Documente Academic
Documente Profesional
Documente Cultură
Procreative Health Is The Moral Obligation of Parents To Have The Healthiest Children Through All Natural and Artificial Means Available
Încărcat de
Frankie MacabadaDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Procreative Health Is The Moral Obligation of Parents To Have The Healthiest Children Through All Natural and Artificial Means Available
Încărcat de
Frankie MacabadaDrepturi de autor:
Formate disponibile
Liceo de Cagayan University Cagayan de Oro
Home work in Maternal 101 Definition of Procreative Health Procreative Health and Theories Process of Human Creation Risk Factors that will lead to Genetic Disorders Common Tests for Determination of Genetic Abnormalities Utilization of the Nursing process in the Genetic Alteration & in the care of clients seeking services before & during Conception
Submitted by: Franklin Macabada BSN2
Submitted to: Ms. Judith T. Dalman NCM 101 Lecture CI
June 29, 2011
Procreative Health is the moral obligation of parents to have the healthiest children through all natural and artificial means available. Different Theories Creation is the making of all things from nothing, by an act of God, at some time in the past. God's action could have taken a second, or 6 days, or a million years. Evolutionary theory is the theory that all things came about by the repeated random actions of natural selection, whereby: 1. Life came into existence, and then 2. Primitive life evolved into more and more complex organisms, and eventually producing mankind. Evolutionary theory requires the assumption of billions of years for its processes. A Malthusian catastrophe (also called a Malthusian check, crisis, disaster, or nightmare) was originally foreseen to be a forced return to subsistence-level conditions once population growth had outpaced agricultural production. Later formulations consider economic growth limits as well. Based on the work of political economist Thomas Malthus (17661834), theories of Malthusian catastrophe are very similar to the subsistence theory of wages. The main difference is that the Malthusian theories predict over several generations or centuries, whereas the subsistence theory of wages predicts over years and decades. Process: Fertilization The primary goal of sex is to merge the sperm and egg (fertilization) to make a baby. In many organisms, sex occurs outside of the body. For example, in most fish or amphibians, females lay eggs somewhere (usually on the sea/river bed), the male comes along and sprays the eggs with sperm and fertilization takes place. In reptiles and mammals (including humans), fertilization takes place inside the body of the female (internal fertilization). This technique increases the chances of successful sexual reproduction. Because we use internal fertilization, our sexual organs are specialized for this purpose. Delivering Sperm Cells The sperm are made in the testes. During sexual intercourse, smooth muscles contract and propel mature sperm from the end portions of the epididymis through a long tube (vas deferens or ductus deferens) inside the body, just beneath the bladder. From there, the sperm get mixed with nutrientrich fluids from the seminal vesicles and a milky secretion from the prostate gland. This combination of sperm and fluids is called semen. The semen does three things:
Provides a watery environment in which the sperm cells can swim while outside the body Provides nutrients for the sperm cells (fructose, amino acids, vitamin C) Protects the sperm cells by neutralizing acids in the female's sexual tract
Once the semen is made, it passes through another tube (urethra) within the penis, exiting the body through the opening of the penis. One last male organ is a tiny, pea-sized set of glands inside the body at the base of the penis, called the bulbourethral or Cowper's glands. During sexual excitation, and just prior to the ejection of sperm (ejaculation), the Cowper's glands secrete a tiny amount of fluid that neutralizes any traces of acidic urine that may be leftover in the urethra. It is also believed that these secretions are designed to lubricate the penis and female tract during sexual intercourse.
Female Sex Organs All of the female's sexual organs are located within her body except the vulva. The vulva consists of two sets of folded skin (labia major, labia minor) that cover the opening to the reproductive tract, and a small nub of sensitive, erectile tissue (clitoris), which is the remnant of the fetal penis (see next page). The two ovaries are the major female sex organs, the counterpart of the male testes. The ovaries make the eggs, or oocytes, which are the female gametes, and produce estrogen, the female sex hormone. Estrogen causes female secondary sexual characteristics such as pubic hair, breast development, widening of the pelvis and deposition of body fat in hips and thighs. The ovaries are located in the abdomen. Eggs develop inside the ovary and are released upon ovulation into a tube (the oviduct or Fallopian tube) lined with fingerlike projections. The egg travels through the Fallopian tube, where fertilization can take place, to a muscular chamber called the uterus. The uterus is where the baby develops. It is made of smooth muscle and is normally about the size and shape of a small pear turned upside down. During pregnancy, it can stretch to about the size of a basketball to hold the developing baby. The base of the uterus (neck of the pear) is a muscular wall called the cervix. In the cervix is a tiny opening, about the size of a pinhead, called the external os. The external os is filled with a thick plug of protein (mucus) that serves as a barrier to the entrance of the uterus. The cervix leads into a smooth-muscle-walled tube called the vagina, or birth canal. The vagina connects the uterus to the outside of the body, and its opening is covered by the labia. The vagina receives the male's penis during sexual intercourse and delivers the baby during childbirth. The vagina is normally narrow (except around the cervix), but can stretch during intercourse and childbirth. Finally, two sets of glands, the greater vestibular gland (Bartholin's gland) and the lesser vestibular gland, are located on either side of the vagina and empty into the labial folds of skin. The secretions from these glands lubricate the labial folds during sexual excitation and intercourse. Development of Sex Organs When we first develop, we have two sets of organs: one that can develop into the female sex organs (Mullerian duct) and one that can develop into the male sex organs (Wolffian ducts). Which sex organs develop depends on the presence of the male hormone testosterone (in humans, the default sex is female):
If the embryo is a male (XY chromosomes), then testosterone will stimulate the Wolffian duct to develop male sex organs, and the Mullerian duct will degrade. If the embryo is female (XX), then no testosterone is made. The Wolffian duct will degrade, and the Mullerian duct will develop into female sex organs. The female clitoris is the remnants of the Wolffian duct. If the embryo is a male (XY), but there is a defect such that no testosterone is made, then the Wolffian duct will degrade, and the Mullerian duct will develop into non-functional female sex organs.
