (P = 0.26 t test).
6-month follow-up; parallel A calculation yielded an OR = 0.63 (CI 95%: 0.09 to 4.28;
study; 36 patients (18 per P = 0.63) in favour of CAF.
group); single recessions.
McGuire CAF+CTG vs. CAF+CM Fifteen out of 25 sites belonging to the CAF+CM group At 1-year follow-up, the CAF+CM procedure showed a reduc-
& Scheyer showed CRC, while 23 out of 25 sites treated with CAF+CTG tion of 2.78 mm; while the CAF+CTG technique resulted in
2010240 1-year follow-up; split- obtained CRC 6 months after treatment. At the 12-month 3.17 mm reduction. The difference was statistically significant
mouth study; 25 patients at evaluation, 17 out 23 (CAF+CM) (74%) and 22 out 23 sites (P = 0.0172) favouring CAF+CTG.
6 months and 23 at 1 year; (CAF+CTG) (96%) achieved CRC. P value was not reported
single recessions. (P >0.05).
Nazareth CAF vs. CAF+Anorganic Ten out 15 sites (67%) belonging to the CAF+ABM/P-15 CAF+ABM/P-15 procedure showed a reduction of
& Cury Bovine-derived hydroxyapa- showed CRC, while 11 out 15 sites (73%) treated with CAF 2.20 ± 0.54 mm; while CAF technique resulted in
201086 tite Matrix/cell-binding only obtained CRC. P value was not reported. A calculation 2.40 ± 0.80 mm reduction. The difference (-0.20 ± 0.14 mm,
peptide (ABM/P-15) pro- yielded an OR = 0.73 (CI 95%: 0.18 to 2.86; P = 0.65) in favouring CAF group) was not statistically significant (P = 0.33).
cedure favour of CAF.
6-month follow-up; split-
mouth study; 15 patients;
single recessions.
McGuire et CAF+CTG vs. CAF+EMD 5 out of 9 sites (56%) belonging to the CAF+EMD group CAF+EMD procedure showed a reduction of 3.33 ± 0.87 mm;
al 2101287 showed CRC, while 7 out of 9 sites (78%) treated with while CAF+CTG technique resulted in 3.67 ± 1.12 mm reduc-
10-year follow-up (the CAF+CTG obtained CRC (P = 0.157). tion. The difference was not statistically significant (P = 0.625).
1-year follow-up was previ-
ously published, McGuire &
Nunn 2003195); split-mouth
study; 9 patients (out of
17); single recessions.
Zucchelli et CAF+CTG vs. Laterally CRC was achieved in 12 out of 25 defects of the CAF+CTG The CAF+CTG procedure showed a reduction of
al 201288 Moved Coronally Advanced group (48%), while in 1 out of 25 of the LPF group (4%). 4.04 ± 0.64 mm, while the LPF technique resulted in
Flap (LPF) The difference was statistically significant (P <0.05) favouring 3.68 ± 0.75 mm of recession reduction. The difference was not
CAF+CTG. statistically significant (P = 0.07 t test).
1-year follow-up; parallel
study; 50 patients; 50 single
recessions.
Jepsen et CAF vs. CAF+CM CRC was achieved in 16 out of 45 sites (36%) treated The CAF+CM procedure showed a reduction of
al 201389 with the CAF+CM group, while in 14 out of 45 sites 2.59 ± 1.11 mm, while the CAF technique resulted in
(31%) were treated with CAF. The difference was not 2.32 ± 0.99 mm of recession reduction. The difference was
6-month follow-up; multi-
statistically significant (P = 0.3870). statistically significant (P = 0.0175) in favour of CAF+CM.
centre split-mouth study;
45 patients; 90 single
recessions.
