Documente Academic
Documente Profesional
Documente Cultură
Propofol Vs Midazolam For ICU Sedation
Încărcat de
Liszt AlcantaraDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Propofol Vs Midazolam For ICU Sedation
Încărcat de
Liszt AlcantaraDrepturi de autor:
Formate disponibile
clinical investigations in critical care
Propofol vs Midazolam for ICU Sedation*
A Canadian Multicenter Randomized Trial
Richard I. Hall, MD, FCCP; Dean Sandham, MD, FCCP; Pierre Cardinal, MD;
Martin Tweeddale, MD; David Moher, MSc; Xiaohua Wang, MSc STAT; and
Aslam H. Anis, PhD; for the Study Investigators†
Study objectives: To determine whether sedation with propofol would lead to shorter times to
tracheal extubation and ICU length of stay than sedation with midazolam.
Design: Multicenter, randomized, open label.
Setting: Four academic tertiary-care ICUs in Canada.
Patients: Critically ill patients requiring continuous sedation while receiving mechanical ventilation.
Interventions: Random allocation by predicted requirement for mechanical ventilation (short
sedation stratum, < 24 h; medium sedation stratum, > 24 and < 72 h; and long sedation stratum,
> 72 h) to sedation regimens utilizing propofol or midazolam.
Measurements and results: Using an intention-to-treat analysis, patients randomized to receive
propofol in the short sedation stratum (propofol, 21 patients; midazolam, 26 patients) and the
long sedation stratum (propofol, 4 patients; midazolam, 10 patients) were extubated earlier (short
sedation stratum: propofol, 5.6 h; midazolam, 11.9 h; long sedation stratum: propofol, 8.4 h;
midazolam, 46.8 h; p < 0.05). Pooled results showed that patients treated with propofol (n ⴝ 46)
were extubated earlier than those treated with midazolam (n ⴝ 53) (6.7 vs 24.7 h, respectively;
p < 0.05) following discontinuation of the sedation but were not discharged from ICU earlier
(94.0 vs 63.7 h, respectively; p ⴝ 0.26). Propofol-treated patients spent a larger percentage of
time at the target Ramsay sedation level than midazolam-treated patients (60.2% vs 44.0%,
respectively; p < 0.05). Using a treatment-received analysis, propofol sedation either did not
differ from midazolam sedation in time to tracheal extubation or ICU discharge (sedation
duration, < 24 h) or was associated with earlier tracheal extubation but longer time to ICU
discharge (sedation duration, > 24 h, < 72 h, or > 72 h).
Conclusions: The use of propofol sedation allowed for more rapid tracheal extubation than when
midazolam sedation was employed. This did not result in earlier ICU discharge.
(CHEST 2001; 119:1151–1159)
Key words: ICU; mechanical ventilation; midazolam; multicenter; propofol; randomized clinical trial; sedation;
Abbreviations: APACHE ⫽ acute physiology and chronic health evaluation; CI ⫽ confidence interval
*From the Queen Elizabeth II Health Sciences Centre (Dr. This research was supported by Zeneca Pharma Inc. Canada.
Hall), Halifax, Nova Scotia, Canada; Foothills Hospital (Dr. Dr. Hall has received consultation fees from Zeneca Pharma Inc.
Sandham), University of Calgary, Calgary, Alberta, Canada; and Hoffman-LaRoche Limited. He has no equity interest in
Ottawa General Hospital (Dr. Cardinal), Ottawa, Ontario, Can- either company. Drs. Sandham, Cardinal, Tweeddale, and Anis,
ada; Vancouver General Hospital (Dr. Tweeddale), Vancouver, and Mr. Moher and Mrs. Wang have no financial relationship
British Columbia, Canada; Ottawa Civic Hospital (Mr. Moher), with either company.
Ottawa, Ontario, Canada; St. Paul’s Hospital (Mrs. Wang), Manuscript received March 11, 1999; revision accepted Septem-
Vancouver, British Columbia, Canada; and the Department of ber 7, 2000.
Health Care and Epidemiology (Dr. Anis), University of British Correspondence to: Richard I. Hall, MD, FCCP, Department of
Columbia, Vancouver, British Columbia, Canada. Anesthesia, Queen Elizabeth II Health Sciences Centre, 1796
†A list of additional study investigators is located in Appendix 1. Summer St, Halifax, Nova Scotia, Canada B3H 3A7; e-mail:
Presented in part to the American College of Chest Physicians rihall@is.dal.ca
Annual Meeting, New Orleans, LA, October 26 –30, 1997.
CHEST / 119 / 4 / APRIL, 2001 1151
P noxious
atients in an ICU are exposed to a variety of
stimuli including pain after surgery, fre-
protocol and consent process. Physicians made an assessment as
to whether patients would require sedation for short-term (ⱕ 24
h), medium-term (⬎ 24 and ⬍ 72 h), or long-term (ⱖ 72 h)
quent venipuncture, and discomfort from the pres- mechanical ventilation on admission to the ICU. Patients then
ence of an endotracheal tube.1,2 Sedation is fre- were stratified by predicted sedation time while receiving me-
quently required as a component of compassionate chanical ventilation, were randomized, and were entered into the
care in these patients. While a variety of agents have trial.
been employed for the provision of sedation, two
currently popular ones are midazolam and propo- Eligibility Criteria
fol.3–5 Both are rapid-acting drugs and do not sup- Inclusion Criteria: Patients were of either gender, ⱖ 18 years
press adrenal function when administered to the of age, and required immediate sedation so as to permit the
critically ill patient.6,7 Randomized studies, largely initiation and tolerance of mechanical ventilation.
from European centers, comparing propofol to mi- Exclusion Criteria: Exclusion criteria included a known or
dazolam for the sedation of ICU patients suggest that suspected allergy or intolerance to propofol or midazolam,
suspected pregnancy, coma due to a cerebrovascular accident or
propofol is as good as midazolam for this purpose unknown etiology, cranial trauma or neurosurgical intervention,
and that its pharmacokinetic profile may permit or status epilepticus. In situations in which patients could not give
more rapid dissipation of effects, thus allowing rapid consent, surrogate consent was obtained from next-of-kin at the
weaning from mechanical ventilation and tracheal earliest possible time following ICU admission.
extubation.8 –17 Data regarding the safety and effi-
cacy of propofol when used for prolonged sedation Randomization and Stratification
(ie, ⬎ 72 h) are limited,8,11,12,15,16,18,19 and it is not
Patients were individually assigned to treatment group by a
currently recommended for long-term sedation due random allocation process using a computer-generated (Zeneca
to lack of such information.20 Pharma Inc; Mississauga, Ontario, Canada) random block design.
