Documente Academic
Documente Profesional
Documente Cultură
103 108 PDF
Încărcat de
Matiyas ZewdeTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
103 108 PDF
Încărcat de
Matiyas ZewdeDrepturi de autor:
Formate disponibile
Research and Reviews
History of Antimicrobial Agents and Resistant
Bacteria
JMAJ 52(2): 103–108, 2009
Tomoo SAGA,*1 Keizo YAMAGUCHI*2
Abstract
Antimicrobial chemotherapy has conferred huge benefits on human health. A variety of microorganisms were
elucidated to cause infectious diseases in the latter half of the 19th century. Thereafter, antimicrobial chemo-
therapy made remarkable advances during the 20th century, resulting in the overly optimistic view that infectious
diseases would be conquered in the near future. However, in response to the development of antimicrobial
agents, microorganisms that have acquired resistance to drugs through a variety of mechanisms have emerged
and continue to plague human beings. In Japan, as in other countries, infectious diseases caused by drug-
resistant bacteria are one of the most important problems in daily clinical practice. In the current situation, where
multidrug-resistant bacteria have spread widely, options for treatment with antimicrobial agents are limited, and
the number of brand new drugs placed on the market is decreasing. Since drug-resistant bacteria have been
selected by the use of antimicrobial drugs, the proper use of currently available antimicrobial drugs, as well as
efforts to minimize the transmission and spread of resistant bacteria through appropriate infection control, would
be the first step in resolving the issue of resistant organisms.
Key words Antimicrobial agents, Resistant bacteria, History
not achieve beneficial effect, and moreover,
Introduction may lead to a worse prognosis. In addition, in
a situation where multidrug-resistant organisms
Antimicrobial drugs have caused a dramatic have spread widely, there may be quite a limited
change not only of the treatment of infectious choice of agents for antimicrobial therapy. At
diseases but of a fate of mankind. Antimicrobial present, fewer brand new antimicrobial agents
chemotherapy made remarkable advances, result- are coming onto the market. Considering this
ing in the overly optimistic view that infectious situation together with the increasing awareness
diseases would be conquered in the near future. of drug safety, we are now facing a situation of
However, in reality, emerging and re-emerging severely limited options among antimicrobial
infectious diseases have left us facing a counter- agents.
charge from infections. Infections with drug- This paper provides an outline of the history
resistant organisms remain an important problem of antimicrobial agents, and thereafter describes
in clinical practice that is difficult to solve. resistant organisms that have emerged in response
If an improper antimicrobial agent happens to antimicrobial agents and discusses practical
to be chosen for the treatment of infection with clues to prevent resistant microorganisms.
drug-resistant microorganisms, the therapy may
*1 Assistant Professor, Department of Microbiology and Infectious Disease, Faculty of Medicine, Toho University, Tokyo, Japan
(sagatomoo@med.toho-u.ac.jp).
*2 Professor, Department of Microbiology and Infectious Disease, Faculty of Medicine, Toho University, Tokyo, Japan.
This article is a revised English version of a paper originally published in the Journal of the Japan Medical Association (Vol.137, No.3, 2008,
pages 513–517).
JMAJ, March / April 2009 — Vol. 52, No. 2 103
Saga T, Yamaguchi K
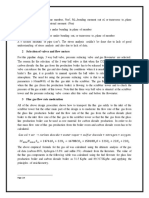
Emergence of drug-resistant bacteria Development of antimicrobial agents
Discovery of penicillin
Discovery of a sulfonamide
Clinical application of penicillin
Emergence of penicillinase-producing
Staphylococcus aureus Discovery of aminoglycoside, chloramphenicol,
tetracycline, and macrolide
Emergence and spread of multidrug-resistant
S. aureus Discovery of vancomycin
Synthesis of methicillin
Emergence of MRSA
Synthesis of nalidixic acid
Emergence of PISP Development of first-generation cephems
Emergence of penicillinase-producing
H. influenzae Development of second-generation cephems
Emergence of PRSP
Emergence of BLNAR H. influenzae Development of third-generation cephems
Emergence of ESBL-producing Gram-negative
Development of carbapenem Development of
bacilli
and monobactam new quinolones
Emergence of VRE
Increased infections with MRSA, PRSP, BLNAR,
etc. Increased use of third-generation
Increase of resistant gonococci cephem, carbapenem, oral cephem, and
new quinolone antimicrobials
Increase of MDRP
Increase of quinolone-resistant E. coli (Decrease in newly developed antimicrobial agents)
Fig. 1 Trend of development of antimicrobial agents and emergence of drug-resistant bacteria
nated blue mold (a fungus from the Penicillium
History of the Development of genus) in culture dishes, leading to the finding
Antimicrobial Agents1,2 (Fig. 1) that a microorganism would produce substances
that could inhibit the growth of other micro-
Looking back on the history of human diseases, organisms. The antibiotic was named penicillin,
infectious diseases have accounted for a very large and it came into clinical use in the 1940s. Peni-
proportion of diseases as a whole. It was not until cillin, which is an outstanding agent in terms
the latter half of the 19th century that micro- of safety and efficacy, led in the era of antimicro-
organisms were found to be responsible for a bial chemotherapy by saving the lives of many
variety of infectious diseases that had been plagu- wounded solders during World War II.