CRC: Complete Root Coverage; LAS: Level of Aesthetic Satisfaction; RecRed: Recession Reduction; SR: Systematic Review; RCTs: Randomised Controlled Trials; OR: Odds
Ratio; RR: Relative Risk; CAF: Coronally Advanced Flap; CTG: Connective Tissue Graft; BM: resorbable and non-resorbable Barrier Membrane; EMD: Enamel Matrix Deriva-
tive; ADM: Acellular Dermal Matrix; PRP: Platelet-Rich Plasma; HF-DDS: Human Fibroblast-Derived Dermal Substitute; CM: Xenogenic Collagen Matrix; ST: Semilunar Tech-
nique; FGG: Free Gingival Graft; LPF: Laterally Positioned Flap; ET: Envelope Technique; ADMP15: Anorganic Bovine Derived Hydroxyapatite Matrix Cell Bridging Peptide; R:
Resin Composite Restoration.
Eur J Oral Implantol 2014;7(1):9–43
Pini-Prato et al Guidelines for single gingival recessions 43
Results
LAS Hypersensitivity Postoperative pain/complications Cost effectiveness
NR NR No postoperative pain or complications were NR
observed in any patients.
The estimates were not reported. No statistic- NR The estimates were not reported. No statistically NR
ally significant difference could be discerned. significant difference could be discerned in pain
or discomfort.
NR NR No postoperative pain and complications were NR
observed in any patients.
As regard to the aesthetic satisfaction, six Three out of 9 sites of the CAF+EMD proced- At the 10-year
patients had no preference for a particular type ure and 1 out of 9 sites of CAF+CTG procedure follow-up visit,
of treatment, two declared better aesthetic showed dental sensitivity. The difference was not patients were asked
results following CAF+EMD procedure and statistically significant (P = 0.157). to indicate the
one preferred the aesthetic outcomes with preference of the
CAF+CTG procedure (P = 0.564). CAF+EMD procedure: 6 out of
sites showed an equivalent texture to sur- 9 patients preferred
rounding tissues in 8 out of 9 sites versus 5 the CAF+EMD
out of 9 sites in CAF+CTG group. The differ- treatment, 1
ence was not statistical significant (P = 0.083). favoured CAF+CTG
When examining the colour equivalence of the procedure, and 2
surgical sites to the adjacent tissues, 8 out of had no preference.
9 CAF+EMD sites and 6 out of 9 CAF+CTG The difference was
sites were judged to have equivalent colour not statistically sig-
to surrounding tissues. The difference was not nificant
statistical significant (P = 0.157). (P = 0.059).
Eight out of 8 CAF+EMD sites and 1 of 8
CAF+CTG sites had equivalence of tissue con-
tour. The difference was statistically significant
(P = 0.008) favouring CAF+EMD sites.
Aesthetic patient evaluation in a VAS was Sensitivity VAS was 94.0 ± 6.5 for CAF+CTG After 7 days, the VAS values relating to pain were NR
91.2 ± 9.3 for CAF+CTG (25 patients) and and 87.6 ± 8.3 for LPF. The difference favouring 77.2 ± 16.4 for CAF+CTG and 93.2 ± 8.0 for
89.6 ± 7.9 for LPF (25 patients). CAF+CTG was statistically significant (P <0.01). LPF. The difference favouring LPF was statistically
The difference was not statistically significant significant (P <0.01).
(P = 0.52 t test). After 7 days, the VAS values related to chewing
ability was 72.8 ± 14.3 for CAF+CTG and
88.8 ± 8.3 for LPF. The difference favouring LPF
was statistically significant (P <0.01).
NR NR After 7 days, pain VAS was 2.32 ± 2.08 for NR
CAF+CM and 0.04 ± 1.82 for CAF.
After 14 days, pain VAS was 0.68 ± 1.21 for
CAF+CM and 0.59 ± 0.91 for CAF. The dif-
ferences were not statistically significant (P
>0.05).
