Documente Academic
Documente Profesional
Documente Cultură
National Voluntary Blood Services Blood Safety Report
Încărcat de
Corachea LabTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
National Voluntary Blood Services Blood Safety Report
Încărcat de
Corachea LabDrepturi de autor:
Formate disponibile
National Voluntary Blood Services
Blood Safety Indicators Report Form
Program
GLOBAL DATABASE ON BLOOD SAFETY (GDBS) 2010
GLOBAL DATABASE ON BLOOD SAFETY
The World Health Organization (WHO) programme on Blood Transfusion Safety would appreciate your kind cooperation in completing
this questionnaire which has been designed to obtain information for the WHO Global Database on Blood Safety.
The GDBS was established by WHO to address global concerns about the availability, safety, and equitable accessibility of blood for
transfusion. It covers the four major components of the integrated strategy for blood safety advocated by WHO:
§ The establishment of well-organized, nationally-coordinated blood transfusion services with quality systems in all areas
§ The collection of blood from voluntary non-remunerated blood donors from low-risk populations and the phasing out of
family/replacement and paid donation
§ The screening of all donated blood for transfusion-transmissible infections, including HIV, hepatitis B and C, syphilis and other
infectious agents; blood grouping and compatibility testing
§ A reduction in unnecessary transfusions through the effective clinical use of blood.
The objective of the GDBS is to collect and analyse data from all Member States of WHO in order to enable the Organization to:
§ Obtain the best available information on blood transfusion services in each Member State
§ Assess the global situation on blood safety, availability and access and monitor trends and progress
§ Identify priority countries for support and technical assistance
§ Plan research and develop appropriate strategies to address specific needs.
The GDBS was initiated in 1998. GDBS reports are available on the WHO website (http://www.who.int/bloodsafety/global database/) and
from WHO Headquarters and Regional Offices. Please contact WHO for further information or assistance on completing the GDBS
DATA COLLECTION FOR THE PERIOD JANUARY - DECEMBER 2009
The GDBS questionnaire should be completed by an authorized person in the respective BSF. Please provide details of the person who
completes the questionnaire so that Philippine Blood Center can contact, if necessary, for clarification and further information.
The questionnaire should be completed with data for the period January to December 2010. If calendar year information is not
available, please provide information for the nearest 12-month period (e.g. April 2009 to March 2010),and indicate the period covered
on the form.
DATA COLLECTION QUESTIONNAIRE
You are requested to complete the electronic version of the questionnaire, if possible.
Please enter your responses only in the yellow boxes that are shown on the screen. The questionnaire has been protected to prevent
responses from being entered outside these boxes. You will also find that some boxes are grey in colour. These boxes contain formulae
and are also protected; automatic calculations will be made in these boxes as the relevant data are entered.
Options of "Yes" and "No" are offered for responses to qualitative questions. To answer this type of question, click on the box for your
preferred answer; a black point will then appear in the centre of the box. If you wish to change your answer, simply click on another
box. If you feel that a "Yes" or "No" answer alone is insufficient to capture some aspects of the situation in your country, please provide
further information in the "Comment" box at the bottom of each worksheet. Information provided through the "Comment" boxes is an
essential part of the data collected through this questionnaire. If you inadvertently click on a "Yes" or "No" box and wish to revert to the
previous setting where neither "Yes" nor "No" are selected, click on the grey portion of the box beside the choices, press the "Del" (or
"Delete") key (see figure below).
Automatic error checking has been incorporated into the electronic questionnaire. This is designed to prevent the entry of data that are
invalid or obviously incorrect. When such an error occurs, a message will appear to indicate the error and the entry will be rejected.
Before continuing, you should review and change the data just entered.