Sex-organ development is determined by the third month of development. Risk Factors in Pregnancy
Every woman wants to have the best possible pregnancy. However, for some, there are certain things that are just too hard to give up. Caffeine is perhaps one of the hardest things to give up, but it is important to think about the health of your baby and to cut back on your daily intake, even if you're just thinking about becoming pregnant. Recent studies have shown that caffeine can increase a woman's risk of miscarriage. Find out more about how this substance can negatively affect your pregnancy. Before you think about getting pregnanat, also visit your doctor and talk to him about any medications that you are taking especially if they are anti-epileptic drugs for your epilepsy. Some medications can cause birth defects in your baby. Find out more today. Alcohol, Smoke And Eating Disorders If you like to drink, read our article about the effects consuming alcohol during pregnancy. Pregnancy and Alcohol will help you understand better why you need to cut out that glass of wine with your meal. And Beyond Fetal Alcohol Syndrome will show you how the dangers of drinking during pregnancy can be more far-reaching than you've ever imagined. Eating disorders can pose some risks to mother and baby and can also cause emotional difficulties for the pregnant mother. Smoking During Pregnancy and Marijuana and Pregnancy will provide you with invaluable information about why these two common activities can seriously harm your baby. If you are a smoker who's looking to quit, then check out our Tips to Quit Smoking and help yourself butt-out! If you're not a smoker but live with someone who is, then you'll want to read Second Hand Smoke and Pregnancy to learn how breathing in second hand smoke can be just as bad for you and your baby. Toxins, Chemicals and Pesticides Toxins, Pesticides and Pregnancy will help you avoid some common chemicals you may never have thought to avoid during your pregnancy. And if you have an outdoor cat, then take a look at Toxoplasmosis, which outlines a rare but serious infection that you may be at risk of contracting. However, some chemicals you may not have had a choice about being exposed to. Up until the 1970s, many women were prescribed DES to help minimize their rsik of miscarriage. Unfortunately, the drug had the opposite affect and is still impacting women today. Another pregnancy risk factor that you may not have heard of is Fifth Disease, a viral infection that could lead to pregnancy complications. After you give birth, be aware of any heavy bleeding. Although rare, postpartum hemorrhaging can be very dangerous to a woman. Common Tests During Pregnancy What is Prenatal Screening? First Trimester Prenatal Screening Tests First trimester screening is a combination of fetal ultrasound and maternal blood testing performed during the first trimester of pregnancy. This screening process can help to determine the risk of the fetus having certain birth defects. Screening tests may be used alone or in combination with other tests.
There are three parts of first trimester screening:
ultrasound test for fetal nuchal translucency (NT) Nuchal translucency screening uses an ultrasound test to examine the area at the back of the fetal neck for increased fluid.
two maternal serum (blood) tests The blood tests measure two substances found in the blood of all pregnant women:
o o
pregnancy-associated plasma protein screening (PAPP-A) - a protein produced by the placenta in early pregnancy. Abnormal levels are associated with an increased risk for chromosome abnormality. human chorionic gonadotropin (hCG) - a hormone produced by the placenta in early pregnancy. Abnormal levels are associated with an increased risk for chromosome abnormality.
