Documente Academic
Documente Profesional
Documente Cultură
Orthodontic and Non - Orthodontic Root Resorption
Încărcat de
Gaurav PoplaiDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Orthodontic and Non - Orthodontic Root Resorption
Încărcat de
Gaurav PoplaiDrepturi de autor:
Formate disponibile
Orthodontic and Nonorthodontic Root
Resorption: Their Impact on Clinical
Dental Practice
Vincent G. Kokich, D.D.S., M.S.D.
Abstract: Occasionally, general dentists are challenged with providing restorative treatment for a postorthodontic patient who
has had moderate to severe root resorption. When this happens, a number of questions about the cause of such resorption and the
appropriate treatment arise in the dentist’s mind. This article will describe the orthodontic and restorative management of three
patients with severe maxillary incisor root resorption, provide a thorough discussion of the currently available literature on the
topic of root resorption, and answer clinical questions regarding this relatively infrequent but devastating sequel to orthodontic
treatment.
Dr. Kokich is Professor, Department of Orthodontics, School of Dentistry, University of Washington. Direct correspondence and
requests for reprints to him at Department of Orthodontics, School of Dentistry, University of Washington, Box 357446, Seattle,
WA 98195-7446; 206-543-5788 phone; 206-685-8163 fax; vgkokich@u.washington.edu.
Key words: postorthodontic root resorption
O
ccasionally, general dentists are challenged
with providing restorative treatment for a Orthodontic and
postorthodontic patient who has had mod-
erate to severe root resorption. When this happens, Restorative Management
a number of questions often arise in the minds of
dentists: What causes root resorption? Is it due to
of Three Patients
heavy orthodontic forces placed on the teeth? What
is the incidence of root resorption among orthodon- Case 1
tic patients? Is the tendency for root resorption This thirty-six-year-old female lobbyist was
inherited? What is the prognosis for teeth that have concerned about the esthetics of her smile (Figure
had significant root resorption? Will the resorptive 1A). She had received orthodontic treatment dur-
process continue? Can these teeth be safely restored? ing childhood, and her appliances were removed
Do they require root canal therapy? Do they need at age fifteen. Two maxillary first premolars had
to be splinted to the adjacent teeth? Should they be been removed to reduce her anterior overjet, but her
replaced with implants? What if the patient requires maxillary incisors suffered severe root resorption
further orthodontic therapy? Will the resorption during the orthodontic treatment (Figure 1B). Her
continue? Get worse? How does all of this affect maxillary right lateral incisor was hopeless and was
the placement of restorations? The answers to these extracted. A resin-bonded lingual splint had been in
questions are important for the dentist who inherits place for twenty years to replace the maxillary right
a patient with significant root resorption. lateral incisor and stabilize the remaining anterior
This article will describe the orthodontic and teeth. Now she wanted to improve the appearance of
restorative management of three patients with severe her smile. She had an anterior open bite and excess
maxillary incisor root resorption, provide a thorough overjet (Figure 1C). How would you restore this
discussion of the currently available literature on the patient’s anterior teeth?
topic of root resorption, and answer the aforemen- The options included extraction of the remain-
tioned clinical questions regarding this relatively ing incisors and the placement of either four implants
infrequent but devastating sequel to orthodontic or two implants and an implant-supported maxillary
treatment. anterior bridge. Another option would be to leave
the central incisors and replace the maxillary left
lateral incisor and missing right lateral incisors with
August 2008 ■ Journal of Dental Education 895
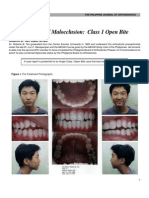
Figure 1. Orthodontic and restorative management of patient 1
This thirty-six-year-old patient was unhappy with the appearance of her maxillary anterior teeth (A). She had had previous orth-
odontic treatment, including the extraction of two maxillary first premolars. Moderate to severe root resorption had occurred,
so her anterior teeth were splinted with a cast lingual splint (B). However, her root length had not diminished in twenty years.
So her malocclusion was corrected (D), and the roots did not get shorter during the orthodontic retreatment (E). A provisional
bridge (F) was worn for one year. A six-unit porcelain-fused-to-metal bridge, shown five years after orthodontics (G, H, I), has
successfully restored esthetics and function and stabilized the teeth.
implants. A third option would be to place another had not suffered further root resorption of the central
resin-bonded splint. A fourth option would be to incisors during the twenty years after the original
remove the maxillary left lateral incisor and place a orthodontics, it was believed that further resorption
six-unit conventional bridge attached to the maxillary was not likely. Orthodontic appliances were placed
canines and central incisors replacing the lateral inci- on all teeth, the maxillary right central incisor was
sors. However, all plans required further orthodontic intruded to level the gingival margins between the
therapy in order to reduce the overjet, align the man- central incisors, the overjet was corrected, and the
dibular incisors, and close the open bite. open bite was closed (Figure 1D). No further root
After a thorough discussion among the perio- resorption occurred during the orthodontic therapy
dontist, orthodontist, general dentist, and patient, it (Figure 1E). A maxillary anterior provisional bridge
was decided that extraction of the left lateral incisor was worn for one year after the orthodontic treatment
and restoration of the remaining teeth with a con- (Figure 1F), and then a porcelain-fused-to-metal
ventional fixed bridge would not only improve the bridge was placed on the maxillary canines and
esthetics, but would also stabilize the central incisors central incisors and has been stable for five years
and canines with the short roots. Since the patient (Figure 1G, H, and I).
