Documente Academic
Documente Profesional
Documente Cultură
General Features of The Immune System
Încărcat de
Minerva Bautista RoseteDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
General Features of The Immune System
Încărcat de
Minerva Bautista RoseteDrepturi de autor:
Formate disponibile
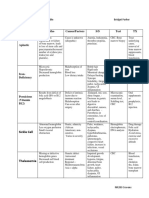
General Features of the Immune System Deficiency infections, tumor Hyperactive fatal disease Autoimmunity immune reaction vs own
tissues and cells Mechanisms of immunity: 1. Innate immunity - inherent 2. Adaptive immunity Only IgG passes placenta passive immunity Innate natural, native immunity -defense mechanism -1st line of defense Epithelial barriers (intact skin, mucous mem), phago cells, dendritic cells, NK, plasma proteins no need for previous exposure Lymphocyte one nucleus, dense, chromatin basophilic and faint ring of bluish cytoplasm Vs Natural killer more cytoplasm, + granules in cytoplasm 2 most impt cellular rxns 1. Inflammation phago cells (neutron, then monocytes) 2. Anti-viral defense dendritic and NK cells - Dendritic: Langerhan cells immature cells in epithelium with dendrites (endings have projections which pick up viruses) Adaptive Acquired, specific Mechanisms that are stimulated by microbes and capable of recognizing non microbial substances (Ag) Ag char large molecules; have specific complex configuration Develop later after exposure to microbes More powerful immune response Consists of lymphocytes and their products like Aby + cytokines a. Cell mediated or cellular vs IC and EC microbes, parasites, abnormal cells - Mediated by T cells (passes through thymus where genes are assembled and where it possesses receptors by
which it recognizes Ag; immature to immunocompetent); thymic dependent lymphocyte - i.e. TB with lipid covering resistant - virus-infected cells, tumors b. Humoral vs EC microbes and toxins (diffused in the tissue) - Mediated by B cells and Aby - Birds: cloaca has lymphoid follicles called Bursa of Fabricius equivalent to B cells in humans which mature in bone marrow (gene rearrangement in bm progenitor B cells possess receptors) transform to plasma cells after stimulation plenty of RER which synthesize proteins (gamma globulins) called antibodies Components of the Immune system Lymphocytes - CD4+ (T4) and CD8+ (T8) - Nave lymphocytes/ progenitors immunologically inexperienced - Effector cells eliminates microbes - First exposure clone first (mitosis) one population produces cytokines, the others become memory cells (with heightened awareness because they have previous exposure) - Memory cells: basis of vaccination Homing: lymph node Cortex and medulla T cells go to the paracortical/ parafollicular area B cells go to the germinal center T cells from bm stem cells Mature in thymus Found in blood 60-70% and tcell zones = paracortical TCR recognizes peptides presented by MHC of APC needed before activation of Tcells Don t recognize Ag by themselves Macrophages engulf bacteria digest protein mac has MHC or HLA (human lymphocyte antigen) through the MHC, give Ag to T cell which has TCR
B cells from bm precursors Found in blood 10-20% and lymphoid follicles (GC) Recognize Ag by Bcell Ag rec complex (IgM) that can recognize Ag (bacteria, not processed peptide) directly Stimulation by Ag and other signals Develop into plasma cells eccentric nucleus, chromatin condensed at periphery, many ER (SER, RER) Aby gamma globulins Electrophoretic tracing: Albumin, alpha, beta, gamma (increases during immune response) Antibody H chain L chain Fab key-lock interaction, specific i.e. staphyloccus has M protein, heart muscle has M protein so anti-streptococcal