Documente Academic
Documente Profesional
Documente Cultură
Final DX Results
Încărcat de
zysheaiDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Final DX Results
Încărcat de
zysheaiDrepturi de autor:
Formate disponibile
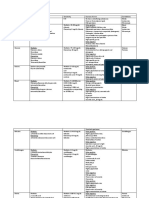
DIAGNOSTIC TESTS AND LABORATORY RESULTS
DIAGNOSTIC TEST AND DESCRIPTION CBC ANALYSIS : A complete blood count (CBC) is a group of tests used for basic screening purposes. It is probably the most widely ordered laboratory test. Results provide the enumeration of the cellular elements of the blood, measurement of RBC indices, and determination of cell morphology by automation and evaluation of stained smears. The results can provide valuable diagnostic information regarding the overall health of the patient and the patients response to disease and treatment. RBC INDICATION AND CONTRAINDIC ATION CLIENT PREPARATION AND POST PROCEDURE INSTRUCTIONS PREPARATIONS: Inform the patient that the test is used to evaluate numerous conditions involving red blood cells, white blood cells, and platelets. The test is also used to indicate inflammation, infection, and response to chemotherapy. Obtain a history of the patients complaints, including a list of known allergens (especially allergies or sensitivities to latex), and inform the appropriate health care practitioner accordingly. Obtain a history of the patients gastrointestinal, hematopoietic, immune, and respiratory systems, as well as results of previously performed laboratory tests, surgical procedures, and other diagnostic procedures. For related laboratory tests, refer to the Gastrointestinal, Genitourinary, Hematopoietic, Immune, and Respiratory System tables. Obtain a list of medications the patient is taking, including herbs, nutritional supplements, and nutraceuticals. The requesting health care practitioner and laboratory should be advised if the patient NORMAL FINDINGS ACTUAL FINDINGS CLINICAL SIGNIFICANCE
HEMATOCRIT
Detect hematologic disorder, neoplasm, leukemia, or immunologic abnormality Determine the presence of hereditary hematologic abnormality Evaluate known or suspected anemia and related treatment Monitor blood loss and response to blood replacement Monitor the effects of physical or emotional stress Monitor fluid imbalances or treatment for fluid imbalances Monitor hematologic status during pregnancy Monitor progression of nonhematologic disorders, such as chronic obstructive pulmonary disease, malabsorption syndromes, cancer, and renal disease Monitor response to chemotherapy and evaluate undesired reactions to drugs that may cause blood dyscrasias
4.00-5.40 g/L
4.3
Pt. has normal level of RBC and indicates still functional transportation of 02 from the lungs to body tissues
0.31-.47 g/L
0.38
The pt. has a normal level of hct which indicates good skin hydration .
HEMOGLOBIN
WBC
Provide screening as part of a general physical examination, especially on admission to a health care facility or before surgery
regularly uses these products so that their effects can be taken into consideration when reviewing results. Explain to the patient that there may be some discomfort during the venipuncture. Post-test: Observe venipuncture site for bleeding or hematoma formation. Apply paper tape or other adhesive to hold pressure bandage in place, or replace with a plastic bandage. Nutritional considerations: Instruct patients to consume a variety of foods within the basic food groups, maintain a healthy weight, be physically active, limit salt intake, limit alcohol intake, and be a nonsmoker. A written report of the examination will be sent to the requesting health care practitioner, who will discuss the results with the patient. Reinforce information given by the patients health care provider regarding further testing, treatment, or referral to another health care provider. Answer any questions or address any concerns voiced by the patient or family. Depending on the results of this procedure, additional testing may be performed to evaluate or monitor
12.0-15.0 g/L
12.6
Pt. has normal level of RBC and indicates still functional transportation of 02 from the lungs to body tissues
4.50-11.00 g/L
3.50
Pt. has low level of WBC that may indicate decreased with some medications (such as methotrexate), some autoimmune conditions, some severe infections, bone marrow failure, and congenital marrow aplasia (marrow doesn't develop normally)
NEUTROPHILS
51-67%
53
The pt. Has a normal of Neutrophils which indicate still functional in removal of noxious stimuli that cause cell death that lead to inflammation. ---------
STABS/BANDS
0.03-0.06 g/L
----------
EOSINOPHILS
0.02-0.05g/L
------------
Eosinophils is responsible for engulfing and killing bacteria. Patient has still functional immune system. --------Lymphocytes produce antibodies and also fight viruses. Therefore a high lymphocyte count indicates an infection or virus such as the common cold.
