Documente Academic
Documente Profesional
Documente Cultură
Notes in Pediatrics. 2 Ed. 2001/02 Senior & Junior Peds Rotations
Încărcat de
opis08Descriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Notes in Pediatrics. 2 Ed. 2001/02 Senior & Junior Peds Rotations
Încărcat de
opis08Drepturi de autor:
Formate disponibile
Notes in Pediatrics. 2nd ed.
2001/02
Senior & Junior Peds Rotations.
Genetics
READ MCCQE NOTES 2002 PEDIATRICS: GENETICS. IT COVERS WELL
DOWN, TURNER & KLINEFILTER SNDROMES.
Flat newborn = not breathing.
Achondroplasia:
AD.
Short limbs.
Guthrie test = test for phenyl-alanine screening.
Down synd:
P/E:
o Dysmorphic features.
o ENT exam: hearing test, otoscopy, eye tests.
o Heart exam.
o Resp exam: infection (due to immunity).
o Developmental:
Head lag.
Tone.
Smile.
Recommended investigations at 2 & 12 years: atlanto-occipital x-ray, Thyroid
Function tests (TFT), Echo.
Short girl + failure of sexual development think of Turner synd.
CFx:
o Has shield chest (broad chest).
o Can present in neonatal period with:
Coarctation of aorta + bicuspid aortic valve HF.
Edema of hand & feet.
Causes:
A. Non-dysjunction (commonest):
o Occur in meiosis I (commonest) or II.
o One mother cell has XX & other is empty:
B. Mosaic:
o XX cells + XO cells (might have menstruation but infertility). OR
o XO cells + XY cells.
Mx:
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 1 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
o GH.
o Estrogen at puberty 2° sexual characteristics, but before that, remove
any testes!
o Psychological support.
Evaluate short child:
o Upper: lower segment ratio.
o FHx.
Karyotyping = Chromosomal pattern.
Chromosomal analysis.
Cri de chat:
Abnormality in larynx.
5p-
Like cat cry disappears.
Severe MR.
Radiology
Lungs:
IRDS:
o In premature babies.
Wet lungs =Transient Tachypnea of Newborn (TTN):
o Delayed resorption of fetal fluid in lung after delivery.
If you don't see R. heart border PN in Right middle lobe.
Meconium aspiration.
Broncho-PN:
o Patchy infiltration of lung.
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 2 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
Diaphragmatic hernia:
o Bowel in chest (air bubbles) + scaphoid abdomen. (MCQ)
o Confirmation by:
Auscultating chest.
Ba meal.
Abdo / GU:
Palpable mass in abdo in neonates:
Causes:
1. Hydronephrosis: commonest: (MCQ in MCCEE)
o Do US.
o Most likely due to post. Urethral valve.
2. Wilm's tumor calyceal system distorted.
3. Polycystic kidney a/w liver cysts:
o In 100% in infantile type.
o In 30% in adult type.
Ix:
o US.
o Voiding Cysto-Urethro-Gram (VCUG) = Micturation urethrogram.
Fill bladder take out catheter.
Tracheo-esophageal fistula:
o Eat cough & vomit.
o Ix: plain abdominal x-ray (AXR), NG tube.
o Confirmation: Ba swallow.
Heart:
Congenital cardiac disease.
Cyanotic (blue babies) Tetralogy of Fallot:
o Best appearance on CXR: boot-shaped.
o Echo.
How to read an XR:
1. AP / Lateral.
2. Inspiration vs. expiration.
o > 5 & 1/2 of anterior ribs OR 9 posterior ribs good inspiratory film.
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 3 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
3. Bones fractures + soft tissue abnormality.
4. Heart shadow + silhouette + size: 1/2, ↓ in hyperinflated lung.
5. Lung field:
o Infiltration.
o Pulm. Vascularity.
6. Diaphragm:
o Flattened & pushed down in hyper-aeration.
7. check costophrenic angle: if obliterated pleural effusion.
Veno-occlusive disease:
o Stricture in hepatic venules.
o Big hepatic veins are patent.
Budd-Chiare synd:
o Hepatic vein occluded.
o a/c: occlusion + ascites.
o Chronic: collateral veins inside liver occluded in both lobes.
Caroli synd:
o a/w infantile polycystic kidney.
o a/w congenital hepatic fibrosis Portal HTN.
Peds Surgery
Foreign body aspiration
Objects which can be analyzed chemically e.g. battery should not be let into GI
tract you must take them out.
