Documente Academic
Documente Profesional
Documente Cultură
Cardiovascular System Adaptation at Birth
Încărcat de
gita novaTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Cardiovascular System Adaptation at Birth
Încărcat de
gita novaDrepturi de autor:
Formate disponibile
SYMPOSIUM: CARDIOVASCULAR MEDICINE
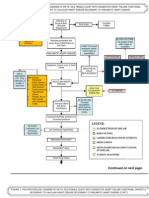
Cardiovascular system The fetal cardiovascular system
The cardiovascular system is the first to function in the
adaptation at birth embryo, with blood beginning to circulate by the end of the
third week when heart contractions begin. The myocardium
Joanna Berhrsin continues to grow by progressive cell division until birth and
cardiac contractility steadily improves over the second half of
Alan Gibson
pregnancy. An effective functional circulation is maintained by
the presence of three shunts in the fetal cardiovascular system;
the ductus venosus, ductus arteriosus and foramen ovale
Abstract (Figure 1). In addition the presence of fetal haemoglobin means
Due to the presence of fetal haemoglobin and the patency of anatomical that the organs in the fetus are able to extract oxygen at low
shunts the fetal circulation is perfectly adapted to intrauterine life, utilizing saturations. Relatively oxygenated blood leaves the placenta
the placenta as the organ of gas exchange. Immediate adaptation must through the umbilical vein and passes through the ductus
occur at birth as the lungs take over this role. Initially the pulmonary vascular venosus into the inferior vena cava. It then enters the right side
resistance is high but pulmonary blood flow progressively increases in the of the heart and traverses the foramen ovale in the inter-atrial
newborn due to vasodilatation as a consequence of increased oxygenation septum to reach the left ventricle from which it is pumped
and activation of pulmonary stretch receptors. Changes in the pulmonary through the aorta to feed the coronary circulation and the
vasculature are mediated through a number of vasoactive substances, major body organs. Deoxygenated blood passes through the
including nitric oxide. Increased pulmonary blood flow leads to an increase caval veins into the right side of the heart where there is some
in left atrial pressure with subsequent closure of the foramen ovale. mixing in the right atrium before blood either passes through
In some babies this normal adaptation fails and persistent fetal circula- the foramen ovale to the left atrium or through the tricuspid
tion may develop, leading to the symptoms of persistent pulmonary hyper- valve to the right ventricle. High pulmonary vascular resistance
tension of the newborn. The mainstay of treatment is to maximize results in the majority of the blood that leaves the right
oxygenation by use of an appropriate ventilatory strategy and to maintain ventricle being preferentially shunted through the ductus arte-
blood pH within normal range using inotropic support as indicated to sustain riosus into the aorta. The amount of blood entering the
an adequate systemic blood pressure. Nitric oxide has proved to be pulmonary circulation varies during pregnancy, increasing
an extremely effective treatment for this condition in some cases but from around 13% of the combined cardiac output at mid-
ECMO may be required as a rescue therapy. Persistent pulmonary hyperten- gestation to around 25% after 30 weeks. The ductus arteriosus
sion of the newborn still carries a 10e20% mortality rate despite modern bypasses the pulmonary circulation and the different imped-
intervention. ance between the pulmonary vasculature and the ductal
circulation results in the majority of blood remaining in the
Keywords hypertension, pulmonary, of newborn, persistent; infant, systemic circulation. This is under the control of prostacyclin
newborn; persistent fetal circulation syndrome; physiology, cardiovascular (PGI2).
Oxygen saturations in different parts of the fetal circulation
are shown in Table 1. It is of interest to note that the difference in
oxygen saturations between the blood leaving the left and right
ventricles is only 10%, increasing to 12% during hypoxaemia.
Introduction This is a reflection of the large volume of blood that is shunted
through the foramen ovale.