896 Journal of Dental Education ■ Volume 72, Number 8
Case 2 that time (Figure 2C). So, over the past four years,
This thirteen-year-old female had been under the pressure of the erupting maxillary canines had
the care of a pediatric dentist since age six. Her caused the resorption of the maxillary lateral inci-
mother decided to transfer her daughter to their sor roots.1 How would you eventually restore this
family general dentist. She was in the transitional patient? She obviously needed orthodontic therapy.
dentition and was erupting her maxillary canines Would implants be necessary to replace the lateral
(Figure 2A). incisors? If so, when?
The patient was congenitally missing her Since the patient was already missing her
maxillary right and left second premolars. Current maxillary right and left second premolars, and since
periapical radiographs showed that the maxillary she was too young for implants, it was decided that
right and left lateral incisors had severely resorbed the maxillary lateral incisors should not be extracted
roots (Figure 2B). This girl had never had previous until after the orthodontic treatment, so they could
orthodontic treatment. Periapical radiographs taken provide space for eventual implants. The orthodontic
by the pediatric dentist of the girl at age eight years treatment lasted over two years. However, at the end
showed that no root resorption had occurred up until of orthodontic therapy the patient was only fifteen
years of age, still growing, and therefore too young
Figure 2. Orthodontic and restorative management of patient 2
This thirteen-year-old female had been under the care of a pediatric dentist since age six years. She was now transferring to
the family dentist. Current periapical radiographs (B) reveal extensive resorption of the maxillary lateral incisor roots. Compari-
son with radiographs taken four years earlier (C) show that the root resorption was caused by the erupting maxillary canines.
Because the patient was too young for implants, the lateral incisors were maintained during the orthodontics (D), and she had
no further root resorption after bracket removal (E). The teeth were not mobile nor did they need restoration, so they were left for
the next thirteen years. At twenty-eight years of age, the patient’s alignment, esthetics, occlusion, and root length appear stable
(G, H, I).
August 2008 ■ Journal of Dental Education 897
for implants. So the maxillary lateral incisors were eight years of age (Figure 3A). However, for the past
not extracted (Figure 2D). No further root resorp- four years she had not been seen by the dentist due to
tion had occurred over the two years of orthodontics the divorce of her parents and custody issues regard-
(Figure 2E). An Essix retainer was worn in the ing their children. Current periapical radiographs
maxillary arch to help stabilize the teeth. After two show that this patient has had severe resorption of the
years, when the patient had completed her growth, maxillary right and left lateral incisors (Figure 3B).
the maxillary lateral incisor roots had not shortened A review of the periapical radiographs taken at ten
further, and the teeth were relatively stable (Figure years of age showed that the root resorption occurred
2F). So they were not extracted. Thirteen years after gradually as the maxillary canines erupted (Figure
completion of the orthodontic treatment, the patient 3C). This girl was unhappy with the hypoplastic ap-
was now twenty-eight years of age, and the lateral pearance of her maxillary anterior teeth and wanted
incisors were still stable with no further root resorp- to have her smile improved. The general dentist
tion (Figure 2G, H, and I). planned to temporarily bond the facial surfaces of
the central incisors with composite and to restore
Case 3 these teeth with porcelain veneers when she was
older. But what should be done with the maxillary
This fourteen-year-old female had been under
lateral incisors? This girl was still growing and too
the supervision of a general dentist since she was
Figure 3. Orthodontic and restorative management of patient 3
This fourteen-year-old girl had not seen her dentist for four years (A). Current radiographs (B), compared with those taken at age
ten (C), show that severe resorption of the maxillary lateral incisors occurred during the eruption of the maxillary canines. Minor
orthodontics was accomplished in nine months, and a bonded lingual splint was used to stabilize the teeth (D, E, F). Eventually,
porcelain veneers were placed on all four maxillary incisors, and after fifteen years, the maxillary anterior esthetics, occlusion,
and root length appear stable (G, H, I).
898 Journal of Dental Education ■ Volume 72, Number 8
young for implants. She needed some minor correc- cal studies have compared pre- and post-treatment
tive orthodontic treatment. periapical radiographs to determine the incidence
After consultation among the general dentist, of root resorption after orthodontic treatment.2-6
the orthodontist, and the patient and her mother, it However, radiographs only provide a crude two-
was decided that the lateral incisors not be extracted dimensional assessment of root resorption and will
until after orthodontics. The orthodontic treatment usually underestimate the true amount of root resorp-
lasted for nine months, and the roots of the lateral in- tion. Therefore, the only accurate assessment of root
cisors did not get any shorter during that time (Figure resorption must come from a histologic assessment of
3D and F). The incisors were bonded with composite the root surface after orthodontic movement. These
(Figure 3E), and a wire splint was bonded on the studies have been accomplished in both animals7 and
lingual to stabilize the teeth until the patient was old humans,8-10 and they clearly show that root resorp-
enough to have implants. At seventeen years of age, tion occurs in over 90 percent of the cases when a
the patient had stopped growing and was ready for tooth root is compressed against the alveolar socket.
implants. However, the gingival tissue and papillae Therefore, root resorption is a common sequel of
around the lateral incisors were healthy, at normal orthodontic movement.
