Documente Academic
Documente Profesional
Documente Cultură
OS214 Gastrointestinal Tract Imaging FINAL
Încărcat de
upcm2014blockADescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
OS214 Gastrointestinal Tract Imaging FINAL
Încărcat de
upcm2014blockADrepturi de autor:
Formate disponibile
Vicente Francisco
Augustina R. Hizon, M.D.
D. Abelardo, MD, Patho 1
FPCR, FPROS, FUSP,
FPSP, FESTRO, FPSO
MIAC 2
OS 214
OS 215 Digestionand
Reproduction and Excretion
Hormonal Regulation F
Gastrointestinal
Lec 2A: Pathology ofTract Imaging
the Female Genital Tract (Vulva and Vagina)
pharyngogram shown on the left), abnormal luminal contour, or
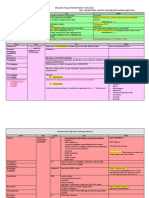
OUTLINE focal increased density;
I. Pharynx (2) mucosal irregularity owing to ulceration or mucosal elevation
II. Esophagus (3) asymmetric distensibility caused by infiltrating tumor or
III. Abdomen extrinsic nodal mass.
IV. Stomach & Duodenum
V. Small Intestines 4. Computed Tomography Scan (CT-Scan)
VI. Large Intestines, including Rectum and Anus
VII. Liver, Hepatobiliary Tree & Gall Bladder • For a more detailed evaluation
VIII. Pancreas • For less radiation exposure: request for with multi-
slice ||>
Disclaimer: Don’t hate us for this trans. This is our first trans on Imaging
Modalities and we tried our best to make this at par with our usual transes. If you
• May allow better
find any difficulty appreciating the figures, please see Dr. Hizon;s slides. The
visualization and
file’s uploaded in our Scribd account. evaluation of osseous
structures, soft tissues and
PHARYNX vascular networks;
• Uses contrast agents
Radiographic Evaluation administered
intravenously, takes a
1. Plain Radiograph or X-ray longer scanning time, and
• most common imaging modality is more expensive.
• Soft tissues of the neck viewed laterally
• Neck is positioned in hyperextension 5. Magnetic Resonance Imaging (MRI)
• even better than CT-scan
• Usually x-ray comes from the patient’s right side, film is
• uses a magnetic beam to
at the left
visualize tissue
• Done to evaluate the thickness and osseous structures • Soft tissue appearance is
of the pharyngeal area; normal pharyngeal airspace: 1-2 much better than CT-Scan
cm in thickness • Metallic implants/objects-
contraindicated
• ||> This is a • titanium, porcelain – MRI
lateral view of the neck to friendly
image the normal pharynx.
The neck should be
• This modality is best for soft
hyperextended and it is tissues and is only reserved for difficult cases.
important to instruct the • MRI provides much greater contrast between the
patient not to move. Note the different soft tissues of the body
thickness of the soft tissues
and check for abnormal Pharyngeal Disorders that need imaging:
indentations
• Normal: Homogenous image; air column seen anterior 1. Diverticula
vertebra • Can be anterior, lateral or posterior; congenital or
acquired
2. Fluoroscopy • “Zenker’s Diverticulum”
• next most common o Also known Pharyngo-esophageal
• Evaluation of structures in real life time – flexion, Diverticulum,
extension and in swallowing o Originates in Laimer’s triangle or Kilian’s
• In swallowing – soft tissue density of prevertebral dehiscence
structures can be seen o It is a diverticulum of the mucosa of
• If there’s a foreign body, this can be used have the pharynx, just above the cricopharyngeal
patient swallow barium so that the defect can be seen. muscle (i.e. above the upper sphincter of
• Divided into the nasopharnyx, oropharynx and the oesophagus)
hypopharnyx o Take a look at thickness of prevertebral face
• Fluoroscope- consists of an X-ray source and
fluorescent screen
• Modified barium swallow study - Barium-impregnated
liquids and solids are ingested by the patient. A
radiologist records and, with a speech pathologist (a.k.a
speech therapist), interprets the resulting images to
diagnose oral and pharyngeal swallowing dysfunction.
This is also used in studying normal swallow function.
3. Double Contrast Pharyngography
• Makes use of contrast agent
like Barium, in addition to X-
ray. 2. Retropharyngeal Abscess
• Allows detection of tumors • Note the marked swelling of
that are difficult to visualize the prevertebral space, which
endoscopically. indicates mass infection.
• Radiographic signs : • Lucencies: indicate tissue
(1) intraluminal mass- seen as a breakdown compatible with
filling defect (pointed by arrows in the tubular abscesses
Tel, Ther, Joram, Roland Thurs, Feb. 24, 2011 Page 1 of 13
Vicente Francisco
Augustina R. Hizon, M.D.
D. Abelardo, MD, Patho 1
FPCR, FPROS, FUSP,
FPSP, FESTRO, FPSO
MIAC 2
OS 214
OS 215 Digestionand
Reproduction and Excretion
Hormonal Regulation F
Gastrointestinal
Lec 2A: Pathology ofTract Imaging
the Female Genital Tract (Vulva and Vagina)
• If with calcifications may be indicative of chronic Only a small amount of contrast or light barium is used because
tuberculosis. there is always the danger of aspiration and obstruction of the
respiratory tree.
• Take note of the
In cases of aspiration (which can cause pneumonitis), the patient
thickness w/c is > 2 cm A mass posterior to the pharynx;
streaks of lucency
should be immediately hydrated by nebulization and administered with
expectorants. This won’t work if thick contrast media is used. Water-
3. Functional Disorders
soluble media are also not used in this procedure because it may lead
• to detect impairment of function. to pulmonary edema.
May be caused by spasm due to: 1. Chemical Esophagitis
A. Neuromuscular Dysfunction
• CNS Disease
• Muscle Disease
• Myasthenia Gravis
• Peripheral Nerve Disease
B. Abnormalities in the crico-pharnygeal sphincter
• Achalasia, Myotonic Dystrophy, Familial
Dysautonomia (Riley-Day Syndrome)
C. Malignant Epithelial Neoplasms (Tumors) • Ingestion of corrosive material
• Nasopharynx – more common for Filipinos • Perforations indicate spillage
better diagnosed with CT-Scan or MRI
• Oropharynx 2. Motility Disorders
• Hypopharynx
PRIMARY
ESOPHAGUS • Achalasia: most common indication for
esophagogram
A. Radiographic Evaluation
• Cardiospasm
B. CT-Scan – can be used for a dynamic study
C. MRI
• Deficiency of the ganglion cells of
Auerbach’s plexus
Radiographic Evaluation • Failure of relaxation of the Lower
Esophageal Sphincter (LES)
1. Contrast Esophagography • Mecholyl Test
• Usually done because the esophagus collapses • Usually 30-50 yrs.
