Documente Academic
Documente Profesional
Documente Cultură
Aseptic Meningitis: Diagnosis and Management
Încărcat de
Sandrio UtomoDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Aseptic Meningitis: Diagnosis and Management
Încărcat de
Sandrio UtomoDrepturi de autor:
Formate disponibile
ADVANCES IN PEDIATRICS Year : 2005 | Volume : 72 | Issue : 1 | Page : 57-63
Aseptic meningitis: Diagnosis and management
Kumar Rashmi Department of Pediatrics, King George Medical University, Lucknow, Uttar Pradesh, India Abstract The term aseptic meningitis encompasses all types of inflammations of the brain meninges other than that caused by pus producing organisms. It is usually a benign illness. Etiology of aseptic meningitis is very wide and includes many infections - both viral and non viral, drugs, malignancy and systemic illness. The most common cause is viral infection and enteroviruses - Coxsackie and ECHO viruses account for more than half of all cases. Clinical manifestations include headache, fever, malaise, photophobia and meningeal signs. Convulsions, neurological deficits and severe obtundation are rare except with certain non viral infectious meningitis. Diagnostic work up includes blood and cerebrospinal fluid (CSF) examination and serology for infectious meningitis. The polymerase chain reaction is a rapid and accurate method for detection of microbial DNA in CSF. Treatment is mainly supportive, except for the nonviral infectious etiology. The term aseptic meningitis is used for all types of inflammation of the brain meninges which is not caused by pus producing bacteria. It is usually a benign syndrome.[1] Although viruses are a major cause, many different etiologies - both infective and non infective can cause aseptic meningitis. Hence the term is not synonymous with viral meningitis although the two are often used interchangeably. Magnitude Aseptic meningitis is one of the most common inflammatory disorders of the meninges. It occurs at all ages, although more common in children. No racial differences in occurrence have been reported. The incidence of aseptic meningitis in the US has been reported as 11 per 100,000 person - years, compared to 8.6 per 100,000 for bacterial meningitis.[2] The illness is responsible for 26,000 - 42,000 hospitalisations each year in the US.[3] A recent study in children from Singapore found an incidence of 37 cases per 10,000 hospital admissions.[4] Comparable figures for India are not available. Etiology
Aseptic meningitis may be considered as a syndrome with many possible etiologies. The various causes of aseptic meningitis are listed in [Table - 1]. Viral Meningitis This is the most common cause of aseptic meningitis.[5] Viral infections of the central nervous system may involve primarily the brain parenchyma, the meninges, the anterior horn cells, cranial nerves etc. When the infectious agent primarily attacks the brain parenchyma the clinical picture of 'encephalitis' with obtundation, seizures and coma is produced. When the inflammation is primarily of the meninges, a milder syndrome of viral or aseptic meningitis is produced. Pathologically and clinically there is a continuum between the two and some degree of meningeal inflammation is found with encephalitis and vice versa. Therefore the term 'viral meningoencephalitis' appears more appropriate. Most of these viruses characteristically cause either an 'encephalitic' or 'meningitic' picture. However, it must be borne in mind that the same agent may cause a very wide range of severity and occasionally produce an atypical illness.[6] The most common viruses causing aseptic meningitis are the enteroviruses, which account for more than half the cases.[7] More than 50 serotypes have been linked with meningitis. Mumps is another important cause of viral meningitis. Herpes viruses both type 1 (herpes labialis) and type 2 (genital herpes) can cause meningitis in children, especially infants. Varicella zoster virus can also cause meningitis but only in those who are immunocompromised. HIV may cause aseptic meningitis mostly at the time of seroconversion. It is difficult to assess the overall contribution of arboviruses, but in epidemics a sizeable number of patients especially children will exhibit a benign illness with neurologic manifestations.[5] This assumes special importance since Japanese encephalitis - an arboviral encephalitis is widely rampant in India. In the US, western equine encephalitis virus causes more cases of meningitis than the Eastern equine encephalitis virus, which causes a more serious illness. The St Louis encephalitis virus may cause a meningitic picture in upto 60% of children affected. The lymphocytic choreomeningitis virus - an arena virus, is a rare cause of aseptic meningitis. The respiratory viruses - influenza A & B, adenoviruses and rhinoviruses can occasionally cause meningitis.[8], [9], [10] Epidemiology The illness occurs at all ages and no racial differences are known. It tends to occur 3 times more commonly in males than females. Epidemiology of infectious meningitis reflects that of the infectious agent. Polio, Coxsackie and ECHO virus are spread by direct person to person transfer of infected oropharyngeal secretion or by feco-oral route. Enteroviruses are worldwide in distribution and humans are the only known natural hosts for these viruses. Infections with these viruses increase during late summer and early fall in the US.[1], [9], [10] The incubation period of enteroviruses varies widely.[5] Mumps meningitis has come down drastically in countries where the vaccine is widely used, but is still prevalent in India. Lymphocytic choreomeningitis occurs in individuals having