This multicenter study conducted in four Cana- Groups of four opaque, sealed, sequentially numbered envelopes
dian ICUs sought to examine whether, given that with the group allocation coded for each center were provided for
midazolam is a longer-acting4 agent than propofol, each of the three strata based on predicted sedation time while
the patient was receiving mechanical ventilation as follows: short
this difference in pharmacokinetic properties would term (expected duration, ⬍ 24 h); medium term (ⱖ 24 h but
lead to significant differences in time to tracheal ⬍ 72 h); and long term (ⱖ 72 h).
extubation and ICU discharge. Because the benefits
of a shorter-acting sedative might be offset by the Infusion Regimens
duration of infusion21 (ie, patients requiring pro-
longed infusions during mechanical ventilation re- Once randomized, patients allocated to the propofol group
received an infusion of 0.3 to 0.6 mg/kg/h initially, which was
ceive more sedation and have prolonged recovery subsequently titrated to achieve a target Ramsay sedation score22
times), a secondary question was in which segment (see Appendix 2) that was specified for each patient at least daily
of the ICU population (ie, those requiring sedation and was adjusted based on the patient’s response to therapy.
for short-term, medium-term, or long-term mechan- When necessary to achieve a very rapid induction of sedation (eg,
ical ventilation) did this benefit apply? Our null to treat acute agitation), the infusion rate could be increased so as
to provide a bolus dose prior to adjustment of the standard
hypothesis was that there would be no difference in infusion regimen.
time to tracheal extubation or ICU length of stay Patients randomized to the midazolam group received an
when propofol was compared to midazolam as the infusion of 0.012 to 0.024 mg/kg/h adjusted to achieve the target
primary sedative agent in patients requiring mechan- Ramsay sedation score. As for the propofol group, in situations in
ical ventilation. which the rapid control of sedation was desired, an infusion bolus
could be administered.
No restrictions were placed on the type or amount of analgesia
required to achieve patient comfort.
Materials and Methods
Masking
Trial Design
We elected not to mask the treatment groups. The physical
This study was a multicenter, randomized, open-label trial appearance of propofol (formulated in a white lipid emulsion) is
conducted in four ICUs in academic medical centers across different from midazolam (clear liquid), and any leakage of
Canada. These centers were characterized as follows: center 1, a solution would unmask the study. We also reasoned that there are
surgical and trauma ICU; center 2, a mixed population of sufficient differences in the onset of drug effect that knowledge-
medical-surgical patients and the regional trauma unit; center 3, able caregivers would likely recognize treatments on this basis
a mixed medical-surgical unit that also admitted postoperative alone. Furthermore, when necessary to administer bolus infu-
cardiac surgical cases; and center 4, a mixed medical-surgical unit sions for acute agitation, knowledge of the treatment groups
that was a referral center for patients with difficult, long-term would prevent potentially hazardous hemodynamic changes
mechanical ventilation problems. All centers had 24-h coverage through appropriate care with drug infusion rates. The practical-
by staff intensivists and in-house coverage by resident house staff. ity of masking infusions by wrapping bags and tubing, for
The research review board of each institution approved the example, at all hours of the day or night was limited. Indeed,
1152 Clinical Investigations in Critical Care
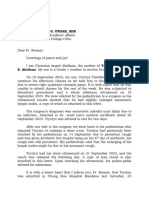
Figure 1. Trial flow diagram.
when sedation was required to rapidly achieve patient control of, in intubated patients.24,25 Patients were judged to be awake when
eg, postoperative emergence delirium, the time factor required to the Glasgow coma score was ⱖ 12.
prepare and mask solutions was thought to be such as to be
detrimental to patient care. The purpose of our study was to Measurements
inquire whether real-world use of the agents in a diverse group of
Canadian ICUs would lead to measurable differences in out- The Ramsay score (target and actual) was recorded hourly for
comes.23 the first 72 h or up to the time of discharge from ICU if this
Once patients were entered into the study, all investigators occurred prior to 72 h. After 72 h, it was recorded as the patient’s
agreed in advance that patient crossover between sedative regi- condition or infusion rate was altered. Time to tracheal extuba-
mens was prohibited unless a clear treatment failure could be tion, time to ICU discharge, and requirements for reintubation
demonstrated (eg, increasing paradoxical excitement in response were recorded. A record of vital signs was maintained every 20
to benzodiazepine administration or hyperlipidemia in response min for 40 min, then every 6 h for 48 h following extubation or
to propofol administration). Patients who died or crossed over until ICU discharge, whichever came first. Admission therapeutic
were eliminated from the study, and the data were censured. intervention scoring system score26 and APACHE II score27 were
recorded.
Measurement Scales Decisions as to when a patient was ready for a trial of
extubation or for discharge from the ICU were left to the
The Ramsay sedation score22 was utilized to quantitate the attending intensivists.
desired degree of sedation specified at regular intervals and Primary Outcome Measures: The time from withdrawal of
adjusted as the patient’s condition (ie, recovery or deterioration) sedation until tracheal extubation and ICU discharge for each
dictated. Patients receiving muscle relaxants and sedation were stratum was taken as the primary outcome measures. In situa-
given a Ramsay sedation score of 6. Recovery of consciousness tions in which patients required multiple independent periods of
was determined by measurement of the acute physiology and sedation or reintubation due to alterations in their disease
chronic health evaluation (APACHE) III modification of the process, the first period of sedation accompanied by tracheal
Glasgow coma score to allow for scoring of the verbal component extubation was utilized for data collection surrounding this event.
CHEST / 119 / 4 / APRIL, 2001 1153
Data were collected for the duration of the patient’s ICU stay. leading to death developed in one patient receiving
ICU length of stay was recorded as the time from admission to propofol, and propofol administration was thought to
ICU until the patient was discharged to the floor.
Secondary Outcome Measures: The time when the patient was
have possibly contributed to that death by the safety
deemed ready for extubation (as assessed by attending physicians review board. Hypertriglyceridemia developed in
clinically and by use of weaning parameters in most cases) was one propofol-treated patient who subsequently died.
recorded as well as the interval between when the patient was Lack of response to sedation occurred in four mida-
deemed ready for discharge and when discharge actually oc- zolam-treated patients (one of whom died) and in
curred.
seven propofol-treated patients (four of whom died)
(p ⫽ 0.30). Lack of response to sedation was attrib-
Safety Review Board uted to paradoxical excitement and agitation in three
All reports of deaths and serious adverse events, as identified midazolam-treated patients and in one propofol-
by site investigators, were examined by a blinded safety review treated patient. Unacceptable hypotension devel-
board that determined whether the event was attributable to oped in two propofol-treated patients.