• Ask patient to hold the contrast medium in his/her mouth
and swallow it slowly
• Single Contrast
- Employs the most usual contrasts
- Use of Barium (non water-soluble) or other
Water-soluble contrasts
B
A
• Double Contrast
- Other liquid media such as Sprite® or 7-Up®
can be added to the contrast medium
• normally a part of upper GI series
• look for mucosal irregularities A. Take note of the nasograstic tube and the lucent area compatible
with achalasia. B. Dilated terminal part of the esophagus. Balloon-like
• look for abnormal filling defects, areas of narrowing or dilatation is always ABNORMAL.
dilatation
• seen in segments due to normal persistalsis of the • Diffuse Esophageal Spasm
esophagus • Presbyoesophagus
• 1st step: Drink contrast then hold in mouth • Chalasia
2nd step: Swallow then contrast is traced • Idiopathic Pseudo-obstruction –constriction of
esophagus
A B C D
SECONDARY
• Connective Tissue Disorders (i.e. Scleroderma, SLE,
etc.)
• Reflux Esophagitis
• Metabolic & Endocrine Disorders (i.e. DM, Alcoholism,
etc.)
• Neuromuscular Disease
• Can be secondary to radiographic treatment
A. AP view. B. Lateral view. Look at where the esophagus is resting.
The esophagus is not usually seen since it usually collapsed when 3. Congenital Anomalies
empty. C. Done under fluoroscopic guidance. Check for filling defects • esophageal contrast study is usually indicated
and mucosal irregularities. D. Esophagogram of a normal esophagus
as it enters the esophageal hiatus. Observe the smoothness of the • *Note: If there’s suspicion of tracheoesophageal
mucosal surface. reflux -> ALERT RADIOLOGIST due to possibility of
aspiration
B. Esophageal Disorders that warrant imaging studies
Atresia and TracheoEsophageal Fistula
(TEF): most common cause: Iatrogenic due to chemicals
Tel, Ther, Joram, Roland Thurs, Feb. 24, 2011 Page 2 of 13
Vicente Francisco
Augustina R. Hizon, M.D.
D. Abelardo, MD, Patho 1
FPCR, FPROS, FUSP,
FPSP, FESTRO, FPSO
MIAC 2
OS 214
OS 215 Digestionand
Reproduction and Excretion
Hormonal Regulation F
Gastrointestinal
Lec 2A: Pathology ofTract Imaging
the Female Genital Tract (Vulva and Vagina)
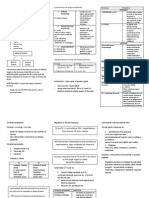
Types: ABDOMEN
• A: Atresia with Distal TEF
A. Radiographic Evaluation
• B: Atresia without TEF
B. Contrast Study (barium enema, upper GI series
There is a filling defect in the C. CT-Scan
image (blind pouch) compatible
with complete obstruction. In
D. MRI
this case, no TEF is observed. E. Ultrasound
F. Nuclear (Radioisotope) Scanning
• C: TEF without Atresia
(H-type) Radiographic Evaluation
• D: Atresia with Proximal
1. Plain Abdomen X-ray
TEF
• Patient in supine position. (X-ray beam above, X-ray
• E: Atresia with Double TEF
plate below)
Duplication • Plain abdominal X-ray: upper limit should include the
diaphragm; primarily for visualization of Upper GI Tract
BronchoEsophageal Fistulas
• KUB studies: film should extend down the pubis and
4. Esophageal Tumors cover the whole pelvis
• Squamous: most common in the upper 2/3 • What to Examine:
• Gastric: distal 3rd o Gas Pattern – look at distribution of bowel gas
o Extraluminal Air
• Esophagogram can reveal tumors well, provided that it
o Soft Tissue Masses
is not yet fully obstructed
o Calcifications – especially in the area of the
• If with complete obstruction: length cannot be
gallbladder and the kidneys and urinary tract
determined so need to request CT-scan o Psoas Muscles & Flank stripes
• Diagnosed nowadays by Esophagoscopy and o Liver, Spleen & Bladder (esp. visible when
Endoscopy
distended)
o Osseous structures
• Malignant Neoplasms • Normal Gas Pattern:
• Carcinomas (Squamous, Adenocarcinoma, Carcinoid) o Stomach: Always present (gastric bubble)
A B C o Small Bowel: 2 or 3 loops of non-distended
bowel; finer lucencies
o Rectum or Sigmoid: Almost always present
A. The image shows complete obstruction. B. Partial obstruction
secondary to tumor mass. Take note of the irregularities in the esophageal
mucosa suggesting multi-focus type of esophageal cancer. C. This is a
classical picture of “shouldering defect” in esophageal carcinoma
(Concentric carcinoma): irregular outline of esophagus.
• Sarcomas (Leiomyosarcoma, Fibrosarcoma, etc.)
• Metastasis
• Benign Neoplasms
• Normal Fluid Levels:
• Mucosal (Papilloma or Adenoma)
• Submucosal (Neurofibroma, Leiomyoma, • Stomach: Always present (except in supine film)
Hemangioma, Lipoma, Fibroma, Myeloblastoma, etc.) • Small Bowel: Possibly present in 2 or 3 levels (few)
• Large Bowel: None normally because water is
• Non-neoplastic absorbed
• Polyps • Hematoma
• Varices • Hamartoma
• Cysts • Chemical Esophagitis
• Focal Infection • Foreign Body
5. Foreign body - Ingested coin
• Small vs. Large Bowel
Tel, Ther, Joram, Roland Thurs, Feb. 24, 2011 Page 3 of 13
Vicente Francisco
Augustina R. Hizon, M.D.