close contact with rodents like mice, hamster etc. Herpes simplex is again worldwide in distribution, sporadic and non seasonal. Arboviruses tend to occur in fairly characteristic geographical settings. Tuberculous meningitis is still an important cause of childhood hospital admissions in developing countries like India and has resurfaced in developed countries in association with HIV - AIDS. Pathophysiology Infectious meningitis results when the protective barriers of the brain - skull, meninges and blood brain barrier are overcome by the infecting agent. Meningitis can result either by the hematogenous route (as in tuberculous meningitis, HIV meningitis, arboviruses, respiratory viruses etc.) or by neurotropic spread of the agent as in herpes virus, rabies and polio.[6] Predisposing factors include otitis media, immunosuppression, pneumonia, sinusitis and pre-existing diabetes. Clinical features Viral Meningitis This has common clinical manifestations with variations depending on the particular virus. Although in some cases, pointers to specific viral agents may exist, in most cases the clinical findings are not sufficiently distinct to allow a specific etiologic diagnosis. The most common symptoms are headache, fever, myalgias, malaise, chills, sore throat, abdominal pain, nausea, vomiting, photophobia, stiff neck and drowsiness. Occasionally the child may exhibit altered consciousness in the form of confusion, drowsiness or visual hallucinations. Examination may reveal meningeal signs in the form of neck stiffness, Kernig's or Brudzinsky's signs. Severe meningeal irritation may result in the patient assuming the tripod position with the knees and hips flexed, neck extended and arms brought back to support the thorax. Meningeal irritation is also manifested by jolt accentuation of headache. Worsening of headache on turning the head to and fro horizontally at 2-3 times per second constitutes a positive sign. Seizures, focal neurologic deficits or profound sensorial alteration are rare manifestations. Many viruses causing the illness also produce a characteristic rash. Papilledema or absence of venous pulsations upon fundoscopic examination suggests increased intracranial pressure.[9],[10] In most cases, viral meningitis runs a mild course and is a self limiting, often transient illness. Some patients may exhibit a biphasic illness with nonspecific constitutional symptoms followed by meningitis. Presence of severe or prolonged sensorial alteration should prompt the clinician to exclude other treatable conditions. Distinction from non viral etiologies may also be difficult.[9],[10]
Enteroviruses These are small non enveloped RNA viruses of the picorna virus family. They are subdivided into the ECHO viruses, Coxsackie and Polio viruses, each with several serotypes. More than 50 serotypes have been linked with meningitis. They are spread by hand to mouth contact and to a lesser extent by respiratory and fecal routes. Some enteroviral infections produce a rash that usually accompanies the onset of fever and persists for 4-10 days. Coxsackievirius A 5, 9 or 16 and Echoviruses 4, 6, 9, 16 or 30 typically cause a maculopapular, nonpruritic rash confined to the face and trunk but sometimes involving extremities including palms and soles. Coxsackie A16 and rarely other group A serotypes may produce a vesicular rash on face, feet and oropharynx. Group A coxsackie virus may also produce herpangina characterized by grey, vesicular lesions on the tonsillar fossae, soft palate and uvula.[7], [11] Enterovirus 71 has recently been recognized to cause hand-foot-and- mouth disease and neurological manifestations like aseptic meningitis, encephalitis and polio like paralysis in India. The genotype isolated here was distinct from that causing severe epidemics in the Asia-Pacific region. [12] Mumps Meningoencephalitis Meningoencephalitis is the most frequent complication of mumps in childhood. Subclinical involvement, as evidenced by cerebrospinal fluid (CSF) pleocytosis has been reported in > 65% patients with mumps and clinical manifestations occur in >10% of patients. Males are affected 3-5 times as frequently as females and mortality is about 2%. Parotitis usually appears at the same time or following the onset of meningoencephalitis. Aqueductal stenosis and hydrocephalus have been associated with mumps meningoencephalitis.[6] HIV: HIV directly infects the central nervous system causing aseptic meningitis, encephalitis, leucoencephalopathy and myelopathy. Aseptic meningitis occurs mostly at the time of seroconversion. HIV encephalitis is characterised by progressive intellectual impairment, behavior disturbances, and sensorimotor deficits. DNA analysis helps to detect HIV in the brains of these patients and HIV specific immunoglobulin is produced intrathecally. As a result of immunodeficiency, patients are also more susceptible to toxoplasmosis, cryptococcosis, other fungal infections, cytomegalovirus and papova virus infection.[13], [14] Nonviral infectious etiologies In contrast to viral meningoencephalitis, nonviral causes of aseptic meningitis usually have a more complicated course and must be considered because they can be managed with specific therapy.
