Documente Academic
Documente Profesional
Documente Cultură
CFAR Newsletter - Volume 3, Issue 3
Încărcat de
UNC CFARDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
CFAR Newsletter - Volume 3, Issue 3
Încărcat de
UNC CFARDrepturi de autor:
Formate disponibile
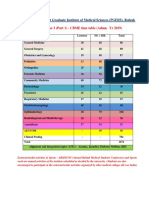
Center for AIDS Research
University of North Carolina at Chapel Hill
The mission of the CFAR is to provide a multidisciplinary environment that promotes basic, clinical, behavioral and translational research in the prevention, detection and treatment of HIV infection.
Volume 3.
Issue 3
August 15, 2011
serodiscordant couples (1). According to the HIV Prevention Trials Network website, data from Africa and Thailand collected during the study shows that there is a correlation between HIV viral load (blood levels) and HIV transmission. Specifically, the higher the viral load in the blood, the more likely the chance for transmission. Antiretroviral therapy (ART) reduces the viral load in the blood, as well as in genital secretions (for men and women), and the drugs can be detected in semen and vaginal and cervical secretions (1). What this information implies is that taking ART may make HIV-infected people less contagious (1). These findings suggest that by taking ART, HIV positive persons could engage in sexual behaviors and still protect their partners from HIV infection. This study has been met with media frenzy, and Cohen has been in high demand around the globe to speak about these incredible findings that could change the way that ART is prescribed and used. These results could serve as the starting point for a great shift in our current methods of ARV drug prescription and use. This issue of our CFAR newsletter explores the possible ethical, clinical, and research implications of the HPTN 052 study. It includes several opinion pieces from members of our CFAR team and their thoughts on how this study could change the way we approach HIV/AIDS healthcare, prevention, education, and treatment in the future.
(1) http://www.hptn.org/research_studies/hptn052.asp
HPTN 052 Study Opens New Doors for HIV/AIDS Treatment Plans and Care
Dr. Myron Cohen, associate director of the UNC Center for AIDS Research, has had a very busy 30 years working in the field of HIV/AIDS medicine. As a Distinguished Professor of Medicine, Public Health, and Microbiology and Immunology at the University of North Carolina at Chapel Hill, he travels, sees patients, and leads research projects that explore the transmission and prevention of transmission of HIV, with a special focus on the role played by STD co-infections. Dr. Cohen received an NIH MERIT award in 2005 and is the author of more than 400 written scholarly works. He also received the Thomas Parran Award in 2005 for lifetime achievement in STD research from the American STD Association. He has extensive experience conducting research in countries such as Malawi, Africa and China. Dr. Cohen is the Chairman of the Scientific Advisory Board of the China CIPRA (at the China CDC) and is co-director of an NIH Ellison Fellowship Program at the National STD Center in Nanjing China. At this summer's Global AIDS Conference in Rome, Dr. Cohen presented a paper on the HPTN 052 study, entitled A Randomized Trial to Evaluate the Effectiveness of Antiretroviral Therapy Plus HIV Primary Care versus HIV Primary Care Alone to Prevent the Sexual Transmission of HIV-1 in Serodiscordant Couples. The study was a multisite, randomized trial designed to determine the effectiveness of two treatment strategies in preventing the sexual transmission of HIV in HIV-
NEWS BRIEF:
-To hear about the HPTN 052 study from Dr. Cohen, listen to his WUNC interview at: http://wunc.org/tsot/archive/ HIV_and_Sex.mp3/view -Watch Dr. Cohen speak on the study at the 6th IAS Conference on HIV Pathogenesis, Treatment and Prevention (July, 2011 in Rome, Italy): http://www.youtube.com/watch? v=P3DPOntJfOs Our Issue Contributors: -Dr. Stuart Rennie is Research Assistant Professor in Social Medicine and co-Chair of UNCs IRB for social and behavioral research. His current teaching and research interests focus on research ethics, public health ethics and medical ethics, particularly in the context of the developing world. -Dr. Christopher Hurt is Clinical Assistant Professor in the Division of Infectious Diseases at UNC. His research interests include acute HIV infection, transmission of antiretroviral drug resistance, HIV phylogenetics, spatial epidemiology, and substance uses impact on HIV risk. -Dr. Ronald Strauss is the Executive Associate Provost and Chief International Officer at UNC. He has held appointments in the School of Dentistrys department of dental ecology, the School of Medicines department of social medicine, and the School of Public Healths department of epidemiology. He also serves as a dental clinician and advisor for the UNC Craniofacial Center.