levels, and the lateral incisors were immobile with Why does root resorption occur in response
the lingual splint. So it was decided that the resorbed to compression of the periodontal ligament? This
teeth, instead of being extracted, would be restored phenomenon is not completely understood, but re-
(along with the central incisors) with porcelain cent studies have found that the presence or absence
veneers and stabilized with a bonded lingual wire. of hyaline in the periodontal ligament affects the
Fifteen years after orthodontics, the lateral incisors incidence of root resorption.11 Hyalinization is a
were still present, the gingival and restorative esthet- common sequel after a compressive load is placed on
ics were good, and the roots had not resorbed any the periodontal ligament. Hyaline has been termed
further (Figure 3G, H, and I). sterile necrosis10 and forms in the interstitial space
within the periodontal ligament after a compressive
load is placed on a tooth root. Hyalinization of the
Discussion periodontal ligament usually occurs after a few days,
and the hyaline may remain within the periodontal
This article has demonstrated the long-term ligament up to four to eight weeks after initiation of
treatment and management of three patients with the compressive load.12,13 During this time, resorp-
severe root resorption. In one case, the root resorption tion of the alveolar socket is virtually prevented, and
was most likely caused by the orthodontic movement. undermining resorption of the alveolar bone may
In the other two cases, eruption of the maxillary occur.11 In addition, root resorption near the areas of
canines caused the resorption of the lateral incisor hyalinization will occur. After about eight weeks in
roots.1 However, the resorbed teeth were maintained. experimental animals, the hyaline has been removed
In two cases they were restored, and in all three cases from the periodontal ligament by macrophages, and
they have remained functional and esthetically natural at this time resorption of the alveolar socket wall
in appearance many years after completion of the occurs that permits the tooth to move.11 However, by
orthodontics and restorative dentistry. this time, extensive resorption lacunae are typically
When a general dentist inherits a patient with found along the length of the root surface.
moderate to severe orthodontic or nonorthodontic Why don’t we see more radiographic evidence
root resorption, the shortened roots on the periapical of root resorption in larger numbers of orthodontic
radiograph make the outlook for these teeth seem patients? Actually, these resorption lacunae will re-
hopeless. However, as one can see from these three pair themselves after the hyaline has been removed
cases, the outcome is far from hopeless. It is there- from the periodontal ligament and cementoblasts
fore important that general dentists understand the begin to secrete cellular cementum.11,14-17 Since most
incidence, cause, and outcome of root resorption of these resorption lacunae repair themselves with
in order to provide the best follow-up treatment time, there is little or no radiographic evidence of root
for their patients who experience this devastating resorption in the majority of orthodontic patients.
problem. What if the cementoblasts do not repair the resorp-
The first question to address is the incidence of tion lacunae? Then the patient may suffer moderate
root resorption in orthodontic patients. Several clini- to severe root resorption.
August 2008 ■ Journal of Dental Education 899
What is the incidence of moderate to severe been controversial. However, recent studies have
root resorption after orthodontic treatment? Sev- suggested that external apical root resorption can
eral radiographic assessments of consecutively be traced to a specific locus on a specific gene.23,25
treated populations of patients have been made to These researchers believe that external apical root
determine the prevalence of moderate to severe root resorption is a complex condition influenced by
resorption in both adolescent and adult populations many factors, with the IL-1B gene contributing an
of orthodontic patients. Moderate to severe root important predisposition to this common problem.
resorption is typically described as a greater than 20 Personally, I have treated two families of parent and
percent reduction in the original root length. Using child, where both experienced moderate to severe root
this definition, the incidence of moderate to severe resorption during orthodontic treatment. It is evident
root resorption in an adolescent sample2,5 is about 3 that more studies evaluating a genetic determination
percent. In adults,18 researchers have shown that the of root resorption susceptibility are needed.
incidence of moderate to severe root resorption is Do specific types of orthodontic movement
near 4 percent. lead to greater root resorption in susceptible patients?
Can root resorption be predicted? Previous Several authors have pointed out the negative impact
studies have used statistical comparisons of gender, of tooth intrusion on the severity of root resorption
pre-treatment root form, pre-treatment root length, in orthodontic patients.26,27 Perhaps this observation
length of orthodontic treatment, premolar extraction, is due to the method of analyzing root resorption
and linear amount of root movement as independent or root shortening on two-dimensional periapical
variables to determine if there are any accurate radiographs. Resorption of the root apex after tooth
predictors of root resorption related to orthodontic intrusion can be seen easily on two-dimensional
treatment. In general, three of these variables show radiographs, whereas the root resorption seen on
an association: amount of linear root movement, periapical radiographs after lateral root movement
length of orthodontic treatment, and premolar extrac- is not as clearly visible.
tion.5,6,19-22 If a patient were susceptible to significant What is the effect of root resorption on tooth
root resorption, then the farther the tooth is moved vitality? Although no studies have analyzed this
and the longer the duration of the orthodontic treat- relationship, from a clinical perspective I have not
ment, the more root resorption would likely occur. encountered a tooth with moderate to severe root re-
In addition, epidemiological studies show that pre- sorption whose pulp became nonvital. Unless there is
molar extraction cases tend to demonstrate more root some bacterial or traumatic insult to the tooth, pulp vi-
resorption in susceptible patients, probably because tality does not seem to be related to the amount of root
of the increased distance that the teeth move in ex- resorption experienced during orthodontic therapy.