In order to understand how, at birth, the cardiovascular system In the mature circulation, where no intracardiac shunting
of the fetus adapts to that of baby, it is important to appreciate takes place, the stroke volume of the right ventricle should equal
how the two systems differ in design and function. This also that of the left ventricle. In the fetus the two ventricles pump in
permits an understanding of the mechanisms of the pathological parallel and the right ventricle is responsible for the majority of
processes that result in a failure of this normal adaptive process the cardiac output, pumping blood into the pulmonary artery
and the clinical presentations that are not infrequently encoun- with the majority then passing through the ductus arteriosus to
tered in neonatal practice. enter the descending aorta and supply the lower body and
This article will review the normal cardiovascular system of placenta. Blood enters the left ventricle through the foramen
the fetus and of the newborn infant and address the means by ovale and left atrium and is pumped into the ascending aorta to
which birth leads to transition. It will also address what happens supply the cerebral and coronary circulations. This blood is more
when the adaptive processes at birth do not progress normally. oxygenated than that in the descending aorta, hence facilitating
the delivery of oxygen to the tissues that require it most. In
contrast to the mature heart, where the left ventricle is thicker
Joanna Berhrsin MBChB MRCPCH is a Neonatology Specialist Registrar in
than the right, the comparative thickness of the fetal ventricles is
the Jessop Wing, Sheffield Teaching Hospitals NHS Foundation Trust,
similar. This results in a minimal pressure difference between left
Tree Root Walk, Sheffield S10 2SF, UK. Conflict of interest: none.
and right ventricles in contrast to the significant gradient
observed in postnatal life.
Alan Gibson MB BS BSc PhD FRCP FRCPCH is a Consultant Neonatologist in
The ability of the fetal heart to alter stroke volume according to
the Jessop Wing, Sheffield Teaching Hospitals NHS Foundation Trust,
preload is impaired when compared to the mature heart. The fetal
Tree Root Walk, Sheffield S10 2SF, UK. Conflict of interest: none.
PAEDIATRICS AND CHILD HEALTH 21:1 1 Ó 2010 Elsevier Ltd. All rights reserved.
Downloaded from ClinicalKey.com at Universitas Gadjah Mada January 20, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
SYMPOSIUM: CARDIOVASCULAR MEDICINE
Figure 1 Schematic diagram of the fetal circulation.
myocardium is relatively “stiff” and there is limited capacity to to ongoing angiogenesis in the pulmonary circulation rather than
increase stroke volume in response to an increase in diastolic being due to changes in individual vessels.
filling. In the mature heart, early passive ventricular diastolic
filling occurs prior to active atrial contraction but this is impaired Normal physiological adaptation of the term baby at birth
in the fetus and active atrial contraction is primarily responsible
Normal birth is associated with major and very important changes
for ventricular filling. Fetal stroke volume may be limited due to
in the cardiovascular system as both the cardiovascular and respi-
a number of possible mechanisms. The myocardial architecture is
ratory system adapt to extra-uterine life (Figure 2). The lungs must
immature and is likely to exhibit poor compliance and there is
swiftly take over from the placenta as the site of gas exchange, the
likely to be a degree of extrinsic compression of the fetal heart due
shunts present in the fetus must close and left ventricular output
to restricted movement of the chest wall and the collapsed fluid
must increase so as to ensure that blood oxygenated by the lungs is
filled lungs. Limitation of movement by the pericardium has been
delivered to the tissues by an efficient and effective systemic
postulated as an additional contributory factor. Lung inflation at
circulation. Although pulmonary vascular resistance (PVR) has
birth and clearance of lung liquid may lead to an increase in left
gradually fallen in late gestation it is still comparatively high at the
ventricular preload and the improvement in stroke volume that is
time of birth but must decrease further dramatically and rapidly
seen in the newborn. As the fetus nears term there is a gradual
following separation from the placental circulation. This may result
reduction in pulmonary vascular resistance. This is thought to be
from interaction of a number of factors. The first breaths to inflate
the result of an increased surface area of the vascular bed related
the lungs are thought to stimulate pulmonary stretch receptors
which mediate reflex dilatation of the pulmonary vessels, and
improved oxygenation of the blood also contributes to a reversal of
Oxygen saturations in the fetal circulation pulmonary vasoconstriction and a reduction in PVR. The reduction
in pulmonary vascular resistance leads to increased venous return
Vessel Oxygen saturation from the lungs and a greater volume of blood entering the left
Umbilical vein 80e90% atrium. As blood flow from the placenta reduces e either by normal
Ascending aorta 65% physiological mechanisms or by cord clamping e blood flow
Descending aorta 60% through the ductus venosus and into the inferior vena cava is
Pulmonary artery 55% reduced. This in turn means that less blood enters the right atrium.
