Documente Academic
Documente Profesional
Documente Cultură
Evs Prject
Încărcat de
Dipen VyasDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Evs Prject
Încărcat de
Dipen VyasDrepturi de autor:
Formate disponibile
Bronchitis Overview Bronchitis is an acute inflammation of the air passages within the lungs.
It occurs when the trachea (windpipe) and the large and small bronchi (airways) within the lungs become inflamed because of infection or irritation from other causes. The thin mucous lining of these airways can become irritated and swollen. The cells that make up this lining may leak fluids in response to the inflammation. Coughing is a reflex that works to clear secretions from the lungs. Often the discomfort of a severe cough leads a person to seek medical treatment. Both adults and children can get bronchitis. Symptoms are similar for both.
Object 1 2
Infants usually get bronchiolitis, which involves the smaller airways and causes symptoms similar to asthma. Asthmatic bronchitis occurs when asthma and bronchitis coexist. Asthma is an inflammatory airway condition that leads to tightening of the muscles around the airways and swelling, both of which cause the airways to narrow. In combination with the inflammation of the inner lining of the airways and mucus production this can lead to severe wheezing and shortness of breath. Picture of the lung, bronchi, and airways of the lung Bronchitis Causes Bronchitis occurs most often during the cold and flu season, usually coupled with an upper respiratory infection. Several viruses cause bronchitis, including influenza A and B, commonly referred to as "the flu." A number of bacteria are also known to cause bronchitis, such as Mycoplasma pneumoniae, which causes so-called "walking pneumonia." Bronchitis also can occur when a person inhales irritating fumes or dust. Chemical solvents and smoke, including tobacco smoke, have been linked to acute bronchitis. People at increased risk both of getting bronchitis and of having more severe symptoms include the elderly, those with weakened immune systems, smokers, and anyone with repeated exposure to lung irritants. Is Bronchitis Contagious? Bronchitis describes a group of symptoms (including airway inflammation, over-production of phlegm, cough), which can have various causes. If the cause of the bronchitis is viral or bacterial, it can be contagious. If the cause of the bronchitis is due to smoking, air pollution, or other inhaled irritants, it is not contagious. Bronchitis Symptoms Acute bronchitis most commonly occurs after an upper respiratory infection such as the common cold or a sinus infection. The affected person may have symptoms such as fever with chills, muscle aches, nasal congestion, and sore throat. Cough is a common symptom of bronchitis. The cough may be dry or may produce phlegm. Significant phlegm production suggests that the lower respiratory tract and the lung itself may be infected, and you may have symptoms that suggest pneumonia. The cough may last for more than 2 weeks. Continued forceful coughing may make your chest and abdominal muscles sore. Coughing can be severe enough at times to injure the chest wall or even cause a person to pass out (faint). Wheezing may occur because of the muscular tightness and inflammation of the airways. This may leave the affected individual short of breath. Asthmatic bronchitis symptoms include a combination of wheezing and shortness of breath, in addition to the other symptoms of bronchitis. When to Seek Medical Care When to call the doctor for bronchitis Although most cases of bronchitis resolve on their own, some people may have complications; however, their health care practitioner can relieve some of these symptoms.
Severe coughing that interferes with rest or sleep can be reduced with prescription cough medications. Wheezing may respond to an inhaler with albuterol (Proventil, Ventolin) or fluticasone and salmeterol (Advair), which dilates the airways. If fever continues beyond 4 to 5 days, see the doctor for a physical examination to rule out pneumonia. See a health care practitioner if the patient is coughing up blood, rust-colored sputum, or an increased amount of green phlegm. When to go to the hospital for bronchitis If the patient experiences difficulty breathing with or without wheezing and they cannot reach their doctor, go to a hospital's emergency department for evaluation and treatment. Bronchitis Diagnosis Doctors diagnose bronchitis generally on the basis of symptoms and a physical examination. Usually no blood tests are necessary. If the doctor suspects the patient has pneumonia, a chest X-ray may be ordered. Doctors may measure the patient's oxygen saturation (how well oxygen is reaching blood cells) using a sensor placed on a finger. This is referred to as pulse oximetry. Sometimes a doctor may order an examination and/or culture of a sample of phlegm that is coughed up to look for bacteria. Bronchitis Treatment Bronchitis Self-Care at Home By far, the majority of cases of bronchitis stem from viral infections. This means that most cases of bronchitis are short-term and require nothing more than treatment of symptoms to relieve discomfort. Antibiotics will not cure a viral illness. Experts in in the field of infectious disease have been warning for years that overuse of antibiotics is allowing many bacteria to become resistant to the antibiotics available. Doctors often prescribe antibiotics because they feel pressured by patient's expectations to receive them. This expectation has been fueled by both misinformation in the media and marketing by drug companies. Don't expect to receive a prescription for an antibiotic if your infection is caused by a virus. Acetaminophen (Tylenol), aspirin, ibuprofen (Motrin, Nuprin, Advil), or naproxen (Aleve) will help with fever and muscle aches. Drinking fluids is very important because fever causes the body to lose fluid faster. Lung secretions will be thinner and easier to clear when the patient is well hydrated. A cool mist vaporizer or humidifier can help decrease bronchial irritation. An over-the-counter (OTC) cough suppressant may be helpful. Preparations with guaifenesin (Robitussin, Breonesin, Mucinex) will loosen secretions; dextromethorphan-the "DM" in most over the counter medications (Benylin, Pertussin, Trocal, Vicks 44) suppresses cough. Natural treatments for bronchitis include honey, lemon, ginger, bay leaf, and almonds. Each of these foods has properties that reportedly reduce symptoms of bronchitis. Consult your health care practitioner before taking or using any natural remedies. Bronchitis Medical Treatment Treatment of bronchitis can differ depending on the suspected cause. Medications to help suppress the cough or loosen and clear secretions may be helpful. If the patient has severe coughing spells they cannot control, see the doctor for prescription strength cough suppressants. In some cases only these stronger cough suppressants can stop a vicious cycle of coughing leading to more irritation of the bronchial tubes, which in turn causes more coughing.