study drug treatment or not. Diagnostic categories for the remaining 124 pa-
tients who survived and were discharged from the
Sample Size Calculation ICU are presented in Table 1. Demographic infor-
Statistical power was estimated using reduction in recovery
mation is provided in Table 2. There were more
time as the primary outcome. The recovery time for patients women in the midazolam group with a tendency to a
assigned to midazolam treatment was taken from the data of lower weight distribution. There were no differences
Carrasco et al.11 In that study, the mean (⫾ SD) recovery time for
midazolam was 3.6 ⫾ 0.8 h in the short-term sedation group (ie,
⬍ 24 h) 21.0 ⫾ 5.8 h in the medium-term sedation group (ie, ⬍ 7
days), and 54.7 ⫾ 12.3 h in the long-term sedation group (ie, ⬎ 7 Table 1—Distribution of Study Population by Center,
days). We assumed an interest in detecting a 20% relative Group, and Diagnosis*
reduction in recovery time using propofol ( ⫽ 0.1; ␣ ⫽ 0.05;
2-sided). The statistical power was calculated for each stratum Center 1 Center 2 Center 3 Center 4
separately (short term [⬍ 24 h], 22 per group to detect a Diagnosis Mid Prop Mid Prop Mid Prop Mid Prop
difference of 0.95 h; medium term [⬎ 24 and ⬍ 72 h], 31 patients
per group to detect a difference of 4.95 h; and long term [⬎ 72 Surgical
h], 22 patients per group to detect a difference of 12.97 h). Elective 2 4 1 2 5 1 1 0
postoperative
Vascular 1 3 3 3 2 1 0 1
Statistical Analysis surgery
Cardiac 0 0 0 0 13 14 0 0
The primary analysis was by intention-to-treat and was based
surgery
on differences in time to tracheal extubation and time to ICU
Trauma 1 2 4 1 0 0 1 0
discharge from the withdrawal of sedation using data from
Liver 0 1 0 0 0 0 0 0
patients as assigned to the original stratum. Probability values
transplant
ⱕ 0.05 were considered to be statistically significant. Ninety-five
Intra-abdominal 4 1 3 4 0 3 1 0
percent confidence intervals (CIs) were constructed for all data.
sepsis
A two-way analysis of variance was used to assess differences in
Necrotizing 0 0 0 1 0 1 1 0
tracheal extubation time by treatment group and sedation stra-
fasciitis
tum. A similar analysis was used to compare differences in the
Mediastinitis 1 0 0 0 0 0 0 0
time of ICU length of stay. The incidence of adverse events and
Burn 0 0 0 0 0 1 1 0
mortality was compared using a contingency table analysis.
Aspiration 2 2 1 0 0 0 0 1
A second analysis was performed post hoc to determine
pneumonia
differences between groups based on the time from sedation
Medical
reduction to tracheal extubation and ICU discharge using the
Pulmonary 0 0 1 1 0 0 0 0
data for patients as actually sedated (ie, those patients sedated for
edema
ⱕ 24 h, 24 to 72 h, or ⱖ 72 h regardless of initial randomization
(CHF)
assignment).
COPD 0 0 2 2 0 0 0 0
Acute MI 0 0 2 0 1 0 0 0
Pneumonia 0 1 4 4 1 1 0 0
Results Guillain-Barré 0 0 0 0 0 1 1 0
Pancreatitis 2 0 0 0 1 0 0 0
The trial flow diagram28 is presented in Figure 1. Hemorrhage 0 1 1 0 0 1 0 0
(GI bleed)
Initial treatment assignment and stratification were
Diagnosis 0 0 0 0 1 0 0 0
equally distributed among centers (data not shown). unknown
The trial was terminated prematurely for fiscal reasons. Total 13 15 22 18 24 24 6 2
There were 11 deaths in the midazolam group *Excluding patients who died or were sedation failures.
(13.9%) and 15 deaths (19.5%) in the propofol group CHF ⫽ congestive heart failure; MI ⫽ myocardial infarction;
(p ⫽ 0.37). Hypotension and ventricular tachycardia Mid ⫽ midazolam; Prop ⫽ propofol.
1154 Clinical Investigations in Critical Care
Table 2—Demographic Information*
Midazolam Propofol
Variables (n ⫽ 65) (n ⫽ 59) p Value
Age, yr 59.8 (55.3–64.4) 60.3 (55.2–66.0) 0.82
Weight, kg 72.1 (68.2–75.9) 78.0 (73.2–82.8) 0.06
Gender, No.
M 34 40 0.05
F 29 16
TISS score† 40 (35.7–45.0) 43 (37.7–48.4) 0.45
APACHE II score† 22 (20.4–24.0) 21 (18.6–22.6) 0.23
SBP,† mm Hg 124 (116.3–131.4) 126 (119.3–133.6) 0.62
DBP,† mm Hg 67 (62.4–71.2) 68 (62.8–73.0) 0.74
Heart rate,† beats/min 98 (92.1–104.6) 92 (86.4–98.2) 0.16
Respiratory rate,† beats/min 15 (13.1–16.3) 16 (13.2–18.0) 0.50
Pao2,† mm Hg 134 (113.0–155.2) 115 (100.4–130.4) 0.15
Paco2, mm Hg 42 (36.0–47.7) 39 (35.6–42.1) 0.36
Repeated tracheal intubation, No. 6 12 0.07
Median length of stay, h 72.7 69.8 0.94
*Excluding data from patients who died or did not respond to sedation. Values given as mean (95% CI), unless otherwise indicated.
TISS ⫽ therapeutic intervention scoring system; SBP ⫽ systolic BP; DBP ⫽ diastolic BP.
†At admission.
between groups for baseline hemodynamic parame- ated with earlier tracheal extubation and longer
ters of BP, heart rate, respiratory rate, or arterial times to ICU discharge. Propofol-treated patients
blood gas levels. had lower diastolic BP, heart rate, and respiratory
Center analysis showed that the average length of rate than did midazolam-treated patients at the time
stay was shorter for center 3 but that there was no of tracheal extubation (data not shown). Respiratory
difference in length of stay between treatment rate continued to be lower over the next 12 h.
groups within each center. Therefore, data were Otherwise, no differences were detected.
