Documente Academic
Documente Profesional
Documente Cultură
Congestive Heart Failure and Pulmonary Edema: Nursing Diagnoses Interventions
Încărcat de
Lovely CacapitDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Congestive Heart Failure and Pulmonary Edema: Nursing Diagnoses Interventions
Încărcat de
Lovely CacapitDrepturi de autor:
Formate disponibile
PATHOPHYSIOLOGY:
SIGN AND SYMPTOMS
-heart failure may present accurately as a result of CONGESTIVE HEART FAILURE and
myocardial ischemia secondary to myocardial infarction.-the PULMONARY EDEMA Fatigue
cardiac muscle is weakened that is why CO is decreased. SOB
The decreasing cardiac output then triggers and increased in Distended neck veins
systemic vascular resistance and afterload and fluids begin Weakness
to shoot back through the pulmonary veins and fills the lungs.
Dizziness
In CHF with acute pulmonary edema this will be the terminal
Syncope
event if the systemic vascular resistance is not promptly
Anxiety
reversed.
Decrease exercise tolerance
Interventions
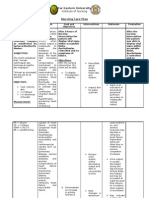
Continually assess for signs and symptoms of precipitating heart failure. Nursing Diagnoses
Monitor for signs of bleeding due to anticoagulation and blood thinning Decreased Cardiac Output
therapies. Risk for ineffective coping
Try to find underlying cause and treat the cause. PC: Pulmonary Embolism
Monitor ST segment continuously to determine changes in myocardial tissue Risk for infection
perfusion. Ineffective tissue perfusion
Assess that urine output hourly, alert physician if less than 30 ml/hr. Acute pain
Maintain the patient in the semi-fowlers position to lessen the work of Impaired gas exchange
breathing and facilitate venous return. Impaired verbal communication
Continuously monitor O2 and assess vital signs.
(Ackley & Ladwig, 2011)
(Ignatavicius &Workman, 2010; Urden, Stacy, & Lough, 2008)
Risk Factors Medications Treatments
Coronary artery disease Loop diuretics. The first priority of treatment is airway management. This is judged by the severity of the
Male gender Vasodilators- should be used to lower the systemic presenting symptoms. Could include supplemental oxygen via nasal cannula or mask,
History of hypertension,diabetes mellitus, vascular resistance and therefore decrease the noninvasive ventilation or in this patient’s case endotracheal intubation.
valvular disease, and myocardial infarction. cardiac afterload. Urinary catheter should be placed to closely monitor renal function and allow patient to
Alcohol, cardiac surgery, kidney conditions, Beta-blockers should be used to decrease the rest.
pericarditis, myocarditis, viruses. preload and afterload placed on the heart. A 12-lead ECG to assess for cardiac abnormalities.
Congenital heart defects, sleep apnea, Anticoagulation therapy drugs IV access to provide prompt medication administration.
ACE inhibitor regimen should be started because of Frequent vital sign assessments to monitor for a decline in cardiac function.
(Ignatavicius &Workman, 2010; Urden et al., 2008) their effect on slowing even reversing left ventricular
remodeling over time. (Ignatavicius &Workman, 2010; Urden et al., 2008)
.