RETURNING THE GDBS QUESTIONNAIRE
Philippine Blood Center
IBBIS Department
BRL Building, Department of Health, Tayuman
Tel no. 7317578
E-mail: pbcbsi@gmail.com, pbcbsi@yahoo.com
Global Database on Blood Safety (GDBS) 2008 Page 1 of 7
National Voluntary Blood
Blood Safety Indicators Report Form 2012
Services Program
v.1.1
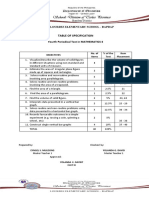
Section 1: Administrative Information
1.1 Date July 10, 2019
1.2 Region Region 4A
1.3 Blood Service Facility/ Hospital
H.M. Corachea General Hospital
1.4 Classification Blood Station
Information provided by:
1.5 Name Danielle Jane P. Perez, RMT
1.6 Position Chief Medical Technologist
1.7 Organization H.M. Corachea General Hospital
1.8 Address
324 Brgy. Santor, Tanauan City, Batangas
1.9 Tel. no. (043) 778 1293
1.10 Fax no.
1.11 E-mail corachea.lab@gmail.com
1.12 Period covered by report January 2018- July 2019
Section 2: Blood Donors and blood collection
2.1 Do you use standard operating procedures (SOPs) or local written instruction for: Yes No
2.1.1 Blood donor recruitment ●
2.1.2 Pre-donation counselling and donor selection
2.1.3 Blood collection and donor care
2.1.4 Post-donation counselling
2.2 Do you maintain records of the following
2.2.1 Blood donor recruitment
2.2.2 Pre-donation counselling and donor selection
2.2.3 Blood collection and donor care
2.2.4 Post-donation counselling
2.3 How many blood donors donated whole blood during the reporting period?
2.3.1 Total number of donors who donated blood 0
2.3.2 Total number of voluntary non-remunerated donors who donated blood 0
2.4 How many deferrals were there from whole blood donation, by types of deferral?
2.4.1 Permanent deferral 0
2.4.2 Temporary deferral 0
2.4.3 Total number of deferrals 0
2.5 How many deferrals were there from whole blood donation, by reasons for deferral?
2.5.1 Low haemoglobin (in the old monitoring forms this is Hemoglobin) 0
2.5.2 Other medical conditions (in the old monitoring forms this is PE&Hx) 0
2.5.3 High-risk behaviour (in the old monitoring forms this is under TTDs) 0
2.5.4 Travel and other reasons (in the old monitoring forms this is under Other Reasons) 0
2.5.5 Total number of deferrals 0
2.6 How many whole blood donations were collected, by types of donation?
2.6.1 Voluntary non-remunerated donations 0
2.6.2 Family/replacement donations 0
2.6.3 Paid donations 0
2.6.4 Total number of donations 0
2.7 How many whole blood donations were collected from:
2.7.1 Male donors
2.7.2 Female donors
2.7.3 Total number of donations 0
2.8 How many whole blood donations were collected from:
2.8.1 Donors under 18 years 0
2.8.2 Donors aged 18 to 24 years 0
2.8.3 Donors aged 25 to 44 years 0
2.8.4 Donors aged 45 to 64 years 0
2.8.5 Donors aged 65 years or older 0
2.8.6 Total number of donations 0
2.9 How many whole blood donations were collected from first-time voluntary non-remunerated
0
donors?
2.10 Donation: donor ratio for voluntary non-remunerated whole blood donors #DIV/0!
2.11 Are any blood donations collected through apheresis procedures?
If yes, how many apheresis donations were collected by types of donation?
2.11.1 Voluntary non-remunerated apheresis donations
2.11.2 Family/ replacement apheresis donations
2.11.3 Paid apheresis donations
2.11.4 Others (please specify):
2.11.5 Total number of apheresis donations 0
2.11.6 Total number of donors who donated through apheresis procedures during
reporting period
2.12 Do you have a system for post-donation counselling of blood donors who test positive
for transfusion-transmissible infections?
Section 3: Screening for transfusion-transmissible infections
3.1 Do you perform laboratory screening of blood donations for transfusion transmissible
infections?
3.1.1 Do you use EIA for screening blood donations for TTIs?
3.2 Do you use standard operating procedures or local written instructions for laboratory
screening of blood donations for transfusion transmissible infections?