pooled (Table 3). Individual data are given for duration of sedation
Tracheal extubation occurred while continuous vs time from end of sedation to tracheal extubation
sedation was ongoing in 25 patients (midazolam, 12 (Fig 2, top) and vs time from end of sedation to ICU
patients; propofol, 13 patients), preventing the ascer- discharge (Fig 2, bottom). Of the four patients whose
tainment of extubation time. Data for the primary time from end of sedation to tracheal extubation
outcome variables for the remaining 99 patients by exceeded 80 h (Fig 2, top), all were treated with
stratum, as determined using an intention-to-treat midazolam. One of these patients required repeated
analysis, are listed in Table 4. Significant differences tracheal intubation. Of the patients who had a time
between groups for the short-term and long-term from end of sedation to ICU discharge of ⬎ 300 h
strata for time to extubation, but not for time to ICU (Fig 2, bottom), three were sedated with propofol
discharge, were noted. When the data were pooled,
the mean time from reduction of sedation to tracheal
extubation was shorter for propofol-treated patients
than for midazolam-treated patients (midazolam, Table 3—Overall Length of Stay by Stratum*
24.7 h [95% CI, 14.5 to 35.0]; propofol, 6.7 h [95% Sedation Strata Midazolam Propofol p Value
CI, 4.2 to 9.1]) but not the time to ICU discharge
ⱕ 24 h
(midazolam, 63.7 h [44.3 to 83.0]; propofol, 94.0 h
Mean 59.56 70.82 0.606
[44.0 to 143.9]). Patients treated with propofol spent 95% CI 40.9–78.1 29.9–111.7
more time at the target mean Ramsay sedation score Median 46.25 46.67 0.940
level (propofol, 60.2% [range, 52.6 to 67.9]; midazo- 24–72 h
lam, 44.0% [range, 35.0 to 52.9]; p ⬍ 0.05). Mean 151.45 158.26 0.897
95% CI 83.5–219.4 72.6–243.9
Data for the post hoc secondary analysis using
Median 94.67 117.17 0.800
treatment received stratification are given in Table 5. ⱖ 72 h
Using this analysis, no differences in either extuba- Mean 219.28 202.94 0.727
tion time or time to ICU discharge were detected 95% CI 159.8–278.7 89.4–316.5
between groups for the short sedation stratum. In Median 207.50 207.33 0.990
the other two strata, the use of propofol was associ- *Excluding data from patients who died or were sedation failures.
CHEST / 119 / 4 / APRIL, 2001 1155
Table 4 —Time From Sedation Reduction to Tracheal Extubation and ICU Discharge by Strata*
Sedation
Stratum End Point Midazolam Propofol p Value
ⱕ 24 h Extubation (n ⫽ 26) (n ⫽ 21)
ICUdischarge 11.9 (7.0–16.8) 5.6 (2.6–8.6) 0.029
32.7 (23.7–41.7) 49.5 (10.2–88.9) 0.394
24–72 h Extubation (n ⫽ 17) (n ⫽ 21)
ICUdischarge 31.3 (5.7–57.0) 7.4 (3.1–11.7) 0.068
72.6 (41.5–103.7) 147.2 (44.9–249.5) 0.158
ⱖ 72 h Extubation (n ⫽ 10) (n ⫽ 4)
ICUdischarge 46.8 (14.4–79.3) 8.4 (0–25.0) 0.03
129.0 (47.5–210.5) 47.6 (0–108.1) 0.20
*Positive values only were used with an intention-to-treat analysis. Values given as mean (95% CI), unless otherwise indicated.
and one with midazolam. All of these patients re- have required more ongoing care in the ICU than
quired repeated tracheal intubation. patients treated with midazolam. Propofol-treated
patients had lower respiratory rates following extu-
bation. Perhaps the ongoing release of propofol from
Discussion fat stores4 contributed to residual sedation leading to
an impairment of cough, atelectasis, and pulmonary
In this multicenter randomized trial, the use of
propofol compared to midazolam for sedation of dysfunction, thus necessitating retention of patients
patients in the ICU was associated with a reduced in the ICU for longer periods of time. Both propo-
time to tracheal extubation in evaluable patients, but fol29,30 and midazolam31 have been demonstrated to
there was either no difference or a prolonged time to reduce neutrophil function in vitro. The degree to
ICU discharge. which this may have contributed to the results is
We can only speculate as to why ICU discharge unknown. Although not statistically significant, there
was delayed. It could perhaps be explained by were more deaths among the propofol-treated pa-
problems in the systematic handling of patients tients, and they required reintubation more fre-
within these institutions. For example, any pharma- quently than midazolam-treated patients. Unfortu-
cokinetic advantage to earlier tracheal extubation nately, we did not capture the reason for
associated with propofol use will be lost if there are reintubation in our data set.
routine difficulties associated with discharging pa- Our trial confirms the findings of the majority of
tients from the ICU due to, for example, lack of floor previous randomized studies, which have demon-
beds available to receive these patients. Alterna- strated more rapid times to awakening9,11–14,16,17 and
tively, propofol-treated patients, although they were reduced times to tracheal extubation11,15 with the
extubated earlier (and perhaps prematurely), may use of propofol for ICU sedation. However, Higgins
Table 5—Time From Sedation Reduction to Tracheal Extubation and ICU Discharge by Stratum as
Determined by Post Hoc Analysis*
Sedation
Stratum End Point Midazolam Propofol p Value
ⱕ 24 h Extubation (n ⫽ 30) (n ⫽ 28)
ICUdischarge 9.1 (5.5–12.7) 6.3 (3.4–9.2) 0.17
33.7 (24.3–43.0) 43.4 (30.9–55.9) 0.22
24–72 h Extubation (n ⫽ 8) (n ⫽ 7)
ICUdischarge 31.0 (6.3–55.7) 9.9 (1.3–18.5) 0.014
76.7 (29.7–123.7) 156.5 (0–335.8) 0.008
ⱖ 72 h Extubation (n ⫽ 15) (n ⫽ 11)
ICUdischarge 52.7 (25.6–79.8) 5.3 (1.4–9.2) 0
121.7 (63.1–180.3) 154.7 (0–316.6) 0.004
*Positive values only were used. Values given as mean (95% CI).
1156 Clinical Investigations in Critical Care
conducted in a trauma population, showed an in-
creased ICU length of stay for propofol-treated
patients (propofol-treated patients, 24 days; midazo-
lam-treated patients, 18 days).16 A study conducted
by Weinbroum et al17 in Israel, while able to show a
difference in time to awakening, did not measure a
significant difference in ICU discharge time (mida-
zolam-treated patients, 31 days; propofol-treated pa-
tients, 21 days) when patients were sedated for ⬎ 24
h. ICU costs were five times higher in propofol-
treated patients in that study. It would appear,
therefore, that to capitalize on the more rapid awak-
ening and tracheal extubation produced by the use of
propofol sedation, the ability to rapidly discharge the
patient once tracheal extubation occurs is essential.
In situations in which this is not possible (ie, those in
which the patient’s disease process will require
further ICU stay after extubation [eg, trauma pa-
tients]) or those in which there are systematic diffi-
culties in arranging the timely transfer of patients
once they are extubated out of the ICU (as exists in
the Canadian health-care system as a consequence of
bed closures), the use of propofol may not be
cost-effective.
The Society of Critical Care Medicine has pub-
lished guidelines for sedation in the ICU.20 They
recommend propofol or midazolam for sedation
intervals of ⬍ 24 h and lorazepam for sedation
intervals of ⬎ 24 h. In part, their recommendations
are predicated on a lack of information concerning
the safety of propofol for long-term sedation. A
Figure 2. Top: time from the end of sedation to tracheal
extubation vs duration of sedation. Note the increased variability recent meta-analysis32 suggested a need for more
for patients who received midazolam for sedation. Each point randomized trials of ICU sedation. Our study adds to
represents results for an individual patient. Bottom: time from a growing body of knowledge concerning the safety
the end of sedation to ICU discharge vs duration of sedation.
