Documente Academic
Documente Profesional
Documente Cultură
PQCNC SIVB LS 1 Bucket List
Încărcat de
kcochran0 evaluări0% au considerat acest document util (0 voturi)
197 vizualizări16 paginiPQCNC Support for Intended Vaginal Birth Learning Session 1 - "The Bucket List' - or - Induction of Labor in the NTSV Patient
Drepturi de autor
© Attribution Non-Commercial (BY-NC)
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentPQCNC Support for Intended Vaginal Birth Learning Session 1 - "The Bucket List' - or - Induction of Labor in the NTSV Patient
Drepturi de autor:
Attribution Non-Commercial (BY-NC)
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
197 vizualizări16 paginiPQCNC SIVB LS 1 Bucket List
Încărcat de
kcochranPQCNC Support for Intended Vaginal Birth Learning Session 1 - "The Bucket List' - or - Induction of Labor in the NTSV Patient
Drepturi de autor:
Attribution Non-Commercial (BY-NC)
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 16
Primary focus of PQCNC SIVB initiative
MATERNAL RISKS LATER MATERNAL
ASSOCIATED WITH RISKS ASSOCIATED
CESAREAN SECTION WITH CS
•Hysterectomy
•Uterine Rupture
•Post partum hemorrhage
•Planning for timing
•Venous
and route of next
thromboembolism
•pregnancy
•Wound complications
•Placenta accreta
•Other surgical site
infections
•Decreased success at
breast feeding
•Hospital readmission
7804 NSTV
40% Induction rate
40.7% had cervical ripening**
Indications for induction
◦ Fetal indications 13.6%
◦ Fetal macrosomia 3.3%
◦ Maternal indications 24.9%
◦ “Post term” but less than 41weeks 14.3%
◦ Post term ≥ 41 weeks 18.3%
◦ Elective 25.6%
◦ Elective with cervical ripening 37%
◦ **BISHOP SCORE < 6
Indications for cesarean section
◦ Labor dystocia 75.1%
◦ Fetal distress 28.2%
◦ Maternal medical indication—1.6%
◦ “Other” 2.9%
◦ Labor dystocia 79.0% for induced, 68.9% for
spontaneous labor (p<0.05)
April 2010 Obstetrics &
Gynecology
FACTOR April 2010 Green Jl, 3) aOR
Black Race 1.44
≥35 years 1.71
BMI
< 18.5 Referent
18.5-24.9 1.36
25-29.9 1.96
30-39.9 3.24
≥40 4.51
Weight gain ≥18.14 kg 1.37
Gestational diabetes 1.38
Gestational hypertension 1.38
EGA ≥41 weeks 1.58
Induced labor 1.93
Multivariate Analysis
BlackRace aOR 1.35
Age 35 or older aOR 1.83
Wt gain >18.14kg aOR 1.28
Induced labor aOR 2.03
Restriction to NTSV with no
co-morbidities
29.9% induced overall
CS in 13.6% not induced, 25.5% induced
CONCLUSION: 20% of all CS
among low risk women and all
NSTV women could be attributed
to labor induction!!!!
Study of >200,000 deliveries >23 weeks, looked at
intended vaginal births across many hospitals, 2002-
2008
36.2% induction rate overall
Among intended vaginal births, induction rate was
43.8% (underestimate on birth certificate?)
Overall c-section rate was 30.5%, range 20%-44%
◦ C/S rate was 21.1% for those whose labor was induced
◦ C/S rate was 11.8% for those with spontaneous labor
Among nulliparous women with singleton, vertex
babies:
◦ C/S rate was 31.4% for those whose labor was induced
◦ C/S rate was 14.2% for those with spontaneous labor
Almost one-third of all C/S were prelabor repeats
47.1% of intrapartum C/S were performed for failure to
progress or cephalopelvic disproportion
27.3% were performed for nonreassuring fetal heart rate
Half of C/S for dystocia among inductions were done at
<6cm
◦ When is active labor? In nullips?
