Documente Academic
Documente Profesional
Documente Cultură
Context Sensitive Airway Management
Încărcat de
Kavya AradhyaTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Context Sensitive Airway Management
Încărcat de
Kavya AradhyaDrepturi de autor:
Formate disponibile
EDITORIAL
Context-Sensitive Airway Management
Orlando Hung, MD, and Michael Murphy, MD
T he case presented by Mathew et al.1 in this issue of approach to the airway evaluation and management of
Downloaded from https://journals.lww.com/anesthesia-analgesia by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3I7ucIJ5GOrRpYM+K+I01f+cRsRyCGMRkYTkdxO1vmnOBFPy4RcQUfg== on 09/03/2019
Anesthesia & Analgesia presents us with an opportu- patients about to undergo an anesthetic. Although it is
nity to explore a broader view of difficult airway difficult to assess the true impact of these guidelines on
management: first, how a situation or context influences clinical outcomes, a recent review of the closed claims
our approach to the problem; second, the “unwritten truth” database showed that there are signs of improvement, with
of bronchoscopic intubation; and third, the importance of reduction in the number of adverse events (especially death
gas-exchange preservation over devices and techniques. and brain death) associated with airway management
In Chinese, the written word for “crisis,” “Wei Ji,” is misadventures.5 Unfortunately, this improvement was lim-
formed by combining 2 separate words: “Wei” or “danger” ited to the management of the airway on induction of
and “Ji” or “opportunity.” This combination most likely anesthesia, but not outside the operating room.5 Clearly,
originated from ancient teachings about how to live a life continuing efforts to increase awareness of the difficult
that thrives while responding to unpredictable mystical, airway and improve airway assessment and education,
political, and environmental forces. This frame of reference coupled with the enhancement of predictive and manage-
reflects a deep-seated philosophy of cultural survival. His- ment strategies, are crucial to the difficult airway manage-
tory provides a unique context that has resonance and ment approach in a controlled environment. The findings
reverberations in this day and age. In other words, al- of Peterson et al.5 also suggest that a broader understand-
though what we do today is often shaped by history and ing and approach to airway management is needed to
guided by evidence, our actions are frequently tempered by improve overall outcome.
the circumstances (or “context”) in which we act. It has During the last 2 decades, many new airway devices and
been said that we are in the midst of a medical-legal techniques have been developed, and these have changed
“crisis.” Perhaps, as the ancient Chinese did, we ought to the landscape of airway practice and management. In
seize this as an “opportunity,” though alert to the “danger” addition, there has been a major paradigm shift in airway
posed by this “crisis.” But in this modern context, the management, emphasizing gas exchange (ventilation and
“opportunity” is shaped by evidence rather than mystical, oxygenation) over tracheal intubation.6,7 Clinicians use
environmental, and political forces. only 4 methods of ventilation and oxygenation: a bag mask,
Caplan et al.2 first reported alarmingly poor outcomes an extraglottic device (e.g., a laryngeal mask airway), a
related to the management of the difficult airway in their tracheal tube, and a surgical airway.7 Selection of one of
review of the American Society of Anesthesiologists (ASA) these techniques to provide gas exchange depends not only
closed claims database in 1990. They reported that adverse on the devices best suited to the patient’s anatomy but also
outcomes associated with respiratory events constituted on the situation faced by the clinician. In other words,
the single largest class of injury, and litigation, in anesthesia in airway management is “context sensitive” in that it is
the United States (34%). The review also identified that most heavily dependent on the clinical situation and the envi-
of these airway management–related adverse respiratory ronment. If, for instance, a patient presents with a history or
outcomes were preventable. Recognizing that reversing clinical features predictive of an “impossible” tracheal
this finding was paramount to our specialty, the ASA intubation using a laryngoscope, and also possesses predic-
formed a task force to review the existing evidence and to tors of difficult bag-mask ventilation8,9 and difficulty in
recommend corrective airway management strategies. The using an extraglottic device, such as the laryngeal mask
ASA Difficult Airway Algorithm and Guidelines were airway,7 it would be prudent for the clinician in the setting
published in 19933 and subsequently revised in 2003.4 of an operating room to secure the airway awake, fre-
Although there are limitations to the recommendations, the quently utilizing a flexible fiberoptic bronchoscope. How-
ASA guidelines provide clinicians with an evidence-based ever, the management plan would be quite different if this
