Documente Academic
Documente Profesional
Documente Cultură
Roils Case Study
Încărcat de
api-4833397570 evaluări0% au considerat acest document util (0 voturi)
49 vizualizări3 paginiThe document describes a case study reported to the Radiation Oncology Incident Learning System (RO-ILS) where a patient's radiation therapy treatment was delivered to the wrong vertebral body. There were two contributing factors - the lack of a timeout with the radiation oncology team present, and the failure to verify the correct vertebral level with onboard imaging. To prevent similar errors, the document recommends requiring timeouts and onboard imaging to verify patient alignment, as well as establishing standard procedures for shifts greater than 2 cm.
Descriere originală:
Titlu original
roils case study
Drepturi de autor
© © All Rights Reserved
Formate disponibile
DOCX, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentThe document describes a case study reported to the Radiation Oncology Incident Learning System (RO-ILS) where a patient's radiation therapy treatment was delivered to the wrong vertebral body. There were two contributing factors - the lack of a timeout with the radiation oncology team present, and the failure to verify the correct vertebral level with onboard imaging. To prevent similar errors, the document recommends requiring timeouts and onboard imaging to verify patient alignment, as well as establishing standard procedures for shifts greater than 2 cm.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
49 vizualizări3 paginiRoils Case Study
Încărcat de
api-483339757The document describes a case study reported to the Radiation Oncology Incident Learning System (RO-ILS) where a patient's radiation therapy treatment was delivered to the wrong vertebral body. There were two contributing factors - the lack of a timeout with the radiation oncology team present, and the failure to verify the correct vertebral level with onboard imaging. To prevent similar errors, the document recommends requiring timeouts and onboard imaging to verify patient alignment, as well as establishing standard procedures for shifts greater than 2 cm.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca DOCX, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 3
1
Haley Kroeplin
DOS 518 Professional Issues
September 26, 2020
Radiation Oncology Incident Learning System (RO-ILS) Case Study
Radiation therapy is a therapeutic treatment modality used to treat a wide variety of
cancer patients with curative or palliative intent. Although most treatments are delivered safely
and effectively, there have been a few incidents that have received national attention in the past
due to catastrophic treatment errors.1 In light of these unfortunate events, the American Society
for Radiation Oncology (ASTRO) and American Association of Physicists in Medicine (AAPM)
developed the Radiation Oncology Incident Learning System (RO-ILS) in June 2014, through
ASTRO’s Target Safely program.2 The mission of this national error reporting system is to
promote safe and superior quality of care in radiation oncology by implementing a database for
institutions to learn from each other in a secure and non-disciplinary setting in order to prevent
similar mistakes occurring in their departments in the future.3 Since its introduction in 2014,
more than 550 United States healthcare organizations have joined RO-ILS to provide patient
safety information to the database.2 The following case was logged into the RO-ILS and will be
evaluated with a focus of identifying what went wrong in the process and providing
recommendations that may prevent the mistake from occurring again.
The specifics of this case are as follows: for one fraction out of course of 45 fractions, a
patient’s radiation therapy treatment was delivered to the wrong vertebral body. The patient was
positioned in a stereotactic body fix system and aligned to their three-point tattoos. Once the
patient’s tattoos were aligned with the lasers in the room, the therapists stepped out of the room
to perform daily shifts from the tattoos to the isocenter. On the day that the error was made, the
stereotactic system requested a shift of 2.5 cm in the sup/inf direction which was applied by the
therapists. A conebeam computed tomography (CBCT) was performed thereafter and a -0.4 cm
correction was made in the sup/inf direction. This resulted in a total offset from the correct
isocenter to be 2.1 cm. It wasn’t until after the treatment, that a physician who was reviewing the
CBCT images noticed that the radiation therapy treatment was delivered to the wrong vertebral
body.