D. Abelardo, MD, Patho 1
FPCR, FPROS, FUSP,
FPSP, FESTRO, FPSO
MIAC 2
OS 214
OS 215 Digestionand
Reproduction and Excretion
Hormonal Regulation F
Gastrointestinal
Lec 2A: Pathology ofTract Imaging
the Female Genital Tract (Vulva and Vagina)
• Small Bowel
o Central
o Valvulae conniventes (mucosal foldings of the
small intestines) extend across lumen
o Has a maximum diameter of 2 in. (dilated if >
2)
• Large Bowel
o Peripheral
o Haustral markings
(sacculations in the wall of
the large intestines) don’t
extend from wall-to-wall
Supine Prone
• Complete Abdomen: Obstruction Series No air-fluid levelling; Presence of gas in the rectum; Diameter is about 2 inches
(Abdominal X-ray positions)
□ Generalized Adynamic Ileus
• Supine – this is done first for
economic reasons: radiologist Gas in dilated small bowel and large bowel to
recommends whether to proceed rectum
with the obstruction series or not Long air-fluid levels
• Prone Only post-op patients have Generalized Ileus
Can be caused by surgery or medications that
□ Look for: affect GI motility
Gas in Rectum/Sigmoid
Gas in Ascending and
Descending Colon
□ Alternative: Lateral Rectum if patient cannot lie
prone
• Erect
□ Look for:
Free Air/bowel
gas
Air under the diaphragm
Supine Erect
(pneumoperitoneum)
Air-fluid
leveling No presence of differential air-fluid level (2 air-fluid interfaces in 1 bowel);
□ Alternative: Left Lateral Decubitus – if unable to
sit up or stand up • Mechanical Obstruction
• Chest-Erect □ Small Bowel Obstruction (SBO)
□ Look for: Dilated small bowel
Changes in the
pleural cavity
Fighting loops: dilating loops are
very prominent; walls are thickened
Blunting of the Little gas in colon, esp. rectum
costophrenic sulci
Free Air
Differential air-fluid levels: may indicate
obstruction
Pneumonia at bases
Pleural effusions Key: Disproportionate dilatation of the small
bowel
□ Alternative: Chest-Supine if unable to sit/stand
Causes:
*Collateral Findings: basal pneumonitis, blunting of the Adhesions
costophrenic sulci etc. Hernia*
Volvulus**
• Causes of Abnormal Gas Patterns Gallstone Ileus* -
• Functional Ileus (medical) obstruction of the
□ Localized (Sentinel Loops) ileus by a gallstone
from the biliary tree
One or two persistently dilated loops of large or
small bowels Intussusception**
**may be visible on
There should always be gas in plain film
rectum or sigmoid no gas = obstruction **Medical emergencies;
No gas in the rectum
Most common
Seen in Gastroenteritis Thickening of bowel walls
emergency In upright –there is air fluid
Pitfall: may resemble early procedures levelling in areas proximal
mechanical SBO
Pitfall: Early
SBO may resemble
localized Ileus (get follow up abdominal x-ray
after 24 hours to see if it progresses)
Tel, Ther, Joram, Roland Thurs, Feb. 24, 2011 Page 4 of 13
Vicente Francisco
Augustina R. Hizon, M.D.
D. Abelardo, MD, Patho 1
FPCR, FPROS, FUSP,
FPSP, FESTRO, FPSO
MIAC 2
OS 214
OS 215 Digestionand
Reproduction and Excretion
Hormonal Regulation F
Gastrointestinal
Lec 2A: Pathology ofTract Imaging
the Female Genital Tract (Vulva and Vagina)
□ Large Bowel Obstruction (LBO) • A radiologic emergency
Dilated colon proximal to point of
• Golden period for correcting volvulus: 72 hours to 1
week (if 1 week: proceed with caution!)
obstruction
Little or no air in rectum/sigmoid • Be careful during palpation because volvulus may rupture
Little or no gas in small bowel, if… • In this case, a Barium enema would both be
Ileocecal valve remains competent diagnostic and therapeutic.
• In the figures below, take note of the different air-fluid
If incompetent, then small bowel air is seen levels
Causes:
Tumor
Volvulus
Hernia
Diverticulitis
Intussusception
Pitfalls: Incompetent Ileocecal Valve
Large bowel decompresses into small
bowel
May look like SBO 1st: dilated bowel loop
2nd: differential levelling limited to large gut
Get Barium Enema or F/O
||> Intraperitoneal Calcification
• For Higher Learning: The
radiological detection of
peritoneal calcification is rare
but potentially of major clinical
importance because such
findings have been
associated with
□ primary and secondary
peritoneal malignancies;
Supine Prone
□ benign causes:
Sclerosing peritonitis due to
peritoneal dialysis
Table 1.
Peritoneal tuberculosis
Air in Rectum Air in Small Air in Large Prior meconium peritonitis
or Sigmoid Bowel Bowel
Hyperparathyroidism
Localized 2-3 distended Air in rectum
ileus
Yes
loops or sigmoid Pneumocystis carinii infection
Generalized Multiple Yes Postsurgical heterotopic ossification.
Yes
ileus Distended loops (Distended)
Multiple Dilated ||> Intussusception
SBO No No
loops
• An emergency situation
None (unless
LBO No ileocecal valve is
Yes • a part of the intestine has invaginated into another
(Dilated) section of intestine
incompetent)
• Intussuscepiens (R)
||> Gallstone Ileus □ The “receiver”
• Occurs when the gallstone obstructs the lumen
□ The part of the bowel into which another part is
invaginated in;
between the Ileum and the Cecum
□ The portion of the bowel containing the
• May cause transient obstruction
intussusceptum
• Intussusceptum (I)
□ The “invaginator”
□ The portion of the bowel that has been
invaginated within another part
R
R
I
I
||> Volvulus
• Bean-shaped structure/Inverted U-loop structure in a
radiograph is indicative of volvulus ‘Barium enema: incomplete filling of cecum
Tel, Ther, Joram, Roland Thurs, Feb. 24, 2011 Page 5 of 13
Vicente Francisco
Augustina R. Hizon, M.D.
D. Abelardo, MD, Patho 1
FPCR, FPROS, FUSP,
FPSP, FESTRO, FPSO
MIAC 2
OS 214
OS 215 Digestionand
Reproduction and Excretion
Hormonal Regulation F
Gastrointestinal
Lec 2A: Pathology ofTract Imaging
the Female Genital Tract (Vulva and Vagina)
||> Extraluminal Air: Free Intraperitoneal Air Free Air
• Signs of Free Air (Pneumoperitoneum):
□ Air beneath diaphragm
□ Falciform Ligament Sign
□ Air on both sides of bowel wall – Rigler’s Sign
Rigler's sign (also, double wall sign), is seen on an X-
ray of the abdomen when air is present on both sides of
the intestine; a Rigler's sign is present when air is present
on the inside (lumenal side) and the outside (peritoneal
side).
||> Chilaiditi Syndrome
• Normal findings
• Loop of large colon insinuates between diaphragm
and liver (hepatic flexure)
• asymptomatic
• Transposition of a loop of large intestine (usu. the
Transverse colon) in between the Liver and the Right
Diaphragm, causing extreme abdominal pain, volvulus
and shortness of breath
□ Air in Lesser Sac (the most anterior part of the • Manifests in the abdominal X-ray as Chilaiditi’s Sign –
peritoneum) – since mataas presence of gas in the right Colic angle between the
Liver and Right Diaphragm
□ Football Sign and the Falciform ligament sign
– seen bulging to the right
The Football Sign appears as a large oval
radiolucency reminiscent of an American football seen
on supine radiographs of the abdomen. The football
sign is most frequently seen in infants with
spontaneous or iatrogenic or iatrogenic gastric
perforation causing pneumoperitoneum.