same patient required airway management in the prehos-
From the Department of Anesthesia, Dalhousie University, Queen Elizabeth pital setting, in the emergency department, or in the
II Health Sciences Centre, Halifax, Nova Scotia, Canada. magnetic resonance imaging suite where skill sets and
Accepted for publication January 8, 2010. limited resources play decisive roles. The selection of an
Address correspondence and reprint requests to Dr. Orlando Hung, Dal- airway approach might also be different if the patient
housie University, Queen Elizabeth II Health Sciences, Victoria General
Hospital, 1278 South Park St., Halifax, NS, Canada B3H 2Y9. requires immediate and rapid emergency airway interven-
Copyright © 2010 International Anesthesia Research Society tion, if the patient is a small child who is extremely
DOI: 10.1213/ANE.0b013e3181d48bbb uncooperative, or if the patient is pregnant. There are
982 www.anesthesia-analgesia.org April 2010 • Volume 110 • Number 4
Editorial
multiple situational modifiers that influence how the clini- with stridor. The mass was pedunculated, moving in and
cian approaches airway management. The availability of out of the glottic opening with each respiratory cycle. To
equipment, the expertise of available assistance, and the avoid inadvertent traumatic excision of the mass, with
skill sets of the airway practitioner are all “contextual possible displacement of the mass into the trachea during
modifiers” that can determine the approach to airway orotracheal intubation, Mathew et al. used 2 endoscopes to
management. These “modifiers” may be even more signifi- aid the tracheal intubation. One flexible bronchoscope was
cant considerations in a battlefield environment or in used to advance the ETT through the glottis while a second
developing countries. telelaryngoscope was used to observe and guide the ETT in
Stated another way, airway management is fundamen- such a manner that trauma to the pedunculated glottic
tally about gas exchange, not only about placing a tracheal mass was avoided.
tube by whatever chosen method. The technique used to This case serves to remind clinicians that tracheal intu-
assure gas exchange will be dictated largely by the clinical bation using a bronchoscope is not “direct-vision” intuba-
situation and circumstances of the environment. In many tion and great caution is needed to avoid trauma and other
situations, simply waking the patient or “cancelling the complications when a bronchoscope is used to intubate the
case” is not a realistic option, particularly in an emergency. trachea. This case also serves to remind clinicians that all
Context-sensitive airway management implies that airway devices have limitations. Successful outcomes in
managing a difficult or failed airway should be driven by airway management rely not only on the clinician’s knowl-
the principles of “gas exchange” and not be “device depen- edge of and skill in using the airway technique but also on
dent.” Clinicians must be trained to understand the basic the application of such airway management techniques in a
principles of airway management using basic techniques manner that recognizes the prevailing environment and
and learn how to apply these techniques properly in an circumstances. In other words, careful evaluation and in-
appropriate environment. Many clinicians believe that tra- terpretation of “context” are essential guides to safe airway
cheal intubation should always be performed under direct management practices.
vision and that there is no place for nonvisual or “blind” In summary, we wish to make 2 points:
techniques of airway management. Unfortunately, in many 1. Airway management is context sensitive, and
clinical situations, tracheal intubation under direct vision is 2. Gas exchange is a fundamental principle of airway
not possible for a variety of reasons, such as large management.
amounts of blood in the oropharynx. Even devices that “see
around corners,” such as videolaryngoscopes, are not per- A change in airway management focus from “devices
fect. Although visualization of the glottis may be relatively and techniques” to the “preservation of gas exchange” is
easy, placement of an endotracheal tube (ETT) under the crucial. To cling to traditional ways of thinking is to be
indirect vision provided by these devices is often more overwhelmed by the “Wei,” the danger, of a crisis, and to
difficult than under direct vision. miss the “Ji,” the opportunity, to better serve the needs of
More importantly, the clinician may select an inappro- patients in that crisis. Rather than being buffeted by mys-
priate device because of a misunderstanding of how the tical, political, or environmental forces, we must seize the
device works. For example, it would be inappropriate to opportunity to recognize and welcome a new era: context-
use a lightwand intubation technique in a morbidly obese sensitive airway management.
patient when transillumination of the neck tissues is pre-
dicted to be poor. Similarly, it is a mistake to assume that REFERENCES
performing flexible bronchoscopic intubation is a “direct- 1. Mathew JS, Padhy S, Lata S, Balachander H, Gopalakrishnan S.