Partial occlusion:
o Most foreign bodies are not visible on CXR because they're not round
partial occlusion (ball-valve mechanism) = air goes in, but not out. (MCQ)
o On XR blackness in affected lung + diaphragm flattened in affected side.
Complete occlusion:
o e.g. rubber of pencil, uncooked nuts.
o You might see white lung (bottle neck appearance).
Criteria for Dx: (MCQ)
o Hx: choking.
o P/E: wheezing (unilateral, in anterior chest)
Mx:
o Immediate bronchoscopy & removal of foreign body.
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 4 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
o Should be done by expert, otherwise ↑ mortality.
N.B. In adults complete obstruction (e.g. tooth) atelectasis fever.
Pulm sequestration
o 85% in postero-lateral area of (L) lobe.
o Liable to infection.
Aspiration synd
In R. upper lung.
Because babies are put in supine position.
Babies don't handle swallowing properly.
Causes:
1. GERD:
o Sometimes presents without organic cause gastric acid burns vocal cords.
o Indications for anti-reflux surgery:
Diaphragmatic hernia.
TE fistula.
o Surgery seldom done before 9 months.
2. Vascular ring:
o a/w double aortic arch.
o Presents with repeated infection.
o Have musical resp (noisy).
3. H-type TE fistula.
4. Hiatus hernia.
5. Compression (polyps, bronchial adenoma).
6. Neurological:
a. Laryngo-pharyngeal neurological disproportion Self-limiting.
b. Laryngo-pharyngeal dysplasia permanent.
Ix:
o Tube pressure upper esophagogram.
o CT of nasopharyngeal area: one study only has shown its benefit!
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 5 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
Nephrology
If you want to Ix palpable kidney:
o Daily wt.
o BUN, Creatinine.
o Electrolytes.
o Hb.
o Urinalysis.
o US hydronephrosis, polycystic kidney.
o Voiding cysto-urethrogram (VCUG).
Berger's disease = IgA nephropaty
Hematuria (doesn't harm pt): coca-cola urine.
Proteinuria (harms pt) ACEi
changes pressure b/w afferent & efferent arterioles ↓GFR ↓ proteinuria.
Use Captopril no response ↑ dose no response change to Enalpril 5 mg/day bd.
Do Creatinine clearance: collect 24 hr urine (0.45 X Height) / S-Cr (mg/dL).
Normal proteinuria = up to 100 mg/m2/24 hrs (4.2 mg/m2/hr)
[MCQ in NMBE]
Nephrotic synd
Proteinuria > 40 mg/m2/hr + hypoalbuminemia + edema +
hypercholesterolemia.
If severe pleural effusion + ascites.
Hypercoagulability renal vein thrombosis (rare, due to loss of anti-thrombin
III in urine).
Infections (loss of factor B ↓ opsonization E. coli, Pneumococcus):
cellulitis, spontaneous bacterial peritonitis (SPB), bacteremia.
Mx:
o Non-pharmacologic:
1. No added salt diet. Fluid restriction not necessary.
2. Thiazide diuretics
If uncomfortable from edema.
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 6 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
If aggressive diuresis risk of hypercoagulability.
o Pharmacologic: Prednisolone:
2 mg/Kg/day X 6 weeks same dose alternating day for another 6
weeks Taper.
o Relapse:
Pt usually relapse during Autumn & Spring ? allergy component.
3. Prednisolone:
2 mg/Kg/day X 6 weeks same dose alternating day for another 6
weeks Taper.
4. No improvement biopsy.
5. Cyclophosphamide:
In multiple relapses ≥ 3 X / year OR steroid-dependent.
Cytotoxic BM suppression, affects testes: azoospermia, infertility,
hemorrhagic cystitis.
Use it for ONE month.
Post-Strep GN:
Ix ASO:
Takes 2 weeks to rise, 70% of pts are (+).
0% ASO titer If preceded skin infection e.g. impetigo caused by Strep.
Chronic Renal Failure = S-Cr > 200 μmol/L X 2 months.
When child is growing (approaching puberty) ↑S-Cr ↑ Cr clearance
(glomerular hypertrophic theory) ↓ Protein intake.
Child born with multicystic dysplastic kidney + hydronephrosis in contra-lateral
kidney, due to UPJ obstruction.
↑ Demand ↑S-Cr ↓ Protein intake for lifetime.
DDx of nephrocalcinosis:
1. 1° Hyper-oxaluria: inherited.
