Documente Academic
Documente Profesional
Documente Cultură
F.01 NEUROLOGIC AND PSYCHIATRIC DISEASES IN PREGNANCY (Dr. Arcellan) 04-10-2019 PDF
Încărcat de
Dasha VeeTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
F.01 NEUROLOGIC AND PSYCHIATRIC DISEASES IN PREGNANCY (Dr. Arcellan) 04-10-2019 PDF
Încărcat de
Dasha VeeDrepturi de autor:
Formate disponibile
OBSTETRICS 2
phenomena such
F.01 NEUROLOGIC AND PSYCHIATRIC DISEASES IN as visual scotoma
PREGNANCY or hallucination
Dr. Arcellana | April 10, 2019
Management:
OUTLINE: o Non-pharmacological – biofeedback techniques,
I. HEADACHE acupuncture and transcranial magnetic stimulation
II. SEIZURE DISORDERS (TMS)
III. CEREBROVASCULAR DISEASE o Pharmacologic – NSAID, Triptans, Amitriptyline,
IV. DEMYELINATING OR DEGENERATIVE DISEASES *Propanolol, *Metorpolol
V. NEUROPATHIES o Β-blockers are contraindicated in pregacy however we
VI. SPINAL CORD INJURY have to weigh the risks versus the benefits
VII. IDIOPATHIC INTRACRANIAL HYPERTENSION
VIII. MATERNAL VENTRICULAR SHUNTS II. SEIZURE DISORDERS
IX. MATERNAL BRAIN DEATH Next most prevalent neurological condition encountered in
X. PSYCHIATRIC DISORDERS IN PREGNANCY pregnant women; 1 in 200 pregnancies
Associated with altered mental development; adversely
NEUROLOGICAL DISORDERS IN PREGNANCY affect other pregnancy outcomes
1. Headache Paroxysmal disorder on the CNS characterized by abnormal
2. Seizure Disorders neuronal discharge with or without loss of consciousness
3. Cerebrovascular Disease Seizure disorder is different from eclampsia. In eclampsia
4. Demyelinating or Degenerative Diseases there should be a pre-eclampsia or hypertension with
5. Neuropathies proteinuria during pregnancy and then that patient develops
6. Spinal Cord Injury seizures, that is eclampsia
7. Idiopathic Intracranial Hypertension When a patient finds out that she is pregnant what does she
8. Maternal Ventricular Shunts usually do with her anti-seizure medications? She stops.
9. Maternal Brain Death When she stops then there could be a recurrence of seizure
disorders. And also, because of the physiologic changes
I. HEADACHE (decreased gastric emptying type, increased glomerular
Most common neurological complaint during filtration rate…) together with intake of antacids (for nausea
pregnancy and vomiting), what do you think happens to the serum
Decrease in prevalence of all headache types during level of anti-convulsants? It decreases, and when the
pregnancy in nulliparas especially during 3rd trimester therapeutic dose is not achieved there is increased
Primary headaches > secondary headaches frequency of seizure activity
Headache is relieved during pregnancy MOST OF THE TIME CAUSES: head trauma, alcohol- and other drug-induced
Severe headache itself could cause hypertension in withdrawals, cerebral infarctions, brain tumors, biochemical
pregnancy abnormalities and AV malformations
Some medications used for headache are teratogenic and Pre-conceptional counseling is important
can cause adverse outcomes Advise intake of Folic acid 1 month prior to conception, if
they have a higher risk then start it 3 months prior to
A. TENSION HEADACHE conception
Most common Goal of monotherapy using the least teratogenic medication
FEATURES: Major pregnancy-related risks: increased seizure
o Muscle tightness rates with attendant mortality risk and fatal
o Mild to moderate pain for hours in the back of the neck malformations
and head Seizure control is the main priority
o No associated neurological disturbances or Increased seizure frequency is seen
nausea The effect of seizure in pregnancy:
o Responds to rest, massage, application of heat or ice, o Increased cesarean section rate
anti-inflammatory meds or mild tranquilizers Patient in active seizure must be
stabilized first
B. MIGRAINE HEADACHE o Increased risk for hypertension and post-partum
Frequently encountered during pregnancy depression
FEATURES:
o Periodic sometimes incapacitating A. FOCAL SEIZURES
o Episodic attacks of severe headache and ANS Originated in one localized brain area an affect a
dysfunction localized area of neurological functions
Prevalence in 1st trimester: 2% Result from trauma, abscess, tumor or perinatal factors
Most have improvement during pregnancy
May increase risk for fetus with limb-reduction defects, FOCAL SEIZURES WITHOUT FOCAL SEIZURES WITH
preeclampsia and other CV morbidities DYSCOGNITIVE FEATURES DYSCOGNITIVE FEATURES
3 TYPES: Start in region of the body and Often preceded by an aura
Migraine Migraine with Chronic migraine progress toward ipsilateral areas – and followed by impaired
without aura aura tonic and then clonic movements awareness manifested by
Common migraine Classic migraine Occurring at least 15 sudden behavioral arrest or
days each month for motionless state
>3 months Involuntary movements
Unilateral Similar symptoms such as picking motions or
throbbing HA, preceded by lip smacking are common
nausea, vomiting, premonitory
photophobia neurological
Transcribers: ESTEPA, LAPEÑA, HIDALGO Page 1 of 9
OBSTETRICS 2
B. GENERALIZED SEIZURES
Involve both brain hemispheres and may be preceded
by an aura before an abrupt loss of consciousness
GENERALIZED TONIC-CLONIC ABSENCE SEIZURES – PETIT
SEIZURES MAL
Loss of consciousness is followed Brief loss of consciousness
by tonic contraction of the muscles without muscle activity
and rigid posturing and then by Immediate recovery of
clonic contractions of all the consciousness and
extremities while the muscles orientation
gradually relax
Some identifiable causes of convulsive disorders in young
adults include head trauma, alcohol- and other drug-induced
withdrawals, cerebral infections, brain tumors, biochemical
abnormalities, and arteriovenous malformations
Pre-conceptional counseling is very important
C. EPILEPSY DURING PREGNANCY
The major pregnancy-related risks to women with epilepsy
are increased seizure rates with attendant mortality risks and
fetal malformations
Seizure control is the main priority and increased seizure
activity during pregnancy.
Increased CS rate, non-proteinuria HPN and labor induction,
postpartum depression
Children with epileptic mothers have a 10% risk of
developing seizure disorder
Untreated epilepsy is not associated with increased
fetal malformation, medications do.