When used together as first trimester screening tests, nuchal translucency screening and maternal blood tests have a greater ability to determine if the fetus might have a birth defect, such as Down syndrome, trisomy 18, or trisomy 13. If the results of these first trimester screening tests are abnormal, genetic counseling is recommended. Additional testing such as chorionic villus sampling or amniocentesis may be needed for accurate diagnosis. Second Trimester Prenatal Screening Tests Second trimester prenatal screening may include several blood tests, called multiple markers. These markers provide information about a woman's risk of having a baby with certain genetic conditions or birth defects. Screening is usually performed by taking a sample of the mother's blood between the 15th and 20th weeks of pregnancy (16th to 18th is ideal). The multiple markers include:
alpha-fetoprotein screening (AFP) - a blood test that measures the level of alphafetoprotein in the mothers' blood during pregnancy. AFP is a protein normally produced by the fetal liver and is present in the fluid surrounding the fetus (amniotic fluid), and crosses the placenta into the mother's blood. The AFP blood test is also called MSAFP (maternal serum AFP). Abnormal levels of AFP may signal the following:
o o o o o o
open neural tube defects (ONTD) such as spina bifida Down syndrome other chromosomal abnormalities defects in the abdominal wall of the fetus twins - more than one fetus is making the protein a miscalculated due date, as the levels vary throughout pregnancy
hCG - human chorionic gonadotropin hormone (a hormone produced by the placenta) estriol - a hormone produced by the placenta inhibin - a hormone produced by the placenta
Abnormal test results of AFP and other markers may indicate the need for additional testing. Usually an ultrasound is performed to confirm the dates of the pregnancy and to look at the fetal spine and other body parts for defects. An amniocentesis may be performed to assess for elevated amniotic fluid levels of AFP and other chemicals which may indicate the presence of spina bifida. Multiple marker screening is not diagnostic. It is only a screening test to determine who in the population should be offered additional testing for their pregnancy. There can be false positive
results, indicating a problem when the fetus is actually healthy. There can also be false negative results, indicating a no abnormality when the fetus actually does have a health problem. When a woman has both first and second trimester screening tests performed, the ability of the tests to detect an abnormality is greater than using just one screening independently. Over 80 percent of fetuses affected with Down Syndrome can be detected when both first and second trimester screening are used. What is an amniocentesis? An amniocentesis is a procedure used to obtain a small sample of the amniotic fluid that surrounds the fetus to diagnose chromosomal disorders and open neural tube defects (ONTDs) such as spina bifida. There is a small risk of miscarriage associated with amniocentesis which must be balanced with the risk of an abnormality and the patients desires. Testing is available for other genetic defects and disorders depending on the family history and availability of laboratory testing at the time of the procedure. An amniocentesis is generally offered to women between the 15th and 20th weeks of pregnancy who are at increased risk for chromosome abnormalities, such as women who are over age 35 years of age at delivery, or those who have had an abnormal maternal serum screening test, indicating an increased risk for a chromosomal abnormality or neural tube defect
How is an amniocentesis performed? An amniocentesis is a procedure that involves inserting a thin needle through the mother's abdomen into the amniotic sac to withdraw a small sample of the amniotic fluid for examination. The amniotic fluid contains cells shed by the fetus, which contain genetic information. Although specific details of each procedure vary slightly, generally, an amniocentesis follows this process:
The woman's abdomen is cleansed with an antiseptic. The physician may/may not give a local anesthetic to numb the skin. Ultrasound is used to help guide a hollow needle into the amniotic sac. A small sample of fluid is withdrawn for laboratory analysis. Strenuous activities should be avoided for 24 hours following an amniocentesis. Women may feel some cramping during or after the amniocentesis.
Women with twins or other multiples need sampling from each amniotic sac, in order to study each baby. Depending on the position of the baby, placenta, amount of fluid, or patient's anatomy, sometimes the amniocentesis cannot be performed. The fluid is sent to a genetics laboratory so that the cells can grow and be analyzed. Alpha-fetoprotein, a protein made by the fetus that is present in the fluid, is also measured to rule out an open neural tube defect, such as spina bifida. Results are usually available in about 10 days to two weeks, depending on the laboratory. What is a chorionic villus sampling (CVS)? Chorionic villus sampling (CVS) is a prenatal test that involves taking a sample of some of the placental tissue. This tissue contains the same genetic material as the fetus and can be tested for chromosomal abnormalities and some other genetic problems. Testing is available for other genetic defects and disorders depending on the family history and availability of laboratory testing at the time of the procedure. In comparison to amniocentesis (another type of prenatal test), CVS does not provide information on neural tube defects such as spina bifida. For this reason, women who undergo CVS also need a follow-up blood test between 16 to 18 weeks of their pregnancy, to screen for neural tube defects. How is CVS performed?
CVS may be offered to women who are at increased risk for chromosomal abnormalities or have a family history of a genetic defect that is testable from the placental tissue. CVS is usually performed between the 10th and 12th weeks of pregnancy. Although exact methods can vary, the procedure involves inserting a small tube called a catheter through a woman's vagina and into her cervix and usually follows this process. Another method is transabdominal CVS, which involves inserting a needle through the woman's abdomen and into her uterus to sample the placental cells. Ultrasound is used to guide the catheter (for transvaginal CVS) or needle (for transabdominal CVS) into place near the placenta. Tissue is removed using a syringe on the other end of the catheter. Women may feel some cramping during and after the CVS procedure. The tissue samples are sent to a genetic laboratory to grow and be analyzed. Results are usually available in about 10 days to two weeks, depending on the laboratory.
