Documente Academic
Documente Profesional
Documente Cultură
Sub Clinical Thyroid Disease
Încărcat de
Yeon Ae NaritaDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Sub Clinical Thyroid Disease
Încărcat de
Yeon Ae NaritaDrepturi de autor:
Formate disponibile
I n v i t e d
R e v i e w
Singapore Med J 2003 Vol 44(11) : 595-600
Subclinical Thyroid Disease
P C Kek, S C Ho, D H Khoo
Thyroid disease is common and may present to a wide range of doctors. With the advent of serum thyrotropin (TSH) radioimmunoassay in the 1970s, the entity of mildly elevated TSH and normal serum thyroid hormones levels was recognised, the introduction of the second and third generation sensitive TSH in the 1980s identified the entity of subclinical hyperthyroidism in which serum TSH is suppressed and serum thyroxine T4 and triiodothyronine T3 levels are normal(1). Controversy centers on whether early treatment or close follow-up is warranted in apparently healthy persons in whom the only indication of a thyroid disorder is an abnormal test result. We will summarise the existing epidemiological and clinical data on subclincal hyperthyroidism and hypothyroidism and discuss the rationale of management. SUBCLINCAL HYPERTHYROIDISM Subclinical hyperthyroidism is defined as a persistently suppressed serum TSH with normal thyroxine and triiodothyronine in patients who do not have symptoms. Subclinical hyperthyroidism can be caused by the same thyroid disorders that result in clinical hyperthyroidism. Suppressed TSH levels may occasionally result from non-thyroidal causes (Table I(2,3)). The most common cause of subclinical hyperthyroidism is excessive thyroid hormone therapy.
Department of Endocrinology Singapore General Hospital Outram Road Singapore 169608 P C Kek, MBBS, MRCP (UK) Registrar S C Ho, MBBS, MMed, MRCP Consultant D H Khoo, MBBS, MMed, FRCP (Ed) Senior Consultant Correspondence to: Dr D H Khoo Tel: (65) 6321 4654 Fax: (65) 6227 3576 Email: geckhc@ sgh.com.sg
Survey(4) and 12% in the Framingham study(5). More recently, the Colorado Thyroid Disease Prevalence Study involving 25,862 subjects showed a prevalence of 2.1%(6). Joseph et al studied a representative population of 17,353 people aged 12 and above and found that the prevalence of subclinical hyperthyroidism was only 0.7%(7). The precise pathophysiology and natural history of subclinical hyperthyroidism are unknown. In the Whickham Survey where 2,779 subjects were followed up for 20 years, the incidence of hyperthyroidism in the surviving women was 3.9% and the calculated incidence rate was only 0.8/1,000/year(8). The initial TSH level also appears to influence outcome. Subclinical hyperthyroid subjects with initial suppressed but detectable TSH levels tend to return to normal on follow-up while those with undetectable TSH remained unchanged with a small risk of progression to frank hyperthyroidism(9). The rate of progression to overt hyperthyroidism has been estimated to be 5% per year with subjects with autonomous thyroid adenoma and nodular goiter(10). Therefore, the likelihood of progression of subclincal hyperthyroidism to overt hyperthyroidism is small. CLINICAL IMPLICATIONS Increasingly, it is recognised that subclinical hyperthyroidism is not merely a biochemical abnormality dissociated from the clinical manifestations and sequelae of thyrotoxicosis. In fact, clinical features of thyrotoxicosis can be identified in subclinical hyperthyroidism albeit of insufficient severity to cause major symptoms. The clinical significance of subclinical hyperthyroidism thus relates to three risk factors: (1) progression to overt hyperthyroidism, (2) cardiac effects, and (3) skeletal effects. CARDIAC EFFECTS The data on cardiac effects of subclinical hyperthyroidism come largely from studies of patients on L-T4 suppresive therapy. A study on 20 patients receiving oral L-T4 to suppress TSH secretion for a period of one to nine years showed a number of significant
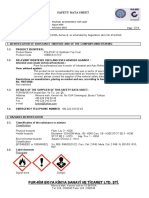
Table 1 Endogenous thyroid conditions Graves disease autonomous adenoma multinodular goiter thyroiditis (subacute, silent, autoimmune) euthyroid sick syndrome acute psychiatric disease pituitary and hypothalamic disorders pregnancy drugs: thyroxine, dopamine, glucocorticoids, aspirin, fenclofenac, furosemide
Non-thyroidal conditions
PREVALENCE AND NATURAL HISTORY The prevalence of subclinical hyperthyroidism varies amongst the reports. Prevalence of subclinical hyperthyroidism was reported to be 10% in Whickham
Singapore Med J 2003 Vol 44(11) : 596
cardiovascular changes: 1) increased heart rate, 2) increased incidence of atrial arrhythmia such as atrial premature beats, 3) increased left ventricular mass, left ventricular posterior wall and interventricular septal thickness, and 4) enhanced left ventricular systolic function(11). Some of these effects such as heart rate, arrhythmia, cardiac wall thickness can be reduced with addition of -blocker which result in amelioration of symptoms such as palpitations, nervousness, tremor, heat intolerance and sweating(12). These findings show that many patients taking L-T4 at suppressive doses complain of symptoms similar to those present in hyperthyroid patients, which, even if of minor importance, contribute to their poor quality of life. The beneficial effect of -blockade was further confirmed in a study by Fazio et al(13) which also found that there was significant prolongation of isovolumic relaxation time, suggestive of impaired diastolic function. This was significantly reduced by -blockade. Long-term thyrotropin suppressive therapy with levothyroxine also adversely affect cardiac reserve and exercise capacity. Biondi et al found that the maximal exercise capacity was markedly impaired in all patients, with significant reduction in peak workload and exercise duration. The left ventricular ejection fraction fell markedly during exercise, due to changes in the endsystolic left ventricular volume(14). Therefore, long term L-T4 therapy can cause subtle cardiac abnormalities that can be potentially harmful. Attempts at tailoring TSH suppressive dosage showed beneficial effect in individuals on titration dose. These patients had improvement in thyrotoxic scores, echocardiographic parameters and maximal exercise workload(15). These concerns over adverse cardiac effects can be extrapolated to subclinical hyperthyroidism. Patients with endogenous subclinical hyperthyroidism were more symptomatic with higher Symptom Rating Scale scores with higher prevalence of palpitations, nervousness, tremor, heat intolerance, and sweating. Similar to the situtation in suppressive L-T4 therapy, there was significant increased in the average heart rate, prevalence of atrial premature beats, mean interventricular septum and left ventricular posterior wall thickness and left ventricular mass. The left ventricular systolic function was significantly higher in the patients and the isovolumic relaxation time was also significantly prolonged in the patients(16) . Another well-known complication of thyrotoxicosis is atrial fibrillation. Subclinical hyperthyroidism is a risk factor for the development of atrial fibrillation. The strongest evidence emerged from the Framingham Study(17) in which a cohort of 2,007 persons aged 60 years and above was followed up for 10 years.The cumulative incidence of atrial fibrillation over this period was 28% and relative