2. Hyper-parathyroidism.
3. Renal tubular acidosis (RTA): distal type.
You see calcifications in kidney on US.
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 7 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
Metabolic acidosis (H+ retention, HCO3- loss).
Hypercholesterolemia.
RTA or Steroid Rx.
7 years old boy, local presented with fever, dysphagia. On P/E you ruled out
meningitis, otitis media & pneumonia. He has fiery throat, and anterior cervical
LNs.
N.B. Bacterial tonsillitis (Strep pyogenes):
1. Sudden.
2. Without URTI.
3. Fever.
4. Fiery throat.
5. Anterior cervical LNs.
Management: Penicillin:
Penicillin G (250-500 mg) or 200,000-400,000 units, tid, X 3 days.
OR 1 shot IM Benzyl Penicillin (comes usually with procainamide).
N.B. Penicillin G = IV Benzyl Penicillin.
Penicillin V = Oral Benzyl Penicillin.
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 8 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
Hematology
Hb structure & production:
Fetal Hb, HbF, (α2γ2) switches to adult forms HbA (α2β2) & HbA2 (α2δ2) at 3-6
months of life.
Thalassemia:
RDW (Red cell Distribution Width) is normal = RBCs have same size,
compared to Fe+ deficiency anemia (RDW ↑).
Heterozygous = β Thalassemia minor:
o Point mutation/ deletion of 1 or 2 of β globin genes.
o CFx: mild/ no anemia + spleen may be palpable.
o Dx:
CBC normal / mild ↓ in Hb + MCV < 70 (microcytic anemia).
Peripheral blood film:
Microcytosis hypochromia.
Target cells.
Basophilic stippling.
Hb electrophoresis: ↑ HbA2 to 2.55%. (MCQ)
o Mx: no necessary Rx:
Homozygous = β Thalassemia major (Cooley's anemia):
o Pathophysiology:
Ineffective β chains synthesis excess α chains relative to β chain
ineffective erythropoiesis & hemolysis of RBC compensatory ↑ HbF.
o CFx:
Start presenting at 3-6 months, due to replacement of HbF by HbA.
Severe anemia in 1st year of life.
Jaundice.
Stunted growth & development.
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 9 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
Gross hepatosplenomegaly extra-medullary hematopoiesis.
Skeletal changes due to expanded marrow activity:
Frontal bossing + maxillary hypertrophy with exposure of upper teeth +
flattened nasal bridge.
Skill x-ray has "hair on end" appearance expanded diploic spaces.
Cortical thinning of long bones pathological fractures.
Evidence of ↑ Hb catabolism (e.g. gallstones).
Death from:
1. Untreated anemia.
2. Infection.
3. Hemochromatosis (late, secondary to transfusion).
o Dx:
CBC ↓ Hb + normal RDW.
Peripheral blood film:
Hypochromic microcytosis.
Basophilic stippling.
Target cells.
↑ Retics.
Hb electrophoresis HbA (0-10%) + HbF (90-100%)
Skull x-ray.
o Mx:
Hyper-transfusion: q 3-4 weeks prevents marrow expansion.
Fe+ chelator (Desferrioaxamine) is given IV in special pumps for 6 nights
whenever there's blood transfusion prevent iron overload.
Folic acid supplements.
HBV vaccine.
α Thalassemia:
o Pathophysiology:
AR.
Defect of α chains.
4 grades of severity depending on number of defective α genes:
Silent.
Trait.
Hb H disease (present in adults).
Hb Bart's (γ4) = hydrops fetalis not compatible with life!
o Dx:
Peripheral blood film: microcytosis, hypochromia.
N.B. Hb electrophoresis not diagnostic!
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 10 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
o Mx: same as β Thalassemia.
Sickle Cell Anemia: [PMP, MCQ]
AR. ↑ Incidence in Blacks & Mediterranean.
Amino acid substitution of Valine for Glutamate in position of 6 of β globin
chain.
Features appear after 6-9 months of age with fall in fetal Hb, anemia, jaundice,
splenomegaly.
Mechanism of sickling:
Heterozygous (Hb S trait)
o Sickling occurs @ pO2 of 40 mmHg.
o Pt appears normal except at times of extreme hypoxia & infection.
o Dx:
CBC normal Hb.
Peripheral blood normal except for a few target cells.
Hb electrophoresis (confirmatory test) Hb A (65%), Hb S (35%).