Partially Treated Bacterial Meningitis This may be confused with a non pyogenic or aseptic meningitis because CSF becomes sterile and cellular reaction changes from polymorphonuclear to lymphocytic. The condition is not benign or transient however and rapid deterioration occurs in absence of antibiotic therapy. In India, this is an important differential diagnosis of tuberculous meningitis. Tuberculous Meningitis This remains an important cause of childhood hospital admissions, mortality and permanent disability in India. Tuberculosis produces a basal meningitis thereby causing damage especially to basal structures - brain stem, cranial nerves and basal ganglia. The illness usually has a subacute onset with 3 clinical stages. In stage I, symptoms are nonspecific with irregular fever, irritability, occasional vomiting, headache, lethargy or malaise. Stage II is characterised by appearance of meningeal signs, convulsions or neurodeficits while stage III is accompanied by coma, decerebration and persisting deficits.[15] Prognosis is closely related to the stage of the disease in which it is diagnosed and treatment is started. A high index of suspicion is therefore extremely important to prevent permanent disability. A study from Lucknow revealed 5 clinicolaboratory features which are suggestive of TBM in a child hospitalised with meningoencephalitis : a prodromal stage of >7 days, extrapyramidal signs, focal deficits, optic atrophy and CSF pleocytosis with > 50% lymphocytes.[16] Lyme Disease This is the most common vector borne disease in the US, caused by Borrelia burgdorferi i - a fastidious, microaerophillic spirochete. Its prevalence in India is not known. In a study from Delhi, none of 27 patients presenting with mono/oligo arthritis of unknown etiology, 12 healthy blood bank donors, 25 patients with rheumatoid arthritis and 20 deer handlers were positive for IgG antibodies to Borrelia burgdorferi.[17] The illness is divided into early localised disease with a rash at the site of the tick bite often accompanied by fever, myalgia, headache and malaise; early disseminated disease with secondary erythema migrans lesions, constitutional symptoms, aseptic meningitis, cranial nerve palsies and carditis and late disease with chronic polyarthritis. Central nervous system manifestations are common in Lyme disease. Meningitis manifests several weeks after appearance of skin lesions, but while erythema migrans lesions are still present. Hypoglycorrhachia is not a prominent finding in the CSF. Facial nerve palsy, sometimes bilateral, may be observed. Diagnosis may be established by detection of specific IgM by ELISA, validated by Western Blot assay or by culturing the organism from a symptomatic patient.[6],[8] A study on differentiating features between Lyme meningitis and other aseptic meningitis showed that lyme meningitis should be suspected in cases of meningitis with very low CSF neutrophilic counts and high protein levels associated with prolonged duration of symptoms, low grade fever and absence of pronounced signs of meningitis.[18]
Brucellosis More Details This is a systemic infection caused by a small, aerobic, non spore bearing, nonmotile Gram negative coccobacillary bacteria, seen usually in persons living or working in close contact with animals, or consuming animal products such as raw milk or cheese made from raw milk. It is most common in the Mediteranean region, Asia, Africa, Mexico, South and Central America. Clinical features are extremely variable. In the acute form the illness presents with a flu like illness with fever, night sweats, malaise, anorexia, headache and myalgias. In the undulant form, symptoms are again fever, arthritis and epididymo-orchitis. Neurological involvement occurs in about 5% of patients. Diagnosis is confirmed by the isolation of Brucella More Details organisms from bacterial culture or increase over time of specific antibodies in blood.[6],[9] A study from Bikaner (Rajasthan) revealed 92 cases of brucellosis diagnosed on the basis of a history of contact with animals, fever, arthralgia and brucella antigen in serum in a titre of 1: 160 or more. Of these, 12 had neurobrucellosis - 4 aseptic meningitis, 2 myelitis, 5 polyradiculoneuropathy and 1 polyradiculomyeloencephalopathy.[19] Ehrlichiosis Acute monocytic ehrlichiosis is a tick borne infection caused by a small, pleomorphic obligate intracellular bacteria that possess Gram negative cell walls. The mammalian host is the deer or other domestic ruminants. The usual presentation is with fever, headache, myalgia, anorexia and vomiting. Nearly two-third of children develop a maculopapular rash. The infection may occasionally produce aseptic meningitis. Other manifestations include photophobia, conjunctivitis, pharyngitis, lymphadenopathy, hepatosplenomegaly and arthritis. Laboratory tests may reveal pancytopenia and elevated hepatic transaminases, blood urea nitrogen and creatinine. Diagnosis is established by high single antibody titres or seroconversion. PCR amplification of DNA sequences may be helpful in early stage when antibodies may not be detected.[6] Leptospirosis This is a zoonotic disease caused by the leptospiral spirochete. It may have an icteric or anicteric course. Anicteric leptospirosis usually presents as aseptic meningitis. A large epidemiological study in Kolenchery, Kerela after irrigation of dry lands picked up 976 cases of leptospirosis. The main reservoir for this zoonosis is the rat. In children and housewives, the main source of infection is a pet dog. IgM ELISA test is very sensitive though less specific for the diagnosis.[20] Syphilitic Meningitis This is becoming more common in the AIDS era. The secondary stage of the disease is heralded by a generalised nonprurutic rash, fever, headache, malaise and anorexia. Meningitis occurs in upto 30% of cases in this stage but may not produce neurological symptoms. Because of a lack of typical clinical presentation, CSF VDRL test should always be included in the diagnostic work up of aseptic meningitis.[6],[9],[10]
