Documente Academic
Documente Profesional
Documente Cultură
Vitiligo - Management and Prognosis - UpToDate
Încărcat de
BoneyJalgarTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Vitiligo - Management and Prognosis - UpToDate
Încărcat de
BoneyJalgarDrepturi de autor:
Formate disponibile
Author: Pearl E Grimes, MD
Section Editor: Hensin Tsao, MD, PhD
Deputy Editor: Rosamaria Corona, MD, DSc
Contributor Disclosures
All topics are updated as new evidence becomes available and our peer review process is complete.
Literature review current through: Jun 2019. | This topic last updated: May 05, 2017.
INTRODUCTION
Vitiligo is a relatively common acquired chronic disorder of pigmentation characterized
by the development of white macules on the skin due to loss of epidermal melanocytes
[1,2]. The depigmented areas are often symmetrical and usually increase in size with
time. Given the contrast between the white patches and areas of normal skin, the
disease is most disfiguring in darker skin types and has a profound impact on the
quality of life of children and adults [3,4]. Patients with vitiligo often experience
stigmatization, isolation, and low self-esteem [5-8].
Although there is no cure for the disease, the available treatments may halt the
progression of the disease and induce varying degrees of repigmentation with
acceptable cosmetic results in many cases. This topic review will discuss the
management of vitiligo. The pathogenesis, clinical features, and diagnosis of vitiligo are
discussed separately. Other pigmentation disorders are also discussed separately.
● (See "Vitiligo: Pathogenesis, clinical features, and diagnosis".)
● (See "Acquired hypopigmentation disorders other than vitiligo".)
● (See "Acquired hyperpigmentation disorders".)
● (See "Melasma".)
● (See "Postinflammatory hyperpigmentation".)
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 1 of 29
PATIENT EVALUATION
Assessment of severity — The evaluation of the patient with vitiligo involves a
detailed history and a complete skin examination to assess disease severity and
individual prognostic factors. Factors that may influence the approach to treatment
include:
● Age at onset of lesions
● Type of vitiligo (segmental, nonsegmental)
● Mucosal involvement, Koebner phenomenon
● Rate of progression or spread of lesions
● Previous episodes of repigmentation
● Type and response to previous treatments
● Family history of vitiligo and/or autoimmune diseases
● Presence of concomitant diseases
● Current medications and supplements
● Occupation, exposure to chemicals
● Effects of disease on the quality of life
A full-body skin examination should be performed to assess the extent of the disease,
with particular attention to sites of vitiligo predilection, such as the lips and perioral area,
periocular areas, dorsal surface of the hands, fingers, flexor surface of the wrists,
elbows, axillae, nipples, umbilicus, sacrum, groin, inguinal/anogenital regions, and
knees [9]. The percentage of the body area involved can be estimated by the so-called
1 percent rule or "palm method." In both children and adults, the palm of the hand,
including the fingers, is approximately 1 percent of the total body surface area (TBSA),
while the palm excluding the fingers is approximately 0.5 percent of the TBSA. An
alternative method is the "rule of nines":
● Each leg represents 18 percent of the TBSA.
● Each arm represents 9 percent of the TBSA.
● The anterior and posterior trunk each represent 18 percent of the TBSA.
● The head represents 9 percent of the TBSA.
Goals of treatment — The goals of treatment for vitiligo should be set with the
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 2 of 29
individual patient or parents in the case of children, based upon the patient's age and
skin type, the extent, location, and degree of disease activity, and the impact of the
disease on the patient's quality of life. An open discussion with the patient about the
limitations of treatment may be helpful to create realistic expectations.
Nonsegmental vitiligo has an unpredictable course, and treatment is often challenging.
However, multiple therapies, including topical agents, light therapies, and autologous
grafting procedures, have demonstrated efficacy for repigmentation of vitiligo [10]. The
response to treatments is generally slow and may be highly variable among patients
and among different body areas in the same patient. The best outcomes are often
achieved in darker skin types (Fitzpatrick IV to VI), although satisfactory results are
often seen also in lighter skin types (Fitzpatrick II, III). Facial and truncal lesions
respond well to treatment, while acral areas are extremely difficult to treat.
Psychosocial aspects — The patient's psychologic profile and ability to cope with a
lifelong disease should be carefully evaluated at the time of treatment planning.
Psychologic support should be offered to patients if needed. (See 'Psychologic
interventions' below.)
APPROACH
Our approach to the management of patients with vitiligo is generally consistent with
published guidelines [11,12]. Topical, systemic, and light-based therapies are available
for the stabilization and repigmentation of vitiligo (table 1) [13-17]. Treatment modalities
are chosen in the individual patient on the basis of the disease severity, patient
preference (including cost and accessibility), and response evaluation. Combination
therapies, such as phototherapy plus topical or oral corticosteroids, are usually more
effective than single therapies [18]. Despite treatment, however, vitiligo has a highly
unpredictable course, and the long-term persistence of repigmentation cannot be
predicted [18].
Stabilization of rapidly progressive disease — For patients who experience rapid
progression of vitiligo, with depigmented macules spreading over a few weeks or
months, we suggest low-dose oral corticosteroids as first-line therapy for the
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 3 of 29
stabilization (cessation of spread) of the disease (table 1). Oral prednisone is given at
the dose of 5 to 10 mg per day in children and 10 to 20 mg per day in adults for a
maximum of two weeks. If needed, treatment can be repeated in four to six weeks.
In adult patients, alternatives to oral prednisone include oral mini-pulse therapy with
dexamethasone 2.5 mg on two consecutive days weekly for an average of three
months or intramuscular triamcinolone 40 mg in a single administration. Treatment with
triamcinolone can be repeated in four to six weeks for a maximum of three injections.
(See 'Systemic corticosteroids' below.)
Stabilization therapy can be given with or without concomitant narrowband ultraviolet B
(NB-UVB) phototherapy. However, for patients with active disseminated disease
affecting multiple anatomic sites, we suggest that systemic corticosteroids and NB-UVB
phototherapy be initiated concomitantly. The disease is expected to stabilize in one to
three months.
In both adults and children in whom systemic corticosteroids are contraindicated, NB-
UVB phototherapy alone may be used to stabilize active vitiligo. NB-UVB is
administered two to three times weekly. (See 'Narrowband ultraviolet B phototherapy'
below.)
Vitiligo involving <10 percent of the TBSA
Localized disease — In patients with nonsegmental stable vitiligo (no increase in
size of existing lesions and absence of new lesions in the previous three to six months)
that involves <10 percent of the total body surface area (TBSA) and is limited to the
face, neck (picture 1), trunk, or extremities, mid- to high-potency topical corticosteroids
(groups two to four (table 2)) are the first-line therapy [12,19]. High-potency and mid-
potency topical corticosteroids are applied to the involved skin once and twice daily,
respectively. Agents with negligible systemic or local side effects, such as mometasone
furoate, are preferred [12]. (See 'Topical corticosteroids' below.)
There are no studies evaluating the optimal duration of treatment with topical
corticosteroids. In the author's experience, topical corticosteroids can be used safely for
two to three months, interrupted for one month, and then resumed for an additional two
or three months. Others suggest a discontinuous scheme (eg, once-daily application for
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 4 of 29
15 days per month for six months) [11,12,20].
Patients must be monitored closely for adverse effects of topical corticosteroids, which
include skin atrophy, telangiectasias, hypertrichosis, and acneiform eruptions. Limited
quantities should be prescribed.
Topical calcineurin inhibitors (tacrolimus and pimecrolimus) are the preferred first-line
therapy in patients with limited disease involving the face or areas at high risk for skin
atrophy. Topical calcineurin inhibitors are generally applied twice daily. They can also be
used in combination with a topical corticosteroid for the first month or two, applying
each one once daily. (See 'Topical calcineurin inhibitors' below.)
For patients with limited disease who do not respond to topical corticosteroids or topical
calcineurin inhibitors, targeted phototherapy administered twice weekly is an option
(picture 2). (See 'Targeted phototherapy' below.)
Disseminated disease — For patients with disseminated areas of depigmentation
affecting multiple anatomic sites but overall involvement of less than 10 percent of the
TBSA, we suggest NB-UVB phototherapy as first-line therapy. NB-UVB phototherapy is
administered two to three times weekly. In the author's experience, less than 50
treatments are usually sufficient to achieve optimal outcomes. (See 'Narrowband
ultraviolet B phototherapy' below.)
