Documente Academic
Documente Profesional
Documente Cultură
Jama Maclaren 2020 VP 200024
Încărcat de
Yeyen amaliahTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Jama Maclaren 2020 VP 200024
Încărcat de
Yeyen amaliahDrepturi de autor:
Formate disponibile
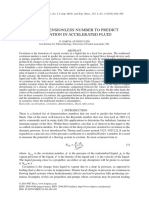
Opinion
Preparing for the Most Critically Ill Patients With COVID-19
VIEWPOINT
The Potential Role of Extracorporeal Membrane Oxygenation
Graeme MacLaren, The novel coronavirus has now infected tens of thou- greater. To address this, prompt mobilization of exist-
MSc sands of people in China and has spread rapidly around ing registries and clinical research groups should help fa-
Cardiothoracic the globe. 1 The World Health Organization (WHO) cilitate the systematic collection of data. For example,
Intensive Care Unit,
has declared the disease, coronavirus disease 2019 the Extracorporeal Life Support Organization (ELSO)
National University
Health System, (COVID-19), a Public Health Emergency of International Registry is being adapted to acquire new information
Singapore. Concern and released interim guidelines on patient about COVID-19 and prospective observational studies
management.2 Early reports that emerged from Wuhan, are under way.
Dale Fisher, MBBS the epicenter of the outbreak, demonstrated that the ECMO does not provide direct support for organs
Division of Infectious
clinical manifestations of infection were fever, cough, other than the lungs or heart beyond increasing
Diseases, University
Medicine Cluster, and dyspnea, with radiological evidence of viral systemic oxygen delivery and mitigating ventilator-
National University pneumonia.3,4 Approximately 15% to 30% of these pa- induced lung injury. A substantial proportion of criti-
Health Systems, tients developed acute respiratory distress syndrome cally ill patients with COVID-19 appear to have devel-
Singapore; and
Department of (ARDS). The WHO interim guidelines made general rec- oped cardiac arrhythmias or shock,3 but it is unknown
Medicine, Yong Loo Lin ommendations for treatment of ARDS in this setting, in- how many have or will develop refractory multiorgan
School of Medicine, cluding that consideration be given to referring pa- failure, for which ECMO may be of more limited use. To
National University of
tients with refractory hypoxemia to expert centers postulate about the potential benefit of ECMO in this
Singapore, Singapore.
capable of providing extracorporeal membrane oxygen- infection, more data on the mechanism of death and
Daniel Brodie, MD ation (ECMO).2 disease are required. The virus may cause death
Division of Pulmonary, ECMO is a form of modified cardiopulmonary by- through progressive hypoxic respiratory failure, septic
Allergy and Critical Care pass in which venous blood is removed from the body shock, refractory multiorgan failure, or by precipitating
Medicine, Columbia
and pumped through an artificial membrane lung in pa- exacerbation of comorbid diseases such as ischemic
University College of
Physicians and tients who have refractory respiratory or cardiac failure.5 heart disease or cardiac failure, but the relative propor-
Surgeons/New Oxygen is added, carbon dioxide is removed, and blood tions of these diseases in large cohorts of patients with
York-Presbyterian is returned to the patient, either via another vein to pro- COVID-19 infection are unknown.
Hospital, New York;
and Center for Acute vide respiratory support or a major artery to provide cir- The global spread of COVID-19, although the num-
Respiratory Failure, culatory support. ECMO is a resource-intensive, highly ber of cases outside of China remains small, will likely
New York-Presbyterian specialized, and expensive form of life support with the occur via many dispersed epicenters where local trans-
Hospital, New York.
mission has become established. If
these epicenters occur in sophisticated
ECMO is not a therapy to be rushed health care systems with preexisting
ECMO programs, this will provide
to the frontline when all resources vital information about the utility of
are stretched in a pandemic. ECMO and help anticipate global de-
mand. Should the initial experience be
potential for significant complications, in particular hem- encouraging, it is likely that non-ECMO centers will
orrhage and nosocomial infection. Recent evidence sug- refer early to ECMO centers in anticipation of impend-
gests that use of ECMO in the most severe cases of ARDS ing clinical deterioration. This will disproportionately
is associated with reduced mortality.6 There is some evi- affect hospitals with ECMO programs, even when
dence that outcomes from ECMO are better in higher- ECMO is not required.
