Documente Academic
Documente Profesional
Documente Cultură
History and PE Student Guide
Încărcat de
Mary Rose DomalantaTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
History and PE Student Guide
Încărcat de
Mary Rose DomalantaDrepturi de autor:
Formate disponibile
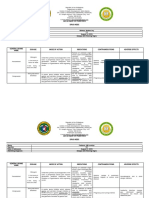
PEDIATRIC PHYSICAL DIAGNOSIS
Module 1: Vaccination
VACCINATION SKILLS
Explains to mother the diseases prevented by the vaccines to be administered (BCG, Hepa B,
MMR)
Explains to mother possible complications and gives instructions on what to do in case there
are any (rashes, irritability, vomiting, fever, seizures)
Washes hands or uses alcohol to clean hands, wears gloves
Cleans the area to be vaccinated using cotton with alcohol
Changes the needle used to aspirate vaccine with a new one for injection to patient
Correctly administers BCG – Intradermal
vaccine using the right Hepa B - Intramuscular
route (with proper Measles - Subcutaneous
angle) and technique
Places dry cotton with tape on vaccination site
MODULE 2: Observed History-taking (Syncope Case)
HISTORY TAKING SKILLS YES NO Information gathered
Opening Greets the patient and
the relative
interview Introduces self and role on
healthcare team
Acknowledges
caregiver/child and calls
them by name
Data Name
gathering: Age or date of birth
General Gender
data Address
Informant/relationship to
patient
Chief Asks reason for seeking
complaint care/presenting problem
History of Onset: when the problem
present started, chronologic order
illness of events, previous
episodes
Activity prior to syncope
Duration of loss of
consciousness
Last meal intake prior to
syncope
Relieving factors
Associated symptoms like
seizure, pallor, fever,
cyanosis, etc.
Were medications given?
Was consultation done?
Review of General: weight loss, fever,
systems decreased appetite,
Skin: rashes
Eyes: discharge, redness
Ears: discharge, redness,
swelling
Respiratory: cough, colds.
Difficulty breathing
Neuromuscular: seizures,
weakness, increased
sleeping time
Past Medical illnesses
illnesses
Previous hospitalizations
Drug reactions/allergies
Accidents, surgeries
Feeding Sample Diet
history: Any feeding problem?
Infancy
Maternal Maternal check-ups,
and birth illnesses, medications taken
history: Alcohol intake, smoking,
Prenatal attitude towards pregnancy
OB score, miscarriages
Natal Type of delivery, assisted
by: OB or midwife, location,
complications
Postnatal Apgar score, condition upon
birth, birth weight, duration
of hospital stay ,
complications: jaundice,
sepsis, cyanosis
Develop- Behavioral problems?
mental School performance
history: Any incident of bullying at
school?
Immuni- Date of administration
zations Allergic/adverse reactions
to vaccines
Family Size of family
history Illnesses in other family
members, causes of death
Heredofamilial diseases
Personal Home conditions; economic
and social status
history Parents’ occupations
Principal caregiver
Religion/ cultural beliefs
HEADSSS • H- ome (relationships
(you may at home)
ask the • E- ducation (school
parent if it performance, subjects
is ok for doing well and
her to subjects having
leave the difficulty, any learning
room so disability?),
you can E-Employment, Eating
privately habits
speak to
the child • A- ctivities (sports,
only. Be hobbies)
very • D- rugs (use of illicit
careful drugs, alcohol,
with your cigarette smoking)
questions, • S- exuality (sexual
and be preference, sexual
sensitive. relationships and
Avoid experience)
laughing. )
• S- afety (risk-taking
behavior)
• S- uicidal
ideations/Depression
Closing Asks caregiver if he/she has
the any question, concerns
interview Closes the interview with
appropriate gestures and
statements
PEDIATRIC PHYSICAL DIAGNOSIS
MODULE 2: Observed Physical Exam
SKILLS Yes No PE FINDINGS
PREPARATION a. Minimizes patient discomfort/anxiety
b. Explains to child and caregiver what
he/she is doing
VITAL SIGNS a. Measures temperature Temp:
b. Counts heart rate for 1 minute HR:
c. Counts respiratory rate for 1 minute RR:
