Documente Academic
Documente Profesional
Documente Cultură
J Infect Dis.-1999-Georges-s65-75 (Article Ebola Virus)
Încărcat de
David Brayan Reyna GomezTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
J Infect Dis.-1999-Georges-s65-75 (Article Ebola Virus)
Încărcat de
David Brayan Reyna GomezDrepturi de autor:
Formate disponibile
S65
Ebola Hemorrhagic Fever Outbreaks in Gabon, 1994–1997: Epidemiologic and
Health Control Issues
Alain-Jean Georges, Eric M. Leroy, André A. Renaut, Centre International de Recherches Médicales de Franceville,
Carol Tevi Benissan, René J. Nabias, Minh Trinh Ngoc, Franceville, Ministère de la Santé Publique, Faculté de Médecine,
Paul I. Obiang, J. P. M. Lepage,* Eric J. Bertherat,* Université Omar Bongo, Mission Française de Cooperation et d’Action
Culturelle, and Ministère de la Santé Publique, Libreville, Gabon
David D. Bénoni, E. Jean Wickings, Jacques P. Amblard,*
Joseph M. Lansoud-Soukate, J. M. Milleliri, Sylvain Baize,
and Marie-Claude Georges-Courbot*
From the end of 1994 to the beginning of 1995, 49 patients with hemorrhagic symptoms were
hospitalized in the Makokou General Hospital in northeastern Gabon. Yellow fever (YF) virus was
first diagnosed in serum by use of polymerase chain reaction followed by blotting, and a vaccination
campaign was immediately instituted. The epidemic, known as the fall 1994 epidemic, ended 6
weeks later. However, some aspects of this epidemic were atypical of YF infection, so a retrospective
check for other etiologic agents was undertaken. Ebola (EBO) virus was found to be present concomi-
tantly with YF virus in the epidemic. Two other epidemics (spring and fall 1996) occurred in the
same province. GP and L genes of EBO virus isolates from all three epidemics were partially
sequenced, which showed a difference of õ0.1% in the base pairs. Sequencing also showed that all
isolates were very similar to subtype Zaire EBO virus isolates from the Democratic Republic of the
Congo.
Downloaded from jid.oxfordjournals.org by guest on May 8, 2011
Johnson et al. [1] isolated and identified Ebola (EBO) virus associated with a mortality rate similar to that seen during the
from human cases during a 1976 epidemic of hemorrhagic DRC and Sudan epidemics [7].
fever (HF) in the Democratic Republic of the Congo (DRC). During 1994 and 1995, an outbreak of HF occurred in north-
During the same year, EBO virus was isolated from patients eastern Gabon. It was first considered to be caused only by
during an HF epidemic in Sudan [2]. The viruses, which were yellow fever (YF) virus on the basis of the clinical symptom-
closely related to Marburg virus (all members of the Filoviri- atology, routine biochemical tests, and specific laboratory re-
dae), had an 88% and a 53% case fatality rate in DRC [3] and sults provided by the Centre National de Référence des Fièvres
Sudan [2], respectively. A third outbreak, with a case fatality Hemorragiques Virales (Institut Pasteur, Paris) [8, 9]. However,
of 60%, occurred in Sudan in 1979 [4]. In addition, a death retrospective serologic tests detected concomitant EBO virus
was registered in Tandala, DRC, in 1979 [5]. In 1994, a new antibodies among some of the patients and the general popula-
strain of EBO virus was isolated from a Swiss researcher with tion [10, 11]. Later efforts to isolate the EBO virus from some
a dengue-like syndrome, who had likely been infected during of the specimens from the first epidemic (1994) were success-
the necropsy of a chimpanzee (see Formenty et al., this supple- ful. One year later, in February and in July 1996, two more
ment). The animal had been found dead in the TaıF National HF outbreaks occurred in northeastern Gabon [10 – 13].
Forest (Côte d’Ivoire) during a 2-year epidemic that killed half Herein, we report on three EBO epidemics that occurred
of the population of chimpanzees [6]. A third serious human between late 1994 and early 1997 in northeastern Gabon [10].
epidemic of EBO occurred in 1995 in Kikwit, DRC; it was
The Epidemics
Informed consent was obtained from the patients or their parents or guard-
It is important to note that during this investigation, we
ians. continually faced many difficulties (e.g., logistics problems and
Financial support: CIRMF is supported by the Republic of Gabon, the French cultural and political constraints) in the collection of data and
Ministry of Foreign Affairs (Coopération et Action Culturelle), and ELF GA-
BON Co. Ltd. (Libreville).
management of our research on this disease. Despite our efforts,
Reprints or correspondence (current affiliation): Dr. Alain-Jean Georges, the difficulties sometimes led to the loss of important informa-
Chefferie, Hopital d’Instruction des Armées Desgenettes, 108 Bd Pinel, 69 tion, and at times, forced us to report the scientific data in a
275 Lyon, Cedex 03, France (ajgeorges@wanadoo.fr).
* Current affiliations: CHA, Lamalou les Bains, France (J.P.M.L.); IMTSSA,
rather unorthodox manner.
Le Pharo, Marseille Armées, France (E.J.B.); Ministère Affaires Etrangères, First epidemic (fall 1994). The first epidemic in Gabon
Service de l’Action Humanitaire, Paris (J.P.A.); and CBMS, Institut Pasteur, had two waves of patients, with the first beginning in early
Paris (M-C.G.C.).
December 1994 and the second beginning at the end of January
The Journal of Infectious Diseases 1999;179(Suppl 1):S65–75
q 1999 by the Infectious Diseases Society of America. All rights reserved.
to February 1995. All patients in the first wave came from 3
0022–1899/99/79S1–0013$02.00 gold-panning encampments (Mékouka, Andock, and Minkébé)
/ 9d49$$se13 01-12-99 11:06:39 jinfa UC: J Infect
S66 Georges et al. JID 1999;179 (Suppl 1)
situated in small clearings of 2000 – 3000 m2 at the edge of the the physicians in charge of the Makokou hospital (a very poorly
rain forest. Figure 1 and table 1 show the geographic location equipped facility), was rather broad, and at least 4 of the 49
of these and other villages with case-patients. Table 1 also patients appeared unlikely to have HF. On 18 December 1994,
shows the chronology of illness for the cases. Three hundred during the middle of the first wave, the Gabonese health author-
fifty people, mainly of the Bakota ethnic group but also some ities requested that we examine 9 patients in Makokou General
Bakwélé, inhabit this area (30 in Mékouka, 20 in Andock, and Hospital. Biologic samples from those patients led to the identi-
300 in Minkébé). fication of the etiologic agents.