antibody reacts with the heart (cross-reaction autoimmune disease) Fc complement Monomer D, E, G Dimer A; in mucous membranes; secretory Ig - In the intestines, dimer form is resistant to digestion Pentamer M; 10 binding sites; first Aby produced; immune response later on changes to IgG DC interdigitating - Most important APC (first to encounter because present in muc mem, skin; under the epithelium) - Located under epithelia and interstitial - Dendritic langerhans cells Follicular DC - Found in GC - Has Fc rec for IgG and rec for C3b Macrophages -APC in T cell activation Key effectors in CMI Involved in effector phase humoral immunity
(because T helper cells activate B cells) NK cells 10-15% of blood lymphocytes Large granular lymphocytes Ability to kill infected and tumor cells without prior exposure or activation to the Ag Part of innate immune sys CD16 , Cd56 aby-dependent cell mediated cytotoxicity (ag must first react with aby) They have inh rec which are inh from reacting against self-antigens Fxns balanced by activating and inhibtory rec Secretes cytokines like ifn gamma (antiviral protein) Cytokines messenger molecules of immune system Tissues of the Immune System Generative lymphoid organs thymus and bm Peripheral lymphoid organs - Ln, spleen, mucosal and cutaneous lymphoid tissues, mucosal associated lymphoid tissue (MALT) - B cell in white pulp, t cell around splenic arterioles - MALT: tonsils, peyer s patches, in appendix Lymphocyte recirculation More on T cells B cells stay, Aby circulates T cell t cell zone ag from APC activation circulation tissues, microbes MHC mol -
Impt in Ag recognition by T cells Assoc with many autoimmune dse Products of genes that evoke rejection of transplanted organs Display peptide fragments of proteins for recog by Ag-specific T cells Chromosome 6 Mhc complex or HLA complex
Class I Expressed on all nucleated cells and platelets Encoded by HLA-A, B, C Bind peptides derived from proteins like viral Ag in the cytoplasm recognized by CD8 T cells Class II CD4 T cells Encoded by HLA-D Mhc locus also has genes that encode complement component, tnf, endotoxin? HLA and Dse assoc 1. Inflame dse hla-B27 asso with ankylosing spondylitis 2. Inherited errors of metab Hla bw47 21 hydroxylase def Hla a hereditary hemochromatosis 3. Autoimmune DR locus Cytokines produced by T cells Messenger mol of IS Short acting soluble mediators IL Mediate innate immunity TNF, il1, 12, type 1 ifn, ifn-y, chemokines Adaptive responses il 2, 4, 5, 17, ifn y Stimulate hemtopoiesis CSFs Hypersensitivity Reactions Altered reaction Exogenous and endogenous ag may trigger hypersensitivity rxns Often assoc with inheritance of susc genes Imbalance bet effector mech of immune responses and control mechanisms 1. 2. 3. 4. Immediate hypersensitivity Aby-mediated affects cells Immune complex mediated Cell mediated delayed type because i.e. tuberculin test if sensitized to TB, after 48 hours, reaction occurs 1-3 are humoral involved 4 are CMI
Immediate -rapid immunologic rxn within iminutes after combi of Ag (allergen with Ab IgE bound to mast cells (in tissues) of previously sensitized individuals -allergy - IgE: very minimal in the blood (measured in nanograms) in allergic rxn, increase Basophilic cells in tissue mast cells Most mediated by TH2, IgE Aby, mast cells Release of mediators and proinflammatory cytokines A. Systemic usu. Fallows injection of Ag -may be in state of shock within mins (anaphylactic shock) B. Local 1. Immediate or initial phase 2. Late phase Mast cells bm derived - Near bv, n, subepith - Have cytoplasmic membrane bound basophilic granules with mediators - Have igE Fc receptors - Sensitizing dose (1st exposure) Allergen -> APC -> TH cells -> cytokines (IL4) -> B cells -> Ig E mast cells release granules which are mediators (i.e. histamine) --IL3, IL 5 GMCSF eosinophilic recruitment (figure: initial response, late-phase) More than 2 hrs to 8 hrs. Basophils similar to mast cells; found in circulation; recruited to inflam sites TH2 ini and propag - IL4 B cells switch to IgE and THw production (autocrine) -promotes inflammation Preformed mediators (w/in mast cells) 1. Vasoactive amines hista 2. Enzymes 3. Proteoglycans