ing humanity from ancient days. Accordingly, During the subsequent two decades, new classes
chemotherapy aimed at the causative organisms of antimicrobial agents were developed one after
was developed as the main therapeutic strategy. another, leading to a golden age of antimicrobial
The first antimicrobial agent in the world was chemotherapy. In 1944, streptomycin, an amino-
salvarsan, a remedy for syphilis that was synthe- glycoside antibiotic, was obtained from the soil
sized by Ehrlich in 1910. In 1935, sulfonamides bacterium Streptomyces griseus. Thereafter, chlor-
were developed by Domagk and other researchers. amphenicol, tetracycline, macrolide, and glyco-
These drugs were synthetic compounds and had peptide (e.g., vancomycin) were discovered from
limitations in terms of safety and efficacy. soil bacteria. The synthesized antimicrobial agent
In 1928, Fleming discovered penicillin. He nalidixic acid, a quinolone antimicrobial drug,
found that the growth of Staphylococcus aureus was obtained in 1962.
was inhibited in a zone surrounding a contami- Improvements in each class of antimicrobial
104 JMAJ, March / April 2009 — Vol. 52, No. 2
HISTORY OF ANTIMICROBIAL AGENTS AND RESISTANT BACTERIA
Penicillin antimicrobials Quinolone antimicrobials
Nalidixic acid
Penicillin G
Ampicillin
Norfloxacin
Methicillin
Levofloxacin
Piperacillin
Fig. 2 Evolution of antimicrobial agents (penicillin and quinolone antimicrobials)
agents continued to achieve a broader antimicro- microbial spectra. First-generation cephems (cefaz-
bial spectrum and higher antimicrobial activity. - olin, etc.) are effective only for Gram-positive
lactam antibiotics will be described as an example. organisms and Escherichia coli, although their
The -lactam antibiotics include penicillins (Fig. 2), antimicrobial activity against these organisms is
cephems, carbapenems, and monobactams. potent. Second-generation cephems (cefotiam,
Penicillins were originally effective for Gram- etc.) have an extended antimicrobial spectrum
positive organisms such as S. aureus. Later, to that covers not only Gram-positive but also Gram-
address penicillin-resistant S. aureus which pro- negative organisms including other Enterobacte-
duces the penicillin-hydrolysing enzyme penicil- riaceae. Third-generation cephems (ceftazidime,
linase, methicillin was developed. On the other cefotaxime, etc.) have higher efficacy for Gram-
hand, attempts to expand the antimicrobial spec- negative organisms, and some drugs of this
trum yielded ampicillin, which is also effective for generation are also effective for P. aeruginosa,
Gram-negative Enterobacteriaceae, and piper- although the antimicrobial activity against Gram-
acillin, which is effective even for Pseudomonas positive organisms is generally lower than that of
aeruginosa. the first generation.
Cephems were developed in the 1960s, and Carbapenem is an antibiotic class including
came into widespread use. Cephems are classified panipenem, imipenem, and meropenem. These
into several generations according to their anti- drugs are effective not only for Gram-positive
JMAJ, March / April 2009 — Vol. 52, No. 2 105
Saga T, Yamaguchi K
Table 1 Clinically important drug-resistant bacteria in Japan
Microorganisms Drugs Resistant bacteria Mechanism of resistance
Staphylococcus -lactam MRSA Production of an additional enzyme that avoids drug
aureus (methicillin) binding (PBP2’)
Vancomycin VISA Thickening of cell wall
(VRSA) Consequent changes in target (vanA, vanB, etc.)
Enterococcus Vancomycin VRE Consequent changes in target (vanA, vanB, etc.)