Superior vena cava 45% These factors lead to equalization of left and right atrial pressures
Inferior vena cava 35% and closure of the atrial connection as the flap of the foramen ovale
pushes against the atrial septum and become adherent. This initial
Table 1 “functional” closure generally happens within the first few hours
PAEDIATRICS AND CHILD HEALTH 21:1 2 Ó 2010 Elsevier Ltd. All rights reserved.
Downloaded from ClinicalKey.com at Universitas Gadjah Mada January 20, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
SYMPOSIUM: CARDIOVASCULAR MEDICINE
muscle cells and results in smooth muscle relaxation and arteriolar
vasodilation. The pathway involves the activation of guanylate
Fetal cyclase leading to the conversion of GTP to cyclic GMP (Figure 4).
circulation Changes in the activity of cyclo-oxygenase (COX) also appear to be
involved in adaptation. After birth there is an inhibition of COX-2
enzyme pathways leading to a reduction in levels of thromboxane
and in the amount of arteriolar vasoconstriction it may cause. In
Pulmonary addition, inhibition of vascular endothelial growth factors leads to
Lung vascular an inhibition of smooth muscle proliferation. In animal models it
inflation resistance
falls has been shown that prostaglandin synthesis changes with
Pulmonary advancing gestation. In early gestation there is a predominance of
blood PGFa2, a vasoconstrictor prostaglandin, while nearer term the pre-
flow dominating prostaglandins are those that are primarily vasodilating
increases such as PGI2 and PGE2. The normal cardiovascular transition that
Left
Shunt atrial occurs at birth discussed above is also reliant on a number of
Closure* pressure hormonal influences if it is to progress smoothly. Corticosteroids
increases are known to play a central role in successful neonatal adaptation
and endogenous levels rise as the fetus approaches term levels, and
appear essential for pulmonary and cardiovascular adaptation at
*Shunt closure due to: birth. Incomplete cardiopulmonary adaptation may therefore occur
Neonatal • Reduced venous return to right atrium in the preterm, especially if inadequate maternal antenatal steroids
circulation • Closure of ductus arteriosus due to
increased PaO2 and decreased PGE2 have been administered. Thyroid hormones and catecholamines
also have a role in ensuring that this transition takes place and
recent evidence suggests that leptin may also be involved. Evidence
Figure 2 Summary of mechanisms leading to transition from fetal to for this has been derived from studies on large for gestational age
neonatal circulation. babies from both diabetic and non-diabetic mothers.
Echocardiography studies have clearly demonstrated the
after birth. The same physiological principle is evident in newborn changes that occur in the transitional circulation. In one study
resuscitation when sustained inflation breaths given to the apnoeic the pulmonary artery pressure was shown to fall rapidly in the
infant at birth bring about lung inflation and a reduction in PVR, first 30 hours in term newborns and normally leads to ductal
precipitating the rest of the cardiopulmonary adaptive cascade that closure. However, the fall in preterm babies was slower and
characterizes the transformation from fetus to newborn. As these
changes happen, blood flow through the ductus arteriosus becomes
bidirectional and steadily reduces as the duct closes. This closure is
brought about by smooth muscle constriction related to increased
Vascular endothelial cell
oxygenation and by a reduction in levels of prostaglandin E2.