Lipid mediators synth in mast cell mem - Activates PLA2 - LT, PG D2 LT C4 and D4 most potent vasoactive and spasmogenic agents - B4 chemotactic for neutrophils, eosinophils, monocytes PG D2 most abundant mediator from COX pathway - Bronchospasm - Increased mucus secretion PAF PL aggregation -histamine release - bronchospasm Inc vasc perm Cytokines tnf , il-1,4, chemokines; many from mast cells Eosinophils -recruited by chemokines -il5 most potent eosinophil activating cytokine -liberate proteolytic enzymes, MBP, eosinophilic cationic proteins Type 1 hypersensitivity -susc genetically determined Basis not clear Chr 5q31 and 69 Atopy predisposition to develop localized immediate hypersensitivity Non-atopic allergy triggered byt T extremes and exercise; no TH2 cells nor IgE involved Systemic anaphylaxis vascular shock (vasodilation, pooling of blood, cold extremities); edema; DOB - May go into shock - i.e. penicillin, food allergens, insect toxins local immediate hypersens -allergic rxns -atopic allergy -dses: urticaria, angioedema, allergic rhinitis, bronchial asthma Aby mediated hypersens (type ii) cytotoxic type
mediated by aby directed toward ag on cell surfaces or ECM - 3 mech o Opsoni and phago o Complement and Fc mediated inflame o Aby-mediated cellular dysfunction I. Opsonization - Cells opsonized by IgG aby are recognized by phagocyte Fc rec - Phago and destruction of opsonized cell follows - C3b is an opsonin; c3a is anaphylatoxic and chemotactic - Act of complement also occurs - Formation of MAC c5b-c9 cell lysis - MAC acts like an enzyme phospholipase destroy cell mem Complement pathway - Transfusion reactions (type A patient transfused with type b blood) - Erythroblastosis fetalis (HDN) RhAg of baby plus anti-Rh (from previous exposure) of mother who is Rh - Autoimmune hemolytic anemia, agranulocytosis, thrombocytopenia - Drug reactions i.e. malarial drugs which combine with RBC ag ADCC Cell lysis without phagocytosis Nk cells reproduce perforin which perforate CM
Complement and Fcrec mediated inflammation -abs deposit into fixed tissues, injuries due to inflame Complement activated c3a, c5a (chemotactic to neutrophils) Fc rec involvement -GN, vascular rejection Aby mediated cellular dysfunction -impariment; no injury no inflammation (?) - MG, pemphigus vulgaris, Grave s disease
- thyroid has TSH rec bind TSH from pituitary hyperplasia, produce T3, T4 negative feedback - abN: autoimmune Aby vs receptor thyroid is stimulated without hormone excess T3, T4 because no negative feedback Type 3 Tissue damage by inflame at the site of deposition of the immune complex (IC) Mostly Ag-aby within circulation
