Documente Academic
Documente Profesional
Documente Cultură
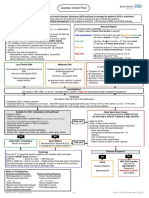
AICD
Încărcat de
anscstDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
AICD
Încărcat de
anscstDrepturi de autor:
Formate disponibile
review
Current Status of the Implantable Cardioverter-Defibrillator*
Michael H. Gollob, MD; and John J. Seger, MD
Clinical trials have established the superiority of the implantable cardioverter-defibrillator (ICD) over antiarrhythmic drug therapy in survivors of sudden cardiac death and in high-risk patients with coronary artery disease. The ICD has evolved to overcome the limitation of earlier devices that required thoracotomy for implantation and were fraught with inappropriate shock delivery. Current ICDs are implanted in a similar manner to cardiac pacemakers and incorporate sophisticated rhythm-discrimination algorithms to prevent inappropriate therapy. Managing the patient with an ICD requires an understanding of the multiprogrammable features of modern devices. Drug interactions and potential sources of electromagnetic interference may adversely affect ICD function. Driving restrictions may be necessary under certain conditions. The cost-effectiveness of ICD therapy appears favorable, given the marked survival benefit seen in randomized trials relative to antiarrhythmic drug treatment. The growing number of ICD recipients necessitates an understanding of the specialized features of the modern ICD and the role of device therapy in clinical practice. (CHEST 2001; 119:1210 1221)
Key words: implantable cardioverter-defibrillator; sudden cardiac death Abbreviations: ATP antitachycardia pacing; AVID Antiarrhythmics Versus Implantable Defibrillator Trial; CABG-PATCH Coronary Artery Bypass Graft-Implantable Cardioverter-Defibrillator Study; CIDS Canadian Implantable Defibrillator Study; DFT defibrillation threshold; EGM electrogram; EF ejection fraction; EP electrophysiologic; ICD implantable cardioverter-defibrillator; LV left ventricular; MADIT Multicenter Automatic Defibrillator Trial; MI myocardial infarction; NSVT nonsustained ventricular tachycardia; NYHA New York Heart Association; PG pulse generator; SCD sudden cardiac death; VF ventricular fibrillation; VT ventricular tachycardia
n the I (SCD)United Statesanalone, sudden cardiac death accounts for estimated 350,000 lives lost annually.1 The majority of these events occur outside the hospital setting and are associated with consequential delays in implementing external defibrillation. The ability of the implantable cardioverterdefibrillator (ICD) to provide therapy within 5 to 15 s of arrhythmia detection allows for defibrillation success rates approaching 100%. Numerous clinical trials have established the superiority of the ICD over drug therapy in reducing mortality rates for survivors of cardiac arrest or
*From the Section of Cardiology (Dr. Gollob), Baylor College of Medicine, Houston, TX; Division of Cardiology (Dr. Seger), Texas Heart Institute, Houston, TX. Manuscript received June 20, 2000; revision accepted August 3, 2000. Correspondence to: Michael H. Gollob, MD, Section of Cardiology, RM 507D, Baylor College of Medicine, One Baylor Plaza, Houston, TX 77030; e-mail: mgollob@bcm.tmc.edu
1210
patients at high risk for SCD.27 On the basis of these studies, the ICD is now recommended as the treatment of choice in survivors of SCD and in patients with symptomatic, sustained ventricular arrhythmias.8 Current ICD implantation rates exceed 30,000 per year and will continue to grow as clinical indications evolve.9 The majority of physicians will be involved in the care of ICD recipients. In this review, we provide the generalist with an overview of ICD function and the management of ICD patients in clinical practice. The Modern ICD Early Beginnings The first human ICD implant occurred in 1980.10 Approval for general use was granted by the US Food and Drug Administration in 1985. These early devices consisted of a large pulse generator (PG)
Review
(Fig 1) and patch electrodes for defibrillation placed directly on the heart or pericardium. Epicardial screw-in leads also were placed for rate sensing (Fig 2). Implant procedures required general anesthesia, thoracotomy, were associated with longer hospital stays, and had a perioperative mortality rate in the range of 4%.11 In addition to the limitations imposed by size, early devices offered few options for patient-specific programming. The ICD was ordered by the physician specifying a detection heart rate and delivered by the manufacturer to perform defibrillation should the patients ventricular rate exceed this value. No programming options existed for changing the prespecified detection rate. Therefore, should an antiarrhythmic agent be required and have the effect of slowing ventricular tachycardia (VT) below the preset detection rate, ICD therapy would not be delivered. A further limitation of early devices was the inability to discriminate rapid ventricular rhythms of supraventricular origin from ventricular-based rhythms, leading to a high incidence of inappropriate shocks. Analysis of stored electrograms (EGMs) in later device models confirmed a rate of inappropriate shocks in the range of 25 to 40%.1215 Advances in ICD lead systems and defibrillation waveforms allowed for successful transvenous, pectoral ICD implants (Fig 3). ICD systems are now implanted in a manner similar to cardiac pacemakers and without the need for general anesthesia. Perioperative mortality is 1%.16 Complications such as infection, pneumothorax, pericardial tamponade, and pocket hematoma occur at rates similar to those seen with pacemaker implantation ( 3%).17,18 As ICD system hardware has evolved, so too has the internal circuitry responsible for the specialized features of the device. The modern ICD may now be programmed to detect several specified tachycardia
Figure 2. An early ICD system showing epicardial patch electrodes used for defibrillation and epicardial screw-in leads for rate sensing. The large PG was placed in the abdominal wall.
zones, with the alternative of less aggressive antitachycardia pacing (ATP) therapy for slower, hemodynamically stable VT. Further, sophisticated rhythm-discrimination algorithms now exist to discern VT from rapid supraventricular arrhythmias. This has resulted in the decline of the inappropriate shock rate to 5%.19,20 ICD Rhythm Discrimination: Rapid Supraventricular Tachycardia vs Ventricular Arrhythmia Current ICDs allow for the programming of at least three tachyarrhythmia detection zones. The highest rate zone is referred to as the ventricular fibrillation (VF) zone. In the VF zone, the risk of sudden hemodynamic collapse mandates 100% sensitivity in detection. This is achieved by employing an X/Y algorithm that requires a certain proportion (eg, 12/16) of R-R intervals to be within the programmed zone for detection. Additional slower VT zones may be programmed for detection of more hemodynamically stable ventricular arrhythmias. In contrast to the more rapid rate of the VF zone, rate criterion as the sole method for detection in VT zones results in a significant number of inappropriate shocks.
CHEST / 119 / 4 / APRIL, 2001
Figure 1. An early ICD (weight, 290 gm) (left) and a current ICD model (39 gm) (right).