A total of 32 sick persons from the three forest encampments Between December 1994 and March 1995, CIRMF collected
(23 from Mékouka, 4 from Andock, and 5 from Minkébé) 22 samples in Mayela from contacts (all §15 years old) of
traveled 100 km south by river to the nearest hospital at Mako- sick persons and 88 samples from the local population of
kou, the main town of the region, for treatment. In addition to Ogooué-Ivindo Province, Gabon, where the epidemic occurred.
the primary cases in Andock, we were also informed that deaths At that time, many people had fled the area in terror; therefore,
had occurred in the local population of great apes (chimpan- it was difficult to conduct an investigation. A year later (January
zees, Pan p. troglodytes, and gorillas, Gorilla g. gorilla). How- 1996), we sampled 236 people from the three initially infected
ever, despite intensive searches of the forest by teams from villages and from villages in the Makokou area in order to
Centre International de Recherches Médicales de Franceville further assess exposure to EBO virus in the local population.
(CIRMF), no cadavers or skeletons were ever found, even when Second epidemic (spring 1996). A second epidemic began
a patient told us that he had killed a chimpanzee with abnormal during early February 1996 in the village of Mayibout 2, Ga-
behavior inside his encampment. This report could be anec- bon, which is located on the Ivindo River. Mayibout 2 is 40
dotal, but it cannot be totally ignored. km south (6 h by boat) of Mékouka and Andock, where the
The second wave of patients did not originate from the en- first epidemic broke out, and north of Makokou (7 h by boat).
campments: They were what we should have called (in a survey Eighteen people who had skinned and chopped a chimpanzee
Downloaded from jid.oxfordjournals.org by guest on May 8, 2011
following accepted procedures) secondary (or tertiary ?) cases. cadaver that they found became ill (fever, headache, bloody
Unfortunately, the information that was available from the au- diarrhea). They were evacuated from Mayibout 2 to Makokou
thorities regarding these patients did not provide a precise gene- on the decision of the village chief, despite governmental in-
alogy of all cases. The first patient in the second wave was structions to the contrary. All patients were admitted to Mako-
from Mayela, a small village close to Makokou, far from the kou Général Hospital, where 4 moribund patients died within
forest encampments. This person, who was probably the first 48 h.
secondary or tertiary case, lived near a traditional healer (a The bodies of the 4 patients were returned by river to Mayi-
‘‘nganga’’) and was probably infected as a result of contact bout 2; a fifth patient, who was moribund when he escaped
with a hospitalized patient who, against medical advice, left from the hospital, died after returning to Mayibout 2. Tradi-
the hospital to seek care from the nganga. Sixteen more cases tional burial ceremonies were performed without any special
(table 1) occurred in mid January: 1 case at Makokou Général precautions to avoid disease transmission. Two other ‘‘primary
Hospital, 12 cases from Mayela, and 3 cases from two villages cases’’ occurred, which appeared not to be connected to the
(Ekataniabé, 1 patient; Ekobakoba, 2 patients) on the road chimpanzee episode; 1 died. Fifteen serum samples from these
running south toward Franceville. None of these patients had initial 18 primary cases and 6 from secondary and tertiary cases
been in the area affected by the first wave of the epidemic were obtained. An additional 205 serum samples were obtained
during the previous 3 months; however, all had been either in from the population of Mayibout 2 and neighboring villages
direct contact with sick relatives (people hospitalized at Mako- (Mayibout 1 and Mvadi, which are 2 km south and 20 km
kou Général Hospital or sleeping in the nganga traditional heal- north, respectively, of Mayibout 2).
er’s home) or with people caring for patients. Third epidemic (fall 1996). On 5 October 1996, we in-
The last reported case (infected while caring for a relative formed the Gabonese health authorities (who 1 week earlier
at Makokou’s hospital) occurred at Ekobakoba on 9 February had requested our assistance in the investigation) that we had
1995, and the epidemic was declared over by Gabonese health isolated EBO viruses from 2 of 6 samples from patients hospi-
authorities on 17 February 1995. talized at Booué. Personnel from CIRMF carried out a retro-
Overall, 49 persons were admitted to Makokou’s hospital spective investigation of this third epidemic, which probably
with suspected HF. Patients were suspected of having HF if started as early as 13 July with the death (undeclared) of a 39-
they had a well-identified contact with an ill person or at least year-old hunter in a logging camp near Booué (0706* S, 11757*
two of the following clinical signs: fever, diarrhea, vomiting, E) between Ovan and Koumameyong, 200 km from Mékouka
melena, conjunctivitis, arthralgia or myalgia, diarrhea, or vom- and 120 km from Makokou to the southwest (figure 1). The
iting. Of the first 9 patients, 2 who we examined during the symptoms of this first case were suggestive of viral HF (VHF;
first wave also had jaundice, which has never been described fever, bleeding, vomiting, diarrhea, and headache). At the be-
as a symptom of EBO infection but is consistent with YF ginning of August 1996, information was obtained that several
infection. This case definition of HF, which was proposed by chimpanzees may have died in the same area, and a field collab-
/ 9d49$$se13 01-12-99 11:06:39 jinfa UC: J Infect
Downloaded from jid.oxfordjournals.org by guest on May 8, 2011
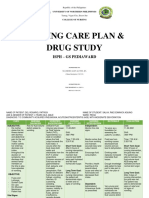
Figure 1. Geographic location of sites of primary and secondary cases of hemorrhagic fever. A, Gabon, B, Africa, C, sites.
/ 9d49$$se13 01-12-99 11:06:39 jinfa UC: J Infect
S68 Georges et al. JID 1999;179 (Suppl 1)
Table 1. Geographic location (in order of occurrence of illness) of sites of primary and secondary
human Ebola infections during the fall 1994 outbreak in Gabon.
Samples from Samples from Samples from
sick patients patients’ contacts general population
Village Geographic location (first epidemic) (first epidemic) (1996)
Mékouka 1724* N 12759* E 23 — 12
Andock 1729* N 12755* E 4 — 8
Minkébé 1744* N 12749* E 5 — 86
Mayela (December 1994) 0738* N 12756* E — 22 12
Makokou 0733* N 12750* E 1 28 72
Mayela (February 1995) 0738* N 12756* E 13 32 24
Etakaniabé 0732* N 12757* E 1 12 12
Ekobakoba 0736* N 13705* E 2 1 10
Mayibout 2 1707* N 13706* E — — 175
Mayibout 1 1707* N 13706* E — — 10
Mvadi 1746* N 13709* E — — 20
orator was able to obtain skin samples from 1 cadaver for The epidemic was declared over in March 1997 (last offi-
pathologic examination at the Centers for Disease Control and cially declared patient: 18 January), with a total of 60 cases
Prevention (CDC, Atlanta), with which CIRMF was in contact. and 45 deaths. Unfortunately, the information made available
Six weeks later, at the end of August, a second hunter (35 to us from the local authorities did not allow for a very precise
Downloaded from jid.oxfordjournals.org by guest on May 8, 2011
years old) died in the same Gabonese logging camp, but his genealogy of all cases; however, we did obtain accurate data
death, which was also suggestive of VHF, was not linked to on 47 of the 60 cases (Milleliri JM, unpublished data).
