Documente Academic
Documente Profesional
Documente Cultură
PIIS1473309920302735
Încărcat de
mostafa shahrabiDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
PIIS1473309920302735
Încărcat de
mostafa shahrabiDrepturi de autor:
Formate disponibile
Articles
Connecting clusters of COVID-19: an epidemiological and
serological investigation
Sarah Ee Fang Yong*, Danielle Elizabeth Anderson*, Wycliffe E Wei, Junxiong Pang, Wan Ni Chia, Chee Wah Tan, Yee Leong Teoh,
Priyanka Rajendram, Matthias Paul Han Sim Toh, Cuiqin Poh, Valerie T J Koh, Joshua Lum, Nur-Afidah Md Suhaimi, Po Ying Chia,
Mark I-Cheng Chen, Shawn Vasoo, Benjamin Ong, Yee Sin Leo, Linfa Wang*, Vernon J M Lee*
Summary
Background Elucidation of the chain of disease transmission and identification of the source of coronavirus disease Lancet Infect Dis 2020
2019 (COVID-19) infections are crucial for effective disease containment. We describe an epidemiological investigation Published Online
that, with use of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) serological assays, established links April 21, 2020
https://doi.org/10.1016/
between three clusters of COVID-19. S1473-3099(20)30273-5
See Online/Comment
Methods In Singapore, active case-finding and contact tracing were undertaken for all COVID-19 cases. Diagnosis for https://doi.org/10.1016/
acute disease was confirmed with RT-PCR testing. When epidemiological information suggested that people might S1473-3099(20)30322-4
have been nodes of disease transmission but had recovered from illness, SARS-CoV-2 IgG serology testing was used *Contributed equally
to establish past infection. Ministry of Health, Singapore
(S E F Yong MMed, W E Wei MPH,
Findings Three clusters of COVID-19, comprising 28 locally transmitted cases, were identified in Singapore; these P Rajendram MPH, C Poh MPH,
V T J Koh MPH, J Lum BA,
clusters were from two churches (Church A and Church B) and a family gathering. The clusters in Church A and N-A M Suhaimi PhD, B Ong FRCP,
Church B were linked by an individual from Church A (A2), who transmitted SARS-CoV-2 infection to the primary V J M Lee PhD); National
case from Church B (F1) at a family gathering they both attended on Jan 25, 2020. All cases were confirmed by University Health System,
RT-PCR testing because they had active disease, except for A2, who at the time of testing had recovered from their Singapore (S E F Yong, B Ong);
Programme in Emerging
illness and tested negative. This individual was eventually diagnosed with past infection by serological testing. ELISA Infectious Diseases,
assays showed an optical density of more than 1·4 for SARS-CoV-2 nucleoprotein and receptor binding domain Duke-National University
antigens in titres up to 1/400, and viral neutralisation was noted in titres up to 1/320. of Singapore Medical School,
Singapore (D E Anderson PhD,
W N Chia PhD, C W Tan PhD,
Interpretation Development and application of a serological assay has helped to establish connections between Prof L Wang PhD); National
COVID-19 clusters in Singapore. Serological testing can have a crucial role in identifying convalescent cases or people Centre for Infectious Diseases,
with milder disease who might have been missed by other surveillance methods. Singapore (W E Wei,
M P H S Toh MMed,
P Y Chia MRCP, M I-C Chen PhD,
Funding National Research Foundation (Singapore), National Natural Science Foundation (China), and National S Vasoo MRCP,
Medical Research Council (Singapore). Prof Y S Leo FRCP); Centre for
Infectious Disease
Epidemiology and Research
Copyright © 2020 Elsevier Ltd. All rights reserved.
(J Pang PhD), and
Saw Swee Hock School of
Introduction recovered and no longer shed the virus. Hence, serological Public Health (J Pang,
As of April 15, 2020, more than 1·9 million cases of tests are needed to identify convalescent cases and aid Y L Teoh MMed, M P H S Toh,
M I-C Chen, V J M Lee), National
coronavirus disease 2019 (COVID-19), and more than investigations and containment efforts.
University of Singapore,
120 000 deaths from the disease, have been recorded We present findings of investigations from Jan 29 to Singapore (B Ong); Singapore
worldwide.1 Many initial cases reported outside of China Feb 24, 2020, that linked two people with COVID-19 from Clinical Research Institute,
were imported or were linked to travellers from China.2,3 Wuhan, China, to three clusters of COVID-19 cases in Singapore (Y L Teoh); Ministry
of Health Office for Healthcare
However, as community transmission has become Singapore. Serological testing had a crucial role in estab Transformation, Singapore
widespread, the source of cases of COVID-19 in several lishing a link between clusters, showing its use in (Y L Teoh); and Tan Tock Seng
countries has not been established. identifying convalescent COVID-19 cases and supporting Hospital, Singapore (P Y Chia,
In Singapore, a globally connected city-state in southeast epidemiological investigations. S Vasoo, Prof Y S Leo)
Asia, health officials have attempted to contain the spread Correspondence to:
of COVID-19 through intensive epidemiological investi Methods Dr Vernon J M Lee,
Communicable Diseases
gations coupled with isolation of cases and quarantine of Surveillance methods and identification of cases Division, Ministry of Health,
close contacts. However, establishing the source of infec In Singapore, several surveillance methods are used to Singapore 169854
tion to ascertain the possible extent of spread can be identify people with COVID-19. On Jan 2, 2020, a suspect vernon_lee@moh.gov.sg
difficult, because scant epidemiological data might be case-definition of COVID-19 was circulated to all doctors
available. Even when possible nodes of transmission are in Singapore;4 doctors are legally required to notify
retrospectively identified through epidemiological investi the Ministry of Health of cases of COVID-19.5 From
gations, nucleic acid-based tests would not be diag Jan 31, 2020, Singapore began testing all patients
nostically useful if these infected individuals have with pneumonia in hospital for severe acute respiratory
www.thelancet.com/infection Published online April 21, 2020 https://doi.org/10.1016/S1473-3099(20)30273-5 1
Articles
Research in context
Evidence before this study establish links between clusters. RT-PCR testing alone
We searched PubMed on March 3, 2020, for reports on is limited by its ability to detect convalescent cases of
serological testing in individuals with coronavirus disease 2019 COVID-19, because RT-PCR can only detect severe acute
(COVID-19). We used the keywords (“COVID-19”, OR respiratory syndrome coronavirus 2 during the period of viral
“2019-nCoV”, OR “SARS-CoV-2”) AND (“serology” OR shedding, which is the acute phase of infection. Serological
“serologic testing”). Our search did not identify any reports testing can be useful in detecting previous infection in people
of the epidemiological application of serological tests in with suspected infection who have recovered, assisting in
COVID-19. In one report, researchers described serological epidemiological investigation and containment efforts.