1211
Figure 3. Evolving ICD systems. Left, A: the earliest ICD system, illustrating the epicardial patch electrodes used for defibrillation and epicardial leads used for rate sensing. This system required thoracotomy for implantation. Middle, B: the development of leads integrating both sensing and shocking elements allowed for nonthoracotomy implants. PG size remained too large for routine pectoral implantation. Right, C: the modern ICD utilizes the PG as an active can in the defibrillation circuit and is of sufficiently small size for pectoral implantation.
Most unnecessary therapies are due to sinus tachycardia or atrial fibrillation with ventricular rates overlapping with programmed VT detection zones.11,2124 Therefore, rhythm-discrimination algorithms have been developed to prevent inappropriate therapy and to increase specificity for VT within a programmed VT zone. Unfortunately, increasing specificity is at the expense of diminishing sensitivity. Thus, all rhythm-discrimination algorithms are programmable only for the presumed more hemodynamically stable, slower VT zones. The two most commonly employed rhythm-discrimination algorithms utilize onset and stability reference criteria. The onset algorithm monitors for abrupt changes in the R-R interval from beat to beat. In the scenario of sudden-onset tachycardia within a VT zone, should the R-R interval of the first two beats of tachycardia decrease (reflecting an increased heart rate) by more than the programmed onset criterion (eg, 40 ms), then the tachycardia is considered to be ventricular in origin. The onset algorithm is intended to prevent inappropriate therapy for sinus tachycardia rates that progress into the slow VT zone. Thus, a gradual change in R-R interval entering a VT zone, as is the case in sinus tachycardia, would not satisfy onset criteria and would be considered supraventricular in origin, averting therapy. The limitation of this feature is the potential failure to detect VT that arises during exercise and lacks abrupt onset. The onset criterion has been reported to underdetect 5 to 13% of VTs.2527 Stability refers to the R-R interval variability of the detected tachycardia. Ventricular rates due to atrial fibrillation would be expected to show a wide range of R-R intervals, as opposed to monomorphic
1212
VT. A programmable R-R stability algorithm would detect as VT any rhythm with R-R intervals varying less than the programmed value, for example, 40 ms. A potential difficulty is polymorphic VT, although this rhythm tends to be faster and detected within the VF zone. The availability of dual-chamber ICD systems with the capability of A-V sequential pacing and sensing has allowed the design of newer enhancementdetection algorithms. The sensing of atrial EGMs permits comparison of atrial and ventricular rates. Rapid tachycardias with an atrial rate more than the ventricular rate would appropriately be detected as supraventricular in origin. Similarly, dissociation of atrial and ventricular rates during tachycardia may be recognized, accurately identifying the rhythm as VT. The assessment of ventricular EGMs has been incorporated as another method to differentiate VTs from supraventricular tachycardias. The EGM width criterion is based on the assumption that ventricularbased rhythms will have a wider EGM compared to EGMs derived from normal AV conduction. While the addition of this criterion to onset and stability significantly lowers inappropriate shocks, it is known that EGM width can change significantly at high sinus rates and over time.28 Morphology discrimination (MD; Ventritex; Sunnyvale, CA) is a novel algorithm whereby the device stores a template of the baseline (sinus) ventricular EGM morphology (Fig 4). During tachycardia detection, each complex is compared to the template, and the algorithm determines the percent match. Should the tachyarrhythmia EGM complex be less than a programmable percent match, therapy is initiated. Limitations of
Review
therapy is programmable and is followed as needed until an episode is terminated. These programmable options include ATP, low-energy synchronized cardioversion, and defibrillation. The objective of ATP is to terminate monomorphic VT promptly with little discomfort to the patient. Delivery of ATP is applied in successive paced beats at a rate faster than the tachycardia cycle length. ATP therapy successfully terminates approximately 90% of episodes of spontaneous VT.29 In addition, the use of this therapy is associated with a statistically significant 36 to 28% reduction of first ICD shocks over a 2-year follow-up period.30 The risk of this therapy is the potential for accelerating VT to VF, which may occur in up to 10% of attempts.31 Therefore, tiered therapy must always include the programming of back-up defibrillation. Diagnostic Storage Early ICDs stored little information, noting only the number of device discharges. Current devices store and display extensive data. An updated therapy history is provided on each interrogation. A large number of episodes may be stored and their details viewed individually. Specifics regarding the date/ time, therapy delivered, detection zone and criteria satisfied, and total length of the episode are displayed. Intracardiac EGMs of episodes requiring therapy are retrievable, including the onset segment. Marker annotations indicating R-R intervals and the devices interpretation of the ongoing rhythm are displayed. Simultaneous EGMs from atrial and ventricular leads may be viewed, assisting the physician in determining the appropriateness of the applied therapy (Fig 5).
Figure 4. Morphology discrimination (Ventritex). A stored ventricular EGM is compared to the detected ventricular EGM with alignment of the three largest contiguous peaks. A morphology score or percent match is calculated. The tachycardia is assumed to be ventricular in origin if the percent match is less than a programmable value or if the initial complex alignment is not possible.
EGM morphology exist for patients with underlying bundle branch block or rate-related bundle branch block. Most electrophysiologists will utilize rhythm-discrimination algorithms individually or in combination, depending on the clinical history of the patient. Although these features increase detection specificity and lower inappropriate shock rates to 5%, underdetection and inhibition of therapy for true VT may occur. A programmable safety feature known as sustained rate duration can apply therapy if the heart rate remains in a VT zone over a programmed duration of time, thereby returning sensitivity for true VT to near 100%.19,20,26 ICD Therapy All ICDs use electrical defibrillation as the only therapeutic option for heart rates detected in the VF zone. Multiple or tiered therapeutic options are available for VT detection zones. A sequence of
Clinical Trials of the ICD Secondary Prevention of SCD The impact of the ICD on survival in patients with a history of life-threatening arrhythmias has now been assessed in three randomized trials (Table 1). The Antiarrhythmics Versus Implantable Defibrillator Trial (AVID)2 evaluated the efficacy of the ICD in reducing total mortality in patients with an ejection fraction (EF) 40% and a history of SCD or sustained VT with syncope or hemodynamic compromise. In the control arm of the study, 90% of patients received empiric amiodarone, and the remainder received Holter-guided sotalol. This trial was terminated early due to a clear benefit in the ICD-treated group. At follow-up after 3 years, survival rates were 75% for the ICD group vs 61% for the antiarrhythmic group. Although -blocker use
CHEST / 119 / 4 / APRIL, 2001
1213
Figure 5. Intracardiac EGMs. Top: the panel illustrates the successful termination of VT by a single burst of ATP. Middle: the panel demonstrates the electrical cardioversion of VT. Bottom: the panel indicates a rapid supraventricular tachycardia with ventricular rates detected in a VT zone. Rhythmdiscrimination algorithms correctly identified this as atrial fibrillation/flutter (AF) and prevented inappropriate therapy. AR atrial sensed beats during pacing refractory periods; AS atrial sense; CD charge delivered; TD tachycardia detected; TP antitachycardia paced beat; TS tachycardia sense; VR ventricular sensed beats during pacing refractory periods; VS ventricular sense VP ventricular paced beat.
was more prevalent in the ICD group, adjusting for this imbalance did not alter the mortality rate reduction attributable to the ICD. The Cardiac Arrest Study-Hamburg Trial4 randomly assigned survivors of cardiac arrest to ICD or to treatment with propafenone, metoprolol, or amiodarone. The propafenone arm was withdrawn early
1214
due to an observed excess mortality rate. The allcause mortality rate was 12.1% in the ICD arm vs 19.6% in the combined arms of amiodarone and metoprolol at follow-up after 2 years, a statistically significant reduction. Interestingly, no difference was observed between the amiodarone and metoprolol arms.