risk of atrial fibrillation in those with low serum thyrotropin was 3.1. Auer et al also reported a fivefold increased in risk of developing atrial fibrillation in subjects with subclinical hyperthyroidism(18). SKELETAL EFFECTS Most data on skeletal effects of subclinical hyperthyroidism are derived from small, retrospective and non-randomised studies It has been shown thus far that endogenous subclinical hyperthyroidism in the premenopausal period is not associated with increased bone metabolism(19) or a decrease in BMD in the lumbar spine, femeral neck or mid shaft of radius. The situation during the postmenopausal period is more controversial. Foldes et al found significant decrease in the BMD of the lumbar spine, femoral neck and mid-shaft of radium in postmenopausal women(20). Kung et al showed reduction in BMD affecting both cortical and trabecular bones in postmenopausal women taking long term suppressive therapy(21). In contrast, Grant et al showed no significant changes in BMD in another study involving postmenopausal patients(22). A meta-analysis done by Uzzan et al found that thyroid hormone therapy has no effect on bone mass in premenopausal women except in the spine where thyroid hormone had a paradoxical beneficial effect but had a significant detrimental effect at all sites (including spine and femur neck) in postmenopausal women (23). With respect to fracture risk, Bauer et al follow-up 686 women above 65 years of age for a mean of 3.7 years. The authors found a three fold increase in risk of hip fracture among women with low TSH compared to those with normal TSH even after adjustment for age, previous hyperthyroidism, self-rated health, and current use of estrogen. The risk of new vertebrae fracture was also threefold higher with the adjusted relative hazard ratio at 4.5. This prospective study showed that those with TSH levels of 0.1mIU/l or less has a significantly increased risk for new hip and vertebral fractures(24). TREATMENT From the results presented above, it can be seen that patients with subclinical hyperthyroidism of exogenous or endogenous origins, are symptomatic. The occurrence of cardiovascular abnormalities in subclinical hyperthyroidism emphasises that subclinical hyperthyroidism should be considered as a mild form of tissue thyrotoxicosis. Parle et al found an increased in mortality from all causes and from circulatory disease in patients with subclinical hyperthyroidism after following a cohort of 1,209 subjects for 10 years(25). Sgarbi et al studied the effect of early antithyroid therapy for endogenous subclinical hyperthyroidism(26).
597 : 2003 Vol 44(11) Singapore Med J
In this study, significant reduction in the heart size was observed six months after treatment with methimazole, accompanied by a significant reduction in the symptomatic score after reaching the euthyroid state. Euthyroid state was related to an improvement of clinical, laboratory, and cardiac parameters. It suggests that early subclinical hyperthyroidism should be considered. In contrast, Yonem et al found no favourable effects of antithyroid treatment on BMD, heart rate and arrhythmia incidence in a young group of patients during a six-month period although there was partial symptomatic relief(27). Faber et al demonstrated that RAI treatment of postmenopausal women with nodular goitre and subclinical hyperthyroidism results in normalisation of TSH levels. Bone mass at both the spine and the hip remains unchanged for at least two years at a time when a decline of about 1-2% per year in bone mass is expected in normal euthyroid women. In contrast, untreated postmenopausal women with nodular goitre and subclincial hyperthyroidism demonstrated continued decline in bone mass of approximately 2% per year(28). This effect had been shown by Mudde et al in 1994 after normalising the subclinical hyperthyroidism with methimazole(29). Treatment of subclinical hyperthyroidism remains controversial, particularly with regard to young and middle-aged people. Young and middle aged patients with untreated subclinical hyperthyroidism are at risk of untoward events: 1. Impaired quality of life. 2. Adverse cardiac effect. 3. Cardiovascular risks, related to onset of overt thyrotoxicosis in heart previously exposed to prolonged periods of subclincial hyperthyroidism. 4. Skeletal diseases as in decrease bone mineral in postmenopausal women and increased risk of fracture. The prognostic significance of increase in left ventricular mass in patients with subclinical hyperthyroidism remains unknown because of lack of epidemiology studies of cardiovascular risk in these patients. However increased left ventricular mass, not necessarily above the hypertrophic threshold, has been found to be associated with increased risk of sudden death in subjects 45 years of age or older(30). The American Association of Clinical Endocrinology had recommended treatment in patients with symptoms of hyperthyroidism, atrial fibrillation, or unexplained weight loss and also women with osteopenia (31) . However, Biondi et al and Sgarbi et al suggested early treatment of persistent endogenous subclinical hyperthyroidism not only in older but also young and middle-age patients to improve their quality of life and avoid the consequences of long-term exposure
of cardiovascular system to small increase in the thyroid hormone. The treatment options include antithyroid drugs or radioactive iodine and surgery. Samuels had proposed that it may be prudent to initiate a trial of antithyroid drug therapy prior to decisions about definitive therapy(32). SUBCLINICAL HYPOTHYROIDISM Subclinical hypothyroidism is the term used to describe patients with normal thyroxine and raised thyroid stimulating hormone concentration who do not have symptoms(1). The findings of slightly elevated TSH and normal thyroid hormone levels do not necessarily imply the presence of subclinical hypothyroidism. Several medications and conditions are known to cause an elevation in TSH. Some drugs such as sulfonyureas, lithium, amiodarone, ethionamide, phenylbutazone, aminoglutethimide, and iodine can interfere with thyroid hormone production or release and secondarily result in a slight elevation of TSH. In addition, dopamine antagonist such as metoclopromide and domperidone may cause exaggerated TSH response to TRH stimulation by altering the inhibitory effect of dopamine on TSH secretion. Furosemide has also been shown to increase levels of TSH, especially in recovering critically ill patients. Other conditions that causes elevated TSH include thyroid hormone resistance, thyroid hormone secreting tumors (both should be associated with high free thyroxine level), psychiatric illness, adrenal insufficiency, renal failure, hyperprolactinemia and systemic illness(33). PREVALENCE AND NATURAL HISTORY Large population studies have suggested that the prevalence of subclinical hypothyroidism is much higher in women than men and increases with age. In the Whickham survey, TSH levels above 6mIU/l were approximately three times more common in females (7.5%) than in males (2.8%) and occurred more frequently in females over 45 years of age. TSH levels also showed a progressive increase with age in women but not in men(4). The prevalence of subclinical hypothyroidism varies from 4.3-9% (6,7). The local prevalence is estimated at 6.5% in a study on 75 subjects admitted to a geriatric ward in a restructured hospital(34). There is also a strong association between positive antithyroid antibodies and elevated TSH. Generally the prevalence of elevated TSH levels parallels that of antibody positivity(4). A high prevalence of antibodies was found in a UK study where antibodies were present in 81% of those with TSH concentration over 10 mU/l, 46% of those with TSH over 5 mU/l and less than or equal to 10 mU/l and only in 5.7% of those whose TSH concentration was less than
Singapore Med J 2003 Vol 44(11) : 598