a. Presence of immune reaction specific for self-ag or self-tissue b. Reaction is not secondary to tissue damage c. Absence of another well defined cause of dse. Types: organ specific or generalized/systemic Tolerance lack of rxn to self ag Autoimmune dse loss of self tolerance Immunological tolerance: phenomenon of unresponsiveness to an ag as a result to exposure of lymphocytes to that Ag Self tolerance Central tolerance death of slef reactive t and b cells clones cduring maturation ___ - In thymus, immature t cells with tcrs enocutner ag and die by apopotosis (negative selection or deletion) - Autoimmune regulatore AIRE stimulates expression of some peripheral ____________ - In bm, b cell receptor editing renders b cell not specific for self aG; apoptosis occurs if editing doesn t occur - _____ Peripheral tolerance mech that silence self reactive cells inperipheral tissues a. Prolonged or irreversible functional inactivation of lymphocytes b. Suppression by regulatory T cells regulatory t cells dvelop in thymus or ______ CD 25 c. Deletion by activation induced cell death mutation in Foxp3 causes sever AI _________ - Cd4 T cells undergo apoptosis Ag sequestration some Ag are hidden from the immune system - Testis, eye, brain (immune privileged sites) - Sympathetic ophthalmia (Ag released from damaged eye have
Formation, deposition, inflammation (fibrinoid necrosis) 2 types: 1. Generalized 2. arthus reaction Table 6-5 Immunofluor microscopy Granular fluor exogenous Linear fluor endogenous (i.e. glomerular basement membrane) Type 4 -initiated by Ag activated t cells 1. delayed - CD4 2. Direct cell toxicity CD8 Delayed Granulomatous disease (mycobacteria, fungi) Tuberculin skin test Transplant rejection Contact dermatitis Macrophage epitheliod giant cells CTL mediated Neoplastic cell lysis Transplant rejection Virus infected cells (hepatitis) Type1 diabetes -produce perforin and introduce granzyme Autoimmune diseases - Immune rxns against self-ag 3 requirements
aby that attack ag in the other eye which was initially inflamed) Combi of inheritance of susc genes and environmental triggers - Inheritance of susc genes o Contribute to breakdown of self-tolernace__________ - Environmental o Promote activation of selfreactive lympho o i.e. infections, tissue damage o mechanisms ______ general features: single organ RA, hashimoto s 2-3 sjogren Multi-system sle, scleroderma, mixed CT dse RA Arthrtiogenic Ag loss of self-tolerance CD4 T cell activation release cytokines and inflame mediators >> Pannus reaction of T4 with Ag in joint Sjogren Chronic dse characterized by dry eyes, dry mouth Immunologic destruction of ____ 2 forms: primary, secondary Sicca syndrome 3rd and 4th branchial pouch thymus, parathyroid
S-ar putea să vă placă și
- DR - Gold Immunology NotesDocument11 paginiDR - Gold Immunology NotesAaron PhuaÎncă nu există evaluări
- Epilepsy: Causes of Seizures (Non-Epileptic)Document5 paginiEpilepsy: Causes of Seizures (Non-Epileptic)humdingerÎncă nu există evaluări
- Immune Disorders ExplainedDocument5 paginiImmune Disorders ExplainedThalia Fortune100% (1)
- University of Santo Tomas: Faculty of Pharmacy - Department of Medical TechnologyDocument7 paginiUniversity of Santo Tomas: Faculty of Pharmacy - Department of Medical TechnologyWynlor AbarcaÎncă nu există evaluări
- The Immune System DefencesDocument6 paginiThe Immune System DefencesKa-Shun Leung100% (1)
- Inflammatory Response and Vascular Permeability ChangesDocument20 paginiInflammatory Response and Vascular Permeability Changesjeffaguilar100% (2)
- Immune System Lecture NotesDocument2 paginiImmune System Lecture NotesPrabin KumarÎncă nu există evaluări
- NSAID's "Non-Steroidal Anti-Inflammatory Drugs": Mmbakhaitan@uqu - Edu.saDocument19 paginiNSAID's "Non-Steroidal Anti-Inflammatory Drugs": Mmbakhaitan@uqu - Edu.saAhmed HossamÎncă nu există evaluări
- Pathology B - Gastrointestinal Tract (Esguerra, 2015)Document18 paginiPathology B - Gastrointestinal Tract (Esguerra, 2015)Ars MoriendiÎncă nu există evaluări
- Safety Moment Manual LiftingDocument1 paginăSafety Moment Manual LiftingEvert W. VanderBerg100% (1)