Eur J Oral Implantol 2014;7(1):9–43
S-ar putea să vă placă și
- J 1600-051x 2012 01903 XDocument9 paginiJ 1600-051x 2012 01903 XDiyaa SakrÎncă nu există evaluări
- Clinical Efficacy of Periodontal Plastic Surgery Procedures Consensus Report of Group 2 of The 10th European Workshop On PeriodontologyDocument8 paginiClinical Efficacy of Periodontal Plastic Surgery Procedures Consensus Report of Group 2 of The 10th European Workshop On PeriodontologyImplant DentÎncă nu există evaluări
- Minimally Invasive Surgical Technique and Enamel Matrix Derivative in Intra-Bony Defects. I - Clinical Outcomes and MorbidityDocument7 paginiMinimally Invasive Surgical Technique and Enamel Matrix Derivative in Intra-Bony Defects. I - Clinical Outcomes and MorbidityAnissa Citra UtamiÎncă nu există evaluări
- Cairo, 2010Document14 paginiCairo, 2010Maximiliano Jara ContrerasÎncă nu există evaluări
- Connections of Dental ImplantsDocument8 paginiConnections of Dental ImplantsVijay Prabu GÎncă nu există evaluări
- J Clinic Periodontology - 2021 - Martin - Effect of Orthodontic Therapy in Periodontitis and Non Periodontitis Patients ADocument30 paginiJ Clinic Periodontology - 2021 - Martin - Effect of Orthodontic Therapy in Periodontitis and Non Periodontitis Patients Apaulina becerraÎncă nu există evaluări
- Art 1Document15 paginiArt 1Carol LozanoÎncă nu există evaluări
- 08 PRD GTR OrthoDocument11 pagini08 PRD GTR OrthoVictor Corona BuenfilÎncă nu există evaluări
- J Clinic Periodontology - 2021 - MartinDocument30 paginiJ Clinic Periodontology - 2021 - Martinjeffry francisco campusano torresÎncă nu există evaluări
- Minimally Invasive Approaches in Endodontic PracticeDe la EverandMinimally Invasive Approaches in Endodontic PracticeGianluca PlotinoÎncă nu există evaluări
- Peri的手術作法guide s1532-3382 (12) 70021-0Document12 paginiPeri的手術作法guide s1532-3382 (12) 70021-0黃道中Încă nu există evaluări
- Implant Survival Rates, Marginal Bone Level Changes, and Complications in Full-Mouth Rehabilitation With Flapless Computer-Guided SurgeryDocument10 paginiImplant Survival Rates, Marginal Bone Level Changes, and Complications in Full-Mouth Rehabilitation With Flapless Computer-Guided SurgeryLuis Fernando RodriguesÎncă nu există evaluări
- The Effectiveness of Adjunctive Light-Activated Disinfection (LAD) in The Treatment of Peri-Implantitis: 4-Month Results From A Multicentre Pragmatic Randomised Controlled TrialDocument12 paginiThe Effectiveness of Adjunctive Light-Activated Disinfection (LAD) in The Treatment of Peri-Implantitis: 4-Month Results From A Multicentre Pragmatic Randomised Controlled TrialJarvin Buitrago GalindezÎncă nu există evaluări
- 10 1016@j Ijom 2020 03 008Document12 pagini10 1016@j Ijom 2020 03 008runit nangaliaÎncă nu există evaluări
- Case Report Enlargement GinggivaDocument3 paginiCase Report Enlargement GinggivaAnindya LaksmiÎncă nu există evaluări
- Class IIMeta FixedDocument14 paginiClass IIMeta FixedGuillermo Alvarado LassoÎncă nu există evaluări
- Apiko 2Document7 paginiApiko 2Asri DamayantiÎncă nu există evaluări
- Article NVDocument7 paginiArticle NVhaidarhamzaaaÎncă nu există evaluări