Falciform ligament sign: seen bulging to the right;
linked to the football sign seen as the football’s
seam
Falciform
Ligament Sign
||> Bochdaleck’s Hernia
• One of two forms of a Congenital Diaphragmatic
Hernia
• Posterior and lateral in location
• Heart is displace dot the rught
• Bochdalek Foramen is found on the left posterolateral
portion of the diaphragm.
• Causes of Free Air:
□ Rupture of a hollow viscus (an internal organ;
• Congenital abnormality wherein an opening that exists
singular form of viscera) in the infant’s diaphragm allows intra-abdominally
located organs (i.e. stomach and intestines) to
Perforated Ulcer
protrude into the thoracic cavity
Perforated Diverticulitis
Perforated Carcinoma • Has the potential to be life-threatening – can cause
Trauma or Instrumentation deformities in the lungs that can lead to its
□ 5-7 days Post-op compression
□ NOT caused by a perforated Appendix • Differential: Morgagni’s Hernia: medial in position
Because the Appendix is retroperitoneum; and
therefore, outside the peritoneum
Tel, Ther, Joram, Roland Thurs, Feb. 24, 2011 Page 6 of 13
Vicente Francisco
Augustina R. Hizon, M.D.
D. Abelardo, MD, Patho 1
FPCR, FPROS, FUSP,
FPSP, FESTRO, FPSO
MIAC 2
OS 214
OS 215 Digestionand
Reproduction and Excretion
Hormonal Regulation F
Gastrointestinal
Lec 2A: Pathology ofTract Imaging
the Female Genital Tract (Vulva and Vagina)
• Small Intestinal Series (will be tackled later)
STOMACH & DUODENUM 3. CT-Scan – will not be able to see the small intestine well – due
to collapse; useful for locating nodes in malignancies
RADIOLOGIC STUDIES
4. MRI
1. Plain Abdomen X-Ray
ACID-RELATED DISORDERS
1. Gastritis
||> Radiologic Findings
• Acute
□ Mucosal erosions and shallow ulcers that do not
penetrate the gastric mucosa
Look for abnormal gas pattern, calcification, outline of liver, psoas • Chronic
shadow □ Mucosal thinning and atrophy which is why in
image below almost everything is contrast
2. Upper GastroIntestinal Series markings
||> Components:
• Esophagogram (refer to previous figures)
• Gastric Series
Gastric irregularities’ mucosal changes
2. Benign Ulcer Disease
||> Radiologic Findings
• Hampton’s Line – represents the edge of the over-
hanging gastric mucosa
• Ulcer Collar (pointed by arrow in the figure below)
• Ulcer Niche (adjacent )
• Edematous gastric folds radiating towards the ulcer
Gastric series: Check for the rugal patterns as well as the patency of the Gastro-
Duodenal junction. Normal gastric folds: Parallel to each other; Usually
smooth
• Duodenal Series
Edematous
Gastric Folds
Ulcer Collar
Ulcer Niche
Mucosal bump at the periphery/ ulcer collar; Turn it en passé --<>
Hampton’s line
3. Gastric Ulcer
Duodenal series: Loperamide or Buscopan are administered
for the relaxation of the Duodenum
- look for mucosal irregularities
- reading: spastic duodenum – refuses to relax
Buscopan – will dilate duodenum
Tel, Ther, Joram, Roland Thurs, Feb. 24, 2011 Page 7 of 13
Vicente Francisco
Augustina R. Hizon, M.D.
D. Abelardo, MD, Patho 1
FPCR, FPROS, FUSP,
FPSP, FESTRO, FPSO
MIAC 2
OS 214
OS 215 Digestionand
Reproduction and Excretion
Hormonal Regulation F
Gastrointestinal
Lec 2A: Pathology ofTract Imaging
the Female Genital Tract (Vulva and Vagina)
Irregular mucosa; Cecal shape; Does not expand
Hamptom’s Sign irregardless of contrast
• Gastric Lymphoma
□ The stomach is a very common extranodal site
for lymphomas
□ Characterized by mucosal elevations and
multiple erosions
□ Extraluminal: gentler curves as compared to an
intraluminal mass: distinct border from mass to
mucosa
4. Gastric Diverticulum (may develop from gastric ulcer due to
weakening of the walls; not much mucosal changes seen)
OTHER DISEASES
1. Diaphragmatic Hernia
GASTRIC CANCER ||> A defect or hole in the diaphragm that allows the
abdominal contents to move into the chest cavity
||> Radiologic Procedures ||> Treatment is usually surgical (make sure no part of the
• Contrast studies (UGIS): not used so much nowadays hernia is strangulated, it might cause Peritonitis)
• Endoscopic Ultrasound
• CT-Scan (Staging)
||> Radiologic Classification
• Type I : Polypoid (> 0.5 cm.)
• Type II : Superficial
□ IIA : elevated (>0.5 cm)
□ IIB : flat
□ IIC : depressed (erosions not extending beyond
Muscularis Mucosa)
• Type III: Excavated (Ulceration)
Diaphragmatic Hernia: Look for the portion of the stomach outside the
A B C hiatus
2. Duodenal Ulcer
||> Also known as Peptic Ulcer Disease (PUD)
||> Majority are associated with Helicobacter pylori infections
||> Most Peptic Ulcers arise from the Duodenum (rather than
the Stomach)
Stomach (Gastric) Cancer: A. Antral Cancer compressing the pylorus; ||> Are generally benign
filling defect B. intraluminal mass; C. Note the irregular borders.
||> Examples
• Linitis Plastica (Diffuse Infiltrative Carcinoma)
□ A Diffuse infiltrative Carcinoma of the Stomach
□ Also known as Brinton’s Disease or Leather
Bottle Stomach
Antrum: ulcer NICHE at the proximal part of the duodenum
Leather Bottle Sign
Tel, Ther, Joram, Roland Thurs, Feb. 24, 2011 Page 8 of 13
Vicente Francisco
Augustina R. Hizon, M.D.
D. Abelardo, MD, Patho 1
FPCR, FPROS, FUSP,
FPSP, FESTRO, FPSO
MIAC 2
OS 214
OS 215 Digestionand
Reproduction and Excretion
Hormonal Regulation F
Gastrointestinal
Lec 2A: Pathology ofTract Imaging
the Female Genital Tract (Vulva and Vagina)
• Also known as Ileocecal Tuberculosis
• Difficult to differentiate from Crohn’s Disease
• Can be seen as irregularities in the Terminal Ileum
3. Ileocecal TB with Abscess
Duodenal Ulcer: Note the folds toward the ulcer niche. The walls are
edematous.