3.3 Do you participate in an external quality assessment scheme/external evaluation or
performance for transfusion-transmissible infections?
3.4 How many donations (whole blood and apheresis) were screened for the following transfusion-transmissible
infections?
3.4.1 HIV 0 #DIV/0!
3.4.2 Hepatitis B 0 #DIV/0!
3.4.3 Hepatitis C 0 #DIV/0!
3.4.4 Syphilis 0 #DIV/0!
3.4.5 Malaria 0 #DIV/0!
3.5 How many donations (whole blood and apheresis) were: (a) reactive in the screening test; and (b) positive in
the confirmatory test?
Screening test Confirmatory test
TTI Markers
reactive positive
3.5.1 HIV 0 #DIV/0! 0 #DIV/0!
3.5.2 Hepatitis B 0 #DIV/0! 0 #DIV/0!
3.5.3 Hepatitis C 0 #DIV/0! 0 #DIV/0!
3.5.4 Syphilis 0 #DIV/0! 0 #DIV/0!
3.5.5 Malaria 0 #DIV/0! 0 #DIV/0!
3.6 What was the prevalence of the following TTI markers in donated blood during the reporting period?
3.6.1 HIV #DIV/0!
3.6.2 Hepatitis B #DIV/0!
3.6.3 Hepatitis C #DIV/0!
3.6.4 Syphilis #DIV/0!
3.6.5 Malaria #DIV/0!
3.7 Details in which screening for TTIs is performed: number of donations tested, use of standard operating
procedures (SOPs) and participation in external quality assessment/external evaluation of performance
Total Number of donations screened for each TTI SOPs used Participate in EQA
donations HIV HBV HCV Syphilis Malaria Yes No Yes No
0 0 0 0 0 0
3.8 Were any blood units issued without screening due to:
3.8.1 Non-availability of test kits/reagents
3.8.2 Emergency situations
3.8.3 Staff shortages
3.8.4 Equipment failure/breakdown/power loss
3.8.5 Other reasons (please specify)
Section 4: Blood group serology testing of blood donations
4.1 Do you perform blood group serology testing of blood donations?
4.1.1 Do you use tube method for blood group serology testing?
4.2 Do you use standard operating procedures or local written instructions for blood group
serology testing of blood donations?
4.3 Do you maintain records of blood group serology testing?
4.4 Do you participate in an external quality assessment scheme/external evaluation of
performance for blood serology?
Section 5: Blood component preparation, storage and transportation
5.1 Do you prepare blood components?
5.2 How many whole blood donations were separated into components? #DIV/0!
5.3 How many units of blood components were prepared from whole blood donations?
Component
5.3.1 Red cell preparations 0
5.3.2 Platelet concentrates 0
5.3.3 Plasma 0
5.3.4 Fresh Frozen Plasma 0
5.3.5 Cryoprecipitate 0
5.4 How many units of blood components were prepared through apheresis procedures?
5.4.1 Apheresis red cells 0
5.4.2 Apheresis platelets 0
5.4.3 Apheresis plasma 0
5.4.5 Total blood components 0
5.5 Do you use standard operating procedures or local written instructions for the
preparation of blood components?
5.6 Do you maintain records of blood component preparation?
5.7 Do you store whole blood and whole blood components in temperature-monitored
equipment?
5.8 Do you transport whole blood and whole blood components in temperature-monitored
equipment?
5.9 Do you store test kits and reagents in temperature-monitored equipment?
5.10 How many units of whole blood were discarded due to faulty collection? 0
5.11 How many units of whole blood and blood components were discarded due to other reasons?
Component Reason for discard
Processing Storage Transport Date
TTI Problem Total
Problem problem expiry
5.11.1 Whole blood 0
5.11.2 Red cells 0
5.11.3 Platelets 0
5.11.4 Plasma 0
5.11.5 Fresh frozen plasma 0
5.11.6 Cryoprecipitate 0
5.11.7 Total component discarded 0 0 0 0 0 0
Section 6: Hospital transfusion process and clinical use of blood & blood components
6.1 Do you perform blood transfusion?
6.2 Do you perform compatibility testing?
6.2.1 Do you use standard operating procedures or local written instructions for
compatibility testing?