Women with twins or other multiples usually need sampling from each placenta. However, because of the complexity of the procedure, and positioning of the placentas, CVS is not always feasible or successful with multiples. Some women may not be candidates for CVS or may not obtain results that are 100 percent accurate, and may therefore require a follow-up amniocentesis. In some cases there is an active vaginal infection such as herpes or gonorrhea, which will prohibit the procedure. Other times the physician obtains a sample that does not have enough tissue to grow in the laboratory, such that results are incomplete or inconclusive. What is fetal monitoring? During late pregnancy and during labor, your physician may want to monitor the fetal heart rate and other functions. Fetal heart rate monitoring is a method of checking the rate and rhythm of the fetal heartbeat. The average fetal heart rate is between 110 and 160 beats per minute. The fetal heart rate may change as the fetus responds to conditions in the uterus. An abnormal fetal heart rate or pattern may mean that the fetus is not getting enough oxygen or there are other problems. An abnormal pattern also may mean that an emergency or cesarean delivery is needed. How is fetal monitoring performed? Using a fetoscope (a type of stethoscope) to listen to the fetal heart beat is the most basic type of fetal heart rate monitoring. Another type of monitoring is with a hand held Doppler device. This is often used during prenatal visits to count the fetal heart rate. During labor, continuous electronic fetal monitoring is often used, especially if an abnormal rhythm is heard with the fetoscope. Although the specific details of each procedure vary slightly, generally, electronic fetal monitoring follows this process:
Gel is applied to the mother's abdomen to act as a medium for the ultrasound transducer. The ultrasound transducer is attached to the abdomen with straps and transmits the fetal heartbeat to a recorder. The fetal heart rate is displayed on a screen and printed onto special paper. During contractions, an external tocodynamometer (a monitoring device that is placed over the top of the uterus with a belt) can record the patterns of contractions.
Sometimes, internal fetal monitoring is necessary for a more accurate reading of the fetal heart rate. Your bag of waters (amniotic fluid) must be broken and your cervix must be partially dilated to use internal monitoring. Internal fetal monitoring involves inserting an electrode through the dilated cervix and attaching the electrode to the scalp of the fetus, called a fetal scalp electrode.
What is a glucose tolerance test? A glucose tolerance test, usually conducted in the 24 to 28 weeks of pregnancy, measures levels of sugar (glucose) in the mother's blood. Abnormal glucose levels may indicate gestational diabetes. How is a glucose tolerance test performed? Although the specific details of each procedure vary slightly, generally, a glucose tolerance test follows this process:
The mother-to-be may be asked to only drink water on the day the glucose tolerance test is given. An initial fasting sample of blood is drawn from a vein. You will be given a special glucose solution to drink. Blood will be drawn several times over the course of several hours to measure the glucose levels in your body.
What is a Group B strep culture? Group B Streptococcus (GBS) are bacteria found in the lower genital tract of about 25 percent of all women. GBS infection usually causes no problems in women before pregnancy, but can cause serious illness in the mother during pregnancy and the newborn after delivery. GBS may cause chorioamnionitis (a severe infection of the placental tissues) and postpartum infection. Urinary tract infections caused by GBS can lead to preterm labor and birth. GBS is the most common cause of life-threatening infections in newborns, including pneumonia and meningitis. Newborn babies contract the infection during pregnancy or from the mother's genital tract during labor and delivery.
The Centers for Disease Control and Prevention (CDC) recommends screening of all pregnant women for vaginal and rectal group B strep colonization between 35 to 37 weeks gestation. Treatment of mothers with certain risk factors or positive cultures is important reduce the risk of transmission of GBS to the baby. Babies whose mothers receive antibiotic treatment for a positive GBS test are 20 times less likely to develop the disease than those without treatment. What is an ultrasound? An ultrasound scan is a diagnostic technique which uses high-frequency sound waves to create an image of the internal organs. A screening ultrasound is sometimes done during the course of a pregnancy to check normal fetal growth and verify the due date. Ultrasounds may be performed at various times throughout pregnancy for different reasons: In the first trimester:
to establish the dates of a pregnancy to determine the number of fetuses and identify placental structures to diagnose an ectopic pregnancy or miscarriage to examine the uterus and other pelvic anatomy in some cases to detect fetal abnormalities
Mid-trimester: (sometimes called the 18 to 20 week scan)
to to to to to to to to to to
confirm pregnancy dates determine the number of fetuses and examine the placental structures assist in prenatal tests such as an amniocentesis examine the fetal anatomy for presence of abnormalities check the amount of amniotic fluid examine blood flow patterns observe fetal behavior and activity examine the placenta measure the length of the cervix monitor fetal growth
Third trimester:
to monitor fetal growth to check the amount of amniotic fluid as part of other testing such as the biophysical profile to determine the position of a fetus to assess the placenta
How is an ultrasound scan performed? Although the specific details of each procedure vary slightly, generally, ultrasounds follow this process. Two types of ultrasounds can be performed during pregnancy:
abdominal ultrasound In an abdominal ultrasound, gel is applied to the abdomen and the ultrasound transducer glides over the gel on the abdomen to create the image.
transvaginal ultrasound In a transvaginal ultrasound, a smaller ultrasound transducer is inserted into the vagina and rests against the back of the vagina to create an image. A transvaginal ultrasound produces a sharper image and is often used in early pregnancy.