traction cases. None of the pulps of the resorbed roots of the three
Does the amount of force used during or- patients illustrated in this article were nonvital.
thodontics affect the amount of root resorption? It What happens over the long term to tooth roots
seems logical that, in a susceptible sample, greater that have undergone moderate to severe root resorp-
orthodontic forces would cause more root resorption. tion? Researchers have reevaluated patients with
However, this assumption is not valid. Studies in both moderate to severe root resorption many years after
animals and humans have shown that the amount of orthodontics28-30 and have found that root resorption
force placed on a tooth root has neither a positive nor stops after orthodontic treatment has been discontin-
negative effect on the amount of root resorption.8,23 ued. Although there may be some remodeling of the
On the other hand, studies in humans have shown irregular resorbed edges of the root with time due to
that quadrupling the force on a tooth root does not reparative deposition of cellular cementum, this type
produce greater root resorption, but can increase the of remodeling merely produces a smoother surface
speed of root movement through the bone.9 Does it long term. However the length of the root does not
make a difference if the orthodontic force is continu- continue to shorten after orthodontic appliances have
ous or intermittent? Researchers have clearly shown been removed.
that although considerable variation typically exists, Do teeth with moderate to severe root resorption
continuous forces tend to produce more extensive require splinting? There are no studies that provide
root resorption than intermittent forces.13,14,24 us with the answer to this important clinical ques-
Is the tendency or susceptibility for root resorp- tion. In two of the cases presented in this article, the
tion an inherited trait? In the past, this question has teeth were splinted either with a conventional bridge
900 Journal of Dental Education ■ Volume 72, Number 8
or a bonded lingual wire. But these teeth required
restoration. In the third patient, no permanent reten- REFERENCES
tion other than a removal retainer was used for the 1. Heimisdottir K, Bosshardt D, Ruf S. Can the sever-
ity of root resorption be accurately judged by means of
patient. After thirteen years, the patient without a fixed
radiographs? A case report with histology. Am J Orthod
retainer has retained her severely resorbed maxillary Dentofacial Orthop 2005;128:106–9.
lateral incisors. However, this patient has a two-mil- 2. Sameshima GT, Sinclair PM. Characteristics of patients
limeter overjet in centric occlusion and does not have with severe root resorption. Orthod Craniofacial Res
any parafunctional or destructive occlusal habits. I 2004;7:108–14.
3. Smale I, Artun J, Behbehani F, Doppel D, van’t Hof M,
believe that parafunctional habits, crown mobility,
Kuijpers-Jagtman AM. Apical root resorption 6 months
and the need for restoration tend to determine the after initiation of fixed orthodontic appliance therapy. Am
necessity for a permanent lingual splint. If a patient J Orthod Dentofacial Orthop 2005;128:57–67.
has a protrusive bruxing habit with mobile maxillary 4. Artun J, Smale I, Behbehani F, Doppel D, van’t Hof M,
incisors and will require some sort of restoration of Kuijpers-Jagtman AM. Apical root resorption six and
these teeth, then perhaps splinting will help to avoid twelve months after initiation of fixed orthodontic appli-
ance therapy. Angle Orthod 2005;75:919–26.
the negative effects of each of these parameters. 5. Nigul K, Jagomagi T. Factors related to apical root re-
If the patient requires further orthodontic sorption of maxillary incisors in orthodontic patients.
treatment, will the roots continue to resorb? This Stomatologiia 2006;8:76–9.
research question has not been explored. However, 6. Mohandesan H, Ravanmehr H, Valaei N. A radiographic
most orthodontists have had to retreat patients who analysis of external apical root resorption of maxillary
incisors during active orthodontic treatment. Eur J Orthod
have had root resorption during an earlier phase of 2007;29:134–9.
orthodontic treatment. The three patients described 7. Maltha JC, van Leeuwen EJ, Dijkman GE, Kuijpers-
in this article all had orthodontic treatment ranging Jagtman AM. Incidence and severity of root resorption
in length from nine months to over two years, and the in orthodontically moved premolars in dogs. Orthod
tooth movement was started after the root resorption Craniofac Res 2004;7:115–21.
8. Owman-Moll P, Kurol J, Lundgren D. Effects of a doubled
had occurred. None of these patients exhibited any
orthodontic force magnitude on tooth movement and root
further root resorption as a result of the orthodontic resorption: an interindividual study in adolescents. Eur J
retreatment. However, in these cases I tried to limit Orthod 1996;18:141–50.
the amount of tooth movement, limit the length of 9. Owman-Moll P, Kurol J, Lundgren D. The effects of a
orthodontic treatment, and avoid intrusive tooth four-fold increased orthodontic force magnitude on tooth
movement and root resorption: an intra-individual study
movements. Also, histologic follow-up after root
in adolescents. Eur J Orthod 1996;18:287–94.
resorption showed that reparative dentin and cellular 10. Kurol J, Owman-Moll P. Hyalinization and root resorption
cementum form after the tooth movement had ceased. during early orthodontic tooth movement in adolescents.