Segmental vitiligo — Topical corticosteroids, calcineurin inhibitors, or targeted
phototherapy are the first-line therapy for segmental vitiligo. (See 'Topical
corticosteroids' below and 'Topical calcineurin inhibitors' below and 'Targeted
phototherapy' below.)
NB-UVB phototherapy can be used for more extensive disease affecting multiple
dermatomes. For patients who do not respond to topical or light therapies, autologous
grafting is a second-line option [21]. Given the stable nature of segmental vitiligo, long-
term repigmentation can be achieved with autologous melanocyte transplantation [22].
(See 'Narrowband ultraviolet B phototherapy' below and 'Surgical therapies' below.)
Localized recalcitrant vitiligo — Surgical procedures are a therapeutic option for
patients with localized stable vitiligo that does not respond to topical agents or NB-UVB
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 5 of 29
phototherapy. Autologous grafting techniques include 1-mm punch grafts, suction blister
grafts, or cellular suspensions. While all these techniques have proven success, most
are technically challenging and expensive. One-millimeter punch grafts, however, can
be performed with ease and without the need of special devices or equipment. (See
'Surgical therapies' below.)
Vitiligo involving 10 to 40 percent of the TBSA — For adults and children with stable
nonsegmental vitiligo involving 10 to 40 percent of the TBSA, we suggest NB-UVB as
first-line therapy (picture 3). (See 'Narrowband ultraviolet B phototherapy' below.)
NB-UVB is administered two to three times per week for an average of 9 to 12 months.
Follicular areas of repigmentation usually begin to appear after 15 to 20 NB-UVB
treatments (picture 4). If patients are responding well with continued repigmentation,
treatment can be maintained beyond 9 to 12 months and up to 24 months or 200
sessions and then tapered off. Mid-potency topical corticosteroids or topical calcineurin
inhibitors are often intermittently used in combination with phototherapy.
Home NB-UVB phototherapy is an option for patients unable to travel to the clinician's
office for weekly treatments [23]. Whole-body or portable, handheld units are available
on the market (sample brand names include Daavlin, National Biological Solarc
Systems). Patients should be provided with detailed instructions on the use of the home
phototherapy units and return for in-office clinician follow-up on a regular basis.
Vitiligo involving >40 percent of the TBSA — NB-UVB is the first-line therapy for
patients with extensive vitiligo involving greater than 40 percent of the TBSA. The
suggested regimen and duration of treatment are similar to that discussed above for
patients with more limited disease. (See 'Vitiligo involving 10 to 40 percent of the TBSA'
above.)
However, for patients with extensive recalcitrant vitiligo that does not respond to
repigmentation regimens and for patients with extensive vitiligo who do not desire
undergoing repigmentation treatments, depigmentation of residual normally pigmented
areas utilizing topical monobenzyl ether of hydroquinone (monobenzone) may be an
option. Depigmentation therapy is usually initiated with monobenzone 10% cream for
one month and then continued with monobenzone 20% cream. Monobenzone is
applied on the areas of residual pigmentation once or twice daily; we typically treat
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 6 of 29
exposed areas first. These sites include the face, neck, upper extremities, chest, and
lower legs. Depigmentation usually begins at distant sites (where the drug has not been
applied) after three to six months of continued use. Depigmentation therapy may
require one to three years to achieve optimal outcomes. (See 'Depigmentation' below.)
Side effects of monobenzone are dose-dependent and include irritant contact dermatitis
and severe xerosis. Monobenzone should never be used as a lightening agent in cases
other than vitiligo. It will induce vitiligo in normal individuals.
Response assessment — Initial response to treatment is in most cases indicated by
the appearance of perifollicular areas of repigmentation in the vitiliginous patch, which
usually begins 8 to 12 weeks after the initiation of treatment or after 15 to 20 NB-UVB
sessions (picture 4). Some patients may show a diffuse repigmentation pattern or a
combination of diffuse and perifollicular [24,25]. Photographs should be taken before
starting treatment and at each follow-up visit to evaluate the degree of repigmentation.
In patients who respond well to treatment and achieve optimal repigmentation,
therapies can be gradually tapered and then discontinued. However, some patients may
require maintenance treatment. Intermittent use of topical corticosteroids or topical
calcineurin inhibitors (eg, twice weekly) and phototherapy every other week may be
used as long-term maintenance treatments. For patients who relapse after stopping
treatment or during the maintenance phase, another cycle of phototherapy can be
administered.
TREATMENT MODALITIES
Topical therapies
Topical corticosteroids — Mid- to super-high-potency topical corticosteroids are
commonly used as a first-line therapy for the treatment of limited vitiligo. Their efficacy
is attributed to modulation of the immune response.
The efficacy of topical corticosteroids as monotherapy for the treatment of vitiligo is
supported by a few small randomized trials [16]. A systematic review of 17 randomized
trials examined the effect of topical corticosteroids in combination with other therapies
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 7 of 29
(eg, narrowband ultraviolet B [NB-UVB], psoralen plus ultraviolet A with sunlight
[PUVAsol], excimer laser) [26]. The combination of potent or super-potent topical
corticosteroids (eg, betamethasone dipropionate, mometasone furoate, clobetasol
propionate) with light therapies is more effective than light therapies alone in inducing
repigmentation [27-29]. However, the quality of studies was generally poor, and the
study results could not be pooled because of considerable heterogeneity in study
design and outcome measure.
Adverse effects related to a prolonged use of topical corticosteroids, including folliculitis,
mild atrophy, telangiectasia, and hypertrichosis, have been reported, generally in a
small number of patients, in nearly all studies. Systemic absorption resulting in adrenal
suppression is a concern when large areas of skin and areas with thin skin are treated
for a prolonged time with potent steroids, especially in children [19].
Topical calcineurin inhibitors — Tacrolimus and pimecrolimus are topical
immunomodulatory agents that affect the T-cell and mast-cell function and inhibit the
synthesis and release of multiple proinflammatory cytokines, including interferon-
gamma, tumor necrosis factor-alpha, interleukin (IL)-4, IL-5, and IL-10 [30-32]. In
contrast with topical corticosteroids, topical calcineurin inhibitors do not induce skin
atrophy, striae, or telangiectasias and are increasingly used for the treatment of facial
vitiligo.
The efficacy of tacrolimus and pimecrolimus alone or in combination with other
therapies for the treatment of nonsegmental vitiligo has been evaluated in several
randomized trials including either adults or children with vitiligo [26].
● In a randomized trial, 100 children (55 children with facial vitiligo; 45 with nonfacial
vitiligo) were treated with topical corticosteroid (clobetasol propionate 0.05%),
tacrolimus 0.1%, or placebo for six months [33]. Among children with facial vitiligo,
the success rate (defined as repigmentation >50 percent) was the same in the
topical corticosteroid and tacrolimus groups (58 percent); however, among children
with nonfacial vitiligo, the success rate was higher in the topical corticosteroid
group compared with the tacrolimus groups (39 versus 23 percent). The success
rate in the placebo group was 7 percent.
● Another randomized trial including 44 adult patients with stable vitiligo compared
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 8 of 29
0.1% tacrolimus ointment twice daily, 1% pimecrolimus cream twice daily, and NB-
UVB phototherapy three times a week for 24 weeks [34]. At the end of the study,
there was no significant difference among treatments in the repigmentation for any
anatomical site.
● In a 12-week open, randomized study, 53 patients with vitiligo were treated with
308 nm monochromatic excimer light (MEL) twice weekly plus 0.1% tacrolimus and
oral vitamin E daily, 308 nm MEL twice weekly plus daily oral vitamin E, or daily
oral vitamin E alone [35]. At the end of the study, good to excellent repigmentation
was achieved in 70 percent of patients in the MEL plus tacrolimus and vitamin E
group, 55 percent of those in the MEL plus vitamin E group, and in none of the
patients in the vitamin E group.
● In an open trial, 40 children with nonsegmental, focal, or segmental vitiligo were
treated with 0.1% mometasone furoate cream once daily or 1% pimecrolimus
cream twice daily for three months [36]. Moderate or marked responses were seen
in 11 patients (55 percent) in the mometasone furoate group and in 7 (35 percent)
in the pimecrolimus group, but the difference was not statistically significant.