Homozygous (Hb S disease):
o Sickling occurs @ pO2 of 80 mmHg.
o CFx:
1. Hemolytic crisis = Chronic hemolytic anemia + Jaundice.
2. Vaso-occlusive (infarctive) crisis =
Pain + fever + leukocytosis.
Organs affected include:
Ankle leg ulcers.
Abdo:
Intestine a/c abdo.
Gallbladder stones.
Spleen
Enlarged in children, but atrophic in adults.
Susceptibility to infections by encapsulated organisms by 5
years due to auto-infarction.
Lung acute chest synd.
Brain stroke, seizures.
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 11 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
Others: eye (hemorrhage), kidney (hematuria), penis (priapism),
femoral head (aseptic necrosis).
Retarded growth & development.
3. Aplastic crisis = transient RBC aplasia after parvovirus B19 infection (↓ Retics,
↓ Hb).
4. Splenic sequestration crisis = sickling in spleen large pooling of blood with
acute ↓ Hb, shock (↑ Retics).
o Dx:
Peripheral blood sickled cells.
Screening test: sickle cell prep.
Hb electrophoresis (confirmatory test) Hb S > 80%.
Mx:
o Prevention of crisis is the key:
Avoid conditions that favor sickling (hypoxia, acidosis, dehydration, fever).
Vaccination in childhood (pneumococcus, meningococcus).
Prophylactic daily Penicillin V (oral).
Good hygiene & nutrition (e.g. folic acid to avoid folate deficiency).
o Hydroxyurea:
If frequent crises.
Enhances production of HbF presence of HbF in Hb SS ↓polymerization
& precipitation of Hb S.
S.E. Cytotoxic BM suppression!
Precipitating factors of vaso- Mx
occlusive crisis
Hypoxia. O2.
Dehydration. Hydration (↓ viscosity).
Infection. Anti-microbials.
Acidosis. Correct acidosis.
Analgesia / narcotics.
Mg+ (inhibits K+ & H2O efflux from RBC
prevents dehydration).
Exchange transfusion if stroke.
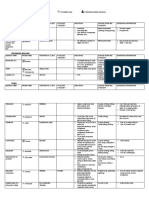
Hb electrophoresis confirms clinical suspicion of thalassemia & sickle cell
disease.
HbA HbA2 HbF
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 12 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
Adults 97% 2% 2-5%
SS S Normal ↑↑↑
SA SA Normal ↑
β Thal major - Normal ↑↑
β Thal minor A ↑ Slight ↑
Intra-medullary hemolysis = ineffective erythropoeisis.
Causes of epistaxis:
Local:
o Injury & trauma.
Systemic:
o Coagulation diseases.
o HTN.
Henoch-Schönlein purpura: [PMP, MCQ]
o Purpuric, petechial rash in lower limbs + extremities.
o Abdo pain:
Vasculitis: affects kidney.
Perforation, hemorrhage.
Intussusception.
Hemolytic Uremic Syndrome (HUS):
o If you suspect HUS look @ schistiocytes & helmet cells in blood film.
In acute hemolysis:
o Transfusion should be done if Hb < 6 mg/dL.
o You don't have to bring Hb to normal levels (contrary to thalassemia).
o Give Packed RBC (10-15 mL/Kg) small transfusion over 4 hours.
o Cx: Pulm edema.
Monitor clinically & give Lasix (Frusemide) half way during transfusion.
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 13 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
Miscellaneous
Signs of dehydration:
o Vitals: ↓ BP + Tachycardia.
o Oligouria.
o Depressed fontanelles.
o Sunken eyes + not tearing.
o Dry mouth.
o Loss of skin turgor.
o Cold extremities hypovolemia.
o Altered sensorium.
N.B. If child is crying with tears not dehydrated.
If child is severely dehydrated bolus of N/S (20 mL/Kg X 30 min).
Anion Gap (AG):
Normal AG = Na+ - (HCO3- Cl-)
Metabolic acidosis:
Normal (up to 13) ↑
DURHAM MUD PILES
o Gastro-enteritis (Diarrhea). o Alcohol: Methanol / Ethanol.
o Ureteral diversion. o Uremia.
o RTA = Renal Tubular Acidosis o DKA.
o Hyperalimentation.
o Ammonium chloride / o Paraldehyde ingestion.
Acetazolamide. o Ischemia Lactic acidosis.
o Miscellaneous: o Ethylene glycol.
CaCl ingestion. o ASA intoxication.
Cholystramine.
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 14 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
Hyperparathyroidism.