- ToonHub - Articles of PartnershipDocument13 paginiToonHub - Articles of PartnershipKingÎncă nu există evaluări
- Autoimmune Disorders: DR Muhammad ZUBAIR Consultant Chemical PathologistDocument52 paginiAutoimmune Disorders: DR Muhammad ZUBAIR Consultant Chemical PathologistZubair YousafÎncă nu există evaluări
- B Cell PDFDocument65 paginiB Cell PDFChandan KumarÎncă nu există evaluări
- The Immune SystemDocument15 paginiThe Immune SystemAslak Torgersen100% (1)
- Overview of The Immune System 2020Document31 paginiOverview of The Immune System 2020mehakÎncă nu există evaluări
- Deadly UnnaDocument2 paginiDeadly Unnaroflmaster22100% (2)
- Diseases of ImmunityDocument13 paginiDiseases of ImmunityRose AnnÎncă nu există evaluări
- Nephrotic Nephritic SyndromsDocument4 paginiNephrotic Nephritic SyndromsKimiwari100% (2)
- Complement SystemDocument4 paginiComplement SystemFait HeeÎncă nu există evaluări
- Kargil Untold StoriesDocument214 paginiKargil Untold StoriesSONALI KUMARIÎncă nu există evaluări
- Application Performance Management Advanced For Saas Flyer PDFDocument7 paginiApplication Performance Management Advanced For Saas Flyer PDFIrshad KhanÎncă nu există evaluări
- English: Quarter 1 - Module 1Document16 paginiEnglish: Quarter 1 - Module 1Ryze100% (1)
- World War 2 Soldier Stories - Ryan JenkinsDocument72 paginiWorld War 2 Soldier Stories - Ryan JenkinsTaharÎncă nu există evaluări
- Human Resource Development's Evaluation in Public ManagementDocument9 paginiHuman Resource Development's Evaluation in Public ManagementKelas KP LAN 2018Încă nu există evaluări
- 03 Adaptive Immune SystemDocument14 pagini03 Adaptive Immune SystemEnea NastriÎncă nu există evaluări
- Handouts Immune Defenses F11Document12 paginiHandouts Immune Defenses F11Kelly Trainor100% (1)
- NephroticDocument8 paginiNephroticsangheetaÎncă nu există evaluări
- Patho CA - Acute PancreatitisDocument1 paginăPatho CA - Acute PancreatitisKÎncă nu există evaluări
- Essential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsDocument5 paginiEssential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsRika Ariyanti SaputriÎncă nu există evaluări
- Goljan Notes on Oxygen Transport and Tissue HypoxiaDocument5 paginiGoljan Notes on Oxygen Transport and Tissue HypoxiaDaniyal AzmatÎncă nu există evaluări
- Nephrotic Syndrome WikipediaDocument10 paginiNephrotic Syndrome WikipediaJohn KevlarÎncă nu există evaluări
- Skin Structure and Function GuideDocument10 paginiSkin Structure and Function GuideyassrmarwaÎncă nu există evaluări
- Renal SyndromeDocument13 paginiRenal SyndromeAndreas KristianÎncă nu există evaluări
- SYPHYLISDocument1 paginăSYPHYLISkhadzxÎncă nu există evaluări
- Non-Pathogenic Intestinal Amoebae Cyst MorphologyDocument2 paginiNon-Pathogenic Intestinal Amoebae Cyst MorphologyCoy NuñezÎncă nu există evaluări
- Chronic Inflammatory Dermatoses Inflammatory Blistering DisordersDocument4 paginiChronic Inflammatory Dermatoses Inflammatory Blistering DisordersspringdingÎncă nu există evaluări
- MCB 252 Final Exam Study GuideDocument62 paginiMCB 252 Final Exam Study GuideJay ZÎncă nu există evaluări
- Abdominal Wall, Omentum, Mesentery, Retroperitoneum Anatomy and ConditionsDocument6 paginiAbdominal Wall, Omentum, Mesentery, Retroperitoneum Anatomy and ConditionsMon Ordona De GuzmanÎncă nu există evaluări
- Histo Review 2Document13 paginiHisto Review 2Coy NuñezÎncă nu există evaluări
- Pelvis and Perineum Clinical CorrelationDocument4 paginiPelvis and Perineum Clinical CorrelationKeesha Mariel AlimonÎncă nu există evaluări
- Cytogenetics Basics: Chromosomes, Analysis & AbnormalitiesDocument11 paginiCytogenetics Basics: Chromosomes, Analysis & Abnormalitiesjo_jo_mania100% (1)