Functional closure of the three shunts typically happens in the first Bradykinin L-arginine + Oxygen + NADPH
48 hours and is followed by tissue proliferation that results in
anatomical closure and formation of the ligamentum arteriosus and
ligamentum venosus, while fusion of the inter-atrial septum pri-
Calcium
mum and septum secundum results in formation of an intact atrial Acetylcholine Cofactors
partition. Remnants of the closed umbilical vein are enclosed within Nitric oxide
the ligamentum teres. synthase
The changes in the pulmonary arteriolar lumen diameter are
under the control of several vasoactive chemicals and are summa- Shear stress Citrulline + Nitric Oxide + NADP
rized in Figure 3. Bradykinin has been shown to be released
following oxygenation of the lungs. Studies have shown that
exposure to oxygen in mature fetal lambs was associated with an
increase in bradykinin and a reduction of the precursor kininogen in
the bloodstream which did not occur in lambs when the lung was Nitric oxide
exposed to nitrogen. The increase in bradykinin then appears to
operate by stimulating the influx of calcium into endothelial cells, GTP cGMP
an essential stage in the pathway of nitric oxide production. There is
increasing activity of endothelial nitric oxide synthase (NOS) during Smooth Muscle relaxation
the third trimester, and at birth there is upregulation of nitric oxide
synthase activity, probably as a direct consequence of the increased Vascular smooth muscle
oxygenation associated with lung inflation. This enzyme acts as
a catalyst in the production of nitric oxide from arginine in endo- Figure 3 The role of vasoconstrictors and vasodilators in the control of
thelial cells and the nitric oxide produced diffuses into smooth pulmonary vascular resistance.
PAEDIATRICS AND CHILD HEALTH 21:1 3 Ó 2010 Elsevier Ltd. All rights reserved.
Downloaded from ClinicalKey.com at Universitas Gadjah Mada January 20, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
SYMPOSIUM: CARDIOVASCULAR MEDICINE
ventilation and ECMO that PPHN often requires. Some babies
may be more susceptible to the development of PPHN and the
three principal proposed aetiologies are detailed in Table 2.
Fetus Neonate A number of studies have addressed the causation of PPHN
and several factors have been identified. Many, including babies
born post dates, non-vertex presentations, fetal distress during
labour, meconium staining leading to meconium aspiration
Vasoconstrictors
Vasoconstrictors syndrome, neonatal sepsis and pneumonia are well recognized
• Endothelin 1 ↓
• Endothelin 1 ↑ while other less well recognized factors include delivery by
• Thromboxane ↓
caesarian section and late preterm as well as post dates deliv-
eries. Ethnicity has been shown to be relevant as incident is
reported to be higher in babies of black or Asian race. Maternal
Vasodilators Vasodilators
health may have an impact on the development of PPHN as the
• Nitric oxide ↓ • Nitric oxide ↑
condition is encountered more commonly in babies born to
• Prostaglandin I2 ↓ • Prostaglandin I2↑
mothers who were overweight or who had diabetes or asthma.
The molecular basis of PPHN appears multifactorial and
complex. Inflammatory cytokines, cyclo-oxygenase pathway
Increased Reduced metabolites and thromboxane all appear to have the potential to
pulmonary pulmonary
vascular vascular contribute to the development of PPHN. During direct lung injury or
resistance resistance sepsis there is an immediate rise in inflammatory cytokines,
particularly TNF-a, IL-1b, IL-6 and IL-10. This rise may lead to
contraction of arteriolar smooth muscle and proliferation of smooth
muscle. Thromboxane A2, a potent vasoconstrictor, is also impli-
cated in the pathophysiology of PPHN due to sepsis. Hypoxia causes
Figure 4 The pathway of nitric oxide production in endothelial cells. diminished COX-1 and prostacyclin synthase activity and inhibition
of other metabolizing pathways that in turn leads to the production
of more thromboxane from arachidonic acid. Hypoxia may also
often incomplete and it is well recognized that the shunts which
lead to sensitization of the smooth muscle myocytes to the effects of
usually close shortly after birth may persist for a significantly
thromboxane A2 and increased vascular reactivity when compared
longer period of time in a preterm infant. The combination of
to normoxia. Hypoxia induced endothelial dysfunction results in
structural and hormonal immaturity may contribute to a delay in
increased production of endothelin that also acts a vasoconstrictor.