Ultrasound images may be captured in still photographs or on video to document findings. Ultrasound is a technique that is constantly being improved and refined. As with any test, results may not be completely accurate. However, ultrasound can provide valuable information for parents and health care providers to help manage and care for the pregnancy and fetus. In addition, ultrasound gives parents have a unique opportunity to see their baby before birth, helping them to bond and establish an early relationship. What is genetic screening? Many genetic abnormalities can be diagnosed before birth. Your physician may recommend genetic testing during the pregnancy if you or your partner have a family history of genetic disorders and/or you have had a fetus or baby with a genetic abnormality. Examples of genetic disorders that can be diagnosed before birth include the following:
cystic fibrosis Duchenne muscular dystrophy
hemophilia A thalassemia sickle cell anemia polycystic kidney disease Tay-Sachs disease
What do genetic screening methods include? Genetic screening methods may include the following:
ultrasound scan alpha-fetoprotein test (AFP) or multiple marker test chorionic villus sampling (CVS) amniocentesis percutaneous umbilical blood sampling (withdrawing a small sample of the fetal blood from the umbilical cord)
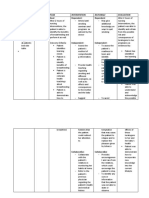
Pregnancy Nursing Care Plans Nurses specializing in obstetrics understand the importance of ensuring a healthy mother and a healthy baby. In order to design a tailored pregnancy nursing care plan, it is necessary to have a baseline of the pregnant or post-partum patient's condition, whether that be hemorrhage, preeclampsia or ectopic pregnancy, to name a few. An effective nursing care plan for pregnancy patients should include assessment, promoting autonomy and patient teaching. Assessment
Assessment, the first element in the nursing process, is what nurses use to establish baseline information for patients. This begins with a thorough head-to-toe overview. Assess the patient's head and neck, noting any enlarged lymph nodes, thyroid or other abnormalities. Moving down, check the patient's heart rate and breathing, and report any signs of shortness of breath. Also document the patient's fundal height and fetal assessment. Pay special attention to any edema in the extremities or subjective reports of pain in the calves. Laboratory results are also reviewed and documented.
Promoting Autonomy
As the pregnant patient watches their body change, she may begin to feel at a loss of control of her body or well-being. A pregnancy nursing care plan acknowledges and respects those feelings, while focusing on promoting patient autonomy. Interventions that the patient can perform for themselves should be included in the nursing care plan. For example, if a particular goal on the nursing care plan states that the patient will be free of nausea and vomiting by their third trimester, a patient intervention might include avoiding areas with strong or offensive smells and eating crackers. This allows the patient to feel proactive and more involved in their own health care maintenance.
Patient Education
Pregnancy nursing care plans most often include patient education listed as a goal and as a nursing intervention. Teaching the pregnant patient how to recognize normal and abnormal symptoms in her body provides an extra line of defense against fetal health risks that might otherwise go unnoticed or addressed too late. It also helps mothers-tobe feel more comfortable about the birthing process and post-partum life. This may include information about proper diet, the risks and benefits of medications and activities that should be avoided during pregnancy and immediately post-partum. Patient teaching also should include information on birthing options, breastfeeding and bottle feeding.
S-ar putea să vă placă și
- Philippine Health Agenda - Dec1 - 1 PDFDocument26 paginiPhilippine Health Agenda - Dec1 - 1 PDFreyalene gallegosÎncă nu există evaluări
- Evolution of PHN in The PhilippinesDocument34 paginiEvolution of PHN in The PhilippinesRika MaeÎncă nu există evaluări
- Elderhood: Jerry Mae Chiong Joliza Lancara Dianne Kay Fernandez Rhea Joy GolenaDocument50 paginiElderhood: Jerry Mae Chiong Joliza Lancara Dianne Kay Fernandez Rhea Joy GolenaRj Santiago0% (1)
- Nursing Associations in The PhilippinesDocument18 paginiNursing Associations in The PhilippinesGumama AmeiyrhaÎncă nu există evaluări