Intralaryngeal rhinosporidiosis. Anesth Analg 2010;110:1066 – 8
vision” technique equivalent to laryngoscopic visualization 2. Caplan RA, Posner KL, Ward RJ, Cheney FW. Adverse respira-
of the glottis. The clinician using the flexible bronchoscope tory events in anesthesia: a closed claims analysis. Anesthesiol-
for intubation visualizes the glottic opening indirectly via a ogy 1990;72:828 –33
camera or through fiberoptic bundles and passes the tip of 3. Practice guidelines for the difficult airway. A report by the Ameri-
the bronchoscope into the tracheal lumen positioning the can Society of Anesthesiologists Task Force on Management of the
Difficult Airway. Anesthesiology 1993;78:597– 602
tip just short of the carina. Negotiating the ETT over the 4. American Society of Anesthesiologists Task Force on Manage-
bronchoscope into the trachea is done blindly; the broncho- ment of the Difficult Airway. Practice guidelines for manage-
scope serves merely as an “intubating guide,” much like an ment of the difficult airway: an updated report by the American
Eschmann tracheal introducer or “bougie.” Although the Society of Anesthesiologists Task Force on Management of the
Difficult Airway. Anesthesiology 2003;98:1269 –77
bronchoscope can be used to confirm the location of the tip 5. Peterson GN, Domino KB, Caplan RA, Posner KL, Lee LA,
of the ETT after the tube placement, at no time during the Cheney FW. Management of the difficult airway: a closed claims
insertion of the ETT over the bronchoscope can the tip of analysis. Anesthesiology 2005;103:33–9
the ETT be visualized by the operator. As a result, tracheal 6. Murphy M, Hung O, Launcelott G, Law JA, Morris I. Predicting
intubation using a flexible bronchoscope should be used the difficult laryngoscopic intubation: are we on the right track?
Can J Anaesth 2005;52:231–5
with great caution in patients with upper airway lesions, 7. Hung O, Murphy M. Changing practice in airway management:
such as retropharyngeal abscess, pedunculated polyps or are we there yet? Can J Anaesth 2004;51:963– 8
tumors at the glottis, and foreign bodies in the upper 8. Kheterpal S, Martin L, Shanks AM, Tremper KK. Prediction and
airway. outcomes of impossible mask ventilation: a review of 50,000
anesthetics. Anesthesiology 2009;110:891–7
Mathew et al.,1 in this issue of Anesthesia & Analgesia, 9. Langeron O, Masso E, Huraux C, Guggiari M, Bianchi A, Coriat
illustrate this principle. They reported the management of a P, Riou B. Prediction of difficult mask ventilation. Anesthesiol-
patient with intralaryngeal rhinosporidiosis presenting ogy 2000;92:1229 –36
April 2010 • Volume 110 • Number 4 www.anesthesia-analgesia.org 983
S-ar putea să vă placă și
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Case 4Document5 paginiCase 4angelica dizonÎncă nu există evaluări
- The Science of SingingDocument18 paginiThe Science of SingingK100% (2)
- Case StudyDocument49 paginiCase StudyLennie Marie B Pelaez100% (1)
- Version Structures and Functions of Living Organisms 8.L.1.1Document28 paginiVersion Structures and Functions of Living Organisms 8.L.1.1Marianna HernandezÎncă nu există evaluări
- Ectoparasites Killed by Kle and Nco Soap: Kakawate (Gliricidia Sepium) LeafDocument2 paginiEctoparasites Killed by Kle and Nco Soap: Kakawate (Gliricidia Sepium) LeafRyan Bacarro BagayanÎncă nu există evaluări
- Worksheet 8Document2 paginiWorksheet 8Jocel OclaritÎncă nu există evaluări