the fall in pulmonary artery pressure after preterm birth which
In addition hypoxia leads to an inhibition in endogenous nitric
has obvious clinical implications. The presence of a persistent
oxide production due to a reduction in the activity of nitric oxide
ductus arteriosus may have an impact on the clinical course of
synthase and is also implicated in a reduced sensitivity of smooth
a preterm infant and often leads to deliberations over medical or
muscle to nitric oxide. The summation of the effects of all these
surgical closure e an area that remains a cause of much debate.
mechanisms is an increase in pulmonary arteriolar tone and the
development of pulmonary hypertension. Considering the patho-
When physiological adaptation goes wrong-persistent
physiology of this condition and the common pathway of nitric
pulmonary hypertension of the newborn
Persistent pulmonary hypertension of the newborn (PPHN) is
said to affect 0.1e0.2% of all births each year. In some cases
a definite causative factor is implicated but in many such factors
cannot be identified. Whatever the cause may be the underlying
mechanism of this condition appears to be that the pulmonary
arterioles remain very active in the neonate and can undergo Hypoxia
profound vasoconstriction in response to a variety of stimuli and acidosis
such as hypoxia, acidosis, hypercarbia and cold. The vasocon-
striction is sufficiently severe to result in a large rise in pulmo-
nary vascular resistance which leads to right to left shunting Right to left Pulmonary
through the ductus arteriosus and foramen ovale. The reduced shunting of blood vasoconstriction
pulmonary flow worsens the hypoxia and leads to a perpetuating
cycle of increasing PVR and worsening hypoxia and acidosis if no
Increased
intervention takes place (Figure 5). Even despite interventions
pulmonary vascular
such as inhaled nitric oxide and ECMO, PPHN still has resistance
a mortality of 10e20%. Survivors of PPHN may have consider-
able morbidity due to chronic lung disease, seizures and neuro-
developmental problems. Increased morbidity is in part a result
of the hypoxaemia relating to the underlying condition but may Figure 5 The perpetuating cycle of persistent pulmonary hypertension of
also be related to the nature of treatments such as high pressure the newborn.
PAEDIATRICS AND CHILD HEALTH 21:1 4 Ó 2010 Elsevier Ltd. All rights reserved.
Downloaded from ClinicalKey.com at Universitas Gadjah Mada January 20, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
SYMPOSIUM: CARDIOVASCULAR MEDICINE
Pulmonary perfusion will be affected by systemic perfusion and
The aetiology of PPHN the magnitude of the persisting right to left shunt and hypoten-
sion should be investigated and treated by whatever strategy is
Pathological basis Mechanism and examples indicated by the apparent causation. Maintaining an adequate
Pulmonary hypoplasia Abnormal development of both blood pressure to sustain pulmonary perfusion will not infre-
respiratory and vascular components quently require inotropic support. A ventilatory strategy should
of the lung may lead to very severe be chosen that will ensure maximal oxygenation while mini-
and often unresponsive pulmonary mizing potential lung trauma. High frequency oscillation can be
hypertension. Significant component useful in these babies, both alone and in combination with
of many cases with congenital inhaled nitric oxide. Therapies which reduce right to left shunt-
diaphragmatic hernia or long ing through a direct vasodilatory effect on the pulmonary circu-
standing oligo/anhydramnios. lation without having a similar effect on the systemic circulation
Increased muscularisation Typically considered to be the are the mainstay of treatment of severe cases and such selective
of pulmonary arterioles basis of idiopathic PPHN where mechanisms have only become available relatively recently. In
increased muscularisation of the the past, several comparatively non-selective vasodilator drugs
pulmonary arterioles occurs due have been used. These included tolazoline, prostacyclin and
to congenital remodelling of the magnesium sulphate, with tolazoline being the most commonly
pulmonary vasculature. used medication in routine practice and reportedly being effec-
Maladaptation to The circulation comprises the usual tive in treating between 25 and 50% of babies with this condi-
circulatory transition number of arterioles with an tion. It is not a selective pulmonary vasodilator however, and
appropriate degree of muscularisation. systemic hypotension can be a commonly encountered side
Circulatory maladaptation is thought effect, so common in fact that many practitioners believed that in
to be due to a reduction in the absence of a fall in systemic blood pressure there was
production of, or responsiveness to, unlikely to be an appreciable fall in pulmonary vascular resis-
vasodilators such as nitric oxide and tance. Prostacyclin in doses of 5e40 ng/kg/min has also been
prostacyclin. Compounded by an used and at times could be an effective pulmonary vasodilator.