- Self-Ligating Brackets Do Not Reduce Discomfort or Pain When Compared To Conventional Orthodontic Appliances in Class I Patients: A Clinical StudyDocument5 paginiSelf-Ligating Brackets Do Not Reduce Discomfort or Pain When Compared To Conventional Orthodontic Appliances in Class I Patients: A Clinical StudySai BabaÎncă nu există evaluări
- 5 Year Outcomes After Coverage of Soft Source Eur J Oral Impl...Document10 pagini5 Year Outcomes After Coverage of Soft Source Eur J Oral Impl...hzycasperÎncă nu există evaluări
- J Clinic Periodontology - 2020 - Sanz - Treatment of Stage I III Periodontitis The EFP S3 Level Clinical Practice GuidelineDocument57 paginiJ Clinic Periodontology - 2020 - Sanz - Treatment of Stage I III Periodontitis The EFP S3 Level Clinical Practice GuidelineKeHuyDietÎncă nu există evaluări
- Arduino 2011Document4 paginiArduino 2011Fahmi Nur SuwandiÎncă nu există evaluări
- Treatment Stage I-Iii J Clinic Periodontology - 2020 - Sanz - Treatment of Stage I III Periodontitis The EFP S3 Level Clinical Practice GuidelineDocument57 paginiTreatment Stage I-Iii J Clinic Periodontology - 2020 - Sanz - Treatment of Stage I III Periodontitis The EFP S3 Level Clinical Practice GuidelineSofia Zaematul ArifahÎncă nu există evaluări
- Treatment of Stage I-III Periodontitis-The EFP S3 Level Clinical Practice GuidelineDocument57 paginiTreatment of Stage I-III Periodontitis-The EFP S3 Level Clinical Practice GuidelinePaulina Müller100% (1)
- Arnett Combined Orthodontic and Surgical Open Bite CorrectionDocument12 paginiArnett Combined Orthodontic and Surgical Open Bite CorrectionAlex ReaÎncă nu există evaluări
- Reconstructive Surgical Therapy of Peri-Implantitis: A Multicenter Randomized Controlled Clinical TrialDocument24 paginiReconstructive Surgical Therapy of Peri-Implantitis: A Multicenter Randomized Controlled Clinical Trialrmartins76Încă nu există evaluări
- Clinical Assessment of Short Implants Retsining Removsble Partial DenturesDocument7 paginiClinical Assessment of Short Implants Retsining Removsble Partial DenturesLouis HutahaeanÎncă nu există evaluări
- Cortellini Et Al-2017-Journal of Clinical PeriodontologyDocument9 paginiCortellini Et Al-2017-Journal of Clinical PeriodontologyCloudcynaraaÎncă nu există evaluări
- J Clinic Periodontology - 2021 - Jentsch - Flapless Application of Enamel Matrix Derivative in Periodontal Retreatment ADocument9 paginiJ Clinic Periodontology - 2021 - Jentsch - Flapless Application of Enamel Matrix Derivative in Periodontal Retreatment ATamara Pereira SanchezÎncă nu există evaluări
- CortelinniDocument12 paginiCortelinniAlin OdorÎncă nu există evaluări
- 2017 Laleman - Guided Implant Surgery in The Edentulous Maxilla - A Systematic ReviewDocument15 pagini2017 Laleman - Guided Implant Surgery in The Edentulous Maxilla - A Systematic ReviewFabio FabrettiÎncă nu există evaluări
- Trombelli Et Al-2017-Journal of Clinical PeriodontologyDocument7 paginiTrombelli Et Al-2017-Journal of Clinical PeriodontologyAlexandra BuhaianuÎncă nu există evaluări
- Artículo de Técnica Del Muro. G. ZucchelliDocument10 paginiArtículo de Técnica Del Muro. G. ZucchelliBasma DerdabiÎncă nu există evaluări
- Sopravvivenza Perioprotesi Di FeboDocument6 paginiSopravvivenza Perioprotesi Di FeboSadeer RiyadÎncă nu există evaluări