- Encephalitis ChildDocument8 paginiEncephalitis ChildJeane SuyantoÎncă nu există evaluări
- J.N. Hays - The Burdens of Disease - Epidemics and Human Response in Western History, Revised Edition (2010) PDFDocument391 paginiJ.N. Hays - The Burdens of Disease - Epidemics and Human Response in Western History, Revised Edition (2010) PDFMarry Lim100% (4)
- PeritonitisDocument21 paginiPeritonitischrisyenÎncă nu există evaluări
- CPG On CTGDocument5 paginiCPG On CTGТони ДиасÎncă nu există evaluări
- Pediatric Drug Dosage - All in One PDFDocument15 paginiPediatric Drug Dosage - All in One PDFHuang Hasjim33% (9)
- CSOMDocument29 paginiCSOMsuciÎncă nu există evaluări
- Handout and Questions of HysterosalpingDocument12 paginiHandout and Questions of Hysterosalpingahmad shaltout100% (2)
- Reflexology Intake FormDocument1 paginăReflexology Intake FormJael PistioÎncă nu există evaluări
- The Infant of An Addicted MotherDocument15 paginiThe Infant of An Addicted Mothernursereview100% (8)
- BMJ 46330 Original - Research KayaDocument8 paginiBMJ 46330 Original - Research KayaBerry BancinÎncă nu există evaluări
- Poultry Diseases and Their TreatmentDocument159 paginiPoultry Diseases and Their TreatmentAbubakar Tahir Ramay67% (12)
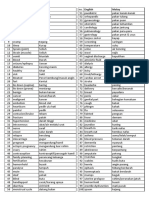
- Medic Term English MalayDocument1 paginăMedic Term English MalaySyamimi SuhaimiÎncă nu există evaluări
- NCM 101 Health AssessmentDocument7 paginiNCM 101 Health AssessmentCristoper Bodiongan100% (1)
- Bites by Crotalinae Snakes (Rattlesnakes, Water Moccasins (Cottonmouths), or Copperheads) in The United States - Management - UpToDateDocument19 paginiBites by Crotalinae Snakes (Rattlesnakes, Water Moccasins (Cottonmouths), or Copperheads) in The United States - Management - UpToDateAlin VázquezÎncă nu există evaluări
- Medical Aptitude and Its AssessmentDocument9 paginiMedical Aptitude and Its AssessmentMINU MARY MATHEW 1444603Încă nu există evaluări
- BPT Notes Applied PsychologyDocument36 paginiBPT Notes Applied PsychologyVivek Chandra0% (1)
- AMSTAR-2 ChecklistDocument10 paginiAMSTAR-2 ChecklistMuammar EmirÎncă nu există evaluări
- Perioperative Care For CABG PatientsDocument32 paginiPerioperative Care For CABG PatientsAya EyadÎncă nu există evaluări
- Hubungan Ketepatan Penulisan Informasi Diagnosis Dengan Keakuratan Kode Diagnosis Kasus Obstetry Di Rumah Sakit Umi Barokah BoyolaliDocument5 paginiHubungan Ketepatan Penulisan Informasi Diagnosis Dengan Keakuratan Kode Diagnosis Kasus Obstetry Di Rumah Sakit Umi Barokah BoyolaliirmasariÎncă nu există evaluări
- Case ScenarioDocument1 paginăCase ScenarioIrish Eunice FelixÎncă nu există evaluări
- Use of "Zingiber Officinale Roscoe L" Root in Various DiseasesDocument8 paginiUse of "Zingiber Officinale Roscoe L" Root in Various DiseasesCentral Asian StudiesÎncă nu există evaluări
- Baxter (Flo-Gard 6201) Volumetric Infusion Pump Flow Rate Accuracy - Test Design and Performance VerificationDocument21 paginiBaxter (Flo-Gard 6201) Volumetric Infusion Pump Flow Rate Accuracy - Test Design and Performance VerificationKousha TalebianÎncă nu există evaluări
- Workcover Guides Evaluation Permanent Impairment 3rd Edition 0970Document104 paginiWorkcover Guides Evaluation Permanent Impairment 3rd Edition 0970workcovervictim8242Încă nu există evaluări
- Patient'S Bill of Rights: MedsurgDocument3 paginiPatient'S Bill of Rights: MedsurgIvy VillalobosÎncă nu există evaluări