6.2.2 Do you maintain records of compatibility testing?
6.2.3 Do you participate in an external quality assessment scheme/external evaluation
of performance for compatibility testing?
6.2.4 Do you store whole blood and whole blood components in temperature-monitored
equipment?
6.3 Do you participate in:
6.3.1 Hospital transfusion committee
6.3.2 System for monitoring clinical transfusion practice
6.3.3 System for reporting adverse transfusion incidents
6.4 How many patients were transfused?
6.5 How many patients were transfused by age and gender? Male Female
6.5.1 Patients under 5 years
6.5.2 Patients aged 5 to 14 years
6.5.3 Patients aged 15 to 44 years
6.5.4 Patients aged 45 to 59 years
6.5.5 Patients aged 60 years older
6.5.6 Total number of patients transfused by gender 0 0
6.6 How many units of each of the following blood components were transfused?
6.6.1 Whole blood
6.6.2 Red cells
6.6.3 Plasma and fresh frozen plasma
6.6.4 Platelets, whole blood-derive
6.6.5 Platelets, apheresis
6.6.6 Cryoprecipitate
6.7 Do you use standard operating procedures or local written instructions for the
transfusion of blood to patients?
6.8 Do you maintain records of blood transfusion to patients?
6.9 How many serious adverse transfusion incidents or reactions were reported?
Comment (optional)
S-ar putea să vă placă și
- Mapeh ViDocument4 paginiMapeh ViFrances Diane Arnaiz Segurola50% (2)
- Summative Test in Music 6Document1 paginăSummative Test in Music 6jackelyn jamon100% (1)
- Worksheet: Grade Six Second QuarterDocument5 paginiWorksheet: Grade Six Second QuarterCatherine Lagario Renante100% (1)
- Gsis Loan Borrower ManifestationDocument1 paginăGsis Loan Borrower Manifestationxannderendab100% (1)
- FIRST QUARTER EXAMINATION IN MAPEH 6Document5 paginiFIRST QUARTER EXAMINATION IN MAPEH 6Tintin Frayna GabalesÎncă nu există evaluări
- Transfusion-Transmitted Diseases: 6 EditionDocument31 paginiTransfusion-Transmitted Diseases: 6 EditionKaycee Gretz Loresca100% (1)
- Activity Sheet In: English 6Document9 paginiActivity Sheet In: English 6maricel pampilo100% (1)
- 1st Midterm ExamDocument19 pagini1st Midterm ExamCherry Mae Lopez CarredoÎncă nu există evaluări
- Second Periodic Test in English V NAME: - GR.& SEC. - SCORE: - Read The Paragraphs Below Then Answer The Questions That FollowDocument5 paginiSecond Periodic Test in English V NAME: - GR.& SEC. - SCORE: - Read The Paragraphs Below Then Answer The Questions That FollowGoldine Barcelona EteÎncă nu există evaluări
- Summ. Test GR, 6 2020Document8 paginiSumm. Test GR, 6 2020luisaÎncă nu există evaluări
- Grade 6 2nd Quarter Pointers To ReviewDocument1 paginăGrade 6 2nd Quarter Pointers To ReviewKristerann JimenezÎncă nu există evaluări
- Diagnostic Least Mastered Skills 2019-2020Document3 paginiDiagnostic Least Mastered Skills 2019-2020Mabelle Mengote NardoÎncă nu există evaluări
- Army's Integrated School Science TestDocument6 paginiArmy's Integrated School Science TestSher SherwinÎncă nu există evaluări
- Periodical Test in CLE 5Document2 paginiPeriodical Test in CLE 5Anna AÎncă nu există evaluări
