Documente Academic
Documente Profesional
Documente Cultură
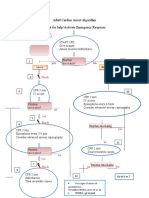
ACLS Cardiac Arrest Algorithm For Suspected or Confirmed COVID-19 Patients
Încărcat de
Deny PamungkasTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
ACLS Cardiac Arrest Algorithm For Suspected or Confirmed COVID-19 Patients
Încărcat de
Deny PamungkasDrepturi de autor:
Formate disponibile
ACLS Cardiac Arrest Algorithm 8
for Suspected or Confirmed COVID-19 Patients C
P
Updated April 2020 A R
Don PPE
• Limit personnel 2
• Consider resuscitation appropriateness
1 m
Start CPR i
• Give oxygen (limit aerosolization) n
• Attach monitor/defibrillator • Amiodarone or
• Prepare to intubate lidocaine
• Treat reversible
causes
Yes Rhythm No 12
2 shockable?
9
VF/pVT Asystole/PEA
3 © 2020 American Heart Association
Shock
B
Prioritize Intubation / Resume CPR
• Pause chest compressions for intubation
• If intubation delayed, consider supraglottic airway or bag-mask device with filter and tight seal
• Connect to ventilator with filter when possible
4 10
CPR 2 min CPR 2 min
IV/IO access • IV/IO access
• Epinephrine every 3-5 min
• Consider mechanical
compression device
Rhythm No Rhythm Yes
shockable? shockable?
Yes
5
Shock No
6 11
CPR 2 min CPR 2 min
• Epinephrine every 3-5 min Treat reversible causes
• Consider mechanical
compression device
Rhythm No No Rhythm Yes
shockable? shockable?
Yes
7
Shock
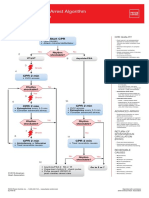
CPR Quality
• Push hard (at least 2 inches [5 cm]) and fast (100-120/min) and allow complete chest recoil.
• Minimize interruptions in compressions.
• Avoid excessive ventilation.
• Change compressor every
2 minutes, or sooner if fatigued.
• If no advanced airway, 30:2 compression-ventilation ratio.
• Quantitative waveform capnography
– If Petco2 <10 mm Hg, attempt to improve CPR quality.
• Intra-arterial pressure
– If relaxation phase (diastolic) pressure <20 mm Hg, attempt to improve CPR quality.
Shock Energy for Defibrillation
• Biphasic: Manufacturer recommendation (eg, initial dose of 120-200 J); if unknown, use maximum available.
Second and subsequent doses should be equivalent, and higher doses may be considered.
• Monophasic: 360 J
Advanced Airway
• Minimize closed-circuit disconnection
• Use intubator with highest likelihood of first pass success
• Consider video laryngoscopy
• Endotracheal intubation or supraglottic advanced airway
• Waveform capnography or capnometry to confirm and monitor ET tube placement
• Once advanced airway in place, give 1 breath every 6 seconds (10 breaths/min) with continuous chest compressions
Drug Therapy
• Epinephrine IV/IO dose:
1 mg every 3-5 minutes
• Amiodarone IV/IO dose: First
dose: 300 mg bolus. Second
dose: 150 mg. or
Lidocaine IV/IO dose:
First dose: 1-1.5 mg/kg. Second
dose: 0.5-0.75 mg/kg.