Although the increased risk of skin cancer among transplant patients treated with
systemic calcineurin inhibitors is well recognized, the use of topical calcineurin inhibitors
does not seem to be associated with an increased risk for skin or systemic
malignancies [37-39]. However, based upon animal studies documenting an increased
risk of lymphoma and skin cancers associated with topical or systemic exposure to
calcineurin inhibitors and to reports of cancer cases in children who used topical
pimecrolimus or tacrolimus for atopic dermatitis, in 2006 the US Food and Drug
Administration placed a boxed warning on the prescribing information for these
medications. Labeling also recommends that these agents should not be used in
combination with ultraviolet (UV) light therapy.
Unproven topical therapies — The benefit of topical vitamin D3 analogues in the
treatment of vitiligo is controversial. A few small randomized trials evaluated the role of
calcipotriol and tacalcitol in combination with psoralen plus ultraviolet A (PUVA),
narrowband ultraviolet (NB-UV), or natural sunlight for the treatment of nonsegmental
vitiligo with conflicting results [40-42].
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 9 of 29
● In a prospective right-left 24-week comparative study including 24 patients with
vitiligo, there were no statistically significant differences between the sides treated
with NB-UVB monotherapy and the sides treated with NB-UVB plus calcipotriol
[41].
● In another right-left comparative study, 35 patients with generalized vitiligo applied
calcipotriol 0.05 mg/g cream or placebo to the reference lesions one hour before
PUVA treatment twice weekly [40]. Lesions on the side treated with calcipotriol plus
PUVA had a fourfold increase in the likelihood of achieving greater than 75 percent
repigmentation sooner than the side treated with placebo plus PUVA (mean
number of PUVA sessions 9 and 12, respectively).
Phototherapy
Narrowband ultraviolet B phototherapy — NB-UVB involves the use of UV lamps
with a peak emission of approximately 311 nm [43]. These shorter wavelengths provide
higher-energy fluences and induce less cutaneous erythema. NB-UVB induces local
immunosuppression and apoptosis; stimulates the production of melanocyte-stimulating
hormones, basic fibroblasts, growth factor, and endothelin I; and increases melanocyte
proliferation and melanogenesis [43-45]. (See "UVB therapy (broadband and
narrowband)".)
Due to its lack of systemic toxicity and its good safety profile in both children and adults,
NB-UVB phototherapy has emerged as the initial treatment of choice for patients with
vitiligo involving >10 percent of the body surface area (BSA). NB-UVB can be used for
both stabilization and repigmentation of vitiligo (picture 3).
A meta-analysis of three randomized trials comparing oral PUVA with NB-UVB found a
60 percent higher proportion of participants achieving >75 percent repigmentation in the
NB-UVB group compared with the oral PUVA group [26]. The additive effect of
tacrolimus ointment (0.1%) applied once daily combined with NB-UVB in the treatment
of vitiligo has been evaluated in one randomized trial [46]. In this study, 40 patients with
stable, symmetrical vitiligo were treated with tacrolimus ointment 0.1% on one side of
their body and a placebo ointment on the other side plus whole-body NB-UVB two or
three times weekly for at least three months. In 27 of 40 patients, a greater reduction in
the target lesion area was seen in the side treated with tacrolimus compared with the
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 10 of 29
side treated with NB-UVB alone (42 versus 29 percent). However, a possible increase
in the risk of skin cancer with this combination therapy cannot be excluded.
A 2017 meta-analysis of 35 randomized and nonrandomized studies including 1428
patients compared the repigmentation rates of NB-UVB and PUVA by treatment
duration [47]. For NB-UVB, a ≥75 percent repigmentation was achieved by 13, 19, and
36 percent of patients at 3, 6, and 12 months of treatment, respectively. For PUVA, ≥75
percent repigmentation was achieved by 9 percent of patients at 6 months and 14
percent at 12 months. The results of this meta-analysis confirm the superiority of NB-
UVB over PUVA and suggest that phototherapy should be continued for at least 12
months to achieve a maximal response.
Only a few small observational studies have evaluated the duration of repigmentation in
patients with vitiligo treated with phototherapy. In a small observational study of 11
patients followed up for two years after treatment with NB-UVB phototherapy, five
maintained areas of repigmentation and six experienced complete or partial relapse of
vitiligo at previously repigmented sites [48]. In another study including 15 children
treated with NB-UVB phototherapy and followed up for a mean of 12 months after
completing treatment, six showed stable repigmentation, four further improvement, and
three complete or partial regression of the pigmentation achieved with treatment [49].
PUVA photochemotherapy — Historically, photochemotherapy with topical or
systemic PUVA radiation was the "gold standard" treatment for the repigmentation of
vitiligo but has been largely replaced by NB-UVB phototherapy. PUVA is associated with
substantial adverse effects, including phototoxicity and gastrointestinal discomfort, and
requires patients to use ocular protection for 12 to 24 hours following treatment. In
addition, the long-term risk of skin cancer is well established for PUVA [50]. (See
"Psoralen plus ultraviolet A (PUVA) photochemotherapy".)
Targeted phototherapy — Targeted phototherapy using 308 nm monochromatic
excimer lamps or lasers has demonstrated efficacy for the treatment of localized vitiligo
(picture 2) [51]. These devices deliver high-intensity light only to the affected areas
while avoiding exposure of the healthy skin and lowering the cumulative ultraviolet B
(UVB) dose. (See "Targeted phototherapy".)
A systematic review of six randomized trials (411 patients with 764 lesions) found that
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 11 of 29
excimer lamps and excimer lasers were equally effective in inducing ≥50 percent and
≥75 percent repigmentation [52]. Although the repigmentation may occur more rapidly
with more frequent weekly treatments, the final result appears to be related to the
overall number of treatment sessions rather than their frequency [53].
As with NB-UVB, targeted phototherapy can work synergistically with topical therapies,
including tacrolimus ointment and topical corticosteroids [12,54].
● In a study of eight patients with vitiligo, 24 symmetric vitiliginous areas were treated
with the excimer laser three times per week for a total of 24 treatments [55]. Topical
tacrolimus ointment or placebo was applied to randomized affected areas twice
daily throughout the length of the trial. Fifty percent of the areas treated with the
combination excimer laser and topical tacrolimus achieved ≥75 percent
repigmentation compared with 20 percent of the areas treated with placebo.
● In a 12-week open randomized study, 53 patients with vitiligo were treated with 308
nm MEL twice weekly plus 0.1% tacrolimus and oral vitamin E daily, 308 nm MEL
twice weekly plus daily oral vitamin E, or daily oral vitamin E alone [35]. At the end
of the study, good to excellent repigmentation was achieved in 70 percent of
patients in the MEL plus tacrolimus and vitamin E group, 55 percent of those in the
MEL plus vitamin E group, and in none of the patients in the vitamin E group.
Systemic therapies
Systemic corticosteroids — Low-dose oral corticosteroids are generally utilized for
the stabilization of rapidly progressive vitiligo, often in combination with NB-UVB
phototherapy. Evidence for their efficacy in halting the spread of vitiligo is limited to a
few uncontrolled studies [56-58].
● In one study, 81 patients were treated with prednisolone 0.3 mg/kg per day for two
months, and then the dose was progressively reduced in the subsequent three
months [56]. Control of disease progression was achieved in approximately 90
percent of patients and repigmentation in 74 percent.
● In another study, 40 patients with extensive or rapidly spreading vitiligo were
treated with oral mini-pulses of betamethasone or dexamethasone (5 mg in single
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 12 of 29
dose) on two consecutive days per week for several months. After one to three
months, vitiligo progression was arrested in 32 of 36 patients with active disease
[57].
Oral corticosteroids are not effective as a repigmenting therapy for stable vitiligo. In a
small open-label trial, 86 patients with progressive nonsegmental vitiligo were treated
with oral mini-pulses of betamethasone (0.1 mg/kg twice weekly on two consecutive
days for three months followed by 1 mg every month for the following three months)
alone or in combination with PUVA, NB-UVB, or broadband UVB [59]. At six months,
marked or moderate improvement was achieved in 15 percent of patients treated with
corticosteroids alone versus 85 percent of patients treated with corticosteroids plus
PUVA, 81 percent of those treated with corticosteroids plus NB-UVB, and 33 percent of
those treated with corticosteroids plus broadband-UVB.
