Documente Academic
Documente Profesional
Documente Cultură
Eview Rticle: Classifications of Esophagitis: Who Needs Them?
Încărcat de
Eliud GrajedaDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Eview Rticle: Classifications of Esophagitis: Who Needs Them?
Încărcat de
Eliud GrajedaDrepturi de autor:
Formate disponibile
REVIEW ARTICLE
Classications of esophagitis: Who needs them?
Devjit S. Nayar, MD, Michael F. Vaezi, MD, PhD
Cleveland, Ohio
GERD is a common condition, one that aficts a substantial proportion of the American population. It is estimated that 40% to 45% of Americans have symptoms of GERD each month. The diagnosis of GERD often is established on the basis of symptoms of heartburn and regurgitation. EGD is an important modality for assessing esophageal damage caused by GERD; however, the assessment of the degree of esophageal injury (i.e., esophagitis) observed at EGD is often subjective. To make this assessment more objective, multiple classication schemes for esophagitis have been proposed (Table 1).1-8 An important goal behind the effort to establish an endoscopic classication of esophagitis is an objective gradation of disease severity that can serve as a benchmark when comparing studies of esophagitis. However, given the multiple schemes currently available and the varied utility of these classications, this effort has lead to more confusion than clarity. Furthermore, because GERD often is treated empirically, based on presenting symptoms, the value of any grading scheme appears academic at best. Given this confusion, it is timely to review the various classications for grading esophagitis. From the early part of the twentieth century, esophagoscopy was dominated by specialists who dealt with diseases of the ears, nose, and throat (ENT). Savary was professor and chairman of the Department of Otorhinolaryngology at the University of Lausanne Medical School, Switzerland, when his seminal work, The Esophagus: Handbook and Atlas of Endoscopy, was published.1 Initially, the rigid endoscope was the only technology available for esophagoscopy and ENT specialists were procient in using this instrument to examine the esophagus.
Current afliation: Department of Gastroenterology and Hepatology, Center for Swallowing and Esophageal Disorders, Cleveland Clinic Foundation, Cleveland, Ohio. Reprint requests: Michael F. Vaezi, MD, PhD, FACG, Department of Gastroenterology and Hepatology, Center for Swallowing and Esophageal Disorders, Cleveland Clinic Foundation, 9500 Euclid Ave., Cleveland, OH 44195. Copyright 2004 by the American Society for Gastrointestinal Endoscopy 0016-5107/$30.00 PII: S0016-5107(04)01555-X VOLUME 60, NO. 2, 2004
By 1969, with the arrival of the beroptic endoscope, the gastroenterologist became even more closely involved in the evaluation of esophageal pathophysiology. In 1977, Savary and Miller (an academic gastroenterologist in Switzerland) collaborated in the creation of the Savary-Miller classication of esophagitis, which includes 4 grades of reux esophagitis (Table 2). Mild, and presumably early, esophagitis was graded 1 or 2, based on the presence of erosive lesions and their relationship to mucosal folds. Grade 3 included circumferential erosive lesions; grade 4 was reserved for chronic lesions: ulcer, stricture, columnar epithelium, and short esophagus. This classication was among the rst to describe the effects of gastroesophageal reux on the esophagus and was generally accepted through the 1980s. However, debate over the inclusion of complications of GERD, especially Barretts esophagus within grade 4, lead to the modied SavaryMiller classication (Table 2). The main distinction of this new classication was that the complication of columnar epithelium was transferred from grade 4 to a new grade 5.2 The Savary-Miller classication is still one of the most commonly used classication systems and is more popular in Europe than the United States. Hetzel et al.3 published the results of a study of the healing and relapse of reux esophagitis in response to treatment with omeprazole in 1988. Their classication of esophagitis (Hetzel-Dent) differed from the Savary-Miller classication in that it included mucosal changes such as erythema, friability, and hyperemia as grade 1 (Table 3). Unlike the Savary-Miller classication, the HetzelDent system graded the degree of injury, not by the number of lesions but by the surface area of injury, especially within the distal 5 cm of the esophageal squamous mucosa. A major criticism of this classication has been the subjective nature of grade 1 lesions and the inability of endoscopists to accurately and consistently label a mucosal lesion as red or friable. Given this subjectivity, interobserver reproducibility often is poor with the HetzelDent classication, especially for the lower grades of esophagitis.4 After its introduction, the Hetzel-Dent classication was commonly used in the United States and Australia. However, its use decreased markedly after introduction of the modied Los Angeles classication in 1999. Armstrong et al.5 proposed a new classication system for practicing clinicians and researchers in 1991. They criticized the prior classication schemes for using subtle mucosal changes as diagnostic criteria and because improvement in endoscopic grade was not associated with a corresponding
GASTROINTESTINAL ENDOSCOPY 253
D Nayar, M Vaezi
Classications of esophagitis: who needs them?