MANAGEMENT IN PREGNANCY
Major goal is seizure prevention
Treatment for nausea and vomiting is provided
Seizure-provoking stimuli are avoided
Medication compliance is emphasized
Breastfeeding – no obvious deleterious effects (of
anticonvulsant medications)
Some anticonvulsants are associated with increased OCP
failures
TERATOGENIC EFFECTS OF COMMON ANTICONVULSANTS A. ISCHEMIC STROKE
The known teratogenic drugs are valproate (embryo-fetal Acute occlusion or embolization of an intracranial blood
risk) vessel causes cerebral ischemia which may result in death of
Higher risk in polydrug treatment over single drug therapy, it brain tissue
is better to find a single drug that would have the least Sudden onset of severe headache, hemiplegia or
teratogenic effect and take it in compliance other neurological deficits or seizures
Evaluation: echocardiography and cranial imaging with CT,
III. CEREBROVASCULAR DISEASES MRI or angiography, serum lipids, antiphospholipid
1. Stroke: ischemic, hemorrhagic antibodies and lupus anticoagulant
2. AV malformations
3. Aneurysms B. HEMORRHAGIC STROKE
Risk factors: hypertensive disorders, GDM, obstetrical
hemorrhage, and CS 1. INTRACEREBRAL HEMORRHAGE
Is pregnancy good for cerebrovascular events? No. Because Bleeding into the brain parenchyma most common is caused
there’s increase risk because the physiologic changes in by spontaneous rupture of small vessels previously damaged
pregnancy affect the coagulation system. Most strokes by chronic hypertension
manifest during labor. Patients are immobile. Advise patients Higher mortality and morbidity rates
to ambulate after 8 hours. Chronic hypertension is uniquely associated with Charcot-
Pregnancy increases the immediate and lifetime risk of both Bouchard aneurysms
ischemic and hemorrhagic stroke Cautions for the importance of proper management for
Major strokes manifest during labor and delivery or in the gestational hypertension
puerperium
Common factor in ischemic and hemorrhagic stroke is 2. SUBARACHNOID HEMORRHAGE
hypertension Incidence is 5.8 per 100,000 pregnancies, half being
postpartum
Bleeds are most likely caused by underlying CV malformation
in an otherwise normal patient
80% secondary to ruptures saccular or “berry” aneurysms
Transcribers: ESTEPA, LAPEÑA, HIDALGO Page 2 of 9
OBSTETRICS 2
Rare during pregnancy GOAL OF MANAGEMENT: Avoid systemic disease, concurrent
Treatment: need to operate is usually based on neurological infections and emotional upset which exacerbates condition
considerations MANAGEMENT: manageable but not curable
Thymectomy, anticholinesterase medications
C. CEREBRAL VENOUS THROMBOSIS (Pyridostigmine), immunosuppressive treatment
7% associated with pregnancy Myasthenia and pregnancy: pregnancy does not
Greatest risk in late pregnancy and puerperium affect the overall course of MG, fatigue common to
Diagnosis: MR imaging most pregnancies and may be exacerbated and
Management: anticonvusants expanding uterus may compromise respiration
Prognosis: better compared non-pregnant because after MG has no significant adverse effects on pregnancy
delivery the physiology would go back to normal outcomes
Neonatal effects – antibodies transported
IV. DEMYELINATING OR DEGENERATIVE DISEASES transplacentally causing hydramnios
These are rare in pregnancy. So it’s nice to know, that I will
ask this in your exam . V. NEUROPATHIES
General term used to describe disorders of the peripheral
A. MULTIPLE SCLEROSIS nerve/s of any cause
Demyelinating characteristic of this disorder results from Mononeuropathies are more common in pregnancy than
predominantly T cell-mediated autoimmune polyneuropathies
destruction of oligodendrocytes that synthesize myelin
Genetic susceptibility and environmental trigger such A. GUILLAIN-BARRE SYNDROME
as exposure to Chlamydophila pneumonia, human herpes Commonly associated with: Campylobacter jejuni, CMV, EBV,
virus 6 or EBV surgical procedures and immunizations
Pregnancy in relation to multiple sclerosis is good. Relapse is Sensory and motor conduction blockade
reduced during pregnancy but post-partum it could be Not common in pregnancy
increased CLINICAL FEATURES: areflexic paralysis with or without
sensory disturbances
CLINICAL TYPES
B. BELL’S PALSY
RELAPSING- Unpredictable recurrent episodes of focal
Pregnant women are at a four-fold risk
REMITTING MS or multifocal neurological dysfunction
Facial nerve inflammation associated with reactivation of
usually followed by full recovery
HZV
SECONDARY Relapsing-remitting that begins to pursue
Abrupt painful onset with maximum weakness by 48 hours
PROGRESSIVE MS a progressive downhill course after each
Increased association in gestational hypertension and
relapse
preeclampsia
PRIMARY Gradual progression of disability from the
MANAGEMENT: supportive, Prednisone 1mg/kg, orally x 5 days
PROGRESSIVE MS time of initial diagnosis
Corticosteroid improves outcome
PROGRESSIVE- Refers to primary progressive MS with
Treatment includes facial muscle massage and eye
RELAPSING MS apparent relapses
protection against corneal lacerations from drying.