Each point represents results for an individual patient. No of propofol for ICU sedation in adults.8,11,12,15,16,18,19
differences between groups were identified. In the current study, hypertriglyceridemia developed
in one patient receiving propofol who subsequently
died, and significant hypotension developed in three
others (one of whom died), prompting a change in
et al10 did not find a difference in time to tracheal the sedation regimen. Our results suggest that, while
extubation when comparing propofol to midazolam propofol may be a satisfactory agent for ICU seda-
for sedation in a cardiac surgical patient population. tion, attention should be given to the monitoring of
Comparative studies reporting the role of propofol hemodynamics and serum triglyceride levels on a
sedation to accelerate ICU discharge have produced regular basis as a proportion of patients will develop
mixed results. Our findings were that the use of hemodynamic and metabolic complications.
propofol for sedation did not shorten ICU length of Prolonged tracheal intubation may be associated
stay. In contrast, Carrasco et al11 demonstrated that with adverse clinical events, including development
the use of propofol was associated with earlier ICU of nosocomial pneumonia33 and barotrauma.34 Intu-
discharge and, consequently, with cost savings in itively, drugs that reduce the time that a patient
patients having ICU stays of ⬍ 1 day. Barrientos- receives mechanical ventilation should lead to reduc-
Vega and colleagues15 also were able to show cost tions in such adverse events. In this study, no
savings due to earlier ICU discharge in patients differences in adverse events were detected between
sedated with propofol for approximately 150 h. Both the two drug regimens, but the study was not
studies were conducted in Spain and may reflect designed to detect measurable differences.
differences in ICU practice and patient mix in that The strengths of our study include its randomized
country vs Canada. However, another Spanish trial, nature, size, multicenter design, and differences in
CHEST / 119 / 4 / APRIL, 2001 1157
case mix. A weakness is the lack of masking, but, for cology and a review of its clinical efficacy in intensive care
reasons already expounded, we did not think that we sedation. Drugs 1995; 50:636 – 657
5 Mirenda J, Broyles G. Propofol as used for sedation in the
could mask the study treatments in any practical
ICU. Chest 1995; 108:539 –548
fashion. By chance alone, more women were ran- 6 Shapiro JM, Westphal LM, White PF, et al. Midazolam
domized to the midazolam treatment group. Un- infusion for sedation in the intensive care unit: effect on
known gender differences in pharmacokinetics may adrenal function. Anesthesiology 1986; 64:394 –398
have played a role in the results. For budgetary 7 Newman LH, McDonald JC, Wallace PG, et al. Propofol
reasons, we did not complete the recruitment of infusion for sedation in intensive care. Anesthesia 1987;
42:929 –937
sufficient numbers of patients in the medium-term 8 Harris CE, Grounds RM, Murray AM, et al. Propofol for
sedation stratum (24 patients) and the long-term long-term sedation in the intensive care unit: a comparison
sedation stratum (40 patients), which may have with papaveretum and midazolam. Anesthesia 1990; 45:366 –
affected our ability to detect differences within the 372
medium-term sedation stratum and suggests that 9 Boyd O, Mackay CJ, Rushmer F, et al. Propofol or midazolam
for short-term alterations in sedation. Can J Anaesth 1993;
caution should be exercised in the interpretation of 40:1142–1147
the data from the long-term stratum. 10 Higgins TL, Yared JP, Estafanous FG, et al. Propofol versus
midazolam for intensive care unit sedation after coronary
artery bypass grafting. Crit Care Med 1994; 22:1415–1423
11 Carrasco G, Molina R, Costa J, et al. Propofol vs midazolam
Conclusion in short-, medium-, and long-term sedation of critically ill
patients: a cost-benefit analysis. Chest 1993; 103:557–564
Propofol was a satisfactory agent for ICU sedation 12 Chamorro C, de Latorre FJ, Montero A, et al. Comparative
study of propofol versus midazolam in the sedation of criti-
in this randomized multicenter trial. It permitted cally ill patients: results of a prospective, randomized, multi-
earlier tracheal extubation compared to midazolam center trial. Crit Care Med 1996; 24:932–939
but did not permit earlier ICU discharge. 13 Ronan KP, Gallagher TJ, George B, et al. Comparison of
propofol and midazolam for sedation in intensive care unit
patients. Crit Care Med 1995; 23:286 –293
14 Kress JP, O’Connor MF, Pohlman AS, et al. Sedation of
Appendix 1: Additional Study Investigators critically ill patients during mechanical ventilation: a compar-
ison of propofol and midazolam. Am J Respir Crit Care Med
David Stewart, MSc, Study Monitor, Ottawa Civic Hospital,
1996; 153:1012–1018
Ottawa, Ontario, Canada; Hugh Devitt, MD, Safety Review
15 Barrientos-Vega R, Mar S, Morales-Garcia C, et al. Prolonged
Committee, Sunnybrook Health Sciences Centre, Toronto, On-
sedation of critically ill patients with midazolam or propofol:
tario, Canada; Craig Guenther, MD, Safety Review Committee,
impact on weaning and costs. Crit Care Med 1997; 25:33– 40
University of Alberta Hospitals, Edmonton, Alberta, Canada;
16 Sanchez-Izquierdo-Riera JA, Caballero-Cubedo RE, Perez-
Mauricio Calero, MD, Commercial Products Manager, Zeneca
Vela JL, et al. Propofol versus midazolam: safety and efficacy
Pharma Inc., Mississauga, Ontario, Canada; and Hector Leon,
for sedating the severe trauma patient. Anesth Analg 1998;
BSc STAT, Data Entry and Statistical Analysis, St. Paul’s Hospi-
86:1219 –1224
tal, Vancouver, British Columbia, Canada.