CONTACT: UNC CFAR Website: http://cfar.med.unc.edu/ Ronald Swanstrom PI riscunc@med.unc.edu CFAR Community Outreach and Education(CODE Office) Contacts: Dr. Ron Strauss (ron_strauss@unc.edu) & Vanessa White (VMWhite@email.unc.edu) Newsletter written/compiled by Danielle Strauss Disponible en Espaol: contacta VMWhite@email.unc.edu
WE ARE ON FACEBOOK and TWITTER!!! Search for UNC Center for AIDS Research and click the Like button to get news and more!
The Big Questions: Ethical Issues Inspired by the HPTN 052 Study by Dr. Stuart Rennie
This month, we asked Dr. Stuart Rennie, ethicist and HIV/AIDS researcher at UNC-CH, to share his thoughts on ethical issues that may stem from the newly released HPTN 052 study results. He shared these very thought-provoking questions with us: Clinical Questions: Doctors armed with the knowledge of HPTN 052 are faced with something of a dilemma. When should their patients start ARVs? On the one hand, if they start them early, before the patients immune system is compromised, is that decision really in that patients interest? HPTN 052 showed there are some clinical benefits to the early initiation of treatment, but these have to be weighed against countervailing factors such as the possibility of drug resistance and drug side-effects. On the other hand, waiting until the patient has a lower CD4 count before initiating treatment will increase risks to that persons (seronegative) sexual partner(s). On the internet, there are already worries expressed that treatment as prevention will lead to clinicians treat HIV-positive persons more as disease vectors than as patients. Overall, HPTN 052 will force physicians to make some ethically tricky decisions in particular cases. Research Questions: The ethics of some ongoing research studies on HIV prevention may be seriously affected by the results of HPTN 052. For example, some PREP studies involve serodiscordant couples. If the results of HPTN 052 are taken into account, then providing treatment to some of those HIV+ persons (depending on their CD4 count) should be the standard of care/ prevention. It would seem to follow that the design of those studies is now unethical, according to the Declaration of Helsinki, or at least the design is open to debate. One could also go further,
Continued on Page 2
Page 2
Center for AIDS Research
The Big Questions by Stuart Rennie, Continued from Page 1
and ask if PREP studies make sense anymore post-HPTN 052. Why bother giving ARVs to seronegatives as an HIV prevention strategy? Why not just give all HIV+ persons ARVs early, so their at-risk partners do not get infected? Health Policy Questions: Many ethical problems will be confronted when translating the results of HPTN 052 into policy. In theory, if all HIV+ persons were put on ARVs early worldwide, there would be a massive decrease in new HIV infections. In practice, it has taken decades to increase access to those who desperately need ARVs, especially in resource-poor countries. Despite decades of effort, the rates of HIV testing are still very low in many settings. The state of health infrastructure in many countries is fragile, including shortages of competent health care professionals. Given all this, and the current economic crisis, how can we reasonably expect rollout of early initiation of ARV treatment to have an impact as a prevention strategy? Who is going to pay for all this? Besides cost, there are questions of equity. Since we already cant give ARVs to everyone who needs it, now that we know more about treatment as prevention, we face some difficult rationing decisions. When distributing ARVs, should we give priority to those more likely to transmit the virus to others? That may seem justified from a public health perspective, but what about those who need ARVs but are less likely to transmit the virus, such as HIV-positive children and faithful HIVpositive sexual partners. In addition, there is the problem of coercion: should the policy on early initiation of ARVs be voluntary? Should patients be allowed to refuse early treatment if they do not want it? There are good (ethical) reasons to make the policy voluntary, but those in public health may want to limit the potential for refusal in order to have the greatest epidemiological impact. These are all extremely important questions and issues raised by Dr. Rennie, and the UNC CFAR looks forward to an active dialogue among clinicians, researchers, and the community in the months to come on these topics.
