Documente Academic
Documente Profesional
Documente Cultură
AKI
Încărcat de
Winona Jennifer0 evaluări0% au considerat acest document util (0 voturi)
30 vizualizări1 paginăPenjelasan mengenai aki
Drepturi de autor
© © All Rights Reserved
Formate disponibile
DOCX, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentPenjelasan mengenai aki
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
30 vizualizări1 paginăAKI
Încărcat de
Winona JenniferPenjelasan mengenai aki
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 1
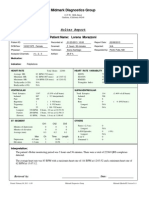
Angiotensin converting enzyme, or
ACE, as it is known, is secreted by our
lungs in response to low blood pressure
or decreased blood volume
(hypovolemia), and it converts
angiotensin I into a more powerful
vasoconstrictor, angiotensin II.
Angiotensin II acts on the renal
vasculature to constrict efferent
arteriole, in order to maintain
glomerular filtration rate (GFR). This in
turn, also leads to increase in the blood
pressure, as concomitantly secreted
aldosterone helps in fluid and salt
conservation by the kidneys.
In diseases like hypertension and
diabetes mellitus, nephropathic and vascular injuries result in increased amount of protein being filtered by the glomerulus, which
is subsequently lost in the urine.
ACE inhibitors, such as enalapril, captopril, etc., stop this
entire cascade from forming, by inhibiting the ACE enzyme.
Hence, a reduction in the GFR will also reduce the amount
of protein being filtered by the nephrons, thus, serving the
dual function of reducing the
hypertension/hypervolemia/hypernatraemia and reducing
the proteinuria.
One has to be careful in prescribing these medications to
those patients who have preexisting renal artery stenosis,
especially when present bilaterally, because an ACE
mediated vasoconstriction of the efferent arteriole is what is
keeping the flitration pressure from dropping, which will
reduce GFR, and with that, cause renal failure.
Reduced perfusion pressure with an angiotensin-
converting enzyme
inhibitor (ACE-I) or an angiotensin receptor blocker
(ARB). Loss of angiotensin II action reduces efferent
resistance; this causes the glomerular
capillary pressure to drop below normal values and
the GFR to decrease. (From JG Abuelo: N Engl J Med
357:797-805, 2007; with permission.)
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5795)
- P7b11toc Gastroenterology and NutritionDocument19 paginiP7b11toc Gastroenterology and NutritionWidya Lestari CapawatyÎncă nu există evaluări
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Breech BirthDocument10 paginiBreech Birthcirlce:twoworldsconnectedÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Infection Control in ORDocument10 paginiInfection Control in ORaaminah tariqÎncă nu există evaluări
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Osteogenesis ImperfectaDocument1 paginăOsteogenesis ImperfectaAdelia Putri Kharisma DewiÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Announcement BIRCDocument8 paginiAnnouncement BIRCHendarsyah SuryadinataÎncă nu există evaluări
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Prometric SoalDocument42 paginiPrometric SoalSandra IrhamÎncă nu există evaluări
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Breastfeeding FinalDocument25 paginiBreastfeeding FinalWengel RedkissÎncă nu există evaluări
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Introduction To Serology - Immunology, HSV & H.pyloriDocument37 paginiIntroduction To Serology - Immunology, HSV & H.pyloritriaclaresiaÎncă nu există evaluări
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- Taking Anthropometric Measurements of NewbornDocument25 paginiTaking Anthropometric Measurements of NewbornClarissa MaglalangÎncă nu există evaluări
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- Prepare A Plan of Establishment of ICU: Intensive Care UnitDocument9 paginiPrepare A Plan of Establishment of ICU: Intensive Care UnitNikhil SawantÎncă nu există evaluări
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Assignment # 1Document4 paginiAssignment # 1Abrar AhmadÎncă nu există evaluări
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Bedside Emergency Cardiac Ultrasound in ChildrenDocument11 paginiBedside Emergency Cardiac Ultrasound in ChildrenNikhil KumarÎncă nu există evaluări
- 2021-10-07 St. Mary's County TimesDocument32 pagini2021-10-07 St. Mary's County TimesSouthern Maryland OnlineÎncă nu există evaluări
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Diagnosis Management of HypertensionDocument23 paginiDiagnosis Management of Hypertensionarahman168Încă nu există evaluări
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Uganda - Advanced HIV Disease - Screening ToolDocument47 paginiUganda - Advanced HIV Disease - Screening Toolithran khoÎncă nu există evaluări
- Nursing Care Plan Funds 2Document7 paginiNursing Care Plan Funds 2Yash RamawatÎncă nu există evaluări
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- ECMO, Adults BJA 2011Document5 paginiECMO, Adults BJA 2011RAGHAVENDRA VAGYANNAVARÎncă nu există evaluări
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1091)
- PARASITOLOGYDocument12 paginiPARASITOLOGYBr1nfoÎncă nu există evaluări
- Case Study 1Document10 paginiCase Study 1api-242123281Încă nu există evaluări
- Adult Blood Transfusion: Answers To Some Common QuestionsDocument4 paginiAdult Blood Transfusion: Answers To Some Common QuestionsEdward NodzoÎncă nu există evaluări
- Full Report Holter Lorena M 1-23-13Document36 paginiFull Report Holter Lorena M 1-23-13traja_vlrÎncă nu există evaluări
- A Profile of The Vaccination Awareness Movement in AustraliaDocument44 paginiA Profile of The Vaccination Awareness Movement in AustraliaMeryl DoreyÎncă nu există evaluări
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Exploratory Laparotomy Part 1Document3 paginiExploratory Laparotomy Part 1vishwanathÎncă nu există evaluări
- Head To Toe Exam: ChestDocument2 paginiHead To Toe Exam: Chestnicolas lastreÎncă nu există evaluări
- Brazil Maritime Authority Standards For The Pilotage Servives 2011Document83 paginiBrazil Maritime Authority Standards For The Pilotage Servives 2011borman2008Încă nu există evaluări
- EpistaxisDocument9 paginiEpistaxisapi-285171922Încă nu există evaluări
- Jjad038.pdftoken AQECAHi208BE49Ooan9kkhW Ercy7Dm3ZL 9Cf3qfKAc485ysgAAAugwggLkBgkqhkiG9w0BBwag PDFDocument51 paginiJjad038.pdftoken AQECAHi208BE49Ooan9kkhW Ercy7Dm3ZL 9Cf3qfKAc485ysgAAAugwggLkBgkqhkiG9w0BBwag PDF160835Încă nu există evaluări
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Typical and Atypical Motor DevelopmentDocument2 paginiTypical and Atypical Motor DevelopmentVirnabe PeliasÎncă nu există evaluări
- Trauma in The Aging PopulationDocument21 paginiTrauma in The Aging PopulationBruce Fredy Chino ChambillaÎncă nu există evaluări
- CH 25 Mycoplasma and UreaplasmaDocument14 paginiCH 25 Mycoplasma and UreaplasmashericeÎncă nu există evaluări
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)