Fungal Meningitis Meningeal involvement can occur as the most serious manifestation of disseminated fungal infections. This occurs primarily in patients with AIDS, after organ transplantation, on immunosuppressive therapy or long term steroids. However, the most common fungal pathogen, Cryptococcus neoformans can occur in immunocompetent patients. Subacute or chronic meningitis is the most common clinical manifestation of disseminated cryptococcosis. Cryptococcal antigen assay in the CSF may be helpful in diagnosis.[6],[10] Drug induced aseptic meningitis The acute aseptic meningitis syndrome is being recognized as a complication of many drugs.[21],[22],[23],[24],[25],[26],[27],[28],[29] Intrathecal administration of anticancer drugs like methotrexate is known to sometimes result in aseptic meningitis. Many antimicrobials such as trimethoprim - sulfamethoxazole, ciprofloxacin, cephalexin, metronidazole, amoxicillin, penicillin and isoniazid are causes of aseptic meningitis. The xanthine oxidase inhibitor allopurinol and many other drugs - the nonsteroidal antiinflammatory drugs (NSAIDs), ranitidine, carbamazepine, vaccines against hepatitis B and mumps, immunoglobulins, radiographic agents and muromonab -CD3 (OKT3) have all been implicated. Pathophysiology of meningitis varies with different agents. A hypersensitivity reaction is considered for cases related to NSAIDs while OKT3 cases are believed to be mediated at least partly by cytokine release. The clinical features and CSF profile does not help in differentiating drug induced aseptic meningitis from infectious meningitis. A high index of suspicion is needed to reach a correct diagnosis. Every effort should be made to exclude treatable causes. Treatment includes discontinuation of the drug . Full recovery without sequelae is the rule.[30] Neoplastic meningitis Carcinomatous meningitis due to leukemic infiltration or primary and secondary tumours of the brain is well known and can produce the aseptic meningitis syndrome. CSF examination may reveal malignant cells.[31],[32],[33] Diagnosis Rapid, definitive differentiation of bacterial and viral infections of the central nervous system is a common clinical problem. Presence of severe obtundation, seizures and focal
deficits suggest the former. Analysis of CSF for acid base changes, aminoacids, LDH and its isoenzymes, nitroblue tetrazolium test of CSF polymorphonuclear cells, immunoglobulins, C reactive protein and lactate have all been suggested as differentiating tests. [Table - 2] lists the essential laboratory tests as well as those indicated by clinical suspicion. Laboratory Diagnosis CSF : Suspicion of viral meningitis is based on the clinical presentation and presence of supportive CSF findings. CSF pressure is usually increased. CSF shows generally less than 500 cells/cu mm. Early examination may occasionally show acellular fluid or predominance of polymorphonuclear leukocytes. Typical mononuclear pleocytosis devlops after 8-48 hours. CSF protein is elevated upto 100 mg % wheras glucose is normal or modestly decreased. Bacterial culture, Gram stain and bacterial antigen tests are uniformly negative. Levels of tumour necrosis factor (TNF) and lactate are low. Viral isolation from CSF is the standard criterion for diagnosis but is not positive in all patients.[9] Measurement of interferon alpha levels in CSF provides evidence of active viral invasion of the CNS but this test is not widely available. IgG index which is derived by calculating the ratios of IgG and albumen in CSF and serum is another indicator of intrathecal synthesis of antibodies. Specific IgG ratios in CSf and serum can also be used to identify infection with specific viruses but these are seldom helpful in the early stages of the illness.[34] The polymerase chain reaction (PCR) is an important advance in diagnosis of infectious meningitis.[35],[36] In recent years, it has become avalable for more and more agents. Stellrecht et al (2002) studied the impact of enteroviral Reverse Transcriptase PCR assay (RT-PCR) in the diagnosis and management of enteroviral meningitis in 1056 hospitalised patients. They concluded that RT-PCR for enteroviral meningitis is an important tool in the diagnosis of children with meningitis and nonspecific febrile illness which translated into shortened hospital stay and significant health care savings.[37] Viral isolation Besides CSF, arboviruses and enteroviruses can be isolated from blood but are seldom recoverable once clinical meningitis has set in. Specimen for viral culture from respiratory secretions, throat swab, CSF, blood, urine and stool should be taken as early in the illness as possible. Coxsackie and Echo viruses can be isolated from stool or throat swabs. Mumps virus can be isolated from saliva or throat swabs, HSV-2 from genital lesions and LCMV from blood.[10] Serology Seroconversion as demonstrated by a 4 fold rise in antobody titre in acute and convalescent phase sera can be helpful in making a diagnosis. However, virus specific
IgM provides a quick, early and accurate diagnosis. As IgM does not cross the blood brain barrier, presence of CSF IgM is highly suggestive of brain invasion by the pathogen.[9] Imaging CT or MRI brain is not helpful in the usual viral meningitis. These imaging techniques may help to exclude other diagnoses. Imaging is particularly helpful in later stages of tuberculous meningitis which shows basal enhancement and hydrocephalus.[38] Nigrovic, Kuppermann & Malley (2002) developed a multivariable prediction model to distinguish bacterial from aseptic meningitis in a retrospective cohort of 696 children aged 29 days to 19 years. 125 (18%) had bacterial meningitis and 571 (82%) had aseptic meningitis. Significant predictors for bacterial meningitis were gram stain of CSF showing bacteria, CSF protein > = 80 mg/dl, peripheral absolute neutrophil count >=10,000 , seizure before or at presentation and CSF absolute neutrophil count >= 1000. A score giving 1 point for each of these predictors except the first which was given 2 points accurately identified patients with bacterial and aseptic menigitis with sensitivity of 87%.[39] Treatment Many patients with aseptic meningitis can be treated on an outpatient basis, after initial lumbar puncture. Those who have seizures, altered consciousness or severe symptoms or those in whom the diagnosis is in doubt should be hospitalised. Treatment is mostly supportive and includes analgesics, antipyretics, antiemetics, maintainence of fluid balance and prevention and treatment of complications. No specific therapy is presently recommended for most viral pathogens. Whenever there is a suspicion or doubt as to presence of bacterial meningitis, empiric antibiotic therapy should be instituted after obtaining specimen for culture. Antiviral therapy is available against HSV, varicella and cytomegalovirus. Acyclovir, valacyclovir and foscarnet are used for herpes or varicella infections and gangcyclovir is used for cytomegaloviral infection.[6] Specific antimicrobial therapy would be required for infectious agents. For tuberculous meningitis, antitubercular therapy with 4 drugs - Streptomycin, isoniazid, rifampicin and pyrazinamide for the initial 2 months followed by 3 drugs for another 10 months is generally recommended, along with 4-6 weeks of steroids initially. Penicillin and ceftriaxone are used for meningitis caused by actinomyces and spirochetes. Doxycycline or rifampicin is used for Brucella infection and gentamycin for Pasteurella tularensis. Antifungal agents that can be used are amphoterecin B, fluconazole and flucytosine.