characteristics of COVID-19, and in other publications,
Implications of all the available evidence
researchers have commented on the potential importance
COVID-19 laboratory testing is focused on use of quantitative
of COVID-19 serological tests. In another study, epidemiological
RT-PCR for diagnosis, and serological testing can be
investigations were reported of the epidemic in Singapore,
overlooked. We have highlighted the importance of serological
but serological methods had not been used.
testing for epidemiological investigation of COVID-19 cases,
Added value of this study and we urge further development of serological testing
In our epidemiological investigation, we used RT-PCR and capabilities.
serological testing to diagnose cases of COVID-19 and
syndrome coronavirus 2 (SARS-CoV-2); this testing was was established at the Duke-National University of
later expanded to include people with pneumonia in Singapore Medical School ABSL3 facility using a
primary care. The diagnosis of COVID-19 is confirmed SARS-CoV-2 virus isolate (BetaCoV/Singapore/2/2020;
either by a respiratory sample testing positive for GISAID accession number EPI_ISL_407987) cultured
SARS-CoV-2 using a laboratory-based RT-PCR6 or by a from a patient in Singapore; VNT was done using protocols
serum sample testing positive for SARS-CoV-2 on sero previously published for severe acute respiratory syndrome
logical analysis.7 coronavirus (SARS-CoV).7 For ELISA assays, we used
Once individuals with COVID-19 were identified, their recombinant nucleocapsid protein from SARS-CoV and
activities from 14 days before symptom onset until they SARS-CoV-2 expressed in mammalian cell culture using
were isolated were mapped and their close contacts traced. the pcDNA3.1 vector (ThermoFisher Scientific, Carlsbad,
Contact tracing before symptom onset was done to identify CA, USA), according to previously published methods,8
the source of exposure that led to the case being infected, and a recombinant receptor binding domain (RBD) of
allowing for further active case-finding around the source. the SARS-CoV-2 spike protein custom-produced by a
Contact tracing after symptom onset until isolation was commercial provider (GenScript, Piscataway, NJ, USA).
done to identify exposed individuals for quarantine to ELISA wells were coated with 100 ng of the respective
break the transmission chain. Both these approaches were protein per well and serum samples were used at dilutions
part of the containment strategy. A close contact was from 1/50 to 1/400, followed by horseradish peroxidase-
defined as anyone who had prolonged contact within 2 m conjugated goat anti-human IgG (Santa Cruz, Dallas, TX,
of the case. All close contacts with active or recent USA) used at a dilution of 1/2000.
symptoms were tested, whereas those who were asymp
tomatic and exposed while the case was symptomatic were Role of the funding source
quarantined. Activity maps were reviewed and cross- The funders had no role in study design, data collection,
checked to establish potential expo sures and identify data analysis, data interpretation, or writing of the report.
possible epidemiological links between cases and clusters. The corresponding author had full access to all data
All epidemiological investigations and outbreak con in the study and had final responsibility for the decision
tain
ment measures were implemented under the to submit for publication.
Infectious Diseases Act,5 which allows use of data for
analysis to control outbreaks. Results
As of April 6, 2020, Singapore had recorded 1375 cases of
Laboratory techniques COVID-19, of which 554 were imported and 821 locally
For laboratory confirmation of COVID-19, we did RT-PCR transmitted. Three clusters were identified that involved
testing for SARS-CoV-2, using previously published two churches (Church A and Church B) and one family
methods.6 Two serological platforms were developed for gathering. These clusters comprised 28 locally transmitted
confirmation of specific antibody responses to SARS-CoV-2 cases. The clusters were linked to two travellers (W1 and
in people with suspected infection or individuals with W2) from Wuhan, China, who attended a church service
PCR-confirmed disease. A virus neutralisation test (VNT) at Church A on Jan 19, 2020 (figure 1). The clusters at
2 www.thelancet.com/infection Published online April 21, 2020 https://doi.org/10.1016/S1473-3099(20)30273-5
Articles
W1
W2
A1
A2
A3
A4
A5
F1
F6
F2
F3
A2
F4
F5
F7
B6
Case B11
B1
Primary case of a cluster F1 B13
Church A service Jan 19, 2020
Wuhan travellers B14
B2 B3
Church A B4
Family gathering B15
Church B B5
Transmission B7
Possible transmission B8
Indirect link B16
Attended Church A service B9
B10
B12
19 20 21 22 23 24 25 26 27 28 29 30 31 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17
January February
Date
Figure 1: Transmission map of COVID-19
Map shows how COVID-19 was linked to two travellers from Wuhan, China, and two church clusters and a family gathering in Singapore. COVID-19=coronavirus
disease 2019.
Church A and Church B were linked by one individual the church. Although all five people had developed
from Church A (A2), who probably transmitted the symptoms by Feb 2, 2020 (figure 2), only A1, A4, and A5
infection to the primary case of the Church B cluster (F1) were diagnosed (between Feb 6 and Feb 8, 2020), because
at a family gathering on Jan 25, 2020. All cases were they had been hospitalised for pneumonia and tested for
confirmed by RT-PCR testing, except for A2, who was SARS-CoV-2 as part of enhanced surveillance measures
diagnosed by serological testing. to test all patients admitted to hospital with pneumonia.