Streptococcus Penicillin PISP/PRSP Mutation in target (PBP)
pneumoniae
Macrolide Macrolide-resistant Modification of target (erm )
S. pneumoniae Drug efflux pump (mef )
Haemophilus Ampicillin BLNAR Mutation in target (PBP)
influenzae
Pseudomonas Multiple drugs MDRP Multiple factors including loss of porin, drug efflux
aeruginosa pump, and drug-modifying enzyme
Metallo--lactamase- Drug-degrading enzyme
producing bacteria
Enterobacteriaceae -lactam ESBL-producing Drug-degrading enzyme
(e.g., Escherichia coli ) (carbapenem) bacteria
Quinolone Quinolone-resistant Mutation in target (gyrA, parC )
E. coli
Gonococci Quinolone Quinolone-resistant Mutation in target (gyrA, parC )
gonococci
and Gram-negative bacteria but also anaerobes, was metabolized rapidly in the human body.
and their antimicrobial activity is strong. The In contrast, norfloxacin, which came to market
monobactam antibiotic aztreonam exerts an anti- in 1984, maintains a stable metabolic state and
microbial effect only on Gram-negative bacteria. exhibits good tissue distribution. Its antimicro-
Continuing improvements have been made for bial spectrum is extensive, covering both Gram-
antimicrobial agents in various aspects in addi- positive and Gram-negative bacteria including
tion to the antimicrobial spectrum and activity. P. aeruginosa. Quinolone antimicrobials developed
The drugs have been developed to achieve better after norfloxacin have been called new quinolones,
pharmacodynamics including the absorption of and they have still been key drugs. Levofloxacin
oral drugs, concentration in the blood, and distri- is the S-(ⳮ) enantiomer of the new quinolone
bution to the inflammatory focus. In addition, as ofloxacin. This enantiomer has higher antimicro-
antimicrobial chemotherapy has been established bial activity than that of the other R-(Ⳮ) enanti-
and matured, more importance has been attached omer of ofloxacin, and is associated with weaker
to the drug safety. Antimicrobial agents that are side effects on the central nervous system, such as
associated with serious side effects have been restlessness and vertigo.
replaced by other safer drugs. Although a large number of companies in
Quinolone antimicrobials represent an example various countries have competed in the develop-
of drugs with improved pharmacodynamics and ment of newer antimicrobial agents, the number
safety (Fig. 2). Nalidixic acid, the first drug of of brand new drugs has been remarkably decreas-
this class, was active only against Gram-negative ing in recent years, with few antimicrobial agents
bacteria, and its use was limited to urinary tract of new classes becoming available. In contrast,
infections because it achieves only low blood infectious diseases continue to attack human
concentrations and poor tissue distribution, and beings as emerging and re-emerging infectious
106 JMAJ, March / April 2009 — Vol. 52, No. 2
HISTORY OF ANTIMICROBIAL AGENTS AND RESISTANT BACTERIA
diseases, opportunistic infectious diseases, and thickening of the cell wall contributes to decreased
infection with drug-resistant microorganisms sensitivity to this drug. On the other hand,
that will be discussed in the next section. Effec- vancomycin-resistant S. aureus (VRSA) reported
tive utilization of the current limited options is in the US seemed to acquire the resistance
much more important under the dearth of new genes horizontally from vancomycin-resistant
drugs on the market. enterococci (VRE).5 In Japan, there have been
no reports of VRSA strains so far, partially at
History of the Emergence of Resistant least, due to lower detection rates of VRE than
Bacteria those in Western countries.
Although S. pneumoniae was originally sus-
The capacity of microorganisms to acquire resis- ceptible to penicillin, penicillin-intermediate S.
tance to antimicrobial agents has surpassed our pneumoniae (PISP) strains were found in the
imagination. In some cases, antimicrobial agents latter half of the 1960s, and penicillin-resistant
formerly effective are no longer useful. The history S. pneumoniae (PRSP) strains in the latter half
of resistant bacteria will be outlined below and of the 1970s. In Japan, PRSP was found in the
in Table 1. 1980s, and the detection of PRSP strains began
S. aureus is the resistant bacterium most familiar to increase around 1990. Frequent use of oral
in the clinical setting. This bacterium rapidly cephem antibiotics seems to be responsible for
acquired resistance to sulfonamides when they this increase in PRSP. There has also been a
were in use. Penicillin was initially effective remarkable increase in macrolide resistance in
to this microorganism, but resistant strains that this species, which seems also due to the frequent
produce penicillinase increased in the 1950s. use of macrolides in this country.