(Urden et al., 2008)
S-ar putea să vă placă și
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtDe la EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtEvaluare: 5 din 5 stele5/5 (1)
- B. Create Your Concept Map of The Disorder. Use A Separate Paper For This. Use Short Coupon Bond and Draw Your Concept Map Using This FormatDocument5 paginiB. Create Your Concept Map of The Disorder. Use A Separate Paper For This. Use Short Coupon Bond and Draw Your Concept Map Using This FormatPatricia Jean FaeldoneaÎncă nu există evaluări
- Acute Anterior Wall Myocardial InfarctionDocument2 paginiAcute Anterior Wall Myocardial InfarctionMelinda Cariño BallonÎncă nu există evaluări
- 1 Acute Arterial OcclusionDocument3 pagini1 Acute Arterial Occlusionchristine louise bernardoÎncă nu există evaluări
- Mi PresentationDocument65 paginiMi PresentationJobelyn TunayÎncă nu există evaluări
- Angina PectorisDocument8 paginiAngina PectorisJoanne LagusadÎncă nu există evaluări
- Concept Map For Anterior Myocardial Infarction: I. Introduction and ObjectivesDocument6 paginiConcept Map For Anterior Myocardial Infarction: I. Introduction and ObjectivesLouise GudmalinÎncă nu există evaluări
- Assignment On Nursing Process of Acute Myocardial InfarctionDocument3 paginiAssignment On Nursing Process of Acute Myocardial InfarctionAlexÎncă nu există evaluări
- PY6030 Term 1Document13 paginiPY6030 Term 1AlexaJoiceJumao-AsÎncă nu există evaluări
- MYOCARDIAL INFARCTION EditedDocument27 paginiMYOCARDIAL INFARCTION Editedczars cajayonÎncă nu există evaluări
- 2022 Pharmacology s2t2 HeartfailureDocument6 pagini2022 Pharmacology s2t2 Heartfailurejed larsen capulong gavinoÎncă nu există evaluări
- Acute Manifestations of Neuromuscular DiseaseDocument10 paginiAcute Manifestations of Neuromuscular DiseasetsyrahmaniÎncă nu există evaluări
- Proposal Hubungan NO & TNF - A DGN EF Pada Hipotensi IntradialitikDocument40 paginiProposal Hubungan NO & TNF - A DGN EF Pada Hipotensi IntradialitikJunita Nelly Esther JosephÎncă nu există evaluări
- Cardiac Malformation: Left To Right ShuntsDocument11 paginiCardiac Malformation: Left To Right Shuntsenjel vinluanÎncă nu există evaluări
- Heart Failure Complicating: Acute MyocardialDocument14 paginiHeart Failure Complicating: Acute MyocardialDiannokaIhzaGanungÎncă nu există evaluări
- MI SlidesDocument65 paginiMI SlidesJobelyn TunayÎncă nu există evaluări
- Myocardial Infarction, NursingDocument17 paginiMyocardial Infarction, NursingApril Mae Magos LabradorÎncă nu există evaluări
- Nursing Diagnosis Nursing Intervention Rationale: Prioritized Nursing Problem For Congestive Heart FailureDocument2 paginiNursing Diagnosis Nursing Intervention Rationale: Prioritized Nursing Problem For Congestive Heart FailureMyrshaida IbrahimÎncă nu există evaluări
- InfarctionDocument8 paginiInfarctionnewtihstishÎncă nu există evaluări
- Cardio Dra. Deduyo: Ischemic Heart DiseaseDocument4 paginiCardio Dra. Deduyo: Ischemic Heart DiseaseIm SharaÎncă nu există evaluări
- Mixed BloodDocument17 paginiMixed BloodSlepy chngÎncă nu există evaluări
- Pedia Cardio Lecture AidDocument5 paginiPedia Cardio Lecture AidStephanie Pearl AldaÎncă nu există evaluări