- Math IV PTDocument3 paginiMath IV PTKristine Joy Linsangan - NacionÎncă nu există evaluări
- 1st Summative Test in EspDocument4 pagini1st Summative Test in EspMyrna LagapaÎncă nu există evaluări
- I. Analogy A. Complete The Analogy of The Given Pair of Words. (5pts)Document3 paginiI. Analogy A. Complete The Analogy of The Given Pair of Words. (5pts)Rimah Macabangon AlamadaÎncă nu există evaluări
- SCIENCE 6 Summative Test #1 QTR 2Document4 paginiSCIENCE 6 Summative Test #1 QTR 2Jovelyn L. Lucio100% (1)
- LS2 - Herbal Medicine - WorksheetsDocument3 paginiLS2 - Herbal Medicine - WorksheetsMarbz AlsteacherÎncă nu există evaluări
- Personal Data SheetDocument6 paginiPersonal Data SheetJanice DaquelÎncă nu există evaluări
- Grade 6 Q2 Filipino LASDocument115 paginiGrade 6 Q2 Filipino LASLampa Ana KareninaÎncă nu există evaluări
- 1st PeriodicTest English 4Document4 pagini1st PeriodicTest English 4Jay-Ar Ricafranca MitraÎncă nu există evaluări
- Quarterly Grades Summary for Grade 7-PEACEDocument2 paginiQuarterly Grades Summary for Grade 7-PEACEMel PangalÎncă nu există evaluări
- Pre Test - Training On Malaria Elimination Surveillance Strategy & ToolsDocument6 paginiPre Test - Training On Malaria Elimination Surveillance Strategy & ToolsRuffy AbdulazisÎncă nu există evaluări
- Gr6 Alliteration, Assonance, Onomatopoeia, Consonance WorksheetDocument1 paginăGr6 Alliteration, Assonance, Onomatopoeia, Consonance WorksheetFema Emper AcostaÎncă nu există evaluări
- MAPEH Exam Prepares Students for Healthy LivesDocument4 paginiMAPEH Exam Prepares Students for Healthy LivesMelanie Nina ClareteÎncă nu există evaluări
- Worksheets LS2 Climate ChangeDocument7 paginiWorksheets LS2 Climate ChangeAngeline Panaligan AnselaÎncă nu există evaluări
- GRATITUDE SPEECH G6 - Jaslene TijingDocument1 paginăGRATITUDE SPEECH G6 - Jaslene TijingChantilly Marie VillarinÎncă nu există evaluări
- ADM Template Gr.7 10 v2.2 EnglishDocument16 paginiADM Template Gr.7 10 v2.2 EnglishAngelica Pampag50% (2)
- Summative Test 3 English 5 Quarter1 Week 56Document2 paginiSummative Test 3 English 5 Quarter1 Week 56Ginalyn Manalaysay RegenciaÎncă nu există evaluări
- Math 5 Achievement Test (Review)Document1 paginăMath 5 Achievement Test (Review)John Paul Medrano100% (1)
- The Milestones of Polomolok Central Elementary SchoolDocument2 paginiThe Milestones of Polomolok Central Elementary SchoolLee Ziel0% (1)
- Rounding Numbers ToolDocument20 paginiRounding Numbers ToolEn CyÎncă nu există evaluări
- Homeroom Guidance Module 2Document2 paginiHomeroom Guidance Module 2Rd DavidÎncă nu există evaluări
- EnglishDocument2 paginiEnglishEdgar Miralles Inales Manriquez100% (2)
- Grade 5 CLEDocument5 paginiGrade 5 CLEGinaly0% (1)
- Community BrochureDocument1 paginăCommunity BrochureDeadX GamingÎncă nu există evaluări
- Science IV ReviewerDocument3 paginiScience IV ReviewerPrecilla Ugarte HalagoÎncă nu există evaluări
- Fourth Quarter ExamDocument17 paginiFourth Quarter ExamRuel AcebronÎncă nu există evaluări