- Cycle CellDocument16 paginiCycle CellRohingya EnglishÎncă nu există evaluări
- NPTEL – Cellular and Molecular Immunology: Antibodies and AntigensDocument33 paginiNPTEL – Cellular and Molecular Immunology: Antibodies and AntigensAygul RamankulovaÎncă nu există evaluări
- Harrisons: Introduction To Infectious DiseasesDocument3 paginiHarrisons: Introduction To Infectious Diseasesapi-3704562Încă nu există evaluări
- Kidney Physiology (Q & A)Document28 paginiKidney Physiology (Q & A)ramadan100% (1)
- Clin Path Trans 3.05 Urinalysis (2b)Document6 paginiClin Path Trans 3.05 Urinalysis (2b)Reymart FernandezÎncă nu există evaluări
- Cell Adaptation and Necrosis: Hypertrophy, Atrophy, MetaplasiaDocument8 paginiCell Adaptation and Necrosis: Hypertrophy, Atrophy, MetaplasiaivankcurryÎncă nu există evaluări
- Cytogenetics Course Module at AMYA Polytechnic CollegeDocument29 paginiCytogenetics Course Module at AMYA Polytechnic Collegeanonymous squashÎncă nu există evaluări
- The Complement SystemDocument4 paginiThe Complement SystemExamville.com100% (1)
- Identify viscus from histological featuresDocument1 paginăIdentify viscus from histological featuresNaser Hamdi ZalloumÎncă nu există evaluări
- Immune System Review QuestionsDocument2 paginiImmune System Review Questionsapi-521773978Încă nu există evaluări
- Kidney NewDocument4 paginiKidney NewParth BhayanaÎncă nu există evaluări
- 2011 07 Microbiology Mycobacterium Skin InfectionDocument6 pagini2011 07 Microbiology Mycobacterium Skin InfectionCristinaConcepcionÎncă nu există evaluări
- 5 Cyto AbnormalDocument9 pagini5 Cyto AbnormalMerli Ann Joyce CalditoÎncă nu există evaluări
- Source Hormone Major Action: Adrenal CortexDocument3 paginiSource Hormone Major Action: Adrenal CortexReisha FungoÎncă nu există evaluări
- Actinic Keratosis: (Aka Bowen's Disease)Document5 paginiActinic Keratosis: (Aka Bowen's Disease)fadoÎncă nu există evaluări
- Major Bacterial Genera TableDocument12 paginiMajor Bacterial Genera TablemojdaÎncă nu există evaluări
- 4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangDocument4 pagini4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangMiel Raphael AranillaÎncă nu există evaluări
- Generic Name Brand Name Drug Class Mechanism of Action StructureDocument4 paginiGeneric Name Brand Name Drug Class Mechanism of Action StructurenoelkiddoÎncă nu există evaluări
- (8!5!13) Cell Injury OutlineDocument9 pagini(8!5!13) Cell Injury OutlineBhumiShahÎncă nu există evaluări
- Anatomy Formative Preview of Thorax and BackDocument22 paginiAnatomy Formative Preview of Thorax and Backmvs hardhikÎncă nu există evaluări
- Systemic Effects of Inflammation: The Acute Phase ResponseDocument3 paginiSystemic Effects of Inflammation: The Acute Phase ResponseJenward Hostallero100% (1)
- Anemia Table283Document2 paginiAnemia Table283Bridget ParkerÎncă nu există evaluări
- Robbins Notes: Aging, Radiation, and Inflammation Self StudyDocument44 paginiRobbins Notes: Aging, Radiation, and Inflammation Self StudyJustine HungÎncă nu există evaluări
- Immunology Course SummaryDocument30 paginiImmunology Course SummaryKiller VÎncă nu există evaluări
- Immunity: Innate Defenses Specific Immunity Cell Mediated Immunity Self RecognitionDocument56 paginiImmunity: Innate Defenses Specific Immunity Cell Mediated Immunity Self RecognitionMiranda sekar arumÎncă nu există evaluări
- Basic Immunology IDocument57 paginiBasic Immunology Idevika priyavathi0% (1)
- J PamintuanDocument9 paginiJ PamintuanMinerva Bautista RoseteÎncă nu există evaluări
- Bliss vs. DiazDocument11 paginiBliss vs. DiazMinerva Bautista Rosete100% (1)