volume centers.7 Furthermore, with the apparent contagiousness
The role of ECMO in the management of COVID-19 of this virus and the relatively high numbers of
is unclear at this point. It has been used in some pa- patients who require intensive care, this may prove
tients with COVID-19 in China but detailed information very resource-consumptive. Countries will need to
is unavailable.3 ECMO may have a role in the manage- pay specific attention to the considerable investment
Corresponding ment of some patients with COVID-19 who have refrac- needed to provide ECMO during this outbreak. Judg-
Author: Graeme tory hypoxemic respiratory failure.6 However, much ment will be needed to decide when ECMO may be
MacLaren, MSc, about the virus is unknown, including the natural his- worthwhile and when it may not, understanding that
Cardiothoracic
Intensive Care Unit,
tory, incidence of late complications, viral persistence, the risk-to-benefit ratio of performing ECMO in these
National University or the prognoses in different subsets of patients. This un- circumstances is dynamic and dependent on many
Health System, 5 Lower certainty might be compared to the emergence of in- factors. If the mechanism of death in COVID-19 ulti-
Kent Ridge Rd,
fluenza A(H1N1) in 2009, when it was initially unclear mately includes a substantial number of patients with
Singapore 119074
(gmaclaren@iinet.net. what the role of ECMO should be.8 However, the de- septic shock or refractory multiorgan failure, then the
au). gree of uncertainty surrounding COVID-19 is much shift away from ECMO is likely to occur earlier because
jama.com (Reprinted) JAMA April 7, 2020 Volume 323, Number 13 1245
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 05/10/2020
Opinion Viewpoint
the most severely ill patients in this cohort would be less likely to provide ECMO to be overwhelmed with critically ill patients unless
benefit. The higher the all-cause mortality, the less relevant interhospital transfers are centrally coordinated.
ECMO becomes. With the WHO recommendation for ECMO in place and the tro-
Regardless, ECMO is clearly a finite resource. In a large out- pism of the COVID-19 virus for severe respiratory illness, the num-
break, additional limitations to providing ECMO may include a lack ber of cases in which ECMO is used may increase over the course of
of ECMO consoles or disposable equipment, suitably trained staff, this outbreak. However, there may come a tipping point. Should the
or isolation rooms with the requisite infrastructure. Many materials case volume in any given region increase beyond the ability to pro-
necessary to make ECMO circuitry are manufactured in China and vide routine care, any earlier increase in ECMO use may give way,
it is conceivable that the outbreak may disrupt supply chains. with utilization later decreasing in proportion to the overwhelming
A number of different models of ECMO service provision demands on the system as a whole.
exist worldwide, ranging from a relative lack of regulation and Support with ECMO is for the most critically ill patients in
centralization—with many hospitals having ECMO capability but regions with the extensive resources required to provide this
often with very low case volumes (eg, in the US or Japan)—through therapy. ECMO is not a therapy to be rushed to the frontline when
to regional or national coordination of ECMO referral centers with all resources are stretched in a pandemic. In less well-resourced
dedicated interhospital retrieval teams (eg, New Zealand, Australia, countries, many more lives will be saved by ensuring oxygen and
Singapore, Qatar, the United Kingdom, or Sweden). In response to pulse oximetry are widely available. Mitigation efforts to slow the
influenza A(H1N1) in 2009, some countries such as Italy adopted outbreak are critical so that health care systems are not over-
the latter model and it is possible that COVID-19 could be ad- whelmed and all patients receive the correct management,
dressed similarly. The advantages of such an approach include stan- whether simply confirmation of the diagnosis and appropriate
dardization of indications, management, data collection, and quarantine, oxygen therapy alone, mechanical ventilation or, for
containment.5,7 The disadvantage is the potential for hospitals that those most likely to benefit, ECMO.
ARTICLE INFORMATION www.who.int/publications-detail/clinical- 6. Goligher EC, Tomlinson G, Hajage D, et al.