Table 1. Classications of esophagitis
Year 1977 Classication system Savary-Miller and Modied Savary-Miller (1989)
d
Strengths Contains: Degree of esophagitis Presence of stricture Presence of Barretts Radial extent is examined in more detail
d
Weaknesses Requires assessment of erosions and ulcers (depth of injury) Based on number of erosions Uses erythema and other minimal changes that are highly subjective ndings Must assess depth injury Limited to last 5 cm Few comparative studies Requires assessment of: Erosions and ulcers (depth of injury) Difcult to differentiate stricture from stenosis Lengthy Few comparative studies Does not incorporate presence/absence of Barretts Must assess length of mucosal break
1988
Hetzel-Dent
d d d
1991
MUSE
Contains: Degree of esophagitis Degree of stricture Degree of Barretts
d d
1996
Los Angeles and Modied Los Angeles (1999)
d d
Uses term mucosal break (no need to assess depth) More accurate assessment of radial extent Physiologically correlated Good comparative agreement studies
Table 2. Original (grades 1-4) and modied (grades 1-5) Savary-Miller classication
Grade 1 2 Lesion Single or isolated erosive lesion(s), oval or linear, but affecting only one longitudinal fold Multiple erosive lesions, non-circumferential, affecting more than one longitudinal fold, with or without conuence Circumferential erosive lesions Chronic lesions: ulcer(s), stricture(s) and/or short esophagus. Alone or associated with lesions of grades 1 to 3 Columnar epithelium in continuity with the Z line, non-circular, star-shaped, or circumferential. Alone or associated with lesions of grades 1 to 4 *Grade 5 was included in the original grade 4 classication.
Table 3. The Hetzel-Dent classication
Grade 0 1 2 Lesion No mucosal abnormalities No macroscopic erosions but erythema, hyperemia, or mucosal friability Supercial erosions involving <10% of the mucosal surface of the last 5 cm of esophageal squamous mucosa Supercial erosions or ulceration involving 10%-50% of the mucosal surface of last 5 cm of esophageal squamous mucosa Deep peptic ulceration anywhere in the esophagus or conuent erosion of >50% of the mucosal surface of the last 5 cm esophageal squamous mucosa
3 4
5*
improvement in symptoms. Their new system became known as the MUSE classication because it assessed the presence of columnar Metaplasia, mucosal Ulceration, Stricture formation, and Erosion(s) (Table 4). The severity of each type of lesion was subclassied by using 4 levels (0 = absent, 1 = mild, 2 = moderate, 3 = severe). The aim of Armstrong et al.5 was to create a classication for GERD that could be used in research and in clinical practice. However, because it is cumbersome, the MUSE classication has never been widely used. A more practical esophagitis classication system was introduced in 1996 at the meeting of the World Organization of Gastroenterology in Los Angeles.
254 GASTROINTESTINAL ENDOSCOPY
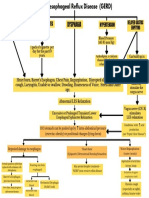
Called the Los Angeles (LA) classication, it used a grading scale from A through D (Table 5; Fig. 1).6 The goal of this classication was to reduce interpreter variability in the assessment of esophageal injury according to depth. Instead, the LA classication focuses on number, length, and location of mucosal breaks to determine the grade of esophageal injury. In the original study, good interobserver agreement was found for grades A and D, while that for grades B and C was poor. Thus, the LA classication was modied in 1999 by redening grade C as injury involving less than 75% of the circumference of the esophagus (Table 5).7 With this change, interobserver agreement for grades B and C improved. A review of major publications since 1980 (Table 6) shows that the Savary-Miller and the LA classiVOLUME 60, NO. 2, 2004
Classications of esophagitis: who needs them?
D Nayar, M Vaezi
Figure 1. Illustration depicting various grades of esophagitis according to the modied Los Angeles classication (1999).