- CHN 1 Module 1Document10 paginiCHN 1 Module 1Dianne LabisÎncă nu există evaluări
- 1 Community Immersion Leadership PlanDocument6 pagini1 Community Immersion Leadership PlanmarcamilleÎncă nu există evaluări
- Abnormal uterine bleeding case studyDocument37 paginiAbnormal uterine bleeding case studyMary Grace MasÎncă nu există evaluări
- An Overview of Community Health Nursing Practice in The PhilippinesDocument21 paginiAn Overview of Community Health Nursing Practice in The PhilippinesWilma BeraldeÎncă nu există evaluări
- New Technologies Related To Public Health Electronic InformationDocument20 paginiNew Technologies Related To Public Health Electronic InformationMarlon Glorioso II100% (2)
- NCM 117J (Maladaptive Pattern of Behavior) : Overview of Psychiatric Mental Health Nursing Module 1/7Document41 paginiNCM 117J (Maladaptive Pattern of Behavior) : Overview of Psychiatric Mental Health Nursing Module 1/7Abdelmar Susulan100% (1)
- AILYNDocument98 paginiAILYNArvin EstebanÎncă nu există evaluări
- OVERVIEW OF Public Health Nursing in The PhilippinesDocument13 paginiOVERVIEW OF Public Health Nursing in The Philippinesjanina myka100% (1)
- Spiritual Needs of A Patient With Acute IllnessDocument3 paginiSpiritual Needs of A Patient With Acute IllnessMarimiel PagulayanÎncă nu există evaluări
- National Health Situation On MCNDocument1 paginăNational Health Situation On MCNLuiciaÎncă nu există evaluări
- Filipino Culture and Myths Related to Maternal CareDocument4 paginiFilipino Culture and Myths Related to Maternal CareKatie Holmes0% (1)
- NCM 109 Care of Mother and Child at RiskDocument10 paginiNCM 109 Care of Mother and Child at RiskMia Fe Cuaya Lorenzo100% (1)
- Standards of Public Health Nursing in The PhilippinesDocument18 paginiStandards of Public Health Nursing in The PhilippinesWilma BeraldeÎncă nu există evaluări
- EPI - AND - IMCI - Docx Filename - UTF-8''EPI AND IMCIDocument14 paginiEPI - AND - IMCI - Docx Filename - UTF-8''EPI AND IMCIYvonne Carmel Aguilar SunigaÎncă nu există evaluări
- Code of Good Governance As Applied To Nursing PracticeDocument7 paginiCode of Good Governance As Applied To Nursing PracticeLoi Ocampo CrespoÎncă nu există evaluări
- Agenda in The PhilippineDocument10 paginiAgenda in The PhilippineMikhaela Andree Mariano100% (1)
- Nursing Care of Pregnancy ComplicationsDocument3 paginiNursing Care of Pregnancy ComplicationsGynesis Lim Roquero100% (1)
- I. Framework For Maternal and Child Health Nursing (MCN) Focusing On At-Risk, High Risk, and Sick ClientsDocument5 paginiI. Framework For Maternal and Child Health Nursing (MCN) Focusing On At-Risk, High Risk, and Sick ClientsSophia Loraine Dorone Jesura100% (1)
- 1.2 NCM 109 - Genetic Assessment and Genetic CounselingDocument7 pagini1.2 NCM 109 - Genetic Assessment and Genetic CounselingSittie Haneen Tabara100% (1)
- Legal Mandates R/T Nutrition and Diet TherapyDocument6 paginiLegal Mandates R/T Nutrition and Diet TherapySam Albert RenaciaÎncă nu există evaluări
- Making of Homemade Salt and Sugar SolutionDocument2 paginiMaking of Homemade Salt and Sugar SolutionShing Mae MarieÎncă nu există evaluări
- A. Nursing Process in The Care of Population, Groups, and CommunityDocument6 paginiA. Nursing Process in The Care of Population, Groups, and Communityanne marie50% (2)
- Balance Skeletal TractionDocument5 paginiBalance Skeletal TractionRachel Ann JimenezÎncă nu există evaluări
- CHN Bag ContentsDocument1 paginăCHN Bag ContentsJulia Shane BarriosÎncă nu există evaluări
- Child Discharge Plan: Medication, Therapy, Diet, Follow Up CareDocument1 paginăChild Discharge Plan: Medication, Therapy, Diet, Follow Up CareInosanto May AnnÎncă nu există evaluări
- 10 Herbal Medicines Approved by DOH for Various AilmentsDocument10 pagini10 Herbal Medicines Approved by DOH for Various AilmentsMark Cruze100% (1)
- Philippine Health Care LawsDocument5 paginiPhilippine Health Care LawstonytorrejonÎncă nu există evaluări
- Care - of - Mother - Child - and - Adolescent 2Document48 paginiCare - of - Mother - Child - and - Adolescent 2Jmarie Brillantes PopiocoÎncă nu există evaluări
- A Framework For Maternal and Child Health Nursing CareDocument3 paginiA Framework For Maternal and Child Health Nursing CarePatricia OrtegaÎncă nu există evaluări
- NCM 109N: Frameworks For Maternal & Child Health NursingDocument37 paginiNCM 109N: Frameworks For Maternal & Child Health NursingZudotaÎncă nu există evaluări
- Family Health NursingDocument11 paginiFamily Health NursingKBD100% (1)
- Concept of unitive and procreative healthDocument5 paginiConcept of unitive and procreative healthDONITA DALUMPINESÎncă nu există evaluări