A Study of Huge Magnitude: Thoughts on HPTN 052 from Dr. Christopher Hurt
The United Nations estimates that in 2009, 2.6 million new HIV infections occurred worldwide. In order to combat the spread of the HIV pandemic, a variety of behavioral and biomedical interventions have been proposed, but combinations of the two seem to hold the greatest promise for the future. UNC has long been a leader in studying the dynamics of the sexual spread of HIV (and other STIs) among both heterosexuals and men who have sex with men. Critical basic science and translational research by current and former UNC investigators examined the relationship between blood and semen viral loads during chronic and acute infection, and laid the groundwork for what has evolved into the treatment as prevention strategy. This approach posits that broad antiretroviral utilization by HIV-infected persons can reduce infectiousness to others, thus reducing overall incidence. Ecological and cohort data supported this concept, but it remained unproven until now. Earlier this year, the results of HPTN 052 were released, showing conclusively that the strategy of treatment as prevention works. This randomized, placebo-controlled study, chaired by our Infectious Diseases division chief, Dr. Myron Cohen, demonstrated that when the HIVinfected partner in a serodiscordant heterosexual couple is treated with antiretrovirals (ARVs), there is a 96% reduction in the risk of transmission to the uninfected partner. These results are clinically important for many reasons, but three warrant specific mention here. First, the magnitude of the effect was by no means subtle. Often in clinical research, the effect size is modest, leaving some question about whether or not its worth it to implement the new treatment in practice. Here, with so large an effect, there is very little room to dither about efficacy. Second, it augments the data we already have about the benefits of having ones HIV infection controlled by ARV therapy. Large cohort studies like SMART and D:A:D have suggested that uncontrolled virus may predispose some HIV-infected persons to medical complications of chronic inflammation, such as premature coronary or cerebrovascular disease. While these prior data reflect individual-level effects of being treated, HPTN 052 shows the altruistic effects of therapy for others and for public health. For some patients (especially women) who put their loved ones health before their own, the results may prove useful in discussions about the pros and cons of starting ARVs. Finally, 052 presents a powerful counterargument to proponents of pre-exposure prophylaxis (PrEP), another treatment as prevention strategy. Instead of treating persons already living with HIV, PrEP is used as primary prevention among those who are HIV-uninfected but at high risk for acquiring the virus. The preventive effect seen with the four PrEP major studies released to date (iPrEx, CAPRISA, TDF2, and Partners PrEP) has ranged between 40-80% and much lower than the 96% seen in HPTN 052. It is clear that PrEP will have a specific niche in prevention especially among marginalized, at-risk persons unable to negotiate for safer sex practices but from a perspective of allocation of scarce resources, it makes much more sense to treat those already living with HIV than to provide medications to those not yet infected. Treatment as prevention is not a panacea; it remains to be seen how these findings can be implemented on a large scale, and clearly we continue to have difficulties in this country with finding at-risk persons, testing them, and linking them to care. However, HPTN 052 provides critical evidence that those efforts have a potentially big payoff: reduction in the numbers of new HIV infections, and the beginning of the end of the pandemic.