- People vs. SalazarDocument7 paginiPeople vs. SalazarMinerva Bautista RoseteÎncă nu există evaluări
- Cournot CompetitionDocument1 paginăCournot CompetitionMinerva Bautista RoseteÎncă nu există evaluări
- 21st Century Literature Course PaperDocument4 pagini21st Century Literature Course PaperMinerva Bautista Rosete33% (3)
- List of Philippine PresidentsDocument1 paginăList of Philippine PresidentsMinerva Bautista RoseteÎncă nu există evaluări
- What's at Stake in Our Case Vs ChinaDocument5 paginiWhat's at Stake in Our Case Vs ChinaMinerva Bautista RoseteÎncă nu există evaluări
- Bir Vat QueriesDocument8 paginiBir Vat QueriesMinerva Bautista RoseteÎncă nu există evaluări
- BMW E9x Code ListDocument2 paginiBMW E9x Code ListTomasz FlisÎncă nu există evaluări
- Karnataka PUC Board (KSEEB) Chemistry Class 12 Question Paper 2017Document14 paginiKarnataka PUC Board (KSEEB) Chemistry Class 12 Question Paper 2017lohith. sÎncă nu există evaluări
- Dealer DirectoryDocument83 paginiDealer DirectorySportivoÎncă nu există evaluări
- Sustainable Marketing and Consumers Preferences in Tourism 2167Document5 paginiSustainable Marketing and Consumers Preferences in Tourism 2167DanielÎncă nu există evaluări
- License Key Windows 8Document7 paginiLicense Key Windows 8Juned FahriÎncă nu există evaluări
- Dr. Xavier - MIDocument6 paginiDr. Xavier - MIKannamundayil BakesÎncă nu există evaluări
- UNIT 1 Sociology - Lisening 2 Book Review of Blink by Malcolm GladwellDocument9 paginiUNIT 1 Sociology - Lisening 2 Book Review of Blink by Malcolm GladwellNgọc ÁnhÎncă nu există evaluări
- ILOILO Grade IV Non MajorsDocument17 paginiILOILO Grade IV Non MajorsNelyn LosteÎncă nu există evaluări
- Virtuoso 2011Document424 paginiVirtuoso 2011rraaccÎncă nu există evaluări
- FIITJEE Talent Reward Exam 2020: Proctored Online Test - Guidelines For StudentsDocument3 paginiFIITJEE Talent Reward Exam 2020: Proctored Online Test - Guidelines For StudentsShivesh PANDEYÎncă nu există evaluări
- PRI Vs SIP Trunking WPDocument3 paginiPRI Vs SIP Trunking WPhisham_abdelaleemÎncă nu există evaluări
- EB - Lecture 2 - ECommerce Revenue Models - HDocument8 paginiEB - Lecture 2 - ECommerce Revenue Models - HXolani MpilaÎncă nu există evaluări
- Network Profiling Using FlowDocument75 paginiNetwork Profiling Using FlowSoftware Engineering Institute PublicationsÎncă nu există evaluări
- Concepts of Human Development and Poverty: A Multidimensional PerspectiveDocument3 paginiConcepts of Human Development and Poverty: A Multidimensional PerspectiveTasneem Raihan100% (1)
- Intracardiac Echo DR SrikanthDocument107 paginiIntracardiac Echo DR SrikanthNakka SrikanthÎncă nu există evaluări
- Com 10003 Assignment 3Document8 paginiCom 10003 Assignment 3AmandaÎncă nu există evaluări
- First Time Login Guidelines in CRMDocument23 paginiFirst Time Login Guidelines in CRMSumeet KotakÎncă nu există evaluări
- Plo Slide Chapter 16 Organizational Change and DevelopmentDocument22 paginiPlo Slide Chapter 16 Organizational Change and DevelopmentkrystelÎncă nu există evaluări
- Syllabus For The Post of ASI - Traffic - WardensDocument2 paginiSyllabus For The Post of ASI - Traffic - WardensUbaid KhanÎncă nu există evaluări
- Decision Support System for Online ScholarshipDocument3 paginiDecision Support System for Online ScholarshipRONALD RIVERAÎncă nu există evaluări
- Does social media improve or impede communicationDocument3 paginiDoes social media improve or impede communicationUmar SaleemÎncă nu există evaluări
- String length recommendations and brace height advice for Uukha bowsDocument1 paginăString length recommendations and brace height advice for Uukha bowsPak Cik FauzyÎncă nu există evaluări