Review
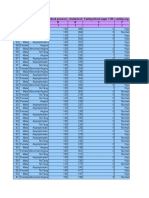
Table 1Randomized Clinical Trials of the ICD*
Trial Primary prevention MADIT Patient Population Prior MI, LV EF 35%, NSVT, and inducible VT not suppressible with IV procainamide Coronary artery bypass grafting, LV EF 35%, and positive signal-averaged ECG Coronary artery disease, LV EF 40%, nonsustained VT, and inducible VT Control Medical therapy Result Significant reduction in total mortality in the ICD group No difference in total mortality Significant reduction in SCD and/or resuscitated cardiac arrest in the ICD group Ongoing Ongoing Ongoing
CABG-PATCH MUSTT
Medical therapy Medical therapy or EP-guided antiarrhythmic therapy Medical therapy Placebo or amiodarone Medical therapy
MADIT II SCD-HEFT DINAMIT
DEFINITE
Prior MI and LV EF 30% without arrhythmia entry criteria NYHA class II or III congestive heart failure and LV EF 35% Acute MI ( 30 d), LV EF 35%, and depressed heart rate variability or mean 24-h heart rate 80 beats/min Nonischemic cardiomyopathy, LV EF 35%, and nonsustained VT or 10 PVCs/h
-blocker and conventional heart failure therapy Amiodarone or sotalol Propafenone or metoprolol or amiodarone Amiodarone
Ongoing
Secondary Prevention AVID CASH
LV EF 40% and cardiac arrest, syncopal VT, or symptomatic sustained VT Resuscitated cardiac arrest
Significant reduction in total mortality in the ICD group Significant reduction in total mortality in the ICD group Nonsignificant reduction in total mortality in the ICD group
CIDS
Resuscitated cardiac arrest, syncopal VT, or symptomatic sustained VT with LV EF 35% or syncope and inducible VT
*PVC premature ventricular contraction; MUSTT Multicenter Unsustained Trial; SCD-HEFT Sudden Cardiac Death in Heart Failure Trial; DINAMIT Defibrillator in Acute Myocardial Infarction Trial; DEFINITE Defibrillator in Nonischemic Cardiomyopathy Treatment Evaluation; CASH Cardiac Arrest StudyHamburg.
The Canadian Implantable Defibrillator Study (CIDS) randomized a patient population, which was similar to the one in the AVID trial, to an ICD or to empiric amiodarone. At 5 years, a trend in favor of reduced all-cause mortality in the ICD treatment group was present, although this was not statistically significant.3 The trial design of CIDS may have lessened the impact of ICD therapy in this study. In contrast to the AVID trial, this study did not mandate a poor EF for all patients enrolled. Included in enrollment were patients with syncope without spontaneous VT who subsequently underwent electrophysiologic (EP) study. Evidence from an EP study of inducible VT satisfied enrollment criteria, without regard to EF. This is reflected in the difference between the average EF for the CIDS patient population (34%) and that for the AVID population (27%). The difference in EF between the patient populations of the CIDS and the AVID trial also extends to New York Heart Association (NYHA) heart failure class, a known correlate to the risk of SCD.32 In CIDS, 50% of patients were of asymptomatic heart failure status, whereas in the AVID
trial 70% of patients had NYHA class II-III heart failure. Thus, the results of CIDS suggest that patients with symptomatic VT and milder degrees of left ventricular (LV) dysfunction (EF, 35%) may be adequately treated with amiodarone, whereas patients experiencing episodes of VT who have poorer EF values and NYHA status are best treated with ICD implantation. Indeed, a subgroup analysis of CIDS indicates a much stronger trend to improved survival in ICD-treated patients with EFs 35%. Presently, treatment with an ICD is a class I indication for secondary prevention in survivors of cardiac arrest not due to a reversible cause, for patients with syncope of unknown etiology and inducible VT/VF, and in patients with spontaneous, sustained VT (Table 2).8 Primary Prevention of SCD Since only 2 to 30% of persons who have cardiac arrest survive, a strong impetus to identify high-risk patients for the primary prevention of SCD exCHEST / 119 / 4 / APRIL, 2001
1215
Table 2Clinical Indication for ICD Implantation*
Class I Indications for ICD therapy Cardiac arrest due to VF or VT, not due to a transient or reversible cause Spontaneous sustained VT Syncope of undetermined origin with clinically relevant, hemodynamically significant sustained VT or VF induced at EP study when drug therapy is ineffective, not tolerated, or not preferred NSVT with coronary disease, prior MI, LV dysfunction, and inducible VF or sustained VT and EP study that is not suppressible by a class I antiarrhythmic drug None Cardiac arrest presumed to be due to VF when EP testing is precluded by other medical conditions Severe symptoms attributable to sustained VTs while awaiting cardiac transplantation Familial or inherited condition with a high risk for life-threatening VTs such as long QT syndrome or hypertrophic cardiomyopathy Nonsustained VT with coronary artery disease, prior MI, and LV dysfunction, and inducible sustained VT or VF at EP study Recurrent syncope with undetermined etiology in the presence of ventricular dysfunction and inducible ventricular arrhythmias at EP study when other causes of syncope have been excluded Syncope of undetermined cause in a patient without inducible ventricular tachyarrhythmias Incessant VT or VF VF or VT resulting from arrhythmias amenable to surgical or catheter ablation; for example, atrial arrhythmias associated with the Wolff-Parkinson-White syndrome, right ventricular outflow tract VT, idiopathic LV tachycardia, or fascicular VT VTs due to a transient or reversible disorder (eg, AMI, electrolyte imbalance, drugs, or trauma) Significant psychiatric illnesses that may be aggravated by device implantation or may preclude systematic follow-up Terminal illnesses with projected life expectancy 6 mo Patients with coronary artery disease with LV dysfunction and prolonged QRS duration in the absence of spontaneous or inducible sustained or NSVT who are undergoing coronary bypass surgery NYHA class IV drug-refractory congestive heart failure in patients who are not candidates for cardiac transplantation acute myocardial infarction. Adapted from American Heart Association/American College of Cardiology guidelines.8
IIa IIb
III
*AMI
ists.3335 EP testing is a well-established procedure that has been shown to predict the risk of SCD in patients with coronary artery disease.36,37 This test has played a key role in clinical trial designs for primary prevention. The Multicenter Automatic Defibrillator Trial (MADIT)5 was the first prospective, randomized trial assessing the value of the ICD. Patients with prior myocardial infarctions (MIs), LV EFs 35%, evidence of documented nonsustained VT (NSVT) and inducible VT on EP study that was not suppressed by IV procainamide randomly received an ICD or conventional therapy. A statistically significant difference in the total mortality rate was observed, 15% in the ICD group and 39% in the conventional therapy group over an average follow-up period of 2.5 years. Although a striking benefit for the ICD was present, the trial was criticized for the lack of a unified approach to drug therapy in the conventional treatment group. At last patient contact, only 5% of patients in the conventional group were receiving -blocker therapy vs 27% in the ICD group. The proportion of participants in the conventional group receiving therapy with angiotensin-converting enzyme inhibitors was 51%, and the proportion receiving amiodarone was 45%.5 The recently completed Multicenter Unsustained Tachycardia Trial6 randomized a patient population