that of the first hunter. A third hunter (26 years old) became
ill 12 days later and was hospitalized at Booué. He subsequently
Materials and Methods
evaded the medical authorities at Booué and died in the village
of Balimba, where he was being treated by a nganga. Shortly Routine Clinical Chemistry Tests
after the hunter’s death, both the nganga and his nephew fell
ill in mid-September and were admitted first to Booué Hospital Routine clinical chemistry tests were done on sera from some
hospitalized cases in each epidemic.
and then transferred to Makokou General Hospital, where they
died. Three other cases, including another nganga, occurred
among people living in the same area. Serologic Assays
After we confirmed that the patients had EBO HF (EHF),
the authorities decided to apply the same clinical and epidemio- IFAs. IFAs were used to detect viruses causing HF (including
logic definitions that were used during the outbreaks in Yam- Crimean-Congo HF fever virus, Rift Valley fever virus, subtype
Zaire of EBO virus [EBO-Z; Mayinga and Boniface strains], Lassa
buku, DRC, in 1976 and in Kikwit to diagnose EHF patients
fever virus, and Marburg virus) in sera from some patients in each
[1, 7]. The disease spread around Booué; 24 cases, including
epidemic. The IFAs were done using CRELM (initials of each
17 deaths, were officially declared by 13 November 1996. A virus) microscope slides [14] provided by the CDC and US Army
Gabonese doctor, who had performed an endoscopy in a private Medical Research Institute of Infectious Diseases (Fort Detrick,
hospital in Libreville on an EBO-infected patient from Booué, Frederick, MD).
developed signs and symptoms of EHF. On 27 October, without IgM anti-EBO EIA. ELISAs were also used to detect EBO
first requesting a serologic diagnosis of VHF and without con- virus infection [15]. For IgM detection, an immunocapture test
sidering the possible etiology of such a diagnosis, he went to was used. Polyvinyl chloride 96-well microtiter plates (no. 1000-3,
Johannesburg for treatment. A South African nurse who cared Bioblok; Dynatech, Strasbourg, France) were adsorbed overnight
for the doctor became ill on 2 November and died on 24 at 47C, using goat anti-human m-chain (Tago, Burlingame, CA)
November (Swanepoel R, personal communication). diluted 1:500 in 0.01 M PBS (pH 7.4). All steps of the assay were
done using volumes of 100 mL/well. Sera from persons who were
At the end of November 1996, a second wave of this third
infected or were suspected of being infected and sera from their
epidemic appeared in three locations around Booué: Lolo (3
contacts were added to the wells at a 1:100 dilution in serdil (5%
deaths, 6 cases), SHM, a timber company (4 deaths, 5 cases), skim milk [Bacto milk], PBS, 0.1% Tween 20). After the plates
and the logging camp of Balimba (1 death, 1 case). A confirmed were washed with PBS with 0.1% Tween 20 (Bio-Rad, Richmond,
case spread to Lastourville (130 km southeast of Booué) from CA), sera were added (first at a 1:100 dilution and then at 4- to
Balimba, and again to Libreville, with subsequent transmission 800-fold dilutions), and the plates were incubated for 60 min at
of the disease to the capital (11 deaths, 15 cases). 377C in a humid chamber. For each serum and each dilution, in
/ 9d49$$se13 01-12-99 11:06:39 jinfa UC: J Infect
JID 1999;179 (Suppl 1) Ebola Outbreaks in Gabon, 1994–1997 S69
one well, we used as antigen a cell slurry made in EBO-infected known from previous experience to identify EBO antigen for dif-
Vero E6 cells diluted 1:1000 in PBS; in another well, we used a ferent strains of virus in tissues. Molecular identification of the
slurry of uninfected Vero E6 cells. Anti-EBO (subtypes Z, Sudan EBO virus strains following extraction of RNA from whole blood
[S], and Reston [R]) hyperimmune rabbit serum was diluted 1:2000 clots or from the peripheral blood mononuclear cells separated on
in serdil. Plates were incubated for 1 h with anti-rabbit IgG (no. ficoll have been described elsewhere [16].
074-1506; Kirkegaard & Perry, Gaithersburg, MD) diluted At Institut Pasteur, attempts to isolate YF virus by inoculation
1:10,000 in serdil (as conjugate) and then incubated for 30 min of suckling mice, mosquitoes, and mosquito cell cultures (AP 61,
using an H2O20 ABTS substrate (Kirkegaard & Perry). C6–36) failed to give positive results. Therefore, RNA was ex-
In the first assays we used 2 standard serum samples as positive tracted according to the method of Chomczynski and Sacchi [18],
controls. As soon as we had confirmed the EBO cases, we added and the presence of the YF viral genomic RNA was revealed by
our own 2 positive controls, which were run in standard dilution reverse transcriptase–polymerase chain reaction (RT-PCR) ampli-
series for providing standard curves, which allowed the determina- fication [19] using consensus primers for flaviviruses. The ampli-
tion of the limits of detection of the assay. A panel of 4 negative fied DNA fragment was then transferred onto a nitrocellulose
sera (from healthy persons) were run in all tests to determine the membrane and hybridized with a YF virus–specific probe.
background of the assay (the limit at which the positive controls
are positive) and to provide the mean and standard deviation (SD)
of that background. A sample was considered to be positive if its Antigenemia
optical density exceeded the mean / 3 SD of the controls. Plates
were read spectrophotometrically at an optical density of 410 nm The sera of sick people, their contacts, and people suspected of
on a microcomputer (LP 200; Sanofi Diagnostics Pasteur, Marnes- having EHF were tested by EIA for the presence of EBO antigen,
la-Coquette, France). as were the supernatants of Vero E6 cells seeded with sera from
IgG anti-EBO EIA. For IgG detection, half of a 96-well mi- these persons. Half of a 96-well microtitration plate was coated
crotitration plate was coated with a lysate of EBO-Z–, EBO-S–, (overnight at 47C) with a mouse monoclonal antibody recognizing
and EBO-R–infected Vero E6 cells, and the other half was coated EBO virus epitopes; the other half was coated with normal my-
eloma ascites diluted 1:1000 in PBS. Biologic samples to be
Downloaded from jid.oxfordjournals.org by guest on May 8, 2011
with a lysate of uninfected Vero E6 cells to determine the specific
binding of antibody to virus antigens (the background); both ly- checked for the presence of EBO antigen were then added (first
sates were diluted 1:1000 in PBS. Plates were incubated overnight at a dilution of 1:4 and then 4- to 64-fold). After a 1-h incubation
at 47C. The plates were washed three times with PBS plus 0.1% at 377C in a humid chamber, the plates were washed 3 times, and
(vol/vol) Tween 20, and then sera were added at a 1:100 and 4- rabbit anti-EBO (subtypes Z, S, and R) diluted 1:2000 in serdil
to 800-fold dilutions in serdil and allowed to react with the antigen- was added and incubated for 1 h at 377C in a humid chamber.