- Art. FisuradosDocument11 paginiArt. FisuradosInma Coronado de la TorreÎncă nu există evaluări
- Quality Guidelines For Endodontic Treatment: Consensus Report of The European Society of EndodontologyDocument10 paginiQuality Guidelines For Endodontic Treatment: Consensus Report of The European Society of EndodontologyARTÎncă nu există evaluări
- Class IIMeta FixedDocument14 paginiClass IIMeta FixedDr. Pooja VoraÎncă nu există evaluări
- Immediate Loading of Mandibular Overdentures Retained by Two Mini-Implants: A Case Series Preliminary ReportDocument7 paginiImmediate Loading of Mandibular Overdentures Retained by Two Mini-Implants: A Case Series Preliminary Reportdrmezzo68Încă nu există evaluări
- Clinical Oral Implants Res - 2022 - Jung - Effect of Peri Implant Mucosal Thickness On Esthetic Outcomes and The EfficacyDocument9 paginiClinical Oral Implants Res - 2022 - Jung - Effect of Peri Implant Mucosal Thickness On Esthetic Outcomes and The EfficacyGustavo BerrioÎncă nu există evaluări
- Soft Tissue Management at Implants Summary and Consensus Statements of Group 2. The 6th EAO Consensus Conference 2021Document8 paginiSoft Tissue Management at Implants Summary and Consensus Statements of Group 2. The 6th EAO Consensus Conference 2021Od. Valeria Gutierrez GÎncă nu există evaluări
- Surgical Treatment of Peri-Implantitis: 3 - Year Results From A Randomized Controlled Clinical TrialDocument10 paginiSurgical Treatment of Peri-Implantitis: 3 - Year Results From A Randomized Controlled Clinical TrialFabian SanabriaÎncă nu există evaluări
- 10 Years Randomised Cotrolled Study 2012Document11 pagini10 Years Randomised Cotrolled Study 2012Hicham AL KHAYARÎncă nu există evaluări
- 2022 Orto X PerioDocument9 pagini2022 Orto X PerioKatia ValÎncă nu există evaluări
- J Clinic Periodontology - 2020 - Stavropoulos - Medium and Long Term Clinical Benefits of Periodontal RegenerativeDocument21 paginiJ Clinic Periodontology - 2020 - Stavropoulos - Medium and Long Term Clinical Benefits of Periodontal RegenerativejcÎncă nu există evaluări
- Nonsurgical Management of Complex Endodontic Cases With Several Periapical Lesions: A Case SeriesDocument10 paginiNonsurgical Management of Complex Endodontic Cases With Several Periapical Lesions: A Case SeriesAlyaÎncă nu există evaluări
- 1 s2.0 S1761722723001201 MainDocument18 pagini1 s2.0 S1761722723001201 MainDANTE DELEGUERYÎncă nu există evaluări
- Jurnal Laser GingivectomyDocument6 paginiJurnal Laser GingivectomyFajar RamadhanÎncă nu există evaluări
- Artículo CirugíaDocument7 paginiArtículo CirugíaRobin FernandezÎncă nu există evaluări
- Endodontic J - 2006 - Quality Guidelines For Endodontic Treatment Consensus Report of The European Society ofDocument10 paginiEndodontic J - 2006 - Quality Guidelines For Endodontic Treatment Consensus Report of The European Society ofZelallem AnileyÎncă nu există evaluări
- Efficacy of Periodontal Plastic Surgery Procedures in The Treatment of Localized Facial Gingival Recessions. A Systematic ReviewDocument19 paginiEfficacy of Periodontal Plastic Surgery Procedures in The Treatment of Localized Facial Gingival Recessions. A Systematic Reviewanwer safeerÎncă nu există evaluări