0.5 mU/l(9). Interestingly, the NHANES III survey found a significant association between anti-thyroid peroxidase antibody with hypo- or hyperthyroidism but not thyroglobulin antibody(7). After 20 years of follow-up of subjects in the Whickham Survey, the risk of overt hypothyroidism was found to be 4.3% per year in women with elevated TSH and antithyroid antibodies at baseline. This is a 38 times increased risk over normal women Moreover, an isolated elevation in TSH or presence of antithyroid antibodies alone at baseline also conferred an increased risk of overt hypothyroidism (2.6% per year and 2.1% per year respectively)(8). Progression to hypothyroidism was noted to be more common in those with initial TSH value greater than 10 mU/l and in those with positive anti-thyroid antibodies(9). Huber et al found that basal TSH, thyroid reserve (increase in T3 after TRH stimulation) and the presence of antimicrosomal antibody are important prognostic factors for the development of overt hypothyroidism. Interestingly, antibodies against thyroglobulin did not have a predictive value(35). CLINICAL IMPLICATIONS The potential benefits and risks of therapy for subclinical hypothyroidism have been debated for two decades. The possible advantages of treating subclinical hypothyroidism generally include, firstly, preventing the progression to overt hypothyroidism. Secondly, thyroxine therapy may improve the serum lipid profile and thereby potentially decrease the risk of death from cardiovascular causes. Finally, treatment may reverse the symptoms of mild hypothyroidism, including psychiatric and cognitive abnormalities(36). EFFECTS ON SERUM LIPID LEVELS The relationship between mild thyroid failure and reversible elevation in serum lipid levels has been widely investigated, but the findings remain controversial. Several cross-sectional studies suggest that serum cholesterol concentrations are elevated in individuals with mild thyroid failure when compared with euthyroid controls (37,38). In other similar studies, however, the observed differences between euthyroid and mild hypothyroid individuals have not been significant(39,40). The Colorado study which screened 25,862 subjects found that mean total cholesterol and low density lipoprotein cholesterol progressively increased with increasing serum TSH levels(6). A reanalysis by Tanis et al in 1996 found that subclinical hypothyroidism was two to three times more frequent in people with elevated total plasma cholesterol. Thyroid substitution therapy restoring the TSH levels to normal decreased total cholesterol by 0.2 to 0.4 mmol/l(41) and mean LDL
cholesterol by 0.26mmol/l and increased in HDL cholesterol by 0.08 mmol/l(41,42) while triglycerides, and apolipoprotein AI levels remained unchanged(43). In another study, total cholesterol and LDL cholesterol levels decreased only in pretreatment TSH values greater than 10 mU/l(44). The decrease in total cholesterol and LDL levels with pretreatment TSH values greater than 40 mU/l was greater than in those levels between 10 and 40 mU/l(45). CARDIAC EFFECTS Cardiac changes are evident in subclinical hypothyroidism. These include impairment of left ventricular diastolic function at rest (affecting the relaxation of the left ventricle and hence ventricular filling), reduced LV systolic function, prologation of pre-ejection time and lastly, impaired intrinsic myocardial contractility(46-49). There is evidence that these abnormalities improve with L-T4 treatment, demonstrating that adequate thyroid replacement improves cardiac output accompanied by substantial decrease in systemic vascular resistance, a reversal of diastolic dysfunction, and importantly an improvement in left ventricular ejection fraction during exercise(46-48,50). It has been demonstrated in the Rotterdam Study that subclinical hypothyroidism is a strong indicator risk for atherosclerosis and myocardial infarction(51). Inadequately treated hypothyroidism has also been demonstrated to have angiographic evidence of coronary atherosclerosis progression(52). Impairment of endothelium-dependent vasodilatation, a harbinger of atherosclerosis, has also been detected in patients with subclinical hypothyroidism(53) which can be reversed by levothyroxine supplementation(54). In view of clear structural and biological cardiovascular risks associated with the presence of subclinical hypothyroidism, treatment of this condition would be expected to provide protection against the development of cardiovascular disease, although there have been no long term outcome studies published to date. SOMATIC AND NEUROMUSCULAR EFFECTS Patients with subclinical hypothyroidism can have subtle clinical manifestations and non-specific symptomatology such as dry skin, cold intolerance, constipation, and easy fatigability (55). In addition, patients with muscular symptoms have mitochondrial oxidative dysfunction with significant lactate increment during exercise(56). Misiunas et al also demonstrated the presence of subclinical polyneuropathy of probable axonal origin in patients with subclinical hypothyroidism(57). Subclinical hypothyroid subjects reported significantly more total symptoms than euthyroid individual in the Colarado study(6) and these symptoms do improve with
599 : 2003 Vol 44(11) Singapore Med J
L-T4 therapy. The greatest improvement seen is of patients with baseline TSH of >12 mU/l (43). Kong et al observed no improvement in symptoms score after trial of thyroxine for six months in patients with TSH level between 5 and 10 mU/l(58). Prospective studies suggest that patients with mild thyroid failure have a higher prevalence of somatic symptoms, mood disorders, cognitive dysfunction, and atypical responses to standard psychiatric therapeutic interventions(59). The lifetime frequency of depression is significantly higher in patients with subclinical hypothyroidism compared with patients with normal thyroid function, suggesting that subclinical hypothyroidism lowers the threshold for depression(53). TREATMENT To date, there is still no consensus regarding the treatment of subclinical hypothyroidism. Evidence seems to indicate that subclinical hypothyroidism represent the mildest form of thyroid hormone deficiency and may be associated with adverse consequences. Some authors have taken the approach of treating patients with subclinical hypothyroidism with view to overall symptomatic improvement, lowering effect of lipoprotein fractions and prevention of progression of cardiac abnormalities(33,54,55,60-62) . Others take a more cautious approach(36,59,63-65). Most agree that patients with serum TSH greater 10mU/l should be treated with thyroxine. The AACE has recommended treatment in patients with TSH levels between 5 and 10 mU/l in conjunction with a goitre or positive anti-thyroid peroxidase antibodies or both and also in the presence of symptoms. If the patients are antibody negative and TSH levels are between 5 and 10 mU/l, then an annual check of serum TSH is recommended, with commencement of T4 once the serum TSH rises above 10 mU/l. The goal of the therapy is to maintain TSH levels within the normal biological range and usually a small dose of levothyroxine is sufficient. Special caution should be exercised in patients with ischemic heart disease. In these cases, a more conservative approach to starting therapy is indicated to prevent dysrhythmias, worsening angina, or even precipitation of myocardial infarction. REFERENCES
1. Vanderpump MPJ, Ahlquist JAO, Franklynm JA, Clayton RN. Consensus statement for good practice and audit measures in the management of hypothyroidism and hyperthyroidism. BMJ 1996; 313:539-44. 2. Fatourechi V. Subclinical thyroid disease. Mayo Clin Proc 2001; 76:413-7. 3. Surks, Martin I, Ocampo, Enrico. Subclinical thyroid disease. American Journal of Medicine 1996; 100(2):217-23. 4. Wang C, Crapo LM. The epidemiology of thyroid disease and implications for screening. Endocrinology and Metabolism Clinics 1997; 26(1):189-218.
