Documente Academic
Documente Profesional
Documente Cultură
Case Study Illness
Încărcat de
alexxx99Descriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Case Study Illness
Încărcat de
alexxx99Drepturi de autor:
Formate disponibile
ELECTROCARDIOGRAPHIC MONITORING AND CONDUCTION ABNORMALITIES Cardiac Conduction
1. Match terms with correct descriptions. P wave ___C____ PR interval ___D___ QRS complex ___E___ ST segment ____F___ T wave ____G____ QT interval ____A___ Ejection fraction ____B___ a. Interval shortens with increase in heart rate b. Ratio of stroke volume to volume of blood remaining in the ventricle at end diastole c. Atrial depolarization d. Atrial impulse conduction through AV node e. Ventricular depolarization f. Deflections indicate ventricular muscle injury g. Ventricular repolarization
Sinus Dysrhythmias
Scenario: An elderly patient presents to the emergency department with complaint of chest pain and fatigue. The cardiac monitor shows a heart rate of 35. The patients color is pale, and the skin is warm and dry. Blood pressure is 90/50, respiratory rate is 22, and temperature is 99.1F. 2. Why is this patient having symptoms? 1. The Patient is suffering from Bradycardia (HR 35), it as reduced his cardiac output, and as a consequence, he is suffering from hypotension and chest pain (Reduced O2 to his heart = Angina). Because of that, the quantity of O2 to his tissus and cells also has decrease, giving him a pale color to his skin, also his body is attempting to compensate by increasing his respiratory rate. Bradycardia can be cause by an infectious process, which would explain his fever and his warm and dry skin??? 3. What treatments should this patient receive and why? 1. He should receive first Atropine , to get his Heart Rate up, probably solve at the same time his chest pain, Hypotension, and Tachypnea. The Underlining cause of his Bradycardia should also be explored, be it an infectious disease of an atrial malfunction. An external pacemaker could also be temporarily install to prevent further bradycardia.
Atrial Dysrhythmias
Scenario: A patient presents to the doctors office with the complaint of shortness of breath. When the nurse takes the patients radial pulse, she obtains 160 beats per minute. This rate is confirmed by apical auscultation. 4. Different arrhythmias can produce a rate of 160. How will the medical team differentiate the cause? 1. First by doing an EKG, we will be able to see the kind of rhythm this is, SVT, VT, Rapid Atrial Fibrillation?? 5. What are the treatment options for SVT? 1. First, we could try the valsalva manoever, and then Adenosine is the medication of choice, it blocks for a short time the AV node conduction. Other medications that could be use are Calcium Channels blocking agents, Beta-Blockers,or Digitalis. If all fails, Electrc Cardioversion should be used. 6. List nursing responsibilities during adenosine administration. 1. First we should warn the patient about the effect of Adenosine and that he could feel like he is dying, chest pressure, facial flushing or dyspnea, but that it will pass very quickly. The patient should have a cardiac monitor. His pulse and Pressure should be monitored during the procedure, a brief periods of AV block or Pause can be observed, and should be monitored very closely.
Conduction Abnormalities
7. Complete the table. AV Block First-degree AV block Second-degree, type 1 AVB Characteristics Pr intervals greater that 0.20 seconds, rhythm is regular Pr intervals gradually lengthens until a P wave is blocked (No QRS follow). Rhythm is irregular. Atrial rate faster than ventricular rate. PR interval will be constant when P is followed be QRS. There is blocked P waves, their appearance can be variable or fixed (2:1, 3:1...) Rhythm is Treatment Options Usually not treated unless patient is symptomatic, can be medication related. Atropine, Dopamine, Epinephrine, transcutaneus pacemaker or permanent pacemaker. If related to digitalis, it will be stopped. Atropine, Dopamine, Epinephrine, Temporary or permanent pacemaker.
Second-degree, type 2 AVB
Third-degree heart block
Bundle branch block (right or left)
irregular. PR interval never constant, Rhythm is regular, but should patient is usually bradycardic, P waves are constant between them. QRS could be widened. More P waves than QRS. QRS is widened, depend on an anomaly is the His branches where the impulsion is slower on one side. Rhythm is usually regular.
Atropine, Dopamine, Epinephrine, Temporary or permanent pacemaker.