coated wells for 60 min at 377C in a humid chamber. Bound IgG Plates were incubated for 1 h with anti-rabbit IgG conjugate (no.
was detected with mouse anti-human IgG conjugated to horserad- 074-1506; Kirkegaard & Perry) diluted 1:10,000 in serdil and then
ish peroxidase. Further identification was done as in the IgM EIA incubated for 30 min using an H2O20 ABTS substrate (Kirke-
assay. A panel of specific IgG-positive controls and specific IgG- gaard & Perry), and bound rabbit IgG was detected.
negative sera (from healthy persons) was run in all tests in order
to determine the cutoff value. For each assay, the mean and SD
Results
of the adjusted optical density were accumulated and used to calcu-
late a value equal to the mean / 3 SD, which represented the Serologic surveys. The occurrence of HF cases in the fall
cutoff value. Plates were read as above. of 1994 initially led us to suspect an outbreak of sylvatic YF
Anti-YF IgM EIA. At the beginning of the first VHF epidemic, infection. However, we were aware that another HF agent (in
YF virus was strongly thought to be the probable cause of illness,
particular EBO virus) could be circulating, given the possible
on the basis of the clinical and epidemiologic results of the 9
fatalities observed in nonhuman primates (apes replicate YF
patients examined. Therefore, we tested for YF virus infection,
using IgM capture techniques [17]. virus, but they usually do not die from it; Monath TP, personal
communication).
In the first instance, we screened 9 patients (all from Mako-
Virus Isolation Attempts kou General Hospital) for HF virus. EBO IFA on CRELM
slides was negative for all 9 serum samples, whereas 6 of 9
Vero E6 cell 6-well plates were inoculated with sera from pa- patients showed evidence of recent YF virus infection (IgM
tients suspected of harboring a VHF virus. During the first epi- capture). Of the 49 sick patients, another 14 cases who had
demic, the biosafety level 4 facilities of the Institut Pasteur were never been vaccinated against YF were also screened. Of the
used for all virologic manipulations of patient-derived material;
14 cases, 8 had evidence of recent YF infection as determined
further work on the two last epidemics was carried out at CIRMF’s
by IgM capture or Southern blot, but none had evidence of
site or at CDC’s Special Pathogens laboratories or at both sites
for part of the molecular biology testing of EBO virus strains [16]. antibodies to the main African viral HFs as determined by use
To identify the EBO virus, EBO reference antisera were tested of IFA on CRELM slides. However, the antigen used in our
against the virus isolates cultured on Vero E6 cells. Tests were IFA test was several years old, so in June and July 1995 we
done using polyclonal antibodies raised in mice (IFA test) and a used ELISAs and fresh antigens to retrospectively test these
pool of monoclonal antibodies (antigen-capture test) that were same 23 samples (ELISA is generally more sensitive than IFA).
/ 9d49$$se13 01-12-99 11:06:39 jinfa UC: J Infect
S70 Georges et al. JID 1999;179 (Suppl 1)
Nineteen patients had signs of a recent infection with EBO as For the spring 1996 epidemic, the case fatality rate was
determined on the basis of at least one of the following: positive 67.7% (21 of 31 cases died) as determined using the accepted
for EBO IgM, positive for antigenemia, positive for virus iso- (Yambuku and Kikwit) case definition. There were 17 male
lated from cultured Vero E6 cells. and 14 female patients (sex ratio, 1.2) with a mean age of 27.6
We also used ELISA to test the 88 serum samples obtained years.
in January 1995 (before YF vaccination) from the population In the fall 1996 epidemic, there were 60 cases and 45 deaths
living around the three encampments (Andock, Minkébé, and (case fatality rate, 75%). The sex ratio was 2.4. We were unable
Mékouka) where the first epidemic broke out and the 22 serum to conduct adequate surveys during the epidemic, so complete
samples obtained from contacts in Mayela. Two of these sera age-range data are unavailable.
(1.8%) were positive for anti-EBO IgG but not EBO IgM, The development (geographically and chronologically) of the
while 9 YF-unvaccinated people (8.1%) were positive by YF first two epidemics is shown in table 1 and figures 2 and 3,
IgM capture, indicating a recent YF virus circulation. respectively. When tracing the computerized (MS Access software;
One year later, we obtained samples from 236 persons from Microsoft, Redmond, WA) polynomial regression curves obtained
the same area (table 1). For various reasons, only 56 of the from histograms, the first epidemic shows two waves of morbidity,
original 110 people were part of this second cohort (e.g., use whereas in the second outbreak, there is only one peak of morbid-
of given name in the place of family name in original survey, ity. These observations are related to the notably different types
fear of being identified and accused of causing the original of spread in the two epidemics. Persons in several villages were
epidemic, and migrations of populations). Of 236 subjects, 24 infected during the first epidemic, which lasted longer than the
(9.7%) had anti-EBO IgG by ELISA without any anti-EBO second, in which only persons in a confined area were affected.
IgM (1 of these IgG-positive cases was the first case of the The exact origin(s) of the virus in the first epidemic is uncertain,
first wave in the 1994 epidemic and had survived a typical and despite reports of the death of great apes, we were unable to
EBO-type illness). confirm these reports.
Downloaded from jid.oxfordjournals.org by guest on May 8, 2011
During the second epidemic, 205 samples were collected Exploitation of the area by gold miners has caused substan-
from people living in 3 villages (Mayibout 1 and 2, where tial disturbance to the forest canopy. This disturbance may
EBO was known to have occurred, and Mvadi, where 1 uncon- have caused contact between other species and humans that
firmed death of a hunter was said to have occurred). High otherwise would not have occurred. None of the specimens
frequencies of anti-EBO IgG (14.9% – 30%) and IgM (5.7% – (small mammals and insects) collected in the field so far have
10.0%) by ELISA in all three villages (table 2) may suggest yielded any sign of harboring the virus; however, these studies
the presence of an asymptomatic or mild form of the disease are ongoing.
concomitant with the classical severe form of EBO, or they In the second outbreak, there is no doubt that the virus came
may demonstrate the limits, in terms of specificity, of the EBO from one source, a chimpanzee infected by EBO (for which
IgG and IgM ELISAs that we used. the chain of infection is unknown). The chimpanzee seems to
During the initial phases of the third epidemic, we were have been the index case for infecting 18 primary human cases.
unable to carry out serologic surveys due to local reasons that There were 2 other primary cases, for whom we have no infor-
were out of our control. mation on the source of infection (the role of a nganga was
Fatality and descriptive epidemiology. We reviewed files suspected), making a total of 20 primary cases for this epi-
at Makokou General Hospital for persons who were seen during demic. Only those people who had been in contact with the
the first epidemic in fall 1994; 49 patients were identified with dead chimpanzee before it was cooked for eating were affected;
at least two signs of VHF, 29 of whom died (case fatality rate, nobody was infected by eating the cooked meat. We identified
59%). There were 26 male and 23 female patients (sex ratio, 10 secondary cases involving close contacts of dead or dying
1.1) with a mean age of 37 years. people and 1 tertiary case. It is important to note that no cases
of infection occurred among the professional medical personnel
because of preventive measures that were set in place on the
Table 2. Anti-Ebola antibodies among the general population of second day of the epidemic. All equipment and material neces-
three villages in Ogooué-Ivindo Province, Gabon, during the second sary for barrier nursing and prevention of the spread of disease
epidemic (spring 1996), as determined by ELISA. were provided. One hundred ninety-one contacts were traced,
with no evidence of infection by EBO virus.