Return of Spontaneous Circulation (ROSC)
• Pulse and blood pressure
• Abrupt sustained increase in Petco2 (typically ≥40 mm Hg)
• Spontaneous arterial pressure waves with intra-arterial monitoring
Reversible Causes
• Hypovolemia
• Hypoxia
• Hydrogen ion (acidosis)
• Hypo-/hyperkalemia
• Hypothermia
• Tension pneumothorax
• Tamponade, cardiac
• Toxins
• Thrombosis, pulmonary
• Thrombosis, coronary
S-ar putea să vă placă și
- Acls 2023Document5 paginiAcls 2023Mohamed Helal100% (5)
- ACLS Pocket Card PDFDocument6 paginiACLS Pocket Card PDFdang vu hoang ducÎncă nu există evaluări
- ECG-Dr - Najeeb-By Kurdish Medico PDFDocument265 paginiECG-Dr - Najeeb-By Kurdish Medico PDFMarwa Ahmad Abdelmohsen75% (4)
- Medical Terminology Cardiovascular SystemDocument35 paginiMedical Terminology Cardiovascular Systemapi-26819951486% (7)
- Adult Cardiac Arrest Algorithm: VF/PVT Asystole/PEADocument8 paginiAdult Cardiac Arrest Algorithm: VF/PVT Asystole/PEAVitor Hugo100% (2)
- Checklist & Algoritma ACLSDocument16 paginiChecklist & Algoritma ACLSNadhif JovaldyÎncă nu există evaluări
- Advanced Cardiac ArrestDocument1 paginăAdvanced Cardiac ArrestDebbie MeyerÎncă nu există evaluări
- Algo ArrestDocument2 paginiAlgo ArrestLocomotorica FK UkiÎncă nu există evaluări
- Caring For Cardiac Arrest: Basic Life Support - AdultDocument4 paginiCaring For Cardiac Arrest: Basic Life Support - AdultLuigi Ricardo BallerasÎncă nu există evaluări
- Acls Study Guide 2016Document2 paginiAcls Study Guide 2016nova939100% (2)
- Figure 4 AlgorithmACLS CACOVID 220101Document1 paginăFigure 4 AlgorithmACLS CACOVID 220101AndhikaÎncă nu există evaluări
- Wa0000.Document7 paginiWa0000.benitez1228Încă nu există evaluări
- 2-Cardiac Arrest AlgrthmDocument1 pagină2-Cardiac Arrest AlgrthmterminallllÎncă nu există evaluări
- Heart: Car I Car Est, Hyt Ias, A Eir Eat E TDocument2 paginiHeart: Car I Car Est, Hyt Ias, A Eir Eat E TatdesamparadÎncă nu există evaluări
- Adult Cardiac Arrest AlgoritmaDocument1 paginăAdult Cardiac Arrest AlgoritmaYouniehacibie Ichisky ChildÎncă nu există evaluări
- Algo Pals Pediatric Cardiac ArrestDocument1 paginăAlgo Pals Pediatric Cardiac Arrestpedjoang fkupr2017Încă nu există evaluări
- Cardiac Arrest Algorithm: Give OxygenDocument2 paginiCardiac Arrest Algorithm: Give OxygenJunius SimarmataÎncă nu există evaluări
- Algorithms of AHA 2020Document23 paginiAlgorithms of AHA 2020Emirhan llkhanÎncă nu există evaluări
- Adult Cardiac Arrest Circular Algorithm: Monitor CPR QualityDocument1 paginăAdult Cardiac Arrest Circular Algorithm: Monitor CPR QualityChris LeeÎncă nu există evaluări
- Adult Cardiac Arrest Circular Algorithm: Monitor CPR QualityDocument1 paginăAdult Cardiac Arrest Circular Algorithm: Monitor CPR QualityAlexis HospitalÎncă nu există evaluări
- Cardiac Arrest VF/Pulseless VT Learning Station ChecklistDocument5 paginiCardiac Arrest VF/Pulseless VT Learning Station ChecklistMaryam FadahÎncă nu există evaluări
- Shock: Shout For Help/Activate Emergency ResponseDocument6 paginiShock: Shout For Help/Activate Emergency ResponseandiyanimalikÎncă nu există evaluări
- Adult Asystole or PeaDocument1 paginăAdult Asystole or PeamayÎncă nu există evaluări
- Algo Pals Pediatric Cardiac ArrestDocument1 paginăAlgo Pals Pediatric Cardiac ArrestDevi ChrestellaÎncă nu există evaluări
- Acls FixDocument20 paginiAcls Fixluthfi adityaÎncă nu există evaluări
- Advance Life Support MaterialDocument2 paginiAdvance Life Support MaterialmayÎncă nu există evaluări
- Algorithm-ACLS CA 200731Document1 paginăAlgorithm-ACLS CA 200731Hyunsoo EllisÎncă nu există evaluări
- Advanced Cardiac Life SupportDocument37 paginiAdvanced Cardiac Life SupportRoy Acosta GumbanÎncă nu există evaluări
- Checklist & Algoritma ACLSDocument16 paginiChecklist & Algoritma ACLSNadhif JovaldyÎncă nu există evaluări
- Adult Advanced Life Support Algorithm 2021 Aug 2023Document1 paginăAdult Advanced Life Support Algorithm 2021 Aug 2023cknihilnewÎncă nu există evaluări