increase in production and However, prostacyclin was also not selective for the pulmonary
responsiveness of pulmonary circulation and there was an extensive list of serious side-effects
vasoconstrictors. This is thought and this combination meant that usage was limited. Magnesium
to be the primary pathological sulphate can be a potent vasodilator and limited trial evidence
mechanism in developmental suggested that it could be useful in PPHN. Responses were rarely
immaturity, meconium aspiration dramatic and usage was sporadic, favoured by some practitioners
syndrome or sepsis. and never considered by others.
The current mainstay drug of treatment is Nitric Oxide, admin-
Table 2 istered as an inhaled gas delivered at extremely low concentrations
through the ventilation system. As endogenous nitric oxide plays
a pivotal role in maintenance of vascular tone and local production
oxide synthesis it is not surprising that the administration of is reduced in PPHN there is a logical expectation that inhaled nitric
exogenous inhaled nitric oxide is an effective treatment in many oxide may restore the balance between production and metabolism,
cases. This is not always the case however and it is apparent that and administration has been shown to improve the outcome in term
endothelial dysfunction is not the whole story in some cases of and near-term hypoxaemic infants. Infants treated with nitric oxide
PPHN. This is not entirely surprising considering the multiple are less likely to require ECMO for the treatment of this condition
factors that may be involved in causation, and the multiple path- although mortality is similar for the two modalities. In babies with
ways that may be invoked in pathogenesis. Unsurprisingly, some PPHN secondary to an underlying diaphragmatic hernia and
babies with this condition do not respond to nitric oxide therapy and pulmonary hypoplasia there is no apparent benefit and no
it seems likely that this group may have abnormal function of improvement in outcome. In addition, in infants who survive PPHN
smooth muscle rather than endothelial dysfunction and in some there is no difference in neuro-developmental outcome when
cases developmental pathways have been affected in such a way as comparing those who received treatment with those who did not,
to make changes irreversible and unresponsive to available and long-term morbidity is not inconsiderable. Approximately 30%
medications. of babies with PPHN fail to respond to inhaled nitric oxide. There is
limited evidence that phosphodiesterase inhibitors such as silde-
nafil or milrinone may be useful pulmonary vasodilators as there
The management of PPHN
are high concentrations of phosphodiesterase in the pulmonary
The management of PPHN involves various treatment modalities vasculature. There is currently insufficient evidence to recommend
where the primary aim is to break the perpetuating cycle of the routine use of sildenafil instead of the current gold standard of
hypoxia, acidosis, vasoconstriction and shunting. In animal nitric oxide. Both may be useful as adjunctive treatment or to aid
models acidosis has been shown to contribute substantially to weaning from inhaled nitric oxide therapy and usage is slowly
pulmonary vasoconstriction, and management should include increasing, fuelled primarily by anecdote as opposed to clinical trial
actions to normalize acid base balance where possible. evidence. If any of these medical treatment strategies are ineffective
PAEDIATRICS AND CHILD HEALTH 21:1 5 Ó 2010 Elsevier Ltd. All rights reserved.
Downloaded from ClinicalKey.com at Universitas Gadjah Mada January 20, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
SYMPOSIUM: CARDIOVASCULAR MEDICINE
then ECMO is a useful rescue but there are concerns that attempts to Kiserud T. Physiology of the fetal circulation. Semin Fetal Neonatal Med
reverse PPHN by sequential use of different ventilation strategies 2005; 10: 493e503.
and medical treatments may substantially delay referral for ECMO. Kopelman AE, Moise AA, Holbert D, et al. A single very early dexameth-
There is some evidence to suggest that the morbidity and mortality asone dose improves respiratory and cardiovascular adaptation in
of ECMO are directly influenced by the length of time that has preterm infants. J Pediatr 1999; 135: 345e50.