Upon evaluation of this incident submitted to the RO-ILS, there are a couple contributing
factors that led to this adverse event in which the radiation therapists administered a patient’s
radiation therapy treatment to the incorrect vertebral body. If this error occurred during the first
treatment, one of the contributing components would have been the lack of members of the
2
Haley Kroeplin
DOS 518 Professional Issues
September 26, 2020
radiation oncology team, such as the radiation oncologist and radiation therapists, present during
the time out or procedural pause prior to treatment. Having various radiation oncology team
members present to verify and agree that the correct vertebral body was localized prior to
treatment delivery would have prevented this error. In addition, this would have eliminated the
error being caught post treatment when a physician was reviewing the patient’s offline CBCT
images. If this error occurred during a subsequent treatment, the therapists could have called a
time-out to double check that the patient was setup correctly and that the correct patient chart
was pulled up. If everything was correct, they should have called a physician to review images if
they were questioning why the stereotactic system calculated a larger than normal shift for this
patient. By taking the time to verify alignment or question unusual shifts, would have hopefully
resulted in a ‘good catch’ and ‘near miss’ rather than a treatment error.
The second contributing factor that led to this error is not verifying the vertebral level
with onboard imaging (OBI). It is well known that without including bony landmark anatomy,
such as the base of skull, first or twelfth thoracic vertebra, or the fifth lumbar spine, localization
of the correct vertebral level can be difficult. During this incident, the radiation therapists could
have shifted the OBI imager to include one of these landmarks in order to count the vertebral
bodies and identify the correct level for treatment prior to utilizing the stereotactic system or
CBCT. Furthermore, they could have also verified the vertebral level after they noticed that a
greater than 2 cm shift was noted with initial imaging. Establishing institutional imaging
guidelines about verifying vertebral level with OBI prior to additional imaging or requiring
verification of vertebral level with OBI if shifts are greater than 2 cm in any direction would
ensure that another radiation therapy treatment delivered to the wrong vertebral body would not
occur.
Although mistakes can happen, it is imperative that institutions learn from the errors
reported in the RO-ILS and develop protocols that would prevent a similar error from occurring
within their departments. As noted by Hendee et al4 empowering team members to declare a time
out if they have any questions or concerns about a patient’s treatment and establishing standard
operating procedures can diminish errors in radiation oncology. By incorporating these
recommendations within a radiation oncology department, ensures that patient safety is the
primary focus and responsibility of all team members.
3
Haley Kroeplin
DOS 518 Professional Issues
September 26, 2020
References
1. Terezakis SA, Pronovost P, Harris K, Deweese T, Ford E. Safety strategies in an academic
radiation oncology department and recommendations for action. Jt Comm J Qual Patient Saf.
2011;37(7):291-299. https://doi.org/10.1016/s1553-7250(11)37037-7
2. Evans SB, Ford EC. Radiation oncology incident learning system: A call to participation.
International Journal of Radiation Oncology Biology Physics. 2014;90(2):249-250.
https://doi.org/10.1016/j.ijrobp.2014.05.2671
3. Radiation Oncology Incident Learning System. American Society for Radiation Oncology
website. https://www.astro.org/Patient-Care-and-Research/Patient-Safety/RO-ILS. Accessed
October 1, 2020.
4. Hendee WR, Herman MG. Improving patient safety in radiation oncology. International