- Prof. Stefano Benedicenti: Dean of Endodotic, Restorative and Laser Dental DepartmentDocument7 paginiProf. Stefano Benedicenti: Dean of Endodotic, Restorative and Laser Dental DepartmentAsif IqbalÎncă nu există evaluări
- Tooth Decay and Highly Conservative TreatmentsDocument26 paginiTooth Decay and Highly Conservative TreatmentsJose Ignacio ZalbaÎncă nu există evaluări
- On A of The Appropriate Timing For Surgical Intervention in Orthognathic SurgeryDocument10 paginiOn A of The Appropriate Timing For Surgical Intervention in Orthognathic SurgeryKira LagoÎncă nu există evaluări
- Peri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentDe la EverandPeri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentÎncă nu există evaluări
- 23 RD JC - SindhuDocument7 pagini23 RD JC - SindhuDadi SindhuÎncă nu există evaluări
- 7-Muller. 2019. Risk Factors For Recurrence of Periodontal Disease in Patients in Maintenance CareDocument9 pagini7-Muller. 2019. Risk Factors For Recurrence of Periodontal Disease in Patients in Maintenance CarePaula YunesÎncă nu există evaluări
- Management of Peri-Implantitis: A Systematic Review, 2010-2015Document9 paginiManagement of Peri-Implantitis: A Systematic Review, 2010-2015Angela RamirezÎncă nu există evaluări
- Mozzati2014 - Song Sieu Am Trong NH Răng 8Document4 paginiMozzati2014 - Song Sieu Am Trong NH Răng 8Hoàng VũÎncă nu există evaluări
- Gulabi2014 PDFDocument10 paginiGulabi2014 PDFZaz ONÎncă nu există evaluări
- Debate Over Delayed vs. Immediate ImplantsDocument1 paginăDebate Over Delayed vs. Immediate ImplantsDentalLearningÎncă nu există evaluări
- 187 FullDocument9 pagini187 FullFernando CursachÎncă nu există evaluări
- Journal of Dental Research: Prevention of Dry SocketsDocument7 paginiJournal of Dental Research: Prevention of Dry SocketsFernando CursachÎncă nu există evaluări
- Implant Failure Etiology PDFDocument3 paginiImplant Failure Etiology PDFFernando CursachÎncă nu există evaluări
- From Prophylaxis To TreatmentDocument8 paginiFrom Prophylaxis To TreatmentFernando CursachÎncă nu există evaluări
- Full Mouth Fixed Implant Rehabilitation in A Patient With Generalized Aggressive PeriodontitisDocument6 paginiFull Mouth Fixed Implant Rehabilitation in A Patient With Generalized Aggressive PeriodontitisFernando CursachÎncă nu există evaluări
- Efectos Del Diodolaser PeriimDocument6 paginiEfectos Del Diodolaser PeriimFernando CursachÎncă nu există evaluări
- Platform SwitchingDocument7 paginiPlatform SwitchingFernando CursachÎncă nu există evaluări
- 2008 03 20 BDocument8 pagini2008 03 20 BSouthern Maryland OnlineÎncă nu există evaluări
- Lesson Plan in Advanced Chemistry AlcohoDocument17 paginiLesson Plan in Advanced Chemistry AlcohoGlaiza Mapute CaringalÎncă nu există evaluări
- BlahDocument8 paginiBlahkwood84100% (1)
- PBL 2 Case PresentationDocument12 paginiPBL 2 Case PresentationRamish IrfanÎncă nu există evaluări
- 8953-Specifications For Doosan Man 9l21 31Document7 pagini8953-Specifications For Doosan Man 9l21 31Bae Juyeon100% (1)
- Exam Questions: Exam Title: Chapter MEK 8Document4 paginiExam Questions: Exam Title: Chapter MEK 8vishnu sharmaÎncă nu există evaluări