Usually not treated unless it is indicatory of another more important problem (ex: MI)
Case Study
Scenario: Eleanor, an 86-year-old retired nurse, presents to the emergency department with complaints of chest pain and shortness of breath. She is immediately placed on a cardiac monitor where it shows ventricular tachycardia, rate 160. Her blood pressure is 70/50, respiratory rate is 22 and rapid. An IV is started, oxygen is administered via face mask, and a 12-lead EKG is obtained. 8. Identify immediate treatment options for Eleanor. 1. Electrical cardioversion During synchronized cardioversion, Eleanor becomes unresponsive. The nurse cannot palpate a carotid pulse. 9. Identify immediate treatment options. 1. Pas sur ici, faut-il y rpondre avec toutes les manoeuvres, ou les mdicaments? Reanimation procedure should be started, physician should be at the side of patient, patient should be monitored to assess if there is a rhythm (Asystolia or Ventricular Fibrillation) Massage should be initiated followed by defibrillation, vitals should be tried to be taken, and medications could be given appropriately. Eleanors rhythm returns as a result of swift resuscitative action. Her new rhythm is atrial fibrillation with multifocal PVCs. Eleanor will require an in-depth cardiac workup to identify the cause of her cardiac problems. Immediately, numerous labs are drawn: CPK, troponin levels, CRP (C reactive protein), CBC, electrolytes, magnesium, renal panel, and coagulation studies. Chest x-ray shows clear lung fields. An echocardiogram is ordered. The physician also requests immediate consult for ICD placement. ( Implantable Cardio Defibrillator) 10. Identify immediate treatment options for continual PVCs during post-resuscitation.
1. Patient has to be under constant cardiac monitoring, Amiodarone should be started and also heparin because of the atrial fibrillation. Electrolytes results should be checked as soon as they come back and corrected if needed. 11. Provide reasons for obtaining specified lab and diagnostic tests. CPK: CPK is an indicator of muscle damage, in our case, it is the damage to the heart muscle that interest us. It can be an indication of Myocardial Infarction. They have a rapid onset, (4 hours) but usually disappear in one or two days. Troponins : Troponin are similar to CPK but are specific to the heart and damage done to it. They take a little longer to appear (4-6 hours) but take around 4 days to disappear. CRP: CRP is usually an indicator of an inflammatory process but can also be used to evaluate patient with MI, it usually follows the levels of CPK but takes 1 to 3 days to attain it's maximum levels, if it stays elevated, it can be an indication of continuing damage to the heart. CBC : Complete Blood count, will give us a basic understanding of bloods cells, anemia or malnutrition could cause chest pain, Electrolytes: Electrolytes are very important to the conduction of electricity in the heart, and low or elevated levels can cause significant changes in electrical pattern of the heart. We should be especially careful about the potassium levels, and they should be corrected immediately. Magnesium : Magnesium is also an electrolyte, but it is not normally dosed and must be taken appart, low level can cause as potassium all kinds of arrythmia, also it is closely related to the level of potassium, so a low level of magnesium will likely also cause a low level of potassium, it must also be quickly corrected. Renal Panel :A decrease renal function could cause and increase in electrolytes, for example Potassium at level greater than 5.5. The creatinine and Bun level could help us determined the actual renal function. (il me semble que l'on pourrait rajouter des choses...) Coagulation studies : MI could be caused by increase coagulation levels, also if patient is now in atrial fibrillation anticoagulant therapy will be started, and we need to assess the starting point of patient. (Ici pas sur sur non plus) 12. Why is an ICD being considered as a treatment option for Eleanor? 1. Multifocal PVC's are arrhythmias that can induced other more dangerous arrhythmias. For example if a PVC goes on during the refractory period of a normal QRS, it could induce Ventricular tachycardia or even worst Ventricular fibrillation. Multifocal PVC are more dangerous, because they come from different ectopic center within the ventricules. Furthermore, a newly diagnosed AF, could also induced theses kinds of arrhythmias. An ICD could prevent theses complications by shocking as soon has theses rhythm appear.