17 Weinbroum AA, Halpern P, Rudick V, et al. Midazolam
versus propofol for long-term sedation in the ICU: a random-
ized prospective comparison. Intensive Care Med 1997;
Appendix 2: Ramsay Sedation Scale 23:1258 –1263
18 Beller JP, Pottecher T, Lugnier A, et al. Prolonged sedation
1. Anxious and agitated, or restless, or both22 with propofol in ICU patients: recovery and blood concen-
2. Cooperative, oriented, and tranquil tration changes during periodic interruptions in infusion. Br J
3. Responding to commands only Anaesth 1988; 61:583–588
19 Valente JF, Anderson GL, Branson RD, et al. Disadvantages
4. Brisk response to glabellar tap of prolonged propofol sedation in the critical care unit. Crit
5. Sluggish response to glabellar tap Care Med 1994; 22:710 –712
6. No response to light glabellar tap 20 Shapiro BA, Warren J, Egol AB, et al. Practice parameters for
intravenous analgesia and sedation for adult patients in the
intensive care unit: an executive summary; Society of Critical
Care Medicine. Crit Care Med 1995; 23:1596 –1600
21 Hughes MA, Glass PS, Jacobs JR. Context-sensitive half-time
References in multicompartment pharmacokinetic models for intrave-
1 Aitkenhead AR. Analgesia and sedation in intensive care. Br J nous anesthetic drugs. Anesthesiology 1992; 76:334 –341
Anaesth 1989; 63:196 –206 22 Ramsay MA, Savege TM, Simpson BR, et al. Controlled seda-
2 Park GR, Gempeler F. The need for sedation and analgesia. tion with alphaxalone-alphadolone. BMJ 1974; 2:656 – 659
In: Park GR, Gempeler F, eds. Sedation and analgesia. 23 Freemantle N, Drummond M. Should clinical trials with
Philadelphia, PA: WB Saunders, 1993; 1–19 concurrent economic analyses be blinded? JAMA 1997; 277:
3 Amrein R, Hetzel W. Pharmacology of drugs frequently used 63– 64
in ICUs: midazolam and flumazenil. Intensive Care Med 24 Knaus WA, Wagner DP, Draper EA, et al. The APACHE III
1991; 17(suppl):S1–S10 prognostic system: risk prediction of hospital mortality for
4 Fulton B, Sorkin EM. Propofol: an overview of its pharma- critically ill hospitalized adults. Chest 1991; 100:1619 –1636
1158 Clinical Investigations in Critical Care
25 Teasdale G, Jennett B. Assessment of coma and impaired migration of human leukocytes through endothelial cell
consciousness: a practical scale. Lancet 1974; 2:81– 84 monolayers. Crit Care Med 1999; 27:1843–1847
26 Keene AR, Cullen DJ. Therapeutic intervention scoring 31 Nishina K, Akamatsu H, Mikawa K, et al. The inhibitory
system: update 1983. Crit Care Med 1983; 11:1–3 effects of thiopental, midazolam, and ketamine on human
27 Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a neutrophil functions. Anesth Analg 1998; 86:159 –165
severity of disease classification system. Crit Care Med 1985; 32 Ostermann ME, Keenan SP, Seiferling RA, et al. Sedation in
13:818 – 829 the intensive care unit: a systematic review. JAMA 2000;
28 Begg C, Cho M, Eastwood S, et al. Improving the quality of 283:1451–1459
reporting of randomized controlled trials: the CONSORT 33 Brun-Buisson C. Risk Factors for nosocomial pneumonia. In:
statement. JAMA 1996; 276:637– 639 Vincent J-L, ed. Yearbook of intensive care medicine 1993.
29 Mikawa K, Akamatsu H, Nishina K, et al. Propofol inhibits New York, NY: Springer-Verlag, 1993; 273–280
human neutrophil functions. Anesth Analg 1998; 87:695–700 34 Parker JC, Hernandez LA, Peevy KJ. Mechanisms of venti-
30 Hofbauer R, Frass M, Salfinger H, et al. Propofol reduces the lator-induced lung injury. Crit Care Med 1993; 21:131–143
CHEST / 119 / 4 / APRIL, 2001 1159
S-ar putea să vă placă și
- Estudio SEDCOMDocument11 paginiEstudio SEDCOMElias Vera RojasÎncă nu există evaluări
- Garcia 2021Document9 paginiGarcia 2021Giancarlo Maruri MunarettoÎncă nu există evaluări
- Idade Acima de 16 Anos MCCREDIEDocument9 paginiIdade Acima de 16 Anos MCCREDIEDaniele PeixotoÎncă nu există evaluări
- Minimum Effective Dose of Midazolam For Sedation of Mechanically Ventilated NeonatesDocument7 paginiMinimum Effective Dose of Midazolam For Sedation of Mechanically Ventilated NeonatesAndrew JoshuaÎncă nu există evaluări
- Penggunaan Sedasi Pada Anak Dengan VentilatorDocument5 paginiPenggunaan Sedasi Pada Anak Dengan VentilatorCalvin AffendyÎncă nu există evaluări
- Daily Interruption of Sedation in Patients Receiving Mechanical VentilationDocument10 paginiDaily Interruption of Sedation in Patients Receiving Mechanical VentilationJim LinÎncă nu există evaluări
- Delayed Sequence Intubation - 2016Document8 paginiDelayed Sequence Intubation - 2016Ivan HarizanovÎncă nu există evaluări
- Enteral1 PDFDocument10 paginiEnteral1 PDFCarlos Eduardo FerrazÎncă nu există evaluări
- Original PapersDocument9 paginiOriginal PapersMárcia SanchesÎncă nu există evaluări
- Comparing Two Methods of Delivering High-Flow Gas Therapy by Nasal Cannula Following Endotracheal Extubation - A Prospective, Randomized, Masked, Crossover TrialDocument5 paginiComparing Two Methods of Delivering High-Flow Gas Therapy by Nasal Cannula Following Endotracheal Extubation - A Prospective, Randomized, Masked, Crossover TrialNathaniel Gilbert DysonÎncă nu există evaluări
- JAnaesthClinPharmacol371114-28986 000449Document5 paginiJAnaesthClinPharmacol371114-28986 000449Ferdy RahadiyanÎncă nu există evaluări
- Ropvacaina VS Lidocaina Premdicacion IotDocument6 paginiRopvacaina VS Lidocaina Premdicacion IotFaith Lu PenalozaÎncă nu există evaluări
- Transtracheal LidocaineDocument4 paginiTranstracheal LidocaineaksinuÎncă nu există evaluări
- ESTEBAN Et Al-2012-American Journal of Respiratory and Critical Care MedicineDocument7 paginiESTEBAN Et Al-2012-American Journal of Respiratory and Critical Care MedicineGustavoGarcíaÎncă nu există evaluări
- Sedation in The Intensive Care Unit A Systematic RDocument13 paginiSedation in The Intensive Care Unit A Systematic RFebri Yudha Adhi KurniawanÎncă nu există evaluări
- Daily Interruption of Sedation in Patients Receiving Mechanical VentilationDocument10 paginiDaily Interruption of Sedation in Patients Receiving Mechanical VentilationEryll Jean SamotÎncă nu există evaluări