Complications Seizures, even status epilepticus can sometimes occur with aseptic meningitis but prophylactic anticonvulsants are not recommended. If seizures occur, they should be controlled with phenytoin and phenobarbital. A variable component of encephalitis may be seen with viral meningitis. Mumps meningoencephalitis can result in sensorineural deafness and aqueductal stenosis causing hydrocephalus.[6] Complications of tuberculous meningitis include hydrocephalus, infarcts, neurological deficits, cranial nerve palsies, epilepsy and mental regression. Prognosis Viral meningitis is usually a benign disease, with low rates of morbidity and mortality. Full recovery occurs within 5-14 days in most patients. Fatigue, lightheadedness and asthenia may persist for a few months in some patients. Other nonviral infectious meningitis is not so benign, however. Tuberculous meningitis is a particularly dangerous illness with high rate of mortality and permanent sequelae unless diagnosed and treated very early. Prevention Patients with measles, chickenpox, rubella or mumps must be isolated. Strict handwashing especially after nappy changes are important in preventing spread of enterovirus infections. Effective vaccines are available for polio, measles, mumps, varicella and rubella. Arboviral vaccines are also available and should be used for populations living in or visiting endemic areas. References 1. Krugman S, Katz SL, Gerston AA, Wilfert C. Aseptic Meningitis in Infectious Diseases of Children. 8th edn. CV Mosby Co, Toronto, 1985; 167-173. 2. Hammer SM, Connolly KJ. Viral aseptic meningitis in the United States: Clinical features, viral etiologies and differential diagnosis. Curr Clin Top Infect Dis 1992; 12 : 1-25. [PUBMED] 3. Centre for Disease Control Morbidity & Mortality Weekly Report 2003: 52 (32); 761-764. 4. Tee WS, Choong CT, Lui RV, Ling AE. Aseptic meningitis in children: The Singapore experience. Ann Acad Med Singapore 2002: 31 (6); 756-760. 5. Middlekamp JN. Aseptic meningitis & viral meningitis. In Feigin, Cherry, eds. Textbook of Pediatric Infectious Diseases. Feigin & Cherry WB Saunders Co, 1981; 319-324. 6. Prober CG. Infections of the Central Nervous System. Behrmann, Kleigman &
7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26.
Jenson, eds. Nelson Textbook of Pediatrics; 16th edn. WB Saunders Co, 2000; 713716. Rotbart HP. Enteroviral infections of the central nervous system. Clin Infect Dis 1995: 20(4); 971-981. Shukla PC, Ramachandran T. Aseptic Meningitis. Emedicine Article 23rd May 2002 Connolly KJ, Hammer SM. The acute aseptic meningitis syndrome. Infect Dis Clin North Am 1990; 4(4); 599-622. Dalton M, Newton RW. Aseptic meningitis. Dev Med Child Neurol 1991; 33(5); 446-451. Muir P, van Loon AM. Enterovirus infections of the central nervous system. Intervirology 1997; 40 (2) : 153-166. Deshpande JM, Nadkarni SS, Francis PP. Enterovirus 71 isolated from a case of acute flaccid paralysis in India represents a new genotype. Curr Sci 2003; 85(10): 1350-1353. Gabudza DH. Neurological disorders associated with HIV infections. J Am Acad Dermatol 1990; 22 (6 pt 2); 1232-1236. Newton HB. Common neurologic complications of HIV -1 infection and AIDS. Am Fam Physician 1995; 51 (2) : 387-398. Medical Research Council: Tuberculosis survey of England & Wales 1978/1979. HMSO London 1980 Kumar R, Singh SN, Kohli N. A diagnostic rule for tuberculous meningitis. Arch Dis Child 1999; 81: 221-224. Handa R, Wali JP, Singh S, Aggarwal P. A propective study of dengue arthritis in north India. Indian J Med Res 1999; 110: 107-9. Tuerlinckx D, Bodart E, Garrino MG, de Bilderling G. Clinical data and cerebrospinal fluid findings in Lyme meningitis versus aseptic meningitis. Eur J Pediatr 2003: 162 (3); 150-153. Kochar DK, Agarwal N, Jain N, Sharma BV, Rastogi A, Meena CB. Clinical profile of neurobrucellosis - a report of 12 cases from Bikaner (north west India). J Assoc Phys India 2000; 48 (4): 376-380. Shah I, Warke S, Deshmukh CT, Kamat JR. Leptospirosis - an underdiagnosed clinical condition. J Postgrad Med 1999; 45: 93-94. Moris G, Garcia-Monco JC. The challenge of drug induced aseptic meningitis. Arch Intern Med 1999; 159 (11); 1185-1194. Marinac JS. Drug and chemical induced aseptic meningitis: a review of the literature. Ann Pharmacother 1992; 26 (6); 813-822. Shapiro WR, Young DF. Neurological complications of antineoplastic therapy. Acta Neurol Scand Suppl 1984; 100: 125-132. Min DI, Monaco AP. Complications associated with immunosuppressive therapy and their management. Pharmacotherapy 1991; 11(5): 119S-125S. Nydegger UE, Sturzenegger M. Adverse effects of immunoglobulin therapy. Drug Saf 1999; 21 (3): 171-185. Alloway JA, Mitchell SR. Sulfasalazine neurotoxicity : a report of aseptic meningitis and a review of the literature. J Rheumatol 1993; 20(2): 409-411.