BASOPHILS LYMPHOCYTES
0.00-0.01 g/L 0.25-0.35 g/L
--------0.47
MONOCYTES
0.02-0.08 g/L
---------
---------
PLATELET COUNT
progression of the disease process and determine the need for a change in therapy. Evaluate test results in relation to the patients symptoms The prothrombin time is done to test the integrity of part of the clotting scheme. The prothrombin time is commonly used as a method of monitoring the accuracy of blood thinning treatment (anticoagulation) with warfarin (Cou madin). Preparation: The patient must be instructed to discontinue all the medications that may interfere with Prothrombin Time such as Warfarin. Aftercare: Aftercare consists of routine care of the area around the puncture mark. Pressure is applied for a few seconds and the wound is covered with a bandage
200.00400.00 g/L
256.00
Normal level of platelet count and may indicate that pt. has no bleeding disorder
Prothrombin Time: a blood test that measures how long it takes blood to clot. A prothrombin time test can be used to check for bleeding problems. PT is also used to check whether medicine to prevent blood clots is working.
Control Patient Activity INR Activated Partial Thromboplastin Time : The activated partial thromboplastin time (APTT) coagulation test evaluates the function of the intrinsic (factors XII, XI, IX, and VIII) and common (factors V, X, II, and I) pathways of the coagulation sequence, specifically the intrinsic thromboplastin system. It represents the time required for a firm fibrin clot to form after tissue thromboplastin PRETEST: Inform the patient that the test is used to evaluate coagulation disorders and monitor therapy. Obtain a history of the patients complaints, including a list of known allergens (especially allergies or sensitivities to latex), and inform the appropriate health care practitioner accordingly. Obtain a history of the patients hematopoietic and hepatobiliary systems, history of any bleeding disorders, and results of previously performed laboratory tests (especially bleeding time, complete blood count, PTT, platelets, and PT), surgical
10-15s 1.23-18.9s 75-130% 0.80-1.20
13.1 17.4 113% 0.92
A normal PT indicates that there is no bleeding problems caused by a problem with the clotting factors.
Detect congenital deficiencies in clotting factors, as seen in diseases such as hemophilia A (factor VIII) and hemophilia B (factor IX) Evaluate response to anticoagulant therapy with heparin or coumarin derivatives Identify individuals who may be prone to bleeding during surgical, obstetric, dental, or invasive diagnostic procedures Identify the possible cause of abnormal
or phospholipid reagents similar to thromboplastin and calcium are added to the specimen. The APTT is abnormal in 90% of patients with coagulation disorders and is useful in monitoring the inactivation of factor II effect of heparin therapy. The test is prolonged when there is a 30% to 40% deficiency in one of the factors required, or when factor inhibitors (e.g., antithrombin III, protein C, or protein S) are present. The APTT has additional activators, such as kaolin, Celite, or elegiac acid, that more rapidly activate factor XII, making this test faster and more reliably reproducible than the partial thromboplastin time (PTT). A comparison between the results of APTT and prothrombin time (PT) tests can allow some inferences to be made that a factor deficiency exists. A normal APTT with a prolonged PT can only occur with factor VII deficiency. A prolonged APTT with a normal PT could indicate a deficiency in factors
bleeding, such as epistaxis, hematoma, gingival bleeding, hematuria, and menorrhagia Monitor the hemostatic effects of conditions such as liver disease, protein deficiency, and fat malabsorption
procedures, and other diagnostic procedures. For related laboratory tests, refer to the Hematopoietic and Hepatobiliary System tables. Obtain a list of the medications the patient is taking, including anticoagulant therapy, acetylsalicylic acid, herbs, nutritional supplements, and nutraceuticals, especially those known to affect coagulation. It is recommended that use of these products be discontinued 14 days before dental or surgical procedures. The requesting health care practitioner and laboratory should be advised if the patient regularly uses these products so that their effects can be taken into consideration when reviewing results. If the patient is receiving anticoagulant therapy, note the time and amount of the last dose. Review the procedure with the patient. Inform the patient that specimen collection takes approximately 5 to 10 minutes. Address concerns about pain related to the procedure. Explain to the patient that there may be some discomfort during the venipuncture. There are no food, fluid, or medication restrictions, unless by medical direction. POST TEST