Journal of Radiation Oncology Biology Physics. 2010;38(1):78-82.
https://doi.org/10.1118/1.3522875
S-ar putea să vă placă și
- Bedside Ultrasound: Level 1 - Second EditionDe la EverandBedside Ultrasound: Level 1 - Second EditionEvaluare: 5 din 5 stele5/5 (1)
- Instant Download Ebook PDF Essentials of Dental Radiography 10th Edition PDF ScribdDocument41 paginiInstant Download Ebook PDF Essentials of Dental Radiography 10th Edition PDF Scribdeugene.hernandez23398% (40)
- Holtzclaw Pterygoid NODocument13 paginiHoltzclaw Pterygoid NOHamesh GangadharanÎncă nu există evaluări
- Radiation Oncology Incident Learning System Case StudyDocument4 paginiRadiation Oncology Incident Learning System Case Studyapi-527613255Încă nu există evaluări
- RoilsDocument4 paginiRoilsapi-585462575Încă nu există evaluări
- RO-ILS Case StudyDocument4 paginiRO-ILS Case Studyapi-458422967Încă nu există evaluări
- Ro-Ils PaperDocument4 paginiRo-Ils Paperapi-502011468Încă nu există evaluări
- Roils ReportDocument5 paginiRoils Reportapi-632526087Încă nu există evaluări
- RoilsDocument2 paginiRoilsapi-478066704Încă nu există evaluări
- Radiation Safety PaperDocument3 paginiRadiation Safety Paperapi-635186395Încă nu există evaluări
- Radiation Oncology Incident Learning SystemDocument4 paginiRadiation Oncology Incident Learning Systemapi-484763634Încă nu există evaluări
- Ro-Ils Paper RsDocument4 paginiRo-Ils Paper Rsapi-379797290Încă nu există evaluări
- Roils PaperDocument5 paginiRoils Paperapi-642376263Încă nu există evaluări
- Radiation Safety-Nicolette SawickiDocument4 paginiRadiation Safety-Nicolette Sawickiapi-484758207Încă nu există evaluări
- Safety EssayDocument5 paginiSafety Essayapi-350437453Încă nu există evaluări
- RoilsDocument4 paginiRoilsapi-631250296Încă nu există evaluări
- Scott Stallard Roils Case StudyDocument4 paginiScott Stallard Roils Case Studyapi-549064749Încă nu există evaluări
- Week2 Submitter PaperDocument3 paginiWeek2 Submitter Paperapi-299189797Încă nu există evaluări
- Acr-Spr Practice Parameter For The Performance and Interpretation of Skeletal Surveys in ChildrenDocument9 paginiAcr-Spr Practice Parameter For The Performance and Interpretation of Skeletal Surveys in ChildrenPediatría grupoÎncă nu există evaluări
- Rad Safety PaperDocument6 paginiRad Safety Paperapi-692616289Încă nu există evaluări
- RoilsDocument3 paginiRoilsapi-635954562Încă nu există evaluări
- Radiation Safety PaperDocument4 paginiRadiation Safety Paperapi-527662950Încă nu există evaluări
- Ro-Ils 1Document3 paginiRo-Ils 1api-529438966Încă nu există evaluări
- Radiation Safety PaperDocument4 paginiRadiation Safety Paperapi-530130628Încă nu există evaluări
- RoilsDocument3 paginiRoilsapi-530935128Încă nu există evaluări
- Roils PaperDocument4 paginiRoils Paperapi-575843507Încă nu există evaluări
- RoilsDocument4 paginiRoilsapi-491087286Încă nu există evaluări
- Roils 1Document4 paginiRoils 1api-574059920Încă nu există evaluări
- Safety PaperDocument4 paginiSafety Paperapi-336793554Încă nu există evaluări
- Ro-Ils Project 1Document4 paginiRo-Ils Project 1api-633652323Încă nu există evaluări
- Continuous Quality Improvements and SafetyDocument3 paginiContinuous Quality Improvements and Safetyapi-518020510Încă nu există evaluări
- RoilspaperDocument5 paginiRoilspaperapi-530717893Încă nu există evaluări
- Myelography PDFDocument13 paginiMyelography PDFAhmad HaririÎncă nu există evaluări
- Ditkofsky 2015Document28 paginiDitkofsky 2015Allython Jureth Peña ReyesÎncă nu există evaluări
- Acr-Spr-Ssr Practice Parameter For The Performance of Radiography of The ExtremitiesDocument8 paginiAcr-Spr-Ssr Practice Parameter For The Performance of Radiography of The ExtremitiesEdiPtkÎncă nu există evaluări
- Radiation Safety PaperDocument5 paginiRadiation Safety Paperapi-691862313Încă nu există evaluări
- IlsDocument3 paginiIlsapi-567185090Încă nu există evaluări