SMALL INTESTINES
RADIOLOGIC STUDIES
1. Plain X-ray
2. Small Intestinal Series 4. Periappendiceal Abscess
||> The Ileum has a feathery appearance as compared to the ||> Usually results from the perforation of an acutely inflamed
Jejunum appendix
A B
SMALL INTESTINAL DISEASES A periappendiceal abscess in a localized area of displacement of
the small intestine
1. Crohn’s Disease
5. Small Intestinal Parasite
• Most common non-specific inflammatory disease of the
Small Intestines
• See thickened folds and mucosal irregularities
• If chronic – narrowing- string or rat-tail
• Findings of small fistula
• Also known as Inflammatory Bowel Disease (IBD)
• Radiologic Findings:
• Thickened intestinal folds
• Fistulas, Sinuses, and thickening/retraction of the
Mesentery
• String Sign – tubular narrowing of the lumen of the
small intestines
• Transmural type of Inflammation (Inflammation may Adult ascaris in the small intestine: Barium-based contrast agents
span the entire thickness of the Intestinal wall): Fine can irritate the worm and promote its migration in other organs like
Granular Pattern Nodular Mucosa (Submucosal the liver. Sometimes, the patient may even expel vomitus with the
Edema) Ulceronodular Mucosa Ulcerations worm.
LARGE INTESTINES & RECTUM
RADIOGRAPHIC EVALUATION
1. Plain Abdominal X-Ray
Crohn’s Disease: Note the thickened mucosal folds
2. Ileocecal Koch’s
Tel, Ther, Joram, Roland Thurs, Feb. 24, 2011 Page 9 of 13
Vicente Francisco
Augustina R. Hizon, M.D.
D. Abelardo, MD, Patho 1
FPCR, FPROS, FUSP,
FPSP, FESTRO, FPSO
MIAC 2
OS 214
OS 215 Digestionand
Reproduction and Excretion
Hormonal Regulation F
Gastrointestinal
Lec 2A: Pathology ofTract Imaging
the Female Genital Tract (Vulva and Vagina)
2. Barium Enema (Single or Double Contrast)
• Also known as Lower Gastrointestinal Series. X-ray
pictures are taken while barium sulfate fills the colon via
the rectum.
• Air may be puffed to provide air contrast into the colon to
distend it and provide better images (often called a
"double-contrast" exam). There is a risk for hypotension
associated with valsalva in the elderly undergoing this
procedure.
4. Ultrasound
Double contrast improves visualization of the mucosa
5. Abdominal CT-Scan
||> If there is a suspected bowel perforation, a water-soluble
contrast is used instead of barium. 6. Rice-Wangensteen Radiograph
||> The Rice-Wangensteen radiographic technique is an
inverted lateral radiograph of an infant
||> It is performed when the baby is at least 6 hours old
||> The baby is turned upside down in a lateral position with
the hips flexed
||> Mainly used for the assessment of an Imperforate Anus
Wangensteen-Rice radiograph: The infant is held in invert position.
Triangular metallic marker identifies the anal dimple. The arrow
points to the occlusion on the lateral view. Additional UTZ
examination helps to decide the real extent of the rectal atresia.
The distal blind pouch plugged with meconium (outlined) disturbs
A and B. Supine image, Arrow points to the insertion of the foley the judgment of the exact level of atresia.
catheter that introduces the contrast until the level of the splenic
flexure; C. Lateral Decubitus image. Note the smooth mucosal
surface of the colon visualized by Barium Enema. DISEASES OF THE COLON AND RECTUM
Post evacuation radiography 1. Congenital Disorders
||> Hirschsprung’s Disease
• Also known as Aganglionic Megacolon
• Enlargement of the colon secondary to bowel
obstruction caused by the persistent contraction of a
part of the colon with absent enteric nerves (hence the
term ‘aganglionic’) for relaxation
Redundant rectosigmoid colon
• condition where extra loops form, resulting in a longer
than normal colon; a mass is felt and then
disappears/changes place; presents with constipation
||> Congenital Rectal Atresia
3. Defecography ||> Imperforate Anus
• Also known as Defecating Proctogram
• An imaging study in which the mechanics of a patient’s
defecation are visualized real-time, with the use of a
fluoroscope 2. Diverticula
• Not done anymore
Tel, Ther, Joram, Roland Thurs, Feb. 24, 2011 Page 10 of 13
Vicente Francisco
Augustina R. Hizon, M.D.
D. Abelardo, MD, Patho 1
FPCR, FPROS, FUSP,
FPSP, FESTRO, FPSO
MIAC 2
OS 214
OS 215 Digestionand
Reproduction and Excretion
Hormonal Regulation F
Gastrointestinal
Lec 2A: Pathology ofTract Imaging
the Female Genital Tract (Vulva and Vagina)
Dangerous if spiculed: May rupture
□ Ileocecal Tuberculosis with Abscess: mucosal
irregularities indicate inflammation
3. Inflammatory Diseases
||>Ulcerative Colitis
• Radiologic Findings:
□ Acute
Fine granulations
Stippled appearance
of the mucosa
Failure of the colonic
walls to collapse on
post-evacuation study 4. Polyps - there’s a filling defect
□ Chronic ||> Morphologic Types
Loss of haustral markings • Sessile
Coarse granulations (due to multiple □ Broad base
ulcerations which increase in size and number) □ With mound-like protuberances or flattened
affecting the entire length of the colon plaques
Accompanied by polypoid changes • Pedunculated
• Secondary Changes: □ With stalks
□ Foreshortening of the
Colon
□ Lack of haustrations
markings and tubular
narrowing (Stove-pipe or
Garden-hose sign)
□ Increase in Presacral
space (> 1 cm)
□ Fibrosis or strictures may
develop
5. Malignancies
□ Increase in presacral
space ||> Radiographic Patterns
• Annular Constricting
CECAL ABSCESS:
□ Apple-core appearance (mass is black part beside the core)
||> Granulomatous Colitis
• i.e. Crohn’s Disease
• Polypoid
||> Infectious Colitis
• Examples:
□ Cecal Abscess:appears almost the same as a
malignant mass
• Infiltrating or Stenosing
Tel, Ther, Joram, Roland Thurs, Feb. 24, 2011 Page 11 of 13
Vicente Francisco
Augustina R. Hizon, M.D.
D. Abelardo, MD, Patho 1
FPCR, FPROS, FUSP,
FPSP, FESTRO, FPSO
MIAC 2
OS 214
OS 215 Digestionand
Reproduction and Excretion
Hormonal Regulation F
Gastrointestinal
Lec 2A: Pathology ofTract Imaging
the Female Genital Tract (Vulva and Vagina)
• Manifests with the String Sign
• Ulcerative
Filling defect in the cecum.