Complementary and alternative therapies — Oral supplementation with
antioxidants and vitamins is often used as an adjunctive treatment for vitiligo, usually in
combination with phototherapy. However, there is limited evidence from high-quality
studies to support their use.
● Vitamins – A few small uncontrolled studies have reported stabilization and
repigmentation in vitiligo patients treated with UVB phototherapy and high-dose
vitamin supplementation, vitamin C, vitamin B12, and folic acid [60,61].
● Alpha-lipoic acid – Alpha-lipoic acid is an organosulfur compound derived from
octanoic acid. It is widely available as an over-the-counter nutritional supplement
and has been marketed as an antioxidant. The efficacy of alpha-lipoic acid in
vitiligo was demonstrated in one randomized trial including 35 patients with
nonsegmental vitiligo [62]. In this study, twice-daily oral supplementation with
alpha-lipoic acid, vitamin E, polyunsaturated fatty acids, and cysteine monohydrate
combined with NB-UVB twice weekly for six months resulted in significantly more
patients (47 versus 18 percent) achieving >75 percent repigmentation compared
with phototherapy alone. In addition, repigmentation occurred earlier with lower
cumulative UVB dose. Biochemical evaluations at two and six months showed
increased catalase activity, decreased intracellular reactive oxygen species
production, and reduced membrane peroxidation in the combination-treatment
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 13 of 29
group. Despite these promising results, further studies are needed to confirm the
benefit of alpha-lipoic acid supplementation in the management of vitiligo.
● Ginkgo biloba – Extracts from the Ginkgo biloba leaf have long been used in
traditional Chinese medicine to treat various conditions, including cutaneous,
neurologic, and vascular disorders. The two main groups of active constituents
responsible for G. biloba's medicinal effects are terpene lactones (ginkgolides and
bilobalides) and ginkgo flavone glycosides, which are present in varying
concentrations in the leaf of the ginkgo tree. (See "Clinical use of ginkgo biloba".)
Only a few investigations have evaluated ginkgo's use in the management of
vitiligo.
• A small randomized trial reported that the spread of vitiligo was arrested in 20
of 25 subjects receiving 40 mg of G. biloba extract three times daily for six
months but in none of 22 subjects in the placebo group [63]. In addition, 10
patients in the active treatment group but only two in the placebo group
showed >75 percent repigmentation.
• Another pilot study found significant improvements in total Vitiligo Area Scoring
Index and Vitiligo European Task Force assessment in 12 participants
following 12 weeks of supplementation with twice-daily G. biloba extract [64].
In addition to repigmentation, active depigmentation ceased in all patients with
acrofacial vitiligo.
● Polypodium leucotomos – In one randomized trial, NB-UVB in combination with
oral extracts of Polypodium leucotomos, a tropical fern with antioxidant and
immunomodulator properties, was more effective than NB-UVB alone in inducing
repigmentation of vitiligo in the head and neck area (50 versus 19 percent) after 25
weeks [65]. No difference was noted in other body areas.
Surgical therapies — Surgical therapies have been used for vitiligo for the past 25
years and remain viable options for patients with localized depigmented areas that have
been unresponsive to medical intervention [66-69]. They include:
● Autologous suction blister grafts [70,71]
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 14 of 29
● Minigrafts or punch grafts [72-74]
● Split-thickness grafts [75,76]
● Autologous melanocyte cultures
● Cultured epidermal suspensions [77,78]
● Autologous noncultured epidermal cell suspension [79]
● Hair follicle transplantation [80-82]
The scope of transplantation procedures is the transfer of a reservoir of healthy
melanocytes to vitiliginous skin for proliferation and migration into areas of
depigmentation. Transplantation procedures are contraindicated for patients with a
history of hypertrophic scars or keloids.
A systematic review of randomized trials and observational studies of autologous
transplantation methods for vitiligo concluded that maximal repigmentation occurred in
patients treated with split-thickness grafting and epidermal blister grafting [66]. Both
treatment groups achieved success rates of 90 percent repigmentation.
Other studies have reported the benefits of transplantation of autologous melanocyte
cultures and epidermal suspensions containing both melanocytes and keratinocytes
[67,77,79]. In one randomized trial comparing autologous noncultured epidermal cell
suspension with suction blister grafts in 41 patients, a repigmentation ≥75 percent was
achieved in over 85 percent of lesions in both treatment groups [79]. However, more
lesions in the noncultured epidermal cell suspension group achieved a 90 to 100
percent repigmentation compared with those in the suction blister group (70 versus 27
percent).
Adverse effects of surgical therapies include cobblestoning, scarring, graft
depigmentation, and graft displacement. Suction blister grafts and split skin grafts may
be associated with the Koebner phenomenon at the donor site, a complication of major
clinical importance since it results in the development of new vitiligo lesions [26]. Other
adverse effects include hypopigmentation, hyperpigmentation, scarring, and infection at
both donor and recipient sites. Punch grafting or minigrafting adverse effects include
lack of color blending and matching with the surrounding normal skin, cobblestoning,
and "polka dot" appearance [83].
Factors influencing the outcome of transplantation techniques include age, site of
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 15 of 29
lesion, and type of vitiligo. In a series of 117 patients, the best results were achieved for
patients younger than age 20 and patients with segmental vitiligo, whereas the grafting
site did not significantly affect the outcome [68].
Depigmentation — Since the 1950s, monobenzyl ether of hydroquinone
(monobenzone) has been used as a depigmenting agent for patients with extensive
vitiligo [84,85]. Monobenzone causes permanent destruction of melanocytes and
induces depigmentation locally and remotely from the sites of application. Thus, the use
of monobenzone for other disorders of pigmentation is contraindicated. The major side
effects of monobenzone therapy are irritant contact dermatitis and pruritus, which
usually respond to topical and systemic steroids. Other side effects include severe
xerosis, alopecia, and premature graying.
Experimental therapies
● Afamelanotide – Afamelanotide, a potent and longer-lasting synthetic analog of
naturally occurring alpha-melanocyte-stimulating hormone (MSH), is a novel
intervention for vitiligo [86,87]. Its use is based upon the demonstration of defects
in the melanocortin system in patients with vitiligo, including decreased circulating
and lesional skin levels of alpha-MSH [88]. Afamelanotide is delivered as a
subcutaneous, bioresorbable implant that promotes melanocyte proliferation and
melanogenesis.
The safety and efficacy of afamelanotide implants combined with NB-UVB were
assessed in an observational study of four patients with generalized vitiligo [86].
Patients were treated three times weekly with NB-UVB for one month and then
administered a series of four monthly implants containing 16 mg of afamelanotide.
Follicular and confluent areas of repigmentation were evident within two days to
four weeks after the initial implant. Afamelanotide induced fast and deep
repigmentation as well as diffuse hyperpigmentation in all cases. In a subsequent
randomized trial including 55 patients with skin type III to VI and vitiligo involving 15
to 50 percent of the BSA, patients in the NB-UVB plus afamelanotide group
achieved a greater repigmentation than patients in the NB-UVB monotherapy
group at five months (49 versus 33 percent) [87].
● Prostaglandin E2 – Prostaglandin E2 (PGE2) is a potentially beneficial treatment
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 16 of 29
for localized stable vitiligo. PGE2 controls the proliferation of melanocytes by
means of stimulant and immunomodulatory effects. In a consecutive series of
patients with stable vitiligo, repigmentation occurred in 40 of 56 patients treated
with PGE2 0.25 mg/g gel twice daily for six months [89]. The response was
excellent in 22 of 40 patients, with complete repigmentation observed in eight
patients.
● Bimatoprost – Bimatoprost, a synthetic analog of prostaglandin F2-alpha approved
for the topical treatment of glaucoma and hypotrichosis of the eyelashes, is
associated with hyperpigmentation of periocular skin caused by increased
melanogenesis [90]. The efficacy of bimatoprost in the treatment of vitiligo was
initially evaluated in a preliminary study of 10 patients with localized vitiligo treated
with bimatoprost 0.03% ophthalmic solution twice daily for four months [91]. Of the
10 patients, three had 100 percent repigmentation, three had 75 to 99 percent
repigmentation, and one patient had 50 to 75 percent repigmentation. The best
responses were observed on the face.