- Multiple Organ Dysfunction SyndromeDocument4 paginiMultiple Organ Dysfunction SyndromeJenny SisonÎncă nu există evaluări
- Institute of Nursing: Far Eastern UniversityDocument3 paginiInstitute of Nursing: Far Eastern UniversityaleccespirituÎncă nu există evaluări
- Jurnal Past, Present, FutureDocument12 paginiJurnal Past, Present, FuturesunallfingerÎncă nu există evaluări
- Example of Nursing Diagnosis Risk For Decreased Cardiac OutputDocument5 paginiExample of Nursing Diagnosis Risk For Decreased Cardiac OutputAndi Faramida HamzahÎncă nu există evaluări
- Cardiovascular System AppendicesDocument2 paginiCardiovascular System AppendicesKim GonzalesÎncă nu există evaluări
- Taponamiento CardiacoDocument9 paginiTaponamiento CardiacoLiz Aliaga KnutzenÎncă nu există evaluări
- Article 05 PDFDocument5 paginiArticle 05 PDFMuhammad PrimanurjaniÎncă nu există evaluări
- Cardiac Exercise TableDocument16 paginiCardiac Exercise TablePreet KaurÎncă nu există evaluări
- OMedEd - Cardiology - CAD PDFDocument2 paginiOMedEd - Cardiology - CAD PDFJohn DoeÎncă nu există evaluări
- Myocardial Infarction Handout 1Document3 paginiMyocardial Infarction Handout 1Alekxandra Erl ManansalaÎncă nu există evaluări
- 1 s2.0 S0749070421000956 MainDocument13 pagini1 s2.0 S0749070421000956 MainEliseu AmaralÎncă nu există evaluări
- Acute Coronary SyndromeDocument27 paginiAcute Coronary SyndromeSahr Anne Pilar B. ParreñoÎncă nu există evaluări
- Notes On SyncopeDocument8 paginiNotes On SyncopeViswa Giri100% (1)
- Penilaian Awal Pasien SyokDocument33 paginiPenilaian Awal Pasien SyokatikaÎncă nu există evaluări
- Litrev Trauma MuskuloskeletalDocument26 paginiLitrev Trauma Muskuloskeletaldedyalkarni08Încă nu există evaluări
- Jurnal 7 - Petsas2014Document8 paginiJurnal 7 - Petsas2014Ayu Novita KartikaningtyasÎncă nu există evaluări
- Peripheral Artery Disease CompendiumDocument14 paginiPeripheral Artery Disease CompendiumTudor DumitrascuÎncă nu există evaluări
- Hematologic Acute or Chronic Problems: ScenarioDocument36 paginiHematologic Acute or Chronic Problems: ScenariobhavanaÎncă nu există evaluări
- Pulmonary Atresi1Document3 paginiPulmonary Atresi1daylcyma444Încă nu există evaluări
- Pulmonary AtresiaDocument3 paginiPulmonary Atresiadaylcyma444Încă nu există evaluări
- A Standardized and Comprehensive Approach To The Management of Cardiogenic Shock 2020Document13 paginiA Standardized and Comprehensive Approach To The Management of Cardiogenic Shock 2020gloriaÎncă nu există evaluări
- CHF & Cardiac ArrestDocument12 paginiCHF & Cardiac ArrestRadhika BirlaÎncă nu există evaluări
- Shock: Rose Ann J. Raquiza-Perante Post Graduate InternDocument53 paginiShock: Rose Ann J. Raquiza-Perante Post Graduate InternRose Ann RaquizaÎncă nu există evaluări
- Cardiovascular Emergencies: Dr. Bobi Prabowo, SP - EMDocument56 paginiCardiovascular Emergencies: Dr. Bobi Prabowo, SP - EMHiz AnÎncă nu există evaluări
- Cardiac EmergencyDocument56 paginiCardiac Emergency21rayhanf100% (1)
- Review: Management of Acute Decompensated Heart FailureDocument9 paginiReview: Management of Acute Decompensated Heart Failureedi_wsÎncă nu există evaluări
- Medurg MidtermDocument4 paginiMedurg Midtermmark OrpillaÎncă nu există evaluări
- 7MB, Ac, 1PCSDocument1 pagină7MB, Ac, 1PCSRicko CiadyÎncă nu există evaluări