Table 4. The MUSE classication
Grade* Metaplasia M1 M2 Ulcer U1 U2 Stricture S1 S2 Erosion E1 E2 Lesion Fingers +/ islands Circumferential 1 discrete ulcer $2 discrete conuent ulcers >9 mm (standard endoscope passes) #9 mm (standard endoscope does not pass) Only on peaks of folds Conuent: on and between folds
Table 5. The modied Los Angeles classication
Grade A B C Lesion One (or more) mucosal break on longer than 5 mm that does not extend between the tops of two mucosal folds One (or more) mucosal break more than 5-mm long that does not extent between the tops of two mucosal folds One (or more) mucosal break that is continuous between the tops of two or more mucosal folds but that involves less than 75% of the circumference One (or more) mucosal break that involves at least 75% of the esophageal circumference
*The degree was subscripted 0, absent; 1, mild; 2, moderate; and 3, severe, and later modied as above.
cations are currently the most popular systems in use.7-33 There appears to be a geographic variation with respect to the use of these two classications. Before 1999, 8 of 12 (67%) studies, predominantly from Europe, used the Savary-Miller classication. After its introduction, the LA scheme was used in 13 of 19 (68%) studies. In Japan and in the United States, the LA classication appears to predominate (Table 6). The ideal endoscopic grading system for esophagitis must be accurate and reproducible, as well as easy to remember and interpret. There are few comparative studies of the LA and Savary-Miller classications. However, it appears that the LA classication may have two advantages. First, observer agreement is good across the various grades of esophagitis.
VOLUME 60, NO. 2, 2004
In one study, 325 endoscopic photographs were randomly graded twice by 9 endoscopists.8 The intraobserver and the interobserver agreements were good (k = 0.545 and k = 0.556, respectively). Moreover, these agreements were independent of the level of reviewer expertise.6-8 The Savary-Miller classication does not perform as well when used by less experienced interpreters or for lower grades of esophagitis.4 In contrast, the reproducibility for grade A in the LA classication is acceptable (k = 0.65).7 Second, the LA classication may be the only classication in which grades of esophagitis correlate directly with the severity of esophageal acid exposure.7 Esophageal acid exposure was found to increase signicantly (p < 0.01) in a stepwise fashion across the LA esophagitis grading scale (percentage of time pH < 4: grade A, 9.3%; grade D, 19.1%).7 In addition, there was a graded healing response to acid
GASTROINTESTINAL ENDOSCOPY 255
D Nayar, M Vaezi
Classications of esophagitis: who needs them?
Table 6. Studies with endoscopic grade of esophagitis From 1980 to 2004
Investigator Okamoto et al. Shibuya et al.10 Inamori et al.11 Defreitas et al.12 Pandolno et al.8 Manabe et al.13 Dupas et al.14 Adachi et al.15 Sugiura et al.16 Lukas et al.17 Ishikawa et al.18 Deprez et al.19 Lundell et al.7 Fujimoto et al.20* Furukawa et al.21* and Soga et al.22 Kusano et al.23 Vcev et al.24 Watson et al.25 Armstrong et al.6 Csendes et al.26 Omura et al.27 Koop et al.28 Bytzer et al.4 Sciume et al.29 Mitov et al.30 Hetzel et al.3 Tytgat 31 Simon et al.32 Siewert et al.33
9
Publication year 2003 2003 2003 2002 2002 2002 2001 2001 2001 2000 2000 1999 1999 2003 1999 1999 1999 1999 1997 1996 1996 1995 1995 1993 1989 1989 1988 1987 1987 1986
Country Japan Japan Japan Brazil USA Japan France Japan Japan Czech Japan Belgium Worldwide Japan Japan Japan Croatia Australia Worldwide Chile Japan Germany Denmark Italy Bulgaria Australia Netherlands Germany Germany
Study type Cross sectional Retrospective cohort Cross sectional Prospective cohort Agreement Prospective cohort RCT Cross sectional Prospective cohort Retrospective cohort Prospective cohort Prospective cohort Prospective comparative Cross sectional RCT Prospective comparative RCT Prospective cohort Prospective comparative Cross sectional Prospective cohort RCT Prospective comparative Retrospective cohort Retrospective cohort RCT RCT RCT Prospective cohort
No. patients 1199 53 392 89 325 105 461 57 76 65 22 19 22 901 71 20 120 231 143 430 15 249 150 121 436 132 42 49 323
Classication system Los Angeles Los Angeles Los Angeles Savary-Miller Los Angeles and Hetzel-Dent Los Angeles Savary-Miller Los Angeles Los Angeles Savary-Miller Los Angeles Savary-Miller Los Angeles Los Angeles Los Angeles Los Angeles Savary-Miller Savary-Miller Los Angeles Savary-Miller AFP Savary-Miller Savary-Miller modied Savary-Miller Pluoke Hetzel-Dent Savary-Miller Savary-Miller Savary-Miller
RCT, Randomized controlled trial; AFP, anatomic-functional-pathologic classication. *Two studies different outcome measures from one patient population.