Congenital hypothyroidism
o Usually T4 is screened using cord blood on day 4 of life, after child has been
breast-fed.
Hyperthyroidism hypothyroidism.
CAH: [common MCQ]
AR. Commonest enzyme deficiency is 21 Hydroxylase.
Collapse in 2nd week of life.
Ambiguous genitalia
With salt losing.
Mx:
o Hydrocortisone (Cortef) for life.
o Surgery for girls feminizing genitoplasty / clitoroplasty.
How to know if mass is spleen:
1. Moves with respiration.
2. Presence of notch.
3. You can't get over it.
4. Dullness on percussion.
5. Location: left hypochondrium.
6. Enlargement might continue to RIF (right iliac fossa).
How to know if mass is liver:
1. Moves with respiration.
2. You can't get over it.
3. Dullness on percussion which continues to the ribs.
4. Location: right hypochondrium.
5. Enlargement might continue to LIF (left iliac fossa).
DDx of a child with fever + rigors:
1. UTI.
2. Malaria.
3. Pus somewhere (abscess).
Shigellosis:
o Dysentery & other features of GE + seizure (MCQ in NMBE)
Cow's milk has:
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 15 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
o ↑ Proteins.
o ↓↓ Glu.
o ↓ Ca+.
o Caseine.
o Only 10% of Fe+ is absorbed.
o In a newborn:
You can give him cow's milk, but dilute it with H2O + add sugar.
Tubular immaturity hyper-phosphatemia + hypocalcemia
convulsions!
Malnutrition: [OSCE question]
Child with malnutrition:
o Check SC issue (wasted).
o Buttocks wasted.
o Abdo distended due to weakness of rectus abdominis.
o Ribs prominent due to intercostal muscles wasting.
o Peripheral edema:
+ Kwashiorkor (scarce red hair) edema hypo-albuminemia low
protein-to-energy.
marasmus.
o Apathetic.
Malnourished nutrients:
o Proteins.
o Fat.
o Vitamins (ADEK):
Vit A Xerophthalmia, Night blindness.
Vit D Rickets (bowing of legs, rachitic rosary, swelling of wrist bones
earliest, craniotabes, delayed closed fontanels, ↑ALP).
+
o Fe def.
DDx of malnutrition Malabsorption:
1. Infection (Giardiasis).
2. CF.
3. Celiac disease.
4. Cow's milk protein intolerance
5. Lactose intolerance.
Atopic dermatitis: [OSCE]
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 16 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
o Redness in cheeks.
o Mx:
Moisturizers.
Topical steroids if exacerbated.
To determine activity of SLE anti-dsDNA Abs (most sensitive test).
DDx of silent abdomen:
1. Peritonitis.
2. Paralytic ileus hypokalemia (esp. it pt. is vomiting).
3. Intussusception.
Monosaccharide intolerance:
Brush borders in intestine is gone (e.g. in gastroenteritis).
If glucose (C6H12O6) is not absorbed Goes to intestine
bacteria ferment it to acid pH in stool.
Give glucose IV.
You can give child oral glucose slowly give chance for brush borders to be
re-built.
Slowly give fructose (gram by gram) & watch out pH & reducing substance in
stool.
Normal saline can be given in:
1. Pure vomiting.
2. Hypovolemia.
If ESR ↑ + Normal CRP Collagen vascular disease (SLE)
↑ γ-globulin:
1. Parasitic (malaria, L. donovani).
2. Collagen vascular disease.
Every 30 mL (ounce) of breast milk 20 Kcal
Breast-feeding should provide 120 Cal/Kg.
If a child is 3 Kg 3 X 120 = 360 Cal / day.
30 mL 20 Cal.
X mL 360 Cal.
X = 480 mL. This child should be given 480 mL of breast milk.
Normal range of CRP (C-Reactive Protein) < 6 mg/L.
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 17 of 18
Notes in Pediatrics. 2nd ed. 2001/02
Senior & Junior Peds Rotations.
↑ Frequency sound = like the voice of a woman.
↓ Frequency sound = like the voice of a man (deep sound).
Peritone = Chlophineramine
Iron syrup = Ferinole:
o For Fe+ def.
o 30 mg/ 5 mL give 6 mg/Kg/day.
If child has GE + PN You give AB (though it might worsen the diarrhea).
I saw a child with dysmorphic features:
o Hyper-telorism = widening of space of eyes.
o Fanning of ear.
o Low set hair line.
o Macroglossia.
o ↑ HC.