- 4th P.T. Math 4, ESP4, AP4, EPP4 (Ict), English 4, Math 6Document28 pagini4th P.T. Math 4, ESP4, AP4, EPP4 (Ict), English 4, Math 6Jeana LicasÎncă nu există evaluări
- Grade 4 6 Edukasyong Pantahanan at PangkabuhayanDocument54 paginiGrade 4 6 Edukasyong Pantahanan at Pangkabuhayanmary graceÎncă nu există evaluări
- Grade 3 Adjectives WorksheetsDocument3 paginiGrade 3 Adjectives WorksheetsIrene Rodríguez LópezÎncă nu există evaluări
- TEST Science 1st With TOSDocument8 paginiTEST Science 1st With TOSAdor IsipÎncă nu există evaluări
- Second Summative Test in ScienceDocument2 paginiSecond Summative Test in ScienceARRIANE JOY TOLEDO100% (1)
- FRACTIONSDocument95 paginiFRACTIONSJun Ril100% (3)
- Post Test - Training On Malaria Elimination Surveillance Strategy and ToolsDocument7 paginiPost Test - Training On Malaria Elimination Surveillance Strategy and ToolsRuffy AbdulazisÎncă nu există evaluări
- Children Around The WorldDocument2 paginiChildren Around The WorldRezyl Manlangit100% (1)
- Criteria of Judging (TikTok)Document1 paginăCriteria of Judging (TikTok)AJÎncă nu există evaluări
- First Mid-Quarter Examination Review TestDocument24 paginiFirst Mid-Quarter Examination Review TestAivy Ylanan100% (1)
- Science 4 Achievement Test (Review)Document2 paginiScience 4 Achievement Test (Review)John Paul MedranoÎncă nu există evaluări
- English 4 WorksheetsDocument7 paginiEnglish 4 WorksheetsNimfa Lozada100% (1)
- Achievement Test Science 4 Regular ClassDocument9 paginiAchievement Test Science 4 Regular ClassJassim MagallanesÎncă nu există evaluări
- Annex A2 RPMS Tool For Proficient Teachers SY 2023-2024Document20 paginiAnnex A2 RPMS Tool For Proficient Teachers SY 2023-2024Jerry BasayÎncă nu există evaluări
- PT - Mathematics 2 - Q3Document9 paginiPT - Mathematics 2 - Q3Christopher Cabrales0% (1)
- Quarter 1 Science 6 Periodical Test ReviewerDocument12 paginiQuarter 1 Science 6 Periodical Test ReviewerJECONIAH ADONAÎncă nu există evaluări
- PT Q3 Mapeh 3Document8 paginiPT Q3 Mapeh 3Joanne Crystal AzucenaÎncă nu există evaluări
- First Periodical Test in English 6Document9 paginiFirst Periodical Test in English 6Baby AleiraÎncă nu există evaluări
- National Voluntary Blood Services Blood Safety Report 2016Document7 paginiNational Voluntary Blood Services Blood Safety Report 2016Charmaine Corpuz GranilÎncă nu există evaluări
- Blood Safety Indicator 2012Document7 paginiBlood Safety Indicator 2012Fitz Gerald CastilloÎncă nu există evaluări
- Bsi 2020Document140 paginiBsi 2020MK MalaluanÎncă nu există evaluări
- Sex Stories IndonesiaDocument3 paginiSex Stories IndonesiausahamerekaÎncă nu există evaluări
- Microbiology MMV-Sample-MCQsDocument8 paginiMicrobiology MMV-Sample-MCQsMuhammad AttiqueÎncă nu există evaluări
- 04 11 2016.tanzania National Guideline For Management Hiv and Aids May 2015. TaggedDocument290 pagini04 11 2016.tanzania National Guideline For Management Hiv and Aids May 2015. TaggedArdilah Dwiagus SafitriÎncă nu există evaluări
- Six Building Blocks of Health SystemDocument19 paginiSix Building Blocks of Health SystemChala FekaduÎncă nu există evaluări