suppression: after 4 weeks of treatment with omeprazole (10 mg daily), complete healing was achieved in 77% of patients with grade A esophagitis, 50% of those with grade B, and only 20% of patients with grade C esophagitis. A classication of esophagitis is essential in clinical research and for trials of pharmacotherapy, because classication imposes consistency and provides an objective evaluation of response to therapy. For these purposes, the LA classication may be the most appropriate candidate. However, grading systems for esophagitis may have limited relevance in clinical practice. The majority of patients with GERD currently are treated empirically, without prior endoscopic evaluation. Although studies have shown that patients with advanced grades of esophagitis require chronic acid suppression, this level of severity often can be determined clinically based on symptom relapse when treatment is tapered.7 For practical purposes, classication of endoscopic ndings as normal, erosive or ulcerative esophagitis, and Barretts esophagus appears to be
256 GASTROINTESTINAL ENDOSCOPY
reproducible and easy to communicate. In addition, because endoscopic photodocumentation has become routine, a picture is worth a thousand words.
REFERENCES
1. Savary M, Miller G. The esophagus: handbook and atlas of endoscopy. Solothurn (Switzerland): Verlag Gassmann; 1978. p. 119-59. 2. Ollyo JB, Monnier M, Fontolliet C, Savary M. Classication endoscopique de loesophagite par reux. In: Rey JF, edtior. Paris: Video Digest; 1989. p. 145-55. 3. Hetzel DJ, Dent J, Reed WD, Narielvala FM, MacKinnon M, McCarthy JH, et al. Healing and relapse of severe peptic esophagitis after treatment with omeprazole. Gastroenterology 1988;95:903-12. 4. Bytzer P, Havelund T, Hansen JM. Interobserver variation in the endoscopic diagnosis of reux esophagitis. Scand J Gastroenterol 1993;28:119-25. 5. Armstrong D, Monnier P, Nicolet M, Blum AL, Savary M. Endoscopic assessment of oesophagitis. Gullet 1991;1:63-7. 6. Armstrong D, Bennett JR, Blum AL, Dent J, de Dombal FT, Galmiche JP, et al. The endoscopic assessment of esophagitis: a progress report on observer consistency. Gastroenterology 1996;111:85-92. 7. Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, et al. Endoscopic assessment of esophagitis: VOLUME 60, NO. 2, 2004
Classications of esophagitis: who needs them?
D Nayar, M Vaezi
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19. 20.
clinical and functional correlates and further validation of the Los Angeles classication. Gut 1999;45:172-80. Pandolno JE, Vakil NB, Kahrilas PJ. Comparison of interand intraobserver consistency for grading of esophagitis by expert and trainee endoscopists. Gastrointest Endosc 2002;56: 639-43. Okamoto K, Iwakiri R, Mon M, Hara M, Oda K, Danjo A, et al. Clinical symptoms in endoscopic reux esophagitis: evaluation in 8031 adult subjects. Dig Dis Sci 2003;48:2237-41. Shibuya S, Fukudo S, Shineha R, Miyazaki S, Miyata G, Sugawara K, et al. High incidence of reux esophagitis observed by routine endoscopic examination after gastric pull-up esophagectomy. World J Surg 2003;27:580-3. Inamori M, Togawa J, Nagase H, Abe Y, Umezawa T, Nakajima A, et al. Clinical characteristics of Japanese reux esophagitis patients as determined by the Los Angeles classication. J Gastroenterol Hepatol 2003;18:172-6. DeFreitas JA, Lima LM, Ranieri JL, Olivieri JC, Fragoso HJ, Chinzon D. Evaluation of efcacy, safety and tolerability of rabeprazole in treatment of acid-peptic diseases [Portuguese]. Arq Gastroenterol 2002;39:60-5. Manabe N, Yoshihara M, Sasaki A, Tanaka S, Haruma K, Chayama K. Clinical characteristics and natural history of patients wit low-grade reux esophagitis. J Gastroenterol Hepatol 2002;17:949-54. Dupas JL, Houcke P, Samoyeau R. Pantoprazole versus lansoprazole in French patients with reux esophagitis. Gastroenterol Clin Biol 2001;25:245-50. Adachi K, Fujishiro H, Katsube T, Yuki M, Ono M, Kawamura A, et al. Predominant nocturnal acid reux in patients with Los Angeles grade C and D reux esophagitis. J Gastroenterol Hepatol 2001;16:1191-6. Sugiura T, Iwakiri K, Kotoyori M, Kobayashi M. Relationship between severity of reux esophagitis according to the Los Angeles classication and esophageal motility. J Gastroenterol 2001;36:226-30. Lukas K, Mandys V, Marecek P, Aschermaim M, Vernerova Z, Smejkalova K. Occurrence of reux esophagitis in patients with chest pain and a normal selective coronary angiogram [Czech]. Cas Lek Cesk 2000;139:497-9. Isbikawa H, Iwakiri K, Suginra T, Kobayashi M. Effect of nifedipine administration (10 rug) on esophageal acid exposure time. J Gastroenterol 2000;35:43-6. Deprez P, Fiasse R. Healing of severe esophagitis improves esophageal peristaltic dysfunction. Dig Dis Sci 1999;44:125-33. Fujimoto K, Iwakiri R, Okamoto K, Oda K, Tanaka A, Tsunada S, et al. Characteristics of gastroesophageal reux disease in Japan: increased prevalence in elderly women. J Gastroenterol 2003;38:(Suppl 15)3-6.