Perhaps the presence of a cellular cemental layer Angle Orthod 1998;68:161–5.
plays some role in protecting the tooth root during 11. Iino S, Sakoda S, Ito G, Nishimori T, Ikeda T, Miyawaki
orthodontic retreatment. S. Acceleration of orthodontic tooth movement by alveolar
corticotomy in the dog. Am J Orthod Dentofacial Orthop
2007;131:448e1–448e8.
12. Von Bohl M, Maltha JC, Von Den Hoff JW, Kuijpers-
Summary and Conclusions Jagtman AM. Focal hyalinization during experimental
tooth movement in beagle dogs. Am J Orthod Dentofacial
Orthop 2004;125:615–23.
This article has described the treatment of three
13. Von Bohl M, Maltha J, Von Den Hoff H, Kuijpers-Jagtman
orthodontic patients who had experienced severe AM. Changes in the periodontal ligament after experimen-
root resorption but required further orthodontics. All tal tooth movement using high and low continuous forces
three patients had successful long-term outcomes by in beagle dogs. Angle Orthod 2004;74:16–25.
maintaining the severely resorbed roots. In addition 14. Owman-Moll P, Kurol J, Lundgren D. Continuous ver-
sus interrupted continuous orthodontic force related to
to illustrating the logic of the treatment plans as well
early tooth movement and root resorption. Angle Orthod
as the long-term effect, I have tried to answer the 1995;65:395–401.
key questions that arise in the mind of the general 15. Owman-Moll P. Orthodontic tooth movement and root
dentist when he or she inherits a patient with severe resorption with special reference to force magnitude
postorthodontic or nonorthodontic root resorption. and duration: a clinical and histological investigation in
Hopefully, this information will be clinically useful adolescents. Swed Dent J Suppl 1995;105:1–45.
16. Owman-Moll P, Kurol J. The early reparative process of
for the general dentist and orthodontist when plan- orthodontically induced root resorption in adolescents: lo-
ning treatment for these difficult situations. cation and type of tissue. Eur J Orthod 1998;20:727–32.
August 2008 ■ Journal of Dental Education 901
17. Jimenez-Pellegrin C, Arana-Chavez VE. Root resorp- 25. Al-Qawasmi RA, Hartsfield JK Jr, Everett ET, Flury L,
tion repair in mandibular first premolars after rotation: a Lui L, Foroud TM, et al. Genetic predisposition to external
transmission electron microscopy analysis combined with apical root resorption in orthodontic patients: linkage of
immunolabeling of osteopontin. Am J Orthod Dentofacial chromosome-18 marker. J Dent Res 2003;82:356–60.
Orthop 2007;132:230–6. 26. Han G, Huang S, Von den Hoff JW, Zeng X, Kuijpers-
18. Mirabella D, Artun J. Prevalence and severity of apical root Jagtman AM. Root resorption after orthodontic intrusion
resorption of maxillary anterior teeth in adult orthodontic and extrusion: an intra-individual study. Angle Orthod
patients. Eur J Orthod 1995;17:93–9. 2005;75:912–8.
19. Mirabella D, Artun J. Risk factors for apical root resorption 27. Harris DA, Jones AS, Darendeliler MA. Physical proper-
of maxillary anterior teeth in adult orthodontic patients. ties of root cementum: Part 8. Volumetric analysis of root
Am J Orthod Dentofacial Orthop 1995;108:48–55. resorption craters after application of controlled intrusive
20. Sameshima GT, Sinclair PM. Predicting and preventing light and heavy orthodontic forces: a microcomputed
root resorption: Part II. Treatment factors. Am J Orthod tomography scan study. Am J Orthod Dentofacial Orthop
Dentofacial Orthop 2001;119:511–5. 2006;130:639–47.
21. Fox N. Longer orthodontic treatment may result in 28. Remington DN, Joondeph DR, Artun J, Riedel RA,
greater external apical root resorption. Evid Based Dent Chapko MK. Long-term evaluation of root resorption
2005;6:21. occurring during orthodontic treatment. Am J Orthod
22. Segal GR, Schiffman PH, Tuncay OC. Meta analysis- Dentofacial Orthop 1989;96:43–6.
related factors of external apical root resorption. Orthod 29. Levander E, Malmgren O. Long-term follow-up of max-
Craniofac Res 2004;7:71–8. illary incisors with severe apical root resorption. Eur J
23. Al-Qawasmi RA, Hartsfield JK Jr, Everett ET, Flury L, Orthod 2000;22:85–92.
Lui L, Foroud TM, et al. Genetic predisposition to external 30. Becker A, Chaushu S. Long-term follow-up of severely
apical root resorption. Am J Orthod Dentofacial Orthop resorbed maxillary incisors after resolution of an etiologi-
2003;123:242–52. cally associated impacted canine. Am J Orthod Dentofa-
24. Owman-Moll P, Kurol J, Lundgren D. Repair of orthodon- cial Orthop 2005;127:650–4.
tically induced root resorption in adolescents. Angle
Orthod 1995;65:403–8.