I saw a case of Laurence-Moon-Biedl syndrome:
1. Polydactyly
2. Obesity
3. Hyperphagia
4. Retinal problems.
5. Hypogonadism.
Pontine hemorrhage:
– Child had RTA.
– Pinpoint pupil.
– Fever.
– Apneustic breathing.
Oculo-cerebro-renal disease:
o XD inheritance.
o Eye band keratopathy, cataract.
o Kidney RTA.
o MR.
Dr. Khalid A. Yarouf Al-Naqbi. (Intern) Page 18 of 18
S-ar putea să vă placă și
- Neurology Multiple Choice Questions With Explanations: Volume IIDe la EverandNeurology Multiple Choice Questions With Explanations: Volume IIEvaluare: 5 din 5 stele5/5 (2)
- Essential Revision Notes in Paediatrics For The MRCPCH From PastestDocument7 paginiEssential Revision Notes in Paediatrics For The MRCPCH From Pastestarshad100% (1)
- Ankit Yadavendra - Solved Papers Pediatrics For PG Students 3EDocument1 paginăAnkit Yadavendra - Solved Papers Pediatrics For PG Students 3ESham100% (1)
- How To Assess Development in The MRCPCH Clinical ExamDocument9 paginiHow To Assess Development in The MRCPCH Clinical Exammma24100% (2)
- Essential Revision Notes in Paediatrics For The MRCPCH Third EditionDocument26 paginiEssential Revision Notes in Paediatrics For The MRCPCH Third EditionNadejda MarcovaÎncă nu există evaluări
- MRCPCH Clinical The Whole Book PDFDocument108 paginiMRCPCH Clinical The Whole Book PDFtheva_thy100% (3)
- Development Assessment MRCPCH WebsiteDocument1 paginăDevelopment Assessment MRCPCH WebsiteRajiv Kabad100% (3)
- Paediatrics MCQsDocument5 paginiPaediatrics MCQsbalarajuuk100% (1)
- OSCE PaediatricsDocument54 paginiOSCE Paediatricsmoh86-100% (8)
- Nelson 20th MCQDocument593 paginiNelson 20th MCQcharlesy T89% (19)
- Pediatrics Oral ExamDocument13 paginiPediatrics Oral ExamOmar Nayef TaaniÎncă nu există evaluări
- Essentials of Pediatric Emergency MedicineDe la EverandEssentials of Pediatric Emergency MedicineEvaluare: 4.5 din 5 stele4.5/5 (3)
- NCP Risk For Activity IntoleranceDocument4 paginiNCP Risk For Activity IntoleranceBAGUIO CATSÎncă nu există evaluări
- Long Cases ABM ABDULLAH 1st Edition PDFDocument844 paginiLong Cases ABM ABDULLAH 1st Edition PDFProthoma Dey64% (11)
- Q3 - Lesson-Plan Cot English 7Document8 paginiQ3 - Lesson-Plan Cot English 7juvelyn abugan100% (2)
- Dermatology Mini-OSCEDocument322 paginiDermatology Mini-OSCEMarrkÎncă nu există evaluări
- Paediatrics NotesDocument111 paginiPaediatrics NotesShobhit Prasad100% (3)
- Board Review: PediatricsDocument215 paginiBoard Review: Pediatricsokurimkuri94% (16)
- Paediatric Rashes: Ali Faisal SaleemDocument51 paginiPaediatric Rashes: Ali Faisal Saleemarjumand100% (3)
- Case Files PedsDocument54 paginiCase Files PedsSam ZeezÎncă nu există evaluări
- 250 Questions For The MRCPCH Part 2Document250 pagini250 Questions For The MRCPCH Part 2doctor aabiÎncă nu există evaluări
- Ern MRCPCHDocument24 paginiErn MRCPCHPasTestBooksÎncă nu există evaluări
- How To Pass MRCPCH - How To StudyDocument5 paginiHow To Pass MRCPCH - How To Studyalex pinto100% (1)
- MRCPCH Guide New QuestionsDocument11 paginiMRCPCH Guide New QuestionsRajiv Kabad100% (1)
- PediatricsDocument80 paginiPediatrics@r@mis100% (16)
- Mcqs PediatricsDocument155 paginiMcqs PediatricsAhmed Kh. Abu Warda100% (1)
- MRCPCH Clinical Exam TechniqueDocument34 paginiMRCPCH Clinical Exam TechniqueRajiv Kabad50% (2)
- MRCPCH Clinical Exam TechniqueDocument36 paginiMRCPCH Clinical Exam TechniqueHaoKeat Hoe100% (5)