Couples Can Take Care of One Another and more about HPTN 052 from Dr. Ronald Strauss
The HPTN 052 study has changed how HIV scientists, policy makers and clinicians approach HIV/AIDS prevention. In this study, individuals infected with HIV substantially lowered the chance that they would transmit the virus to their long-term uninfected sexual partners by taking antiretroviral medications early, while they were feeling healthy. This was a large clinical study sponsored by the National Institute of Allergy and Infectious Diseases (NIAID) and continues until 2015. The release of findings at the request of the data and safety monitoring board (DSMB) happened because the data was already indicating strongly that early antiretroviral medications taken by HIV-infected individuals quite dramatically reduced transmission to their uninfected partners. Dr. Myron (Mike) Cohen directs the Institute for Global Health and Infectious Diseases at the University of North Carolina at Chapel Hill; he was the study Principal Investigator. This study also suggests that extrapulmonary tuberculosis can be reduced for the HIV infected participant by early antiretroviral treatment, as well. One aspect of this study which is especially exciting to me is that it examines how couples in long-term relationships can help to avoid transmission and also can take care of one another. The study further supports that serodiscordant couples can have relationships in which transmission can be avoided. The implications for public health globally are enormous. We are so proud that a UNC scientist and a global team could implement a study that has changed how HIV will be understood and treated in the years to come. To read more opinions on the HPTN 052 study, visit our CFAR CODE office blog at: http://unccfar.blogspot.com/
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Merrill Singer - The Anthropology of Infectious Disease (2014, Left Coast Press)Document321 paginiMerrill Singer - The Anthropology of Infectious Disease (2014, Left Coast Press)rina100% (1)
- Iso 22442-1-2015Document34 paginiIso 22442-1-2015iipmnpti iipmÎncă nu există evaluări
- BAG Technique: Hamima A. Pandapatan CHN Skills-Level II Group ODocument15 paginiBAG Technique: Hamima A. Pandapatan CHN Skills-Level II Group OHamima Azis PandapatanÎncă nu există evaluări
- HEALTH K 12 Curriculum Guide Grades 1 and 7Document14 paginiHEALTH K 12 Curriculum Guide Grades 1 and 7Vanessa Ann Cabello ElbanoÎncă nu există evaluări
- Nclex TipsDocument93 paginiNclex TipsAmiel Francisco Reyes86% (7)
- May 2012 CFAR Newsletter - Stories of AIDSDocument2 paginiMay 2012 CFAR Newsletter - Stories of AIDSUNC CFARÎncă nu există evaluări
- April 2012 CFAR Newsletter - On The Cutting Edge of HIV/AIDS Research at UNCDocument2 paginiApril 2012 CFAR Newsletter - On The Cutting Edge of HIV/AIDS Research at UNCUNC CFARÎncă nu există evaluări
- August 2012 CFAR Newsletter - International AIDS Meeting in DCDocument2 paginiAugust 2012 CFAR Newsletter - International AIDS Meeting in DCUNC CFARÎncă nu există evaluări
- March 2012 CFAR Newsletter - AIDS in The SouthDocument2 paginiMarch 2012 CFAR Newsletter - AIDS in The SouthUNC CFARÎncă nu există evaluări
- CFAR Newsletter - Volume 4, Issue 1Document2 paginiCFAR Newsletter - Volume 4, Issue 1UNC CFARÎncă nu există evaluări
- CFAR Newsletter - Volume 3, Issue 4Document2 paginiCFAR Newsletter - Volume 3, Issue 4UNC CFARÎncă nu există evaluări
- NIMH Pilot Announcement 2011Document4 paginiNIMH Pilot Announcement 2011UNC CFARÎncă nu există evaluări
- PEPFAR Aps-Oaa-11-000002-1Document51 paginiPEPFAR Aps-Oaa-11-000002-1UNC CFARÎncă nu există evaluări
- Free Rapid HIV Tests by CountyDocument5 paginiFree Rapid HIV Tests by CountyUNC CFARÎncă nu există evaluări