One-third of 2nd stage C/S were done <3 hours in nullips
One-fourth of 2nd stage C/S were done <2 hours in
multips
◦ This includes “decision-to-incision” time
C/S performed at earlier cervical dilations in induction
patients than in spontaneous labor patients
Almost 2/3 of overall CS attributed to 3 groups
with potentially modifiable risk factors:
◦ NTSV with induced labor
Review indications/processes for induction
◦ Previous CS and singleton cephalic term pregnancy
Provide VBAC
◦ Breech presentation
Offer ECV if appropriate
Contribution of select maternal groups to temporal trends in rates of caesarean
section. VM Allan. J Ob Gyn Can July 2010
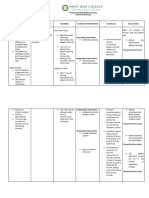
PATIENT EDUCATION
Establish practice
agreements about
elective inductions,
indicated inductions.
Communicate early on in
prenatal care the policy
of preferring
spontaneous labor,
essential ban on elective
inductions prior to 39
weeks.
38 weeks is too late to
have that conversation
and to expect to have
the patient on your team
What sort of analgesia
is available and how/
when is it administered
in labor?
What sort of labor support
is available? ALL LABORS
Do your unit’s MD, CNM
and nursing staff all
share a commitment to
promoting safe vaginal
birth for patients for
whom it is not contra-
indicated?
What labor curve do you
use in your unit and how
do you functionally define
“Failure to progress”?
What is the functional definition
of “LABOR” in your unit?
What is “active labor”?
SPONTANEOUS LABOR
What do you do
with “prodromal
labor”?
Discharge to home?
Therapeutic rest?
Induce?
When, how do you
augment labor?
Who gets induced?
Do you have a policy in your
practice, labor unit
regarding elective
inductions?
INDUCED LABORS
When do you
Induce?
What method(s) of
cervical ripening do
you use?
Who gets cervical
ripening?
What are you pitocin protocols?
Ideas for Quality Projects Around Induction
of Labor for NTSV: The “Bucket List”
•Look at your data to determine the vaginal delivery rate in
your NSTV population.
•What are the key drivers of your IOL rates?
•What are the key drives of your success rates in the
population of NSTV?
•What changes in these drivers are possible to design, vet
and test in 1-2 months?
•Identify 2-4 changes in these drivers that your team will
consider for further exploration during this project.
•If there are issues in spontaneously laboring patients that
are important drives of the C/S rate at your hospital,
consider those as well.
IOL POLICIES
No electives before 39 weeks
No electives with unripe cvx
Use of cervical ripening for indicated, unripe cvx
What kind of documentation required pre-induction
Functional definitions: Labor, prodrome, failure to
progress, failed induction
IOL PROCEDURES
Cervical ripening orders, methods
Pitocoin protocols
Labor support
Use of analgesia, anesthesia
AROM use
LABOR and DELIVERY CULTURE
Is there a will to improve this at your unit?
Are all doctors, CNM’s, and nurses committed?
Do you have a communication issue on your unit?
Are patients educated in general about expectations,
processes?