Therefore, penicillinase-stable methicillin was Ampicillin was initially effective for Haemoph-
developed in 1960, as mentioned previously. ilus influenzae. However, in the 1980s, some of
However, as early as the following year, 1961, this species were found to produce -lactamase,
methicillin-resistant S. aureus (MRSA) was iso- thereby becoming resistant to ampicillin. In
lated in the UK.3 the 1990s, such -lactamase-producing strains
Since around 1990, nosocomial infection with decreased in Japan, however, strains that acquired
MRSA became a social problem. During this highly resistance to -lactam through mutations
period, the target of new antimicrobial agents in PBP genes, increased instead. These are
including second- and third-generation cephems, called as -lactamase-negative ampicillin-resistant
shifted from Gram-positive to Gram-negative (BLNAR) strains, and they are more common
bacteria, and agents with wide spectra but in Japan than in other Western countries. It
weaker activity against Gram-positive bacteria has been speculated that increased use of oral
were widely used (Fig. 1). MRSA acquires resis- cephem antibiotics is also responsible, similar to
tance to most -lactam antibiotics through its the situation with PRSP.
acquisition of the penicillin-binding protein (PBP) Although P. aeruginosa are intrinsically resis-
2’ gene; PBP2’ is an enzyme involved in cell tant to many antimicrobial agents, the emergence
wall synthesis that has low binding affinity for of P. aeruginosa strains resistant to all of three
-lactam antibiotics. In genetic lineage analysis classes of antimicrobials, i.e., carbapenems, quino-
of nosocomial MRSA strains, major nosocomial lones, and aminoglycosides is a recent concern.
clones throughout the world would converge on These multidrug resistant P. aeruginosa (MDRP)
only seven types.4 On the other hand, community- sometimes seems to cause an outbreak in some
associated methicillin-resistant S. aureus (CA- institutions. MDRP has complex mechanisms of
MRSA), which was noticed in the US around drug resistance, including reduced membrane
1997, is of a different type from nosocomial permeability due to decreased outer membrane
MRSA. protein (D2 porin), overexpression of efflux
Fortunately, MRSA so far in Japan have pump, mutation of the quinolone target (DNA
responded to glycopeptide antibiotics such as gyrase), production of aminoglycoside modifi-
vancomycin. However, in the latter half of the cation enzyme, and production of metallo--
1990s, vancomycin-intermediate S. aureus (VISA) lactamase (carbapenem-hydrolysing enzyme).
was reported in this country. It is thought that Some resistance genes are horizontally trans-
JMAJ, March / April 2009 — Vol. 52, No. 2 107
Saga T, Yamaguchi K
ferred by conjugative plasmids.
Gonococci used to be susceptible to penicillin Conclusion
and quinolone, but currently they are resistant
to both agents in Japan. In particular, quinolone In summary, it is clear that the use of antimicro-
had been the first-choice drug for gonococcal bial agents resulted in the selection of resistant
infection in the 1980s because of the potential bacteria. Since the advent of new mighty drugs
advantage in the case of co-infection with is highly difficult, the proper use of currently
Chlamydophila. However, since almost all the available antimicrobial agents as well as efforts
strains have become resistant to quinolones, to minimize the spread of resistant bacteria
the 1999 guidelines declared against the use of through appropriate infection control would be
quinolone for gonococcal infection.6 quite important, and may represent a first step in
solving the issue of resistant microorganisms.7
References
1. Hashimoto H. Why Antimicrobial Agents Become Ineffective: Med. 2007;96(3): 584–595. (in Japanese)
Disease-causing Bacteria Are Evolving. Tokyo: Chuokoron- 5. Appelbaum PC. The emergence of vancomycin-intermediate
Shinsha, Inc.; 2000. (in Japanese) and vancomycin-resistant Staphylococcus aureus. Clin Microbiol
2. Powers JH. Antimicrobial drug development — the past, the Infect. 2006;12(Suppl 1):16–23.
present, and the future. Clin Microbiol Infect. 2004;10(Suppl 4): 6. Yoneda N, Fujimoto Y, Uno M, et al. Annual changes in drug