- Cardio 3B Ischemic Heart DiseaseDocument6 paginiCardio 3B Ischemic Heart DiseaseAndrassy Twinkle AlineaÎncă nu există evaluări
- Peran Perawat Dalam Penangan Kegawatn Jantung - ERWIN (Autosaved)Document64 paginiPeran Perawat Dalam Penangan Kegawatn Jantung - ERWIN (Autosaved)Adrianus AdrianusÎncă nu există evaluări
- ADHF HFrEFDocument14 paginiADHF HFrEFAnonymous NeRC5JYiSÎncă nu există evaluări
- Clinical Case Ventricular Tachycardia Vet Team Brief 2016Document6 paginiClinical Case Ventricular Tachycardia Vet Team Brief 2016Katherina AdisaputroÎncă nu există evaluări
- Summary C19-20Document15 paginiSummary C19-20EleanorÎncă nu există evaluări
- Anesthesia For Dogs With Myxomatous Mitral Valve DiseaseDocument7 paginiAnesthesia For Dogs With Myxomatous Mitral Valve DiseaseMiguel MuunguiiaÎncă nu există evaluări
- Heart Failure Nursing Care Plans - 15 Nursing Diagnosis - NurseslabsDocument13 paginiHeart Failure Nursing Care Plans - 15 Nursing Diagnosis - NurseslabsJOSHUA DICHOSOÎncă nu există evaluări
- Pulmonary ComplicationsDocument45 paginiPulmonary Complicationskyla arachelleÎncă nu există evaluări
- Discussion: Jose Henao, Raynieri Fernandez, Karla Tejada Arias, and Chu ChaeDocument1 paginăDiscussion: Jose Henao, Raynieri Fernandez, Karla Tejada Arias, and Chu Chaejose henaoÎncă nu există evaluări
- Myocardial InfarctionDocument52 paginiMyocardial InfarctionAmad MirulÎncă nu există evaluări
- 2 NCP Chronic Heart FailureDocument5 pagini2 NCP Chronic Heart FailureLovely CacapitÎncă nu există evaluări
- Pathophysiology DKADocument2 paginiPathophysiology DKALovely CacapitÎncă nu există evaluări
- NCP For Diabetic KetoacidosisDocument2 paginiNCP For Diabetic KetoacidosisLovely Cacapit100% (1)
- Experiment 1 Role of Phosphate BuffersDocument5 paginiExperiment 1 Role of Phosphate BuffersLovely CacapitÎncă nu există evaluări
- Case Study SurgW FinalDocument59 paginiCase Study SurgW FinalLovely CacapitÎncă nu există evaluări
- University of Baguio School of Nursing: Case AnalysisDocument7 paginiUniversity of Baguio School of Nursing: Case AnalysisLovely CacapitÎncă nu există evaluări
- Heart FailureDocument7 paginiHeart FailureLovely CacapitÎncă nu există evaluări
- NCP DiverticulitisDocument6 paginiNCP DiverticulitisLovely Cacapit100% (1)
- Prefixes & Meaning 2medical Terms Definition of TermsDocument4 paginiPrefixes & Meaning 2medical Terms Definition of TermsLovely CacapitÎncă nu există evaluări
- Curriculum Vitae Sample Medical DoctorDocument9 paginiCurriculum Vitae Sample Medical Doctore6zsa5kc100% (1)
- Aortic RegurgitationDocument19 paginiAortic RegurgitationsunilgenextÎncă nu există evaluări
- Cardiogenic Shock Patofisiologi and TreatmentDocument40 paginiCardiogenic Shock Patofisiologi and TreatmentRichi Aditya100% (1)
- In Search of The Holy Grail: How To Ensure A Perfect Progress NoteDocument2 paginiIn Search of The Holy Grail: How To Ensure A Perfect Progress NoteGabrielMatiasDosSantosÎncă nu există evaluări
- Taibah University Interns: Umm Al - Qura University SLE Questions 2 EditionDocument531 paginiTaibah University Interns: Umm Al - Qura University SLE Questions 2 EditionFammo MoiduÎncă nu există evaluări