902 Journal of Dental Education ■ Volume 72, Number 8
S-ar putea să vă placă și
- Orthodontically Driven Corticotomy: Tissue Engineering to Enhance Orthodontic and Multidisciplinary TreatmentDe la EverandOrthodontically Driven Corticotomy: Tissue Engineering to Enhance Orthodontic and Multidisciplinary TreatmentFederico BrugnamiÎncă nu există evaluări
- Earl's Pearls: Favorites from the PCSO BulletinDe la EverandEarl's Pearls: Favorites from the PCSO BulletinÎncă nu există evaluări
- A Comparison of Root Resorption Between Invisalign Treatment and Contemporary Orthodontic TreatmentDocument101 paginiA Comparison of Root Resorption Between Invisalign Treatment and Contemporary Orthodontic Treatmentplayer osamaÎncă nu există evaluări
- Mandibular Incisor Extraction TherapyDocument10 paginiMandibular Incisor Extraction TherapyLeonardo LamimÎncă nu există evaluări
- Implants in OrthodonticsDocument13 paginiImplants in OrthodonticsAnant JyotiÎncă nu există evaluări
- Open Bite CaseDocument10 paginiOpen Bite CaseezfreshÎncă nu există evaluări
- Application Form Spespciaistcialist Lists OrthodonticsDocument10 paginiApplication Form Spespciaistcialist Lists OrthodonticsCernei Eduard RaduÎncă nu există evaluări
- Retention Management Decisions A Review of Current Evidence and Emerging Trends 2017 Seminars in OrthodonticsDocument8 paginiRetention Management Decisions A Review of Current Evidence and Emerging Trends 2017 Seminars in Orthodonticsdruzair007Încă nu există evaluări
- Definitions & Branches or OrthodonticsDocument38 paginiDefinitions & Branches or OrthodonticsMohsin Habib100% (2)
- Relapse of Anterior Crowding 3 and 2017 American Journal of Orthodontics AnDocument13 paginiRelapse of Anterior Crowding 3 and 2017 American Journal of Orthodontics Andruzair007Încă nu există evaluări
- Extractions in Orthodontics PDFDocument2 paginiExtractions in Orthodontics PDFJohnÎncă nu există evaluări
- Esthetic in Pediatric DentistryDocument13 paginiEsthetic in Pediatric DentistryAtikahÎncă nu există evaluări
- Newer Orthodontic Archwires Imparting EfDocument244 paginiNewer Orthodontic Archwires Imparting EfSelvaArockiamÎncă nu există evaluări
- Journal Club1 / Orthodontic Courses by Indian Dental AcademyDocument19 paginiJournal Club1 / Orthodontic Courses by Indian Dental Academyindian dental academyÎncă nu există evaluări
- AJODO-2013 Angelieri 144 5 759Document11 paginiAJODO-2013 Angelieri 144 5 759osama-alali100% (1)
- Space Regainers in Pediatric DentistryDocument6 paginiSpace Regainers in Pediatric DentistryDiba Eka DiputriÎncă nu există evaluări
- Review Articles Annals and Essences of DentistryDocument5 paginiReview Articles Annals and Essences of DentistryminuÎncă nu există evaluări
- Trends in Orthodontics: by Julie Ann A. LumagueDocument6 paginiTrends in Orthodontics: by Julie Ann A. LumagueJulie Ann LumagueÎncă nu există evaluări
- Complete Denture Prosthodontics in Children With Ectodermal DysplasiaDocument29 paginiComplete Denture Prosthodontics in Children With Ectodermal DysplasiaAmit BhargavÎncă nu există evaluări
- Orthodontics AssignmentDocument4 paginiOrthodontics AssignmentTasneem SaleemÎncă nu există evaluări
- Managing Congenitally Missing Lateral Incisors. Part III: Single-Tooth ImplantsDocument9 paginiManaging Congenitally Missing Lateral Incisors. Part III: Single-Tooth ImplantsSalma RafiqÎncă nu există evaluări
- Transposition of A Maxillary Canine and A Lateral IncisoDocument11 paginiTransposition of A Maxillary Canine and A Lateral IncisoErik BarbosaÎncă nu există evaluări
- Harris - Root Resorption During Orthodontic Therapy - 2000 PDFDocument12 paginiHarris - Root Resorption During Orthodontic Therapy - 2000 PDFJamal GiriÎncă nu există evaluări
- Indirect Bracket Bonding Orthodontic IDB LAB Bonding Lab Set UpDocument77 paginiIndirect Bracket Bonding Orthodontic IDB LAB Bonding Lab Set UpPruessada DeeyingÎncă nu există evaluări
- CADCAM Vs Traditional Ceramic InlayDocument10 paginiCADCAM Vs Traditional Ceramic InlayAya Ibrahim YassinÎncă nu există evaluări
- Alexander DisiplineDocument17 paginiAlexander DisiplineAshish SharmaÎncă nu există evaluări
- Exo OrthoDocument8 paginiExo OrthoEndriyana NovitasariÎncă nu există evaluări
- Rapid MaxillaryDocument24 paginiRapid MaxillaryDon George GeojanÎncă nu există evaluări
- The Orthodontics Effective RoleDocument31 paginiThe Orthodontics Effective RoleHamza BelhajÎncă nu există evaluări