- US PelvisDocument11 paginiUS PelvisDian Putri NingsihÎncă nu există evaluări
- Radiation Planning Assistant - A Streamlined, Fully Automated Radiotherapy Treatment Planning SystemDocument9 paginiRadiation Planning Assistant - A Streamlined, Fully Automated Radiotherapy Treatment Planning Systemdrrajeshb77Încă nu există evaluări
- Point-of-Care Ultrasound: Not A Stethoscope-A Separate Clinical EntityDocument2 paginiPoint-of-Care Ultrasound: Not A Stethoscope-A Separate Clinical Entityapi-274764147Încă nu există evaluări
- Acr Practice Parameter For The Performance of HysterosalpingographyDocument9 paginiAcr Practice Parameter For The Performance of HysterosalpingographyAsif JielaniÎncă nu există evaluări
- Final Draft-Muna 1Document4 paginiFinal Draft-Muna 1api-693187588Încă nu există evaluări
- Dos 516 Radiation Safety PaperDocument4 paginiDos 516 Radiation Safety Paperapi-530270156Încă nu există evaluări
- IlsDocument5 paginiIlsapi-631272802Încă nu există evaluări
- Jurnal JKMR Digital Analisis RejectDocument35 paginiJurnal JKMR Digital Analisis RejectReeÎncă nu există evaluări
- J Applied Clin Med Phys - 2022 - Fisher - AAPM Medical Physics Practice Guideline 12 A Fluoroscopy Dose Management-1Document19 paginiJ Applied Clin Med Phys - 2022 - Fisher - AAPM Medical Physics Practice Guideline 12 A Fluoroscopy Dose Management-1Roshi_11Încă nu există evaluări
- ScoliosisDocument10 paginiScoliosisSilma FarrahaÎncă nu există evaluări
- Acr-Astro Practice Guideline For Image-Guided Radiation Therapy (Igrt)Document9 paginiAcr-Astro Practice Guideline For Image-Guided Radiation Therapy (Igrt)freemind_mxÎncă nu există evaluări
- Deep Learning Predicts Hip Fracture Using Confounding Patient and Healthcare VariablesDocument17 paginiDeep Learning Predicts Hip Fracture Using Confounding Patient and Healthcare VariablesChrisÎncă nu există evaluări
- Week 5 Case TwoDocument3 paginiWeek 5 Case Twoapi-510897511Încă nu există evaluări
- Radiation SafetyDocument4 paginiRadiation Safetybraith7811Încă nu există evaluări
- Aying Michael AndersonDocument1 paginăAying Michael Andersonptrcksx.jÎncă nu există evaluări
- Discussion 2 RevisedDocument4 paginiDiscussion 2 Revisedapi-332574751Încă nu există evaluări
- Radiation Safety PaperDocument4 paginiRadiation Safety Paperapi-692115810Încă nu există evaluări
- Roils Case StudyDocument4 paginiRoils Case Studyapi-530752813Încă nu există evaluări
- Roils PaperDocument4 paginiRoils Paperapi-633434674Încă nu există evaluări
- Zehnder - The Safety of RadiationDocument5 paginiZehnder - The Safety of Radiationapi-692126663Încă nu există evaluări
- Asa 2013Document1.076 paginiAsa 2013Marwa Mahrous100% (4)
- Radiation Safety Paper Week 2Document3 paginiRadiation Safety Paper Week 2api-299270003Încă nu există evaluări
- Radiaton Safety PaperDocument3 paginiRadiaton Safety Paperapi-692383438Încă nu există evaluări
- Radiation Oncology Incident Learning System (ROILS) Cast StudyDocument4 paginiRadiation Oncology Incident Learning System (ROILS) Cast Studyapi-481226212Încă nu există evaluări
- Electron CompDocument1 paginăElectron Compapi-483339757Încă nu există evaluări
- Employer Service Learning Journal 1Document1 paginăEmployer Service Learning Journal 1api-483339757Încă nu există evaluări
- Capstone Final Revisions 10-29-20-2Document14 paginiCapstone Final Revisions 10-29-20-2api-483339757Încă nu există evaluări
- Community ServiceDocument2 paginiCommunity Serviceapi-483339757Încă nu există evaluări
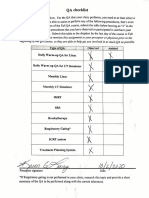
- Qa ChecklistDocument1 paginăQa Checklistapi-483339757Încă nu există evaluări
- Scan Aug 14 2020Document1 paginăScan Aug 14 2020api-483339757Încă nu există evaluări
- Research Proposal Group 10Document6 paginiResearch Proposal Group 10api-483339757Încă nu există evaluări