The effect in pregnancy is bad because it increases the risk
CLASSIC FINDINGS: sensory loss, visual symptoms from optic for gestational hypertension leading to pre-eclampsia
neuritis, weakness, paresthesias
CLINICAL DIAGNOSIS: confirmed by MRI or CSF analysis C. CARPAL TUNNEL SYNDROME
Effects of pregnancy on MS: (according to PRIMS study) Compression of the median nerve
reduction in relapse rate during pregnancy but Most frequent mononeuropathy in pregnancy
increased with postpartum Symptoms: burning, numbness, or tingling along the inner
Effects of MS on pregnancy: no adverse effects on half of 1 or both hands
outcome Bilateral in 80% of pregnant women
MANAGEMENT: Goals to arrest acute or initial attacks, disease- Among pregnant, range of symptoms is marked
modifying agents, symptomatic relief Carpal tunnel syndrome is exacerbated by pregnancy
TREATMENT: High dose IV methylprednisolone - 500 to 1000 mg Is there an adverse effect on the mother? When the patient
daily for 3 to 5 days, followed by oral prednisone for 2 weeks is in severe pain it can lead then they could simulate
gestational hypertension without proteinuria
B. MYASTHENIA GRAVIS MANAGEMENT: splint, surgical decompression, corticosteroid
CARDINAL FEATURES: weakness and easy fatigability of facial, VI. SPINAL CORD INJURY
oropharyngeal, extraocular and limb muscles Not common
Also rare May cause preterm and LBV infants
Diplopia and ptosis are common
Clinical course is marked by exacerbation and remissions VII. IDIOPATHIC INTRACRANIAL HYPERTENSION
Systemic diseases, concurrent infections and emotional upset may “pseudotumor cerebri” or benign intracranial hypertension
precipitate exacerbations Cause: unknown
Cause is unknown but genetics may play a role Symptoms: headache, visual disturbances, papilledema
Self-limited, Acetazolamide, Furosemide, Topiramate
3 TYPES: Pregnancy does not alter management
MYASTHENIA Severe muscle weakness, inability to swallow and Pregnancy complications likely due to obesity
CRISIS respiratory muscle paralysis
REFRACTORY Same symptoms unresponsive to usual therapy; VIII. MATERNAL VENTRICULAR SHUNTS
CRISIS medical emergency (worst prognosis) Have satisfactory outcomes
CHOLINERGIC Excessive cholinergic medication leads to nausea, Vaginal delivery is preferred
CRISIS vomiting, weakness, abdominal pain and diarrhea
Transcribers: ESTEPA, LAPEÑA, HIDALGO Page 3 of 9
OBSTETRICS 2
IX. MATERNAL BRAIN DEATH
Rare in obstetrics
X. PSYCHIATRIC ADJUSTMENTS IN PREGNANCY
Biochemical factors – including hormonal effects – and
life stressors can markedly influence mental illness
Exacerbates some coexisting mental disorders
Indeed, pregnancy-related shifts in sex steroids and
monoamine neurotransmitter levels; dysfunction of the
hypothalamic-pituitary-adrenal axis; thyroid dysfunction; and
alterations in immune response are all associated with an
increased risk mood disorders
What hormone is related to aggravating psychiatric changes
in pregnancy? ESTROGEN
The level of perceived stress is significantly higher for
women whose fetus is at high risk for a malformation, for
those with preterm labor or delivery, and for those with
other medical complications
XI. THE PUERPERIUM
Puerperium: particularly stressful time and carries as increased risk for XIV. DEPRESSIVE DISORDERS
mental illness. Up to 15% of women develop a nonpsychotic 1. Unipolar – MAJOR DEPRESSION
postpartum depressive disorder within 6 months of delivery. 2. Bipolar – MANIC DEPRESSION
3. Others – dysthymia, which is chronic, mild depression
MATERNAL BLUES
Postpartum blues: this is a time-limited period of heightened
emotional reactivity experienced by half of women within
approximately the rest week after parturition
Postpartum blues is different from postpartum psychosis
because postpartum blues are usually limited to the first
week of puerperium, they usually resolve within 10 days. So,
if the symptoms persist beyond 10 days then reevaluate the
patient because they may already be having postpartum
psychosis
Prevalence estimates for the blues range from 26% to
84% depending on criteria used diagnosis emotional state
generally peaks on the fourth or fifth post-partum day
and normalizes by day 10
Predominant mood is happiness
However, affected mothers are more emotionally labile, and
insomnia, weepiness, depression, anxiety, poor
concentration, irritability, and affective lability may be noted
Management: supportive, TLC
XII. PRENATAL EVALUATION
Screening for mental illness is generally done at the first
prenatal visit and during the rest of the prenatal visit.
Factors include a search for psychiatric disorders, including
hospitalizations, outpatient care, prior or current use of
psychoactive medications, and current symptoms A. MAJOR DEPRESSION
Check for family history, history of substance use Most common depressive disorder
Risk factors should be evaluated Lifetime prevalence is 17%, but only half ever seek care
Because eating disorders may be exacerbated by pregnancy, Estrogen has been implicated in increased serotonin
affected women should be followed closely synthesis, decreased serotonin breakdown, and serotonin
receptor modulation
XIII. PREGNANCY OUTCOMES Multi-factorial- both genetics and environmental factors
Only a few reports of psychiatric disorders and pregnancy Women who experience postpartum depression often have
outcomes would have an unfavorable outcome. Some, but higher pre-delivery serum estrogen and progesterone levels
not all, link maternal psychiatric illness with untoward and experience a greater decline postpartum
outcomes such as preterm birth, low birthweight, and Postpartum depression – major or minor – develops in 10 to
perinatal mortality. 20 percent of parturients
Recurrent
Postpartum depression is generally under recognized and
undertreated
Major depression during pregnancy or after delivery can
have devastating consequences for affected women, their
children, and families
Recurrence some time after medication is discontinued
develops in 50 to 85% of women with an initial
postpartum depression episode.
Transcribers: ESTEPA, LAPEÑA, HIDALGO Page 4 of 9
OBSTETRICS 2
ECT in pregnancy is not “low risk” and that it should be XVII. PERSONALITY DISORDERS
reserved for women whose depression is recalcitrant to Characterized by the chronic use of certain coping
intensive pharmacotherapy mechanisms in an inappropriate, stereotyped, and mal-
Management: SSRIs (Citalopram, Fluoxetine, Sertraline); adaptive manner
linked to fetal toxicities Are rigid and unyielding personality traits
3 SUBTYPES BY ACOG:
Paranoid, schizoid, and Oddness or eccentricity
schizotypal personality
disorders
Histrionic, narcissistic, Dramatic presentations
antisocial, and borderline along with self-
disorders centeredness and erratic
behavior
Avoidant, dependent, Underlying fear and anxiety
compulsive, and passive-
aggressive personalities
These cases are difficult to handle, but you just have to be
objective and be really patient with them because some are
not able to communicate or follow instructions well
Are at increased risk for teen and unintended
pregnancies, however, it was not a risk factor for elective
or spontaneous abortion
Personality disorders during pregnancy are probably no
different than in non-pregnant women
Give epidural anesthesia so they will be in less pain and
B. BIPOLAR AND RELATED DISORDERS more comfortable and no added stress to the patient
The lifetime prevalence for manic-depression illness is Treatment: antipsychotic drugs such as: Chlorpromazine
3.9%.