- A Review of Root Resorption in Orthodontics PDFDocument5 paginiA Review of Root Resorption in Orthodontics PDFRahulLife'sÎncă nu există evaluări
- Moving The TeethDocument117 paginiMoving The TeethThirunavukkarasu Srinivasan100% (2)
- Zachrisson Et Al 2011, Canine Substitution PDFDocument6 paginiZachrisson Et Al 2011, Canine Substitution PDFDiana BobÎncă nu există evaluări
- MANAGEMENT OF VERTICAL MAXILLARY EXCESS WWWDocument24 paginiMANAGEMENT OF VERTICAL MAXILLARY EXCESS WWWsweetieÎncă nu există evaluări
- Orthodontic Management of A Maxillary Midline Diastema Using Beggs Mechanics Case ReportDocument3 paginiOrthodontic Management of A Maxillary Midline Diastema Using Beggs Mechanics Case ReportEditor IJTSRDÎncă nu există evaluări
- Orthodontic Update - April 2020 PDFDocument54 paginiOrthodontic Update - April 2020 PDFMaria TzagarakiÎncă nu există evaluări
- Smile Analysis: A Review Part IIDocument4 paginiSmile Analysis: A Review Part IIGustavoAndresGarciaÎncă nu există evaluări
- Fixed Orthodontic Appliances: A Practical GuideDe la EverandFixed Orthodontic Appliances: A Practical GuideEvaluare: 1 din 5 stele1/5 (1)
- History of OrthodonticsDocument3 paginiHistory of OrthodonticsJuliusRanteÎncă nu există evaluări
- Molares InclinadosDocument13 paginiMolares Inclinadosmaria jose peña rojas100% (1)
- Mode of Action of Functional Appliances / Orthodontic Courses by Indian Dental AcademyDocument116 paginiMode of Action of Functional Appliances / Orthodontic Courses by Indian Dental Academyindian dental academyÎncă nu există evaluări
- Anchorage Control in Bioprogressive Vs Straight-Wire Treatment PDFDocument6 paginiAnchorage Control in Bioprogressive Vs Straight-Wire Treatment PDFsolodont1Încă nu există evaluări
- Early Treatment of Class III Malocclusion With Modified Tandem Traction Bow Appliance and A Brief Literature Review 2247 2452.1000644Document5 paginiEarly Treatment of Class III Malocclusion With Modified Tandem Traction Bow Appliance and A Brief Literature Review 2247 2452.1000644kinayungÎncă nu există evaluări
- Third Molars and Late Mandibular Incisor Crowding - A ReviewDocument12 paginiThird Molars and Late Mandibular Incisor Crowding - A ReviewMuthiaraPrazianditeÎncă nu există evaluări
- Arti. 27 A Century of Edgewise Appliance, VadenDocument11 paginiArti. 27 A Century of Edgewise Appliance, VadenLorena ParraÎncă nu există evaluări
- Prediction of Mandibular Growth Rotation, Assessment of The Skieller, Bjork and Linde-Hansen Method PDFDocument9 paginiPrediction of Mandibular Growth Rotation, Assessment of The Skieller, Bjork and Linde-Hansen Method PDFJose CollazosÎncă nu există evaluări
- Vertical Skeletal DysplasiaDocument119 paginiVertical Skeletal DysplasiaAshish Mathew0% (1)
- Retention and Relapse DR Shabeel PNDocument33 paginiRetention and Relapse DR Shabeel PNShabeel Pn100% (2)
- Principles of The Alexander DisciplineDocument5 paginiPrinciples of The Alexander DisciplineSarah Fauzia SiregarÎncă nu există evaluări
- Drugs in Orthodontics - 1Document43 paginiDrugs in Orthodontics - 1Sushma Rayal SAÎncă nu există evaluări
- OrthodonticsDocument14 paginiOrthodonticsimtiyazorthodontistÎncă nu există evaluări
- Adult OrthodonticsDocument70 paginiAdult OrthodonticsTruppti SononeÎncă nu există evaluări
- Analysis of Diagnostic RecordsDocument78 paginiAnalysis of Diagnostic RecordsAtika Iftikhar MirÎncă nu există evaluări
- Diagnostic Limitations of Cephalometrics in OrthodonticsDocument6 paginiDiagnostic Limitations of Cephalometrics in OrthodonticsDevata RaviÎncă nu există evaluări
- January 2018 1516198794 146 PDFDocument1 paginăJanuary 2018 1516198794 146 PDFGaby ZapataÎncă nu există evaluări
- Non XNDocument9 paginiNon XNNaveenÎncă nu există evaluări
- Deepbite Correction With Incisor Intrusion inDocument6 paginiDeepbite Correction With Incisor Intrusion inAbad SalcedoÎncă nu există evaluări
- Introduction To OrthodonticsDocument20 paginiIntroduction To OrthodonticsAroubÎncă nu există evaluări
- Asymmetric Extractions in Orthodontics PDFDocument6 paginiAsymmetric Extractions in Orthodontics PDFOsama MohamedÎncă nu există evaluări
- MARPE AbdAllah Bahaaa Ref NewDocument23 paginiMARPE AbdAllah Bahaaa Ref NewAya ElsayedÎncă nu există evaluări
- Dent 596 - OrthodonticsDocument6 paginiDent 596 - OrthodonticsAndrei JardanÎncă nu există evaluări
- Emax-Press-Monolithicsol Gi en - 672600 Rev1Document86 paginiEmax-Press-Monolithicsol Gi en - 672600 Rev1Fabio WenoÎncă nu există evaluări