XII, XI, IX, VIII, and VIII:C (von Willebrand factor). Factor deficiencies can also be identified by correction or substitution studies using normal serum. These studies are easy to perform and are accomplished by adding plasma from a normal patient to a sample from a patient suspected to be factor deficient. When the APTT is repeated and is corrected, or within the reference range, it can be assumed that the prolonged APTT is caused by a factor deficiency. The administration of prophylactic low-dose heparin does not require serial monitoring of APTT. Control Patient
Observe venipuncture site for bleeding or hematoma formation. Apply paper tape or other adhesive to hold pressure bandage in place, or replace with a plastic bandage. Instruct the patient to report severe bruising or bleeding from any areas of the skin or mucous membranes. Inform the patient with prolonged APTT values of the importance of taking precautions against bruising and bleeding, including the use of a soft bristle toothbrush, use of an electric razor, avoidance of constipation, avoidance of acetylsalicylic acid and similar products, and avoidance of intramuscular injections. Inform the patient of the importance of periodic laboratory testing while taking an anticoagulant. A written report of the examination will be sent to the requesting health care practitioner, who will discuss the results with the patient. Reinforce information given by the patients health care provider regarding further testing, treatment, or referral to another health care provider. Answer any questions or address any concerns voiced by the patient or family. Depending on the results of this procedure, additional
27-43 27-42
36.0 40.1
A normal APTT Indicates no abnormal bleeding problems.
testing may be performed to evaluate or monitor progression of the disease process and determine the need for a change in therapy. Evaluate test results in relation to the patients symptoms and other tests performed.
URINALYSIS A urinalysis consists of a number of physical, chemical and microscopic tests of a urine sample as part of a checkup to help diagnose a urinary tract or metabolic disease. Doctors also use urinalysis as a general health screen. The urinalysis is used as a screening and/or diagnostic tool because it can help detect substances or cellular material in the urine associated with different metabolic and kidney disorders. It is ordered widely and routinely to detect any abnormalities that require follow up. Often, substances such as protein or glucose will begin to appear in the urine before patients are aware that they may have a problem. It is used to detect urinary tract infections (UTI) and other disorders of the urinary tract. In patients with
Routine Physical A routine physical exam often includes a urinalysis to screen for early signs of medical problems. Abnormal waste products or abnormal levels of cells may indicate disease. Monitoring Disease For patients who already have an existing condition like diabetes or kidney disease, urinalysis helps to monitor their status and determines whether their course of treatment requires adjustment Urinary Tract Symptoms Patients who have urinary symptoms undergo urinalysis to help doctors diagnose
Preprocedure: 1.Ask your doctor or health care provider these questions before your urinalysis: o Why does the test need to be done? o What should I do before the test? o Where do I need to go to take the test? o How will the results of this test affect my medical care? o Could my lifestyle habits, like smoking, affect this test? 2 Prepare a list of the medications, vitamins, or supplements you regularly take. Give the list to the lab technician. All drugs can affect the results of your tests.The Mayo Clinic notes that you should eat and drink normally before a routine urinalysis. 3 Follow your doctor's instructions regarding collection of the specimen. Some tests require the urine specimen to be collected when you first awake in the morning because at that time your urine is more concentrated. If your doctor requires a first-in-the-morning specimen, make a mental note the night before. Also, as another reminder, place the specimen container on the closed lid of the toilet
acute or chronic conditions, such as kidney disease, the urinalysis may be ordered at intervals as a rapid method to help monitor organ function, status, and response to treatment.
