Documente Academic
Documente Profesional
Documente Cultură
Comon Peroneal Nerve, Tibial Nerv-Suply
Încărcat de
Richa SoodDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Comon Peroneal Nerve, Tibial Nerv-Suply
Încărcat de
Richa SoodDrepturi de autor:
Formate disponibile
COMMON PERONEAL NERVE1 Anatomy
Formed by: Axons from L4, L5, S1 & S2 roots Course of axons o Through popliteal fossa: Separates from sciatic nerve in upper fossa o Behind head & along fibula: Covered only by skin & subcutaneous tissue o Behind peroneus longus muscle (fibular tunnel): In anterior compartment of leg o Emerge from fibular tunnel: Nerve divides into superficial & deep branches o Deep peroneal nerve passes through: Anterior tarsal tunnel Divides into lateral and medial terminal branches Lateral terminal branch: Supplies Extensor digitorum brevis & Extensor hallucis brevis Medial terminal branch o Supplies adjacent sides of great & 2nd toes (92%) o Absent in 8%: Muslces supplied by Superficial peroneal nerve Branches o Common peroneal in popliteal fossa: Sensory o Superficial peroneal Motor o Peroneus brevis o Peroneus longus o Accessory deep peroneal branch: Innervates Extensor digitorum brevis Cutaneous sensory o Lower leg: Anterolateral o Foot: Dorsum, except between 1st 2 toes o Medial & Intermediate dorsal cutaneous nerves of foot o Deep peroneal Motor branches in leg o Tibialis anterior o Extensor hallucis & Extensor digitorum longus o Peroneus tertius Lateral terminal branch in foot o Extensor digitorum brevis
May also be innervated by accessory deep peroneal from superficial peroneal (28%) Cutaneous: Skin between 1st & 2nd toes
Clinical syndrome
Weakness o Foot: Dorsiflexion & Eversion of foot o Toes: Extension o Gait: Steppage Sensory loss o Lower leg: Anterolateral o Foot & Toes: Dorsum Tendon reflexes: Normal Pain & Tinel's sign: Over lateral fibular neck
Differential diagnosis
L5 root: EHL may be weaker than Anterior tibial Lumbosacral trunk or plexus Sciatic nerve: Lateral trunk
Causes
External compression o Fibular head lesion Etiologies o Especially with weight loss o Altered consciousness: Coma, Anesthesia, Sleep & Bed rest o Crossed legs o Leg braces Partial lesion: More involvement of deep peroneal than superficial peroneal axons o Distal: Superficial peroneal nerve (Sensory branches) Branches: Medial & Intermediate Dorsal cutaneous branches Clinical o Sensory loss: Medial dorsal foot up to ankle Trauma: Blunt; Traction; Fractures o Ankle: Acute plantar flexion & inversion Entrapment o Squatting (Gardners & Farmers): Lesion locations Compression between biceps tendon & lateral head of gastrocnemius + Head of the fibula
Fibular tunnel Anterior tarsal tunnel: Deep peroneal nerve o Masses Ganglia: From the superior tibiofibular joint Baker's cyst Schwannoma & Neurofibromas: Especially in popliteal fossa o Fibular tunnel: Crescentic band at origin of peroneus longus Mononeuropathy in systemic disorder o HNPP o Vasculitis o Diabetes mellitus o Leprosy Deep peroneal o Anterior compartment syndrome Raised pressure in fascial compartment Causes: Excessive exercise, Soft tissue trauma, fractures, haemorrhage, occlusion of anterior tibial artery Clinical associations: Leg swelling o Compression: Ganglia, Osteochondroma, Aneurysm o At ankle Trauma & External compression Weak: Extensor digitorum brevis Superficial peroneal o Peroneal compartment syndrome o Local trauma o Compression of sensory branch when traversing deep fascia of lower leg
External link: Wheeless
POSTERIOR TIBIAL NERVE Anatomy
Formed by: Axons from L4, L5, S1 & S2 roots Anatomy o Anterior component: Muscles of posterior thigh (except short head of biceps) o Popliteal space: Branches to popliteus; Gastrocnemius; Soleus; Plantaris
o o o