S-ar putea să vă placă și
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- New Microsoft Excel WorksheetDocument4 paginiNew Microsoft Excel WorksheetRaheel Neo AhmadÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Annex 8 Qualification of BalancesDocument11 paginiAnnex 8 Qualification of BalancesMassimiliano PorcelliÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Hotel Housekeeping EQUIPMENTDocument3 paginiHotel Housekeeping EQUIPMENTsamahjaafÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- RTG E-One - Manual de Manutenção 41300-41303 (EN)Document328 paginiRTG E-One - Manual de Manutenção 41300-41303 (EN)Conrado Soares100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (894)
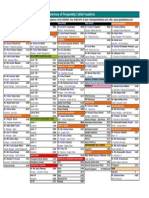
- Directory of Frequently Called Numbers: Maj. Sheikh RahmanDocument1 paginăDirectory of Frequently Called Numbers: Maj. Sheikh RahmanEdward Ebb BonnoÎncă nu există evaluări
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Tugas B InggrisDocument9 paginiTugas B InggrisDellyna AlmaÎncă nu există evaluări
- Life Sciences Part 1 CSIR JRF NET GATE DBT PDFDocument132 paginiLife Sciences Part 1 CSIR JRF NET GATE DBT PDFPavani Reddy68% (22)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Siemens MV Gas Insulated Switch GearDocument14 paginiSiemens MV Gas Insulated Switch GearSajesh Thykoodan T VÎncă nu există evaluări
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Natural Resources in PakistanDocument5 paginiNatural Resources in PakistanSohaib EÎncă nu există evaluări
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Auramo Oy spare parts listsDocument12 paginiAuramo Oy spare parts listsYavuz ErcanliÎncă nu există evaluări
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- Chapter 4Document26 paginiChapter 4Lana AlakhrasÎncă nu există evaluări
- The National Building Code of The PhilippinesDocument390 paginiThe National Building Code of The PhilippinesJohn Joseph EstebanÎncă nu există evaluări
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- CERADocument10 paginiCERAKeren Margarette AlcantaraÎncă nu există evaluări
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Akshaya Trust NgoDocument24 paginiAkshaya Trust NgodushyantÎncă nu există evaluări
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Quality Nutrition and Dietetics PracticeDocument3 paginiQuality Nutrition and Dietetics PracticeNurlienda HasanahÎncă nu există evaluări
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- FileDocument284 paginiFileJesse GarciaÎncă nu există evaluări
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Live Performance Award Ma000081 Pay GuideDocument48 paginiLive Performance Award Ma000081 Pay GuideDan LijndersÎncă nu există evaluări
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- 559 Fault CodeDocument4 pagini559 Fault Codeabdelbagi ibrahim100% (1)
- Comm Part For A320Document1 paginăComm Part For A320ODOSÎncă nu există evaluări
- Right To HealthDocument9 paginiRight To HealthPriya SharmaÎncă nu există evaluări
- 2 English Course BDocument8 pagini2 English Course BAnjana27Încă nu există evaluări
- WSO 2022 IB Working Conditions SurveyDocument42 paginiWSO 2022 IB Working Conditions SurveyPhạm Hồng HuếÎncă nu există evaluări
- Switzerland: Food and CultureDocument18 paginiSwitzerland: Food and CultureAaron CoutinhoÎncă nu există evaluări
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Junayed - 19 39800 1Document11 paginiJunayed - 19 39800 1gurujeeÎncă nu există evaluări
- General JournalDocument11 paginiGeneral JournalZaheer Ahmed Swati100% (2)
- Mufon Ufo JournalDocument21 paginiMufon Ufo JournalSAB78Încă nu există evaluări
- ME JBP 70A Pen Dissolved Oxygen Meter PDFDocument1 paginăME JBP 70A Pen Dissolved Oxygen Meter PDFpiknikmonsterÎncă nu există evaluări
- Cipac MT 185Document2 paginiCipac MT 185Chemist İnançÎncă nu există evaluări
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Fluid Mechanics Sessional: Dhaka University of Engineering & Technology, GazipurDocument17 paginiFluid Mechanics Sessional: Dhaka University of Engineering & Technology, GazipurMd saydul islamÎncă nu există evaluări
- Space Analysis in Orthodontic: University of GlasgowDocument16 paginiSpace Analysis in Orthodontic: University of GlasgowNizam Muhamad100% (1)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)