Published Online: February 19, 2020. management-of-severe-acute-respiratory- Extracorporeal membrane oxygenation for severe
doi:10.1001/jama.2020.2342 infection-when-novel-coronavirus-(ncov)- acute respiratory distress syndrome and posterior
infection-is-suspected probability of mortality benefit in a post hoc
Conflict of Interest Disclosures: Dr Brodie bayesian analysis of a randomized clinical trial. JAMA.
reported receiving grants from Alung Technologies, 3. Wang D, Hu B, Hu C, et al. Clinical characteristics
of 138 hospitalized patients with 2019 novel 2018;320(21):2251-2259. doi:10.1001/jama.2018.
serving on the medical advisory board for Alung 14276
Technologies, Xenios, Breethe, Baxter, and coronavirus-infected pneumonia in Wuhan, China.
Hemovent. No other disclosures were reported. JAMA. Published online February 7, 2020. doi:10. 7. Barbaro RP, Odetola FO, Kidwell KM, et al.
1001/jama.2020.1585 Association of hospital-level volume of
REFERENCES 4. Chen N, Zhou M, Dong X, et al. Epidemiological extracorporeal membrane oxygenation cases and
and clinical characteristics of 99 cases of 2019 mortality. Analysis of the extracorporeal life support
1. Paules CI, Marston HD, Fauci AS. Coronavirus organization registry. Am J Respir Crit Care Med.
infections—more than just the common cold. JAMA. novel coronavirus pneumonia in Wuhan, China:
a descriptive study. Lancet. Published online January 2015;191(8):894-901. doi:10.1164/rccm.201409-
2020. Published online January 23, 2020. doi:10. 1634OC
1001/jama.2020.0757 30, 2020. doi:10.1016/S0140-6736(20)30211-7
5. Brodie D, Slutsky AS, Combes A. Extracorporeal 8. White DB, Angus DC. Preparing for the sickest
2. World Health Organization. Clinical management patients with 2009 influenza A(H1N1). JAMA.
of severe acute respiratory infection when life support for adults with respiratory failure and
related indications: a review. JAMA. 2019;322(6): 2009;302(17):1905-1906. doi:10.1001/jama.2009.
novel coronavirus (2019-nCoV) infection is 1539
suspected—interim guidance. Published January 557-568. doi:10.1001/jama.2019.9302
28, 2020. Accessed February 11, 2020. https://
1246 JAMA April 7, 2020 Volume 323, Number 13 (Reprinted) jama.com
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 05/10/2020
S-ar putea să vă placă și
- AnnalsATS 202003-233PSDocument4 paginiAnnalsATS 202003-233PSambitiousamit1Încă nu există evaluări
- 1 s2.0 S0899707122000298 MainDocument12 pagini1 s2.0 S0899707122000298 Mainrivai anwarÎncă nu există evaluări
- Myocarditis Following COVID-19 VaccineDocument19 paginiMyocarditis Following COVID-19 VaccineVirginia Hernandez100% (1)
- BMJ 2021 065871.fullDocument24 paginiBMJ 2021 065871.fullEfen YtÎncă nu există evaluări
- ELSO COVD MATV66N7 - Text - Issueproof 6-15-20Document15 paginiELSO COVD MATV66N7 - Text - Issueproof 6-15-20ghg sddÎncă nu există evaluări
- Impact of COVID-19 On People With Cystic FibrosisDocument2 paginiImpact of COVID-19 On People With Cystic FibrosisSherry SaidÎncă nu există evaluări
- COVID ECMO Resource PlanningDocument5 paginiCOVID ECMO Resource PlanningTing Churn WongÎncă nu există evaluări
- Pi Is 0025619620311873Document5 paginiPi Is 0025619620311873Achmad RyandaÎncă nu există evaluări
- Diagnosis ParapnemoniaDocument7 paginiDiagnosis ParapnemoniaLam NandaÎncă nu există evaluări