5. Utiger RD. Subclinical hyperthyroidism - just as low serum thyrotropin concentration, or something more? N Engl J Med 1994; 331:1302-3. 6. Canaris GJ, Manowitz NR, Mayor G, Ridgway C. The Colorado Thyroid Disease Prevalence Study. Arch Intern Med 2000; 160:526-34. 7. Hollowell JG, Staehing NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, Braverman LE. Serum TSH, T4, and thyroid antibodies in the United States Population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 2002; 87(2):489-99. 8. Vanderpump MPJ, Tunbridge WMG, French JM, Appleton D, Bates D, Clark F, Grimley Evans J, Hasan DM, Rodgers H, Tunbridge F, Young ET. The incidence of thyroid disorders in the community: a twenty-year follow-up of the Whickham Survey. Clinical Endocrinology 1995; 43:55-68. 9. Parle JV, Franklyn JA, Cross KW, Jones SC, Sheppard MC. Prevalence and follow-up of abnormal thyrotropin(TSH) concentrations in the elderly in the United Kingdom. Clinical Endocrinology 1991; 34:77-83. 10. Wiersinga WM. Subclinical hypothyroidism and hyperthyroidism. I. Prevalence and clinical relevance. Neth J Med 1995; 46(4):197-204. 11. Biondi B, Fazio S, Carbella C, Amato G, Cittadini A, Lupoli G, Sacca L, Bellastella A, Lomardi G. Cardiac Effects of Long Term Thyrotropin-Suppressive Therapy with Levothyroxine. J Clin Endocrinol Metab 1993; 77:334-8. 12. Biondi B, Fazio S, Carbella C, Sabatini D, Amato G, Cittadini A, Bellastella A, Lomardi G, Sacca L. Control of adrenergic overactivity by -blockage improves the quality of life in patients receiving long term suppressive therapy with levothyroxine. J Clin Endocrinol Metab 1994; 78:1028-33. 13. Fazio S, Biondi B, Carbella C, Sabatini D, Cittadini A, Panza N, Lomardi G, Sacca L. Diastolic dysfunction in patients on ThyroidStimulating Hormone Suppressive Therapy with Levothyroxine: beneficial effect of -blockade. J Clin Endocrinol Metab 1995; 80:2222-6. 14. Biondi B, Fazio S, Cuocolo A, Sabatini D, Nicolai E, Lombardi G, Salvatore M, Sacca L. Impaired cardiac reserve and exercise capacity in patients receiving long-term thyrotropin suppressive therapy with levothyroxine. J Clin Endodrinol Metab 1996; 81:4224-8. 15. Mercuro G, Panzuto MG, Bina A, Leo M, Cabula R, Petrini L, Pigliaru F, Mariotti S. Cardiac function, physical exercise capacity, and quality of life during long-term thyrotropin-suppressive therapy with levothyroxine: effect of individual dose tailoring. J Clin Endodrinol Metab 2000; 85:159-64. 16. Biondi B, Palmieri EA, Fazio S, Cosco C, Nocera M, Sacca L, Filetti S, Lombardi G, Perticone F. Endogenous subclinical hyperthyroidism affects quality of life and cardiac morphology and function in young and middle-aged patients. J Clin Endodrinol Metab 2000; 85:4701-5. 17. Sawin CT, Geller A, Wolf PA, Belanger AJ, Baker E, Bacharach P, Wilson P, Benjamin EJ, Agostino RBD. Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. N Engl J Med 1994; 331:1249-52. 18. Auer J, Scheibner P, Mische T, Langsteger W, Eber O, Eber B. Subclinical hyperthyroidism as a risk factor for atrial fibrillation. American Heart Journal 2001; 142:838-42. 19. Gurlek A, Gedik O. Effect of endogenous subclinical hyperthyroidism on bone metabolism and bone mineral density in premenopausal women. Thyroid 1999; 9(6):539-43. 20. Foldes J, Tarjan G, Szathmari M, Varga F, Krasznal I, Horvath Cs. Bone mineral density in patients with endogenous subclinical hyperthyroidism: Is this thyroid status a risk factor for osteoporosis? Clinical Endocrinology 1993; 39:521-7. 21. Kung AWC, Lorentz T, Tam SCF. Thyroxine suppressive therapy decreases bone mineral density in post-menopausal women. Clinical endocrinology 1993; 39:535-40. 22. Grant DJ, McMurdo MET, Mole PA, Paterson CR, Davies RR. Suppressed TSH levels secondary to thyroxine replacement therapy are not associated with osteoporosis. Clinical endocrinology 1993; 39:529-33. 23. Uzzan B, Campos J, Cucherat M, Nony P, Boissel JP, Perret GY. Effects on bone mass of long term treatment with thyroid hormones: a meta-analysis. J Clin Endodrinol Metab 1996; 81:4278-89. 24. Bauer DC, Ettinger B, Nevitt MC, Stone KL. Risk of fracture in women with low serum levels of thyroid stimulating hormone. Ann Intern Med 2001; 134:561-8.