1216
similar to that in the MADIT. Patients with inducible VT received medical therapy alone (excluding antiarrhymic drugs) or an EP-guided approach. Patients in the EP-guided group whose conditions were suppressible by antiarrhythmic drug therapy were maintained on regimens with their respective drugs. Patients with VT not suppressible by antiarrhythmic drug therapy received an ICD. At a median follow-up of 39 months, a statistically significant benefit was evident with respect to the primary end point of SCD or resuscitated cardiac arrest in the EP-guided group (25%) compared to that in the medical therapy group (32%). Further analyses indicated that the benefit seen with the EP-guided approach was due solely to the ICD group (p 0.001). Patients receiving EP-guided antiarrhythmic drug therapy did not show improved outcomes compared to medically treated patients not receiving antiarrhythmic drug therapy. Patients enrolled in this trial who were not inducible at EP study, and therefore were considered to be at low risk for SCD, were followed-up in a registry. Interestingly, this patient population had an unexpectedly high mortality rate of 24% at follow-up.6 The Coronary Artery Bypass Graft-Implantable Cardioverter-Defibrillator Study (CABG-PATCH) study randomized patients prior to coronary surgery with EFs 35% and positive signal-averaged ECGs to either the ICD group or the control group. No
Review
difference in overall mortality was observed.7 The study did not require NSVT or inducible VT for trial enrollment. It is suggested that patients with a similar degree of LV dysfunction but without inducible VT may be at a lower risk for SCD.38,39 In addition, revascularization may have decreased the risk for ischemia-induced arrhythmias in this patient population. These factors may help to explain the much lower mortality rate in the CABG-PATCH control arm (18%) than in the MADIT control group (39%). The ongoing Sudden Cardiac Death in Heart Failure Trial will present the most stringent control intervention thus far vs the ICD. Patients with symptomatic (ie, NYHA class II-III) ischemic or nonischemic cardiomyopathy and EFs 35% are being randomized to treatment with ICD, amiodarone, or placebo. A key component to this trial is the strong encouragement for -blocker use, targeting 70% of the patient population. The relevance of this is highlighted by recent trials40,41 indicating a significant reduction in all-cause and sudden death mortality in congestive heart failure patients randomized to treatment with -blockers. Furthermore, the combination of -blocker and amiodarone has been suggested in post hoc analyses to have a significant impact on reducing the number of deaths from arrhythmia.42 In summary, the current evidence suggests that patients with a history of cardiac arrest or sustained VT and syncope are best treated with an ICD. Patients with EFs 35%, coronary artery disease, and NSVT should be referred for EP study. If inducible, they should receive an ICD.
problems may be evident on analysis of stored EGMs in which nonphysiologic R-R intervals (ie, those of 150 ms) may be observed. Lead problems should be suspected on device interrogation when marked variation of R-wave sensing, pacing thresholds, and impedance measurements exist. Occasionally, having the patient perform physical maneuvers such as straining or arm movements may reproduce electrical chatter while observing ICD telemetry. An overpenetrated chest radiograph may localize a lead fracture. Issues related to lead failure or to loose connections require surgical intervention. Acute management of a patient with inappropriate, incessant shocks not caused by a ventricular arrhythmia should include placing a magnet over the device. This maneuver will disable therapy delivery but will have no effect on required pacing. The inability of therapy to convert an arrhythmia may have dire consequences. Lead failure or malposition may be a culprit, resulting in insufficient energy delivery. Altered tissue substrate may render ATP unsuccessful due to failure to adequately capture. Defibrillation thresholds (DFTs) may be increased due to amiodarone initiation or to severe electrolyte/acid-base abnormalities.46 Increasing the programmed shock energy level may suffice, but a thorough device evaluation is required. Managing an acute ventricular arrhythmia not successfully terminated by ICD therapy should not differ from the approach used in patients without ICDs. An ICD discharge during patient contact by a resuscitating team member will not harm or pose a risk to the individual. Antiarrhythmic Drug-ICD Interactions
Managing Patients With ICDs Troubleshooting Inappropriate ICD Function The first issue in assessing a patient with a recent defibrillation discharge is to determine whether therapy was appropriate. Despite the sophisticated rhythm-discrimination algorithms that are in current use, rapid atrial fibrillation remains the most common cause of inappropriate shocks.21,22 The main reason for this is atrial fibrillation ventricular rates that meet VF zone criteria in which detection is based on the ventricular rate alone and the programming of rhythm-discrimination algorithms is not permitted. Preventive options include increasing the VF detection rate, adding AV nodal blocking agents, or considering AV nodal ablation. Inappropriate therapy also may result from the sensing of electrical chatter. Electrical chatter develops in the presence of lead fractures or insulation breaks, or may result from a loose connection to the PG.43 45 These
ICD implantation may obviate the need for longterm antiarrhythmic drug therapy in a large number of patients. However, frequent shocks due to atrial tachyarrhythmias and/or ventricular arrhythmias will require the initiation of drug therapy in the management of certain patients. In addition to the possibility of decreasing VT rates out of programmed detection zones, therapy with antiarrhythmic drugs also may cause proarrhythmia. An increase in ICD therapies correlating with recent initiation of an antiarrhythmic agent should raise this suspicion. The effect of antiarrhythmic drugs on the minimum energy requirement for successful defibrillation, or DFT, requires special attention. At ICD implantation, the DFT is determined and a 10-J safety margin typically is added to ensure defibrillation efficacy. Some antiarrhythmic agents may alter the DFT as a result of their EP properties (Table 3). In general, class IA antiarrhythmic drugs, such as quinidine and procainamide, appear to have little
CHEST / 119 / 4 / APRIL, 2001
1217
Table 3Effects of Antiarrhythmic Drugs on DFT*
Drug Class IA Drug Quinidine Disopyramide Procainamide Lidocaine Phenytoin Mexiletine Flecainide Propafenone Propranolol Timolol Amiodarone Sotalol Bretylium Effect on DFT 7 7 7 1 1 1,7 1 2 1 7 1 2 7
IB
IC II III
*Based on Vaughn-Williams classification.