The clusters at Church A and Church B were detected A2 and A3 were not diagnosed when symptomatic in late
in early February and mid-February, respectively. January because their symptoms were mild and they did
Although W1 and W2 were diagnosed with COVID-19 at not meet the suspect case-definition at that time. A2 and
the end of January, their possible link to Church A was A3 were tested only after mapping of activities and
only discovered after the Church A cluster was identified, movements of other cases suggested that A2 could be the
through investigation and repeat interviews.5 By that missing link between the clusters at Church A and
time, A2 had recovered from COVID-19 and was not Church B. An RT-PCR test of a nasopharyngeal specimen
immediately linked to either cluster. Family members taken from A3 on Feb 18, 2020, was positive, although
who had been infected at the family gathering on this individual had clinically recovered from the illness,
Jan 25, 2020, were first linked to F1 and were initially which persisted from Jan 28 to Feb 10, 2020. Serological
regarded as part of the cluster at Church B. However, analysis of a serum sample obtained on the same day as
subsequent investigations into case histories indicated the nasopharyngeal specimen was also positive. Although
that the family cluster was a distinct cluster and that A2 A2 had two negative RT-PCR tests, the serological result
was most probably the missing link between the two was positive, indicating past infection.
church clusters; this idea was substantiated when A2’s A2 and A3 attended a Chinese New Year family
serological results were confirmed to be positive. gathering on Jan 25, 2020, at the home of F1. Nine cases
Five locally transmitted cases of COVID-19 (A1–A5) (A2, A3, and F1–F7) were linked to this family gathering.
were linked to Church A. These people attended a church A2, whose symptoms started on Jan 23, 2020, was
service on Jan 19, 2020, the same day W1 and W2 visited unwell at this event and most probably was the primary
www.thelancet.com/infection Published online April 21, 2020 https://doi.org/10.1016/S1473-3099(20)30273-5 3
Articles
Travellers from Wuhan
W1, 56F
W2, 56M
Church A cluster
A1, 53M
A2, 58F
A3, 54M
A4, 39F
A5, 52F
Family gathering cluster
F1, 28M
F2, 79F
F3, 27F
F4, 35F
F5, 38F
F6, 25M
F7, 30F
Church B cluster
B1, 34M
B2, 46M
B3, 48M
B4, 55M
B5, 57M
B6, 51F
B7, 44F
B8, 56F
B9, 43M
B10, 54M
B11, 55F
B12, 54F
Figure 2: Incubation period, B13, 26M
Incubation period
duration of symptoms, and Possible incubation period
length of admission, from Symptom onset until admission B14, 57F
Jan 14 to Feb 26, 2020 Duration of admission
Data for 30 people with Length of current admission B15, 29M
coronavirus disease 2019 are Symptom onset until laboratory confirmation (not admitted)
shown. Individuals are Isolation date B16 50M
labelled with cluster letter and Laboratory confirmation date
number, age (years) and sex
(M=male; F=female). Median 14 19 24 29 3 8 13 18 23 28
age of affected individuals
was 50·5 (IQR 25–79) years January February
and half the cohort (15 of 30)
Date
were female.
4 www.thelancet.com/infection Published online April 21, 2020 https://doi.org/10.1016/S1473-3099(20)30273-5
Articles
A B
2 SARS-CoV-2 NP
1/50 1/100 1/200 1/400 Replicate
1·5
Optical density
1 2 3
1
COVID-19 1/80 1/160 1/80
0·5
SARS Negative Negative Negative
0 Negative Negative Negative
Control
2 SARS-CoV-2 RBD
A2 1/160 1/320 1/320
1·5
A3 1/160 1/160 1/80
Optical density
0·5
0
COVID-19 SARS Control A2 A3
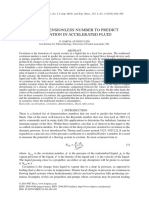
Figure 3: Serological testing of two patients
(A) ELISA testing using SARS-CoV-2 NP and RBD antigens. In addition to serum samples from the two suspected cases (A2 and A3), known positive samples for
COVID-19 and SARS, and negative samples, were included in the testing, and serial dilutions were done. (B) VNT results at the highest dilution that could effectively
neutralise the SARS-CoV-2 infection. COVID-19=coronavirus disease 2019. NP=nucleocapsid protein. RBD=receptor binding domain. SARS=severe acute respiratory
syndrome. SARS-CoV-2=severe acute respiratory syndrome coronavirus 2. VNT=virus neutralisation test.
source of transmission. A3 developed symptoms later, neutralising antibodies), in addition to use of traditional
on Jan 28, 2020, and was, therefore, unlikely to be the epidemiological methods, was important in establishing
source of infection at this gathering. links among locally transmitted COVID-19 cases and
17 locally transmitted cases were linked to Church B tracing the transmission chain to an imported source.
(B1–B16 and F1). Thorough review of activity maps Detection of COVID-19 can be difficult because of the non-
ascertained that F1, who had developed symptoms on specific mild respiratory symptoms in many affected
Jan 29, 2020, and continued to work at Church B while individuals and because some people might recover
ill, was the primary case of the Church B cluster. without being diagnosed.9 Although PCR tests offer a rapid
In mid-February, epidemiological and clinical evidence diagnostic solution, they can only detect SARS-CoV-2
strongly suggested that A2 was the missing link between during the period of viral shedding, which is the acute
the clusters at Church A and Church B through attendance phase of infection. The duration of viral shedding for
at the family gathering on Jan 25, 2020, while symptomatic. COVID-19 is not certain,10 but SARS-CoV data indicate that
However, by the time this link was ascertained, more than 21 days after symptom onset, 53% of cases achieved viral
3 weeks had passed from symptom onset on Jan 23, 2020, clearance in nasopharyngeal aspirate samples.11 As such,
and symptoms had resolved completely a week previously, PCR testing alone is limited by its ability to detect
on Feb 8–10, 2020. A2 had two negative RT-PCR test convalescent cases.