urinary tract diseases, like infections. Abnormal test results in such cases commonly include blood and increased white cells in the urine. Pregnancy A different type of urinalysis for the hormone human chorionic gonadotropin shows pregnancy. You can get this test at your doctor's office, or you can perform a test yourself using a hometesting kit. Drug Screening Employers may use specialized urinalysis tests to screen job applicants and employees for drug use. Sports associations test athletes for drugs. Law enforcement also uses forensic urinalysis to screen for drugs and toxins.
CHEMICAL: COLOR
to avoid forgetting in the morning. Deliver the collected specimen to either your doctor's office or the lab as directed. Your doctor might also instruct you to use the "clean catch method" whether you are at home, at your doctor's office, or at the lab. Clean the urinary opening with the moist towelette provided by the nurse or lab technician before you urinate into the plastic cup provided. You may also be instructed to initiate urination into the toilet, then stop the flow before continuing again into the specimen collection container. 4 Fast the night before your urinalysis, if ordered by your doctor. If your doctor has ordered a urinalysis test in combination with other tests, it is very likely you will have to fast before the test. To fast simply means to stop all eating and drinking, usually at midnight. If your appointment is scheduled for later in the day, such as in the afternoon or evening, you should not consume food or liquids for at least twelve hours prior to the lab exam. If you have specific health problems, such as diabetes, check with your physician for specific fasting instructions prior to the test. Aftercare: The patient may return to normal activities after collecting the sample and may start taking any medications that were discontinued before the test.
straw yellow to amber
yellow
Normal urine is yellow, with concentration increasing the more yellow a sanple is. Some medications can cause a change in urine color, which can alter the urinalysis values and change the way urinalysis interpretation is done by a physician or other medical professional. Cloudy urine or urine with a high level of sediment may be present in cases of urinary tract infection Abnormal causes of turbidity include the presence of blood cells, yeast, and bacteria. The patient has a normal specific gravity which indicates that kidneys are functional to concentrate the urine.(conserve water) There is no presence of sugar in clients urine. No indication of DM There is no indication of kidney problems. ----------------------------
TRANSPARENCY
transparent
hazy/cloudy
S. GRAVITY
1.003-1.035
1.020
SUGAR
(-)
(-)
PROTEIN KETONES BILE UROLOBILINOGE N
(-) (-) (-) (-) 0.2-1.0 Ehr U/dL
(-) ----------------------------
MICROSCOPIC: PUS CELLS 0-2/HPF 4-6/hpf White blood cells (or pus cells), which are a sign of an infection or inflammation in the kidneys, bladder or another area. Red blood cells, which may be a sign of kidney diseases that damage the filtering units of the kidneys, allowing blood cells to leak into the urine. Blood in the urine may also be a sign of problems like kidney stones, infections, bladder cancer or a blood disorder like sickle cell disease. The urinary tract is also lined with epithelial tissues and so, it is normal to find few of these cells in the urine. Presence of mucus threads is nothing to worry about however, an irritating factor could stimulate mucus secretion. Bacteria, or germs, which are usually a sign of an infection in the body. The amorphous urates are the most likely reason that the urine is slightly hazy. Not clinically significant.