- Coagulop CovidDocument11 paginiCoagulop CovidbacchiocchipaoloÎncă nu există evaluări
- Comment: Lancet Infect Dis 2020Document2 paginiComment: Lancet Infect Dis 2020kayegi8666Încă nu există evaluări
- Manejo de Neumonia en Pacientes CriticosDocument24 paginiManejo de Neumonia en Pacientes CriticosMauricio Martinez HernandezÎncă nu există evaluări
- Covid 10Document14 paginiCovid 10jenifer paathÎncă nu există evaluări
- ASE Statement On Point-of-Care Ultrasound During The 2019 Novel Coronavirus PandemicDocument4 paginiASE Statement On Point-of-Care Ultrasound During The 2019 Novel Coronavirus PandemicTuan HaiÎncă nu există evaluări
- Management of Pneumonia in Critically Ill Patients: Catia Cillóniz, Antoni Torres, Michael S NiedermanDocument24 paginiManagement of Pneumonia in Critically Ill Patients: Catia Cillóniz, Antoni Torres, Michael S NiedermanMarvin Josue Bustamante GutierrezÎncă nu există evaluări
- FullDocument12 paginiFulljuan carlosÎncă nu există evaluări
- Ecmo 2017Document19 paginiEcmo 2017Josefina Daza SantamaríaÎncă nu există evaluări
- Mesenchymal Stromal Cell Therapy For Coronavirus Disease 2019 - Which? When? and How Much?Document14 paginiMesenchymal Stromal Cell Therapy For Coronavirus Disease 2019 - Which? When? and How Much?diana.alyÎncă nu există evaluări
- Echocardiography in Pandemic Front Line Perspect - 2020 - Journal of The AmericDocument7 paginiEchocardiography in Pandemic Front Line Perspect - 2020 - Journal of The AmericANESTEGYOÎncă nu există evaluări
- Management of Severe Community-Acquired Pneumonia of Children in Developing and Developed CountriesDocument8 paginiManagement of Severe Community-Acquired Pneumonia of Children in Developing and Developed CountriesEry RiadyÎncă nu există evaluări
- Viewpoint: Dennis Mcgonagle, James S O'Donnell, Kassem Sharif, Paul Emery, Charles BridgewoodDocument9 paginiViewpoint: Dennis Mcgonagle, James S O'Donnell, Kassem Sharif, Paul Emery, Charles BridgewoodMonicafajrinÎncă nu există evaluări
- 1 s2.0 S003962571630090X MainDocument14 pagini1 s2.0 S003962571630090X MainBenjamin NgÎncă nu există evaluări
- Covid Asociado A CoagulopatiaDocument2 paginiCovid Asociado A CoagulopatiaNahui IcatlÎncă nu există evaluări
- Guidelines Extracorporeal Membrane Oxygenation For COVID-19Document11 paginiGuidelines Extracorporeal Membrane Oxygenation For COVID-19bacharelado2010Încă nu există evaluări
- Review: Key MessagesDocument12 paginiReview: Key MessagesLuis Fernando PantojaÎncă nu există evaluări
- Hospital Management of Community-AcquiredDocument5 paginiHospital Management of Community-AcquiredJaerom BernadasÎncă nu există evaluări
- Mesenchymal Stem Cells and Management of COVID-19 PneumoniaDocument3 paginiMesenchymal Stem Cells and Management of COVID-19 Pneumoniadiana.alyÎncă nu există evaluări
- Cryptogenic Organizing PneumoniaDocument12 paginiCryptogenic Organizing Pneumoniavalentina peñaÎncă nu există evaluări
- Nac in The Clinic 2022Document18 paginiNac in The Clinic 2022Nathalie Rodriguez GuamangaÎncă nu există evaluări
- Mediastinal Lymphadenopathy May Predict 30 Day Mortality in PatientsDocument7 paginiMediastinal Lymphadenopathy May Predict 30 Day Mortality in PatientsCess Abad AgcongÎncă nu există evaluări
- Organising PneumoniaDocument12 paginiOrganising PneumoniaA. RaufÎncă nu există evaluări