- AiepiDocument12 paginiAiepiRenzo Iván Marín DávalosÎncă nu există evaluări
- AHA PALS AlgorithmsDocument2 paginiAHA PALS AlgorithmsGulrejÎncă nu există evaluări
- Adult Cardiac Arrest Algorithm Shout For Help/activate Emergency ResponseDocument1 paginăAdult Cardiac Arrest Algorithm Shout For Help/activate Emergency ResponseICU RSBMÎncă nu există evaluări
- Actual SoapiesDocument8 paginiActual SoapiesBeverlyn AsparoÎncă nu există evaluări
- Pulseless Ventricular Tachycardia/Ventricular Fibrillation Algorithm (Figure 8-5)Document1 paginăPulseless Ventricular Tachycardia/Ventricular Fibrillation Algorithm (Figure 8-5)Dyan IslamiÎncă nu există evaluări
- ACLS 2015 Algorithm and Anesthesia ACLS PDFDocument14 paginiACLS 2015 Algorithm and Anesthesia ACLS PDFTaufiqurrahman RizkiÎncă nu există evaluări
- For Healthcare Providers Quick Reference: Ard - PushDocument2 paginiFor Healthcare Providers Quick Reference: Ard - Pushزياد داودÎncă nu există evaluări
- Adult Immediate Post Cardiac Arrest Care Algorithm 2015 UpdateDocument1 paginăAdult Immediate Post Cardiac Arrest Care Algorithm 2015 UpdateRyggie Comelon0% (1)
- Poster 10 PALS 01 01 ENG V20100927 PDFDocument1 paginăPoster 10 PALS 01 01 ENG V20100927 PDFAndy XiaoÎncă nu există evaluări
- Pals TachycardiaDocument1 paginăPals TachycardiadarlingcarvajalduqueÎncă nu există evaluări
- Reanimacion CardiopulmonarDocument15 paginiReanimacion CardiopulmonarVictoriano ValienteÎncă nu există evaluări
- Acute Coronary SyndromeDocument7 paginiAcute Coronary SyndromePuskesmas Pinang JayaÎncă nu există evaluări
- Веб-страница 2Document1 paginăВеб-страница 2Zalina IvanovaÎncă nu există evaluări
- ACLS - Guidelines From 2005USADocument62 paginiACLS - Guidelines From 2005USAsbontchevÎncă nu există evaluări
- Paediatric Advanced Life Support: Call For Help 2222 Commence/continue CPR (5 Initial Breaths Then CV Ratio 15:2)Document1 paginăPaediatric Advanced Life Support: Call For Help 2222 Commence/continue CPR (5 Initial Breaths Then CV Ratio 15:2)Vijay RÎncă nu există evaluări
- 8-Adult Advanced Life Support Algorithm 2021Document1 pagină8-Adult Advanced Life Support Algorithm 2021khaledÎncă nu există evaluări
- Cardiac Arrest Circular Algorithm: Start CPR 2 M IN UT ESDocument1 paginăCardiac Arrest Circular Algorithm: Start CPR 2 M IN UT ESjohndoe1995Încă nu există evaluări
- Cardiac Arrest Vtach and VfibDocument1 paginăCardiac Arrest Vtach and VfibBelle A. BasilioÎncă nu există evaluări
- Acls PDFDocument2 paginiAcls PDFKyrie Diosabeth TumbagaÎncă nu există evaluări
- AclsDocument1 paginăAclsJoice DasÎncă nu există evaluări
- Advanced Paediatric Life Support - A0 PDFDocument1 paginăAdvanced Paediatric Life Support - A0 PDFiulia-uroÎncă nu există evaluări
- ACLS 2020 Algorithms: American Heart Association 2020 GuidelinesDocument8 paginiACLS 2020 Algorithms: American Heart Association 2020 GuidelinesNofi Nurina100% (4)
- Managemen Disritmia: Dr. Rofika Hanifa, SPPDDocument20 paginiManagemen Disritmia: Dr. Rofika Hanifa, SPPDavivlabirdÎncă nu există evaluări
- Algo Pals TachycardiaDocument1 paginăAlgo Pals TachycardiaArdie FratamaÎncă nu există evaluări
- ACLSDocument275 paginiACLSShajahan SideequeÎncă nu există evaluări
- Pediatric Cardiac Arrest Algorithm-2015 UpdateDocument2 paginiPediatric Cardiac Arrest Algorithm-2015 UpdateKholida UlfaÎncă nu există evaluări
- AlgorithmACLS Tachycardia 200612Document1 paginăAlgorithmACLS Tachycardia 200612must dietÎncă nu există evaluări
- PALSposterDocument1 paginăPALSposterJose SesmeroÎncă nu există evaluări
- Advanced Cardiac Life Support Quick Study Guide 2015 Updated GuidelinesDe la EverandAdvanced Cardiac Life Support Quick Study Guide 2015 Updated GuidelinesEvaluare: 4 din 5 stele4/5 (6)
- 2021 AHA ASA Guideline For The Prevention of Stroke in Patients With Stroke and TIA Clinical UpdateDocument43 pagini2021 AHA ASA Guideline For The Prevention of Stroke in Patients With Stroke and TIA Clinical UpdateLê Thị HươngÎncă nu există evaluări