No difference in the prevalence of bipolar disorder between XVIII. FEEDING AND EATING DISORDERS
pregnant and non-pregnant reproductive-aged women All eating disorders begin with the desire to be slim, and
Periods of depression last at least 2 weeks. At other times, women with chronic eating disorders may migrate between
there are manic episodes, distinct periods during which there subtypes
is an abnormally raised, expansive, or irritable mood Anorexia nervosa, in which the patient refuses to maintain
Pregnancy frequently prompts medication discontinuation, minimally normal body weight
and this translates to a two-fold increased risk of relapse Bulimia nervosa, there usually is binge eating followed by
during pregnancy purging or by excessive fasting to maintain normal body
Up to 20% of patients with manic-depression illness commit weight. Has a higher risk for IUGR or large-for-gestational
suicide age infants with a concomitantly increased cesarean delivery
rate
XV. POST-PARTUM PSYCHOSIS There is an increased risk for pregnancy complications with
Usually a bipolar disorder, but it may be due to major both eating disorders, but especially in women with bulimia
depression nervosa
Incidence is estimated to be 1 in every 1000 deliveries, and Additional risk associated with eating disorders include poor
it is more common in primiparas, especially those with wound healing and difficulties with breast feeding
obstetrical complications
Illness manifests within 2 weeks of delivery
Most important risk factor for postpartum psychosis … DURING PREGNANCY
is a history of bipolar disease INCREASED RISK UNCHANGED DECREASED RISK
Manic symptoms include feeling excited, elated, “high”; not Migraine Headache Myasthenia Gravis Subarachnoid
needing sleep or unable to sleep; feeling active or energetic; Seizure disorders (MG) Hemorrhage
and feeling “chatty” Bell’s Palsy (4x) Bipolar and Related Guillain-Barre
Affected women have signs of confusion and disorientation Maternal Blues Disorders Syndrome (GBS)
but may also have episodes of lucidity Bulimia > Anorexia Personality Disorders Spinal Cord Injury
Because those with underlying disease have a 10- to 15- Maternal Brain Death
fold risk for recurrence postpartum, close monitoring is
imperative
PREGNANCY…
INCREASES DECREASES
XVI. ANXIETY DISORDERS
Include panic attack, panic disorder, social anxiety disorder, Seizures Multiple Sclerosis (but
specific phobia, separation anxiety disorder, and generalized Ischemic & Hemorrhagic Stroke increased post-partum)
anxiety disorder Fatigue in MG (But over-all MG is
Characterized by irrational fear, tension, and worry, which unchanged)
Bell’s Palsy GHTN, Pre-eclampsia
are accompanied by physiological changes such as
trembling, nausea, hot or cold ashes, dizziness, dyspnea, Carpal Tunnel Syndrome
Eating Disorders
insomnia, and frequent urination
Treated with psychotherapy and medication, including
selective serotonin-reuptake inhibitors, tricyclic
antidepressants, and monoamine oxide inhibitors
Transcribers: ESTEPA, LAPEÑA, HIDALGO Page 5 of 9
OBSTETRICS 2
XIX. TREATMENT
Checkpoint!
Identify:
1. Most common neurological complaint during
pregnancy
2. Most important risk factor for postpartum psychosis
3. Most common depressive order
4. Most common mononeuropathy in pregnancy
5. Hormone related to aggravation of psychiatric
disorders
Headache, history of bipolar disease, major depression, carpal tunnel
syndrome, estrogen
Transcribers: ESTEPA, LAPEÑA, HIDALGO Page 6 of 9
OBSTETRICS 2
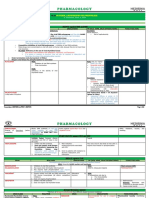
SUMMARY TABLES
FEATURES MANAGEMENT
Most common neurological NON-PHARMA PHARMA
TENSION HA MIGRAINE HA complaint during pregnancy Biofeedback NSAID
MC Frequent but improves during pregnancy Decreased during 3rd Acupuncture Triptans
Muscle tightness Periodic sometimes incapacitating trimester TMS Amitryptiline
Mild-mod pain x hours Episodic attacks of severe HA and ANS dysfunction Primary > secondary Propanolol
Back of neck and head 1st trimester: 2% Metoprolol
No associated neurological disturbances or nausea May increase risk for fetus with limb-reduction
HEADACHE Responds to remedies defects, preeclampsia and other CV morbidities
Migraine without aura Migraine with aura Chronic migraine
Common migraine Classic migraine Occurring at least 15 days each
month for >3 months
Unilateral throbbing HA, nausea, Similar symptoms preceded by
vomiting, photophobia premonitory neurological phenomena
such as visual scotoma or
hallucination
Next most prevalent Pre-conceptional counseling is important
neurological condition Goal of monotherapy: using the least
FOCAL SEIZURES GENERALIZED SEIZURES EPILEPSY
Paroxysmal disorder: teratogenic medication
One localized brain area Both brain hemispheres increased seizure abnormal neuronal discharge Seizure control is main priority
Trauma, abscess, tumor or perinatal Aura abrupt loss of consciousness rates mortality with or without loss of N/V tx
factors risks ,fetal consciousness Avoid Seizure-provoking stimuli
FOCAL SEIZURES FOCAL GENERALIZED ABSENCE malformations
Medication compliance
WITHOUT SEIZURES WITH TONIC-CLONIC SEIZURES – Seizure control is
Breastfeeding – no obvious
SEIZURE DYSCOGNITIVE DYSCOGNITIVE SEIZURES PETIT MAL the main priority deleterious effects
DISORDERS Region of body Aura impaired Loss of Brief loss of Increased CS rate, Anticonvulsants – increased OCP failures
ipsilateral areas – awareness consciousness consciousness HTN, postpartum
tonic-clonic Involuntary tonic contraction without muscle depression
movements movements and rigid posturing activity 10% seizure
clonic Immediate disorder risk in
contractions, recovery children
muscles relax Medications
increased fetal
malformation
HEMORRHAGIC STROKE
CEREBRAL VENOUS
Risk factors: hypertensive
ISCHEMIC STROKE INTRACEREBRAL SUBARACHNOID disorders, GDM, obstetrical
THROMBOSIS
HEMORRHAGE HEMORRHAGE hemorrhage, and CS
Acute occlusion or Chronic hypertension 5.8/100,000, ½ 7%
Major strokes manifest