21. Furukawa N, Iwakiri R, Koyama T, Okamoto K, Yoshida T, Kashiwagi Y, et al. Proportion of reux esophagitis in 6010 Japanese adults: prospective evaluation by endoscopy. J Gastroenterol 1999;34:441-4. 22. Soga T, Matsuura M, Kodama Y, Fujita T, Sekimoto I, Nishimura K, et al. Is a proton pump inhibitor necessary for the treatment of lower grade reux esophagitis [comment]? J Gastroenterol 1999;34:540-1. 23. Kusano M, Ino K, Yamada T, Kawamura O, Toki M, Ohwada T, et al. Interobserver and intraobserver variation in endoscopic assessment of GERD using the Los Angeles classication. Gastrointest Endosc 1999;49:700-4. 24. Vcev A, Stimac D, Vceva A, Takac B, Ivandic A, Pezerovic D, et al. Pantoprazole versus omeprazole in the treatment of reux esophagitis. Acta Med Croatica 1999;53:79-82. 25. Watson DI, Foreman D, Devitt PG, Jamieson GG. Preoperative endoscopic grading of esophagitis versus outcome after laparoscopic Nissen fundoplication. Am J Gastroenterol 1997;92:222-5. 26. Csendes A, Maluenda F, Burdiles P, Henriquez A, Quesada MS, Csendes P. Prospective study of esophageal motor abnormalities in patients with gastroesophageal reux disease according to the severity of endoscopic esophagitis. Hepatogastroenterology 1996;43:394-9. 27. Omura N, Aoki T, Kashiwagi H, Hanyu N, Fukuchi Y. An index to predict outcome of surgery for reux esophagitis based on the AFP classication. Surg Today 1995;25: 861-6. 28. Koop H, Schepp W, Dammann HG, Schneider A, Lubmann R, Classen M. Comparative trial of pantoprazole and ranitidine in the treatment of reux esophagitis results of a German multicenter study. J Clin Gastroenterol 1995;20:192-5. 29. Sciume C, Palazzolo M, Toscano P, Cittati V, Bilardo G, Antona A, et al. Endoscopic study in reux esophagitis. Our experience [Italian]. Ann Ital Chir 1989;60:315-8. 30. Mitov F, Protokhristov K, Bakhchevanska P, Apostolov I, Bodurov I. Current aspects of the diagnosis and surgical treatment of reux esophagitis [Russian]. Khirurgiia (Soia) 1989;42:41-4. 31. Tytgat GN. Clinical efcacy of sucralfate in reux esophagitis. Am J Med 1987;83:38-42. 32. Simon B, Mueller P. Comparison of the effect of sucralfate and ranitidine in reux esophagitis. Am J Med 1987;83:43-7. 33. Siewert JR, Ottenjann R, Heilmann K, Neiss A, Dopfer H. Therapy and prevention of reux esophagitis. Results of a multicenter study with cimetidine. I: epidemiology and results of acute therapy [German]. Z Gastroenterol 1986; 24:381-95.