- 15-Peran Platelet Pada Penyakit Jantung - CAPDocument20 pagini15-Peran Platelet Pada Penyakit Jantung - CAPsukiyantoÎncă nu există evaluări
- 30794136: Aspiration Pneumonia in Older AdultsDocument7 pagini30794136: Aspiration Pneumonia in Older AdultsNilson Morales CordobaÎncă nu există evaluări
- PIIS2213260020302678Document9 paginiPIIS2213260020302678kayegi8666Încă nu există evaluări
- A Clinic Blueprint For Post-Coronavirus Disease 2019 RECOVERY Learning From The Past, Looking To The FutureDocument11 paginiA Clinic Blueprint For Post-Coronavirus Disease 2019 RECOVERY Learning From The Past, Looking To The FutureCARLA CRISTINA DE ARAUJOÎncă nu există evaluări
- Gopalakrishnan 2020Document8 paginiGopalakrishnan 2020jq4rhbh2pzÎncă nu există evaluări
- Congenital Heart Disease in The Era of COVID 19 Pandemic: Raffaele Giordano Massimiliano CantinottiDocument3 paginiCongenital Heart Disease in The Era of COVID 19 Pandemic: Raffaele Giordano Massimiliano CantinottiOkto Sofyan HasanÎncă nu există evaluări
- Cryptogenic Organizing Pneumonia: Review ArticleDocument12 paginiCryptogenic Organizing Pneumonia: Review ArticleMatías Jesús Flamm ZamoranoÎncă nu există evaluări
- 1 s2.0 S0012369220342872 MainDocument12 pagini1 s2.0 S0012369220342872 Mainganda gandaÎncă nu există evaluări
- HCQ Study JamaDocument7 paginiHCQ Study Jamathe kingfishÎncă nu există evaluări
- Community-Acquired Pneumonia in Adults: MedicineDocument13 paginiCommunity-Acquired Pneumonia in Adults: MedicineAntonio Cabrera OjedaÎncă nu există evaluări
- George - Acompanhamento pós-COVIDDocument8 paginiGeorge - Acompanhamento pós-COVIDMichelle TabletÎncă nu există evaluări
- Community Acquired PneumoniaDocument17 paginiCommunity Acquired PneumoniaDaniel Puentes SánchezÎncă nu există evaluări
- Jeaa 072Document7 paginiJeaa 072Hanna KrisÎncă nu există evaluări
- (IJCST-V10I5P29) :mrs R. Jhansi Rani, B. Karunakar ReddyDocument7 pagini(IJCST-V10I5P29) :mrs R. Jhansi Rani, B. Karunakar ReddyEighthSenseGroupÎncă nu există evaluări
- Jurnal Ipd 10Document8 paginiJurnal Ipd 10indra mendilaÎncă nu există evaluări
- Hospital PneumoniaDocument15 paginiHospital Pneumoniarivai anwarÎncă nu există evaluări
- Internal Medicine Journal - 2021 - Chang - Consensus guidelines for the diagnosis and management of cryptococcosis and rareDocument25 paginiInternal Medicine Journal - 2021 - Chang - Consensus guidelines for the diagnosis and management of cryptococcosis and rareumayamajidÎncă nu există evaluări
- Early Rehabilitation For Critically Ill Patients.98018 PDFDocument10 paginiEarly Rehabilitation For Critically Ill Patients.98018 PDFCarolina MancipeÎncă nu există evaluări
- December 2020 - Volume 7 - Article 614569Document11 paginiDecember 2020 - Volume 7 - Article 614569elza pratiwiÎncă nu există evaluări
- Resuscitation: European Resuscitation Council COVID-19 Guidelines ExecutiveDocument11 paginiResuscitation: European Resuscitation Council COVID-19 Guidelines ExecutiveRicardo BarreraÎncă nu există evaluări
- Radiologic Diagnosis of Patients With COVID-19Document19 paginiRadiologic Diagnosis of Patients With COVID-19Muhammad ImamHanafiÎncă nu există evaluări
- Severe Covid-19: Clinical PracticeDocument10 paginiSevere Covid-19: Clinical PracticejoelÎncă nu există evaluări