results from samples taken from the nasopharynx, with Serological testing can be especially useful in detecting
testing done 1 day apart on Feb 18 and Feb 19, 2020. The a previous suspected infection in people who have
sample for serological testing was taken on Feb 18, 2020, recovered. For seroconversion kinetics, past coronavirus
and a positive result was confirmed on Feb 22, 2020. studies indicate that all patients with Middle East
ELISA results for A2 and A3 on Feb 20, 2020 (figure 3A) respiratory syndrome (MERS) seroconverted 3 weeks
showed a strong antibody response to the SARS-CoV-2 after symptoms started,12 and 93% of patients with severe
RBD protein, which was not seen in serum samples acute respiratory syndrome (SARS) seroconverted at
from SARS-CoV patients. The results were further an average of 20 days from symptom onset.11 The first
confirmed by VNT on Feb 22, 2020 (figure 3B). preliminary analysis of SARS-CoV-2 IgM and IgG
indicated that the antibody response in COVID-19
Discussion patients is similar to, if not earlier than, these times.13
This investigation shows how SARS-CoV-2 serological Cross-reactivity of immunoglobulins to closely related
analysis (ELISA detecting IgG and VNT detecting viruses such as SARS-CoV is a potential issue,14 but our
www.thelancet.com/infection Published online April 21, 2020 https://doi.org/10.1016/S1473-3099(20)30273-5 5
Articles
RBD-based ELISA showed sufficient differentiation difficulty in obtaining information from cases and
power, a finding further supported by VNT results. contacts, which could be inaccurate because of recall and
IgM serological testing might hold promise as other biases. In our investigation, information for
a diagnostic method, although for SARS and MERS, limi symptom onset of W1 and W2 was based on case history
tations for its use have been noted.12,13 For MERS, IgM was alone and could not be independently corroborated.5
not detected earlier than IgG, and IgM against prevalent In such instances, determining the transmission chain
human coronaviruses showed cross-reactivity.12 Pre would have to account for possible inconsistencies in
liminary data for SARS-CoV-2 IgM are promising,13 but case history and rely on triangulation with other methods.
more work is needed to assess the feasibility of IgM The development and adoption of additional laboratory
serological analysis as a rapid diagnostic method to techniques, such as serological tests and phylogenetic
enhance COVID-19 detection capabilities. analysis by whole-genome sequencing, could help
For most people in the three clusters we report here, identify possible links between cases.
transmission of infection was accounted for by close Serological testing is a key method in the response to
contact with a symptomatic case. Our findings suggest the COVID-19 epidemic. As shown in our study, it enabled
that COVID-19 is largely transmitted by close contact, detection of a convalescent case, which could be key in
particularly when contact occurs over a prolonged period initial containment efforts to discover transmission links
and in close congregation. Two churches were the to support containment efforts. Serological testing also
setting for COVID-19 transmission in our report. detects people with mild or asymptomatic disease who
A church cluster has also been reported in South Korea.15 have recovered, allowing for more accurate determination
Churches host prolonged repeated activities, during of the number of people probably infected in a cluster or
which close contact occurs, thus providing the oppor the population. Identifying people who were probably
tunity for disease spread through droplets or fomites. infected in household or school clusters could help
Singing (a common practice in churches) can generate ascertain attack rates by age, particularly among children
droplets in a similar quantity to coughing.16,17 Repeated who mostly manifest less severe disease.18 Calculating
social interactions of church groups has also facilitated population-level attack rates is also important to estimate
discovery of transmission, compared with other settings disease incidence and the case-fatality rate (CFR). Thus
in which people might not know each other. The inter far, the CFR for COVID-19 has been based on PCR-
actions are similar in nature to large family gatherings, diagnosed symptomatic cases. Serological surveys would
which other cases in our report were linked to. Other be important to estimate CFR more accurately and would
similar settings include school and workplaces, in which better inform calibrated responses to COVID-19. As the
respiratory disease transmission is not uncommon and pandemic progresses, monitoring seroprevalence would
should be the focus for preparedness, surveillance, and enable countries to track transmission dynamics and
containment measures. population immunity levels and to inform disease
Risk of transmission could be reduced if symptomatic control policies. Such monitoring would necessitate the
people do not attend events in which prolonged social development of ready serological testing solutions that are
interactions take place (eg, at the family gathering when cost-effective and the establishment of population-level
A2 was unwell, and F1 who continued to work at surveillance programmes to obtain blood samples.
Church B while unwell). Other risk reduction measures Development and application of serological assays
could include having smaller group activities and has helped to unravel connections between three
prevention of interactions across these groups. Moreover, clusters of COVID-19 in Singapore, linking the disease
there may be common touchpoints within each setting to two travellers from China. Serological assays should
that could result in contact transmission. To prevent be considered to identify mild or subclinical infections
transmission, people should practice increased personal in the community.
hygiene and reduce physical contact to minimise indirect Contributors
transmission risks. VJML and YLT had the idea for the study and contributed to study design.
Linking disease transmission to an imported source CP, VTJK, JL, N-AMS, and PYC contributed to the epidemiological
investigation and data collection. VJML, YLT, SEFY, PR, MPHST, JP, and
and contact tracing for each identified case has facilitated WEW contributed to analysis and interpretation of epidemiological data.
a high capture of cases in Singapore. This successful LW, DEA, WNC, and CWT developed the serological methods and
linking of a large proportion of cases to imported sources contributed to the analysis and interpretation. SEFY, WEW, and JP wrote
provides encouraging evidence that the intense contain the report, and VJML, MI-CC, SV, BO, YSL, LW, and DEA contributed to
critical revision.
ment measures undertaken in Singapore have been
effective. The three clusters we report here occurred Declaration of interests
We declare no competing interests.
relatively early in the emergence of COVID-19 in
Singapore, within 4 weeks of the first imported case. Acknowledgments
The development of serological tests was funded in part by a joint grant
As the epidemic continues, it might be progressively under the National Research Foundation (Singapore) and the National
difficult to establish linkages by relying on traditional Natural Science Foundation of China (NRF2016NRFNSFC002-013).
epidemiological methods alone. Challenges include The study was partly funded by the National Medical Research Council
6 www.thelancet.com/infection Published online April 21, 2020 https://doi.org/10.1016/S1473-3099(20)30273-5
Articles
(Singapore) COVID19 research fund (COVID19RF-001). We thank our 9 Novel Coronavirus Pneumonia Emergency Response Epidemiology
colleagues who contributed to the investigations, including the Team. The epidemiological characteristics of an outbreak of 2019
COVID-19 epidemiology workgroup, contact tracing team, and hospital novel coronavirus diseases (COVID-19) in China.
epidemiology teams; and Viji Vijayan, Benson Ng, and Velraj Sivalingam, Zhonghua Liu Xing Bing Xue Za Zhi 2020; 41: 145–51 (in Chinese).
(Duke-National University of Singapore ABSL3 facility) for logistics 10 Vetter P, Eckerle I, Kaiser L. Covid-19: a puzzle with many missing
management and assistance. pieces. BMJ 2020; 368: m627.