S-ar putea să vă placă și
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- PQCNC 2024 Kickoff Long Story Short 20240110Document26 paginiPQCNC 2024 Kickoff Long Story Short 20240110kcochranÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- PQCNC 2024 Initiative - Maternal SepsisDocument12 paginiPQCNC 2024 Initiative - Maternal SepsiskcochranÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- PQCNC 2024 Kickoff OB Sepsis Statewide Implementation 20240116Document33 paginiPQCNC 2024 Kickoff OB Sepsis Statewide Implementation 20240116kcochranÎncă nu există evaluări
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- PQCNC clOUDi LS2 OUD Pregnancy RyanDocument53 paginiPQCNC clOUDi LS2 OUD Pregnancy RyankcochranÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- PQCNC 2024 Initiative Maternal CardiacDocument30 paginiPQCNC 2024 Initiative Maternal CardiackcochranÎncă nu există evaluări
- PQCNC 2023 Supporting The Diagnosis and Treatment of Severe HTNDocument11 paginiPQCNC 2023 Supporting The Diagnosis and Treatment of Severe HTNkcochranÎncă nu există evaluări
- PQCNC 2023 Implementing Cardiac Bundle in NCDocument33 paginiPQCNC 2023 Implementing Cardiac Bundle in NCkcochranÎncă nu există evaluări
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- PQCNC 2023 Nutrition in PregnancyDocument12 paginiPQCNC 2023 Nutrition in PregnancykcochranÎncă nu există evaluări
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- PQCNC 2023 Standardizing The Care of Late-Preterm InfantsDocument17 paginiPQCNC 2023 Standardizing The Care of Late-Preterm InfantskcochranÎncă nu există evaluări
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- PQCNC clOUDi LS2 SUD Trauma PregnancyDocument31 paginiPQCNC clOUDi LS2 SUD Trauma PregnancykcochranÎncă nu există evaluări
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- PQCNC 2023 ClOUDi Continuation 2.0Document12 paginiPQCNC 2023 ClOUDi Continuation 2.0kcochranÎncă nu există evaluări
- PQCNC 2023 Safe SleepDocument13 paginiPQCNC 2023 Safe SleepkcochranÎncă nu există evaluări
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- PQCNC AIM RPC LS3 Data 20200303Document16 paginiPQCNC AIM RPC LS3 Data 20200303kcochranÎncă nu există evaluări
- PQCNC NHPC LS3 Noel 2020 Workload Indicators 20200310.Document23 paginiPQCNC NHPC LS3 Noel 2020 Workload Indicators 20200310.kcochranÎncă nu există evaluări
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- PQCNC 2023 Enhancing Perinatal Mental HealthDocument10 paginiPQCNC 2023 Enhancing Perinatal Mental HealthkcochranÎncă nu există evaluări
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- PQCNC 2023 Improving The Use of Mother's Milk at DischargeDocument8 paginiPQCNC 2023 Improving The Use of Mother's Milk at DischargekcochranÎncă nu există evaluări
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- PQCNC clOUDi Kickoff Main 2021Document27 paginiPQCNC clOUDi Kickoff Main 2021kcochranÎncă nu există evaluări
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- North Carolina Perinatal Quality Collaborative Initiative: Standardizing Perinatal Substance Use ScreeningDocument41 paginiNorth Carolina Perinatal Quality Collaborative Initiative: Standardizing Perinatal Substance Use ScreeningkcochranÎncă nu există evaluări
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- PQCNC clOUDi Kickoff Data 2021Document13 paginiPQCNC clOUDi Kickoff Data 2021kcochranÎncă nu există evaluări
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- PQCNC NHPC LS3 Vidant Panel 20200310Document4 paginiPQCNC NHPC LS3 Vidant Panel 20200310kcochranÎncă nu există evaluări