- 6MINUTEWALKTESTABERTODocument5 pagini6MINUTEWALKTESTABERTOpv7j8j6q5rÎncă nu există evaluări
- Reabilitação Após Doença Crítica de CovidDocument5 paginiReabilitação Após Doença Crítica de CovidCristina BoaventuraÎncă nu există evaluări
- (Methods in Molecular Medicine) Andrew J. Pollard, Martin C.J. Maiden - Meningococcal Disease (2001, Humana Press)Document662 pagini(Methods in Molecular Medicine) Andrew J. Pollard, Martin C.J. Maiden - Meningococcal Disease (2001, Humana Press)gnkgbjkgjkÎncă nu există evaluări
- 2021 Lancet Community-Acquired PneumoniaDocument14 pagini2021 Lancet Community-Acquired PneumoniaCarlos Del Valle JaureguiÎncă nu există evaluări
- De Pascale 2012Document9 paginiDe Pascale 2012HellcroZÎncă nu există evaluări
- Covid Long The LancetDocument2 paginiCovid Long The LancetAlexandra IonițăÎncă nu există evaluări
- Gas Pipeline Hydraulics: E. Shashi MenonDocument13 paginiGas Pipeline Hydraulics: E. Shashi Menonmostafa shahrabiÎncă nu există evaluări
- UAE Government Approved Laboratories Dubai 24112020 Tcm8 161089Document1 paginăUAE Government Approved Laboratories Dubai 24112020 Tcm8 161089Mohammed IqbalÎncă nu există evaluări
- (Paperhub - Ir) 10.1002 9781119083948.ch5Document140 pagini(Paperhub - Ir) 10.1002 9781119083948.ch5mostafa shahrabiÎncă nu există evaluări
- Example Letter To Send To EmbassyDocument2 paginiExample Letter To Send To EmbassyEgi Defiska MulyaÎncă nu există evaluări
- App 6Document2 paginiApp 6mostafa shahrabiÎncă nu există evaluări
- 51 Successful Answers For Visa InterviewDocument4 pagini51 Successful Answers For Visa Interviewmostafa shahrabiÎncă nu există evaluări
- Effect of Time On Pipe RoughnessDocument11 paginiEffect of Time On Pipe Roughnessmostafa shahrabiÎncă nu există evaluări
- A Notice: EZ Setup EZ SetupDocument1 paginăA Notice: EZ Setup EZ SetupTheomas AbdiÎncă nu există evaluări
- Effect of Time On Pipe RoughnessDocument11 paginiEffect of Time On Pipe Roughnessmostafa shahrabiÎncă nu există evaluări
- New Dimensionless Number To Predict Cavitation in Accelerated FluidDocument9 paginiNew Dimensionless Number To Predict Cavitation in Accelerated Fluidmostafa shahrabiÎncă nu există evaluări
- Watson IEC 1943Document9 paginiWatson IEC 1943mostafa shahrabiÎncă nu există evaluări
- Computational Compliance Criteria in Water Hammer Modelling: E3S Web of Conferences September 2017Document9 paginiComputational Compliance Criteria in Water Hammer Modelling: E3S Web of Conferences September 2017mostafa shahrabiÎncă nu există evaluări
- Effect of Time On Pipe RoughnessDocument11 paginiEffect of Time On Pipe Roughnessmostafa shahrabiÎncă nu există evaluări
- Visa Interview Questions: Personal InfoDocument5 paginiVisa Interview Questions: Personal Infomostafa shahrabiÎncă nu există evaluări
- New Dimensionless Number To Predict Cavitation in Accelerated FluidDocument9 paginiNew Dimensionless Number To Predict Cavitation in Accelerated Fluidmostafa shahrabiÎncă nu există evaluări
- Author Manuscript: Reference Correlation For The Viscosity of Ammonia From The Triple Point To 725 K and Up To 50 Mpaa)Document27 paginiAuthor Manuscript: Reference Correlation For The Viscosity of Ammonia From The Triple Point To 725 K and Up To 50 Mpaa)mostafa shahrabiÎncă nu există evaluări
- Orifice Gas Flow Chart PDFDocument1 paginăOrifice Gas Flow Chart PDFmostafa shahrabiÎncă nu există evaluări