11 Peiris JSM, Chu CM, Cheng VCC, et al. Clinical progression and
References viral load in a community outbreak of coronavirus-associated SARS
1 WHO. Coronavirus disease 2019 (COVID-19): situation report—86. pneumonia: a prospective study. Lancet 2003; 361: 1767–72.
April 15, 2020. https://www.who.int/docs/default-source/ 12 Corman VM, Albarrak AM, Omrani AS, et al. Viral shedding and
coronaviruse/situation-reports/20200415-sitrep-86-covid-19. antibody response in 37 patients with Middle East respiratory
pdf?sfvrsn=c615ea20_6 (accessed April 16, 2020). syndrome coronavirus infection. Clin Infect Dis 2015; 62: 477–83.
2 Hoehl S, Rabenau H, Berger A, et al. Evidence of SARS-CoV-2 13 Zhang W, Du R-H, Li B, et al. Molecular and serological
infection in returning travelers from Wuhan, China. investigation of 2019-nCoV infected patients: implication of
N Engl J Med 2020; 382: 1278–80. multiple shedding routes. Emerg Microbes Infect 2020; 9: 386–89.
3 Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV 14 Meyer B, Drosten C, Muller MA. Serological assays for emerging
infection from an asymptomatic contact in Germany. coronaviruses: challenges and pitfalls. Virus Res 2014; 194: 175–83.
N Engl J Med 2020; 382: 970–71.
15 Korea Centers for Disease Control and Prevention. The updates
4 Ministry of Health Singapore. Circular no 04/2020: viral pneumonia of COVID-19 in Korea. Feb 29, 2020. https://www.cdc.go.kr/board/
of unknown cause in Wuhan city, China. Singapore: Ministry of board.es?mid=a30402000000&bid=0030&act=view&list_
Health, 2020. no=366406&tag=&nPage=7 (accessed April 1, 2020).
5 Singapore Statutes Online. Infectious Diseases Act 2003. 16 Loudon RG, Roberts RM. Singing and the dissemination of
July 31, 2003. https://sso.agc.gov.sg/Act/IDA1976 (accessed tuberculosis. Am Rev Respir Dis 1968; 98: 297–300.
April 1, 2020).
17 Asadi S, Wexler AS, Cappa CD, Barreda S, Bouvier NM,
6 Pung R, Chiew CJ, Young BE, et al. Investigation of three clusters Ristenpart WD. Aerosol emission and superemission during
of COVID-19 in Singapore: implications for surveillance and human speech increase with voice loudness. Sci Rep 2019; 9: 2348.
response measures. Lancet 2020; 395: 1039–46.
18 Qiu H, Wu J, Hong L, Luo Y, Song Q, Chen D. Clinical and
7 Li W, Shi Z, Yu M, et al. Bats are natural reservoirs of SARS-like epidemiological features of 36 children with coronavirus disease
coronaviruses. Science 2005; 310: 676–79. 2019 (COVID-19) in Zhejiang, China: an observational cohort study.
8 Ge X-Y, Li J-L, Yang X-L, et al. Isolation and characterization Lancet Infect Dis 2020; published online March 25.
of a bat SARS-like coronavirus that uses the ACE2 receptor. https://doi.org/10.1016/S1473-3099(20)30198-5.
Nature 2013; 503: 535–38.
www.thelancet.com/infection Published online April 21, 2020 https://doi.org/10.1016/S1473-3099(20)30273-5 7
S-ar putea să vă placă și
- Connecting Clusters of COVID 19 An EpidemiologicaDocument7 paginiConnecting Clusters of COVID 19 An EpidemiologicaRaisa Mentari MoeisÎncă nu există evaluări
- Asymptomatic and Human To Human Transmission of SARS COV 2Document3 paginiAsymptomatic and Human To Human Transmission of SARS COV 2belinda thaniaÎncă nu există evaluări
- From Sars To CoDocument23 paginiFrom Sars To ComcvilcaÎncă nu există evaluări
- Comment: Lancet Infect Dis 2020Document2 paginiComment: Lancet Infect Dis 2020dlundaÎncă nu există evaluări
- Liu2020 Article ClinicalAndBiochemicalIndexesFDocument11 paginiLiu2020 Article ClinicalAndBiochemicalIndexesFGabriel Ibarra TrujilloÎncă nu există evaluări
- NEJM. COVID CHINA. 10.1056@NEJMoa2002032Document13 paginiNEJM. COVID CHINA. 10.1056@NEJMoa2002032Boris CabreraÎncă nu există evaluări
- ARTIKELDocument6 paginiARTIKELandi susiloÎncă nu există evaluări
- Ciaa242 2 PDFDocument8 paginiCiaa242 2 PDFHesbon MomanyiÎncă nu există evaluări
- JMV 25815Document2 paginiJMV 25815fadil ahmadiÎncă nu există evaluări
- Estudo DiabetesDocument9 paginiEstudo DiabetesFulano de TalÎncă nu există evaluări
- Pages From WhuDocument2 paginiPages From Whurahat879Încă nu există evaluări
- Covid 19 Patients' Clinical Characteristics, Discharge Rate, and Fatality Rate of Meta AnalysisDocument7 paginiCovid 19 Patients' Clinical Characteristics, Discharge Rate, and Fatality Rate of Meta AnalysisDelfina RubioÎncă nu există evaluări
- Nejmoa 2002032Document13 paginiNejmoa 2002032Juan Antonio LópezÎncă nu există evaluări
- Clinical Characteristics of Children With Coronavirus Disease 2019 in Hubei, ChinaDocument6 paginiClinical Characteristics of Children With Coronavirus Disease 2019 in Hubei, ChinaBobanBisercicÎncă nu există evaluări
- Covid-19 in South Korea - Challenges of Subclinical ManifestationsDocument2 paginiCovid-19 in South Korea - Challenges of Subclinical ManifestationsSuwandi ChangÎncă nu există evaluări
- Novel Coronavirus-From Discovery To Clinical DiagnosisDocument2 paginiNovel Coronavirus-From Discovery To Clinical DiagnosisBoris ZegarraÎncă nu există evaluări
- Jurnal Chen Et AlDocument31 paginiJurnal Chen Et AlUtami MÎncă nu există evaluări