A subsequent proof-of-concept randomized trial compared the efficacy of
bimatoprost 0.03% ophthalmic solution alone and in combination with a topical
steroid (mometasone) with mometasone alone in 32 patients with nonsegmental,
nonfacial stable vitiligo involving <5 percent of the body surface area [92]. At 20
weeks, none of the patients achieved the prespecified end point of 50 to 75 percent
repigmentation. However, in a post-hoc analysis using a less stringent definition of
response (25 to 50 percent repigmentation), patients treated with bimatoprost,
either alone or with mometasone, achieved a greater repigmentation in the neck
and trunk than patients treated with mometasone alone.
● Topical ruxolitinib – Ruxolitinib is a Janus kinase 1 and 2 inhibitor approved for the
treatment of intermediate- or high-risk myelofibrosis and polycythemia vera. In a
phase 2, proof-of-concept trial, topical ruxolitinib 1.5% cream was administered
twice daily to 11 adult patients with vitiligo involving at least 1 percent of the body
surface area for 20 weeks [93]. Eight of 11 patients had some response to
treatment, with a mean improvement of the Vitiligo Area Scoring Index of 23
percent. The best response was observed in patients with facial vitiligo. The main
adverse effect was erythema over the treated lesion.
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 17 of 29
PSYCHOLOGIC INTERVENTIONS
There is a scarcity of high-quality studies evaluating the efficacy of psychologic
interventions in the management of patients with vitiligo. One small randomized trial
found that cognitive-behavioral therapy in addition to conventional therapies was
effective in improving the quality of life, self-esteem, and perceived body image in adult
patients with vitiligo and even influenced the course of the disease itself [94].
CAMOUFLAGE
Cosmetic camouflage can be beneficial for patients with vitiligo affecting exposed areas
such as the face, neck, and hands. Camouflage products include foundation-based
cosmetics and self-tanning products containing dihydroxyacetone (DHA). DHA-based
products are most popular because they provide lasting color for up to several days and
are not immediately rubbed off onto clothing. Tattooing or micropigmentation should be
avoided, given the risk of koebnerization and oxidation of tattoo pigment causing further
dyschromia. (See "Vitiligo: Pathogenesis, clinical features, and diagnosis", section on
'Koebner phenomenon'.)
PROGNOSIS
Vitiligo is a chronic disease with a highly unpredictable course. Early-onset vitiligo
appears to be associated with involvement of a greater body surface area involvement
and increased rate of disease progression [95]. Despite treatment, most patients
experience alternating periods of pigment loss and disease stability for their entire life.
Occasionally, patients may experience spontaneous repigmentation.
Patients who have organ-specific autoantibodies have an increased risk of developing
subclinical or overt autoimmune disease [96]. (See "Vitiligo: Pathogenesis, clinical
features, and diagnosis", section on 'Associated disorders'.)
SUMMARY AND RECOMMENDATIONS
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 18 of 29
● Vitiligo is a chronic, relapsing disease. The goals of treatment include the
stabilization of active disease and the repigmentation of depigmented patches.
However, the response to treatments is slow and may be highly variable among
patients and among different body areas in the same patient. (See 'Patient
evaluation' above and 'Assessment of severity' above and 'Goals of treatment'
above.)
● In patients with rapidly progressive vitiligo (ie, depigmented macules spreading
over a few weeks or months), we suggest systemic corticosteroids as adjunct
therapy to narrowband ultraviolet B (NB-UVB) phototherapy for stabilization (Grade
2C). (See 'Stabilization of rapidly progressive disease' above.)
● For patients with vitiligo involving <10 percent of the total body surface area
(TBSA), we suggest topical corticosteroids as initial therapy (Grade 2C). Topical
corticosteroids are applied once daily for two to three months and then interrupted
for one month. Topical calcineurin inhibitors are preferred to topical corticosteroids
for body areas at increased risk of atrophy. Targeted phototherapy is an option for
patients with limited vitiligo who do not respond to topical therapies. (See 'Vitiligo
involving <10 percent of the TBSA' above.)
● For patients with vitiligo involving 10 to 40 percent of the TBSA, we suggest
phototherapy with NB-UVB (Grade 2B). Phototherapy is administered two to three
times per week for 9 to 12 months or up to 200 treatments. Topical corticosteroids
or topical calcineurin inhibitors may be intermittently used in combination with NB-
UVB phototherapy. (See 'Vitiligo involving 10 to 40 percent of the TBSA' above.)
● Surgical therapies involving the autologous transplantation of healthy melanocytes
in depigmented areas are an option for patients with localized, recalcitrant vitiligo
and for patients with segmental vitiligo. (See 'Localized recalcitrant vitiligo' above
and 'Segmental vitiligo' above.)
● Depigmentation of residual pigmented areas with monobenzyl ether of
hydroquinone (monobenzone) can be considered for patients with extensive
recalcitrant vitiligo that does not respond to repigmentation regimens and for those
with extensive vitiligo who do not desire undergoing repigmentation treatments.
(See 'Vitiligo involving >40 percent of the TBSA' above.)
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 19 of 29
Use of UpToDate is subject to the Subscription and License Agreement.
REFERENCES
1. Ezzedine K, Eleftheriadou V, Whitton M, van Geel N. Vitiligo. Lancet 2015;
386:74.
2. Mohammed GF, Gomaa AH, Al-Dhubaibi MS. Highlights in pathogenesis of
vitiligo. World J Clin Cases 2015; 3:221.
3. Krüger C, Schallreuter KU. Stigmatisation, Avoidance Behaviour and Difficulties in
Coping are Common Among Adult Patients with Vitiligo. Acta Derm Venereol
2015; 95:553.
4. Silverberg JI, Silverberg NB. Quality of life impairment in children and adolescents
with vitiligo. Pediatr Dermatol 2014; 31:309.
5. Robins A. Biological Perspectives on Human Pigmentation, Cambridge University
Press, Cambridge, UK 2005. Vol 7.
6. Grimes PE. Disorders of pigmentation. In: ACP Medicine, Dale DC, Federman DD
(Eds), WebMD Scientific American Medicine, New York 2012. p.526.
7. Porter J. The psychological effects of vitiligo: Response to impaired appearance. I
n: Vitiligo, Hann SK, Nordlund JJ (Eds), Blackwell Science, Oxford, UK 2000. p.97
.
8. Daniel BS, Wittal R. Vitiligo treatment update. Australas J Dermatol 2015; 56:85.
9. Alikhan A, Felsten LM, Daly M, Petronic-Rosic V. Vitiligo: a comprehensive
overview Part I. Introduction, epidemiology, quality of life, diagnosis, differential
diagnosis, associations, histopathology, etiology, and work-up. J Am Acad
Dermatol 2011; 65:473.
10. Whitton M, Pinart M, Batchelor JM, et al. Evidence-based management of vitiligo:
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 20 of 29
summary of a Cochrane systematic review. Br J Dermatol 2016; 174:962.
11. Oiso N, Suzuki T, Wataya-Kaneda M, et al. Guidelines for the diagnosis and
treatment of vitiligo in Japan. J Dermatol 2013; 40:344.
12. Taieb A, Alomar A, Böhm M, et al. Guidelines for the management of vitiligo: the
European Dermatology Forum consensus. Br J Dermatol 2013; 168:5.
13. Yaghoobi R, Omidian M, Bagherani N. Vitiligo: a review of the published work. J
Dermatol 2011; 38:419.
14. Faria AR, Tarlé RG, Dellatorre G, et al. Vitiligo--Part 2--classification,
histopathology and treatment. An Bras Dermatol 2014; 89:784.
15. Falabella R, Barona MI. Update on skin repigmentation therapies in vitiligo.
Pigment Cell Melanoma Res 2009; 22:42.
16. Njoo MD, Spuls PI, Bos JD, et al. Nonsurgical repigmentation therapies in vitiligo.
Meta-analysis of the literature. Arch Dermatol 1998; 134:1532.
17. Grimes PE. Vitiligo. An overview of therapeutic approaches. Dermatol Clin 1993;
11:325.