d. Measures blood pressure (for >3yo) BP:
with age appropriate cuff
ANTHROPO- a. Weight Wt:
METRIC b. Height Ht:
MEASURE-
MENTS
GENERAL a. Level of consciousness:
SURVEY awake/lethargic/unconscious
comfortable/irritable
b. Ambulatory/carried by caregiver
c. Poorly/fairly/well nourished
d. Cyanotic/pale/pinkish
e. With or without respiratory distress –
shortness of breath
HEENT a. Checks pupillary response to light
b. Looks for sunken eyes
c. Inspects for dryness of lips and oral
mucosa
d. Inspects oropharynx using a light
source and tongue depressor if
necessary
e. Examines tympanytic membranes
using otoscope
f. Checks nares for polyps/congestion
g. Palpates neck for lymph
nodes/mass/enlarged thyroid
HEART a. Palpates point of maximal impulse
b. Palpates for heaves/thrills
c. Auscultates the heart in 4 areas
(ULSB, URSB, LLSB, apex)
d. Notes if there is regular or irregular
heart rate and/or murmur
e. Palpates pulses on wrists (radial
pulse) and feet (dorsalis pedis pulse)
and reports whether full, fair or poor
f. Checks capillary refill time
LUNGS a. Inspects chest for deformities and
chest retractions
b. Auscultates all lung fields starting at
apices and works downward
comparing symmetric points
sequentially (anteriorly and
posteriorly)
c. Demonstrates egophony (“E” to “A”)
in an older, cooperative child
d. Checks for symmetric chest
expansion by palpation and
inspection
e. Percusses the thorax and reports if it
is resonant
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Who Dengue Classification and Differentials ModuleDocument14 paginiWho Dengue Classification and Differentials ModuleKevin AgbonesÎncă nu există evaluări
- Orbital TraumaDocument42 paginiOrbital TraumaMary Rose DomalantaÎncă nu există evaluări
- App Nut MidtermsDocument8 paginiApp Nut MidtermsMary Rose DomalantaÎncă nu există evaluări
- Endo FinalsDocument3 paginiEndo FinalsMary Rose DomalantaÎncă nu există evaluări
- Patutoy DBDocument2 paginiPatutoy DBMary Rose DomalantaÎncă nu există evaluări
- Department of Pediatrics Drug IndexDocument10 paginiDepartment of Pediatrics Drug IndexMary Rose DomalantaÎncă nu există evaluări
- North Avenue, Diliman Quezon CityDocument2 paginiNorth Avenue, Diliman Quezon CityMary Rose DomalantaÎncă nu există evaluări
- Jose R. Reyes Memorial Medical Center Department of Surgery: Clinical DatabaseDocument2 paginiJose R. Reyes Memorial Medical Center Department of Surgery: Clinical DatabaseMary Rose DomalantaÎncă nu există evaluări
- Jose R. Reyes Memorial Medical Center Department of Surgery: Clinical DatabaseDocument2 paginiJose R. Reyes Memorial Medical Center Department of Surgery: Clinical DatabaseMary Rose DomalantaÎncă nu există evaluări
- X Pedia TicklerDocument8 paginiX Pedia TicklerAndrew Jason HilarioÎncă nu există evaluări
- History and PE Student GuideDocument5 paginiHistory and PE Student GuideMary Rose DomalantaÎncă nu există evaluări
- Eng-Letter of Guarantee PDFDocument1 paginăEng-Letter of Guarantee PDFJanna Robles SantosÎncă nu există evaluări
- Junior Intern Daily Progress NotesDocument5 paginiJunior Intern Daily Progress NotesMary Rose DomalantaÎncă nu există evaluări
- North Avenue, Diliman Quezon CityDocument2 paginiNorth Avenue, Diliman Quezon CityMary Rose DomalantaÎncă nu există evaluări
- Schedule of Stay Itinerary Template Free WordDocument2 paginiSchedule of Stay Itinerary Template Free WordheyoooÎncă nu există evaluări
- Schedule of Stay Itinerary Template Free WordDocument2 paginiSchedule of Stay Itinerary Template Free WordheyoooÎncă nu există evaluări
- VMMC HX PEDocument4 paginiVMMC HX PEMary Rose DomalantaÎncă nu există evaluări
- Eng-Letter of Guarantee PDFDocument1 paginăEng-Letter of Guarantee PDFJanna Robles SantosÎncă nu există evaluări
- Eng-Letter of Guarantee PDFDocument1 paginăEng-Letter of Guarantee PDFJanna Robles SantosÎncă nu există evaluări