- Management of Sedation and Delirium in Ventilated ICU PatientsDocument35 paginiManagement of Sedation and Delirium in Ventilated ICU PatientsJheng-Dao YangÎncă nu există evaluări
- JeradDocument10 paginiJeradzaimmuhtarÎncă nu există evaluări
- Haloperidol Combined With DexamethasoneDocument6 paginiHaloperidol Combined With Dexamethasoneapi-741687858Încă nu există evaluări
- Jurnal IcuDocument7 paginiJurnal IcuoktavienniÎncă nu există evaluări
- Jurnal Cma 3Document7 paginiJurnal Cma 3Ririn AptÎncă nu există evaluări
- 110schweickert2009 PDFDocument9 pagini110schweickert2009 PDFJulieta EvangelistaÎncă nu există evaluări
- Ferrer 2006Document7 paginiFerrer 2006Fermin LombardiaÎncă nu există evaluări
- Dsi Vs Rsi in TraumaDocument7 paginiDsi Vs Rsi in TraumaAbhi JeetÎncă nu există evaluări
- Anaesthesia - 2012 - Geldner - A Randomised Controlled Trial Comparing Sugammadex and Neostigmine at Different Depths ofDocument8 paginiAnaesthesia - 2012 - Geldner - A Randomised Controlled Trial Comparing Sugammadex and Neostigmine at Different Depths ofMario AbdiwijoyoÎncă nu există evaluări
- Nava 1998Document8 paginiNava 1998Fermin LombardiaÎncă nu există evaluări
- Early Physical and Occupational Therapy in Mechanically Ventilated, Critically Ill Patients A Randomised Controlled Trial - Barker2010Document2 paginiEarly Physical and Occupational Therapy in Mechanically Ventilated, Critically Ill Patients A Randomised Controlled Trial - Barker2010RodrigoSachiFreitasÎncă nu există evaluări
- Postoperative Nausea and Vomiting in OpioidFree Anesthesia Versus Opioid Based Anesthesia in Laparoscopic CholecystectomyDocument8 paginiPostoperative Nausea and Vomiting in OpioidFree Anesthesia Versus Opioid Based Anesthesia in Laparoscopic Cholecystectomypepe4dwinÎncă nu există evaluări
- JurnalDocument20 paginiJurnalAnonymous PFNzHoÎncă nu există evaluări
- Riker2009 Dexmedetomidine Vs Midazolam For Sedation of Critically Ill Patients, A Randomized TrialDocument11 paginiRiker2009 Dexmedetomidine Vs Midazolam For Sedation of Critically Ill Patients, A Randomized TrialjosefmagnoÎncă nu există evaluări
- Ozaki2014 Article SafetyAndEfficacyOfDexmedetomiDocument13 paginiOzaki2014 Article SafetyAndEfficacyOfDexmedetomiidaÎncă nu există evaluări
- 0300060513485864Document11 pagini0300060513485864Aashish KalikaÎncă nu există evaluări
- Thoracic Segmental Spinal Anaesthesia/ General Anaesthesia For Laproscopy SurgeryDocument8 paginiThoracic Segmental Spinal Anaesthesia/ General Anaesthesia For Laproscopy SurgeryIJAR JOURNALÎncă nu există evaluări
- Surgery 23 3 1Document6 paginiSurgery 23 3 1razaqhussain00Încă nu există evaluări
- MeduriDocument4 paginiMeduriSilvia Leticia BrunoÎncă nu există evaluări
- Articulo 9 JulioDocument10 paginiArticulo 9 JulioPaloma AroliÎncă nu există evaluări
- The Role of Dexmedetomidine (Precedex) in The Sedation of Critically Ill PatientsDocument4 paginiThe Role of Dexmedetomidine (Precedex) in The Sedation of Critically Ill Patientspshz05Încă nu există evaluări
- A Prospective, Randomized, Double-Blind, Multicenter Study Comparing Remifentanil With Fentanyl in Mechanically Ventilated PatientsDocument8 paginiA Prospective, Randomized, Double-Blind, Multicenter Study Comparing Remifentanil With Fentanyl in Mechanically Ventilated PatientsJosé Carlos Sánchez-RamirezÎncă nu există evaluări
- A Prospective, Randomized, Double-Blind, Multicenter Study Comparing Remifentanil With Fentanyl in Mechanically Ventilated PatientsDocument8 paginiA Prospective, Randomized, Double-Blind, Multicenter Study Comparing Remifentanil With Fentanyl in Mechanically Ventilated PatientsJosé Carlos Sánchez-RamirezÎncă nu există evaluări
- Use of High-Flow Nasal Cannula Oxygen Therapy To Prevent Desaturation During Tracheal Intubation of Intensive Care Patients With Mild-to-Moderate HypoxemiaDocument10 paginiUse of High-Flow Nasal Cannula Oxygen Therapy To Prevent Desaturation During Tracheal Intubation of Intensive Care Patients With Mild-to-Moderate HypoxemiaLingga AniÎncă nu există evaluări
- Evid TT 2200305Document4 paginiEvid TT 2200305Muthia Farah AshmaÎncă nu există evaluări
- 10effect of Early Vs Late Tracheostomy Placement On Survival in Patients Receiving Mechanical Ventilation The TracMan Randomized Trial 2013Document9 pagini10effect of Early Vs Late Tracheostomy Placement On Survival in Patients Receiving Mechanical Ventilation The TracMan Randomized Trial 2013Cường Nguyễn HùngÎncă nu există evaluări
- Anesthesia Management in Respiratory DepressionDocument7 paginiAnesthesia Management in Respiratory DepressionGandita AnggoroÎncă nu există evaluări
- Dolor Postop, Ligamentos Cruzados, AmbulatorioDocument7 paginiDolor Postop, Ligamentos Cruzados, AmbulatorioChurrunchaÎncă nu există evaluări
- Regional Versus General Anesthesia in Patients Underwent Hip Fracture Surgery Over 80 Years Old: A Retrospective Cohort StudyDocument6 paginiRegional Versus General Anesthesia in Patients Underwent Hip Fracture Surgery Over 80 Years Old: A Retrospective Cohort Studyeko andryÎncă nu există evaluări
- Casey Et Al 2021 Protocolized Postextubation Respiratory Support To Prevent Reintubation A Randomized Clinical TrialDocument9 paginiCasey Et Al 2021 Protocolized Postextubation Respiratory Support To Prevent Reintubation A Randomized Clinical TrialOla ZahraÎncă nu există evaluări
- Surve Rohini 2016Document7 paginiSurve Rohini 2016Amro MahmoudÎncă nu există evaluări
- 12Hiệu quả mở kq sớm pt gộp 2015Document10 pagini12Hiệu quả mở kq sớm pt gộp 2015Cường Nguyễn HùngÎncă nu există evaluări
- Kacmarek2020 Article NeurallyAdjustedVentilatoryAssDocument11 paginiKacmarek2020 Article NeurallyAdjustedVentilatoryAssHoracio Panzardo GonzálezÎncă nu există evaluări
- Early Neuromuscular Blockade in The Acute Respiratory Distress SyndromeDocument12 paginiEarly Neuromuscular Blockade in The Acute Respiratory Distress SyndromeLiliam GonzalezÎncă nu există evaluări
- Research Article: Prone Position After Liberation From Prolonged Mechanical Ventilation in COVID-19 Respiratory FailureDocument7 paginiResearch Article: Prone Position After Liberation From Prolonged Mechanical Ventilation in COVID-19 Respiratory FailurewiwiÎncă nu există evaluări