No. (%) of villages
Similar to the case in the first epidemic, the source(s) of the
positive for
Geographic No. of
virus in the third epidemic was not immediately obvious, nor
Village location samples IgG IgM could it be traced retrospectively. The lack of identification of
cases at the outset and the lack of adequate containment mea-
Mayibout 1 1707* N 13706* E 10 3 (30.0) 1 (10.0) sures once the diagnosis had been made meant that sick persons
Mayibout 2 1707* N 13706* E 175 26 (14.9) 10 (5.7)
could travel throughout and even outside Gabon. Some contact
Mvadi 1746* N 13709* E 20 5 (22.5) 2 (10.0)
cases could not be identified and isolated.
/ 9d49$$se13 01-12-99 11:06:39 jinfa UC: J Infect
JID 1999;179 (Suppl 1) Ebola Outbreaks in Gabon, 1994–1997 S71
Downloaded from jid.oxfordjournals.org by guest on May 8, 2011
Figure 2. Evolution of 1994 – 1995 Ebola virus epidemic in Gabon. A, Evolution by mortality rate. Curve shows biphasic evolution of
epidemic limited to large no. of secondary cases who have spread virus. B, Geographic evolution of epidemic. Hop Å hospital.
Immunostaining [15] done at the CDC on skin biopsies from tients in the cohort, 6 died. Data were obtained 4 – 7 days after
a chimpanzee found dead in the forest indicated the presence the onset of disease (16 days after the patients were infected
of EBO [16]; however, the ape is very unlikely to have had by a chimpanzee cadaver). The levels of direct and conjugated
any contact with humans. bilirubin were normal, but all patients had signs of liver
Biologic and clinical features. Clinical signs and symp- involvement (i.e., elevations in g-glutamyltransferase, amino-
toms observed in 15 serologically or virologically confirmed transferase, and alkaline phosphatase), and 23% had signs of
patients from the outbreak at Mayibout 2 (spring 1996) are slightly decreased renal dysfunction (elevated serum creatinine
presented in table 3. Fever was always present, while in Ç75% and urea).
of the cases, diarrhea (a dense suspension of black or brown- Most of the other blood parameters (e.g., total serum pro-
red uneven microaggregates õ5 mm in size in liquid or syrupy teins, albumin, uric acid, cholesterol, triglycerides, sodium, po-
stools) and vomiting were seen, and Ç50% had conjunctivitis tassium, and chloride) that we were able to test were normal.
or conjunctival bleeding. Taking only the second epidemic Characterization of virus strains. EBO viruses were iso-
into consideration, since it was the best-documented outbreak, lated from patients from each of the three epidemics. All the
clinical signs and symptoms were observed between days 6 Gabonese virus strains sequenced showed a high level of ho-
and 11 after handling the chimpanzee, and deaths occurred mology with the group of strains from DRC [16]. Viruses
between days 12 and 18 after the appearance of signs or symp- isolated from patients during the same outbreak had identical
toms. Despite a small number of observations, it seemed to us base-pair sequences, but base-pair sequences were slightly dif-
that those who died had a shorter incubation period than those ferent for isolates from the individual outbreaks. There was
who survived. only a four-nucleotide (nt) difference in the GP gene in each
Table 4 presents the biologic and biochemical data for 13 of the 3 Gabonese strains (i.e., the GP gene from the December
patients infected during the spring 1996 outbreak. Of 13 pa- 1994 strain differs from that of the February 1996 strain by
/ 9d49$$se13 01-12-99 11:06:39 jinfa UC: J Infect
S72 Georges et al. JID 1999;179 (Suppl 1)
Downloaded from jid.oxfordjournals.org by guest on May 8, 2011
Figure 3. Evolution of spring 1996 Ebola virus epidemic in Gabon. A, Evolution of epidemic by mortality rate. Curve shows monophasic
evolution of epidemic limited to small no. of secondary cases who spread virus. B, Geographic evolution of epidemic. Not included is case
who died on 19 February 1996 and who had different infection not related to Ebola virus since 20 January 1996. Hop Å hospital.
four nt, and the February strain differs from the October 1996 Discussion
strain by 4 nt).
A conserved region of the L gene was also amplified in virus An epidemic of HF among humans, some of whom had
strains from fall 1994 and fall 1996, using degenerate primers clinical and biologic symptoms suggestive of YF infection,
selected from sequences of EBO-S and Marburg virus strains; started in December 1994 in Ogooué-Ivindo Province. On the
PCR products were subsequently sequenced [13]. The 2 Gabo- basis of clinical, biologic, and serologic data, a diagnosis of
nese strains showed high homology in the first 156-bp se- YF infection was suspected in 6 hospitalized cases, and a diag-
quence, with only a single base change (position 110; A to G) nosis of YF infection was confirmed for 3 other cases on the
separating the 2 strains. As stated, during the first epidemic, 6 basis of molecular biology data, although the complete virus
of 9 patients had anti-YF IgM. At the Institut Pasteur, using could not be isolated, which is not unusual for YF virus. (YF
PCR and specific hybridization techniques, YF sequences were virus is known to be impossible or difficult to isolate from
identified in sera from 2 of the 6 patients who were anti-YF clinical material if samples are taken several days after evolu-
IgM positive and in 1 of the 3 patients who had no anti- tion of the clinical disease; for example, during the 1970 epi-
YF IgM. Those 3 patients, who were negative for all EBO demic in Okwooga and the 1986 epidemic in Oju region, Nige-
investigations, had clinical signs compatible with YF (e.g., ria, it was impossible and difficult, respectively, to isolate YF
severe low back pain, fever, jaundice [2/3 patients], melena, virus [Monath TP, personal communication]). At the time, no
and melanemesis), and biochemical results showed signs of etiologic diagnosis was scientifically established for the 6 pa-
liver and renal failure and slightly raised bilirubin levels. tients who were not confirmed to have YF virus infection;
/ 9d49$$se13 01-12-99 11:06:39 jinfa UC: J Infect
JID 1999;179 (Suppl 1) Ebola Outbreaks in Gabon, 1994–1997 S73
Table 3. Clinical manifestations observed in 15 confirmed cases of of infected case-patients, with barrier nursing, disinfection,
Ebola hemorrhagic fever during the spring 1996 outbreak in Mayibout and insect eradication programs and (2) active reintroduction
1 and Mayibout 2, Gabon.
of a vaccination program against YF virus, which had lapsed
Clinical symptoms % of patients with symptom ú10 years earlier. The fact that the entire YF virus was not
isolated is not a conclusive argument against the fact that YF
Fever 100 occurred during the first VHF epidemic, since samples may
Diarrhea 87 have been collected at a late stage of the disease when the
Vomiting 73
virus is difficult to isolate. However, in fall 1994, there was a
Conjunctivitis 53
Gingival bleeding 40 high prevalence of anti-YF IgM in YF-unvaccinated subjects,
Arthralgia, myalgia 33 which was strongly suggestive of a recent YF outbreak. It is
Cephalgia 27 known that sylvatic YF infection can exist in a mild or symp-
Asthenia 27 tom-free form [17].