LIVER, HEPATOBILIARY TREE & GALLBLADDER
RADIOGRAPHIC TECHNIQUES
1. Ultrasonography procedure of choice
2. ERCP (Endoscopic Retrograde Cholangiopancreatography)
3. CT-Scan
4. MRI
5. MRS (Magnetic Resonance Spectroscopy)
6. Nuclear Medicine (Radionuclide Scanning)
LIVER
6. Others ||> Radiologic Evaluation:
||> Redundant RectoSigmoid Colon 1. CT-Scan – more expensive&detailed; not used for
screening, just for diagnostic purposes
2. MRI
3. Ultrasound
Ultrasound with Doppler – flow can be visualized
4. Angiography
• Done in the Operating Room usually for
checking/screening for Hemangiomas and other
tumors
• Transfemoral catheter through femoral artery then
abdominal aorta then organ of choice
||> Rectal Foreign Body 5. Nuclear (Radioisotope) Scanning
• For ‘hotspots’i.e. Ultrasound with Doppler
A B
C D
You don’t call this the bottle sign. This film
shows an actual bottle claimed to be seated
upon “accidentally”
||> Large and Small Intestine Fistula C
- usually iatrogenic
||> Cecal Cancer
Tel, Ther, Joram, Roland Thurs, Feb. 24, 2011 Page 12 of 13
Vicente Francisco
Augustina R. Hizon, M.D.
D. Abelardo, MD, Patho 1
FPCR, FPROS, FUSP,
FPSP, FESTRO, FPSO
MIAC 2
OS 214
OS 215 Digestionand
Reproduction and Excretion
Hormonal Regulation F
Gastrointestinal
Lec 2A: Pathology ofTract Imaging
the Female Genital Tract (Vulva and Vagina)
Radiologic Evaluation of the Liver. A. CT-Scan; B. MRI; C. Ultrasound,
Normal liver is clear; D. Angiography; and E. Nuclear (Radioisotope)
Scanning (Blue Areas = arterial system and red areas = venous
system)
||> Diseases of the Liver:
1. Tuberculosis of the Liver
A normal cholecystogram. (left) In the initial phase the contrast
medium is seen evenly filling the gal/bladder, the walls of which are
smooth. (right) After a fatty meal, the gallbladder has contracted.
Now both the fundus and the neck of the gallbladder, as well as the
cystic duct is filled with contrast medium and the common bile duct
is demonstrated (arrows).
• Gallstones
The Liver is large with calcifications
2. Subcapsular Hematoma
Gallstones are usually moving in contrast to malignant growths.
If dark mostly fluid; If something becomes bight malignancy; if a lot
of vessels hemangioma
3. Fatty Liver-
• liver brighter than kidneys cholesterol deposits
HEPATOBILIARY TREE
||> Radiologic Evaluation:
1. T-Tube Cholangiography
• If it is done poorly air bubbles will be misinterpreted
as gall stones
• A fluoroscopic procedure in which contrast medium is
A sonogram of a fatty liver showing increased echotexture compared injected through a T-tube into the patient’s Biliary tree
with the adjacent kidney (bright liver). The white round structures on • The T-tube (a tubular device in the shape of the letter
the right sonogram correspond to fats. T) is most commonly inserted during a
cholecystectomy operation when there is a possibility
of having residual gallstones within the Biliary tree
GALLBLADDER
||> Unseen in normal radiographs; unless it is distended or stone-
containing
||> Radiologic Evaluation:
1. Plain Abdomen X-ray
2. Ultrasound
2. ERCP (Endoscopic Retrograde
Cholangiopancreatography)
The normal gallbladder (gb) is seen as a cystic structure with echo- - to view pancreatic and biliary tree
free contents. The walls of the gallbladder are smooth. Normal liver
parenchyma (L) is seen to the left of the gallbladder.
3. Oral Cholecystography
Tel, Ther, Joram, Roland Thurs, Feb. 24, 2011 Page 13 of 13
Vicente Francisco
Augustina R. Hizon, M.D.
D. Abelardo, MD, Patho 1
FPCR, FPROS, FUSP,
FPSP, FESTRO, FPSO
MIAC 2
OS 214
OS 215 Digestionand
Reproduction and Excretion
Hormonal Regulation F
Gastrointestinal
Lec 2A: Pathology ofTract Imaging
the Female Genital Tract (Vulva and Vagina)
||> Diseases of the Biliary Tree:
1. Biliary Ascariasis
2. Pancreatic Mass
If still alive, a white line is seen inside since the parasite is still swallowing.
2. Retained Biliary Stone/Sludge
PANCREAS
RADIOGRAPHIC TECHNIQUES
1. Ultrasonography
2. CT-Scan
DISEASES OF THE PANCREAS
1. Pancreatitis
||> Irregularities and swelling in the Pancreas are observed
here
Tel, Ther, Joram, Roland Thurs, Feb. 24, 2011 Page 14 of 13
S-ar putea să vă placă și
- Tumours of Larynx: A Clinicopathological StudyDe la EverandTumours of Larynx: A Clinicopathological StudyÎncă nu există evaluări
- Xray Kub My Prep FinalDocument109 paginiXray Kub My Prep FinalphoenixibexÎncă nu există evaluări
- Cushing Triad: Bradycardia, Wide Pulse Irregular RespirationsDocument3 paginiCushing Triad: Bradycardia, Wide Pulse Irregular RespirationsZachary T HallÎncă nu există evaluări
- Diagnostic Exam For Bones, Joints and Muscles: 1. Bone Density Test For Osteoporosis BackgroundDocument14 paginiDiagnostic Exam For Bones, Joints and Muscles: 1. Bone Density Test For Osteoporosis BackgroundRoel MarañoÎncă nu există evaluări
- MS Final 49 UrinaryDocument3 paginiMS Final 49 UrinaryZachary T HallÎncă nu există evaluări
- Chest X-Ray InterpretationDocument14 paginiChest X-Ray InterpretationKoya AnushareddyÎncă nu există evaluări
- Gastrointestinal System DisordersDocument112 paginiGastrointestinal System DisordersTaate MohammedÎncă nu există evaluări
- CT KubDocument2 paginiCT KubKumail KhandwalaÎncă nu există evaluări
- Cranial Nerve AssessmentDocument4 paginiCranial Nerve AssessmentAnonymous h2EnKyDbÎncă nu există evaluări