23–31. sensitivity of gonococci derived from urethritis in men. Jpn J
3. Jevons MP. “Celbenin”-resistant Staphylococci. Br Med J. 1961; Chemother. 2004;52(1):31–34. (in Japanese)
1:124–125. 7. Fishman N. Antimicrobial stewardship. Am J Med. 2006;119(6
4. Yamamoto T, Okubo T, Takano T, et al. Recent topics in Suppl 1):S53–S61.
emerging and re-emerging infectious diseases. J Jpn Soc Int
108 JMAJ, March / April 2009 — Vol. 52, No. 2
S-ar putea să vă placă și
- History of Antimicrobial Agents & Resistant BacteriaDocument6 paginiHistory of Antimicrobial Agents & Resistant BacteriaAnurrag KumarÎncă nu există evaluări
- Review On Cephalosporins Re ModifiedDocument6 paginiReview On Cephalosporins Re Modifiedramirezgrisel966Încă nu există evaluări
- Antibiotic Resistance of Bacteria: A Global Challenge: Saswati Sengupta and Madhab K ChattopadhyayDocument15 paginiAntibiotic Resistance of Bacteria: A Global Challenge: Saswati Sengupta and Madhab K Chattopadhyaysourav dasÎncă nu există evaluări
- Antimicrobial Resistance A Tale of The Past Becomes A Terrorfor The PresentDocument7 paginiAntimicrobial Resistance A Tale of The Past Becomes A Terrorfor The PresentdssgssÎncă nu există evaluări
- Antibiotics Past, Present and Future 2019Document9 paginiAntibiotics Past, Present and Future 2019Aylin GarcíaÎncă nu există evaluări
- Hutchings 2019Document9 paginiHutchings 2019nabilahÎncă nu există evaluări
- 321Document5 pagini321mbilouzi589Încă nu există evaluări
- Martens and Demain - , 2017 - The AntibiotiDocument7 paginiMartens and Demain - , 2017 - The AntibiotiJavier CastroÎncă nu există evaluări
- Antibiotic Resistance Mechanisms in M. TuberculosisDocument34 paginiAntibiotic Resistance Mechanisms in M. TuberculosisSofiaMarmolejoÎncă nu există evaluări
- VPT 411 Veterinary Chemotherapy Tanuvas Lecture NotesDocument94 paginiVPT 411 Veterinary Chemotherapy Tanuvas Lecture NotesSunil100% (41)
- Antimicrobial Resistance: The Indian ScenarioDocument14 paginiAntimicrobial Resistance: The Indian Scenariosungita_kÎncă nu există evaluări
- Mekanisme Resistensi Antibiotik - 2014Document10 paginiMekanisme Resistensi Antibiotik - 2014ArdieÎncă nu există evaluări
- Bacterial Resistance To AntibioticsDocument37 paginiBacterial Resistance To Antibioticscristi69230% (1)
- Overview of Antimicrobial Resistance - An Emerging Silent PandemicDocument13 paginiOverview of Antimicrobial Resistance - An Emerging Silent PandemicAbbireddy SairamÎncă nu există evaluări
- Hutchingetal COM 2019 51 72-80Document10 paginiHutchingetal COM 2019 51 72-80Daniel PancuÎncă nu există evaluări
- Antibióticos, Quimioterápicos e Resistência MicrobianaDocument54 paginiAntibióticos, Quimioterápicos e Resistência MicrobianaMarta BarbosaÎncă nu există evaluări
- Antibiotics: BiologyDocument3 paginiAntibiotics: BiologyWamiq SheikhÎncă nu există evaluări
- TX Carbapenem Resistent MoDocument11 paginiTX Carbapenem Resistent MoInes MendonçaÎncă nu există evaluări
- Article 1Document26 paginiArticle 1AGUS DE COLSAÎncă nu există evaluări
- Artículo Resistant To Antibiotics. Alanis, 2005Document9 paginiArtículo Resistant To Antibiotics. Alanis, 2005JUAN ESTEBAN MONJE ROMEROÎncă nu există evaluări
- Antibiotics: Antibiotics and Vaccines Are Among The Biggest Medical Advances Since 1000. (Culver Pictures)Document33 paginiAntibiotics: Antibiotics and Vaccines Are Among The Biggest Medical Advances Since 1000. (Culver Pictures)keydjohnsincoÎncă nu există evaluări
- Antimicrobial Drugs Discovery and ClassificationDocument6 paginiAntimicrobial Drugs Discovery and ClassificationMonisha vÎncă nu există evaluări
- Major WorkDocument12 paginiMajor WorkTamanna WahidÎncă nu există evaluări
- Antimicrobial Resistances: The World's Next Pandemic On The WayDocument11 paginiAntimicrobial Resistances: The World's Next Pandemic On The WayIAEME PublicationÎncă nu există evaluări