- Aneurysmal Disease of The Thoracic and Abdominal Aorta PDFDocument240 paginiAneurysmal Disease of The Thoracic and Abdominal Aorta PDFRAUL EDUARDO GUTIERREZ COITIÑO100% (1)
- Brar 2014Document10 paginiBrar 2014Ismael Rivera DiazÎncă nu există evaluări
- London Core Review Course - (Thurs 18 May - Sun 21 May 2017) - TimetableDocument5 paginiLondon Core Review Course - (Thurs 18 May - Sun 21 May 2017) - Timetablelondon_core_reviewÎncă nu există evaluări
- Atkinson Et Al 2017 Cardiovascular and Ventilatory Consequences of Laparoscopic SurgeryDocument11 paginiAtkinson Et Al 2017 Cardiovascular and Ventilatory Consequences of Laparoscopic Surgeryedu.b.marqueÎncă nu există evaluări
- Cardiac Arrest Pada Setting Icu: Pembimbing: Dr. Tommy Nugroho, SpanDocument38 paginiCardiac Arrest Pada Setting Icu: Pembimbing: Dr. Tommy Nugroho, SpanYeltserÎncă nu există evaluări
- Anatomy MCQDocument9 paginiAnatomy MCQMido TooÎncă nu există evaluări
- Case 27 (LC Fix)Document14 paginiCase 27 (LC Fix)galih suharno0% (1)
- Cardiac - Asthma - Elderly PPT Asma PDFDocument22 paginiCardiac - Asthma - Elderly PPT Asma PDFAfif AuliyaÎncă nu există evaluări
- Consenso Latinoamericano de Hipertension Arterial 1 PDFDocument47 paginiConsenso Latinoamericano de Hipertension Arterial 1 PDFcarlos ujedaÎncă nu există evaluări
- How An AED WorksDocument1 paginăHow An AED WorksKelley StewartÎncă nu există evaluări
- Ekg Plain and Simple 4th Edition Ellis Test BankDocument35 paginiEkg Plain and Simple 4th Edition Ellis Test Banknicoledickersonwmncpoyefk100% (18)
- A Case Study On Ischemic Stroke: J.H. Cerilles State CollegeDocument21 paginiA Case Study On Ischemic Stroke: J.H. Cerilles State CollegeNicole Aranding100% (4)
- Coronary CirculationDocument47 paginiCoronary CirculationSuresh KumarÎncă nu există evaluări
- Digoxin Intoxication & Pericarditis.Document25 paginiDigoxin Intoxication & Pericarditis.louirufi3003Încă nu există evaluări
- Histology of Heart Conducting SystemDocument9 paginiHistology of Heart Conducting SystemTasya AuliaÎncă nu există evaluări
- Perioperative Cardiovascular Evaluation For Noncardiac SurgeryDocument46 paginiPerioperative Cardiovascular Evaluation For Noncardiac SurgeryErinne DefrianiÎncă nu există evaluări
- Antianginal Drugs - Classification and MechanismDocument1 paginăAntianginal Drugs - Classification and MechanismAhmed YT100% (1)
- Basic Ecg InterpratationDocument71 paginiBasic Ecg Interpratationgunawan susantoÎncă nu există evaluări
- PDF Passive Leg Raise PLR Test Stroke Volume Index SviDocument3 paginiPDF Passive Leg Raise PLR Test Stroke Volume Index SviNama ManaÎncă nu există evaluări
- Endovascular Versus Surgical Revascularization For Acute Limb IschemiaDocument9 paginiEndovascular Versus Surgical Revascularization For Acute Limb IschemiaSisca Dwi AgustinaÎncă nu există evaluări
- Ventricular and Atrial Fibrillation and FlutterDocument21 paginiVentricular and Atrial Fibrillation and Flutteryasir ishaqÎncă nu există evaluări
- Lecturio ComDocument7 paginiLecturio ComAlex Ivan Chen TejadaÎncă nu există evaluări
- Curs 9 Myocarditis CardiomyopathyDocument41 paginiCurs 9 Myocarditis CardiomyopathyIliescu DenisaÎncă nu există evaluări
- TOG 2007 915-20 Review Cardiac Disease in Pregnancy Part 1 CongenitalDocument6 paginiTOG 2007 915-20 Review Cardiac Disease in Pregnancy Part 1 Congenitalsaeed hasan saeedÎncă nu există evaluări
- Correlation Between Hba1c Level and Epicardial Fat Thickness in Acute Coronary Syndrome PatientDocument5 paginiCorrelation Between Hba1c Level and Epicardial Fat Thickness in Acute Coronary Syndrome PatientIJAR JOURNALÎncă nu există evaluări
- NCM 101 Vital Signs PPT BSN 1a Group 1Document138 paginiNCM 101 Vital Signs PPT BSN 1a Group 1Brian Anthony100% (1)
- Diagnostic Angiography SOPDocument2 paginiDiagnostic Angiography SOPQuality Assurance DepartmentÎncă nu există evaluări