Singapore Med J 2003 Vol 44(11) : 600
25. Parle JV, Maisonneuve P, Sheppard MC, Boyle P, Franklyn JA. Prediction of all-cause and cardiovascular mortality in elderly people from one low serum thyrotropin result: a 10 year cohort study. Lancet 2001; 358:861-5. 26. Sgarbi JA, Villaca FG, Garbeline B, Villar HE, Romaldini JH. The effects of early antithyroid therapy for endogenous subclinical hyperthyroidism in clinical and heart abnormalities. J Clin Endodrinol Metab 2003; 88:1672-7. 27. Yonem O, Dokmetas HS, Aslan SM, Erselcan T. Is antithyroid treatment really relevant for young patients with subclinical hyperthyroidism? Endocrine Journal 2002; 49(3):307-14. 28. Faber J, Jensen IW, Peterson L, Nygaard B, Hegedus L, Sierbaek-Nielsen K. Normalization of serum thyrotropin by means of radioiodine treatment in subclinical hyperthyroidism: effect on bone loss n postmenopausal women. Clinical Endocrinology 1998; 48:285-90. 29. Mudde AH, Houben AJ, Nieuwenhuijzen Kruseman AC. Bone metabolism during anti-thyroid drug treatment of endogenous subclinical hyperthyroidism. Clinical Endocrinology 1994; 41:421-4. 30. Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med 1990; 322:1561-6. 31. AACE Thyroid Task Force. Amercian Association of Clinical Endocrinologists medical guidelines for clinical practice for the evaluation and treatment of hyperthyroidism and hypothyroidism. Endocrine Practice 2002; 8(6):457-69. 32. Samuels MH. Subclinical thyroid disease in the elderly. Thyroid 1998; 8(9):803-13. 33. Arem R, Escalante D. Subclinical hypothyroidism: epidemiology, diagnosis, and significance. Advances in Internal Medicine 1996; 41:213-50. 34. Chuo AML, Lim JKH. Thyroid dysfunction in elderly patients. Ann Acad Med Singapore 2003; 32:96-100. 35. Huber G, Staub JJ, Meier C, Mitrache C, Guglielmetti M, Huber P, Braveman LE. Prospective study of the spontaneous course of subclinical hypothyroidism: prognostic value of thyrotropin, thyroid reserve, and thyroid antibodies. J Clin Endodrinol Metab 2002; 87(7):3221-6. 36. Cooper DS. Subclinical hypothyoidism. N Engl J Med 2001; 345:260-5. 37. Bauer DC, Ettinger B, Browner WS. Thyroid function and serum lipids in older women: A population based study. Am J Med 1998; 104:546-51. 38. Kung AWC, Pang RWC, Janus ED. Elevated serum lipoprotein(a) in subclinical hypothyroidism. Clin Endocrinology 43:445-9. 39. Geul KW, ILL van Sluisveld, Grobbee DE, Docter R, AM de Bruyn, Hooykaas H, JP van der Merwe, AM van Hermert, Krenning EP, Hennemann G, Weber RFA. The importance of thyroid microsomal antibodies in the development of elevated serum TSH in middle-aged women: association with serum lipids. Clin Endocrinology 1993; 275-80. 40. Parle JV, Franklyn JA, Cross KW, Jones SR, Sheppard MC. Circulating lipids and minor abnormalities of thyroid function. Clin Endocrinology 1992; 37:411-4. 41. Tanis BC, Westerndrop RGJ, Smelt AM. Effect of thyroid substitution on hypercholesterolaemia in patients with subclinical hypothyroidism: a reanalysis of intervention studies. Clinical Endocrinology 1996; 44:643-9. 42. Danese MD, Ladenson PW, Meinert CL, Powe NR. Effect of thyroxine therapy on serum lipoproteins in patients with mild thyroid failure: a quantitative review of the literature. J Clin Endocrinol Metab 2000; 85:2993-3001. 43. Meier C, Staub JJ, Roth CB, Guglielmetti M, Kunz M, Miserez AR, Drewe J, Huber P, Herzog R, Muller B. TSH-controlled L-thyroxine therapy reduces cholesterol levels and clinical symptoms in subclinical hypothyroidism: a double blind, placebo-controlled trial (Basel Thyroid Study). J Clin Endodrinol Metab 2001; 86:4860-6. 44. Caraccio N, Ferrannini E, Monzani F. Lipoprotein profile in subclinical hypothyroidism: response to levothyroxine replacement, a randomized placebo-controlled study. J Clin Endodrinol Metab 2002; 87:1533-8.
45. Diekman T, Lansberg PJ, Kastein JJ, Wiersinga W. Prevalence and correlation of hypothyroidism in a large cohort of patients referred for dyslipidemia. Arch Intern Med 1995; 155:1490-5. 46. Biondi B, Fazio S, Palmieri EA, Carella C, Panza N, Cittadini A, Bone F, Lombardi G, Saccca L. Left ventricular diastolic dysfunction in patients with subclinical hypothyroidism. J Clin Endodrinol Metab 1999; 84:2064-7. 47. Brento G, Mutti LA, Schnitman M, Fretes O, Perrone A, Matute ML. Assessment of left ventricular diastolic fucntion at rest and exercise in subclinical hypothryoidism, and its response to L-thyroxine therapy. Am J Cardiol 2003; 91:1327-30 48. Monazi F, Bello VD, Caraccio N, Bertini A, Giorgi D, Giusti C, Ferrannini E. Effect of levothyroxine on cardiac function and structure in subclinical hypothyroidism: a double blind, placebo-controlled study. J Clin Endodrinol Metab 2001; 86:1110-5. 49. Vitale G, Galderisi M, Lupoli GA, Celentano A, Pietropaolo I, Parenti N, Divitiis OD, Lupoli G. Left ventricular myocardial impairment in subclinical hypothyroidism assessed by a new ultrasound tool: pulsed tissue doppler. J Clin Endodrinol Metab 2002; 87:4350-5. 50. Kahaly GJ. Cardiovascular and atherogenic aspects of subclinical hypothyroidism. Thyroid 2000; 10(8):665-79. 51. Hak AE, Pols HAP, Visser TJ, Drexhage HA, Hofman A, Witteman JCM. Subclinical hypothyroidism is an independent risk factor for atherosclerosis and myocardial infarction in elderly women: the Rotterdam Study. Ann Intern Med 2000; 132:270-8. 52. Perk M, O Neill BJ. The effect of hormone therapy on angiographic coronary artery disease progression. Cand J Cardiol 1997; 13:273-6. 