RBC
0-2/HPF
0-2/hpf
EPITHELIAL CELLS
Few
Few
MUCUS THREAD
Few
Few
BACTERIA
Few
Rare
AMORPHOUS URATES
Few
Rare
Name: J.M Rm207
Date: March 03, 2011 Age: 5y.o
TYPE OF EXAMINATION: DENGUE NS1AG
Dengue NS1Ag: POSITIVE Dengue Virus Test: 1gG: POSITIVE 1gM: POSITIVE
S-ar putea să vă placă și
- Venipuncture Complications and Preexamination Variables: RequistionsDocument19 paginiVenipuncture Complications and Preexamination Variables: RequistionsAngel Cascayan Delos SantosÎncă nu există evaluări
- Prelims Week 3 - Urinalysis - TransDocument16 paginiPrelims Week 3 - Urinalysis - TransLoro JDÎncă nu există evaluări
- Examination of Urine Formation and CompositionDocument7 paginiExamination of Urine Formation and CompositionDaniel LamasonÎncă nu există evaluări
- Group 3 - ParasitologyDocument8 paginiGroup 3 - Parasitologyjulo_05Încă nu există evaluări
- Urine Specimen Collection: Ms. Sneha SehrawatDocument36 paginiUrine Specimen Collection: Ms. Sneha SehrawatRajaÎncă nu există evaluări
- Clearance and GFR: Major DR Arabinda Mohan Bhattarai Lecturer (Biochemistry), NAIHSDocument25 paginiClearance and GFR: Major DR Arabinda Mohan Bhattarai Lecturer (Biochemistry), NAIHSChandan SahÎncă nu există evaluări
- A. B. C. A. B. C. D.: Clinical Chemistry II - Prelims (Bandala)Document19 paginiA. B. C. A. B. C. D.: Clinical Chemistry II - Prelims (Bandala)IceÎncă nu există evaluări
- Analysis of Physical Properties of UrineDocument2 paginiAnalysis of Physical Properties of UrineameerabestÎncă nu există evaluări
- Topic 02 Urinalysis I Review of Ana and Phy of KidneysDocument6 paginiTopic 02 Urinalysis I Review of Ana and Phy of KidneysNatasha MendozaÎncă nu există evaluări
- Physical Examination of UrineDocument4 paginiPhysical Examination of UrineIceÎncă nu există evaluări
- Lec 1 - IntroductionDocument3 paginiLec 1 - IntroductionHaendra Mae DapilagaÎncă nu există evaluări
- ConnectivetissuepptDocument20 paginiConnectivetissuepptChicco De AngelisÎncă nu există evaluări
- Red Blood Cell Anomalies: Elliptocytes & Oval MacrocyteDocument12 paginiRed Blood Cell Anomalies: Elliptocytes & Oval MacrocyteSHUPATUSSAI100% (1)
- Non Protein CompoundsDocument64 paginiNon Protein CompoundsAbigail Mayled LausÎncă nu există evaluări
- Par201 S1lab4 Midterm Phamids Aphasmids PDFDocument27 paginiPar201 S1lab4 Midterm Phamids Aphasmids PDFHanna Alyssa Grace DimarananÎncă nu există evaluări
- AUBF P1 Examination Questions (1-8Document39 paginiAUBF P1 Examination Questions (1-8Charmaine BoloÎncă nu există evaluări
- 3 Chemical Examination of UrineDocument82 pagini3 Chemical Examination of UrineJake Real Dela RocaÎncă nu există evaluări
- Microscopic Examination of UrineDocument4 paginiMicroscopic Examination of UrineGlaiza Erika Baes GudaÎncă nu există evaluări
- Urinalysis 1: Mr. Arian Ray E. MalintadDocument55 paginiUrinalysis 1: Mr. Arian Ray E. MalintadAbraham DemeterioÎncă nu există evaluări
- Intro To ImmunohematoDocument48 paginiIntro To Immunohematojong188Încă nu există evaluări
- COMPLETE BLOOD COUNT Lecture GuideDocument9 paginiCOMPLETE BLOOD COUNT Lecture GuideKaycee Gretz LorescaÎncă nu există evaluări
- Subcutaneous & Systemic MycosesDocument7 paginiSubcutaneous & Systemic MycosesDee GeeÎncă nu există evaluări