- Implementing the FOURmula ONE Framework for Health Sector ReformDocument4 paginiImplementing the FOURmula ONE Framework for Health Sector ReformHEALTH_AMBASSADORS67% (3)
- Overview of Public Health Nursing in The PhilippinesDocument52 paginiOverview of Public Health Nursing in The PhilippinesWilma BeraldeÎncă nu există evaluări
- Supporting Preterm Infant CareDocument3 paginiSupporting Preterm Infant CareWindi Dawn Salleva50% (2)
- Re 111 Notes - Divine RevelationDocument2 paginiRe 111 Notes - Divine RevelationMark Vincent Bautista100% (1)
- Standards For Health Information in The Philippines 1999Document133 paginiStandards For Health Information in The Philippines 1999Alvin MarceloÎncă nu există evaluări
- Case Study 2: A Matter of Freedom: AnswerDocument1 paginăCase Study 2: A Matter of Freedom: AnswerApple Mae ToñacaoÎncă nu există evaluări
- Nursing Informatics Lecture Notes on IT SystemsDocument6 paginiNursing Informatics Lecture Notes on IT SystemsCatherine PradoÎncă nu există evaluări
- MCN National HealthDocument4 paginiMCN National HealthCamille RamosÎncă nu există evaluări
- Essential Intrapartum and Newborn Care (EINC) Bulletin 1Document10 paginiEssential Intrapartum and Newborn Care (EINC) Bulletin 1maxicap7386% (7)
- CHNN211 Week 2 Health Care Delivery SystemDocument7 paginiCHNN211 Week 2 Health Care Delivery SystemABEGAIL BALLORANÎncă nu există evaluări
- Etiology and biological theories of schizophreniaDocument6 paginiEtiology and biological theories of schizophreniaXerxes DejitoÎncă nu există evaluări
- Food AdministrationDocument23 paginiFood AdministrationRareÎncă nu există evaluări
- Nursing Informatics PhilippinesDocument2 paginiNursing Informatics PhilippinesJoji RodrigoÎncă nu există evaluări
- LEGAL MANDATES RELATED TO NUTRITION AND DIET THERAPY - NutriDiet LABDocument4 paginiLEGAL MANDATES RELATED TO NUTRITION AND DIET THERAPY - NutriDiet LABHarlene Joyce ReyÎncă nu există evaluări
- College of Nursing NCM 105A Nutrition and Diet Therapy LaboratoryDocument3 paginiCollege of Nursing NCM 105A Nutrition and Diet Therapy LaboratoryArriane Desepeda100% (1)
- Subjective: Goal: Dependent: Dependent:: Assessment Diagnosis Plan Intervention Rationale EvaluationDocument2 paginiSubjective: Goal: Dependent: Dependent:: Assessment Diagnosis Plan Intervention Rationale EvaluationTrisha Cayabyab100% (1)
- Proclamation No. 499Document21 paginiProclamation No. 499shaitabliganÎncă nu există evaluări
- Interprofessional Care in The CommunityDocument18 paginiInterprofessional Care in The CommunityCreciabullecer100% (1)
- COPAR community organizing researchDocument8 paginiCOPAR community organizing researchRoeder Max Pangramuyen0% (1)
- Sexual Reproduction in Humans CLASS 10Document5 paginiSexual Reproduction in Humans CLASS 10shallowÎncă nu există evaluări
- The Female Reproductive SystemDocument25 paginiThe Female Reproductive SystemIan Mizzel A. Dulfina100% (1)
- Where Women ch04 PDFDocument10 paginiWhere Women ch04 PDF55birdsÎncă nu există evaluări
- Female Reproductive System Research PaperDocument4 paginiFemale Reproductive System Research Paperc9sj0n70100% (1)
- Human Reproductive SystemDocument23 paginiHuman Reproductive SystemQuennie AceronÎncă nu există evaluări
- Philippine Reproductive HealthDocument10 paginiPhilippine Reproductive HealthFrankie MacabadaÎncă nu există evaluări
- National Voluntary Blood Services Program (NVBSP)Document10 paginiNational Voluntary Blood Services Program (NVBSP)Frankie Macabada100% (2)
- GCS WardclassDocument9 paginiGCS WardclassFrankie MacabadaÎncă nu există evaluări
- Geno GramDocument1 paginăGeno GramFrankie MacabadaÎncă nu există evaluări
- Case Study: Acute Myocardial InfarctionDocument1 paginăCase Study: Acute Myocardial InfarctionFrankie Macabada0% (1)
- Chronic Illness Trajectory ModelDocument2 paginiChronic Illness Trajectory ModelFrankie Macabada100% (1)
- Soapie GCP 2Document6 paginiSoapie GCP 2Frankie MacabadaÎncă nu există evaluări
- Flores The Mayo at The Missionaries of Africa CebuDocument1 paginăFlores The Mayo at The Missionaries of Africa CebuFrankie MacabadaÎncă nu există evaluări
- Final CP Taw-AsanDocument29 paginiFinal CP Taw-AsanFrankie MacabadaÎncă nu există evaluări
- Nursing Care Plan Psych 2Document5 paginiNursing Care Plan Psych 2Frankie MacabadaÎncă nu există evaluări
- AgeDocument11 paginiAgeFrankie MacabadaÎncă nu există evaluări
- Nursing Care PlanDocument1 paginăNursing Care PlanFrankie MacabadaÎncă nu există evaluări