Cephalgia 27
A final argument for the presence of YF virus during the
Melena 27
Hiccups 27 first epidemic (fall 1994) comes from Pisano et al. [20], who
Obnubilation 27 identified YF infection in a cohort of 5 patients (different from
Sore throat 20 ours) from the same area by sequencing a cDNA fragment
Cough 20 obtained by RT-PCR and showing 94.4% homology with the
Melanemesis 13
Asibi strain of YF virus [21].
Epistaxis 13
Abdominal pain 7
During the first epidemic, EBO and YF viruses were obvi-
ously coexisting: 9 patients had EBO alone, 11 had EBO and
YF, and 3 had YF alone. Due to the small size of each group,
it is impossible to speculate on the relative lethality of each
Downloaded from jid.oxfordjournals.org by guest on May 8, 2011
nevertheless, we felt, from a public health point of view, that virus alone or in combination, but a nosocomial amplification
there was a risk for reemergence of YF (the last epidemic in of EBO appears to have occurred inside Makokou Général
Gabon was in 1949 [8]) among the unvaccinated population, Hospital. Such an association of YF and EBO viruses during
as confirmed later by the epidemiologic investigations of a the same epidemic has been suspected in the past: In Ethiopia,
World Health Organization expert [9]. where a VHF outbreak occurred in 1961 – 1962, a later sero-
Without waiting for a definitive diagnosis, for which inves- logic retrospective study showed that both EBO and YF viruses
tigations were in progress at the hemorrhagic fever unit at may have been present [22].
the Institut Pasteur, and despite the fact that another etiologic Earlier IFA-based studies looking for the presence of EBO
agent could be involved, CIRMF suggested to the Gabonese virus in other provinces of Gabon were done by Ivanoff et al.
health authorities that they rapidly instigate measures to limit [23] in 1982 and Meunier et al. in 1986 [24]. Data obtained
the spread of YF infection. We suggested (1) passive isolation by use of the same technique showed that EBO is widespread
Table 4. Biochemical results for 13 patients with Ebola hemorrhagic fever during the spring 1996 outbreak in Gabon.
Conjugated Aspartate Alanine Alkaline
Patient No. of days Total bilirubin bilirubin g-glutyltransferase aminotransferase aminotransferase phosphatase Urea
no. after onset Outcome (õ20 mmol/L) (õ10 mmol/L) (õ45 U/L) (õ45 U/L) (õ45 U/L) (õ125 U/L) (2.5 – 7 mmol)
1 7 R 52.0 35.0 246.0 230.0 666.0 419.0 11.0
2 4 D 42.0 30.0 212.0 220.0 512.0 410.0 10.9
3 4 R 17.0 4.7 16.0 155.0 60.0 126.0 3.1
4 4 D 25.0 6.7 52.0 160.0 75.0 166.0 3.1
5 6 D 16.5 4.4 64.0 314.0 109.0 150.0 3.2
6 4 R 18.0 7.2 38.0 226.0 98.0 72.0 6.7
7 4 D 21.0 6.7 21.0 165.0 70.0 136.0 3.2
8 4 R 31.7 19.8 193.0 185.0 1499.0 637.0 17.9
9 5 R 17.9 7.0 30.0 219.0 88.0 69.0 6.5
10 4 D 14.8 3.5 21.0 135.0 74.0 59.0 2.7
11 4 R 15.0 3.7 26.0 140.0 76.0 72.0 5.2
12 4 R 14.2 9.9 15.0 266.0 50.0 82.0 1.3
13 4 D 19.8 9.0 23.0 56.0 22.0 66.0 3.1
Mean 23.5 11.4 73.6 190.1 261.5 189.5 6.0
SD 11.7 10.3 83.7 65.9 420.5 181.8 4.7
NOTE. Data in parentheses are normal values. R Å recovered, D Å died.
/ 9d49$$se13 01-12-99 11:06:39 jinfa UC: J Infect
S74 Georges et al. JID 1999;179 (Suppl 1)
throughout equatorial Africa [25 – 27]. However, these results to limit the spread of this disease. Nosocomial spread of infection
must be examined carefully since others have suggested that due to the lack of recognition of the disease and the dearth of
IFA is likely to give false-positive results [28]. In addition, in training and material available to establish simple barrier nursing
our hands, this test was insensitive for EBO virus, specifically remains the root cause of most of the disease observed to date.
during the fall 1994 epidemic, in which all sera collected during From the public health point of view, this remains a basic goal for
the acute phase of the disease tested negative by IFA, while the prevention of EHF epidemics. Preventing primary infection
some were positive by EIA. Even though ELISA techniques certainly requires the identification of risk factors and the reser-
appear to be very sensitive for assessing EBO infection, we voir, something that continues to elude us all.
must be cautious about their specificity.
No serologic data were available from persons in Ogooué-
Ivindo Province before the first epidemic. However, we had Acknowledgments
kept 58 untested frozen serum samples from the epidemic pe- We thank B. Le Guenno (Institut Pasteur, Paris) for his invalu-
riod. The samples were from asymptomatic adults who were able scientific assistance in affirming the yellow fever diagnosis
not associated with gold-panning; 2 of them had ELISA EBO in January 1995 and for initiating new retrospective serologic stud-
IgM, suggesting recent EBO infection, and the remaining 56 ies on Ebola virus in June 1995 and new attempts at virus isolation
samples were negative for anti-EBO IgG and IgM. This low in samples from the fall 1994 epidemic, which led to the isolation
percentage of seropositivity suggests that the circulation of of the first Ebola isolate from Gabon; P. Tshipamba (CIRMF) for
EBO is a new phenomenon in the area, affecting mainly people providing excellent technical assistance; J. B. McCormick (Institut
living deep in the forest in temporary encampments. Pasteur), S. Fisher-Hoch–McCormick (Fondation Mérieux, Lyon,
There are interesting demographic and ecologic differences France), and P. Rollin (CDC, Atlanta) for valuable and pertinent
suggestions regarding the manuscript; and members of the Special
between the sites of the first two epidemics. The gold panners
Pathogens Branch of the CDC as well as members of Walter Reid
in the fall 1994 outbreak were a transient population and caused Army Institute of Research, US Army Medical Research Institute
Downloaded from jid.oxfordjournals.org by guest on May 8, 2011
considerable damage to the local forest in which they were of Infectious Diseases (Fort Detrick, Frederick, MD), who have
working. Most of those who survived left the area after the generously provided reagents to CIRMF since 1982.
epidemic; a very small population remains. Mayibout 2, a per-
manent, relatively dense settlement whose inhabitants practice
slash-and-burn cultivation, is situated on the river Ivindo and References
is surrounded by forest. The disturbance of the forest integrity 1. Johnson K, Webb P, Lange J, Murphy F. Isolation and partial characterisa-
is one common feature between the two sites, but the one tion of a new virus causing acute haemorrhagic fever in Zaire. Lancet
important difference is the permanence and the size of the 1977; 1:569 – 71.