- Clinical Features, Evaluation, and Diagnosis of Sepsis in Term and Late Preterm Infants - UpToDateDocument42 paginiClinical Features, Evaluation, and Diagnosis of Sepsis in Term and Late Preterm Infants - UpToDatedocjime9004Încă nu există evaluări
- RDG UNIT 2 Skimming Class A 2021Document17 paginiRDG UNIT 2 Skimming Class A 2021Yuly Rumondang Wulan SiallaganÎncă nu există evaluări
- Shoulder Joint Position Sense Improves With ElevationDocument10 paginiShoulder Joint Position Sense Improves With ElevationpredragbozicÎncă nu există evaluări
- HSN-Lube 2007 PDFDocument45 paginiHSN-Lube 2007 PDFCecilio Valderrama100% (3)
- Practice Test For Exam 3 Name: Miguel Vivas Score: - /10Document2 paginiPractice Test For Exam 3 Name: Miguel Vivas Score: - /10MIGUEL ANGELÎncă nu există evaluări
- We Find The Way: Shipping InstructionsDocument10 paginiWe Find The Way: Shipping InstructionsLuke WangÎncă nu există evaluări
- 1Manuscript-BSN-3y2-1A-CEDILLO-222 11111Document32 pagini1Manuscript-BSN-3y2-1A-CEDILLO-222 11111SHARMAINE ANNE POLICIOSÎncă nu există evaluări
- Decision Making in Perioperative Medicine Clinical Pearls 2021Document351 paginiDecision Making in Perioperative Medicine Clinical Pearls 2021Dal RdzÎncă nu există evaluări
- Recommended Practice For Corrosion Management of Pipelines in Oil & Gas Production and TransportationDocument123 paginiRecommended Practice For Corrosion Management of Pipelines in Oil & Gas Production and Transportationsaifoa100% (2)
- Estrogen Dominance-The Silent Epidemic by DR Michael LamDocument39 paginiEstrogen Dominance-The Silent Epidemic by DR Michael Lamsmtdrkd75% (4)
- BottomDocument4 paginiBottomGregor SamsaÎncă nu există evaluări
- Chef Basics Favorite RecipesDocument58 paginiChef Basics Favorite Recipesbillymac303a100% (2)
- BT HandoutsDocument4 paginiBT HandoutsNerinel CoronadoÎncă nu există evaluări
- Full Carrino Plaza Brochure and Application (General)Document8 paginiFull Carrino Plaza Brochure and Application (General)tanis581Încă nu există evaluări
- Epoxy Data - AF35LVE TDS - ED4 - 11.17Document8 paginiEpoxy Data - AF35LVE TDS - ED4 - 11.17HARESH REDDYÎncă nu există evaluări
- Janssen Vaccine Phase3 Against Coronavirus (Covid-19)Document184 paginiJanssen Vaccine Phase3 Against Coronavirus (Covid-19)UzletiszemÎncă nu există evaluări
- Dual Laminate Piping HandbookDocument46 paginiDual Laminate Piping HandbookA.Subin DasÎncă nu există evaluări
- Uppercut MagazineDocument12 paginiUppercut MagazineChris Finn100% (1)
- EE2401 Power System Operation and ControlDocument93 paginiEE2401 Power System Operation and ControlPrasanth GovindarajÎncă nu există evaluări
- RNW Position PaperDocument2 paginiRNW Position PaperGeraldene AcebedoÎncă nu există evaluări
- WEEK 7-8: Health 9 Module 4Document8 paginiWEEK 7-8: Health 9 Module 4Heidee BasasÎncă nu există evaluări
- Nursing Management of Anti Fungal DrugsDocument25 paginiNursing Management of Anti Fungal DrugsJennyDaniel100% (1)
- Region Iii - Central Luzon Padapada National High SchoolDocument2 paginiRegion Iii - Central Luzon Padapada National High SchoolRotipÎncă nu există evaluări
- Fawad Hussain, Feedback On Industrial Visit To Sahiwal Coal Power PlantDocument2 paginiFawad Hussain, Feedback On Industrial Visit To Sahiwal Coal Power PlantSyed Fawad MarwatÎncă nu există evaluări