CEREBRO embolization death of spontaneous rupture of small postpartum Greatest risk: late preg %
brain tissue vessels bleeding in brain CV malformation puerperium during labor, delivery or
VASCULAR puerperium
Sudden onset of severe parenchyma bleeding Puerperium: Lat/sup
DISEASES
headache, hemiplegia or Higher mortality and morbidity 80% saccular or “berry” sagittal venous sinus
neurological deficits or rates aneurysms rupture HA – MC presenting sx
seizures Charcot-Bouchard Rare during pregnancy MRI venography
Echocardiography, CT, MRI or aneurysms = Chronic HTN Need to operate is usually Mgt: anticonvulsants,
angiography, serum lipids, Cautions for gestational based on neurological heparin
antiphospholipid antibodies hypertension management considerations Prognosis: preg/non-preg
and lupus anticoagulant
DEMYELINATING OR DEGENERATIVE DISEASES
MULTIPLE Diagnosis: MRI/CSF analysis T cell-mediated autoimmune Goal: arrest acute or initial attacks,
SCLEROSIS RELAPSING- Unpredictable recurrent episodes of focal or multifocal Pregnancy on MS destruction of oligodendrocytes disease-modifying agents, symptomatic
REMITTING MS neurological dysfunction usually followed by full recovery o during pregnancy Genetic susceptibility and relief
SECONDARY Relapsing-remitting that begins to pursue a progressive o post-partum environmental trigger High dose IV methylprednisolone
PROGRESSIVE MS downhill course after each relapse MS on pregnancy Chlamydophila pneumonia, o 500-1000 mg daily x 3-5 days
PRIMARY Gradual progression of disability from the time of initial o no adverse effects HHV6 or EBV o Then oral prednisone x 2
PROGRESSIVE MS diagnosis Sensory loss, visual symptoms weeks
PROGRESSIVE- Refers to primary progressive MS with apparent relapses from optic neuritis, weakness,
RELAPSING MS paresthesias
MYASTHENIA MYASTHENIA Severe muscle weakness, inability to swallow and respiratory Pregnancy on MG CARDINAL FEATURES: Goal: Avoid exacerbating conditions
GRAVIS CRISIS muscle paralysis o No effect weakness and easy fatigability of Manageable but not curable
o Fatigue facial, oropharyngeal, extraocular Thymectomy, anticholinesterase
Transcribers: ESTEPA, LAPEÑA, HIDALGO Page 7 of 9
OBSTETRICS 2
REFRACTORY Same symptoms unresponsive to usual therapy; medical o Expanding uterus may and limb muscles medications (Pyridostigmine),
CRISIS emergency (worst prognosis) compromise respiration Common: diplopia and ptosis immunosuppressive treatment
CHOLINERGIC Excessive cholinergic medication leads to nausea, vomiting, MG on Pregnancy With exacerbation and
CRISIS weakness, abdominal pain and diarrhea o No effect remissions
Unknown cause ( genetic)
Hydramnios – due to
transplacental Ab transfer
NEUROPATHIES
Campylobacter jejuni, CMV,
EBV, surgical procedures and
immunizations
Sensory and motor
GUILLAIN-BARRE SYNDROME
conduction blockade
Not common in pregnancy
Areflexic paralysis with or
without sensory disturbances
Pregnant – 4x risk Supportive
HZV reactivation Facial nerve Prednisone 1mg/kg, orally x 5 days
inflammation Corticosteroid improves outcome
Abrupt painful onset with Facial muscle massage and eye
BELL’S PALSY maximum weakness by 48 protection against corneal lacerations
hours from drying
Increased association in
gestational hypertension and
preeclampsia
Compression of the median Splint
nerve Surgical decompression
Most frequent mononeuropathy Corticosteroid
in pregnancy
CARPAL TUNNEL SYNDROME
Symptoms: burning,
numbness, or tingling along the
inner half of 1 or both hands
80% bilateral
Not common MATERNAL VENTRICULAR Satisfactory outcomes
SPINAL CORD INJURY
Preterm and LBV infants SHUNTS Vaginal delivery is preferred
“pseudotumor cerebri” or benign intracranial hypertension Rare
Unknown cause
Symptoms: headache, visual disturbances, papilledema
IDIOPATHIC INTRACRANIAL HYPERTENSION MATERNAL BRAIN DEATH
Self-limited, Acetazolamide, Furosemide, Topiramate
Pregnancy does not alter management
Obesity complications
PSYCHOLOGICAL ADJUSTMENTS IN
PRENATAL EVALUATION PUERPERIUM PREGNANCY OUTCOMES
PREGNANCY
Screening for mental illness is generally done at Screening: first prenatal visit and 15% nonpsychotic postpartum depressive disorder within 6 months of delivery Few – unfavorable outcome
the first prenatal visit and during the rest of the during the rest of the prenatal MATERNAL BLUES Some
prenatal visit visit Postpartum blues: time-limited, heightened emotional reactivity o Preterm birth
Factors include a search for psychiatric disorders, Search: psychiatric disorders, including Half of women within rest week after parturition o Low birthweight
including hospitalizations, outpatient care, prior hospitalizations, outpatient care, prior 26%-84% prevalence o Perinatal mortality
or current use of psychoactive medications, and or current use of psychoactive Peaks on the fourth or fifth post-partum day and normalizes by day 10
current symptoms medications, and current symptoms Predominant mood: happiness
Risk factors should be evaluated Risk factors should be evaluated Emotionally labile, and insomnia, weepiness, depression, anxiety, poor
Because eating disorders may be exacerbated by concentration, irritability, and affective lability may be noted
pregnancy, affected women should be followed Management: supportive
closely
Transcribers: ESTEPA, LAPEÑA, HIDALGO Page 8 of 9
OBSTETRICS 2
FEATURES MANAGEMENT
MAJOR Most common depressive disorder ECT – for those recalcitrant to intensive
DEPRESSION 17% lifetime prevalence pharmacotherapy
10-20% parturients
Recurrent
Estrogen
o serotonin synthesis
o serotonin breakdown
o Serotonin receptor modulation
o Higher pre-delivery, same with progesterone
o Greater decline postpartum
Recurrence: 50-85% of women with an initial postpartum depression episode
BIPOLAR AND 3.9% lifetime prevalence
RELATED Pregnant and non-pregnant: no difference in prevalence of bipolar
DISORDERS At least 2 weeks
Manic episodes: abnormally raised, expansive, or irritable mood
Pregnancy stop meds 2% relapse
20% commit suicide