53. Lekais J, Papamichael C, Alevizaki M, Piperingos G, Marafelia P, Mantozs J, Stamatelopoulos S, Koutras DA. Flow-mediated, endothelium-dependent vasodilatation is impaired in sujects with hypothyroidism, borderline hypothyroidism, and high normal serum thyrotropin (TSH) values. Thyroid 1997; 7(3):411-4. 54. Taddei S, Caraccio N, Virdis A, Dardano A, Versari D, Ghiadoni L, Salvetti A, Ferrannini E, Monzani F. Impaired endothelium-dependent vasodilatation in subclinical hypothyroidism: beneficial effect of levothyroxine therapy. J Clin Endodrinol Metab 2003; 88:3731-7. 55. Owen PJD, Lazarus JH. Subclinical hypothyroidism: the case for treatment. Trends in Endocrinology and Metabolism 2003; 14(6):257-61. 56. Monzani F, Caraccio N, Siciliano G, Manca L, Murri L, Ferrannini E. Clinical and biochemical features of muscle dysfunction in subclinical hypothyroidism. J Clin Endodrinol Metab 1997; 82:3315-8. 57. Misiunas A, Niepomniszcze H, Ravera B, Faraj G, Faure E. Peripheral neuropathy in subclinical hypothyroidism. Thyroid 1995; 5(4):283-6. 58. Kong WM, Sheikh MH, Lumb PJ, Freedman DB, Crook M, Dore CJ, Finer N. A six-month randomized trial of thyroxine treatment in women with mild subclincal hypothyroidism. American Journal Med 2002; 112:348-54. 59. Ayala AR, Danese MD, Ladenson PW. Autoimmune thyroid disease: when to treat mild hypothyrodism. Endocrinology and Metabolism Clinics of North America 2000; 29(2):399-415. 60. Ayala AR, Wartofsky L. The case for more aggressive screening and treatment of mild thyroid failure. Cleveland Clinic Journal of Medicine 2002; 69(4):313-20. 61. McDermott MT, Ridgway EC. Subclinical hypothyroidism is mild thyroid failure and should be treated. J Clin Endodrinol Metab 2001; 86(10):4585-90. 62. Biondi B, Palmieri EA, Lombardi G, Fazio S. Subclinical hypothyroidism and cardiac function. Thyroid 2002; 12(6):505-10. 63. Vanderpump M. Subclinical hypothyroidism: the case against treatment. Trends in Endocrinology and Metabolism 2003; 14(6):262-6. 64. Adlin V. Subclinical hypothyroidism: deciding when to treat. American Family Physician 1998; 64(10):1717-24. 65. Chu JW, Crapo LM. The treatment of subclinical hypothyroidism is seldom necessary. J Clin Endodrinol Metab 2001; 86(10):4591-9.
S-ar putea să vă placă și
- Vanderbilt Rating Scale Scoring InstructionsDocument2 paginiVanderbilt Rating Scale Scoring InstructionsYeon Ae Narita100% (2)
- 68rfe IntroductionDocument71 pagini68rfe IntroductionThePokeOne83% (6)
- Adjustment and Impulse Control DisordersDocument19 paginiAdjustment and Impulse Control DisordersArchana50% (4)
- HydrocephalusDocument30 paginiHydrocephalusYeon Ae NaritaÎncă nu există evaluări
- Cytogenectics Reading ListDocument2 paginiCytogenectics Reading ListHassan GillÎncă nu există evaluări
- Public Speaking Skills for Career SuccessDocument7 paginiPublic Speaking Skills for Career SuccessAnish John100% (1)
- Peptan - All About Collagen Booklet-1Document10 paginiPeptan - All About Collagen Booklet-1Danu AhmadÎncă nu există evaluări
- Lim vs. CA DigestDocument2 paginiLim vs. CA Digestsamme1010100% (1)
- Cbydp Draft SK BaracbacDocument13 paginiCbydp Draft SK BaracbacLikey PromiseÎncă nu există evaluări
- Avanto Magnet System Error MessagesDocument21 paginiAvanto Magnet System Error MessagesMuhammad Ahmad75% (4)
- Epidemiological Cutoff Values For Antifungal Susceptibility TestingDocument36 paginiEpidemiological Cutoff Values For Antifungal Susceptibility Testingdadrrui100% (1)
- Effects of subclinical hyperthyroidism on cardiovascular and bone healthDocument9 paginiEffects of subclinical hyperthyroidism on cardiovascular and bone healthDudella Desnani Firman YasinÎncă nu există evaluări
- Approach and Treatment of Thyroid Disorders in the ElderlyDocument14 paginiApproach and Treatment of Thyroid Disorders in the ElderlyJuan ZamoraÎncă nu există evaluări
- Cardiovascular Risks of Subclinical HyperthyroidismDocument8 paginiCardiovascular Risks of Subclinical Hyperthyroidismivan dario hernandez erazoÎncă nu există evaluări
- Management of Subclinical Hyperthyroidism: Special Feature EditorialDocument3 paginiManagement of Subclinical Hyperthyroidism: Special Feature EditorialimorkzoneÎncă nu există evaluări
- Risk HFDocument21 paginiRisk HFTeguh JayaÎncă nu există evaluări
- Cardiovascular Manifestations in Hyperthyroidism: Research ArticleDocument7 paginiCardiovascular Manifestations in Hyperthyroidism: Research Articlenurharyanti darmaningtyasÎncă nu există evaluări
- Association Between Acute Myocardial Infarction, Lipid Profile and Smoking HabitDocument5 paginiAssociation Between Acute Myocardial Infarction, Lipid Profile and Smoking HabitIOSRjournalÎncă nu există evaluări
- Globulin Thyroid Dialy-: TherapyDocument5 paginiGlobulin Thyroid Dialy-: TherapyNurdita KartikaÎncă nu există evaluări
- Hipotiroid SubklinisDocument7 paginiHipotiroid SubklinisAfdhalia Khairunnisa SyammarhanÎncă nu există evaluări
- Thyroid Diseases and Cerebrovascular DiseaseDocument9 paginiThyroid Diseases and Cerebrovascular DiseaseNguyen Minh PhuÎncă nu există evaluări
- Turkish Journal Subclinical HypothyroidismDocument5 paginiTurkish Journal Subclinical HypothyroidismAminaÎncă nu există evaluări
- TSH Suppressive Therapy: An Overview of Long-Term Clinical ConsequencesDocument4 paginiTSH Suppressive Therapy: An Overview of Long-Term Clinical ConsequencescassiolacerdaÎncă nu există evaluări
- Hypothyroidism and Atherosclerosis: Anne R. Cappola Paul W. LadensonDocument7 paginiHypothyroidism and Atherosclerosis: Anne R. Cappola Paul W. LadensonLock ThecodeÎncă nu există evaluări
- Common Variants at Somatostatin Are Significantly A - 2018 - Journal of The AmerDocument20 paginiCommon Variants at Somatostatin Are Significantly A - 2018 - Journal of The AmerSiti Ria RumaisaÎncă nu există evaluări