Posterior compartment of leg: Tibialis posterior, Flexor hallucis longus; Flexor digitorum brevis Behind medial malleolus to plantar side of foot Tarsal Tunnel Anatomy: Behind mdial malleolus; Covered by flexor retinaculum Contents: Tibial nerve; Tibial artery; Tendons FHL, FDL, Tibialis posterior Distal tibial nerve branches Medial & Lateral Calcaneal: Sensory supply to heel of sole Medial Plantar nerve o Sensory: Medial 3 1/2 toes o Motor: Abductor hallucis brevis; Flexor hallucis brevis; Flexor digitorum brevis; Lumbricales Lateral Plantar nerve o Sensory: Little toe & Lateral 4th toe o Motor: Abductor digiti quinti brevis; FDB; Quadratus plantae
Tarsal Tunnel Syndrome
Anatomy: Entrapment of tibial nerve in tarsal tunnel Clinical o Pain Peri-malleolar Ankle & Sole: Burning; Worse with weight bearing & at night Tinel sign: Over tarsal tunnel Ankle dorsiflexion o Paresthesias & Sensory loss Sole of foot o Intrinsic foot muscles: Weak & Wasted o Tendon reflexes: Normal Causes o Mass in tunnel: Lipoma, Ganglia, Neoplasms o Exostosis within the tarsal tunnel o Accessory flexor digitorum longus muscle: 4% to 8% of legs o Hindfoot valgus deformity o Athletics: Heavy stress on ankle joint; Sprinting, Jumping Differential diagnosis o Sensory polyneuropathy o Orthopedic: Fasciitis; Tendonitis
External link: Wheeless
LATERAL FEMORAL CUTANEOUS NERVE
Anatomy o Direct extensions from L2 & L3 roots o Passes under inguinal ligament o Sensory distribution: Anterior lateral thigh o May anatomose with: Superior perforator & Median perforator nerves More anterior thigh sensory field Lateral Femoral Cutaneous Neuropathy: Meralgia paresthetica o Entrapment site: Inguinal ligament o General Male ? > Female Age: Mean 51 years; Range 15 to 81 years; Most frequent 4th & 5th deacde Symptom duration: 0.5 months to 20 years; Mean 3 years o Clinical Pain: Burning, tingling, Aching Sensory loss o Sharply defined region o Anterior or Lateral thigh or Both o Never involves: Patella; Knee; Lateral iliac crest Tendon reflexers: Normal Strength: Normal Bilateral: 10%; Usually asymmetric o Predisposing factors Obesity Tight pants or belt Diabetes: Occasional; Not clearly associated Pregnancy Abdominal pressure: Increased Surgery: Spine; Pelvic osotomy o NCV Side to side variation of orthodromic amplitude >2.3 fold SNAP amplitude < 3 V o Management Conservative in most cases Weight loss Eliminate tight fitting clothes
FEMORAL NERVE
Anatomy o Roots: L2, L3, L4 o Derived from: Lumbar plexus o Branches above inguinal ligament: Psoas; Iliacus o Below inguinal ligament: Divides into anterior & posterior divisions Anterior: Medial & intermediate cutaneous nerves of thigh; Sartorius & Pectineus muscle Posterior: Quadriceps femoris (Vasti & Rectus femoris); Saphenous nerve Neuropathy o General Weakness: Hip flexion; Knee extension Sensory loss: Anterior & Medial thigh; Medial leg to medial malleolus Tendon reflex: Knee reduced or absent o Lesions Compression: Surgical positioning (Lithotomy) & retraction Ischemia: Renal transplantation; Diabetes Retroperitoneal hemorrhage: Lumbar plexopathy with prominent femoral involvement Saphenous nerve: Axonal loss with increasing age
S-ar putea să vă placă și
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Prenatal ExercisesDocument17 paginiPrenatal Exercisesapi-3729544100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Asthma Speaker KitDocument75 paginiAsthma Speaker KitRicha SoodÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Roods ApproachDocument33 paginiRoods ApproachRicha SoodÎncă nu există evaluări
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Term Paper PTY 313Document1 paginăTerm Paper PTY 313Richa SoodÎncă nu există evaluări
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Ankylosing Spondylitis: Dr. Amit DhawanDocument15 paginiAnkylosing Spondylitis: Dr. Amit DhawanRicha SoodÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Gamesmanship Vs SportsmanshipDocument4 paginiGamesmanship Vs SportsmanshipMahendra DashÎncă nu există evaluări
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Lustria Rules Warhammer FantasyDocument26 paginiLustria Rules Warhammer FantasyChris Nye33% (3)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Shoulder Injuries in Baseball PlayersDocument7 paginiShoulder Injuries in Baseball PlayersMahayu Firsty RamadhaniÎncă nu există evaluări