- Health Questionnaire CandidateDocument5 paginiHealth Questionnaire CandidateSaudia Arabia JobsÎncă nu există evaluări
- Drug Therapy For GI Disorders PDFDocument5 paginiDrug Therapy For GI Disorders PDFmeeraÎncă nu există evaluări
- Genitourinary System: 1. Hair DistributionDocument9 paginiGenitourinary System: 1. Hair DistributionPaul Vincent100% (1)
- Fluid & Electrolite Management in Surgical WardsDocument97 paginiFluid & Electrolite Management in Surgical WardsBishwanath PrasadÎncă nu există evaluări
- Assessing The Thorax and LungsDocument3 paginiAssessing The Thorax and LungsZJ GarcianoÎncă nu există evaluări
- Breath Sounds: ConsiderationsDocument10 paginiBreath Sounds: ConsiderationsKarl RobleÎncă nu există evaluări
- 1538 Exam 4 Cell Reg & GriefDocument35 pagini1538 Exam 4 Cell Reg & GriefJade EdanoÎncă nu există evaluări
- Patient Discharge Assessment Nursing Diagnosi S Planning Intervention Rationale EvaluationDocument3 paginiPatient Discharge Assessment Nursing Diagnosi S Planning Intervention Rationale EvaluationVILLANUEVA ARASELÎncă nu există evaluări
- Hip Fracture of Proximal Femur SOAP COMPLETEDocument10 paginiHip Fracture of Proximal Femur SOAP COMPLETEEj TuliaoÎncă nu există evaluări
- MC HeparinDocument7 paginiMC HeparinCliff by the seaÎncă nu există evaluări
- IV Solution Cheat SheetDocument1 paginăIV Solution Cheat SheetMelanie KudoÎncă nu există evaluări
- 3 Antimuscarinic AgentsDocument13 pagini3 Antimuscarinic Agentsmatchees-gone rogueÎncă nu există evaluări
- Clinical Features of Renal DiseaseDocument80 paginiClinical Features of Renal DiseaseIdiAmadouÎncă nu există evaluări
- Cervical CA Case StudyDocument32 paginiCervical CA Case StudyCandy Mae Kabayao CuraÎncă nu există evaluări
- RT 302 Prelim NotesDocument65 paginiRT 302 Prelim NotesNikko L. PescuesoÎncă nu există evaluări
- Lumber Spine and Pelvis RadiographyDocument84 paginiLumber Spine and Pelvis RadiographyMunish DograÎncă nu există evaluări
- Chronic Bowel Disease and SepsisDocument52 paginiChronic Bowel Disease and SepsisOlga Goryacheva100% (1)
- Non Surgical Treatment Modalities of SCCHN: Presentation by Post Gradute StudentDocument113 paginiNon Surgical Treatment Modalities of SCCHN: Presentation by Post Gradute StudentZubair VajaÎncă nu există evaluări
- Chest RadiographyDocument19 paginiChest RadiographyClaraMonet PalomoÎncă nu există evaluări
- Head & Neck TumorsDocument4 paginiHead & Neck TumorsDez RayosÎncă nu există evaluări
- The Radiology AssistantDocument30 paginiThe Radiology AssistantIcha IchaÎncă nu există evaluări
- Muscarinic and Anti-MuscarinicsDocument3 paginiMuscarinic and Anti-MuscarinicsElleJBÎncă nu există evaluări
- Carcinoma of The Breast - Bailey & LoveDocument5 paginiCarcinoma of The Breast - Bailey & LoveKeyshia Yazid100% (1)
- LungsDocument16 paginiLungsJoher100% (1)
- (1479683X - European Journal of Endocrinology) Geographic Variations in The Frequency of Thyroid Disorders and Thyroid Peroxidase Antibodies in Persons Without Former Thyroid Disease Within GermanyDocument9 pagini(1479683X - European Journal of Endocrinology) Geographic Variations in The Frequency of Thyroid Disorders and Thyroid Peroxidase Antibodies in Persons Without Former Thyroid Disease Within GermanyArul ThiyagarajanÎncă nu există evaluări
- NCM 106Document13 paginiNCM 106Calimlim KimÎncă nu există evaluări
- Laryngeal CA MangaserDocument26 paginiLaryngeal CA MangaserBob McRonieÎncă nu există evaluări
- Dulcolax Stool Softener Supp (Docusate Sodium)Document2 paginiDulcolax Stool Softener Supp (Docusate Sodium)EÎncă nu există evaluări
- Nervous System NotesDocument13 paginiNervous System Noteschryan1989100% (1)
- NUR100 Sherpath CH 44 PainDocument23 paginiNUR100 Sherpath CH 44 Paincaloy2345caloyÎncă nu există evaluări
- Presentation Cervical SpineDocument48 paginiPresentation Cervical Spinekholoodrezeq8752Încă nu există evaluări
- Myasthenia Gravis: An Autoimmune Neurologic DisorderDocument16 paginiMyasthenia Gravis: An Autoimmune Neurologic DisorderHibba NasserÎncă nu există evaluări
- Hip FractureDocument4 paginiHip Fracturemariafub100% (1)
- Shock TypesDocument25 paginiShock TypesMuqeet76Încă nu există evaluări
- Pharm Fall Cardiovascular Pharmacology Study Guide-106Document47 paginiPharm Fall Cardiovascular Pharmacology Study Guide-106sean liyanageÎncă nu există evaluări
- Carpal Tunnel Surgery, Hand Clinics, Volume 18, Issue 2, Pages 211-368 (May 2002)Document151 paginiCarpal Tunnel Surgery, Hand Clinics, Volume 18, Issue 2, Pages 211-368 (May 2002)alinutza_childÎncă nu există evaluări
- SchizophreniaDocument43 paginiSchizophreniaJun TangonanÎncă nu există evaluări
- Types of CancerDocument7 paginiTypes of CancerRegina SABSÎncă nu există evaluări
- UntitledDocument6 paginiUntitledFritz Angelo BullonÎncă nu există evaluări
- NEUROPrelims - Cranial Nerves and Neurological ExaminationDocument37 paginiNEUROPrelims - Cranial Nerves and Neurological ExaminationRenatoCosmeGalvanJuniorÎncă nu există evaluări
- Endocrine DisordersDocument3 paginiEndocrine DisordersIrish OrleansÎncă nu există evaluări
- The Balanced Skeletal TractionDocument1 paginăThe Balanced Skeletal TractionGemarie Adarlo CastilloÎncă nu există evaluări
- Oncology Lectures 1 7 DR - FerrolinoDocument24 paginiOncology Lectures 1 7 DR - FerrolinoMiguel Cuevas DolotÎncă nu există evaluări