effect on the DFT at therapeutic doses.46 The short-term administration of class IB agents, including lidocaine, phenytoin, and mexiletine, has been shown to increase the DFT.47 The class III agents amiodarone and sotalol are commonly used for the maintenance of sinus rhythm in patients with paroxysmal atrial fibrillation. Their effects on the DFT are disparate. Amiodarone has been shown in several studies to elevate the DFT, while sotalol consistently has no effect or lowers the DFT.46,48 The addition of an antiarrhythmic agent to the therapy of ICD patients may have a significant effect on the efficacy of ICD therapy. It is necessary, therefore, to review programmed tachycardia zones and to consider repeat DFT testing after drug loading. Electromagnetic Interference Electromagnetic interference may cause an ICD to falsely detect tachycardia and to deliver inappropriate therapy. In the home environment, there have been no reports of normally functioning domestic appliances causing any inappropriate shocks in modern ICDs. Microwave ovens, portable telephones, or personal computers have not been linked to interference in current ICD systems. Inappropriate shocks from electric razors have been reported rarely.49 Hand-held radiofrequency remote controls may produce inappropriate sensing when held in close vicinity to the ICD device but have not been shown to adversely affect device function when held 10 cm from the chest wall.50 Patients should be advised to avoid the strong magnetic fields of electronic theft surveillance systems or to walk through them without pausing. Similarly, patients should present their device identification card to airport security personnel and walk briskly through the security gate. The ICD device
1218
may trigger the alarm. In these instances, brief passage of a hand-held metal detector over the device is innocuous; however, prolonged exposure (ie, 30 s) should be avoided as this may inactivate programmed therapies in some devices. Caution is needed in the use of cellular telephones. When used, the phone should be held on the side opposite to the device. The avoidance of close contact with the PG and lead system is recommended, and, therefore, phones should not be placed in nearby pockets.5153 Patients with occupational exposures to large magnetic fields may have their work environment assessed by an ICD company representative for the possibility of inappropriate device sensing. In the hospital setting, MRI imaging is generally contraindicated. The use of electrocautery in surgery may cause electrical chatter and oversensing. The device is best turned off in this setting with appropriate monitoring and an external defibrillator nearby. In addition, electrocautery should be avoided in close proximity to the device to prevent the risk of damage to internal circuitry. ICDs and Driving The privilege of driving is a quality-of-life issue for ICD recipients. Although the presence of an ICD will terminate sudden, malignant ventricular arrhythmias, loss of consciousness may not be prevented in up to 15% of episodes.54 Current data suggest that the risk of fatal motor vehicle accidents involving ICD recipients is low. European data indicate that only 1.5 to 3.4% of road accidents are attributed to sudden driver incapacity.55 A study observing the driving history of 291 ICD patients over an average of 3 years noted only 11 traffic accidents. Of these accidents, no fatalities occurred and there were no accidents associated with driver syncope or defibrillation therapy. In the remaining patient cohort, 5% of patients received ICD therapy while driving, which was not associated with syncope or accident.56 At present, most US states have no specific laws regarding driving for ICD patients. A consensus statement providing recommendations has been published by the North American Society of Pacing and Electrophysiology/American Heart Association.57 These guidelines recommend against noncommercial driving for a period of 6 months following ICD implantation for survivors of lifethreatening arrhythmias. Similarly, following successful ICD therapy for a ventricular arrhythmia, the patient should refrain from driving for 6 months. The basis for these time frames stems from data indicating that the risk of recurrent arrhythmia is greatest
Review
soon after an index event and decreases to 0.7% per month after the seventh month.58 It is recommended that aircraft piloting and commercial driving be prohibited in patients receiving an ICD. Similar precautions should be followed for patients involved in the handling of heavy machinery.
Future Developments Future advances in ICD technology are motivated by the demographics of an aging population and by the success of various medical interventions in improving the survival of cardiac patients prone to SCD. A goal of newer-generation ICD devices will be to provide intervention prior to arrhythmia onset, avoiding discomforting cardioversion or defibrillation therapy. ECG or physiologic parameters known to increase ventricular arrhythmia risk, such as longshort R-R intervals, T-wave alternans, heart rate variability, or hemodynamic instability, may be intervened on by novel ICD therapies. Such programmable therapies may include pacing to avoid long-short coupling, intermittent antiarrhythmic drug infusion, or multisite pacing to improve hemodynamics.64 68 Further advances in device technology will undoubtedly expand the role of the ICD in the primary and secondary prevention of SCD. References
1 Gillum RF. Sudden coronary death in the United States: 1980 1985. Circulation 1989; 79:756 765 2 The Antiarrhythmics versus Implantable Defibrillators (AVID) Investigators. A comparison of antiarrhythmic drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. N Engl J Med 1997; 337:1576 1583 3 Connolly SJ, Gent M, Roberts RS, et al. Canadian Implantable Defibrillator Study (CIDS): a randomized study of the implantable cardioverter defibrillator against amiodarone. Circulation 2000; 101:12971302 4 Kuck KH, Cappato R, Siebels J, et al. Randomized comparison of antiarrhythmic drug therapy with implantable defibrillator in patients resuscitated from cardiac arrest: the Cardiac Arrest Study Hamburg (CASH). Circulation 2000; 102:748 754 5 Moss AJ, Hall WJ, Cannom DS, et al. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. N Engl J Med 1996; 335:19331940 6 Buxton AE, Lee KL, Fisher JD, et al. A randomized study of the prevention of sudden cardiac death in patients with coronary artery disease. N Engl J Med 1999; 341:18821890 7 Bigger JT Jr. Prophylactic use of implanted cardiac defibrillators in patients at high risk for ventricular arrhythmias after coronary artery bypass graft surgery: Coronary Bypass Graft (CABG) Patch Trial Investigators. N Engl J Med 1997; 337:1569 1575 8 Gregoratos G, Cheitlin MD, Conill A, et al. ACC/AHA Guidelines for Implantation of Cardiac Pacemakers, and Antiarrhythmic devices: executive summary; a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Pacemaker Implantation). Circulation 1998; 97:13251335 9 Wilbur SL, Marchlinski FE. Implantable cardioverter-defibrillator follow-up. Cardiol Rev 1999; 7:176 190 10 Mirowski M, Mower MM, Reid PR. The automatic implantable defibrillator. Am Heart J 1980; 100:1089 1092 11 PCD Investigator Group. Clinical outcome of patients with malignant ventricular tachyarrhythmias and a multiprogramCHEST / 119 / 4 / APRIL, 2001
Cost-Effectiveness Advancements in ICD technology leading to nonthoracotomy, pectoral implantation have resulted in the vast majority of procedures being undertaken in the EP laboratory. This transition from the operating room has significantly reduced the cost associated with ICD implantation. A recent cost-analysis for ICD procedures compared the expense of procedures in an operating-room setting vs an EP laboratory.59 Total costs were significantly less in the EP laboratory ($4,541) than in the operating room ($9,431). This lower cost was attributable to lower physician fees, hospital charges, and the shorter length of postprocedural convalescence. Present data analyzing the cost-effectiveness of the ICD relative to conventional medical therapy are obscured given the rapid technological advances of the ICD. Owens et al60 provided an economic model estimating that a 30% reduction in mortality by the ICD relative to amiodarone would satisfy the current standards of cost-effectiveness ( $50,000 per lifeyear gained). This estimate compares favorably to the observed risk reduction of 31% at 3 years in the AVID trial and the 59% risk reduction at 2 years in MADIT. Prior clinical information regarding the cost-effectiveness of ICDs has been limited by small patient numbers and trial design. 61,62 Completion of MADIT in 1996 has allowed for an adequate duration of patient follow-up to assess the costs accumulated by each treatment group.63 The expenses of recurrent hospitalizations, physician visits, medications, laboratory tests, and procedures were analyzed. In view of the significant mortality reduction in MADIT, the resulting cost-effectiveness ratio was $27,000 per life-year gained. In patients who received nonthoracotomy procedures, this ratio was reduced to $23,000 per life-year gained. Advances in ICD technology will reduce the cost of this therapeutic strategy further. Improved batteries are increasing device longevity, better diagnostic features avoid inpatient or ambulatory Holter monitoring, and dual-chamber pacing capabilities prevent the need for separate pacemaker implantation when required.