18. Ezzedine K, Whitton M, Pinart M. Interventions for Vitiligo. JAMA 2016; 316:1708.
19. Kwinter J, Pelletier J, Khambalia A, Pope E. High-potency steroid use in children
with vitiligo: a retrospective study. J Am Acad Dermatol 2007; 56:236.
20. Meredith F, Abbott R. Vitiligo: an evidence-based update. Report of the 13th
Evidence Based Update Meeting, 23 May 2013, Loughborough, U.K. Br J
Dermatol 2014; 170:565.
21. Mulekar SV, Al Eisa A, Delvi MB, et al. Childhood vitiligo: a long-term study of
localized vitiligo treated by noncultured cellular grafting. Pediatr Dermatol 2010;
27:132.
22. Mulekar SV. Long-term follow-up study of segmental and focal vitiligo treated by
autologous, noncultured melanocyte-keratinocyte cell transplantation. Arch
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 21 of 29
Dermatol 2004; 140:1211.
23. Eleftheriadou V, Thomas K, Ravenscroft J, et al. Feasibility, double-blind,
randomised, placebo-controlled, multi-centre trial of hand-held NB-UVB
phototherapy for the treatment of vitiligo at home (HI-Light trial: Home Intervention
of Light therapy). Trials 2014; 15:51.
24. Parsad D, Pandhi R, Dogra S, Kumar B. Clinical study of repigmentation patterns
with different treatment modalities and their correlation with speed and stability of
repigmentation in 352 vitiliginous patches. J Am Acad Dermatol 2004; 50:63.
25. Gan EY, Gahat T, Cario-André M, et al. Clinical repigmentation patterns in
paediatric vitiligo. Br J Dermatol 2016; 175:555.
26. Whitton ME, Pinart M, Batchelor J, et al. Interventions for vitiligo. Cochrane
Database Syst Rev 2015; :CD003263.
27. Sassi F, Cazzaniga S, Tessari G, et al. Randomized controlled trial comparing the
effectiveness of 308-nm excimer laser alone or in combination with topical
hydrocortisone 17-butyrate cream in the treatment of vitiligo of the face and neck.
Br J Dermatol 2008; 159:1186.
28. Akdeniz N, Yavuz IH, Gunes Bilgili S, et al. Comparison of efficacy of narrow band
UVB therapies with UVB alone, in combination with calcipotriol, and with
betamethasone and calcipotriol in vitiligo. J Dermatolog Treat 2014; 25:196.
29. Khalid M, Mujtaba G, Haroon TS. Comparison of 0.05% clobetasol propionate
cream and topical Puvasol in childhood vitiligo. Int J Dermatol 1995; 34:203.
30. Tharp MD. Calcineurin inhibitors. Dermatol Ther 2002; 15:325.
31. Kang S, Lucky AW, Pariser D, et al. Long-term safety and efficacy of tacrolimus
ointment for the treatment of atopic dermatitis in children. J Am Acad Dermatol
2001; 44:S58.
32. Grimes PE, Soriano T, Dytoc MT. Topical tacrolimus for repigmentation of vitiligo.
J Am Acad Dermatol 2002; 47:789.
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 22 of 29
33. Ho N, Pope E, Weinstein M, et al. A double-blind, randomized, placebo-controlled
trial of topical tacrolimus 0·1% vs. clobetasol propionate 0·05% in childhood
vitiligo. Br J Dermatol 2011; 165:626.
34. Stinco G, Piccirillo F, Forcione M, et al. An open randomized study to compare
narrow band UVB, topical pimecrolimus and topical tacrolimus in the treatment of
vitiligo. Eur J Dermatol 2009; 19:588.
35. Nisticò S, Chiricozzi A, Saraceno R, et al. Vitiligo treatment with monochromatic
excimer light and tacrolimus: results of an open randomized controlled study.
Photomed Laser Surg 2012; 30:26.
36. Köse O, Arca E, Kurumlu Z. Mometasone cream versus pimecrolimus cream for
the treatment of childhood localized vitiligo. J Dermatolog Treat 2010; 21:133.
37. Margolis DJ, Abuabara K, Hoffstad OJ, et al. Association Between Malignancy
and Topical Use of Pimecrolimus. JAMA Dermatol 2015; 151:594.
38. Thaçi D, Salgo R. The topical calcineurin inhibitor pimecrolimus in atopic
dermatitis: a safety update. Acta Dermatovenerol Alp Pannonica Adriat 2007;
16:58, 60.
39. Ormerod AD. Topical tacrolimus and pimecrolimus and the risk of cancer: how
much cause for concern? Br J Dermatol 2005; 153:701.
40. Ermis O, Alpsoy E, Cetin L, Yilmaz E. Is the efficacy of psoralen plus ultraviolet A
therapy for vitiligo enhanced by concurrent topical calcipotriol? A placebo-
controlled double-blind study. Br J Dermatol 2001; 145:472.
41. Khullar G, Kanwar AJ, Singh S, Parsad D. Comparison of efficacy and safety
profile of topical calcipotriol ointment in combination with NB-UVB vs. NB-UVB
alone in the treatment of vitiligo: a 24-week prospective right-left comparative
clinical trial. J Eur Acad Dermatol Venereol 2015; 29:925.
42. Rodríguez-Martín M, García Bustínduy M, Sáez Rodríguez M, Noda Cabrera A.
Randomized, double-blind clinical trial to evaluate the efficacy of topical tacalcitol
and sunlight exposure in the treatment of adult nonsegmental vitiligo. Br J
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 23 of 29
Dermatol 2009; 160:409.
43. Njoo MD, Bos JD, Westerhof W. Treatment of generalized vitiligo in children with
narrow-band (TL-01) UVB radiation therapy. J Am Acad Dermatol 2000; 42:245.
44. Yones SS, Palmer RA, Garibaldinos TM, Hawk JL. Randomized double-blind trial
of treatment of vitiligo: efficacy of psoralen-UV-A therapy vs Narrowband-UV-B
therapy. Arch Dermatol 2007; 143:578.
45. Natta R, Somsak T, Wisuttida T, Laor L. Narrowband ultraviolet B radiation
therapy for recalcitrant vitiligo in Asians. J Am Acad Dermatol 2003; 49:473.
46. Nordal EJ, Guleng GE, Rönnevig JR. Treatment of vitiligo with narrowband-UVB
(TL01) combined with tacrolimus ointment (0.1%) vs. placebo ointment, a
randomized right/left double-blind comparative study. J Eur Acad Dermatol
Venereol 2011; 25:1440.
47. Bae JM, Jung HM, Hong BY, et al. Phototherapy for Vitiligo: A Systematic Review
and Meta-analysis. JAMA Dermatol 2017.
48. Sitek JC, Loeb M, Ronnevig JR. Narrowband UVB therapy for vitiligo: does the
repigmentation last? J Eur Acad Dermatol Venereol 2007; 21:891.
49. Percivalle S, Piccinno R, Caccialanza M, Forti S. Narrowband ultraviolet B
phototherapy in childhood vitiligo: evaluation of results in 28 patients. Pediatr
Dermatol 2012; 29:160.
50. Stern RS, PUVA Follow-Up Study. The risk of squamous cell and basal cell cancer
associated with psoralen and ultraviolet A therapy: a 30-year prospective study. J
Am Acad Dermatol 2012; 66:553.
51. Grimes PE. Advances in the treatment of vitiligo: targeted phototherapy. Cosmet
Dermatol 2003; 16:18.
52. Lopes C, Trevisani VF, Melnik T. Efficacy and Safety of 308-nm Monochromatic
Excimer Lamp Versus Other Phototherapy Devices for Vitiligo: A Systematic
Review with Meta-Analysis. Am J Clin Dermatol 2016; 17:23.
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 24 of 29
53. Hofer A, Hassan AS, Legat FJ, et al. Optimal weekly frequency of 308-nm
excimer laser treatment in vitiligo patients. Br J Dermatol 2005; 152:981.
54. Asawanonda P, Amornpinyokeit N, Nimnuan C. Topical 8-methoxypsoralen
enhances the therapeutic results of targeted narrowband ultraviolet B
phototherapy for plaque-type psoriasis. J Eur Acad Dermatol Venereol 2008;
22:50.
55. Kawalek AZ, Spencer JM, Phelps RG. Combined excimer laser and topical
tacrolimus for the treatment of vitiligo: a pilot study. Dermatol Surg 2004; 30:130.