- Final CP MigabonDocument31 paginiFinal CP MigabonFrankie MacabadaÎncă nu există evaluări
- Nokia 5233 settings guideDocument13 paginiNokia 5233 settings guideFrankie MacabadaÎncă nu există evaluări
- Case Work - Melissa Villaganas EditedDocument6 paginiCase Work - Melissa Villaganas EditedFrankie MacabadaÎncă nu există evaluări
- Pedia Care StudyDocument19 paginiPedia Care StudyFrankie MacabadaÎncă nu există evaluări
- ErniaDocument37 paginiErniaOskar MaÎncă nu există evaluări
- Hemorrhoids Pathophysiology and TreatmentDocument4 paginiHemorrhoids Pathophysiology and TreatmentBianca Freya Porral100% (4)
- Spesifikasi PHILIPS Ultrasound System EPIQ 5 WHC BasicDocument2 paginiSpesifikasi PHILIPS Ultrasound System EPIQ 5 WHC BasichsÎncă nu există evaluări
- Exploratory EssayDocument7 paginiExploratory Essaymd309610Încă nu există evaluări
- Final List DR 120Document153 paginiFinal List DR 120naveed khanÎncă nu există evaluări
- LEGAL MEDICINE EXAMDocument22 paginiLEGAL MEDICINE EXAMsescuzar100% (1)
- Brochure Ultrasonograph y of The Live Ru 42 eDocument132 paginiBrochure Ultrasonograph y of The Live Ru 42 ealiceinwinterÎncă nu există evaluări
- 1 Newborn Care and Physical AssessmentDocument79 pagini1 Newborn Care and Physical AssessmentWaleed AhmadÎncă nu există evaluări
- Apollo Hospital Marketing Assignment: 1. Executive SummaryDocument13 paginiApollo Hospital Marketing Assignment: 1. Executive Summaryraghavi20Încă nu există evaluări
- KINESIOLOGY TEST ON SUSPENSION THERAPYDocument2 paginiKINESIOLOGY TEST ON SUSPENSION THERAPYChaman Lal Karotia0% (1)
- Medical Negligence Dissertation TopicsDocument5 paginiMedical Negligence Dissertation TopicsWriteMyPaperForMeFastNaperville100% (1)
- Simple Kidney Cysts What Are Simple Kidney Cysts?Document3 paginiSimple Kidney Cysts What Are Simple Kidney Cysts?fkic charitasÎncă nu există evaluări
- Issue 22 - The Nurse Advocate - Hamad Medical Corporation - November 2015Document20 paginiIssue 22 - The Nurse Advocate - Hamad Medical Corporation - November 2015Brent ForemanÎncă nu există evaluări
- Patient SafetyDocument10 paginiPatient Safetyapi-324392818Încă nu există evaluări
- Notification Govt Medical College Hospital Chandigarh CMOs Demonstrator Other PostsDocument7 paginiNotification Govt Medical College Hospital Chandigarh CMOs Demonstrator Other PostsJeshiÎncă nu există evaluări
- Complete Septate Uterus in PregnancyDocument6 paginiComplete Septate Uterus in PregnancyfitriamarizkaÎncă nu există evaluări
- Orthodontic Study ModelDocument17 paginiOrthodontic Study ModelFaiznur FauziÎncă nu există evaluări
- Posterior Palatal Seal: DR Muaiyed BuzayanDocument22 paginiPosterior Palatal Seal: DR Muaiyed BuzayanMuhammad Herry SeptianoorÎncă nu există evaluări
- Fetal Neurophysiology According To Gestational Age Aida Salihagic Kadic, Maja PredojevicDocument5 paginiFetal Neurophysiology According To Gestational Age Aida Salihagic Kadic, Maja PredojevicDaniela Isidora San Martin CanalesÎncă nu există evaluări
- PicotDocument8 paginiPicotapi-259267079Încă nu există evaluări
- Structural Magnetic Resonance Imaging in Epilepsy: NeuroDocument11 paginiStructural Magnetic Resonance Imaging in Epilepsy: NeuroAnggit Adhi PrasetyaÎncă nu există evaluări
- Journal of Orthopaedics: A B C D C DDocument5 paginiJournal of Orthopaedics: A B C D C DRisa MarissaÎncă nu există evaluări
- S04 Class of Thora SP FxsDocument31 paginiS04 Class of Thora SP FxsDeep Katyan DeepÎncă nu există evaluări
- Cover Letters For Volunteer NurseDocument1 paginăCover Letters For Volunteer Nursehanna_ong_2100% (2)
- Solution Manual For Basic Allied Health Statistics and Analysis 4th EditionDocument7 paginiSolution Manual For Basic Allied Health Statistics and Analysis 4th EditionMichelleRowecgmeo100% (84)
- LP needle structure lumbar punctureDocument92 paginiLP needle structure lumbar punctureJohn M. Hemsworth100% (1)
- Assessment Skills For Paramedics by Amanda Blaber (Blaber, Amanda)Document509 paginiAssessment Skills For Paramedics by Amanda Blaber (Blaber, Amanda)Joseph Campos Sanchez100% (1)
- ChecklistDocument4 paginiChecklistRysan100% (1)
- Review: Benjamin O Anderson, Riccardo Masetti, Melvin J SilversteinDocument13 paginiReview: Benjamin O Anderson, Riccardo Masetti, Melvin J SilversteinsanineseinÎncă nu există evaluări
- Case Report: Oral White Sponge Nevus: An Exceptional Differential Diagnosis in ChildhoodDocument3 paginiCase Report: Oral White Sponge Nevus: An Exceptional Differential Diagnosis in ChildhoodAjengRamadhantyÎncă nu există evaluări