- Development and Evaluation of A Rapid CRISPR-based Diagnostic For COVID-19Document12 paginiDevelopment and Evaluation of A Rapid CRISPR-based Diagnostic For COVID-19YunaÎncă nu există evaluări
- Journal Pre-Proof: International Journal of Infectious DiseasesDocument14 paginiJournal Pre-Proof: International Journal of Infectious DiseasesKenya EspinozaÎncă nu există evaluări
- Piis1473309920309816 2Document12 paginiPiis1473309920309816 2Utami MÎncă nu există evaluări
- Clinical Characteristics of Coronavirus Disease 2019 in ChinaDocument13 paginiClinical Characteristics of Coronavirus Disease 2019 in ChinaprimaÎncă nu există evaluări
- 1 s2.0 S1473309920300670 Main PDFDocument2 pagini1 s2.0 S1473309920300670 Main PDFAdilla Shafryantyo PurnomoÎncă nu există evaluări
- Clinical Characteristics of CoronavirusDocument13 paginiClinical Characteristics of Coronavirusleonardo almeidaÎncă nu există evaluări
- PIIS0140673622003270Document7 paginiPIIS0140673622003270chaivat kÎncă nu există evaluări
- Clinical Microbiology and InfectionDocument6 paginiClinical Microbiology and InfectionMiguel AngelÎncă nu există evaluări
- International Journal of Infectious DiseasesDocument3 paginiInternational Journal of Infectious DiseasesDetti FahmiasyariÎncă nu există evaluări
- Epidemiological and Clinical Characteristics of 99 Cases of 2019 Novel Coronavirus Pneumonia in Wuhan, China: A Descriptive StudyDocument12 paginiEpidemiological and Clinical Characteristics of 99 Cases of 2019 Novel Coronavirus Pneumonia in Wuhan, China: A Descriptive Studyharapan panjaitanÎncă nu există evaluări
- Guo Et Al 2017Document11 paginiGuo Et Al 2017Ana Beatriz Vasquez RodriguezÎncă nu există evaluări
- Crossm: Culture-Based Virus Isolation To Evaluate Potential Infectivity of Clinical Specimens Tested For COVID-19Document8 paginiCrossm: Culture-Based Virus Isolation To Evaluate Potential Infectivity of Clinical Specimens Tested For COVID-19JefersonMatosdeColaresÎncă nu există evaluări
- PIIS1473309920301961Document10 paginiPIIS1473309920301961agboxÎncă nu există evaluări
- Epidemiological and Clinical Characteristics of 671 COVID-19 Patients in Henan Province, ChinaDocument11 paginiEpidemiological and Clinical Characteristics of 671 COVID-19 Patients in Henan Province, ChinaOrlando JúniorÎncă nu există evaluări
- Clinical Characteristic Covid ChildrenDocument8 paginiClinical Characteristic Covid ChildrenEstirahayuÎncă nu există evaluări
- Covid 19 PandemiaDocument5 paginiCovid 19 PandemiaCarol GomezÎncă nu există evaluări
- Clinical Characteristics and Diagnostic Challenges of Pediatric COVID-19: A Systematic Review and Meta-AnalysisDocument8 paginiClinical Characteristics and Diagnostic Challenges of Pediatric COVID-19: A Systematic Review and Meta-AnalysisArina Al-KhaqÎncă nu există evaluări
- Correspondence: Atypical Presentation of COVID-19 in Young InfantsDocument1 paginăCorrespondence: Atypical Presentation of COVID-19 in Young InfantsAlexRázuriÎncă nu există evaluări
- Diagnostic Utility of Clinical Laboratory Data Determinationsfor Patients With The Severe COVID 19Document6 paginiDiagnostic Utility of Clinical Laboratory Data Determinationsfor Patients With The Severe COVID 19junior rodriguesÎncă nu există evaluări
- Genomic Surveillance of COVID-19 Cases in Beijing: ArticleDocument9 paginiGenomic Surveillance of COVID-19 Cases in Beijing: ArticleCarlos CastroÎncă nu există evaluări
- aksungar2007Document10 paginiaksungar2007twarrenÎncă nu există evaluări
- Journal Pre-Proof: International Journal of Infectious DiseasesDocument18 paginiJournal Pre-Proof: International Journal of Infectious DiseasesKenya EspinozaÎncă nu există evaluări
- Letters: Positive RT-PCR Test Results in Patients Recovered From COVID-19Document2 paginiLetters: Positive RT-PCR Test Results in Patients Recovered From COVID-19samuelwellsÎncă nu există evaluări
- Jama 2020 2467 PDFDocument2 paginiJama 2020 2467 PDFsamon sumulongÎncă nu există evaluări
- Covid 19Document10 paginiCovid 19MonicaÎncă nu există evaluări
- Ciaa 247Document6 paginiCiaa 247berlian gurningÎncă nu există evaluări
- COVID-19: Towards Controlling of A Pandemic: CommentDocument4 paginiCOVID-19: Towards Controlling of A Pandemic: CommentEugenÎncă nu există evaluări
- A Comparative-Descriptive Analysis of Clinical Characteristics in 2019-Coronavirus-Infected Children and AdultsDocument28 paginiA Comparative-Descriptive Analysis of Clinical Characteristics in 2019-Coronavirus-Infected Children and AdultsPatrick NunsioÎncă nu există evaluări
- PIIS1473309920300864Document10 paginiPIIS1473309920300864Virginia ZagorniiÎncă nu există evaluări
- Different Longitudinal Patterns of Nucleic Acid and Serology Testing Results Based On Disease Severity of COVID-19 PatientsDocument5 paginiDifferent Longitudinal Patterns of Nucleic Acid and Serology Testing Results Based On Disease Severity of COVID-19 PatientsagboxÎncă nu există evaluări
- English ProjectDocument18 paginiEnglish ProjectSHADOW BOYÎncă nu există evaluări
- Covid 19Document9 paginiCovid 19MonicaÎncă nu există evaluări