S-ar putea să vă placă și
- The Collected Letters of Flann O'BrienDocument640 paginiThe Collected Letters of Flann O'BrienSean MorrisÎncă nu există evaluări
- John PFTDocument231 paginiJohn PFTAlexander Santiago ParelÎncă nu există evaluări
- Marriage Gift PolicyDocument4 paginiMarriage Gift PolicyGanesh Gaikwad100% (3)
- Internal Medicine - DermatologyDocument125 paginiInternal Medicine - DermatologySoleil DaddouÎncă nu există evaluări
- MeningitisDocument28 paginiMeningitisMarcelo Fabian Lopez Santa CruzÎncă nu există evaluări
- College of Nursing Berhampur: Subject-Medical Surgical Nursing Topic-MeningitisDocument9 paginiCollege of Nursing Berhampur: Subject-Medical Surgical Nursing Topic-MeningitisAmlan jyoti thanapati100% (1)
- MeningococcemiaDocument14 paginiMeningococcemiaMonica Marie MoralesÎncă nu există evaluări
- Viral EncephalitisDocument29 paginiViral Encephalitisruntika100% (1)
- Gavrila Eduard 2Document6 paginiGavrila Eduard 2Eduard Gabriel GavrilăÎncă nu există evaluări
- Amex Case StudyDocument12 paginiAmex Case StudyNitesh JainÎncă nu există evaluări
- Parenteral NutritionDocument78 paginiParenteral NutritionImen YunieÎncă nu există evaluări
- Meningitis and Acute MeningococcemiaDocument16 paginiMeningitis and Acute Meningococcemiaalfaz lakhaniÎncă nu există evaluări
- Aseptic MeningitisDocument24 paginiAseptic Meningitisidno1008100% (1)
- Aseptic Meningitides, Is Caused by A Systemic Viral Infection Whose Infectivity WithinDocument9 paginiAseptic Meningitides, Is Caused by A Systemic Viral Infection Whose Infectivity WithinEveline YuniartiÎncă nu există evaluări
- Cordia Viral MeningitisDocument7 paginiCordia Viral MeningitisAyuagung Chandra Maha DewiÎncă nu există evaluări
- Nonpolio VirusesDocument4 paginiNonpolio VirusesDessy SitompulÎncă nu există evaluări
- Background: Herpes Simplex EncephalitisDocument14 paginiBackground: Herpes Simplex Encephalitisjea_carinoÎncă nu există evaluări
- Acute Viral EncephalitisDocument7 paginiAcute Viral EncephalitisLeanna Mae AustriaÎncă nu există evaluări
- What Is Meningitis? What Is Encephalitis?Document9 paginiWhat Is Meningitis? What Is Encephalitis?Rainy RaiÎncă nu există evaluări
- Viral Diseases of The Central Nervous SystemDocument18 paginiViral Diseases of The Central Nervous System46nv7gphxzÎncă nu există evaluări
- Chapter1: Introduction: E Coli and Other Gram-Negative Enteric Bacilli Such AsDocument6 paginiChapter1: Introduction: E Coli and Other Gram-Negative Enteric Bacilli Such AsAhmed RashadÎncă nu există evaluări
- 5 - Pneumococcal Disease Infections Caused by Stre - 2012 - Netter S InfectiousDocument5 pagini5 - Pneumococcal Disease Infections Caused by Stre - 2012 - Netter S InfectiousstasiulinoÎncă nu există evaluări
- Recognizing Nervous System InfectionsDocument22 paginiRecognizing Nervous System InfectionsZin LimÎncă nu există evaluări
- Signs and SymptomsDocument8 paginiSigns and SymptomsCrystal Joy LabasanÎncă nu există evaluări
- Viral Meningitis: David R. ChadwickDocument14 paginiViral Meningitis: David R. ChadwickVina HardiantiÎncă nu există evaluări
- EncephalitisDocument3 paginiEncephalitisFranciscus BuwanaÎncă nu există evaluări
- Epidemic Cerebrospinal MeningitisDocument76 paginiEpidemic Cerebrospinal MeningitisAngie LawrenceÎncă nu există evaluări
- Brain InfectionDocument8 paginiBrain Infectionsistla naveenÎncă nu există evaluări
- Clin Gui EncephalitisDocument9 paginiClin Gui EncephalitisAl MuzakkiÎncă nu există evaluări
- Brain InfectionDocument8 paginiBrain Infectionsistla naveenÎncă nu există evaluări
- Aseptic Meningitis and Viral Myelitis: David N. Irani, MDDocument21 paginiAseptic Meningitis and Viral Myelitis: David N. Irani, MDJorge DiazÎncă nu există evaluări