- Foundations in Microbiology: Nonspecific Host Defenses TalaroDocument35 paginiFoundations in Microbiology: Nonspecific Host Defenses TalaroOdurÎncă nu există evaluări
- Specimen Considerations (Part 2)Document8 paginiSpecimen Considerations (Part 2)Race MendezÎncă nu există evaluări
- Diagnostic Microbiology - : University of Santo Tomas - Medical TechnologyDocument6 paginiDiagnostic Microbiology - : University of Santo Tomas - Medical TechnologyWynlor AbarcaÎncă nu există evaluări
- Lesson 5: Nature of The Clinical LaboratoryDocument8 paginiLesson 5: Nature of The Clinical LaboratoryJohn Daniel AriasÎncă nu există evaluări
- Compre-Quiz For MedtechDocument18 paginiCompre-Quiz For MedtechynaellyÎncă nu există evaluări
- Test Bank Exam 3Document81 paginiTest Bank Exam 3Sajjad AhmadÎncă nu există evaluări
- AmoebaDocument5 paginiAmoebasarguss14Încă nu există evaluări
- Diagnostic Microbiology: CampylobacterDocument25 paginiDiagnostic Microbiology: Campylobacteranon_914901469Încă nu există evaluări
- Introduction To Hematology 2Document15 paginiIntroduction To Hematology 2Tom Anthony TonguiaÎncă nu există evaluări
- Amoeba ChartDocument4 paginiAmoeba ChartRafael CastilloÎncă nu există evaluări
- Family Neisseriaceae: Joy P. Calayo, RMT, MSMT UST Faculty of Pharmacy Dept. of Medical TechnologyDocument18 paginiFamily Neisseriaceae: Joy P. Calayo, RMT, MSMT UST Faculty of Pharmacy Dept. of Medical Technologypixholic100% (1)
- Why Is A Prothrombin Time Test Performed?: WarfarinDocument6 paginiWhy Is A Prothrombin Time Test Performed?: WarfarinMamta ShindeÎncă nu există evaluări
- HaematologyDocument68 paginiHaematologytapoolnoÎncă nu există evaluări
- Lesson 3Document71 paginiLesson 3Angel joyce ValenciaÎncă nu există evaluări
- Summary of Reagent Strip TestsDocument8 paginiSummary of Reagent Strip TestsDarla YsavelÎncă nu există evaluări
- Coagulation OverviewDocument12 paginiCoagulation Overviewkriss WongÎncă nu există evaluări
- Reviewbasic 130709233435 Phpapp02Document130 paginiReviewbasic 130709233435 Phpapp02Andi Namirah100% (1)
- Studying Fungi Methods Lab DiagnosisDocument74 paginiStudying Fungi Methods Lab DiagnosisKaycee Gretz LorescaÎncă nu există evaluări
- Basic Clinical Chemistry TestsDocument49 paginiBasic Clinical Chemistry TestsMegbaru100% (1)
- CC Reinforcement and Mastery Sessions 1Document16 paginiCC Reinforcement and Mastery Sessions 1Anne MorenoÎncă nu există evaluări
- Assessment Exam in Cc2and3Document7 paginiAssessment Exam in Cc2and3mika de guzmanÎncă nu există evaluări
- (CLINPATH) Lipids and DyslipoproteinemiaDocument5 pagini(CLINPATH) Lipids and DyslipoproteinemiaJolaine ValloÎncă nu există evaluări
- C19 2 Hemopoiesis Eythropoiesis LeukopoiesisDocument11 paginiC19 2 Hemopoiesis Eythropoiesis Leukopoiesisnurul azisyah auraÎncă nu există evaluări
- Aubf Outline EditedDocument16 paginiAubf Outline EditedNoraine Princess TabangcoraÎncă nu există evaluări
- Chapter 1: Introduction To Urinalysis: Urine CompositionDocument74 paginiChapter 1: Introduction To Urinalysis: Urine CompositionMegumi TadokoroÎncă nu există evaluări
- Entamoeba SPPDocument21 paginiEntamoeba SPPragnabulletinÎncă nu există evaluări
- 1 Antigens and AntibodiesDocument31 pagini1 Antigens and AntibodiesJohn Louis RanetÎncă nu există evaluări