- Pulpal Reactions To Caries and Dental ProceduresDocument58 paginiPulpal Reactions To Caries and Dental ProceduresSony RajbhandariÎncă nu există evaluări
- Multicenter Retrospective Analysis of Wide Neck Dental Implants For Single Molar ReplacementDocument1 paginăMulticenter Retrospective Analysis of Wide Neck Dental Implants For Single Molar ReplacementSurya TejaÎncă nu există evaluări
- Working Length Determination in RCTDocument38 paginiWorking Length Determination in RCTDidar Sadiq Kwekha100% (1)
- Periodontal Health During Orthodontic Treatment With Clear Aligners and Fixed AppliancesDocument21 paginiPeriodontal Health During Orthodontic Treatment With Clear Aligners and Fixed AppliancesabocoliÎncă nu există evaluări
- A Simplified Method For Fabricating Customized Arch Form: Clinical InnovationDocument3 paginiA Simplified Method For Fabricating Customized Arch Form: Clinical InnovationCLAUDIA MARCELA GUTIERREZ CARRANZAÎncă nu există evaluări
- Odontogenic Tumor PDFDocument93 paginiOdontogenic Tumor PDFEmad Alriashy100% (1)
- CVDocument5 paginiCVJuan Rafael SilvaÎncă nu există evaluări
- Effect of Enamel Bevel On The Clinical Performance of Resin Composite Restorations Placed in Non-Carious Cervical LesionsDocument11 paginiEffect of Enamel Bevel On The Clinical Performance of Resin Composite Restorations Placed in Non-Carious Cervical LesionsAna-Maria HriscuÎncă nu există evaluări
- Wennstrom J, Lindhe J, Nyman S. The Role of Keratinized Gingiva in Plaque-AssociatedDocument12 paginiWennstrom J, Lindhe J, Nyman S. The Role of Keratinized Gingiva in Plaque-AssociatedSebastián BernalÎncă nu există evaluări
- Topical Fluoride Nov 2019 IDA TIMESDocument2 paginiTopical Fluoride Nov 2019 IDA TIMESDrMrsAyeshaKhushnoorÎncă nu există evaluări
- The Bi-Helix Opening Spring For Lingual OrthodonticsDocument4 paginiThe Bi-Helix Opening Spring For Lingual OrthodonticsLedir Luciana Henley de AndradeÎncă nu există evaluări
- Comparision of Condylar Guidance Setting Obtained From A Wax Record Vs An Extra Oral TracingDocument6 paginiComparision of Condylar Guidance Setting Obtained From A Wax Record Vs An Extra Oral TracingHarsha ReddyÎncă nu există evaluări
- Implant Consent PDFDocument2 paginiImplant Consent PDFtomdienyaÎncă nu există evaluări
- Combined Technique For Bleaching Non-Vital Teeth With 6-Month Clinical Follow-Up: Case ReportDocument5 paginiCombined Technique For Bleaching Non-Vital Teeth With 6-Month Clinical Follow-Up: Case ReportPriska talithaÎncă nu există evaluări
- Post Graduate Student: Dr. RahultiwariDocument158 paginiPost Graduate Student: Dr. RahultiwariVivek Sunil EdayathÎncă nu există evaluări
- Pulpectomy PedoDocument30 paginiPulpectomy PedoFourthMolar.com100% (1)
- Altered Passive Eruption:a Case ReportDocument5 paginiAltered Passive Eruption:a Case ReportIJAR JOURNALÎncă nu există evaluări
- Periimplant Soft Tissue Management in Patients With A Fibula Free Flap Reconstruction Case Series and Description of A New TechniqueDocument6 paginiPeriimplant Soft Tissue Management in Patients With A Fibula Free Flap Reconstruction Case Series and Description of A New TechniqueSudheer KondakaÎncă nu există evaluări
- Pre-Prosthetic SurgeryDocument5 paginiPre-Prosthetic SurgeryŽäíñäb ÄljaÑabìÎncă nu există evaluări
- Library DocumentDocument3 paginiLibrary Documentrahi saungnaÎncă nu există evaluări
- Age-Dependent Biologic Response To Orthodontic Forces: Original ArticleDocument13 paginiAge-Dependent Biologic Response To Orthodontic Forces: Original ArticleAnushriya DuttaÎncă nu există evaluări
- Paramjit Kaur - Oral Cavity of NeonatesDocument27 paginiParamjit Kaur - Oral Cavity of Neonatesdr parveen bathlaÎncă nu există evaluări
- Nobel Rondo User ManualDocument16 paginiNobel Rondo User ManualAntonio PerazaÎncă nu există evaluări
- Andrews 6 Keys-1Document27 paginiAndrews 6 Keys-1Silky GroverÎncă nu există evaluări
- Face BowDocument24 paginiFace BowsavyasachinÎncă nu există evaluări
- Chapter Focus QuestionsDocument4 paginiChapter Focus Questionsapi-284521356Încă nu există evaluări
- of Mouth PreparationDocument106 paginiof Mouth PreparationDrSweta Gandhi100% (2)
- Final Draft of Interview TranscriptDocument7 paginiFinal Draft of Interview Transcriptapi-549369201Încă nu există evaluări
- Full-Mouth Disinfection For The Treatment of Adult Chronic Periodontitis (Review)Document52 paginiFull-Mouth Disinfection For The Treatment of Adult Chronic Periodontitis (Review)AshaAgrawalÎncă nu există evaluări