- Wilkins 6 - Neurological Assessment - AssignmentDocument33 paginiWilkins 6 - Neurological Assessment - AssignmentArifurRahman100% (1)
- LUNG-OVERVIEW (Autosaved)Document132 paginiLUNG-OVERVIEW (Autosaved)Thivashinie Kandy Nazan VelloÎncă nu există evaluări
- PP Drug Classes and IndicationsDocument67 paginiPP Drug Classes and IndicationspninthemakinÎncă nu există evaluări
- A Case of Rectus Sheath HematomaDocument4 paginiA Case of Rectus Sheath HematomadrthirÎncă nu există evaluări
- Avascular NecrosisDocument3 paginiAvascular Necrosisahmad shaltoutÎncă nu există evaluări
- GastrectomyDocument13 paginiGastrectomyrhopmaeÎncă nu există evaluări
- Osteoarthritis: Uyenvy Pham, M.D. Swedish Geriatric Fellow March 22, 2011Document45 paginiOsteoarthritis: Uyenvy Pham, M.D. Swedish Geriatric Fellow March 22, 2011Saya MenangÎncă nu există evaluări
- Flucloxacillin AFTcapssolnDocument6 paginiFlucloxacillin AFTcapssolnEliza ArmanÎncă nu există evaluări
- Laboratory Skills Session On RadiologyDocument7 paginiLaboratory Skills Session On Radiologyupcm2014blockAÎncă nu există evaluări
- Chapter 6Document11 paginiChapter 6KurbulÎncă nu există evaluări
- LU IV SUBSTANCE ABUSE - Jan 2011Document67 paginiLU IV SUBSTANCE ABUSE - Jan 2011upcm2014blockAÎncă nu există evaluări
- Substance AbuseDocument4 paginiSubstance Abuseupcm2014blockAÎncă nu există evaluări
- 2014 A OS211 Rehab of Neurogenic Bladder, Bowel, Spine TransDocument9 pagini2014 A OS211 Rehab of Neurogenic Bladder, Bowel, Spine Transupcm2014blockAÎncă nu există evaluări
- Epulis KongenitalDocument3 paginiEpulis KongenitalFriadi NataÎncă nu există evaluări
- Borg0040 Ifu 2020-06-29 Ka-Ab Lot 127 - PTDocument32 paginiBorg0040 Ifu 2020-06-29 Ka-Ab Lot 127 - PTyousrazeidan1979Încă nu există evaluări
- DUE of PIPERACILLIN and TazobactumDocument73 paginiDUE of PIPERACILLIN and Tazobactumanup jagarlamudiÎncă nu există evaluări
- Teaching PlanDocument6 paginiTeaching PlanAnthony BasantaÎncă nu există evaluări
- A 55-Year-Old Woman With Shock and Labile Blood PressureDocument11 paginiA 55-Year-Old Woman With Shock and Labile Blood PressureMr. LÎncă nu există evaluări
- Episode ListDocument25 paginiEpisode ListhectorÎncă nu există evaluări
- 6 Birth DefectsDocument40 pagini6 Birth DefectsjulieÎncă nu există evaluări
- Basic Knee Arthroscopy Part 4Document2 paginiBasic Knee Arthroscopy Part 4Diego BellingÎncă nu există evaluări
- Urology Resident Handbook3380 PDFDocument65 paginiUrology Resident Handbook3380 PDFKeserovic AdmirÎncă nu există evaluări
- Manajemen Nyeri Dengan DexketoprofenDocument27 paginiManajemen Nyeri Dengan Dexketoprofenmaya santiÎncă nu există evaluări
- Family Systems: Genograms and Ecomaps: Dr. Mergan Naidoo Principal Family PhysicianDocument42 paginiFamily Systems: Genograms and Ecomaps: Dr. Mergan Naidoo Principal Family PhysicianWendy LucasÎncă nu există evaluări
- 69-Article Text-283-2-10-2022Document8 pagini69-Article Text-283-2-10-2022EfanÎncă nu există evaluări
- Florida Nurse-Practice-ActDocument117 paginiFlorida Nurse-Practice-Actapi-251653314Încă nu există evaluări
- Gastric Outlet Obstruction: BY: Tharun Balaji Vinay GautamDocument19 paginiGastric Outlet Obstruction: BY: Tharun Balaji Vinay Gautam7hhdfc8vmwÎncă nu există evaluări
- Basic Life Support in Infants and ChildrenDocument9 paginiBasic Life Support in Infants and ChildrenMelissa Espinoza PeñaÎncă nu există evaluări
- HematuriaDocument32 paginiHematuriaSurya Nirmala DewiÎncă nu există evaluări
- Parameters of Automated Cell Counter Automation in Hematology Laboratory and CBC Via Automated Blood AnalyzerDocument40 paginiParameters of Automated Cell Counter Automation in Hematology Laboratory and CBC Via Automated Blood AnalyzerArslan Arshad100% (1)
- Science 6 - Q2 - L4 - Parts and Function of Excretory SystemDocument28 paginiScience 6 - Q2 - L4 - Parts and Function of Excretory SystemSonny Matias100% (1)
- Hepatitis in Children (Hep A, B, C)Document26 paginiHepatitis in Children (Hep A, B, C)sarÎncă nu există evaluări
- Appeal Letter FfsDocument1 paginăAppeal Letter FfsAndrea LaBarberaÎncă nu există evaluări
- ApoB 2Document7 paginiApoB 2Alex AlexÎncă nu există evaluări
- ACL Postop Instructions - HagenDocument7 paginiACL Postop Instructions - HagenkapsicumadÎncă nu există evaluări
- Jurnal Nausea and VomitingDocument15 paginiJurnal Nausea and VomitingRisa KarmeylithaÎncă nu există evaluări
- DR Swamy's Stations For Precourse PreparationDocument71 paginiDR Swamy's Stations For Precourse PreparationdrsadafrafiÎncă nu există evaluări
- CRE Fixed Wire Balloon Dilatation CatheterDocument2 paginiCRE Fixed Wire Balloon Dilatation CathetermaassingerÎncă nu există evaluări
- FCE Use ESOL 3Document2 paginiFCE Use ESOL 3Fran PasteriÎncă nu există evaluări
- (Pharma-TRANS) 2.09 Geriatric Pharmacology: D. Protein BindingDocument2 pagini(Pharma-TRANS) 2.09 Geriatric Pharmacology: D. Protein BindingStudy ReviewersÎncă nu există evaluări
- Orthokeratology: Orthokeratology (Ortho-K) Is The Fitting of Specially Designed GasDocument4 paginiOrthokeratology: Orthokeratology (Ortho-K) Is The Fitting of Specially Designed GasPUSHPAK DASGUPTAÎncă nu există evaluări
- Course Specification Template EmergencyDocument6 paginiCourse Specification Template EmergencyWael LotfyÎncă nu există evaluări
- Daily Progress NotesDocument2 paginiDaily Progress NotesMuhammad Bilal100% (1)