POST- Usually a bipolar disorder, but may be due to major depression
PARTUM Incidence: 1/1000 deliveries, primiparas with obstetrical complications
PSYCHOSIS 2 weeks after delivery
Most important risk factor: history of bipolar disease
Manic symptoms include feeling excited, elated, “high”; not needing sleep or unable to sleep; feeling active or energetic; and feeling “chatty”
Signs of confusion and disorientation but may also have episodes of lucidity
10-15x recurrence risk postpartum
ANXIETY Include panic attack, panic disorder, social anxiety disorder, specific phobia, separation anxiety disorder, and generalized anxiety disorder Psychotherapy and medication
DISORDERS Irrational fear, tension, and worry, which are accompanied by physiological changes such as trembling, nausea, hot or cold ashes, dizziness, SSRI
dyspnea, insomnia, and frequent urination TCA
MAOI
FEEDING AND Anorexia nervosa: refuses to maintain minimally normal body weight
EATING Bulimia nervosa: binge eatingpurging or by excessive fasting to maintain normal body weight
DISORDERS Higher risk for IUGR or LGA infants increased cesarean delivery rate
Increased risk for pregnancy complications with both eating disorders (bulimia nervosa > anorexia nervosa)
Additional risk with poor wound healing and difficulties with breast feeding
PERSONALITY Chronic use of inappropriate, stereotyped, and mal-adaptive manner of coping mechanisms
DISORDERS Rigid and unyielding personality traits
Increased risk for teen and unintended pregnancies
Not a risk factor for elective or spontaneous abortion
Not different than in non-pregnant women
Paranoid, schizoid, and schizotypal Oddness or eccentricity
personality disorders
Histrionic, narcissistic, antisocial, and Dramatic presentations along with self-
borderline disorders centeredness and erratic behavior
Avoidant, dependent, compulsive, and Underlying fear and anxiety
passive-aggressive personalities
Transcribers: ESTEPA, LAPEÑA, HIDALGO Page 9 of 9
Transcribers: ESTEPA, LAPEÑA, HIDALGO Page 10 of 9
S-ar putea să vă placă și
- Applied Statics and Strength of Materials 6th Edition Ebook PDFDocument61 paginiApplied Statics and Strength of Materials 6th Edition Ebook PDFteri.sanborn87695% (44)
- New England Journal of Medicine Volume 383 Issue 19 2020 (Doi 10.1056 - NEJMra1915327) Ropper, Allan H. Ashina, Messoud - MigraineDocument11 paginiNew England Journal of Medicine Volume 383 Issue 19 2020 (Doi 10.1056 - NEJMra1915327) Ropper, Allan H. Ashina, Messoud - MigraineMarija Sekretarjova100% (1)
- 2023 AAN Myositis Autoantibodies FINALDocument53 pagini2023 AAN Myositis Autoantibodies FINALEvelina ȘabanovÎncă nu există evaluări
- Diagnosis of Systemic Lupus ErythematosusDocument6 paginiDiagnosis of Systemic Lupus ErythematosusMuhammad Akhram ResmanaÎncă nu există evaluări
- Neurology Study Guide Oral Board Exam ReviewDocument1 paginăNeurology Study Guide Oral Board Exam Reviewxmc5505Încă nu există evaluări
- Midterm NEUROLOGYDocument122 paginiMidterm NEUROLOGYAhmad SobihÎncă nu există evaluări
- Hypothyroidism Detection and TreatmentDocument4 paginiHypothyroidism Detection and TreatmentJoseph De Joya100% (1)
- Anes Preoperative-AssessmentDocument6 paginiAnes Preoperative-AssessmentChristine Mendoza100% (1)
- Neuro-Ophthalmology: Introduction: James Goodwin, MD (Attending)Document4 paginiNeuro-Ophthalmology: Introduction: James Goodwin, MD (Attending)Mariano FioreÎncă nu există evaluări
- Topic: Asthma and Copd: Internal Medicine IiDocument8 paginiTopic: Asthma and Copd: Internal Medicine IicarlosÎncă nu există evaluări
- Week 10 - Hypertension, Atherosclerosis, ArrhythmiaDocument14 paginiWeek 10 - Hypertension, Atherosclerosis, Arrhythmiashivani patel100% (1)
- Pedia: NeuroDocument4 paginiPedia: Neuroapi-37045620% (1)
- Anti-Migraine DrugsDocument21 paginiAnti-Migraine DrugsGareth BaleÎncă nu există evaluări
- Enls v4 0 Sah Slides FinalDocument40 paginiEnls v4 0 Sah Slides FinalTariku GelesheÎncă nu există evaluări
- Trans Congenital MalformationsDocument10 paginiTrans Congenital MalformationsRemelou Garchitorena AlfelorÎncă nu există evaluări
- Neuro Radio Part 1: StrokeDocument36 paginiNeuro Radio Part 1: Strokecinnamon swirlÎncă nu există evaluări
- Neurology - Headache NotesDocument3 paginiNeurology - Headache NotessarahÎncă nu există evaluări
- Review: Eduardo Tolosa, Alicia Garrido, Sonja W Scholz, Werner PoeweDocument13 paginiReview: Eduardo Tolosa, Alicia Garrido, Sonja W Scholz, Werner PoeweSaraÎncă nu există evaluări
- Increased ICP: A) HeadacheDocument5 paginiIncreased ICP: A) Headachemohamed nagyÎncă nu există evaluări
- Red Eye: A Guide For Non-Specialists: MedicineDocument14 paginiRed Eye: A Guide For Non-Specialists: MedicineFapuw Parawansa100% (1)
- Neurology Work BookDocument73 paginiNeurology Work BookCastleKGÎncă nu există evaluări
- Childhood Epilepsy Etiology, Epidemiology & ManagementDocument6 paginiChildhood Epilepsy Etiology, Epidemiology & ManagementJosh RoshalÎncă nu există evaluări
- Seizure and EpilepsyDocument18 paginiSeizure and EpilepsyJamal JosephÎncă nu există evaluări
- B5W1L9.Peripheral Neuropathy - Lecture Notes 12Document4 paginiB5W1L9.Peripheral Neuropathy - Lecture Notes 12mihalcea alinÎncă nu există evaluări
- Tinnitus MedscapeDocument15 paginiTinnitus MedscapeAnonymous Puj7S1tÎncă nu există evaluări
- Localization of Brain Stem LesionsDocument35 paginiLocalization of Brain Stem LesionsHrishikesh Jha0% (1)
- Cranial Nerve Nuclei and Their FunctionsDocument6 paginiCranial Nerve Nuclei and Their FunctionsThanat PetchrodÎncă nu există evaluări
- Antithrombotic Therapy For VTE Disease CHEST Guideline and Expert Panel ReportDocument38 paginiAntithrombotic Therapy For VTE Disease CHEST Guideline and Expert Panel ReportAdriana VasilicaÎncă nu există evaluări
- Cholinergics & AnticholinergicsDocument7 paginiCholinergics & AnticholinergicsKimberly MunsayacÎncă nu există evaluări
- Ent Diseases of The Oral and Pharynx Dr. UyDocument7 paginiEnt Diseases of The Oral and Pharynx Dr. UyAileen EmyÎncă nu există evaluări