- CFAR Newsletter - Volume 3, Issue 2Document2 paginiCFAR Newsletter - Volume 3, Issue 2UNC CFARÎncă nu există evaluări
- CFAR Newsletter - Volume 3, Issue 1Document2 paginiCFAR Newsletter - Volume 3, Issue 1UNC CFARÎncă nu există evaluări
- Microbiology Pre Test 1Document6 paginiMicrobiology Pre Test 1thediaber100% (1)
- Channel Catfish Virus DiseaseDocument4 paginiChannel Catfish Virus Diseaseapi-3737467Încă nu există evaluări
- MULTIPLE CHOICE. Read The Following Questions and Choose The Best Answer by Shading TheDocument14 paginiMULTIPLE CHOICE. Read The Following Questions and Choose The Best Answer by Shading ThePrince Mark BadilloÎncă nu există evaluări
- CM 86 192Document4 paginiCM 86 192lucia pereiraÎncă nu există evaluări
- Medical-Surgical Nursing I & Ii Course Description Text:: NCLEX-PN Examination (5Document89 paginiMedical-Surgical Nursing I & Ii Course Description Text:: NCLEX-PN Examination (5Musa yohanaÎncă nu există evaluări
- 2019 CompetDocument64 pagini2019 CompetKshirsagar DarshÎncă nu există evaluări
- 1 - The Covid-19 Vaccine Is GENE THERAPY - David Martin BotW - Transcript - 01!11!2021Document7 pagini1 - The Covid-19 Vaccine Is GENE THERAPY - David Martin BotW - Transcript - 01!11!2021bigbill138Încă nu există evaluări
- Week 3 TLE 101 Implementing and Monitoring Infection Control Policies and ProceduresDocument3 paginiWeek 3 TLE 101 Implementing and Monitoring Infection Control Policies and ProceduresJoel Mamocod100% (1)
- 13 WhydowefallillDocument10 pagini13 WhydowefallillBharati AngadiÎncă nu există evaluări
- AIDS Transcripts Prevention and TreatmentDocument19 paginiAIDS Transcripts Prevention and TreatmentVicky BarreraÎncă nu există evaluări
- JAMA Network JAMA The Third International Consensus Definitions For Sepsis and Septic Shock (Sepsis-3)Document15 paginiJAMA Network JAMA The Third International Consensus Definitions For Sepsis and Septic Shock (Sepsis-3)Siti Fatimah RadÎncă nu există evaluări
- Jib 221 Microbiology: The Main Themes of MicrobiologyDocument47 paginiJib 221 Microbiology: The Main Themes of MicrobiologyNazzÎncă nu există evaluări
- F2 Mid-Year Exam Section BDocument3 paginiF2 Mid-Year Exam Section BAnne Marian Anak JOSEPHÎncă nu există evaluări
- Laurence Franken, Kansas State UniversityDocument16 paginiLaurence Franken, Kansas State UniversityralapubsÎncă nu există evaluări
- Presentation in Ite-325: Donald John H. Borja Bsit-3BDocument8 paginiPresentation in Ite-325: Donald John H. Borja Bsit-3BLea Underscore100% (1)
- Covid in PregnancyDocument30 paginiCovid in Pregnancyvidhi chaudharyÎncă nu există evaluări
- Engineering Probiotics For Therapeutic ApplicationsDocument9 paginiEngineering Probiotics For Therapeutic ApplicationsElinaÎncă nu există evaluări
- Gapuz Communicable Disease NursingDocument46 paginiGapuz Communicable Disease NursingBJ DUQUESAÎncă nu există evaluări
- chn2 Lec ReviewerDocument11 paginichn2 Lec Reviewerella retizaÎncă nu există evaluări
- Antibiotics Lloyd ADocument11 paginiAntibiotics Lloyd AAndrew Lloyd100% (1)
- Deneme 07Document15 paginiDeneme 07Ceyhun Güler ☾☆Încă nu există evaluări
- Deep Neck InfectionsDocument9 paginiDeep Neck InfectionsfayzaÎncă nu există evaluări
- Vancouver Coastal Health Enhanced Surveillance and Precautions ProtocolsDocument1 paginăVancouver Coastal Health Enhanced Surveillance and Precautions ProtocolsIan YoungÎncă nu există evaluări
- Treating The Common Cold and Flu: Special Considerations For ADHD, ADD, and ASD by Kim Gould, RPH, MSDocument4 paginiTreating The Common Cold and Flu: Special Considerations For ADHD, ADD, and ASD by Kim Gould, RPH, MSautismoneÎncă nu există evaluări
- Fever of Unknown Origin in Children - Etiology - UpToDateDocument27 paginiFever of Unknown Origin in Children - Etiology - UpToDatealvaro martinezÎncă nu există evaluări