- As CaseStudy GuideDocument28 paginiAs CaseStudy GuideAli VehbÎncă nu există evaluări
- Symptoms: Signs in NewbornsDocument4 paginiSymptoms: Signs in NewbornshaniÎncă nu există evaluări
- TORCH MedscapeDocument17 paginiTORCH MedscapeAndrea RivaÎncă nu există evaluări
- Health Education For Behavior Change - A Workbook To ImproveDocument42 paginiHealth Education For Behavior Change - A Workbook To ImproveNayyar Raza KazmiÎncă nu există evaluări
- ChildFund AR 2018-Final PDFDocument20 paginiChildFund AR 2018-Final PDFSSÎncă nu există evaluări
- English Case HIV in Pregnancy ArdeDocument48 paginiEnglish Case HIV in Pregnancy ArdeArde Hidayat100% (1)
- Nutrition For AIDSDocument3 paginiNutrition For AIDSLeow Chee SengÎncă nu există evaluări
- Journal of Borderland Research - Vol XLV, No 2, March-April 1989Document38 paginiJournal of Borderland Research - Vol XLV, No 2, March-April 1989Thomas Joseph Brown100% (2)
- Dental Assistant Sample TestDocument10 paginiDental Assistant Sample TestFaye Nervanna Alecha Alferez100% (1)
- Who PCPNC PDFDocument179 paginiWho PCPNC PDFTiffany Joyce MarcellanaÎncă nu există evaluări
- MSF - H Mental Health Guidelines, 9 August 2005Document140 paginiMSF - H Mental Health Guidelines, 9 August 2005Diego Mercado100% (1)
- Catalogue of Organizations Providing Services For Persons With Disabilities in Addis AbabaDocument100 paginiCatalogue of Organizations Providing Services For Persons With Disabilities in Addis AbabaSeid Hussein100% (2)
- Case Study - To All Corners of KenyaDocument8 paginiCase Study - To All Corners of KenyaViweÎncă nu există evaluări
- 13 WhydowefallillDocument10 pagini13 WhydowefallillBharati AngadiÎncă nu există evaluări
- Lymphatic SystemDocument70 paginiLymphatic SystemNang Maizana Megat Yahya100% (1)
- 2015GSHS Philippines FactSheet 2Document8 pagini2015GSHS Philippines FactSheet 2Willa LlanetaÎncă nu există evaluări
- EOI 1 - Program Officer - TLF MFRHR ACERDocument3 paginiEOI 1 - Program Officer - TLF MFRHR ACERAnonymous 3qMquA0QtVÎncă nu există evaluări
- Laws Affecting The Practice of NursingDocument3 paginiLaws Affecting The Practice of NursingAce EsperanzateÎncă nu există evaluări
- Representing HIV: From Icon to MetaphorDocument13 paginiRepresenting HIV: From Icon to MetaphorHaneen HannouchÎncă nu există evaluări
- Safe Motherhood PDFDocument13 paginiSafe Motherhood PDFcarissa rhezaÎncă nu există evaluări
- Interview QuestionsDocument6 paginiInterview QuestionsSam_NimoÎncă nu există evaluări
- No Diagnosa Menurut Kki Level Kode Kode Diagnosa AskesDocument5 paginiNo Diagnosa Menurut Kki Level Kode Kode Diagnosa Askesashri hikmatullohÎncă nu există evaluări
- Icd 10 Excell NewDocument491 paginiIcd 10 Excell Newlilik fitriatulÎncă nu există evaluări
- Beyond Magenta Press ReleaseDocument3 paginiBeyond Magenta Press ReleaseCandlewick PressÎncă nu există evaluări
- FRENLE REVIE NP3 and NP4-1Document49 paginiFRENLE REVIE NP3 and NP4-1eric100% (1)
- Group Personal Accident Insurance Policy SummaryDocument13 paginiGroup Personal Accident Insurance Policy SummarySelvaraj Villy100% (1)