- 2019 A&a Dez MetadonaDocument3 pagini2019 A&a Dez MetadonajaquelinemiyakeÎncă nu există evaluări
- A Comparison of Postoperative Respiratory Complications Associated With The Use of Desflurane and Sevoflurane: A Single-Centre Cohort StudyDocument9 paginiA Comparison of Postoperative Respiratory Complications Associated With The Use of Desflurane and Sevoflurane: A Single-Centre Cohort StudyPaloma LizardiÎncă nu există evaluări
- Obesity and Anticipated Difficult Airway - A Comprehensive Approach With Videolaryngoscopy, Ramp Position, Sevoflurane and Opioid Free AnaesthesiaDocument8 paginiObesity and Anticipated Difficult Airway - A Comprehensive Approach With Videolaryngoscopy, Ramp Position, Sevoflurane and Opioid Free AnaesthesiaIJAR JOURNALÎncă nu există evaluări
- Movilización y Recuperación Precoces en Pacientes Con Ventilación Mecánica en La UCI Un Estudio de Cohorte Prospectivo Binacional, MulticéntricoDocument10 paginiMovilización y Recuperación Precoces en Pacientes Con Ventilación Mecánica en La UCI Un Estudio de Cohorte Prospectivo Binacional, MulticéntricoByron VarasÎncă nu există evaluări
- Effect of Intraoperative Dexmedetomidine On Post-Craniotomy PainDocument9 paginiEffect of Intraoperative Dexmedetomidine On Post-Craniotomy PainIva SantikaÎncă nu există evaluări
- ArdsDocument16 paginiArdsCryptococcus NeoformansÎncă nu există evaluări
- Dexmedetomidine Vs Midazolam For Sedation of Critically Ill Patients A Randomized TrialDocument12 paginiDexmedetomidine Vs Midazolam For Sedation of Critically Ill Patients A Randomized TrialParvathy R NairÎncă nu există evaluări
- Nebulized Dexmedetomidine-Lidocaine Inhalation As A Premedication For Flexible Bronchoscopy: A Randomized TrialDocument8 paginiNebulized Dexmedetomidine-Lidocaine Inhalation As A Premedication For Flexible Bronchoscopy: A Randomized TrialRichard PhoÎncă nu există evaluări
- EVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYDe la EverandEVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYÎncă nu există evaluări
- CGHS HospitalsDocument9 paginiCGHS Hospitalsgarg_mahak3199Încă nu există evaluări
- Nelvin Cleofas ResumeDocument4 paginiNelvin Cleofas ResumeNelvz VeyronÎncă nu există evaluări
- 1971 WL 126685Document142 pagini1971 WL 126685Thalia SandersÎncă nu există evaluări
- Active and Passive Voice ExerciseDocument2 paginiActive and Passive Voice Exerciseela garcia100% (1)
- Acid Base QuestionDocument2 paginiAcid Base QuestionStuff and ThingsÎncă nu există evaluări
- Gruesome Playground InjuriesDocument28 paginiGruesome Playground InjuriesJordanakulak100% (27)
- FMRI Obs Icu & HduDocument13 paginiFMRI Obs Icu & HduApoorv JainÎncă nu există evaluări
- Ortho Endorsements UPDATED MAY 2023Document16 paginiOrtho Endorsements UPDATED MAY 2023GrInDoVe9097Încă nu există evaluări
- Mike Adams - The Healing Power of Sunlight Vitamin DDocument26 paginiMike Adams - The Healing Power of Sunlight Vitamin DJOSEPHÎncă nu există evaluări
- Excuse LetterDocument2 paginiExcuse Letterangeli abellanaÎncă nu există evaluări
- FY2009 State Grants AllDocument1.117 paginiFY2009 State Grants AllPrattvilleRevolutionÎncă nu există evaluări
- DR Form BsuDocument1 paginăDR Form BsumingcatÎncă nu există evaluări
- A Review of The Modern Mongolian Healthcare SystemDocument6 paginiA Review of The Modern Mongolian Healthcare SystemPatrickLnanduÎncă nu există evaluări
- Hal 1-50Document109 paginiHal 1-50Nur AisyahÎncă nu există evaluări
- Perception of Open Spaces Integration in Maternity Hospital Designs in Kaduna Kaduna State NigeriaDocument5 paginiPerception of Open Spaces Integration in Maternity Hospital Designs in Kaduna Kaduna State NigeriamikiyasÎncă nu există evaluări
- DR Goran Stanisavljevic - From Web Crystal Dental CentreDocument4 paginiDR Goran Stanisavljevic - From Web Crystal Dental Centremegica02Încă nu există evaluări
- MPHE Day 1.Document36 paginiMPHE Day 1.Sathish KumarÎncă nu există evaluări
- ProjDocument37 paginiProjM LubisÎncă nu există evaluări
- Marissa Hamby Resume Final DraftDocument2 paginiMarissa Hamby Resume Final Draftapi-353698203Încă nu există evaluări
- 2007 Bielen Demoulin Waiting Time Influence On The Satisfaction-Loyalty Relationship 2007Document21 pagini2007 Bielen Demoulin Waiting Time Influence On The Satisfaction-Loyalty Relationship 2007Thi HoàngÎncă nu există evaluări
- Soal Perioperative Eng VersionDocument22 paginiSoal Perioperative Eng VersionZulaikah Nur IstiqomahÎncă nu există evaluări
- Complications of Total Knee Arthroplasty: Standardized List and Definitions of The Knee SocietyDocument6 paginiComplications of Total Knee Arthroplasty: Standardized List and Definitions of The Knee SocietyotakmesumÎncă nu există evaluări
- Catheter ExamDocument2 paginiCatheter ExamAnjo CincoÎncă nu există evaluări
- Healthcare Transformation and Changing Roles For NursingDocument14 paginiHealthcare Transformation and Changing Roles For NursingCynthia MiclatÎncă nu există evaluări
- Open EMRDocument38 paginiOpen EMRSuhail BhatiaÎncă nu există evaluări
- From The Backyard To The Frontline: Initiatives of Philippine Hospital Workers On Best Environmental PracticesDocument60 paginiFrom The Backyard To The Frontline: Initiatives of Philippine Hospital Workers On Best Environmental PracticesHealth Care Without Harm - AsiaÎncă nu există evaluări
- Endologix ELGX Updated Investor PresentationDocument18 paginiEndologix ELGX Updated Investor PresentationmedtechyÎncă nu există evaluări
- Hasenzahl Professional Meeting Reflective JournalDocument2 paginiHasenzahl Professional Meeting Reflective Journalapi-328448022Încă nu există evaluări
- IELTS Writing Task 2 Sample 524 - Some People Think That Mobile Phones Should Be Banned in Public Places PDFDocument6 paginiIELTS Writing Task 2 Sample 524 - Some People Think That Mobile Phones Should Be Banned in Public Places PDFFotini KalaiÎncă nu există evaluări
- Nurse Interview2Document9 paginiNurse Interview2shalf0xÎncă nu există evaluări