- European Journal of Medicinal Chemistry: Rangappa S. Keri, Sasidhar B.S., Bhari Mallanna Nagaraja, M. Am Elia SantosDocument13 paginiEuropean Journal of Medicinal Chemistry: Rangappa S. Keri, Sasidhar B.S., Bhari Mallanna Nagaraja, M. Am Elia SantosYun NikÎncă nu există evaluări
- Antibacterial Agents Basis of ActionDocument8 paginiAntibacterial Agents Basis of ActionFrancisco BecerraÎncă nu există evaluări
- Therapeutics in Aquaculture (AAH 301 1+1)Document25 paginiTherapeutics in Aquaculture (AAH 301 1+1)RISHIKAÎncă nu există evaluări
- Treatment Options For Carbapenem-Resistant Gram-Negative Bacterial InfectionsDocument11 paginiTreatment Options For Carbapenem-Resistant Gram-Negative Bacterial InfectionsCesar Augusto Cardona OspinaÎncă nu există evaluări
- Anti Microbial ResistanceDocument2 paginiAnti Microbial ResistanceKarthikÎncă nu există evaluări
- Antibiotics Project BeginningDocument3 paginiAntibiotics Project BeginningWamiq Sheikh100% (1)
- Science Project That Takes Me So Long To Do It: What Is Antibiotics?Document4 paginiScience Project That Takes Me So Long To Do It: What Is Antibiotics?Vu Ba SonÎncă nu există evaluări
- MICP LAB (WEEK - 5) Antimicrobial Agents in TherapydocDocument8 paginiMICP LAB (WEEK - 5) Antimicrobial Agents in Therapydoccaitie miracleÎncă nu există evaluări
- Antimicrobial Resistance in Hospital-Acquired Gram-Negative Bacterial InfectionsDocument9 paginiAntimicrobial Resistance in Hospital-Acquired Gram-Negative Bacterial InfectionsAlina BanciuÎncă nu există evaluări
- Microorganisms 09 02297 v2Document17 paginiMicroorganisms 09 02297 v2yeayÎncă nu există evaluări
- MBA Presentation on Antibiotic Resistance and Its SolutionsDocument18 paginiMBA Presentation on Antibiotic Resistance and Its SolutionsAnshuman ParasharÎncă nu există evaluări
- Kingdom Monera - AntibioticsDocument22 paginiKingdom Monera - AntibioticsCaleb TanÎncă nu există evaluări
- Antibiotics: Gsa Notes (Imaz Virk)Document7 paginiAntibiotics: Gsa Notes (Imaz Virk)Umair RaufÎncă nu există evaluări
- Nuevos Antibioticos Vs Gram NegativosDocument11 paginiNuevos Antibioticos Vs Gram NegativosbrenpmÎncă nu există evaluări
- AMR - Current Scenario and ChallangesDocument37 paginiAMR - Current Scenario and ChallangesShonit SharmaÎncă nu există evaluări
- Perspectives: Where Will New Antibiotics Come From?Document6 paginiPerspectives: Where Will New Antibiotics Come From?nabilahÎncă nu există evaluări
- Chapter 69: Odontogenic Infections Larry J. PetersonDocument14 paginiChapter 69: Odontogenic Infections Larry J. PetersonAhmad EidÎncă nu există evaluări
- Mechanisms Efflux Pumps of Acinetobacter To Antibiotics: Baumannii (MDR) : Increasing ResistanceDocument23 paginiMechanisms Efflux Pumps of Acinetobacter To Antibiotics: Baumannii (MDR) : Increasing ResistanceanggaririnÎncă nu există evaluări
- Antibiotics: Antibiotics in Food Chain: The Consequences For Antibiotic ResistanceDocument26 paginiAntibiotics: Antibiotics in Food Chain: The Consequences For Antibiotic ResistanceJafrinta Irma R.A.Încă nu există evaluări
- Polishing The Tarnished Silver Bullet The Quest FoDocument12 paginiPolishing The Tarnished Silver Bullet The Quest FoTamas ZefferÎncă nu există evaluări
- Mechanism of ResistenceDocument26 paginiMechanism of ResistenceDefi OktafiaÎncă nu există evaluări
- Multi Drug ResistanceDocument33 paginiMulti Drug ResistanceEvanslin SantusÎncă nu există evaluări
- Antimicrobial Resistance: The Ticking Time BombDocument67 paginiAntimicrobial Resistance: The Ticking Time BombPatricia DillonÎncă nu există evaluări
- CH631-unit-3 Med Chem PDFDocument77 paginiCH631-unit-3 Med Chem PDFN Khadija BathoolÎncă nu există evaluări
- Study Drug Resistance in Bacteria Using AntibioticsDocument47 paginiStudy Drug Resistance in Bacteria Using Antibioticskioilui;lphio961% (18)
- Jof 09 00171Document20 paginiJof 09 00171Saman Kumara PereraÎncă nu există evaluări
- What Is MicrobiologyDocument3 paginiWhat Is MicrobiologyGillie May SalubreÎncă nu există evaluări