- Nermine-Thyroid Disorders in Subjects With Down Syndrome An UpdateDocument8 paginiNermine-Thyroid Disorders in Subjects With Down Syndrome An Updatehafidhatul aisyÎncă nu există evaluări
- Association of Dyslipidemia and Ischemic Stroke in Pakistan Institute of Medical SciencesDocument3 paginiAssociation of Dyslipidemia and Ischemic Stroke in Pakistan Institute of Medical SciencesvenniariskiaÎncă nu există evaluări
- Association Between TSH Levels and Metabolic Syndrome in Older AdultsDocument7 paginiAssociation Between TSH Levels and Metabolic Syndrome in Older AdultsAlifia RahmaÎncă nu există evaluări
- Committee Opinion: Hormone Therapy and Heart DiseaseDocument4 paginiCommittee Opinion: Hormone Therapy and Heart DiseaseJim ColverÎncă nu există evaluări
- Hypothyroidism and Serum Ferritin Level in Patients With Major SS ThalassemiaDocument4 paginiHypothyroidism and Serum Ferritin Level in Patients With Major SS ThalassemiaRatu Meutia ArythaÎncă nu există evaluări
- Prevalence of Subclinical and Undiagnosed Overt Hypothyroidismin Habitual AbortionDocument7 paginiPrevalence of Subclinical and Undiagnosed Overt Hypothyroidismin Habitual AbortionIJAR JOURNALÎncă nu există evaluări
- Risks and Benefits of Hormone Replacement TherapyDocument11 paginiRisks and Benefits of Hormone Replacement Therapyosama saeedÎncă nu există evaluări
- Physical Activity, Cardiorespiratory Fitness, and Exercise Training in Primary and Secondary Coronary PreventionDocument12 paginiPhysical Activity, Cardiorespiratory Fitness, and Exercise Training in Primary and Secondary Coronary PreventionoghyeÎncă nu există evaluări
- Risks and Benefits of Hormone Replacement Therapy: The Evidence SpeaksDocument10 paginiRisks and Benefits of Hormone Replacement Therapy: The Evidence SpeaksHAVIZ YUADÎncă nu există evaluări
- Recents Advances in Menopause ManagementDocument134 paginiRecents Advances in Menopause ManagementVania ParamithaÎncă nu există evaluări
- Holtorf K Hormone Replace in Geriatric PT Part 2 (Thyriod Section)Document14 paginiHoltorf K Hormone Replace in Geriatric PT Part 2 (Thyriod Section)kent holtorfÎncă nu există evaluări
- Atherosclerosis and Physical Activity: Ali Al-MamariDocument6 paginiAtherosclerosis and Physical Activity: Ali Al-MamarikeylapireÎncă nu există evaluări
- Hormone Therapy and Cardiovascular DiseaseDocument7 paginiHormone Therapy and Cardiovascular Diseaseosama saeedÎncă nu există evaluări
- Subclinical SubclinicalDocument1 paginăSubclinical Subclinicalyaquelin torres DominguezÎncă nu există evaluări
- LettersDocument1 paginăLettersErika Lisseth Saldarriaga GonzálezÎncă nu există evaluări
- AritmiaDocument9 paginiAritmiaDayuKurnia DewantiÎncă nu există evaluări
- Sleep and HypertensionDocument10 paginiSleep and HypertensionPutraÎncă nu există evaluări
- Clinical Features and Outcomes of Takotsubo Stress Cardiomyopathy NEJMoa1406761Document10 paginiClinical Features and Outcomes of Takotsubo Stress Cardiomyopathy NEJMoa1406761William LeeÎncă nu există evaluări
- NIH Public Access: Author ManuscriptDocument11 paginiNIH Public Access: Author Manuscriptosama saeedÎncă nu există evaluări
- IndianJEndocrMetab177184-6475539 175915Document4 paginiIndianJEndocrMetab177184-6475539 175915Atika SugiartoÎncă nu există evaluări
- Gender and Age Impact On The Association Between.26Document10 paginiGender and Age Impact On The Association Between.26saifulmangopo123Încă nu există evaluări
- Hyperthyroidism ArticlesDocument3 paginiHyperthyroidism ArticlesEd ManzanoÎncă nu există evaluări
- JAMA 1998 Hulley 605 13Document9 paginiJAMA 1998 Hulley 605 13ajflca20034Încă nu există evaluări
- Goiter PDFDocument4 paginiGoiter PDFmol3yÎncă nu există evaluări
- Thyroid Dysfunction and Anaemia in A Large Population-Based StudyDocument5 paginiThyroid Dysfunction and Anaemia in A Large Population-Based StudyRaissa Metasari TantoÎncă nu există evaluări
- Association of Breast Cancer With Thyroid Function and Autoimmunity in Yemeni WomenDocument11 paginiAssociation of Breast Cancer With Thyroid Function and Autoimmunity in Yemeni WomenInternational Journal of Innovative Science and Research TechnologyÎncă nu există evaluări
- Life Extension Magazine: The 10 Most Important Blood TestsDocument5 paginiLife Extension Magazine: The 10 Most Important Blood TestsJaffer AftabÎncă nu există evaluări
- Clinical Implications and Management of Sub Clinical Hyperthyroidism: A ReviewDocument9 paginiClinical Implications and Management of Sub Clinical Hyperthyroidism: A ReviewAdi Putra GhifariÎncă nu există evaluări
- International Journal of Pathology and Clinical Research Ijpcr 4 070Document3 paginiInternational Journal of Pathology and Clinical Research Ijpcr 4 070Psyryst AlladoÎncă nu există evaluări
- Literature Review of ThyroidDocument6 paginiLiterature Review of Thyroidea6z9033100% (1)
- American Thyroid Association Guidelines For Detection of Thyroid DysfunctionDocument5 paginiAmerican Thyroid Association Guidelines For Detection of Thyroid DysfunctionUdsanee SukpimonphanÎncă nu există evaluări
- Subclinical Hyperthyroidism: To Treat or Not To Treat?: Best PracticeDocument5 paginiSubclinical Hyperthyroidism: To Treat or Not To Treat?: Best PracticeRaka MahasaduÎncă nu există evaluări
- Editorial: Now RateDocument6 paginiEditorial: Now RateDinka RoselyÎncă nu există evaluări
- 0120 2448 Amc 44 03 8Document8 pagini0120 2448 Amc 44 03 8Lejla HusicÎncă nu există evaluări
- Orthostatism FinlandDocument8 paginiOrthostatism FinlandAndrea MéndezÎncă nu există evaluări