- Ect (Part I) : Mira Hezrina Binti Marzaki Group 5Document13 paginiEct (Part I) : Mira Hezrina Binti Marzaki Group 5f4rog4ieÎncă nu există evaluări
- Diagnosing Secondary Headaches (Practical Neurology) (2020 - 05)Document5 paginiDiagnosing Secondary Headaches (Practical Neurology) (2020 - 05)Apostolos T.Încă nu există evaluări
- Meninges, Ventricles - CSF - Study GuideDocument3 paginiMeninges, Ventricles - CSF - Study Guideshivani patelÎncă nu există evaluări
- A To Z Diseases LISTS For NEETPGDocument5 paginiA To Z Diseases LISTS For NEETPGQworldÎncă nu există evaluări
- CARDIO - Valvular Heart Diseases Table DR BARTOLOMEDocument8 paginiCARDIO - Valvular Heart Diseases Table DR BARTOLOMEShams JailaniÎncă nu există evaluări
- A Seminar Presentation On Mechanism of Drug ActionDocument40 paginiA Seminar Presentation On Mechanism of Drug Actionbellatrix aliaÎncă nu există evaluări
- PARANEOPLASTICDocument8 paginiPARANEOPLASTICMuhammad Imran MirzaÎncă nu există evaluări
- Classification of The Epilepsies: Purpose: For Clinical DiagnosisDocument25 paginiClassification of The Epilepsies: Purpose: For Clinical Diagnosisayu rifqiÎncă nu există evaluări
- Cerebral Vascular Diseases ExplainedDocument115 paginiCerebral Vascular Diseases ExplainedUbaidillah Romadlon AlfairuziÎncă nu există evaluări
- Idiopathic Intracranial HypertensionDocument21 paginiIdiopathic Intracranial HypertensionJorge Dornellys LapaÎncă nu există evaluări
- Internal Medicine - Nephrology Lecture on Cystic Kidney DiseasesDocument3 paginiInternal Medicine - Nephrology Lecture on Cystic Kidney DiseasesVon HippoÎncă nu există evaluări
- Anterior Abdominal Wall Surgery InsightsDocument5 paginiAnterior Abdominal Wall Surgery InsightsAnonymous 2TzM1ZÎncă nu există evaluări
- Neurology Exam Checklist1Document6 paginiNeurology Exam Checklist1Syed AfzalÎncă nu există evaluări
- REVISED Head InjuryDocument4 paginiREVISED Head InjuryJanselle H Arma0% (1)
- Neurology: Timothy E. Welty, Pharm.D., FCCP, BCPSDocument68 paginiNeurology: Timothy E. Welty, Pharm.D., FCCP, BCPSAlmaha AlfakhriÎncă nu există evaluări
- Pituitary Adenoma Classification, Presentation, and TreatmentDocument20 paginiPituitary Adenoma Classification, Presentation, and TreatmentAbdulaziz Al-TaisanÎncă nu există evaluări
- LECTURE 22: Antipsychotic Agents & Lithium: OutlineDocument5 paginiLECTURE 22: Antipsychotic Agents & Lithium: OutlineRosa PalconitÎncă nu există evaluări
- Agitated Patient Treatment MapDocument1 paginăAgitated Patient Treatment MapMuhammed ElgasimÎncă nu există evaluări
- PSGNDocument23 paginiPSGNalpha mae beltranÎncă nu există evaluări
- Embryology of The Renal SystemDocument8 paginiEmbryology of The Renal SystemStd DlshsiÎncă nu există evaluări
- (Surg2) 5.1d Anesthesia PointersDocument12 pagini(Surg2) 5.1d Anesthesia PointersAlloiBialbaÎncă nu există evaluări
- Congenital AnemiaDocument5 paginiCongenital AnemiaharideepÎncă nu există evaluări
- (SURG) 5.4b Management of Soft Tissue SarcomaDocument6 pagini(SURG) 5.4b Management of Soft Tissue SarcomaKenneth TorresÎncă nu există evaluări
- Nsaid: Pharmakokinetics Pharmakodynamics CU AE CI DI Salicylic AcidDocument2 paginiNsaid: Pharmakokinetics Pharmakodynamics CU AE CI DI Salicylic AcidjessmasakiÎncă nu există evaluări
- Neurological Examination: ObserveDocument9 paginiNeurological Examination: ObserveTom MallinsonÎncă nu există evaluări
- Neurological Exam: H.Khorrami PH.DDocument74 paginiNeurological Exam: H.Khorrami PH.Dkhorrami4100% (1)
- CVA or StrokeDocument14 paginiCVA or StrokeJoenalyn AliguinÎncă nu există evaluări
- Pharmacology Student Activity Sheet on Antipsychotic and Anxiolytic DrugsDocument5 paginiPharmacology Student Activity Sheet on Antipsychotic and Anxiolytic DrugsChelsy Sky SacanÎncă nu există evaluări
- CNSexam PDFDocument8 paginiCNSexam PDFkarthiktsvmcÎncă nu există evaluări
- Revell 2014Document6 paginiRevell 2014kemoÎncă nu există evaluări
- Diagnostico y Manejo de Masas AnexialesDocument6 paginiDiagnostico y Manejo de Masas AnexialesChristopher Hernán Valenzuela ArancibiaÎncă nu există evaluări
- Pulmonary Disorders in PregnancyDocument5 paginiPulmonary Disorders in PregnancyDasha VeeÎncă nu există evaluări
- F.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Document3 paginiF.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Dasha VeeÎncă nu există evaluări
- OB OSCE.06 OB GYNE ULTRASOUND (Dr. Ursua) PDFDocument1 paginăOB OSCE.06 OB GYNE ULTRASOUND (Dr. Ursua) PDFDasha VeeÎncă nu există evaluări
- Philippine Journal of Gynecologic Oncology Volume 9 Number 1 2012Document48 paginiPhilippine Journal of Gynecologic Oncology Volume 9 Number 1 2012Dasha VeeÎncă nu există evaluări
- F.03 HEMATOLOGIC DISEASES IN PREGNANCY (DR - Taguiling) 04-25-2019 (Part 1) PDFDocument4 paginiF.03 HEMATOLOGIC DISEASES IN PREGNANCY (DR - Taguiling) 04-25-2019 (Part 1) PDFDasha VeeÎncă nu există evaluări
- The Characteristic Ultrasound Features of Specific Types of Ovarian Pathology (Review) PDFDocument14 paginiThe Characteristic Ultrasound Features of Specific Types of Ovarian Pathology (Review) PDFDasha VeeÎncă nu există evaluări
- WJR 5 113Document13 paginiWJR 5 113Valian IndrianyÎncă nu există evaluări
- Practice Bulletin: Management of Adnexal MassesDocument14 paginiPractice Bulletin: Management of Adnexal MassesDasha VeeÎncă nu există evaluări
- DiagnosisDocument8 paginiDiagnosisDasha VeeÎncă nu există evaluări
- F.02 DERMATOLOGIC DISEASES IN PREGNANCY (Dr. Taguiling) 04-12-2019 PDFDocument5 paginiF.02 DERMATOLOGIC DISEASES IN PREGNANCY (Dr. Taguiling) 04-12-2019 PDFDasha VeeÎncă nu există evaluări
- Pulmonary Disorders in PregnancyDocument5 paginiPulmonary Disorders in PregnancyDasha VeeÎncă nu există evaluări
- F.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Document3 paginiF.07 STD AND INFECTIONS IN PREGNANCY (DR - Jandoc) 05-03-2019 (Part 2)Dasha VeeÎncă nu există evaluări