elapsed before the treatment is commenced. Moore KN, Persaud TVL. The developing human: clinically oriented
Persistent pulmonary hypertension of the newborn remains embryology. 6th Edn. WB Saunders, 2008.
a rare but potentially disastrous complication of normal birth. It not Murphy PJ. The fetal circulation. Contin Educ Anaesth Crit Care Pain 2005;
uncommonly occurs in babies where there are no or minimal 5: 107e12.
specific risk factors and may progress rapidly and insidiously. Each Rudolph AM. Fetal and neonatal pulmonary circulation. Annual Review
year a significant number of babies with no other serious problems Physiology 1979; 41: 383e95.
die from this potentially reversible condition. Early diagnosis and Rychik J. Fetal cardiovascular physiology. Pediatr Cardiol 2007; 25:
swift and appropriate treatment in centres used to the different 201e9.
treatment modalities are the mainstay of management and in those Shah PS, Ohlsson A. Sildenafil for pulmonary hypertension in neonates.
who do not respond swiftly to such treatment early transfer for Cochrane Database Syst Rev 2007; (3): Art. No.: CD005494.
ECMO may be life saving. A Sinha SK, Donn SM. Fetal-to-neonatal maladaptation. Semin Fetal
Neonatal Med 2006; 11: 166e73.
Thérèse P. Persistent pulmonary hypertension of the newborn. Paediatr
FURTHER READING Respir Rev 2006; 7(suppl 1): S175e6.
Dakshinamurti S. Pathophysiologic mechanisms of persistent pulmonary Vela-Huerta M, Aguilera-López A, Alarcón-Santos S, et al. Cardiopulmo-
hypertension of the newborn. Pediatr Pulmonol 2005; 39: 492e503. nary adaptation in large for gestational age infants of diabetic and
Evans NJ, Archer LN. Postnatal circulatory adaptation in healthy term and nondiabetic mothers. Acta Paediatr 2007; 96: 1303e7.
preterm neonates. Arch Dis Child 1990; 65: 24e6.
Finer NN, Barrington KJ. Nitric oxide for respiratory failure in infants born at
or near term. Cochrane Database Syst Rev 2006; (4): Art. No.: CD000399.
Ganong WF. Review of medical physiology. In: Lange basic science. 23rd Key learning points
Edn. McGraw Hill, 2009.
Greenough A, Milner AD. Persistent pulmonary hypertension. In: C Normal cardiovascular adaptation involves a complex inter-
Rennie JA, ed. Roberton’s textbook of neonatology. 4th Edn. Elsevier action of many factors.
Ltd, 2005. C Many different factors may contribute to failure of normal
Hernandez-Diaz S, Van Marter LJ, Werler MM, et al. Risk factors for adaptation.
persistent pulmonary hypertension of the newborn. Pediatrics 2007; C PPHN may have an insidious onset and develop rapidly.
120: e272e82. C Affected infants may be very unstable at the time of presentation.
Hinton M, Mellow L, Halayko AJ, et al. Hypoxia induces hypersensitivity C Treatment should be initiated as early as possible and
and hyperreactivity to thromboxane receptor agonist in neonatal increased rapidly as indicated.
pulmonary arterial myocytes. Am J Physiol Lung Cell Mol Physiol 2006; C Treatment should address both underlying pathophysiology
290: L375e84. and systemic support.
Ho JJ, Rasa G. Magnesium sulfate for persistent pulmonary hypertension of
the newborn. Cochrane Database Syst Rev 2007; (3): Art. No.: CD005588.
PAEDIATRICS AND CHILD HEALTH 21:1 6 Ó 2010 Elsevier Ltd. All rights reserved.