- Capillary Fragility/ Resistance Test: Tourniquet or Rumpel-Leede or Hess TestDocument4 paginiCapillary Fragility/ Resistance Test: Tourniquet or Rumpel-Leede or Hess TestGerly MaglangitÎncă nu există evaluări
- Mycobacteria: Nocardia, Rhodococcus, Tsukamurella and GordoniaDocument7 paginiMycobacteria: Nocardia, Rhodococcus, Tsukamurella and Gordonia20C – Gorospe, Rhai Chezka V.Încă nu există evaluări
- Serological TestsDocument2 paginiSerological TestsKimberly EspaldonÎncă nu există evaluări
- Pharma Unit 1-2 Anti - Adrenergic DrugsDocument21 paginiPharma Unit 1-2 Anti - Adrenergic DrugsMIbrahimÎncă nu există evaluări
- Rickettsial Diseases: DR Sajan Christopher Assistant Professor of Medicine Medical College, ThiruvananthapuramDocument40 paginiRickettsial Diseases: DR Sajan Christopher Assistant Professor of Medicine Medical College, ThiruvananthapuramYogya MandaliÎncă nu există evaluări
- Bacteriology Laboratory OrganizationDocument65 paginiBacteriology Laboratory Organizationtummalapalli venkateswara rao100% (1)
- Aubf Lec (2 Week) Physical Examination of Urine: Color, Clarity Specific GravityDocument38 paginiAubf Lec (2 Week) Physical Examination of Urine: Color, Clarity Specific GravityAngela ReyesÎncă nu există evaluări
- Blood Collection VialsDocument26 paginiBlood Collection VialsMunizah MunirÎncă nu există evaluări
- CLINICAL CHEMISTRY: Passbooks Study GuideDe la EverandCLINICAL CHEMISTRY: Passbooks Study GuideÎncă nu există evaluări
- Problem-based Approach to Gastroenterology and HepatologyDe la EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisÎncă nu există evaluări
- Senior Medical Laboratory Technician: Passbooks Study GuideDe la EverandSenior Medical Laboratory Technician: Passbooks Study GuideÎncă nu există evaluări
- TOFDocument71 paginiTOFViena PetalioÎncă nu există evaluări
- Assessment Nursing Diagnosis Scientific Explanation Planning Implemented Interventions Rationale Evaluation Subjective Cues: Goal: Goal Partially MetDocument3 paginiAssessment Nursing Diagnosis Scientific Explanation Planning Implemented Interventions Rationale Evaluation Subjective Cues: Goal: Goal Partially MetzysheaiÎncă nu există evaluări
- Specialty Practice Series: Best Practices in Nursing Care To Older AdultsDocument2 paginiSpecialty Practice Series: Best Practices in Nursing Care To Older AdultszysheaiÎncă nu există evaluări
- Nosocomial UnfinishedDocument1 paginăNosocomial UnfinishedzysheaiÎncă nu există evaluări
- S.I Assign.Document12 paginiS.I Assign.zysheaiÎncă nu există evaluări
- Sel-ncm-Vasectomy and Tubal LigationDocument5 paginiSel-ncm-Vasectomy and Tubal LigationzysheaiÎncă nu există evaluări
- KEPPRADocument2 paginiKEPPRAzysheaiÎncă nu există evaluări
- Lecture 3. Bleeding Disorders Part 1Document31 paginiLecture 3. Bleeding Disorders Part 1Kekelwa Mutumwenu Snr100% (1)
- Function of FatsDocument14 paginiFunction of FatsPrincess CudalÎncă nu există evaluări
- CSC Dos TestDocument5 paginiCSC Dos TestAnand GaridipuriÎncă nu există evaluări
- Understanding Haemolytic Anaemia (HADocument11 paginiUnderstanding Haemolytic Anaemia (HASonam JoshiÎncă nu există evaluări
- ANSWER SCHEME CHAPTER 1Document24 paginiANSWER SCHEME CHAPTER 1Chen ShyanÎncă nu există evaluări
- Brosur Symex XP-100 PDFDocument4 paginiBrosur Symex XP-100 PDFHari Putra PetirÎncă nu există evaluări