2. WHO/International Study Team. Ebola hemorrhagic fever in Sudan, 1976.
population around Mayibout 2, which might permit the virus,
Bull World Health Organ 1978; 56:271 – 93.
once present in the area, to circulate within the human popula- 3. WHO/International Study Team. Ebola hemorrhagic fever in Zaire, 1976.
tion. Both the reservoir and the vector for the EBO virus are Bull World Health Organ 1978; 56:247 – 70.
still unknown; however, it is apparent that the great apes, or 4. Baron RC, McCormick JB, Zubeir OA. Ebola virus disease in southern
at least chimpanzees, are not involved because they are as Sudan: hospital dissemination in intrafamilial spread. Bull World Health
Organ 1983; 61:997 – 1003.
susceptible as humans to the disease.
5. Heymann D, Weisfeld, Webb P, Johnson K, Cairns T, Berquist H. Ebola
On the basis of a sizeable but incomplete genetic compari- hemorrhagic fever: Tandala, Zaire, 1977 – 1978. J Infect Dis 1980; 142:
son, the viruses from our three outbreaks are essentially indis- 372 – 6.
tinguishable from the viruses isolated in DRC in 1976 and 6. Le Guenno B, Formenty P, Wyers M, Gounon P, Walker F, Boesch C.
1995; however, the viruses isolated in 1976 from Sudan and Isolation and partial characterisation of a new strain of Ebola virus.
Lancet 1995; 345:1271 – 4.
DRC were clearly biologically distinct from one another [29].
7. WHO/International Study Team. Ebola hemorrhagic fever in Zaire (Kik-
We cannot rule out the possibility that varied strains of EBO wit). Bull World Health Organ 1995; 19:13.
virus or even different members of the Filoviridae are circulat- 8. World Health Organization. Yellow fever in Gabon. Bull World Health
ing in these areas, with some being more virulent than others Organ 1995:64.
yet cross-reacting and, therefore, appearing as asymptomatic 9. Cordelier R. Fièvre jaune au Gabon: enquête sur un épisode amaril dans
la Province d’Ogooué-Ivondo (2 au 23 mars 1995). Rapport OMS.
infections in the population. The inability to isolate viruses
Brazzaville: OMS, Bureau Régional pour l’Afrique, 1995.
from the Gabonese environment and from anyone but ill pa- 10. Georges AJ, Le Guenno B, Renaut AA, et al. Recent Ebola virus outbreaks
tients has not allowed us to address this issue. The fact that in Gabon from 1994 to 1996: epidemiologic and control issues. Report
the ELISA test has not been evaluated for specificity against of International Colloquium on Ebola virus research (Antwerp, Bel-
known human infections also does not permit us to eliminate gium). Antwerp: Institute of Tropical Medecine, 1996:47.
11. Amblard J, Obiang P, Edzang S, Prehaud C, Bouloy M, Le Guenno B.
this as a possible explanation for the high level of antibody in
Identification of the Ebola virus in Gabon in 1994. Lancet 1997; 1:
the population of Mayibout 2. 181 – 2.
Finally, it is very clear that the use of simple barrier nursing 12. World Health Organization. Ebola hemorrhagic fever in Gabon. Bull
methods in even the most basic of hospital settings is sufficient World Health Organ, 1996; 9:71.
/ 9d49$$se13 01-12-99 11:06:39 jinfa UC: J Infect
JID 1999;179 (Suppl 1) Ebola Outbreaks in Gabon, 1994–1997 S75
13. Georges-Courbot MC, Lu CY, Lansoud-Soukate J, Leroy E, Baize S. 22. Tignor GH, Casals J, Shope RE. The yellow fever epidemic in Ethiopia,
Isolation and partial molecular characterisation of a strain of Ebola virus 1961 – 1962: retrospective serological evidence for concomitant
during a recent epidemic of viral haemorrhagic fever in Gabon [letter]. Ebola or Ebola-like virus infection. Trans R Soc Trop Med Hyg
Lancet 1997; 349:181. 1993; 87:162.
14. Wulf H, Lange JV. Indirect immunofluorescence for the diagnosis of Lassa 23. Ivanoff B, Duquesnoy P, Languillat G, et al. Hemorrhagic fever in Gabon.
fever infection. Bull World Health Organ 1975; 52:429 – 36. I. Incidence of Lassa, Ebola and Marburg viruses in Haut-Ogooué. Trans
15. Ksiazek T, Rollin P, Jarhling P, Johnson E, Dalgard D, Peters JC. Enzyme R Soc Trop Med Hyg 1982; 76:719 – 20.
immunosorbent assay for Ebola virus antigens in tissues of infected 24. Meunier DMY, Dupont A, Madelon MC, Gonzalez JP, Ivanoff P. Surveil-
primates. J Clin Microbiol 1992; 30:947 – 50. lance sérologique des fièvres hémorragiques virales dans le Haut-
16. Georges-Courbot MC, Sanchez A, Lu CY, et al. Isolation and partial Ogooué (Gabon). Ann Inst Pasteur/Virol, 1987; 138:229 – 35.
characterization of Ebola viruses causing different outbreaks in Gabon. 25. Josse R, Dupont A, Delaporte E, et al. Sero-épidemiologie des affections
Emerg Infect Dis 1997; 3:59 – 62.
virales à haut risque dans la ville de Port Gentil (Republique du Gabon).
17. Monath TP. Yellow fever. In: Monath JP, ed. The arboviruses: epidemiol-
Bull Liais document, OCEAC, 1987; 82:63 – 7.
ogy and ecology. Vol. V. Boca Raton, FL: CRC Press, 1989:139 – 231.
26. Johnson E, Gonzalez JP, Georges AJ. Filovirus activity among selected
18. Chomczynski P, Sacchi N. Single step method of RNA isolation by acid
ethnic groups inhabiting the tropical forest of equatorial Africa. Trans
guanidium thiocyanate – phenol-chloroform extraction. Anal Biochem
R Soc Trop Med Hyg 1993; 87:536 – 8.
1987; 162:156 – 9.