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Orthopedic Secrets, 3rd EditionDocument61 paginiOrthopedic Secrets, 3rd EditionPJHG100% (10)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Crime Scene EssayDocument2 paginiCrime Scene Essayapi-239393191Încă nu există evaluări
- Fluid Management and Obstetric ShockDocument188 paginiFluid Management and Obstetric Shocksprimal50% (2)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Broadcast Wo ToppatsureDocument37 paginiBroadcast Wo ToppatsureYona Yohana SÎncă nu există evaluări
- Dius PDFDocument7 paginiDius PDFIulia MihaelaÎncă nu există evaluări
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Shoulder JointDocument11 paginiShoulder JointsaymynamesÎncă nu există evaluări
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- STITCHES Lyrics and Chords SHAWN MENDES @Document21 paginiSTITCHES Lyrics and Chords SHAWN MENDES @Rova Lavi SynÎncă nu există evaluări
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Electrical SafetyDocument4 paginiElectrical Safetykevin vadhiya kevin vadhiyaÎncă nu există evaluări
- Performance Checklist - ROMDocument3 paginiPerformance Checklist - ROMCrishaGarraÎncă nu există evaluări
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- 3M Venture Tape 1599B TDS v12-2017Document2 pagini3M Venture Tape 1599B TDS v12-2017Hernan Romero RomeroÎncă nu există evaluări
- Letter of ApologyDocument2 paginiLetter of ApologyLaura DorobanțuÎncă nu există evaluări
- P - C M A: RE Ompetition Edical SsessmentDocument15 paginiP - C M A: RE Ompetition Edical Ssessmentalfonsogarciapolo7350Încă nu există evaluări
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Coroner's Report On CyclingDocument42 paginiCoroner's Report On CyclingTorontoistÎncă nu există evaluări
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- RESEARCH THESIS (IZAZ Khan)Document51 paginiRESEARCH THESIS (IZAZ Khan)Izaz KhanÎncă nu există evaluări
- Pre-Trial Brief SampleDocument6 paginiPre-Trial Brief SampleKL Nav100% (1)
- ASCA L1 Fundamental Strength & Power Exercises & TechniquesDocument13 paginiASCA L1 Fundamental Strength & Power Exercises & TechniquesAllyn PreeceÎncă nu există evaluări
- Risk Assessment For Installation of HVAC Duct and AccessoriesDocument15 paginiRisk Assessment For Installation of HVAC Duct and AccessoriesAnandu Ashokan67% (3)
- Evaluating Long Bone Fractures in Children A BiomechanicalDocument20 paginiEvaluating Long Bone Fractures in Children A BiomechanicalIlma Kurnia SariÎncă nu există evaluări
- The Rules With No Name Playsheet 2 Hit Location ChartDocument2 paginiThe Rules With No Name Playsheet 2 Hit Location Chartadlard_matthewÎncă nu există evaluări
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Short Stripping of The Incompetent Great Saphenous Vein by InvisiGrip ® Vein StripperDocument5 paginiShort Stripping of The Incompetent Great Saphenous Vein by InvisiGrip ® Vein StripperFrancesca MazzolaniÎncă nu există evaluări
- Jurisprudence Case StudyDocument9 paginiJurisprudence Case StudyVasuKaushikÎncă nu există evaluări
- SImple Comfort 2210 ManualDocument28 paginiSImple Comfort 2210 ManualGarry HeidornÎncă nu există evaluări
- Arthroscopic Management of Distal Radius FracturesDocument255 paginiArthroscopic Management of Distal Radius FracturesFebryLasantiÎncă nu există evaluări
- People vs. Almonte 56 Phil 54Document7 paginiPeople vs. Almonte 56 Phil 54Emmylou Shayne LayogÎncă nu există evaluări
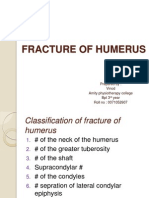
- Fracture of HumerusDocument56 paginiFracture of HumerusDr. Vinod Gupta100% (2)
- Lesson Plan On Post Natal ExercisesDocument11 paginiLesson Plan On Post Natal Exercisesvarshasharma0593% (15)
- Acute Kidney Injury in Crush Syndrome and Renal Disaster-Experience in Bangladesh After Garment Factory CollapseDocument6 paginiAcute Kidney Injury in Crush Syndrome and Renal Disaster-Experience in Bangladesh After Garment Factory CollapseMinerva Medical Treatment Pvt LtdÎncă nu există evaluări
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)