56. Kim SM, Lee HS, Hann SK. The efficacy of low-dose oral corticosteroids in the
treatment of vitiligo patients. Int J Dermatol 1999; 38:546.
57. Pasricha JS, Khaitan BK. Oral mini-pulse therapy with betamethasone in vitiligo
patients having extensive or fast-spreading disease. Int J Dermatol 1993; 32:753.
58. Radakovic-Fijan S, Fürnsinn-Friedl AM, Hönigsmann H, Tanew A. Oral
dexamethasone pulse treatment for vitiligo. J Am Acad Dermatol 2001; 44:814.
59. Rath N, Kar HK, Sabhnani S. An open labeled, comparative clinical study on
efficacy and tolerability of oral minipulse of steroid (OMP) alone, OMP with PUVA
and broad / narrow band UVB phototherapy in progressive vitiligo. Indian J
Dermatol Venereol Leprol 2008; 74:357.
60. Don P, Iuga A, Dacko A, Hardick K. Treatment of vitiligo with broadband ultraviolet
B and vitamins. Int J Dermatol 2006; 45:63.
61. Elgoweini M, Nour El Din N. Response of vitiligo to narrowband ultraviolet B and
oral antioxidants. J Clin Pharmacol 2009; 49:852.
62. Dell'Anna ML, Mastrofrancesco A, Sala R, et al. Antioxidants and narrow band-
UVB in the treatment of vitiligo: a double-blind placebo controlled trial. Clin Exp
Dermatol 2007; 32:631.
63. Parsad D, Pandhi R, Juneja A. Effectiveness of oral Ginkgo biloba in treating
limited, slowly spreading vitiligo. Clin Exp Dermatol 2003; 28:285.
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 25 of 29
64. Szczurko O, Shear N, Taddio A, Boon H. Ginkgo biloba for the treatment of vitilgo
vulgaris: an open label pilot clinical trial. BMC Complement Altern Med 2011;
11:21.
65. Middelkamp-Hup MA, Bos JD, Rius-Diaz F, et al. Treatment of vitiligo vulgaris with
narrow-band UVB and oral Polypodium leucotomos extract: a randomized double-
blind placebo-controlled study. J Eur Acad Dermatol Venereol 2007; 21:942.
66. Njoo MD, Westerhof W, Bos JD, Bossuyt PM. A systematic review of autologous
transplantation methods in vitiligo. Arch Dermatol 1998; 134:1543.
67. van Geel N, Ongenae K, De Mil M, et al. Double-blind placebo-controlled study of
autologous transplanted epidermal cell suspensions for repigmenting vitiligo. Arch
Dermatol 2004; 140:1203.
68. Gupta S, Kumar B. Epidermal grafting in vitiligo: influence of age, site of lesion,
and type of disease on outcome. J Am Acad Dermatol 2003; 49:99.
69. Falabella R. Surgical approaches for stable vitiligo. Dermatol Surg 2005; 31:1277.
70. Ashique KT, Kaliyadan F. Long-Term Follow-up and Donor Site Changes
Evaluation in Suction Blister Epidermal Grafting Done for Stable Vitiligo: A
Retrospective Study. Indian J Dermatol 2015; 60:369.
71. Gou D, Currimbhoy S, Pandya AG. Suction blister grafting for vitiligo: efficacy and
clinical predictive factors. Dermatol Surg 2015; 41:633.
72. Malakar S, Dhar S. Treatment of stable and recalcitrant vitiligo by autologous
miniature punch grafting: a prospective study of 1,000 patients. Dermatology
1999; 198:133.
73. Singh SK. Punch grafting in vitiligo : Refinements and case selection. Indian J
Dermatol Venereol Leprol 1997; 63:296.
74. Kato H, Furuhashi T, Ito E, et al. Efficacy of 1-mm minigrafts in treating vitiligo
depends on patient age, disease site and vitiligo subtype. J Dermatol 2011;
38:1140.
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 26 of 29
75. Al-Mutairi N, Manchanda Y, Al-Doukhi A, Al-Haddad A. Long-term results of split-
skin grafting in combination with excimer laser for stable vitiligo. Dermatol Surg
2010; 36:499.
76. Khandpur S, Sharma VK, Manchanda Y. Comparison of minipunch grafting versus
split-skin grafting in chronic stable vitiligo. Dermatol Surg 2005; 31:436.
77. Chen YF, Yang PY, Hu DN, et al. Treatment of vitiligo by transplantation of
cultured pure melanocyte suspension: analysis of 120 cases. J Am Acad
Dermatol 2004; 51:68.
78. Guerra L, Primavera G, Raskovic D, et al. Erbium:YAG laser and cultured
epidermis in the surgical therapy of stable vitiligo. Arch Dermatol 2003; 139:1303.
79. Budania A, Parsad D, Kanwar AJ, Dogra S. Comparison between autologous
noncultured epidermal cell suspension and suction blister epidermal grafting in
stable vitiligo: a randomized study. Br J Dermatol 2012; 167:1295.
80. Thakur P, Sacchidanand S, Nataraj HV, Savitha AS. A Study of Hair Follicular
Transplantation as a Treatment Option for Vitiligo. J Cutan Aesthet Surg 2015;
8:211.
81. Vinay K, Dogra S, Parsad D, et al. Clinical and treatment characteristics
determining therapeutic outcome in patients undergoing autologous non-cultured
outer root sheath hair follicle cell suspension for treatment of stable vitiligo. J Eur
Acad Dermatol Venereol 2015; 29:31.
82. Mapar MA, Safarpour M, Mapar M, Haghighizadeh MH. A comparative study of
the mini-punch grafting and hair follicle transplantation in the treatment of
refractory and stable vitiligo. J Am Acad Dermatol 2014; 70:743.
83. Mulekar SV, Isedeh P. Surgical interventions for vitiligo: an evidence-based
review. Br J Dermatol 2013; 169 Suppl 3:57.
84. Gupta D, Kumari R, Thappa DM. Depigmentation therapies in vitiligo. Indian J
Dermatol Venereol Leprol 2012; 78:49.
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 27 of 29
85. Tan ES, Sarkany R. Topical monobenzyl ether of hydroquinone is an effective and
safe treatment for depigmentation of extensive vitiligo in the medium term: a
retrospective cohort study of 53 cases. Br J Dermatol 2015; 172:1662.
86. Grimes PE, Hamzavi I, Lebwohl M, et al. The efficacy of afamelanotide and
narrowband UV-B phototherapy for repigmentation of vitiligo. JAMA Dermatol
2013; 149:68.
87. Lim HW, Grimes PE, Agbai O, et al. Afamelanotide and narrowband UV-B
phototherapy for the treatment of vitiligo: a randomized multicenter trial. JAMA
Dermatol 2015; 151:42.
88. Graham A, Westerhof W, Thody AJ. The expression of alpha-MSH by
melanocytes is reduced in vitiligo. Ann N Y Acad Sci 1999; 885:470.
89. Kapoor R, Phiske MM, Jerajani HR. Evaluation of safety and efficacy of topical
prostaglandin E2 in treatment of vitiligo. Br J Dermatol 2009; 160:861.
90. Kapur R, Osmanovic S, Toyran S, Edward DP. Bimatoprost-induced periocular
skin hyperpigmentation: histopathological study. Arch Ophthalmol 2005;
123:1541.
91. Narang G. Efficacy and Safety of Topical Bimatoprost Solution 0.03% in Stable Viti
ligo: A Prelliminary Study. World Congress of Dermatology Seoul, Korea, June 20
11.
92. Grimes PE. Bimatoprost 0.03% Solution for the Treatment of Nonfacial Vitiligo. J
Drugs Dermatol 2016; 15:703.
93. Rothstein B, Joshipura D, Saraiya A, et al. Treatment of vitiligo with the topical
Janus kinase inhibitor ruxolitinib. J Am Acad Dermatol 2017.
94. Papadopoulos L, Bor R, Legg C. Coping with the disfiguring effects of vitiligo: a
preliminary investigation into the effects of cognitive-behavioural therapy. Br J
Med Psychol 1999; 72 ( Pt 3):385.
95. Mu EW, Cohen BE, Orlow SJ. Early-onset childhood vitiligo is associated with a
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 28 of 29
more extensive and progressive course. J Am Acad Dermatol 2015; 73:467.