- Value-Addition of Lateral Cephalometric Radiographs in Orthodontic Diagnosis and Treatment PlanningDocument7 paginiValue-Addition of Lateral Cephalometric Radiographs in Orthodontic Diagnosis and Treatment PlanningMirek SzÎncă nu există evaluări
- Radiologia en EndodonciaDocument12 paginiRadiologia en EndodonciaBelez Jum JumÎncă nu există evaluări
- Condilectomia Intra OralDocument7 paginiCondilectomia Intra OralJuan Carlos MeloÎncă nu există evaluări
- Dental EquipmentDocument30 paginiDental EquipmentMahiraÎncă nu există evaluări
- Dental Computing and Applications PDFDocument407 paginiDental Computing and Applications PDFPallav Ganatra100% (1)
- DR Pavin Sir ImplantsDocument74 paginiDR Pavin Sir ImplantsAME DENTAL COLLEGE RAICHUR, KARNATAKAÎncă nu există evaluări
- Clinical Considerations of Temporary Anchorage Devices in OrthodonticsDocument7 paginiClinical Considerations of Temporary Anchorage Devices in OrthodonticsNAVEEN ROYÎncă nu există evaluări
- Quality Control in Cone-Beam Computed Tomography (CBCT) Efomp-Estro-Iaea ProtocolDocument151 paginiQuality Control in Cone-Beam Computed Tomography (CBCT) Efomp-Estro-Iaea ProtocolWira Hadi KusumaÎncă nu există evaluări
- Marpe V SarpeDocument10 paginiMarpe V SarpeAngieÎncă nu există evaluări
- 2018 3D Family BrochureDocument27 pagini2018 3D Family BrochureSam Al AbabÎncă nu există evaluări
- Yxoss CBR: Customized Bone RegenerationDocument20 paginiYxoss CBR: Customized Bone RegenerationErdeli StefaniaÎncă nu există evaluări
- Date of Lecture Sheet Number Doctor Written by Corrected by Reference Sheets in 2013 (If Present)Document11 paginiDate of Lecture Sheet Number Doctor Written by Corrected by Reference Sheets in 2013 (If Present)Daniel AtiehÎncă nu există evaluări
- Villa Rotograph Evo 3d 2Document8 paginiVilla Rotograph Evo 3d 2Ahmad FakheroÎncă nu există evaluări
- Sjad 341Document9 paginiSjad 341Francisco ChourioÎncă nu există evaluări
- Guided Surgery in ImplantologyDocument101 paginiGuided Surgery in ImplantologynorwingÎncă nu există evaluări
- Iñaki Gamborena 2020Document19 paginiIñaki Gamborena 2020Ulises DiazÎncă nu există evaluări
- Diagnosis and Treatment PlanningDocument9 paginiDiagnosis and Treatment PlanningMohamed GabrÎncă nu există evaluări
- Fona Xpan 3D Plus: Operating InstructionsDocument44 paginiFona Xpan 3D Plus: Operating InstructionsAndrei ruÎncă nu există evaluări
- Three-Dimensional Imaging in Orthodontics: ReviewDocument9 paginiThree-Dimensional Imaging in Orthodontics: Reviewdrzana78Încă nu există evaluări
- Flapless Dental Implant Surgery With Surgical GuideDocument3 paginiFlapless Dental Implant Surgery With Surgical GuideImplant Surgical GuidesÎncă nu există evaluări
- Agreement Between 2D and 3D Radiographic Outcome Assessment 1 Year After Periapical SurgeryDocument11 paginiAgreement Between 2D and 3D Radiographic Outcome Assessment 1 Year After Periapical SurgeryMufidah NurulÎncă nu există evaluări
- Novel Intraoral Ultrasonography To Assess Midpalatal Suture AnatomyDocument2 paginiNovel Intraoral Ultrasonography To Assess Midpalatal Suture AnatomyRommy MelgarejoÎncă nu există evaluări
- The Use of Cone Beam Computer Tomography (CBCT) in EndodonticsDocument8 paginiThe Use of Cone Beam Computer Tomography (CBCT) in EndodonticsLorena MarinÎncă nu există evaluări
- Three-Dimensional Endodontic Guide For Adhesive Fiber Post Removal: A Dental TechniqueDocument4 paginiThree-Dimensional Endodontic Guide For Adhesive Fiber Post Removal: A Dental TechniqueLuisAlpalaÎncă nu există evaluări
- Basal Dental ImplantsDocument5 paginiBasal Dental ImplantsAlina AlbuÎncă nu există evaluări
- Considerations of Maxillary Tuberosity Fractures During Extraction of Upper Molars: A Literature ReviewDocument7 paginiConsiderations of Maxillary Tuberosity Fractures During Extraction of Upper Molars: A Literature Reviewsyawal reazzÎncă nu există evaluări
- Buccal ShelfDocument10 paginiBuccal ShelfGarimaa SurekaÎncă nu există evaluări
- Dental ClinicDocument36 paginiDental ClinicAly Sayed100% (3)