- Sigalos 2017Document12 paginiSigalos 2017medicinainterna.umaepÎncă nu există evaluări
- Assessment of Overweight and High Blood Pressure Among Individuals in Out - Patient Clinic in A Specialist HospitalDocument3 paginiAssessment of Overweight and High Blood Pressure Among Individuals in Out - Patient Clinic in A Specialist HospitalIOSRjournalÎncă nu există evaluări
- Redfield Margaret M Heart Failure With PreservedDocument12 paginiRedfield Margaret M Heart Failure With PreservedNathan Kulkys MarquesÎncă nu există evaluări
- 2017 Article 215Document11 pagini2017 Article 215pelinÎncă nu există evaluări
- Psychosis British Journal of Cardiac NursingDocument5 paginiPsychosis British Journal of Cardiac NursingOQAB13Încă nu există evaluări
- Tiroides en Critico 2015 LancetDocument10 paginiTiroides en Critico 2015 LancetElias Vera RojasÎncă nu există evaluări
- Selección de Resúmenes de Menopausia Semana Del 22 Al 28 de Octubre de 2014Document3 paginiSelección de Resúmenes de Menopausia Semana Del 22 Al 28 de Octubre de 2014rocksurÎncă nu există evaluări
- 1 PBDocument6 pagini1 PBpelinÎncă nu există evaluări
- Goiter: Signs and Symptoms of GoitersDocument15 paginiGoiter: Signs and Symptoms of GoitersGraceLanaÎncă nu există evaluări
- Revalence of Thyroid Disorders in A Tertiary Care CenterDocument5 paginiRevalence of Thyroid Disorders in A Tertiary Care CenterAvisa Cetta CresmaÎncă nu există evaluări
- Complementary and Alternative Medical Lab Testing Part 4: VascularDe la EverandComplementary and Alternative Medical Lab Testing Part 4: VascularÎncă nu există evaluări
- HD Prescr 2Document52 paginiHD Prescr 2Gerrard Ella100% (2)
- ComplicationDocument3 paginiComplicationYeon Ae NaritaÎncă nu există evaluări
- NAP6 Chapter 12 - Deaths, Cardiac Arrests, Profound Hypotension and OutcomesDocument11 paginiNAP6 Chapter 12 - Deaths, Cardiac Arrests, Profound Hypotension and OutcomesYeon Ae NaritaÎncă nu există evaluări
- Burden of Infection in Patients With End-Stage Renal Disease Requiring Long-Term DialysisDocument7 paginiBurden of Infection in Patients With End-Stage Renal Disease Requiring Long-Term DialysisYeon Ae NaritaÎncă nu există evaluări
- Tuberculosis (TB) Blood Test (IGRA) : Minnesota Department of HealthDocument1 paginăTuberculosis (TB) Blood Test (IGRA) : Minnesota Department of HealthYeon Ae NaritaÎncă nu există evaluări
- L o V eDocument1 paginăL o V eYeon Ae NaritaÎncă nu există evaluări
- DutyDocument1 paginăDutyYeon Ae NaritaÎncă nu există evaluări
- HifemaDocument7 paginiHifemaYeon Ae NaritaÎncă nu există evaluări
- Benign Essential BlepharospasmDocument3 paginiBenign Essential BlepharospasmYeon Ae NaritaÎncă nu există evaluări
- Love UDocument5 paginiLove UYeon Ae NaritaÎncă nu există evaluări
- Follow UpDocument12 paginiFollow UpYeon Ae NaritaÎncă nu există evaluări
- Alcoholic CardiomyopathyDocument10 paginiAlcoholic CardiomyopathyYeon Ae NaritaÎncă nu există evaluări
- Folow Up LapsusDocument7 paginiFolow Up LapsusYeon Ae NaritaÎncă nu există evaluări
- RRC Igc1Document6 paginiRRC Igc1kabirÎncă nu există evaluări
- System Bus in Computer Architecture: Goran Wnis Hama AliDocument34 paginiSystem Bus in Computer Architecture: Goran Wnis Hama AliGoran WnisÎncă nu există evaluări
- Session CommandsDocument1.033 paginiSession Commandshan seongÎncă nu există evaluări
- Participatory Assessment of Ragay Gulf Resources and SocioeconomicsDocument167 paginiParticipatory Assessment of Ragay Gulf Resources and SocioeconomicsCres Dan Jr. BangoyÎncă nu există evaluări
- Polifur 1K Synthetic Top Coat MSDS Rev 2 ENDocument14 paginiPolifur 1K Synthetic Top Coat MSDS Rev 2 ENvictorzy06Încă nu există evaluări
- Rustia V Cfi BatangasDocument2 paginiRustia V Cfi BatangasAllen GrajoÎncă nu există evaluări
- Booklet English 2016Document17 paginiBooklet English 2016Noranita ZakariaÎncă nu există evaluări
- BH Tif03Document21 paginiBH Tif03Andres R. OlguinÎncă nu există evaluări
- School newspaper report teaches Present PerfectDocument2 paginiSchool newspaper report teaches Present PerfectMiro MiroÎncă nu există evaluări
- Film set safety rules for COVIDDocument12 paginiFilm set safety rules for COVIDTanveer HossainÎncă nu există evaluări
- ICS Technical College Prospectus 2024 Edition 1Document36 paginiICS Technical College Prospectus 2024 Edition 1samuel287kalumeÎncă nu există evaluări
- MIL (Second Quarter)Document13 paginiMIL (Second Quarter)Menma ChanÎncă nu există evaluări
- Year 2 - Push and Pull FPDDocument18 paginiYear 2 - Push and Pull FPDRebecca LÎncă nu există evaluări
- Rise of NationalismDocument19 paginiRise of NationalismlolaÎncă nu există evaluări
- Ivf Market in IndiaDocument15 paginiIvf Market in IndiaSunil Tak100% (1)
- RCC Lintel and Slab PlanDocument3 paginiRCC Lintel and Slab PlanSaurabh Parmar 28Încă nu există evaluări
- Bimbo Marketing ResearchDocument27 paginiBimbo Marketing Researcheman.konsouhÎncă nu există evaluări
- 74VHCU04Document6 pagini74VHCU04Alexandre S. CorrêaÎncă nu există evaluări
- Liquid Air Energy Storage Systems A - 2021 - Renewable and Sustainable EnergyDocument12 paginiLiquid Air Energy Storage Systems A - 2021 - Renewable and Sustainable EnergyJosePPMolinaÎncă nu există evaluări
- Newly Constructed Masculinity' in Mahesh Dattani's Dance Like A ManDocument4 paginiNewly Constructed Masculinity' in Mahesh Dattani's Dance Like A ManIJELS Research JournalÎncă nu există evaluări
- Unit 5 Vocabulary Basic 1 Match 1-10 With A-J To Make Innovations and InventionsDocument6 paginiUnit 5 Vocabulary Basic 1 Match 1-10 With A-J To Make Innovations and InventionsCristina Garcia50% (2)