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- PQCNC NHPC LS3 NHRMC Acuity Presentation 20200310Document14 paginiPQCNC NHPC LS3 NHRMC Acuity Presentation 20200310kcochranÎncă nu există evaluări
- PQCNC NHPC LS3 Mccaffrey 20200310Document29 paginiPQCNC NHPC LS3 Mccaffrey 20200310kcochran100% (1)
- PQCNC NHPC LS3 Devente 20200310Document8 paginiPQCNC NHPC LS3 Devente 20200310kcochranÎncă nu există evaluări
- IV Fluids in The Mother Baby Unit: Meghan Dougherty, MDDocument8 paginiIV Fluids in The Mother Baby Unit: Meghan Dougherty, MDkcochranÎncă nu există evaluări
- PQCNC AIM RPC LS3 Ketner Posting 20200303Document41 paginiPQCNC AIM RPC LS3 Ketner Posting 20200303kcochranÎncă nu există evaluări
- PQCNC AIM RPC LS2 Scheduling To Improve Labor SupportDocument20 paginiPQCNC AIM RPC LS2 Scheduling To Improve Labor SupportkcochranÎncă nu există evaluări
- PQCNC AIM RPC LS2 Volunteer Doula ProgramDocument23 paginiPQCNC AIM RPC LS2 Volunteer Doula ProgramkcochranÎncă nu există evaluări
- Newborn Hypoglycemia Prevention and CareDocument30 paginiNewborn Hypoglycemia Prevention and CarekcochranÎncă nu există evaluări
- PQCNCNHPCLS2 FINALVidant Scheller 20191014Document22 paginiPQCNCNHPCLS2 FINALVidant Scheller 20191014kcochranÎncă nu există evaluări
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- PQCNC AIM RPC Spinning BabiesDocument71 paginiPQCNC AIM RPC Spinning Babieskcochran50% (2)
- Laporan Diagnosa Dan Kode Obgyn Bulan Feb & MaretDocument4 paginiLaporan Diagnosa Dan Kode Obgyn Bulan Feb & Maretreni riyantiÎncă nu există evaluări
- Mohammed Gogandy - Puerperium History Sheet & - 40 2007-2008& - 41 PDFDocument2 paginiMohammed Gogandy - Puerperium History Sheet & - 40 2007-2008& - 41 PDFJennifer Ross-ComptisÎncă nu există evaluări
- Clinical Findings: ACOG - Cervical Insufficiency As "Document5 paginiClinical Findings: ACOG - Cervical Insufficiency As "lllÎncă nu există evaluări
- NCP Estoesta DystociaDocument3 paginiNCP Estoesta DystociaKyle Albert EstoestaÎncă nu există evaluări
- ACOG Committee Opinion No. 743 Low-Dose Aspirin Use During PregnancyDocument9 paginiACOG Committee Opinion No. 743 Low-Dose Aspirin Use During PregnancyJaime RdÎncă nu există evaluări
- Multiple PregnancyDocument32 paginiMultiple PregnancyRebbeccah NafulaÎncă nu există evaluări
- Chinese Lunar Calendar Baby Gender PredictionDocument3 paginiChinese Lunar Calendar Baby Gender Predictionanand2k1Încă nu există evaluări
- Uterine RuptureDocument40 paginiUterine Rupturevalpretl100% (1)
- Partograph - PPT 1Document46 paginiPartograph - PPT 1sky rainÎncă nu există evaluări
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Multifetal Pregnancy: Amr Nadim, MDDocument36 paginiMultifetal Pregnancy: Amr Nadim, MDsharenÎncă nu există evaluări
- OB SottoDocument2 paginiOB SottoSophia VeralloÎncă nu există evaluări
- The Pathology of Placenta Accreta, A Worldwide EpidemicDocument6 paginiThe Pathology of Placenta Accreta, A Worldwide EpidemicYoga ParipurnaÎncă nu există evaluări
- Abortion TypesDocument19 paginiAbortion TypesFany MaldoÎncă nu există evaluări
- Skills - Care of The Pregnant Patient ComputationsDocument5 paginiSkills - Care of The Pregnant Patient ComputationsMichelle HutamaresÎncă nu există evaluări
- A Comparative Study of Teenage Pregnancy: S. H. Mahavarkar, C. K. Madhu & V. D. MuleDocument4 paginiA Comparative Study of Teenage Pregnancy: S. H. Mahavarkar, C. K. Madhu & V. D. MuleGeorgiana DÎncă nu există evaluări