96. Betterle C, Caretto A, De Zio A, et al. Incidence and significance of organ-specific
autoimmune disorders (clinical, latent or only autoantibodies) in patients with
vitiligo. Dermatologica 1985; 171:419.
Topic 106619 Version 5.0
https://www.uptodate.com/contents/vitiligo-management-an…=1~138&usage_type=default&display_rank=1#H4264468486 09/07/19, 10L47 AM
Page 29 of 29
S-ar putea să vă placă și
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Meeting The Physical Therapy Needs of Children - Effgen, Susan K. (SRG)Document797 paginiMeeting The Physical Therapy Needs of Children - Effgen, Susan K. (SRG)bizcocho4100% (7)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Myeloproliferative Disorders PDFDocument52 paginiMyeloproliferative Disorders PDFBoneyJalgar100% (3)
- Short Answer Questions AnaesthesiaDocument91 paginiShort Answer Questions AnaesthesiaMeena Ct100% (11)
- Biliary Tract Disease - Emmet AndrewsDocument52 paginiBiliary Tract Disease - Emmet AndrewsBoneyJalgarÎncă nu există evaluări
- Why I Desire to Study Medical MicrobiologyDocument2 paginiWhy I Desire to Study Medical MicrobiologyRobert McCaul100% (1)
- Vertigo and Dizziness Guide for Healthcare ProvidersDocument50 paginiVertigo and Dizziness Guide for Healthcare ProvidersAu Ah Gelap100% (1)
- Obstetric Analgesia PDFDocument45 paginiObstetric Analgesia PDFBoneyJalgar100% (1)
- CCN (Feu)Document71 paginiCCN (Feu)Ashley Nicole Lim100% (1)
- McKee's pathology of the skinDocument1 paginăMcKee's pathology of the skinBoneyJalgarÎncă nu există evaluări
- Biliary Tumors: Cholangiocarcinoma and Cancer of The Gall BladderDocument34 paginiBiliary Tumors: Cholangiocarcinoma and Cancer of The Gall BladderBoneyJalgarÎncă nu există evaluări
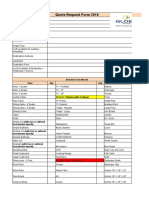
- Quote Request Form 2018: Articles To Be Moved Item Qty QtyDocument6 paginiQuote Request Form 2018: Articles To Be Moved Item Qty QtyBoneyJalgarÎncă nu există evaluări
- Form 1Document3 paginiForm 1BoneyJalgarÎncă nu există evaluări
- Biliary Tumors: Cholangiocarcinoma and Cancer of The Gall BladderDocument34 paginiBiliary Tumors: Cholangiocarcinoma and Cancer of The Gall BladderBoneyJalgarÎncă nu există evaluări
- Ectopic Features. 123 - RecoveredDocument13 paginiEctopic Features. 123 - RecoveredBoneyJalgarÎncă nu există evaluări
- Form 1Document3 paginiForm 1BoneyJalgarÎncă nu există evaluări
- InstructionsDocument1 paginăInstructionsnishtha_singhal_drÎncă nu există evaluări
- Ectopic Features. 123 - RecoveredDocument13 paginiEctopic Features. 123 - RecoveredBoneyJalgarÎncă nu există evaluări
- 27831Document20 pagini27831BoneyJalgarÎncă nu există evaluări
- Classifying The Illness in Young Infants ( 2Mths)Document9 paginiClassifying The Illness in Young Infants ( 2Mths)BoneyJalgarÎncă nu există evaluări
- Anesthesia and Analgesia in ObstetricsDocument45 paginiAnesthesia and Analgesia in ObstetricsBoneyJalgarÎncă nu există evaluări
- Anesthesia and Analgesia in ObstetricsDocument45 paginiAnesthesia and Analgesia in ObstetricsBoneyJalgarÎncă nu există evaluări
- Prevention & Early Outpatient Treatment Protocol For Covid-19Document4 paginiPrevention & Early Outpatient Treatment Protocol For Covid-19jack mehiffÎncă nu există evaluări
- RLE Manual EditedDocument68 paginiRLE Manual EditedReymondÎncă nu există evaluări
- Mental Status Examination - StatPearls - NCBI BookshelfDocument9 paginiMental Status Examination - StatPearls - NCBI BookshelfGRUPO DE INTERES EN PSIQUIATRIAÎncă nu există evaluări
- CONCEPT EpidemilologyDocument13 paginiCONCEPT EpidemilologyKrishnaveni MurugeshÎncă nu există evaluări
- An Analysis of Ethical Issues in Pharmaceutical IndustryDocument19 paginiAn Analysis of Ethical Issues in Pharmaceutical IndustrySuresh KodithuwakkuÎncă nu există evaluări
- Lily Grebe Resume 10Document3 paginiLily Grebe Resume 10api-482765948Încă nu există evaluări
- Arterial Disorders: Arteriosclerosis & AtherosclerosisDocument28 paginiArterial Disorders: Arteriosclerosis & AtherosclerosisManuel Jacob YradÎncă nu există evaluări
- Shalini Tummala ResumeDocument2 paginiShalini Tummala Resumeapi-385467850Încă nu există evaluări
- Tinnitus Today December 1998 Vol 23, No 4Document29 paginiTinnitus Today December 1998 Vol 23, No 4American Tinnitus AssociationÎncă nu există evaluări
- Food Safety Case - The Fat Duck Norovirus Outbreak, UK - 2009Document16 paginiFood Safety Case - The Fat Duck Norovirus Outbreak, UK - 2009OPGJrÎncă nu există evaluări
- Reducing the Risk of Infection in Diabetic PatientsDocument7 paginiReducing the Risk of Infection in Diabetic PatientsAnn Michelle TarrobagoÎncă nu există evaluări
- Doença Celiaca GuidelinesDocument45 paginiDoença Celiaca Guidelinesleonardo mocitaibaÎncă nu există evaluări
- CV DR Shilpa Kalra 2021Document10 paginiCV DR Shilpa Kalra 2021Shilpa Kalra TalujaÎncă nu există evaluări
- Fading Kitten Emergency Protocol: Hypothermia HypoglycemiaDocument1 paginăFading Kitten Emergency Protocol: Hypothermia HypoglycemiaJose Emmanuel MÎncă nu există evaluări
- IsmailDocument9 paginiIsmailapi-547285914Încă nu există evaluări
- Single-payer health care reduces inequality gapsDocument52 paginiSingle-payer health care reduces inequality gapsMetelitswagÎncă nu există evaluări
- Catalogue Rudolf - Instrument Surgical - PT. Graha IsmayaDocument172 paginiCatalogue Rudolf - Instrument Surgical - PT. Graha IsmayayuketamaÎncă nu există evaluări
- (14374331 - Clinical Chemistry and Laboratory Medicine (CCLM) ) Measurement Uncertainty - Light in The ShadowsDocument3 pagini(14374331 - Clinical Chemistry and Laboratory Medicine (CCLM) ) Measurement Uncertainty - Light in The ShadowsJulián Mesa SierraÎncă nu există evaluări
- CHF SIM - Preparation Questions and Notes For LPN StudentsDocument3 paginiCHF SIM - Preparation Questions and Notes For LPN Studentsmercy longÎncă nu există evaluări
- List Cebu AFFIL PHYSICIANS1 (Wo Neuro) - As of 09012011Document6 paginiList Cebu AFFIL PHYSICIANS1 (Wo Neuro) - As of 09012011Irish BalabaÎncă nu există evaluări
- Discharge PlanDocument4 paginiDischarge PlanPaul Loujin LeeÎncă nu există evaluări
- Dual Antiplatelet Therapy Vs Alteplase For Patients With Minor NondisablingDocument10 paginiDual Antiplatelet Therapy Vs Alteplase For Patients With Minor Nondisablingbetongo Bultus Ocultus XVÎncă nu există evaluări
- CT AuditsDocument53 paginiCT Auditsapi-3810976Încă nu există evaluări
- Chemoregimen - Testicular CancerDocument2 paginiChemoregimen - Testicular CancerNanda Asyura RizkyaniÎncă nu există evaluări
- Jurnal Ebn Managemen 1Document7 paginiJurnal Ebn Managemen 1KohakuÎncă nu există evaluări