19. Pierre V, Drouet MT, Deubel V. Identification of mosquito-borne flavivirus 27. Gonzalez JP, Josse R, Johnson ED, et al. Antibody prevalence against
sequences using universal primers and reverse transcription/polymerase hemorrhagic fever viruses in randomized representative Central African
chain reaction. Res Virol 1994; 145:93 – 104. populations. Res Virol 1989; 140:319 – 31.
20. Pisano MR, Durand JP, Tolou H. Partial genomic sequence determination 28. Muhlberger E, Sanchez A, Randolf A, et al. The nucleotide sequence of
of yellow fever virus strain associated with recent epidemic in Gabon. the L gene of Marburg virus, a filovirus: homologies with paramyxovi-
Acta Virol 1996; 40:103 – 5. ruses and rhabdoviruses. Virology 1992; 187:534 – 47.
21. Hahn CS, Dalrymple JM, Strauss JH, Rice CM. Comparison of the virulent 29. McCormick J, Bauer S, Elliott L, Webb P, Johnson K. Biologic differences
Asibi strain of yellow fever virus with the 17D vaccine strain derived between strains of Ebola virus from Zaire and Sudan. J Infect Dis 1983;
from it. Proc Natl Acad Sci USA 1987; 84:2019 – 23. 147:264 – 7.
Downloaded from jid.oxfordjournals.org by guest on May 8, 2011
/ 9d49$$se13 01-12-99 11:06:39 jinfa UC: J Infect
S-ar putea să vă placă și
- Article Ebola HFDocument24 paginiArticle Ebola HFDavid Brayan Reyna GomezÎncă nu există evaluări
- Ebola Virus: The Role of Macrophages and Dendritic Cells in The Pathogenesis of Ebola Hemorrhagic FeverDocument5 paginiEbola Virus: The Role of Macrophages and Dendritic Cells in The Pathogenesis of Ebola Hemorrhagic FeverDavid Brayan Reyna GomezÎncă nu există evaluări
- ELISA Development GuideDocument17 paginiELISA Development GuideDavid Brayan Reyna Gomez100% (2)
- CDC and The Ebola's DeathsDocument2 paginiCDC and The Ebola's DeathsDavid Brayan Reyna GomezÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (72)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Advanced Live Blood Analysis for NutritionDocument7 paginiAdvanced Live Blood Analysis for NutritionPeter HendryÎncă nu există evaluări
- Antiepileptic Drugs 2019 Elearning PDFDocument39 paginiAntiepileptic Drugs 2019 Elearning PDFMalvika BabuÎncă nu există evaluări
- Exercise PrescriptionDocument87 paginiExercise PrescriptionDianne Faye ManabatÎncă nu există evaluări
- Clinical Manifestations and Diagnosis of Acute Colonic DiverticulitisDocument19 paginiClinical Manifestations and Diagnosis of Acute Colonic DiverticulitismohammedÎncă nu există evaluări
- Infectious Diseases and Nutrition: The Vicious CircleDocument2 paginiInfectious Diseases and Nutrition: The Vicious CircleWagdy AminÎncă nu există evaluări
- Escaran - Drug Study - Set ADocument4 paginiEscaran - Drug Study - Set AFrancis Alfred EscaranÎncă nu există evaluări
- - أسئلة التغذيةDocument52 pagini- أسئلة التغذيةMicheal Mikhail YoussefÎncă nu există evaluări
- 16 Feb Afternoon - MedicineDocument13 pagini16 Feb Afternoon - MedicineDrToby KhanÎncă nu există evaluări
- Health7 4TH Quarter ModuleDocument20 paginiHealth7 4TH Quarter Modulearmand bayoranÎncă nu există evaluări
- NLE Comprehensive Exam 3Document27 paginiNLE Comprehensive Exam 3Jofel Laygan Porras RN100% (1)
- This Study Resource Was: Case 1: Hay Fever & ColdsDocument4 paginiThis Study Resource Was: Case 1: Hay Fever & ColdsMary Jennel RosÎncă nu există evaluări
- Salva, R.D NCP & Drug Study (Isph - Gs Pediaward)Document7 paginiSalva, R.D NCP & Drug Study (Isph - Gs Pediaward)Rae Dominick Aquino SalvaÎncă nu există evaluări
- Drug Study ChloromazineDocument5 paginiDrug Study ChloromazineJuko FernandezÎncă nu există evaluări
- Tower of The AscendantsDocument35 paginiTower of The AscendantsMeatlepuppet100% (1)
- DAFTAR PUSTAKA Microbiology ReferencesDocument4 paginiDAFTAR PUSTAKA Microbiology ReferencesTogu NaiposposÎncă nu există evaluări
- Benefits of Everyday Drinking of CoffeeDocument5 paginiBenefits of Everyday Drinking of CoffeeCharmaine AlipayoÎncă nu există evaluări
- Plant Protection Cardamom: Presented byDocument26 paginiPlant Protection Cardamom: Presented byaditya rajÎncă nu există evaluări
- Drug Study GlyburideDocument5 paginiDrug Study GlyburideSchyna Marielle VitaleÎncă nu există evaluări
- G.R. No. 247409 - LEMONCITO V. BSM Crew Service Centre Philippines, IncDocument2 paginiG.R. No. 247409 - LEMONCITO V. BSM Crew Service Centre Philippines, IncJay jogs100% (1)
- Digestive System: Yousef Ali Sazan Falah Snor Dilan KawtharDocument21 paginiDigestive System: Yousef Ali Sazan Falah Snor Dilan Kawtharkauther hassanÎncă nu există evaluări
- Org - Telegram.messenger - Provider Media Telegram Telegram Documents 4 5985610863455765491 PDFDocument2 paginiOrg - Telegram.messenger - Provider Media Telegram Telegram Documents 4 5985610863455765491 PDFsameeÎncă nu există evaluări
- The Cognitive School of PsychologyDocument4 paginiThe Cognitive School of PsychologyJulieann Bagunas KimÎncă nu există evaluări
- 7 10 13 Case Report Allergic Rhinitis ARDocument2 pagini7 10 13 Case Report Allergic Rhinitis ARAlaireled CheIpoÎncă nu există evaluări
- PHD Public Health Doctoral Thesis UpdateDocument163 paginiPHD Public Health Doctoral Thesis UpdateLianne Grace De VeraÎncă nu există evaluări
- AB PSY PRE-BOARD 2 (June 17, 2023)Document8 paginiAB PSY PRE-BOARD 2 (June 17, 2023)sdfghÎncă nu există evaluări
- Necrotizing Pneumonia (Aetiology, Clinical Features and Management)Document8 paginiNecrotizing Pneumonia (Aetiology, Clinical Features and Management)pachomdÎncă nu există evaluări
- Psycho Physiological Disorders 1Document8 paginiPsycho Physiological Disorders 1Cedric Jay Villegas TasicoÎncă nu există evaluări
- The Hall of Fire 06Document27 paginiThe Hall of Fire 06maldreidorÎncă nu există evaluări
- TAMIFLUDocument21 paginiTAMIFLUjaphetnwapiÎncă nu există evaluări