1219
12
13 14
15 16 17 18 19
20
21 22
23
24 25
26
27 28
29
mable implantable cardioverter-defibrillator implanted with or without thoracotomy: an international multicenter study. J Am Coll Cardiol 1994; 23:15211530 Grimm RF, Flores BF, Marchlinski FE. Electrocardiographically documented unnecessary, spontaneous shocks in 241 patients with implantable cardioverter defibrillators. Pacing Clin Electrophysiol 1992; 15:16671673 Neuzner J, Pitschner HF, Schleper M. Programmable VT detection enhancements in implantable cardioverter defibrillator therapy. Pacing Clin Electrophysiol 1995; 18:539 547 Marchlinski FE, Callans DJ, Gottlieb CD, et al. Benefits and lessons learned from stored electrogram information in implantable defibrillators. J Cardiovasc Electrophysiol 1996; 6:832 851 Reiter MJ, Mann DE. Sensing and tachyarrhythmia detection problems in implantable cardioverter defibrillators. J Cardiovasc Electrophysiol 1996; 7:542558 Bardy GH, Yee R, Jung W. Multicenter experience with a pectoral unipolar implantable cardioverter-defibrillator. J Am Coll Cardiol 1996; 28:400 410 Rosenqvist M, Beyer T, Block M, et al. Adverse events with transvenous implantable cardioverter-defibrillators: a prospective multicenter study. Circulation 1998; 98:663 670 Smith PN, Vidaillet HJ, Hayes JJ, et al. Infections in nonthoracotomy implantable cardioverter-defibrillators:can these be prevented? Pacing Clin Electrophysiol 1998; 21:42 45 Schaumann A, von zur Muhlen F, Gonska BD, et al. Enhanced detection criteria in implantable cardioverter-defibrillators to avoid inappropriate therapy. Am J Cardiol 1996; 78:4250 Trappe HJ, Achtelik M, Pfitzner P, et al. Single-chamber versus dual-chamber implantable cardioverter defibrillators: indications and clinical results. Am J Cardiol 1999; 83(suppl): 8D16D Schaumann A. Managing atrial tachyarrhythmias in patients with implantable cardioverter defibrillators. Am J Cardiol 1999; 83(suppl):214D217D Anderson MH, Murgatroyd FD, Hnatkova K, et al. Performance of basic ventricular tachycardia detection algorithms in implantable cardioverter defibrillators: implication for device programming. Pacing Clin Electrophysiol 1997; 20:2975 2983 Wood MA, Stambler BS, Damiano RJ, et al. Lessons learned from data logging in a multicenter clinical trial using a late-generation implantable cardioverter-defibrillator: the Guardian ATP 4210 Multicenter Investigators Group. J Am Coll Cardiol 1994; 24:16921699 Nunain SO, Roelke M, Trouton T, et al. Limitations and late complications of third-generation automatic cardioverter-defibrillators. Circulation 1995; 91:2204 2213 Swerdlow CD, Ahern T, Chen PS, et al. Underdetection of ventricular tachycardia by algorithms to enhance specificity in a tiered-therapy cardioverter-defibrillator. J Am Coll Cardiol 1994; 24:416 424 Weber M, Bocker D, Bansch D, et al. Efficacy and safety of the initial use of stability and onset criteria in implantable cardioverter defibrillators. J Cardiovasc Electrophysiol 1999; 10:145153 Brugada J. Is appropriate therapy a resolved issue with current implantable cardioverter defibrillators? Am J Cardiol 1999; 83(suppl):40D 44D Barold HS, Newby KH, Tomassoni G, et al. Prospective evaluation of new and old criteria to discriminate between supraventricular and ventricular tachycardia in implantable defibrillators. Pacing Clin Electrophysiol 1998; 21:13471355 Porterfield JG, Porterfield LM, Smith BA, et al. Conversion rates of induced versus spontaneous ventricular tachycardia
30
31 32 33
34 35 36 37
38
39
40 41 42
43
44
45 46 47
by a third generation cardioverter defibrillator. Pacing Clin Electrophysiol 1993; 16:170 173 Gross JN, Sackstein RD, Song SL, et al. The antitachycardia pacing ICD: impact on patient selction and outcome. Pacing Clin Electrophysiol 1993; 16:165169 Rosenqvist M. Antitachycardia pacing: which patients and which methods? Am J Cardiol 1996; 78:9297 The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med 1991; 325:293302 De Vreede-Swagemakers JJM, Gorgels APM, Dubois-Arbouw WI, et al. Out-of-hospital cardiac arrest in the 1990s; a population-based study in the Maastricht area on incidence: characteristics and survival. J Am Coll Cardiol 1997; 30:1500 1505 Liberthson RR, Nagel EL, Hirschman JC, et al. Prehospital ventricular defibrillation: prognosis and follow-up course. N Engl J Med 1974; 291:317321 Weaver WD, Hill D, Fahrenbruch CE, et al. Use of the automatic external defibrillator in the management of out-ofhospital cardiac arrest. N Engl J Med 1988; 319:661 666 Roy D, Marcand E, Theroux P, et al. Programmed ventricular stimulation in survivors of an acute myocardial infarction. Circulation 1985; 72:487 494 Iesaka Y, Nogmi A, Aonuma K, et al. Prognostic significance of sustained monomorphic ventricular tachycardia induced by programmed ventricular stimulation using up to triple extrastimuli in survivors of acute myocardial infarction. Am J Cardiol 1990; 65:10571063 Wilber DJ, Olshansky B, Moran JF, et al. Electrophysiologic testing and nonsustained ventricular tachycardia: use and limitations in patients with coronary artery disease and impaired ventricular function. Circulation 1990; 82:350 358 Bhandari AK, Widerhorn J, Sager PT, et al. Prognostic significance of programmed ventricular stimulation in patients surviving complicated acute myocardial infarction: a prospective study. Am Heart J 1992; 124:8796 The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomized trial. Lancet 1999; 353:9 13 Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomized Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet 1999; 353:20012007 Boutitie F, Boissel JP, Connolly SJ, et al. Amiodarone interaction with beta-blockers: analysis of the merged EMIAT and CAMIAT databases; The EMIAT (European Myocardial Infarct Amiodarone Trial) and CAMIAT (Canadian Myocardial Infarct Amiodarone Trial) Investigators. Circulation 1999; 99:2268 2275 Lawton JS, Ellenbogen KA, Wood MA, et al. Sensing leadrelated complications in patients with transvenous implantable cardioverter-defibrillators. Am J Cardiol 1996; 78:647 651 Daoud EG, Kirsh MM, Bolling SF, et al. Incidence, presentation, diagnosis, and management of malfunctioning implantable cardioverter-defibrillator rate-sensing leads. Am Heart J 1994; 128:892 895 Roelke M, ONunsin SS, Osswald S, et al. Subclavian crush syndrome complicating transvenous cardioverter defibrillator systems. Pacing Clin Electrophysiol 1995; 18:973979 Brode SE, Schwartzman D, Callans DJ, et al. ICD-antiarrhythmic drug and ICD-pacemaker interactions. J Cardiovasc Electrophysiol 1997; 8:830 842 Naccarelli GV, Dougherty AH, Wolbrette D. Antiarrhythmic drug-implantable cardioverter-defibrillator interactions. In: Zipes DP, Jalife J, eds. Cardiovascular electrophysiology: from cell to bedside. 2nd ed. Philadelphia, PA: WB Saunders, 1995; 1426 1433
Review
1220
48 Dorian P, Newman D. Effect of sotalol on ventricular fibrillation and defibrillation in humans. Am J Cardiol 1993; 72:72A79A 49 Seifert T, Block M, Borggrefe M, et al. Erroneous discharge of an implantable cardioverter defibrillator caused by an electric razor. Pacing Clin Electrophysiol 1995; 18:15921594 50 Man KC, Davidson T, Langberg JJ, et al. Interference from a hand held radiofrequency remote control causing discharge of an implantable defibrillator. Pacing Clin Electrophysiol 1993; 16:1756 1758 51 Barbaro V, Bartolini P, Belloci F, et al. Electromagnetic interference of digital and analog cellular telephones with implantable cardioverter defibrillators: in vitro and in vivo studies. Pacing Clin Electrophysiol 1999; 22:626 634 52 Fetter JG, Ivans V, Benditt DG, et al. Digital cellular telephone interaction with implantable cardioverter-defibrillators. J Am Coll Cardiol 1998; 31:623 628 53 Occhetta E, Piebani L, Bartnik M, et al. Implantable cardioverter defibrillators and cellular telephones: is there any interference? Pacing Clin Electrophysiol 1999; 22:983989 54 Kou WH, Calkins H, Lewis RR, et al. Incidence of loss of consciousness during automatic implantable cardioverterdefibrillator shocks. Ann Intern Med 1991; 115:942945 55 Halinen MO, Jaussi A. Fatal road accidents caused by sudden death of the driver in Finland and Vaud, Switzerland. Eur Heart J 1994; 15:888 894 56 Trappe HJ, Wenzlaff P, Grellman G. Should patients with implantable cardioverter-defibrillators be allowed to drive?: observations in 291 patients from a single center over an 11-year period. J Interv Card Electrophysiol 1998; 2:193201 57 Epstein AE, Miles WM, Benditt DG, et al. Personal and public safety issues related to arrhythmias that may affect consciousness: implications for regulation and physician recommendations. Circulation 1996; 94:11471166 58 Larsen GC, Stupey MR, Walance CG, et al. Recurrent cardiac events in survivors of ventricular fibrillation or tachy-
59 60
61
62
63
64 65 66 67 68
cardia: implications for driving restrictions. JAMA 1994; 271:13351339 Vorperian VR, Lawrence S, Chlebowski K. Replacing abdominally implanted defibrillators: effect of procedure setting on cost. Pacing Clin Electrophysiol 1999; 22:698 705 Owens DK, Sanders GD, Harris RA, et al. Cost-effectiveness of implantable cardioverter defibrillators relative to amiodarone for prevention of sudden cardiac death. Ann Intern Med 1997; 126:112 Larsen GC, Manolis AS, Sonnenberg FA, et al. Cost-effectiveness of the implantable cardioverter-defibrillator: effect of improved battery life and comparison with amiodarone therapy. J Am Coll Cardiol 1992; 19:13231334 Wever EF, Hauer RN, Schrijvers G, et al. Cost-effectiveness of implantable defibrillator as first choice therapy versus electrophysiologically guided, tiered strategy in post-infarct sudden death survivors: a randomized study. Circulation 1996; 93:489 496 Mushlin AI, Hall WJ, Zwanziger J, et al. The cost-effectiveness of automatic implantable cardiac defibrillators: results from MADIT (Multicenter Automatic Defibrillator Implantation Trial). Circulation 1998; 97:2129 2135 Nearing BD, Huang AH, Verrier RL. Dynamic tracking of cardiac vulnerability by complex demodulation of the T wave. Science 1991; 252:437 440 Zehender M, Faber T, Grom A, et al. Continuous monitoring of acute myocardial ischemia by the implantable cardioverter defibrillator. Am Heart J 1994; 127:10571063 Steinhaus DM, Lemery R, Bresnahan DR Jr, et al. Initial experience with an implantable hemodynamic monitor. Circulation 1996; 93:745752 Daubert J. The compensatory pause prevention algorithm: preliminary results at the ventricular level. New York, NY: Futura Publishing, 1997; 168 179 Pinski SL, Fahy GJ. Implantable cardioverter-defibrillators. Am J Med 1999; 106:446 458
CHEST / 119 / 4 / APRIL, 2001
1221
S-ar putea să vă placă și
- Science Brief: COVID-19 Vaccines and VaccinationDocument25 paginiScience Brief: COVID-19 Vaccines and VaccinationanscstÎncă nu există evaluări
- Migrraine Review 2017 NEJMDocument9 paginiMigrraine Review 2017 NEJManscstÎncă nu există evaluări
- Severe Covid-19: Clinical PracticeDocument10 paginiSevere Covid-19: Clinical PracticeMiguel Angel Palacios FloresÎncă nu există evaluări