- MRCPH PDFDocument972 paginiMRCPH PDFANDRE MAÎncă nu există evaluări
- Abdominal Examination Guide - MRCPCH Clinical RevisionDocument16 paginiAbdominal Examination Guide - MRCPCH Clinical Revisionbairdman12Încă nu există evaluări
- MRCPCH DhanDocument26 paginiMRCPCH DhanRajiv KabadÎncă nu există evaluări
- Pediatrics BookDocument53 paginiPediatrics BookMobin Ur Rehman Khan100% (1)
- Long Case PaedDocument21 paginiLong Case Paedwhee182Încă nu există evaluări
- Osce in Paedo + AnswersDocument96 paginiOsce in Paedo + Answersoluseye100% (2)
- The Following Drugs Are Safe in Breast-Feeding:: AccidentsDocument2 paginiThe Following Drugs Are Safe in Breast-Feeding:: AccidentsRajiv KabadÎncă nu există evaluări
- MRCPCH A&b NotesDocument16 paginiMRCPCH A&b NotesRajiv Kabad100% (1)
- Metabolic Alkalosis: Features of Crohn'S DiseaseDocument15 paginiMetabolic Alkalosis: Features of Crohn'S DiseaseRajiv Kabad100% (1)
- MRCPCH GuideDocument9 paginiMRCPCH GuideRajiv KabadÎncă nu există evaluări
- MRCPCH PART 1 BlogDocument6 paginiMRCPCH PART 1 BlogJooyee BrendaÎncă nu există evaluări
- Step On To Paediatrics 4th EditionDocument376 paginiStep On To Paediatrics 4th EditionTawhid Zihad100% (1)
- Pediatric NotesDocument45 paginiPediatric NoteskkkssbbÎncă nu există evaluări
- Paediatrics in PictureDocument21 paginiPaediatrics in PictureSana Bushra100% (18)
- P.G. Curriculum MD Pediatrics Index: 1. GoalsDocument17 paginiP.G. Curriculum MD Pediatrics Index: 1. GoalsCh RajeshÎncă nu există evaluări
- MRCPCH 1aDocument21 paginiMRCPCH 1aLoai El100% (1)
- PediatricsDocument58 paginiPediatricsbashir019Încă nu există evaluări
- Pediatrics Examination ReviewDocument223 paginiPediatrics Examination Reviewgarlic100100% (15)
- Paediatric Examination Handbook 2015Document66 paginiPaediatric Examination Handbook 2015Ulfa Rahmadanti SetiawanÎncă nu există evaluări
- 09-Pediatrics in Review, September2009 PDFDocument71 pagini09-Pediatrics in Review, September2009 PDFMobin Ur Rehman KhanÎncă nu există evaluări
- Scenarios For MRCPCHDocument11 paginiScenarios For MRCPCHsayedm100% (1)
- MRCPCH Guide DevDocument16 paginiMRCPCH Guide DevRajiv KabadÎncă nu există evaluări
- Guide To MRCPCH Examinations 18.08.11Document18 paginiGuide To MRCPCH Examinations 18.08.11Subhash MadireddyÎncă nu există evaluări
- EMQ For MRCPCH Part 1Document593 paginiEMQ For MRCPCH Part 1Kyaw Zin HtetÎncă nu există evaluări
- OSCE in Pediatrics, 2011Document267 paginiOSCE in Pediatrics, 2011floare de colt0% (1)
- The Unofficial Guide to Paediatrics: Core Curriculum, OSCEs, clinical examinations, practical skills, 60+ clinical cases, 200+MCQs 1000+ high definition colour clinical photographs and illustrationsDe la EverandThe Unofficial Guide to Paediatrics: Core Curriculum, OSCEs, clinical examinations, practical skills, 60+ clinical cases, 200+MCQs 1000+ high definition colour clinical photographs and illustrationsEvaluare: 2.5 din 5 stele2.5/5 (2)
- Problem-based Approach to Gastroenterology and HepatologyDe la EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisÎncă nu există evaluări
- Congenital Heart Diseases, A Simple Guide to these Medical ConditionsDe la EverandCongenital Heart Diseases, A Simple Guide to these Medical ConditionsÎncă nu există evaluări
- INTENSIVE CARDIOVASCULAR NURSING NotesDocument19 paginiINTENSIVE CARDIOVASCULAR NURSING NotesZayne Lucas Gabrielle TadiamonÎncă nu există evaluări