- 2015-Maryam Sana-Miracle-Remedy-Inhibition-Of-Bacterial-Efflux-Pumps-By-Natural-Products-2332-0877-1000213Document6 pagini2015-Maryam Sana-Miracle-Remedy-Inhibition-Of-Bacterial-Efflux-Pumps-By-Natural-Products-2332-0877-1000213Fitria MokodompitÎncă nu există evaluări
- Davies-Bolorundoro Et Al. 2021 - Bioprospecting antiTB DrugsDocument15 paginiDavies-Bolorundoro Et Al. 2021 - Bioprospecting antiTB DrugsaliÎncă nu există evaluări
- Doctorat Biologie-EnglezaDocument96 paginiDoctorat Biologie-EnglezaProiectulTauÎncă nu există evaluări
- Introduction To Antibiotics: Mrs Natasha MahajanDocument17 paginiIntroduction To Antibiotics: Mrs Natasha Mahajannatasha jadhavÎncă nu există evaluări
- How Alexander Fleming's Discovery of Penicillin Revolutionized MedicineDocument5 paginiHow Alexander Fleming's Discovery of Penicillin Revolutionized MedicineSKA PROSÎncă nu există evaluări
- Microbiology Antibiotics AntimicrobialDocument12 paginiMicrobiology Antibiotics AntimicrobialSandeep KumarÎncă nu există evaluări
- PENICILLIN ReportDocument44 paginiPENICILLIN Reportraghavan89100% (1)
- Antifungal Drugs - The Current Armamentarium and Development of New AgentsDocument20 paginiAntifungal Drugs - The Current Armamentarium and Development of New AgentssovalaxÎncă nu există evaluări
- Economics of Self-Medication: Theory and EvidenceDocument19 paginiEconomics of Self-Medication: Theory and EvidenceMatiyas ZewdeÎncă nu există evaluări
- Guideline For Registration of VaccineDocument60 paginiGuideline For Registration of VaccineMatiyas ZewdeÎncă nu există evaluări
- Ecec 03 00052Document4 paginiEcec 03 00052Matiyas ZewdeÎncă nu există evaluări
- Over The Counter Medicines List For Ethiopia 2nd EditionDocument19 paginiOver The Counter Medicines List For Ethiopia 2nd EditionRed Falcon0% (1)
- 5 Ethiopian Medicines Formulary 2013Document1.032 pagini5 Ethiopian Medicines Formulary 2013eyob50% (4)
- Drugs & Therapy: B U L L E T I NDocument4 paginiDrugs & Therapy: B U L L E T I NMatiyas ZewdeÎncă nu există evaluări
- Finalized Promotion Control Guideline 2nd Edition PDFDocument35 paginiFinalized Promotion Control Guideline 2nd Edition PDFElisha ThompsonÎncă nu există evaluări
- 274 551 3 PBDocument6 pagini274 551 3 PBDr-Asif MahmoodÎncă nu există evaluări
- Risks of Self-Medication Practices: October 2010Document28 paginiRisks of Self-Medication Practices: October 2010Matiyas ZewdeÎncă nu există evaluări
- Structural Design Loads CalculationDocument6 paginiStructural Design Loads Calculationfaris11Încă nu există evaluări
- Federal Register / Vol. 64, No. 51 / Wednesday, March 17, 1999 / Rules and RegulationsDocument50 paginiFederal Register / Vol. 64, No. 51 / Wednesday, March 17, 1999 / Rules and RegulationsMatiyas ZewdeÎncă nu există evaluări
- Essential medicines for drug shopsDocument52 paginiEssential medicines for drug shopsDaily BreadÎncă nu există evaluări
- DensityOfWater Vs Temp PDFDocument1 paginăDensityOfWater Vs Temp PDFr_i_k_yÎncă nu există evaluări
- Concentration Size and Density of Total Suspended Particulates at The Air Exhaust of Concentrated Animal Feeding OperationsDocument10 paginiConcentration Size and Density of Total Suspended Particulates at The Air Exhaust of Concentrated Animal Feeding OperationsMatiyas ZewdeÎncă nu există evaluări
- Physometric Chart SIDocument1 paginăPhysometric Chart SIsuathayriÎncă nu există evaluări
- Mo PDFDocument2 paginiMo PDFMatiyas ZewdeÎncă nu există evaluări
- B 36.10mDocument31 paginiB 36.10mmisaelzaÎncă nu există evaluări
- Complicated Intra-Abdominal Infections (Adult and Pediatric Patients)Document4 paginiComplicated Intra-Abdominal Infections (Adult and Pediatric Patients)Jonna Mae TurquezaÎncă nu există evaluări
- Eucast Rast Breakpoint Table V 4.0 PDFDocument14 paginiEucast Rast Breakpoint Table V 4.0 PDFGuneyden GuneydenÎncă nu există evaluări