- F.06 STD and Infections in Pregnancy (Dr. Jandoc) 05-03-2019 (Part 1)Document5 paginiF.06 STD and Infections in Pregnancy (Dr. Jandoc) 05-03-2019 (Part 1)Dasha VeeÎncă nu există evaluări
- Obstetrics 2: Obstetric Hemorrhage (Part 2)Document4 paginiObstetrics 2: Obstetric Hemorrhage (Part 2)Dasha VeeÎncă nu există evaluări
- P.09 OBSTETRIC HEMORRHAGE (Dr. Ursua) 02-07-2019 (Part 1)Document3 paginiP.09 OBSTETRIC HEMORRHAGE (Dr. Ursua) 02-07-2019 (Part 1)Dasha VeeÎncă nu există evaluări
- Embryogenesis & Fetal DevelopementDocument38 paginiEmbryogenesis & Fetal DevelopementDasha Vee100% (1)
- Antiviral Chemotherapy and Prophylaxis: Acyclovir, Valacyclovir, and FamciclovirDocument8 paginiAntiviral Chemotherapy and Prophylaxis: Acyclovir, Valacyclovir, and FamciclovirDasha VeeÎncă nu există evaluări
- 2011 Full Page Calendar - TomKat StudioDocument12 pagini2011 Full Page Calendar - TomKat StudioThe TomKat StudioÎncă nu există evaluări
- F.09 BONE RADIOLOGY - Dr. GalangDocument11 paginiF.09 BONE RADIOLOGY - Dr. GalangDasha VeeÎncă nu există evaluări
- Mental HealthDocument4 paginiMental HealthDasha VeeÎncă nu există evaluări
- Thyroid PDFDocument9 paginiThyroid PDFDasha VeeÎncă nu există evaluări
- m.13 Dietary Supplements & Herbal Medications (Dr. Buñag) 04-04-18Document4 paginim.13 Dietary Supplements & Herbal Medications (Dr. Buñag) 04-04-18Dasha VeeÎncă nu există evaluări
- Philippine CPG On The Diagnosis and Management of Urinary Tract Infections in Adults-2015 Update - Part 2 PDFDocument140 paginiPhilippine CPG On The Diagnosis and Management of Urinary Tract Infections in Adults-2015 Update - Part 2 PDFspringdingÎncă nu există evaluări
- M.10B Drugs Used in Gastrointestinal DisordersDocument3 paginiM.10B Drugs Used in Gastrointestinal DisordersDasha VeeÎncă nu există evaluări
- P.07 Thyroid and Parathyroid Glands Dr. Manalo 9-8-16Document4 paginiP.07 Thyroid and Parathyroid Glands Dr. Manalo 9-8-16Dasha VeeÎncă nu există evaluări
- MEDICAL CERTIFICATIONDocument7 paginiMEDICAL CERTIFICATIONDasha VeeÎncă nu există evaluări
- Ob Osce.04 CTG ReadingDocument6 paginiOb Osce.04 CTG ReadingDasha VeeÎncă nu există evaluări
- f.02 Intellectual Disabilities (Dr. Rebucal) 04-11-2019Document4 paginif.02 Intellectual Disabilities (Dr. Rebucal) 04-11-2019Dasha VeeÎncă nu există evaluări
- 4 Influencing Factors of Learners Career Choice Parents Choice Vs Personal DescisionDocument24 pagini4 Influencing Factors of Learners Career Choice Parents Choice Vs Personal Descisionmatteo mamaloÎncă nu există evaluări
- Equilibruim of Forces and How Three Forces Meet at A PointDocument32 paginiEquilibruim of Forces and How Three Forces Meet at A PointSherif Yehia Al MaraghyÎncă nu există evaluări
- Rapport DharaviDocument23 paginiRapport DharaviUrbanistes du MondeÎncă nu există evaluări
- U2 All That You Can't Leave BehindDocument82 paginiU2 All That You Can't Leave BehindFranck UrsiniÎncă nu există evaluări
- Human Rights Alert: Corrective Actions in Re: Litigation Involving Financial InstitutionsDocument3 paginiHuman Rights Alert: Corrective Actions in Re: Litigation Involving Financial InstitutionsHuman Rights Alert - NGO (RA)Încă nu există evaluări
- A Database of Chromatographic Properties and Mass Spectra of Fatty Acid Methyl Esters From Omega-3 ProductsDocument9 paginiA Database of Chromatographic Properties and Mass Spectra of Fatty Acid Methyl Esters From Omega-3 ProductsmisaelÎncă nu există evaluări
- Revision Worksheet - Matrices and DeterminantsDocument2 paginiRevision Worksheet - Matrices and DeterminantsAryaÎncă nu există evaluări
- Mpu 2312Document15 paginiMpu 2312Sherly TanÎncă nu există evaluări
- KPUPDocument38 paginiKPUPRoda ES Jimbert50% (2)
- Key Fact Sheet (HBL FreedomAccount) - July 2019 PDFDocument1 paginăKey Fact Sheet (HBL FreedomAccount) - July 2019 PDFBaD cHaUhDrYÎncă nu există evaluări
- (123doc) - Chapter-24Document6 pagini(123doc) - Chapter-24Pháp NguyễnÎncă nu există evaluări
- Gabinete STS Activity1Document2 paginiGabinete STS Activity1Anthony GabineteÎncă nu există evaluări
- Excess AirDocument10 paginiExcess AirjkaunoÎncă nu există evaluări
- Oxgen Sensor Cat WEBDocument184 paginiOxgen Sensor Cat WEBBuddy Davis100% (2)
- Advantages of Using Mobile ApplicationsDocument30 paginiAdvantages of Using Mobile ApplicationsGian Carlo LajarcaÎncă nu există evaluări
- United-nations-Organization-uno Solved MCQs (Set-4)Document8 paginiUnited-nations-Organization-uno Solved MCQs (Set-4)SãñÂt SûRÿá MishraÎncă nu există evaluări
- NLP Business Practitioner Certification Course OutlineDocument11 paginiNLP Business Practitioner Certification Course OutlineabobeedoÎncă nu există evaluări
- Ailunce HD1 Software ManualDocument33 paginiAilunce HD1 Software ManualMarc LaBarberaÎncă nu există evaluări
- Individual Performance Commitment and Review Form (Ipcrf) : Mfos Kras Objectives Timeline Weight Per KRADocument4 paginiIndividual Performance Commitment and Review Form (Ipcrf) : Mfos Kras Objectives Timeline Weight Per KRAChris21JinkyÎncă nu există evaluări
- Dance Appreciation and CompositionDocument1 paginăDance Appreciation and CompositionFretz Ael100% (1)
- Developing the cycle of maslahah based performance management system implementationDocument27 paginiDeveloping the cycle of maslahah based performance management system implementationM Audito AlfansyahÎncă nu există evaluări
- Joining Instruction 4 Years 22 23Document11 paginiJoining Instruction 4 Years 22 23Salmini ShamteÎncă nu există evaluări
- Mil STD 2154Document44 paginiMil STD 2154Muh SubhanÎncă nu există evaluări
- Ovr IbDocument27 paginiOvr IbAriel CaresÎncă nu există evaluări
- Felizardo C. Lipana National High SchoolDocument3 paginiFelizardo C. Lipana National High SchoolMelody LanuzaÎncă nu există evaluări
- Rubric 5th GradeDocument2 paginiRubric 5th GradeAlbert SantosÎncă nu există evaluări
- Ofper 1 Application For Seagoing AppointmentDocument4 paginiOfper 1 Application For Seagoing AppointmentNarayana ReddyÎncă nu există evaluări
- IELTS Speaking Q&ADocument17 paginiIELTS Speaking Q&ABDApp Star100% (1)