- Eng-Letter of Guarantee PDFDocument1 paginăEng-Letter of Guarantee PDFJanna Robles SantosÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (120)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- 5 Basic Acupuncture Points For Moxibustion Application in The Prevention of InfluenzaDocument10 pagini5 Basic Acupuncture Points For Moxibustion Application in The Prevention of InfluenzaIvonne Flores FernándezÎncă nu există evaluări
- Ape FormsDocument7 paginiApe FormsLlednew Lavodnas100% (4)
- EP IndexDocument42 paginiEP IndexstephetjÎncă nu există evaluări
- (E) Hostel Form-DPSB - A4Document4 pagini(E) Hostel Form-DPSB - A4ghjegjwÎncă nu există evaluări
- Controlling Microbial Growth in VitroDocument65 paginiControlling Microbial Growth in VitroCarl Elexer Cuyugan Ano100% (15)
- Pathogenesis of Type 1 Diabetes MellitusDocument28 paginiPathogenesis of Type 1 Diabetes MellitusJuan Diego Fernández MurielÎncă nu există evaluări
- 100MCQsinTropicalMedicine (PDF Library)Document76 pagini100MCQsinTropicalMedicine (PDF Library)Abdalla ShibailiÎncă nu există evaluări
- Regional Ethics Bowl Cases 2015Document33 paginiRegional Ethics Bowl Cases 2015Sathvik PalakurtyÎncă nu există evaluări
- Summarized Notes (Infectious Diseases)Document3 paginiSummarized Notes (Infectious Diseases)Amirah HmzÎncă nu există evaluări
- 13 Roles and ResponsibilitiesDocument14 pagini13 Roles and ResponsibilitiesDevendra Singh TomarÎncă nu există evaluări
- Briefing Memo House Vaccine Hesitancy Hearing 2021.05.26Document7 paginiBriefing Memo House Vaccine Hesitancy Hearing 2021.05.26Stephen LoiaconiÎncă nu există evaluări
- 9700 w14 QP 23Document16 pagini9700 w14 QP 23rashmi_harryÎncă nu există evaluări
- Rabies PhilippinesDocument30 paginiRabies PhilippinesChar Caberic100% (1)
- Certificat de Vaccinare Împotriva Covid-19 Vaccination Certificate Against COVID-19Document1 paginăCertificat de Vaccinare Împotriva Covid-19 Vaccination Certificate Against COVID-19Maxim AndrianaÎncă nu există evaluări
- Recording Forms (Masterlist) School Forms - Kinder To Grade 7Document16 paginiRecording Forms (Masterlist) School Forms - Kinder To Grade 7lourdes estopaciaÎncă nu există evaluări
- We Get Results!: Labor Day Weekend!Document39 paginiWe Get Results!: Labor Day Weekend!The WorldÎncă nu există evaluări
- List of Medicinal ProductsDocument10 paginiList of Medicinal ProductsFandossituÎncă nu există evaluări
- National Child Development CenterDocument7 paginiNational Child Development CenterJayson GuerreroÎncă nu există evaluări
- SepticemiaDocument171 paginiSepticemiaThashini Devi Nagaratnam100% (1)
- Prevention, Control Treatment of Nipah Virus Infection: Utsav Kumar Shrestha Roll No.: S-22Document14 paginiPrevention, Control Treatment of Nipah Virus Infection: Utsav Kumar Shrestha Roll No.: S-22utsavshrestha05Încă nu există evaluări
- Biographical DataDocument29 paginiBiographical DataJai - HoÎncă nu există evaluări
- Reverse VaccinologyDocument18 paginiReverse Vaccinologyrahamathunnisha100% (1)
- NCERT Class9 Why Do We Fall IllDocument6 paginiNCERT Class9 Why Do We Fall IllagnelwaghelaÎncă nu există evaluări
- Ambulatory Care Nursing: Coming Soon!Document16 paginiAmbulatory Care Nursing: Coming Soon!fiora.ladesvitaÎncă nu există evaluări
- Bacterial Pneumonia in Cattle - Respiratory System - Veterinary ManualDocument4 paginiBacterial Pneumonia in Cattle - Respiratory System - Veterinary ManualMutiara DarisÎncă nu există evaluări
- Descendants - Of.the - Sun.e15.160413.720p 540p 450p XViD WITH IPOP BarosG LIMO CHAOSrel (Viki Version)Document50 paginiDescendants - Of.the - Sun.e15.160413.720p 540p 450p XViD WITH IPOP BarosG LIMO CHAOSrel (Viki Version)MEILINDAÎncă nu există evaluări
- Immunisation History Statement 3Document2 paginiImmunisation History Statement 3Fordham JessÎncă nu există evaluări
- Jibachha's Textbook of Equine, Rabbit & Pet Animals-By Dr. Jibachha SahDocument16 paginiJibachha's Textbook of Equine, Rabbit & Pet Animals-By Dr. Jibachha SahJibachha Shah100% (1)
- Midterm Activity ScitechDocument3 paginiMidterm Activity ScitechKean KaiÎncă nu există evaluări
- Prednisone TabDocument10 paginiPrednisone TabrantiadrianiÎncă nu există evaluări