- The Organ Systems of AnimalsDocument28 paginiThe Organ Systems of AnimalsJhoncarlo Balagosa 1stÎncă nu există evaluări
- Asbmt: Clinical Guide To ABO-Incompatible Allogeneic Stem Cell TransplantationDocument7 paginiAsbmt: Clinical Guide To ABO-Incompatible Allogeneic Stem Cell TransplantationMohana ReddyÎncă nu există evaluări
- Chapter 11: Transportation in Animals and Plants Science: Page No: 131Document4 paginiChapter 11: Transportation in Animals and Plants Science: Page No: 131Shreyas NairÎncă nu există evaluări
- Anemia Prenatal Care - DR - Rima IrwindaDocument43 paginiAnemia Prenatal Care - DR - Rima IrwindaHari SandiÎncă nu există evaluări
- ROTEM Delta and Platelet en 2016 V01 1Document8 paginiROTEM Delta and Platelet en 2016 V01 1asankandessÎncă nu există evaluări
- PallorDocument16 paginiPallorManal AlQuaimi100% (1)
- Chapter1-The Clinical LabDocument24 paginiChapter1-The Clinical LabNawra AhmadÎncă nu există evaluări
- Research Proposal 2Document29 paginiResearch Proposal 2nickos navajaÎncă nu există evaluări
- Up To Date LMMCDocument23 paginiUp To Date LMMCLuciano LaranjeiraÎncă nu există evaluări
- About Myelodysplastic Syndromes: Overview and TypesDocument12 paginiAbout Myelodysplastic Syndromes: Overview and TypesAulya ArchuletaÎncă nu există evaluări
- Amino acids join to form polypeptide chainsDocument3 paginiAmino acids join to form polypeptide chainsnabilahÎncă nu există evaluări
- Blood Type Review WorksheetDocument2 paginiBlood Type Review WorksheetSofa100% (2)
- Reviewer in Phleb 102 (Week 2)Document6 paginiReviewer in Phleb 102 (Week 2)Hannah Viktoria HernandezÎncă nu există evaluări
- OUS Siemens Healthineers Sysmex CA 600 Systems Brochure 10 2022Document8 paginiOUS Siemens Healthineers Sysmex CA 600 Systems Brochure 10 2022A9 El-EbidiÎncă nu există evaluări
- Scalar Energy PendantDocument12 paginiScalar Energy PendantNicole WeatherleyÎncă nu există evaluări
- 3 A Specific Antidote For Reversal of Anticoagulation byDocument8 pagini3 A Specific Antidote For Reversal of Anticoagulation byBhanuÎncă nu există evaluări
- Direct Oral Anticoagulants From Pharmacology To Clinical PracticeDocument283 paginiDirect Oral Anticoagulants From Pharmacology To Clinical PracticesunhaolanÎncă nu există evaluări
- ModifiedPrinciplesofHaematologyLabManual Fall2016 PDFDocument59 paginiModifiedPrinciplesofHaematologyLabManual Fall2016 PDFGwenÎncă nu există evaluări
- 12 Tissue Remedies of Shcussler by Boerick.Document432 pagini12 Tissue Remedies of Shcussler by Boerick.scientist786100% (7)
- SCD and Hydroxyurea TherapyDocument29 paginiSCD and Hydroxyurea Therapysamuel waiswaÎncă nu există evaluări
- Normal Blood Test Values and Coagulation Tests ExplainedDocument1 paginăNormal Blood Test Values and Coagulation Tests Explainedczeremar chanÎncă nu există evaluări
- Doctor of Veterinary Medicine: Scheme of Study of Five Years Composit Degree ProgrammeDocument62 paginiDoctor of Veterinary Medicine: Scheme of Study of Five Years Composit Degree ProgrammeAhmed Hassan SamatarÎncă nu există evaluări
- Other Blood Group SystemDocument42 paginiOther Blood Group SystemCarla May Orange GualbertoÎncă nu există evaluări
- 0610 w02 QP 1Document20 pagini0610 w02 QP 1LuckÎncă nu există evaluări