- Banco de Preguntas Cardio SincDocument37 paginiBanco de Preguntas Cardio SincnoahÎncă nu există evaluări
- Differentiate Between: Defibrillation CardioversionDocument3 paginiDifferentiate Between: Defibrillation CardioversionStephy SojanÎncă nu există evaluări
- Poster HCS EventDocument1 paginăPoster HCS EventChris LlewellynÎncă nu există evaluări
- 23650Document25 pagini23650Ade FeriyatnaÎncă nu există evaluări
- Resuscitation Training 2016 - KKMDocument60 paginiResuscitation Training 2016 - KKMSiti NabilaÎncă nu există evaluări
- (KEL 1) Jurnal IMA (Pak Arif)Document8 pagini(KEL 1) Jurnal IMA (Pak Arif)Nurul HendrianiÎncă nu există evaluări
- Aetiology Heart Diasease in Children May Be Congenital or AcquiredDocument23 paginiAetiology Heart Diasease in Children May Be Congenital or AcquiredkasondaÎncă nu există evaluări
- Cardiac SurgeryDocument110 paginiCardiac SurgeryChristopher McAndrew100% (1)
- Ophthal MD MnoDocument1 paginăOphthal MD Mnoram kumarÎncă nu există evaluări
- Ecg - Basics For The Anesthesiologists: Dr.K.M.LakshmanarajanDocument145 paginiEcg - Basics For The Anesthesiologists: Dr.K.M.LakshmanarajanKM Lakshmana RajanÎncă nu există evaluări
- Drugs Used in The Treatment of Congestive Heart FailureDocument18 paginiDrugs Used in The Treatment of Congestive Heart Failurekarina azlia amandaÎncă nu există evaluări
- Cardio My OpathiesDocument61 paginiCardio My OpathiesIrina Cabac-PogoreviciÎncă nu există evaluări
- Management of Heart Failure With Preserved EjectionFraction A Review PDFDocument13 paginiManagement of Heart Failure With Preserved EjectionFraction A Review PDFGharbi StrongÎncă nu există evaluări
- Guy's Hospital Prognostic Score Allen's Prognostic Score For Stroke PDFDocument2 paginiGuy's Hospital Prognostic Score Allen's Prognostic Score For Stroke PDFChristopher AdhisasmitaÎncă nu există evaluări
- 12-Adult Post Resuscitation Care Algorithm 2021Document1 pagină12-Adult Post Resuscitation Care Algorithm 2021khaledÎncă nu există evaluări
- Ebook Ekg Plain and Simple 4Th Edition Ellis Test Bank Full Chapter PDFDocument30 paginiEbook Ekg Plain and Simple 4Th Edition Ellis Test Bank Full Chapter PDFalexandercampbelldkcnzafgtw100% (9)
- Ecginami 111115073242 Phpapp02Document104 paginiEcginami 111115073242 Phpapp02ginaul100% (1)
- ACLS AHA Guidelines 2006 PosterDocument1 paginăACLS AHA Guidelines 2006 PosterJeane SuyantoÎncă nu există evaluări
- Medical Terminology - Cardiovascular SystemDocument4 paginiMedical Terminology - Cardiovascular SystemDenisse PortillaÎncă nu există evaluări
- Coronary Angiogram Leaflet (Compatibility MoDocument2 paginiCoronary Angiogram Leaflet (Compatibility MoAgnesthesiaÎncă nu există evaluări
- Multiprofessional Critical Care Review Course - 2005Document16 paginiMultiprofessional Critical Care Review Course - 2005asupicuÎncă nu există evaluări
- Congenital Heart DiseaseDocument36 paginiCongenital Heart DiseaseMaria MumtazÎncă nu există evaluări
- Heart BNHADocument13 paginiHeart BNHAX OloGyÎncă nu există evaluări
- Atrial FibrillationDocument21 paginiAtrial FibrillationAndrea LombiÎncă nu există evaluări
- Rate P Wave QRS Comple X PR Interval: ST RDDocument2 paginiRate P Wave QRS Comple X PR Interval: ST RDPat G.Încă nu există evaluări