- MMSU Encephalitis GuideDocument8 paginiMMSU Encephalitis GuideTheeya QuigaoÎncă nu există evaluări
- Meningitis (Physical Exam)Document6 paginiMeningitis (Physical Exam)MohammadAwitÎncă nu există evaluări
- Meningitis 2Document28 paginiMeningitis 2Mehveen KashifÎncă nu există evaluări
- Approach To The Patient With Suspected Infection of SNCDocument12 paginiApproach To The Patient With Suspected Infection of SNCJosé Miguel FerreiraÎncă nu există evaluări
- The Pathogenesis of Acute Viral Encephalitis and Postinfectious EncephalomyelitisDocument6 paginiThe Pathogenesis of Acute Viral Encephalitis and Postinfectious EncephalomyelitisBill RajagukgukÎncă nu există evaluări
- Neurological Infections: Gerard Gabriel P. Reotutar, RM, RN, MANDocument33 paginiNeurological Infections: Gerard Gabriel P. Reotutar, RM, RN, MANJeremiash Noblesala Dela CruzÎncă nu există evaluări
- LalalaDocument4 paginiLalalanoreka azizahÎncă nu există evaluări
- Microbial Diseases of The Nervous SystemDocument18 paginiMicrobial Diseases of The Nervous SystemInah PagariganÎncă nu există evaluări
- Patho Unit 5Document37 paginiPatho Unit 5Shafiya ShaikÎncă nu există evaluări
- Jurnal NeuroDocument15 paginiJurnal NeuroElisabeth Chinta UliÎncă nu există evaluări
- Suthar 2018Document10 paginiSuthar 2018CARLOS MONCAYO DIAZÎncă nu există evaluări
- Treatmentofviral Encephalitis: Allen J. Aksamit JRDocument11 paginiTreatmentofviral Encephalitis: Allen J. Aksamit JRRicardo Robles AlfaroÎncă nu există evaluări
- Enterovirus DR - MiraDocument28 paginiEnterovirus DR - MiraPranudiah Yulianti NingtiasÎncă nu există evaluări
- Arthropod-Borne Encephalitides - UpToDateDocument21 paginiArthropod-Borne Encephalitides - UpToDateBhargav YagnikÎncă nu există evaluări
- This Is A Document About Chicken PoxDocument24 paginiThis Is A Document About Chicken Poxarul100% (1)
- Encephalitis: Encephalitis Is Inflammation of The Parenchyma of The Brain, Resulting From Direct ViralDocument5 paginiEncephalitis: Encephalitis Is Inflammation of The Parenchyma of The Brain, Resulting From Direct ViralLucky PuspitasariÎncă nu există evaluări
- Viral Diseases of the Nervous SystemDocument41 paginiViral Diseases of the Nervous SystemAiko EscobidoÎncă nu există evaluări
- CNS InfectionsDocument39 paginiCNS InfectionsRaja RuzannaÎncă nu există evaluări
- Viral Encephalitis Seminar Reviews Familiar InfectionsDocument7 paginiViral Encephalitis Seminar Reviews Familiar Infectionsjperez_450881Încă nu există evaluări
- Viral Meningitis in Children Clinical Features and DiagnosisDocument25 paginiViral Meningitis in Children Clinical Features and DiagnosisTrúc QuỳnhÎncă nu există evaluări
- Upload 2Document10 paginiUpload 2zendah123Încă nu există evaluări
- Micro VirologyDocument359 paginiMicro VirologyruthÎncă nu există evaluări
- Encephalitis & Meningoencephalitis GuideDocument7 paginiEncephalitis & Meningoencephalitis GuideChristian Hasudungan NainggolanÎncă nu există evaluări
- Sjogren's Syndrome: Treatment Options, Latest Advances. Trustworthy, Current ReportDocument11 paginiSjogren's Syndrome: Treatment Options, Latest Advances. Trustworthy, Current ReportRona MayÎncă nu există evaluări
- k.16 Inf. Sis. Syaraf PST (Jan 2009)Document66 paginik.16 Inf. Sis. Syaraf PST (Jan 2009)Winson ChitraÎncă nu există evaluări
- Managing Meningoencephalitis in Indian ICU: Neurocritical CareDocument5 paginiManaging Meningoencephalitis in Indian ICU: Neurocritical CareerikafebriyanarÎncă nu există evaluări
- Infectious and Inflammatory Diseases of Brain and Spinal CordDocument50 paginiInfectious and Inflammatory Diseases of Brain and Spinal CordKeerthana BÎncă nu există evaluări