- IJAA - CRAb - Jaidane 2018Document4 paginiIJAA - CRAb - Jaidane 2018Nadia JaidaneÎncă nu există evaluări
- Medicinal Chemistry of Beta-Lactam AntibioticsDocument13 paginiMedicinal Chemistry of Beta-Lactam AntibioticsJosiah O OmobaÎncă nu există evaluări
- Cell Wall Synthesis InhibitorsDocument6 paginiCell Wall Synthesis Inhibitorshoa1212Încă nu există evaluări
- Ijbms 23 1396Document5 paginiIjbms 23 1396Sherwan HusseinÎncă nu există evaluări
- Septic Shock Rapid Recognition and Initial Resuscitation inDocument19 paginiSeptic Shock Rapid Recognition and Initial Resuscitation inCristian Villarroel SÎncă nu există evaluări
- Acineto CrabDocument9 paginiAcineto CrabAndrei GomesÎncă nu există evaluări
- Antibiotic Class by CoverageDocument3 paginiAntibiotic Class by Coverageayy1Încă nu există evaluări
- Amr FactsheetDocument6 paginiAmr FactsheetAhmed .YÎncă nu există evaluări
- PCAP - SummaryDocument4 paginiPCAP - SummaryNani TumlosÎncă nu există evaluări
- Evaluation and Management of Suspected Sepsis and Septic Shock in AdultsDocument62 paginiEvaluation and Management of Suspected Sepsis and Septic Shock in AdultsGiussepe Chirinos CalderonÎncă nu există evaluări
- A Case Report On Faropenem Induced Focal SeizuresDocument3 paginiA Case Report On Faropenem Induced Focal SeizuresInternational Journal of Innovative Science and Research Technology100% (1)
- Acute Bacterial Meningitis: Signs, Symptoms and PathogensDocument37 paginiAcute Bacterial Meningitis: Signs, Symptoms and PathogensrodghzÎncă nu există evaluări
- 1 s2.0 S1473309922008118 MainDocument13 pagini1 s2.0 S1473309922008118 MaindaniaÎncă nu există evaluări
- New Insights Into Citrobacter Freundii Sepsis in NeonatesDocument6 paginiNew Insights Into Citrobacter Freundii Sepsis in NeonatesEduardo Rios DuboisÎncă nu există evaluări
- Ventilator Associated Pneumonia (Vap)Document11 paginiVentilator Associated Pneumonia (Vap)Suresh KumarÎncă nu există evaluări
- Imipenem and Meropenem Comparison of in Vitro ActiDocument14 paginiImipenem and Meropenem Comparison of in Vitro ActipoojaÎncă nu există evaluări
- 30395-Article Text-56938-1-10-20220916Document8 pagini30395-Article Text-56938-1-10-20220916Djim KARYOMÎncă nu există evaluări
- Antibiotic Mechanisms (For Students)Document87 paginiAntibiotic Mechanisms (For Students)Wahab KhaniÎncă nu există evaluări
- 2015 Nelson's Pedi Antimicrobial TX PDFDocument263 pagini2015 Nelson's Pedi Antimicrobial TX PDFMarcel PopaÎncă nu există evaluări
- Community-Acquired Pneumonia 1Document15 paginiCommunity-Acquired Pneumonia 1Jaime BarraganÎncă nu există evaluări
- Expert Review of Carbapenem-Sparing Options for ESBL-Producing EnterobacteriaceaeDocument29 paginiExpert Review of Carbapenem-Sparing Options for ESBL-Producing EnterobacteriaceaeCaio Bonfim MottaÎncă nu există evaluări
- Detection of Beta LactamDocument18 paginiDetection of Beta LactamRajkishor YadavÎncă nu există evaluări
- Philippine Guidelines on Diagnosis and Management of Community-acquired PneumoniaDocument42 paginiPhilippine Guidelines on Diagnosis and Management of Community-acquired PneumoniaMarion Andrea PoblacionÎncă nu există evaluări
- Dr. Megha CVDocument10 paginiDr. Megha CVMegha MaheshwariÎncă nu există evaluări
- Isolation of Nosocomial Multi-Drug Resistant Gram-Negative Bacteria From Some Benghazi HospitalsDocument18 paginiIsolation of Nosocomial Multi-Drug Resistant Gram-Negative Bacteria From Some Benghazi HospitalsInternational Medical Publisher100% (1)
- Double Anaerobic Coverage Guideline AgainstDocument2 paginiDouble Anaerobic Coverage Guideline AgainstioanaÎncă nu există evaluări
- Antimicrobial Stewardship in The Intensive Care Unit, 2023Document10 paginiAntimicrobial Stewardship in The Intensive Care Unit, 2023Jonathan Fierro MedinaÎncă nu există evaluări
- EUCAST Expert Rules on Enterobacterales SusceptibilityDocument6 paginiEUCAST Expert Rules on Enterobacterales SusceptibilityLisa MallinckrodtÎncă nu există evaluări