- A Novel Severity Score To Predict Inpatient Mortality in COVID 19 PatientsDocument8 paginiA Novel Severity Score To Predict Inpatient Mortality in COVID 19 PatientsanscstÎncă nu există evaluări
- Sign up to receive weekly anaesthesia tutorialsDocument10 paginiSign up to receive weekly anaesthesia tutorialsanscstÎncă nu există evaluări
- Drug Dosing in ElderlyDocument7 paginiDrug Dosing in ElderlyanscstÎncă nu există evaluări
- Genetic Dis & AnaesthDocument19 paginiGenetic Dis & AnaesthaksinuÎncă nu există evaluări
- Drugs Liver CirrhosisDocument5 paginiDrugs Liver CirrhosisanscstÎncă nu există evaluări
- Monitoring: DR Stefan ScholzDocument36 paginiMonitoring: DR Stefan ScholzanscstÎncă nu există evaluări
- Dept Crisis For HenriettaDocument2 paginiDept Crisis For HenriettaanscstÎncă nu există evaluări
- Davis CHF PharmacokineticsDocument10 paginiDavis CHF PharmacokineticsanscstÎncă nu există evaluări
- Dept Crisis For HenriettaDocument2 paginiDept Crisis For HenriettaanscstÎncă nu există evaluări
- Corticoids For ARFDocument22 paginiCorticoids For ARFanscstÎncă nu există evaluări
- Pitfalls in TEE EnglDocument53 paginiPitfalls in TEE EnglanscstÎncă nu există evaluări
- Ebstein AnomalyDocument5 paginiEbstein AnomalyanscstÎncă nu există evaluări
- Luminal Loop of Ryanodine ReceptorDocument3 paginiLuminal Loop of Ryanodine ReceptoranscstÎncă nu există evaluări
- CombitubeDocument14 paginiCombitubeanscstÎncă nu există evaluări
- Antiphospholipid Syndrome 7149Document13 paginiAntiphospholipid Syndrome 7149anscstÎncă nu există evaluări
- Anemia and Coagulation AnaesthesiaDocument28 paginiAnemia and Coagulation AnaesthesiaanscstÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (72)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- HCM Case Study in Young AthleteDocument1 paginăHCM Case Study in Young AthleteLADY JOWAHER ALLASÎncă nu există evaluări
- Introduction to Mitral Valve StenosisDocument10 paginiIntroduction to Mitral Valve StenosisSumathi GopinathÎncă nu există evaluări
- Silent Ischemia and Ischemic Heart Disease GuideDocument4 paginiSilent Ischemia and Ischemic Heart Disease GuideKyaw SithuÎncă nu există evaluări
- Chest PainDocument5 paginiChest PainAndrei MurariuÎncă nu există evaluări
- Sgarbossa CriteriaDocument5 paginiSgarbossa Criteriajacknaim7090Încă nu există evaluări
- Rah, Lah, RVH, LVHKDocument12 paginiRah, Lah, RVH, LVHKYuliana AtmayudhaÎncă nu există evaluări
- PALS Precourse Self-Assessment Score ReportDocument3 paginiPALS Precourse Self-Assessment Score ReportAde Novian ParmudityaÎncă nu există evaluări
- 3rd Lecture On Arrythmias by Dr. RoomiDocument16 pagini3rd Lecture On Arrythmias by Dr. RoomiMudassar Roomi100% (2)
- Ecg CmuDocument34 paginiEcg CmuArslan KhanÎncă nu există evaluări
- Claves de Cardiologia CX Cardiovascular VillamedicDocument0 paginiClaves de Cardiologia CX Cardiovascular VillamedicWendy Samaniego MojicaÎncă nu există evaluări
- Interpretation of Stress TestsDocument26 paginiInterpretation of Stress TestsHashini VjkmrÎncă nu există evaluări
- Cardiac Science "Arrhythmia"Document16 paginiCardiac Science "Arrhythmia"jimjose antonyÎncă nu există evaluări
- CARDIOLOGY – “PLABABLE” VALVULAR HEART DISEASE SIGNSDocument22 paginiCARDIOLOGY – “PLABABLE” VALVULAR HEART DISEASE SIGNSTirtha Taposh100% (1)
- Modified Valsalva Manoeuvre for SVTDocument3 paginiModified Valsalva Manoeuvre for SVTJyotirmayeeÎncă nu există evaluări
- 500 Single Best Answers in MedicineDocument443 pagini500 Single Best Answers in MedicineOmar Ahmed100% (1)
- Congenital Heart DiseaseDocument120 paginiCongenital Heart Diseasemerin sunilÎncă nu există evaluări
- Pathophysiology of Cardiogenic Pulmonary Edema - UpToDateDocument14 paginiPathophysiology of Cardiogenic Pulmonary Edema - UpToDateStefani AtlleÎncă nu există evaluări
- FA InglesDocument4 paginiFA InglesDitzon EspinozaÎncă nu există evaluări
- Cardiac Auscultation - Heart MurmursDocument9 paginiCardiac Auscultation - Heart MurmursAli AftabÎncă nu există evaluări
- Atrial Fibrilasi RATE CONTROL (Target HR 110 BPM)Document5 paginiAtrial Fibrilasi RATE CONTROL (Target HR 110 BPM)Melani NauritaÎncă nu există evaluări
- Congenital Heart DiseaseDocument5 paginiCongenital Heart Diseasesarguss14100% (1)
- 6 - Fahad Class 6 Cardiac AnesthesiaDocument18 pagini6 - Fahad Class 6 Cardiac AnesthesiaOne ClickÎncă nu există evaluări
- Treadmill Test GuideDocument22 paginiTreadmill Test GuideJegadeeswari EswarÎncă nu există evaluări
- The P WaveDocument13 paginiThe P Wave成失Încă nu există evaluări
- High Quality CPR, DR Ali Haedar PDFDocument45 paginiHigh Quality CPR, DR Ali Haedar PDFTaufik SuhendarÎncă nu există evaluări
- Cardiac Arrythmia For PathophysiologyDocument47 paginiCardiac Arrythmia For PathophysiologywilzmaxÎncă nu există evaluări
- Age Sex Chest Pain Type Blood Pressure Cholesterol Fasting Blood Sugar 120 Resting Ecg R C C R R C C I I I I I I IDocument14 paginiAge Sex Chest Pain Type Blood Pressure Cholesterol Fasting Blood Sugar 120 Resting Ecg R C C R R C C I I I I I I Isantu4_1111Încă nu există evaluări
- Show Questions One by OneDocument12 paginiShow Questions One by OneCharlie Cheng-Ying HsiehÎncă nu există evaluări
- ACLS Pharmacology Pretest Question Answers PDF (SET-2)Document9 paginiACLS Pharmacology Pretest Question Answers PDF (SET-2)김민길100% (1)
- Acute Coronary Syndromes Acute Coronary Syndromes OverviewDocument8 paginiAcute Coronary Syndromes Acute Coronary Syndromes Overviewمحمد زينÎncă nu există evaluări