- Varicella Zoster (Chickenpox) : Frequently Asked QuestionsDocument2 paginiVaricella Zoster (Chickenpox) : Frequently Asked QuestionsMuhammad mukramÎncă nu există evaluări
- Viral Exanthema: Dharmendra MandalDocument57 paginiViral Exanthema: Dharmendra MandalMaunank TandelÎncă nu există evaluări
- Herpes Zoster in Diverse Situations - A Review PDFDocument21 paginiHerpes Zoster in Diverse Situations - A Review PDFLaras KinasihÎncă nu există evaluări
- Presentation, Diagnosis, and Treatment of Meningitis and Encephalitis A Detailed ReviewDocument7 paginiPresentation, Diagnosis, and Treatment of Meningitis and Encephalitis A Detailed Reviewfitri dwiyantiÎncă nu există evaluări
- Meningitis &encephalitisDocument9 paginiMeningitis &encephalitisSnIP StandredÎncă nu există evaluări
- DasdasDocument4 paginiDasdasAbdurauf SawadjaanÎncă nu există evaluări
- Viral MeningitisDocument19 paginiViral MeningitisUneebÎncă nu există evaluări
- IS 2848 - Specition For PRT SensorDocument25 paginiIS 2848 - Specition For PRT SensorDiptee PatingeÎncă nu există evaluări
- BE 510 Business Economics 1 Problem Set 5 SolutionsDocument5 paginiBE 510 Business Economics 1 Problem Set 5 SolutionsCreative Work21stÎncă nu există evaluări
- Classification of Methods of MeasurementsDocument60 paginiClassification of Methods of MeasurementsVenkat Krishna100% (2)
- Case Study - Help DocumentDocument2 paginiCase Study - Help DocumentRahÎncă nu există evaluări
- Audi A3 Quick Reference Guide: Adjusting Front SeatsDocument4 paginiAudi A3 Quick Reference Guide: Adjusting Front SeatsgordonjairoÎncă nu există evaluări
- Bargaining Power of SuppliersDocument9 paginiBargaining Power of SuppliersPiyumi VitharanaÎncă nu există evaluări
- Mono - Probiotics - English MONOGRAFIA HEALTH CANADA - 0Document25 paginiMono - Probiotics - English MONOGRAFIA HEALTH CANADA - 0Farhan aliÎncă nu există evaluări
- Costing - Type Wise Practical Mcq-Executive-RevisionDocument71 paginiCosting - Type Wise Practical Mcq-Executive-RevisionShruthi ParameshwaranÎncă nu există evaluări
- Country Profile - NigerDocument1 paginăCountry Profile - Nigernana kayÎncă nu există evaluări
- Chapter 1Document2 paginiChapter 1Nor-man KusainÎncă nu există evaluări
- Lignan & NeolignanDocument12 paginiLignan & NeolignanUle UleÎncă nu există evaluări
- Divide Fractions by Fractions Lesson PlanDocument12 paginiDivide Fractions by Fractions Lesson PlanEunice TrinidadÎncă nu există evaluări
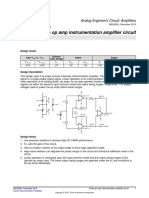
- Opamp TIDocument5 paginiOpamp TIAmogh Gajaré100% (1)
- Performance of a Pelton WheelDocument17 paginiPerformance of a Pelton Wheellimakupang_matÎncă nu există evaluări
- Mutaz Abdelrahim - Doa - MT-103Document17 paginiMutaz Abdelrahim - Doa - MT-103Minh KentÎncă nu există evaluări
- Lay Out New PL Press QltyDocument68 paginiLay Out New PL Press QltyDadan Hendra KurniawanÎncă nu există evaluări
- Module 5 Communication & Change MGT - HS Planning & Policy Making ToolkitDocument62 paginiModule 5 Communication & Change MGT - HS Planning & Policy Making ToolkitKristine De Luna TomananÎncă nu există evaluări
- ROM Magazine V1i6Document64 paginiROM Magazine V1i6Mao AriasÎncă nu există evaluări
- Impression Techniques in Complete Denture Patients: A ReviewDocument6 paginiImpression Techniques in Complete Denture Patients: A ReviewRoja AllampallyÎncă nu există evaluări
- Women Safety AppDocument18 paginiWomen Safety AppVinod BawaneÎncă nu există evaluări
- METRIC_ENGLISHDocument14 paginiMETRIC_ENGLISHKehinde AdebayoÎncă nu există evaluări
- Working With Session ParametersDocument10 paginiWorking With Session ParametersyprajuÎncă nu există evaluări
- 1 20《经济学家》读译参考Document62 pagini1 20《经济学家》读译参考xinying94Încă nu există evaluări
- DMDPrework QuizDocument5 paginiDMDPrework Quizjunpe- yuutoÎncă nu există evaluări