- Group Activity (Prenatal Assessment Form)Document8 paginiGroup Activity (Prenatal Assessment Form)The Mortal HowlerÎncă nu există evaluări
- Pedrosa Et Al. (2020) - Emotional, Behavioral and Psychological Impact of The COVID-19 PandemicDocument18 paginiPedrosa Et Al. (2020) - Emotional, Behavioral and Psychological Impact of The COVID-19 PandemicTangerine TannsÎncă nu există evaluări
- ND RDDocument10 paginiND RDOdyÎncă nu există evaluări
- Psychiatry Made EasyDocument14 paginiPsychiatry Made EasyD. W. S JayarathnaÎncă nu există evaluări
- Cerebral Palsy (CP) : DR Raj Kumar Yadav Assist. Prof., PMR MBBS VI Sem. - 25/04/2019Document38 paginiCerebral Palsy (CP) : DR Raj Kumar Yadav Assist. Prof., PMR MBBS VI Sem. - 25/04/2019Anjali GuptaÎncă nu există evaluări
- Arthritis: Lecture By: M.K. SastryDocument17 paginiArthritis: Lecture By: M.K. SastryOmar Duran CastroÎncă nu există evaluări
- Childwell Training - Food Hygiene Level 2 Course ManualDocument14 paginiChildwell Training - Food Hygiene Level 2 Course ManualJohnÎncă nu există evaluări
- Nose ENT D&R AgamDocument131 paginiNose ENT D&R AgamS Balagopal SivaprakasamÎncă nu există evaluări
- Familial Dilated Cardiomyopathy of Young Portuguese Water DogsDocument9 paginiFamilial Dilated Cardiomyopathy of Young Portuguese Water DogsJessareth Atilano CapacioÎncă nu există evaluări
- Bio All Phylum SummaryDocument7 paginiBio All Phylum SummaryAbhishek yadavÎncă nu există evaluări
- CBSE Class 9 Science Worksheet - Why Do We Fall IllDocument2 paginiCBSE Class 9 Science Worksheet - Why Do We Fall Illkavita sengarÎncă nu există evaluări
- Management Guide: For Laying Hens in Deep Litter, Perchery and Free-Range SystemsDocument34 paginiManagement Guide: For Laying Hens in Deep Litter, Perchery and Free-Range SystemsSri PurwantiÎncă nu există evaluări
- Thesis For Depression Research PaperDocument7 paginiThesis For Depression Research Papergj9zvt51100% (2)
- PWS APEX WriteupDocument1 paginăPWS APEX WriteupJosh BaptieÎncă nu există evaluări
- What Is TuberculosisDocument4 paginiWhat Is TuberculosisJonah Camille Yap FortunaÎncă nu există evaluări
- Complex PTSDDocument21 paginiComplex PTSDRyne ZuziÎncă nu există evaluări
- Croup: Dr. Shveta Sethi Narula A.P. MicrobiologyDocument14 paginiCroup: Dr. Shveta Sethi Narula A.P. Microbiology12. Akshit AtwalÎncă nu există evaluări
- CONTINGENCY PLAN - New Pangasinan ESDocument22 paginiCONTINGENCY PLAN - New Pangasinan ESRoland Doctor-GonzalesÎncă nu există evaluări
- Blood and Tissue Flagellates BSCDocument27 paginiBlood and Tissue Flagellates BSCSisay FentaÎncă nu există evaluări
- The Importance of Plants To HumansDocument36 paginiThe Importance of Plants To HumansAnnie Vidanes LegaspiÎncă nu există evaluări
- Budgeting in Health Care System in IndiaDocument16 paginiBudgeting in Health Care System in IndiaABINASHÎncă nu există evaluări
- Emotional and Behavioral DisordersDocument13 paginiEmotional and Behavioral DisordersIrene FriasÎncă nu există evaluări
- Waxing Full Leg (Final)Document5 paginiWaxing Full Leg (Final)Lionel YdeÎncă nu există evaluări
- 2023 UA Paper Solved by HannanDocument47 pagini2023 UA Paper Solved by HannanHannan syedÎncă nu există evaluări
- ANS - Simulated Exam 06 - Respiratory, Gastrointestina & Hepatobiliary Disorders QuestionnaireDocument5 paginiANS - Simulated Exam 06 - Respiratory, Gastrointestina & Hepatobiliary Disorders QuestionnaireLander EslaoÎncă nu există evaluări