- Journal of Infection: Lists Available atDocument6 paginiJournal of Infection: Lists Available atsameer sahaanÎncă nu există evaluări
- Curso Clinico y Factores de RiesgoDocument9 paginiCurso Clinico y Factores de RiesgoEliana TorresÎncă nu există evaluări
- Nepal's First 2019 Novel Coronavirus Case ReportedDocument2 paginiNepal's First 2019 Novel Coronavirus Case ReportedWiliam Silva CarrilloÎncă nu există evaluări
- Gender Differences in Patients With COVID-19: Focus On Severity and MortalityDocument6 paginiGender Differences in Patients With COVID-19: Focus On Severity and MortalityCamila Miranda LlanesÎncă nu există evaluări
- New Insights of Emerging Sars-Cov-2: Epidemiology, Etiology, Clinical Features, Clinical Treatment, and PreventionDocument22 paginiNew Insights of Emerging Sars-Cov-2: Epidemiology, Etiology, Clinical Features, Clinical Treatment, and PreventionWendi IochÎncă nu există evaluări
- Vertical Transmission of Severe Acute Respiratory Syndrome Coronavirus 2: A Systematic ReviewDocument6 paginiVertical Transmission of Severe Acute Respiratory Syndrome Coronavirus 2: A Systematic ReviewDra Sandra VèlezÎncă nu există evaluări
- Xu2020 Article EvolutionOfTheNovelCoronavirusDocument4 paginiXu2020 Article EvolutionOfTheNovelCoronavirusIkbal HamonanganÎncă nu există evaluări
- The Rapid Assessment and Early Warning Models For COVID-19Document8 paginiThe Rapid Assessment and Early Warning Models For COVID-19Windu SyawalinaÎncă nu există evaluări
- Articles: Heshui Shi, Xiaoyu Han, Nanchuan Jiang, Yukun Cao, Osamah Alwalid, Jin Gu, Yanqing Fan, Chuansheng ZhengDocument10 paginiArticles: Heshui Shi, Xiaoyu Han, Nanchuan Jiang, Yukun Cao, Osamah Alwalid, Jin Gu, Yanqing Fan, Chuansheng Zhengsri karuniaÎncă nu există evaluări
- 2020 02 11 20021493v2 FullDocument17 pagini2020 02 11 20021493v2 FullRogelio MoscosoÎncă nu există evaluări
- Diagnostic Imaging of Novel Coronavirus PneumoniaDe la EverandDiagnostic Imaging of Novel Coronavirus PneumoniaMinming ZhangÎncă nu există evaluări
- Gas Pipeline Hydraulics: E. Shashi MenonDocument13 paginiGas Pipeline Hydraulics: E. Shashi Menonmostafa shahrabiÎncă nu există evaluări
- Example Letter To Send To EmbassyDocument2 paginiExample Letter To Send To EmbassyEgi Defiska MulyaÎncă nu există evaluări
- (Paperhub - Ir) 10.1002 9781119083948.ch5Document140 pagini(Paperhub - Ir) 10.1002 9781119083948.ch5mostafa shahrabiÎncă nu există evaluări
- Visa Interview Questions: Personal InfoDocument5 paginiVisa Interview Questions: Personal Infomostafa shahrabiÎncă nu există evaluări
- Effect of Time On Pipe RoughnessDocument11 paginiEffect of Time On Pipe Roughnessmostafa shahrabiÎncă nu există evaluări
- Effect of Time On Pipe RoughnessDocument11 paginiEffect of Time On Pipe Roughnessmostafa shahrabiÎncă nu există evaluări
- A Notice: EZ Setup EZ SetupDocument1 paginăA Notice: EZ Setup EZ SetupTheomas AbdiÎncă nu există evaluări
- Effect of Time On Pipe RoughnessDocument11 paginiEffect of Time On Pipe Roughnessmostafa shahrabiÎncă nu există evaluări
- Viscosity Measurements of Ammonia, R32, and R134a. Vapor Buoyancy and Radial Acceleration in Capillary ViscometersDocument34 paginiViscosity Measurements of Ammonia, R32, and R134a. Vapor Buoyancy and Radial Acceleration in Capillary Viscometersmostafa shahrabiÎncă nu există evaluări
- New Dimensionless Number To Predict Cavitation in Accelerated FluidDocument9 paginiNew Dimensionless Number To Predict Cavitation in Accelerated Fluidmostafa shahrabiÎncă nu există evaluări
- 51 Successful Answers For Visa InterviewDocument4 pagini51 Successful Answers For Visa Interviewmostafa shahrabiÎncă nu există evaluări
- Author Manuscript: Reference Correlation For The Viscosity of Ammonia From The Triple Point To 725 K and Up To 50 Mpaa)Document27 paginiAuthor Manuscript: Reference Correlation For The Viscosity of Ammonia From The Triple Point To 725 K and Up To 50 Mpaa)mostafa shahrabiÎncă nu există evaluări
- New Dimensionless Number To Predict Cavitation in Accelerated FluidDocument9 paginiNew Dimensionless Number To Predict Cavitation in Accelerated Fluidmostafa shahrabiÎncă nu există evaluări
- Watson IEC 1943Document9 paginiWatson IEC 1943mostafa shahrabiÎncă nu există evaluări
- UAE Government Approved Laboratories Dubai 24112020 Tcm8 161089Document1 paginăUAE Government Approved Laboratories Dubai 24112020 Tcm8 161089Mohammed IqbalÎncă nu există evaluări
- App 6Document2 paginiApp 6mostafa shahrabiÎncă nu există evaluări
- Acs Iecr 9b03512Document26 paginiAcs Iecr 9b03512mostafa shahrabiÎncă nu există evaluări
- Water Hammer EquationsDocument11 paginiWater Hammer Equationsmostafa shahrabiÎncă nu există evaluări
- SN19.4-Matthews-Lessons Learned Express Pipeline ProjectDocument12 paginiSN19.4-Matthews-Lessons Learned Express Pipeline Projectmostafa shahrabiÎncă nu există evaluări
- Adibatic Bulk ModulusDocument2 paginiAdibatic Bulk ModulusTechie HarryÎncă nu există evaluări
- Acs Iecr 9b03512Document26 paginiAcs Iecr 9b03512mostafa shahrabiÎncă nu există evaluări
- Orifice Gas Flow Chart PDFDocument1 paginăOrifice Gas Flow Chart PDFmostafa shahrabiÎncă nu există evaluări