Downloaded from ClinicalKey.com at Universitas Gadjah Mada January 20, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- BIO271 - Practice MCQDocument6 paginiBIO271 - Practice MCQEric LuongÎncă nu există evaluări
- RudrakshaDocument8 paginiRudrakshaSamhitha Ayurvedic ChennaiÎncă nu există evaluări
- DMLS Curricula PDF-1Document28 paginiDMLS Curricula PDF-1Muhammad umarÎncă nu există evaluări
- Blood Pressure PosterDocument1 paginăBlood Pressure Posterapi-385956544Încă nu există evaluări
- Cardiac Cycle JVPDocument70 paginiCardiac Cycle JVPAstrid PramudyaaÎncă nu există evaluări
- NCLEX Practice Questions With RationaleDocument196 paginiNCLEX Practice Questions With RationaleKharen Herrera88% (8)
- Adi Bestara EKG at A Glance NewestDocument113 paginiAdi Bestara EKG at A Glance Newestkarpax21100% (1)
- Chapter 3 - Physical Activity FitnessDocument44 paginiChapter 3 - Physical Activity FitnessSharmila KrishnaswamyÎncă nu există evaluări
- Pathophysiology of Congestive Heart FailureDocument2 paginiPathophysiology of Congestive Heart FailureAnonymous XvwKtnSrMR100% (10)
- Life ProcessesDocument36 paginiLife Processes2erwr100% (1)
- 12 Drugs Acting On The Cardiovascular SystemDocument5 pagini12 Drugs Acting On The Cardiovascular SystemJAN CAMILLE LENONÎncă nu există evaluări
- Zoghbi ASE Guidelines MR AR FINAL - Updated - 0Document34 paginiZoghbi ASE Guidelines MR AR FINAL - Updated - 0DenisseRangelÎncă nu există evaluări
- 6.-NCDs Part II (Cardiovascular Diseases (CVDS) )Document36 pagini6.-NCDs Part II (Cardiovascular Diseases (CVDS) )Nathaniel OrtegaÎncă nu există evaluări
- ArticleDocument3 paginiArticleChristine Joy MolinaÎncă nu există evaluări
- Biology Unit 1 Repeat Questions PDFDocument12 paginiBiology Unit 1 Repeat Questions PDFFarah100% (1)
- Inotropes in PicuDocument2 paginiInotropes in PicuDijattxÎncă nu există evaluări
- Treadmill Test: Khairul Nizam Abdul Rahman 4262143008Document12 paginiTreadmill Test: Khairul Nizam Abdul Rahman 4262143008Dea Amelia YolandaÎncă nu există evaluări
- Exercise:: I. True or False Statements: Put TRUE in Front of The True Sentences and FALSE inDocument6 paginiExercise:: I. True or False Statements: Put TRUE in Front of The True Sentences and FALSE inIssouf BertheÎncă nu există evaluări
- Essay On Cardiac Cycle (With Diagram) - Heart - Human - BiologyDocument28 paginiEssay On Cardiac Cycle (With Diagram) - Heart - Human - Biologydr_swaralipiÎncă nu există evaluări
- The Lymphatic System HandoutDocument2 paginiThe Lymphatic System HandoutbernachurchÎncă nu există evaluări
- 1 s2.0 S0735109722056030 MainDocument15 pagini1 s2.0 S0735109722056030 MainAkhmad HidayatÎncă nu există evaluări
- ScienceMentalphysics PDFDocument188 paginiScienceMentalphysics PDFGuida Lourenco100% (3)
- Definition of Aquatic ExerciseDocument3 paginiDefinition of Aquatic Exercisevenkata ramakrishnaiahÎncă nu există evaluări
- Lonjel&Cleeneron ENGDocument13 paginiLonjel&Cleeneron ENGDeSheliÎncă nu există evaluări
- 05 - ElektrokardiogramDocument39 pagini05 - ElektrokardiogramNauval Zilal FananyÎncă nu există evaluări
- 1 Symptoms#F186Document20 pagini1 Symptoms#F186Natasha LiberisÎncă nu există evaluări
- 1 рівень медикиDocument8 pagini1 рівень медикиHart ElettÎncă nu există evaluări
- Animal DiversityDocument87 paginiAnimal DiversityharshitaÎncă nu există evaluări
- 2 Circulation SystemDocument29 pagini2 Circulation SystemPERTUNIA KORABIÎncă nu există evaluări
- 4th Lab Bio 11 Exam ReviewDocument13 pagini4th Lab Bio 11 Exam ReviewAlly YeeÎncă nu există evaluări