VOLUME 60, NO. 2, 2004
GASTROINTESTINAL ENDOSCOPY
257
S-ar putea să vă placă și
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Pathophysiology of Gastroesophageal Reflux (Gerd)Document1 paginăPathophysiology of Gastroesophageal Reflux (Gerd)Joville DorueloÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5795)
- Presentation PathophysiologyDocument11 paginiPresentation PathophysiologyJade DeopidoÎncă nu există evaluări
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Determination of Acid Neutralizing Capacity of Various Marketed Antacids in NepalDocument40 paginiDetermination of Acid Neutralizing Capacity of Various Marketed Antacids in NepalTshiva AryalÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Candida EsofagitisDocument5 paginiCandida EsofagitisVina IsmawatiÎncă nu există evaluări
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- DR Varsha Atul Shah Senior Consultant Dept of Neonatal and Devt Medicine, SGH Visiting Consultant Dept of Child Devt, KKHDocument47 paginiDR Varsha Atul Shah Senior Consultant Dept of Neonatal and Devt Medicine, SGH Visiting Consultant Dept of Child Devt, KKHJennifer MrjÎncă nu există evaluări
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- NPO GuidelinesDocument12 paginiNPO GuidelinesKi Tae JungÎncă nu există evaluări
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- من جامعة الأردن PDFDocument266 paginiمن جامعة الأردن PDFyousefÎncă nu există evaluări
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Pediatric Cervical Spine DeformityDocument52 paginiPediatric Cervical Spine DeformitySuresh MauryaÎncă nu există evaluări
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- LIVER CHIRROSIS and GERED QUESTION AND ANSWERSDocument10 paginiLIVER CHIRROSIS and GERED QUESTION AND ANSWERSjess_nookieÎncă nu există evaluări
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- Ournal of Utrition Ollege: Journal of Nutrition CollegeDocument11 paginiOurnal of Utrition Ollege: Journal of Nutrition CollegeBunga HalimÎncă nu există evaluări
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Acute Abdomen FinalDocument105 paginiAcute Abdomen FinalAizul AzmiÎncă nu există evaluări
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- BISQDocument4 paginiBISQNanda Asyura RizkyaniÎncă nu există evaluări
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Quiz 3Document7 paginiQuiz 3abezareljvenÎncă nu există evaluări
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- GUJU Product List: WWW - Guju.co - KRDocument10 paginiGUJU Product List: WWW - Guju.co - KRsumanchyÎncă nu există evaluări
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- Gastroesophageal Reflux DiseaseDocument18 paginiGastroesophageal Reflux Diseasebrian3442Încă nu există evaluări
- Gastroesophageal Reflux Disease (Gastroenterology and Hepatology) PDFDocument408 paginiGastroesophageal Reflux Disease (Gastroenterology and Hepatology) PDFaab 1007Încă nu există evaluări
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Berklee Vocal Health For SingersDocument15 paginiBerklee Vocal Health For Singersrosalie_elena89% (9)
- Back To TopDocument2 paginiBack To Topangphone95Încă nu există evaluări
- Lewis CH 42 GIDocument13 paginiLewis CH 42 GIwismommyÎncă nu există evaluări
- Dexlansoprazole Vs Esomeprazole ERGEDocument12 paginiDexlansoprazole Vs Esomeprazole ERGELuis Felipe Gomez AndradeÎncă nu există evaluări
- Pediatrics-Case Presentation: - Sumanga, Juan Cheska Eunice ADocument62 paginiPediatrics-Case Presentation: - Sumanga, Juan Cheska Eunice ALhio Tuguegarao PcbÎncă nu există evaluări
- Drug StudyDocument2 paginiDrug Studycrianne_1180% (5)
- Brett Manning's Singing SuccessDocument18 paginiBrett Manning's Singing Successgabi50% (2)
- Nutrition - Eating and Singing - Musician Health and WellnessDocument4 paginiNutrition - Eating and Singing - Musician Health and WellnessOfori EbenezerÎncă nu există evaluări
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Topic - Diaphragmatic HerniasDocument13 paginiTopic - Diaphragmatic HerniasOlga CerlatÎncă nu există evaluări
- Case Analysis 4 GERDDocument12 paginiCase Analysis 4 GERDCJ100% (1)
- 15 Natural Remedies For Heartburn & Severe Acid RefluxDocument60 pagini15 Natural Remedies For Heartburn & Severe Acid RefluxNISAR_786Încă nu există evaluări
- 18 Amla PittaDocument4 pagini18 Amla PittaAravind BharathiÎncă nu există evaluări
- Why Stomach Acid Is Essential For Our HealthDocument6 paginiWhy Stomach Acid Is Essential For Our HealthGabriel Turlac100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Digestive System KrvaDocument57 paginiDigestive System KrvaFercilyn MarbanÎncă nu există evaluări
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)