- A022003 Aci PDFDocument12 paginiA022003 Aci PDFmostafa shahrabiÎncă nu există evaluări
- Computational Compliance Criteria in Water Hammer Modelling: E3S Web of Conferences September 2017Document9 paginiComputational Compliance Criteria in Water Hammer Modelling: E3S Web of Conferences September 2017mostafa shahrabiÎncă nu există evaluări
- Eng BD Fta1181Document14 paginiEng BD Fta1181mostafa shahrabiÎncă nu există evaluări
- Solar: MCL CDocument37 paginiSolar: MCL Cmostafa shahrabiÎncă nu există evaluări
- Gas Hydrate Formation and Dissociation Numerical Modelling With Nitrogen and Carbon DioxideDocument30 paginiGas Hydrate Formation and Dissociation Numerical Modelling With Nitrogen and Carbon Dioxidemostafa shahrabiÎncă nu există evaluări
- 10 1 1 678 1140 PDFDocument5 pagini10 1 1 678 1140 PDFmostafa shahrabiÎncă nu există evaluări
- Compressor Strategy Overview: AA3 and AA4 PlansDocument43 paginiCompressor Strategy Overview: AA3 and AA4 Plansmostafa shahrabiÎncă nu există evaluări
- HidratosDocument6 paginiHidratosLuis Joel Ramos RamosÎncă nu există evaluări
- Flow Crete OverviewDocument1 paginăFlow Crete OverviewsathiyanÎncă nu există evaluări
- Geoheritage of Labuan Island: Bulletin of The Geological Society of Malaysia December 2016Document14 paginiGeoheritage of Labuan Island: Bulletin of The Geological Society of Malaysia December 2016songkkÎncă nu există evaluări
- TN EpasssDocument2 paginiTN EpasssStephenrajÎncă nu există evaluări
- Official Game GuideDocument30 paginiOfficial Game GuideHhfugÎncă nu există evaluări
- Piping and Valves Trim MaterialsDocument2 paginiPiping and Valves Trim MaterialsDmitriy RybakovÎncă nu există evaluări
- Antihyperlipidemic AgentsDocument71 paginiAntihyperlipidemic AgentsFirda100% (1)
- LESSON 1 PREPARE VEGETABLE DISHES OverviDocument12 paginiLESSON 1 PREPARE VEGETABLE DISHES OverviKeym Garcia Galvez IIIÎncă nu există evaluări
- Guidance On The 2010 ADA Standards For Accessible Design Volume 2Document93 paginiGuidance On The 2010 ADA Standards For Accessible Design Volume 2Eproy 3DÎncă nu există evaluări
- GEK_30375M Lubrication SpecificationsDocument34 paginiGEK_30375M Lubrication SpecificationsMARITZA GABRIELA ARIZABAL MEDINAÎncă nu există evaluări
- Do We Still Need Formocresol in Pediatric DentistryDocument3 paginiDo We Still Need Formocresol in Pediatric DentistryAlexanderDetorakisÎncă nu există evaluări
- NCPDocument18 paginiNCPChristian Karl B. LlanesÎncă nu există evaluări
- Recent Developments in Carbapenems: ReviewDocument16 paginiRecent Developments in Carbapenems: ReviewFrancielleÎncă nu există evaluări
- Final Draft - Banana ChipsDocument34 paginiFinal Draft - Banana ChipsAubrey Delgado74% (35)
- Work Family Conflict Dengan KinerjaDocument11 paginiWork Family Conflict Dengan KinerjaNinaerizaÎncă nu există evaluări
- Calcul BADocument15 paginiCalcul BAHanane BenGamraÎncă nu există evaluări
- Comparative Analysis of Mineral Constituents of Ethanol Leaf and SeedDocument9 paginiComparative Analysis of Mineral Constituents of Ethanol Leaf and SeedKIU PUBLICATION AND EXTENSIONÎncă nu există evaluări
- Litreature On Automatic Dipper Circuit For Vehicle-2Document10 paginiLitreature On Automatic Dipper Circuit For Vehicle-2Rushikesh TajneÎncă nu există evaluări
- Best WiFi Adapter For Kali Linux - Monitor Mode & Packet InjectionDocument14 paginiBest WiFi Adapter For Kali Linux - Monitor Mode & Packet InjectionKoushikÎncă nu există evaluări
- JD - Hygiene Promotion OfficerDocument2 paginiJD - Hygiene Promotion OfficerBeauty ChigwazaÎncă nu există evaluări
- Pastillas DelightDocument12 paginiPastillas DelightBryan DutchaÎncă nu există evaluări
- Everything You Need to Know About Gas Metal Arc Welding (GMAWDocument31 paginiEverything You Need to Know About Gas Metal Arc Welding (GMAWAhmetDuranCeyhanÎncă nu există evaluări
- Chemical Equation CalculationsDocument6 paginiChemical Equation CalculationsHera RiegoÎncă nu există evaluări
- Aquatic Ecology and LimnologyDocument96 paginiAquatic Ecology and LimnologySale AlebachewÎncă nu există evaluări
- YUMMY TUMMY - Beef Biryani Recipe - Beef Dum Biryani RecipeDocument48 paginiYUMMY TUMMY - Beef Biryani Recipe - Beef Dum Biryani RecipeWilliam Cj LyngdohÎncă nu există evaluări
- New Accreditation ToolsDocument52 paginiNew Accreditation ToolsLyle Guion Paguio100% (1)
- Crypto Hash Algorithm-Based Blockchain Technology For Managing Decentralized Ledger Database in Oil and Gas IndustryDocument26 paginiCrypto Hash Algorithm-Based Blockchain Technology For Managing Decentralized Ledger Database in Oil and Gas IndustrySIMON HINCAPIE ORTIZÎncă nu există evaluări
- Fem 3202-1 IntroductionDocument29 paginiFem 3202-1 IntroductionRon ChongÎncă nu există evaluări
- Kovach 1987Document10 paginiKovach 1987Quyen ta thi nhaÎncă nu există evaluări
- Teardrop by Lauren KateDocument47 paginiTeardrop by Lauren KateRandom House Teens88% (16)
- Neonatal Resuscitation: Dr. (Col) C.G.Wilson Professor& H.O.D (Paed)Document38 paginiNeonatal Resuscitation: Dr. (Col) C.G.Wilson Professor& H.O.D (Paed)shaharuddin_yahayaÎncă nu există evaluări