- Ayantu MekonnenDocument30 paginiAyantu Mekonnenmbgeletu1221Încă nu există evaluări
- NCP - Gestational HypertensionDocument3 paginiNCP - Gestational HypertensionCameron De GuzmanÎncă nu există evaluări
- Prolonged LaborDocument6 paginiProlonged LaborBqSafinatun NajaÎncă nu există evaluări
- Ta Daftar PustakaDocument2 paginiTa Daftar PustakaNovi KartikadewiÎncă nu există evaluări
- Kuliah IUGR PPDS 2023Document48 paginiKuliah IUGR PPDS 2023Fransisko ReinardÎncă nu există evaluări
- Iugr FinalDocument35 paginiIugr Finalsanthiyasandy100% (4)
- OBGYN Student Study GuideDocument39 paginiOBGYN Student Study GuideGoffo13100% (4)
- NFDN 2004 Prenatal Teaching Plan Version A V1.22.2Document3 paginiNFDN 2004 Prenatal Teaching Plan Version A V1.22.2ᅮᅮAmalÎncă nu există evaluări
- Leong Et Al-2004-BJOG: An International Journal of Obstetrics & GynaecologyDocument2 paginiLeong Et Al-2004-BJOG: An International Journal of Obstetrics & GynaecologyAngie MandeoyaÎncă nu există evaluări
- The Role of Parity in The Mode of DeliveryDocument11 paginiThe Role of Parity in The Mode of DeliveryKanuyasa GekzÎncă nu există evaluări
- WNHS OG PregnancyFirstTrimesterDocument60 paginiWNHS OG PregnancyFirstTrimesterBharata YudhaÎncă nu există evaluări
- LaborDocument16 paginiLaborREALYN ZAMBASÎncă nu există evaluări
- 10 - 15 - Infectia Cailor Urinare La Gravide.Document6 pagini10 - 15 - Infectia Cailor Urinare La Gravide.MihaiÎncă nu există evaluări
- Preventing Unsafe Abortion and Its Consequences Guttmacher InstituteDocument254 paginiPreventing Unsafe Abortion and Its Consequences Guttmacher InstituteGaby ArguedasÎncă nu există evaluări
- NASKAH PUBLIKASI NurfadilahDocument10 paginiNASKAH PUBLIKASI Nurfadilahfauziah nurÎncă nu există evaluări
- Healing PCOS: A 21-Day Plan for Reclaiming Your Health and Life with Polycystic Ovary SyndromeDe la EverandHealing PCOS: A 21-Day Plan for Reclaiming Your Health and Life with Polycystic Ovary SyndromeÎncă nu există evaluări
- All in Her Head: The Truth and Lies Early Medicine Taught Us About Women’s Bodies and Why It Matters TodayDe la EverandAll in Her Head: The Truth and Lies Early Medicine Taught Us About Women’s Bodies and Why It Matters TodayEvaluare: 4.5 din 5 stele4.5/5 (3)
- The Longevity Book: The Science of Aging, the Biology of Strength, and the Privilege of TimeDe la EverandThe Longevity Book: The Science of Aging, the Biology of Strength, and the Privilege of TimeEvaluare: 3.5 din 5 stele3.5/5 (13)
- The Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouDe la EverandThe Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouÎncă nu există evaluări
- What to Expect When You’re Expecting (5th Edition)De la EverandWhat to Expect When You’re Expecting (5th Edition)Evaluare: 5 din 5 stele5/5 (1)
- Skinny Bitch: A No-Nonsense, Tough-Love Guide for Savvy Girls Who Want to Stop Eating Crap and Start Looking Fabulous!De la EverandSkinny Bitch: A No-Nonsense, Tough-Love Guide for Savvy Girls Who Want to Stop Eating Crap and Start Looking Fabulous!Evaluare: 3.5 din 5 stele3.5/5 (489)
- Awakening Fertility: The Essential Art of Preparing for PregnancyDe la EverandAwakening Fertility: The Essential Art of Preparing for PregnancyEvaluare: 4.5 din 5 stele4.5/5 (36)
- Intoxicating Lies: One Woman’s Journey to Freedom from Gray Area DrinkingDe la EverandIntoxicating Lies: One Woman’s Journey to Freedom from Gray Area DrinkingEvaluare: 5 din 5 stele5/5 (1)
- Natural Hospital Birth: The Best of Both WorldsDe la EverandNatural Hospital Birth: The Best of Both WorldsEvaluare: 5 din 5 stele5/5 (33)