- Viscosity Measurements of Ammonia, R32, and R134a. Vapor Buoyancy and Radial Acceleration in Capillary ViscometersDocument34 paginiViscosity Measurements of Ammonia, R32, and R134a. Vapor Buoyancy and Radial Acceleration in Capillary Viscometersmostafa shahrabiÎncă nu există evaluări
- Compressor Strategy Overview: AA3 and AA4 PlansDocument43 paginiCompressor Strategy Overview: AA3 and AA4 Plansmostafa shahrabiÎncă nu există evaluări
- A022003 Aci PDFDocument12 paginiA022003 Aci PDFmostafa shahrabiÎncă nu există evaluări
- Adibatic Bulk ModulusDocument2 paginiAdibatic Bulk ModulusTechie HarryÎncă nu există evaluări
- SN19.4-Matthews-Lessons Learned Express Pipeline ProjectDocument12 paginiSN19.4-Matthews-Lessons Learned Express Pipeline Projectmostafa shahrabiÎncă nu există evaluări
- Eng BD Fta1181Document14 paginiEng BD Fta1181mostafa shahrabiÎncă nu există evaluări
- Solar: MCL CDocument37 paginiSolar: MCL Cmostafa shahrabiÎncă nu există evaluări
- HidratosDocument6 paginiHidratosLuis Joel Ramos RamosÎncă nu există evaluări
- Acs Iecr 9b03512Document26 paginiAcs Iecr 9b03512mostafa shahrabiÎncă nu există evaluări
- Water Hammer EquationsDocument11 paginiWater Hammer Equationsmostafa shahrabiÎncă nu există evaluări
- 10 1 1 678 1140 PDFDocument5 pagini10 1 1 678 1140 PDFmostafa shahrabiÎncă nu există evaluări
- Gas Hydrate Formation and Dissociation Numerical Modelling With Nitrogen and Carbon DioxideDocument30 paginiGas Hydrate Formation and Dissociation Numerical Modelling With Nitrogen and Carbon Dioxidemostafa shahrabiÎncă nu există evaluări
- Acs Iecr 9b03512Document26 paginiAcs Iecr 9b03512mostafa shahrabiÎncă nu există evaluări
- Rachel Pawa ResumeDocument2 paginiRachel Pawa Resumeapi-283084320Încă nu există evaluări
- Anemia Effect On Burn Wound HealingDocument5 paginiAnemia Effect On Burn Wound HealingAgung Widya PramanaÎncă nu există evaluări
- Team Work and Nurse-Physician RelationshipDocument22 paginiTeam Work and Nurse-Physician Relationshipsamer_esh927Încă nu există evaluări
- ICUC 22 Flow Chart INTENSIVE CARE UNIT RSUDKK RevDocument36 paginiICUC 22 Flow Chart INTENSIVE CARE UNIT RSUDKK RevyudhaÎncă nu există evaluări
- The NHSN Standardized Infection Ratio (Sir)Document49 paginiThe NHSN Standardized Infection Ratio (Sir)dlokus21Încă nu există evaluări
- A Clinical Pathway To Standardize Care of Children With Delirium in Pediatric Inpatient Settings-2019Document10 paginiA Clinical Pathway To Standardize Care of Children With Delirium in Pediatric Inpatient Settings-2019Juan ParedesÎncă nu există evaluări
- Published PDF 2390 6 AssessingtheLevelofStressandAnxietyinFamilyMembersofPatientsHos PitalizedintheSpecialCareUnitsDocument6 paginiPublished PDF 2390 6 AssessingtheLevelofStressandAnxietyinFamilyMembersofPatientsHos PitalizedintheSpecialCareUnitsYiyiz HertikaÎncă nu există evaluări
- Mediclaim Policy - Buy Group Health Insurance Online - Future GeneraliDocument39 paginiMediclaim Policy - Buy Group Health Insurance Online - Future GeneraliRizwan KhanÎncă nu există evaluări
- The POWER of WHEY & MCT For Critically Ill PatientsDocument46 paginiThe POWER of WHEY & MCT For Critically Ill PatientsBayu Residewanto PutroÎncă nu există evaluări
- Detecting and Correcting Patient-Ventilator AsynchroniesDocument8 paginiDetecting and Correcting Patient-Ventilator AsynchroniesPhilip PoerworahjonoÎncă nu există evaluări
- A Model To Predict Short-Term Death or Readmission After Intensive Care Unit DischargeDocument10 paginiA Model To Predict Short-Term Death or Readmission After Intensive Care Unit DischargeInnani Wildania HusnaÎncă nu există evaluări
- Policy Clause New India Mediclaim Policy Wef 1st April 2021Document33 paginiPolicy Clause New India Mediclaim Policy Wef 1st April 2021Chirag SataniÎncă nu există evaluări
- Hospital Introduction and Departements PDFDocument37 paginiHospital Introduction and Departements PDFHenki Tirta herianto100% (1)
- Care bundles in intensive care medicineDocument4 paginiCare bundles in intensive care medicineYashoda PereraÎncă nu există evaluări
- Critical Appraisal, Arif Eko Wibowo (Neurologi)Document7 paginiCritical Appraisal, Arif Eko Wibowo (Neurologi)arif 2006Încă nu există evaluări
- President Kaguta Museveni's Speech On Covid-19 As of 18 June 2021Document26 paginiPresident Kaguta Museveni's Speech On Covid-19 As of 18 June 2021The Campus TimesÎncă nu există evaluări
- Buku Saku Anestesi 2020Document9 paginiBuku Saku Anestesi 2020Angky Satya KusumaÎncă nu există evaluări
- 02 DR Bala Ramachandran - HVAC in Infection ControlDocument48 pagini02 DR Bala Ramachandran - HVAC in Infection ControlVignesh BalajiÎncă nu există evaluări
- Organizing Nursing Services and Patient Care: Case MethodDocument23 paginiOrganizing Nursing Services and Patient Care: Case Methodmerin sunilÎncă nu există evaluări
- Low Cardiac OutputDocument23 paginiLow Cardiac OutputMohamed ElgayarÎncă nu există evaluări
- Pediatric Services Operational Policy-1 PDFDocument132 paginiPediatric Services Operational Policy-1 PDFdmallozziÎncă nu există evaluări
- PhysioEx Exercise 10 Activity 4Document3 paginiPhysioEx Exercise 10 Activity 4Isabel PalaciosÎncă nu există evaluări
- "Wireless Pulse Monitoring System": "BEC 608: Design Project Phase - II"Document19 pagini"Wireless Pulse Monitoring System": "BEC 608: Design Project Phase - II"Salman RayeenÎncă nu există evaluări
- DrNB CRITICAL CARE MEDICINE Paper3Document4 paginiDrNB CRITICAL CARE MEDICINE Paper3aparnapingali0Încă nu există evaluări
- Patterns of Creactive Protein Ratio Response To Antibiotics in Pediatric Sepsis A Prospective Cohort StudyDocument6 paginiPatterns of Creactive Protein Ratio Response To Antibiotics in Pediatric Sepsis A Prospective Cohort StudynicloverÎncă nu există evaluări
- EVMS Critical Care COVID-19 ProtocolDocument23 paginiEVMS Critical Care COVID-19 ProtocoldarwinÎncă nu există evaluări
- Study Title: Protocol Number: 15HC47 Protocol Version: Version 4.0 Short Title or Acronym: The DEPICT StudyDocument50 paginiStudy Title: Protocol Number: 15HC47 Protocol Version: Version 4.0 Short Title or Acronym: The DEPICT StudyThe asdwÎncă nu există evaluări
- Test Bank For Priorities in Critical Care Nursing 8th Edition by UrdenDocument35 paginiTest Bank For Priorities in Critical Care Nursing 8th Edition by Urdenwryneckschist3ktyhl100% (38)
- Kingston Hospital Blue Book 2019Document207 paginiKingston Hospital Blue Book 2019Chris Jardine LiÎncă nu există evaluări
- Glasgow Coma Scale AssesmentDocument18 paginiGlasgow Coma Scale AssesmentnerskittaholisticcareÎncă nu există evaluări