Bronchodilator inhalers will help open airways and decrease wheezing. Though antibiotics play a limited role in treating bronchitis, they become necessary in some situations. In particular, if the doctor suspects a bacterial infection, antibiotics will be prescribed. People with chronic lung problems also usually are treated with antibiotics. In rare cases, the patient may be hospitalized if they experience breathing difficulty that doesn't respond to treatment. This usually occurs because of a complication of bronchitis, not bronchitis itself. Bronchitis Follow-up The affected individual should follow up with their doctor within a week after treatment for bronchitis, or sooner if the symptoms worsen or do not improve. Call the doctor's office if any new problems occur. Bronchitis Prevention Stop smoking. The dangers of secondhand smoke are well documented. Children should never be exposed to secondhand smoke inside the home. Avoid exposure to irritants. Proper protection in the workplace is vital to preventing exposure. Avoiding long exposure to air pollution from heavy traffic may help prevent bronchitis.
ASTHAMA
What is asthma?
Asthma is a chronic inflammation of the bronchial tubes (airways) that causes swelling and narrowing (constriction) of the airways. The result is difficulty breathing. The bronchial narrowing is usually either totally or at least partially reversible with treatments. Bronchial tubes that are chronically inflamed may become overly sensitive to allergens (specific triggers) or irritants (nonspecific triggers). The airways may become "twitchy" and remain in a state of heightened sensitivity. This is called "bronchial hyperreactivity" (BHR). It is likely that there is a spectrum of bronchial hyperreactivity in all individuals. However, it is clear that asthmatics and allergic individuals (without apparent asthma) have a greater degree of bronchial hyperreactivity than nonasthmatic and nonallergic people. In sensitive individuals, the bronchial tubes are more likely to swell and constrict when exposed to triggers such as allergens, tobacco smoke, or exercise. Amongst asthmatics, some may have mild BHR and no symptoms while others may have severe BHR and chronic symptoms. Asthma affects people differently. Each individual is unique in their degree of reactivity to environmental triggers. This naturally influences the type and dose of medication prescribed, which may vary from one individual to another.
The many faces of asthma
The many potential triggers of asthma largely explain the different ways in which asthma can present. In most cases, the disease starts in early childhood from 2-6 years of age. In this age group, the cause of asthma is often linked to exposure to allergens, such as dust mites, tobacco smoke, and viral respiratory infections. In very young children, less than 2 years of age, asthma can be difficult to diagnose with certainty. Wheezing at this age often follows a viral infection and might disappear
later, without ever leading to asthma. Asthma, however, can develop again in adulthood. Adultonset asthma occurs more often in women, mostly middle-aged, and frequently follows a respiratory tract infection. The triggers in this group are usually nonallergic in nature.
Types: allergic (extrinsic) and nonallergic (intrinsic) asthma
Your doctor may refer to asthma as being "extrinsic" or "intrinsic." A better understanding of the nature of asthma can help explain the differences between them. Extrinsic, or allergic asthma, is more common (90% of all cases) and typically develops in childhood. Approximately 80% of children with asthma also have documented allergies. Typically, there is a family history of allergies. Additionally, other allergic conditions, such as nasal allergies or eczema, are often also present. Allergic asthma often goes into remission in early adulthood. However, in 75% of cases, the asthma reappears later. Intrinsic asthma represents about 10% of all cases. It usually develops after the age of 30 and is not typically associated with allergies. Women are more frequently involved and many cases seem to follow a respiratory tract infection. The condition can be difficult to treat and symptoms are often chronic and year-round.
Typical asthma symptoms and signs
The symptoms of asthma vary from person to person and in any individual from time to time. It is important to remember that many of these symptoms can be subtle and similar to those seen in other conditions. All of the symptoms mentioned below can be present in other respiratory, and sometimes, in heart conditions. This potential confusion makes identifying the settings in which the symptoms occur and diagnostic testing very important in recognizing this disorder. The following are the four major recognized asthma symptoms: Shortness of breath, especially with exertion or at night Wheezing is a whistling or hissing sound when breathing out Coughing may be chronic, is usually worse at night and early morning, and may occur after exercise or when exposed to cold, dry air Chest tightness may occur with or without the above symptoms Asthma fact Asthma is classified according to the frequency and severity of symptoms, or "attacks," and the results of pulmonary (lung) function tests. 30% of affected patients have mild, intermittent (less than two episodes a week) symptoms of asthma with normal breathing tests 30% have mild, persistent (two or mores episodes a week) symptoms of asthma with normal or abnormal breathing tests 40% have moderate or severe, persistent (daily or continuous) symptoms of asthma with abnormal breathing tests
How does asthma affect breathing?
Asthma causes a narrowing of the breathing airways, which interferes with the normal movement of air in and out of the lungs. Asthma involves only the bronchial tubes and does not affect the air sacs or the lung tissue. The narrowing that occurs in asthma is caused by three major factors: inflammation, bronchospasm, and hyperreactivity. Inflammation The first and most important factor causing narrowing of the bronchial tubes is inflammation. The bronchial tubes become red, irritated, and swollen. This inflammation increases the thickness of the wall of the bronchial tubes and thus results in a smaller passageway for air to flow through. The inflammation occurs in response to an allergen or irritant and results from the action of chemical mediators (histamine, leukotrienes, and others). The inflamed tissues produce an excess amount of "sticky" mucus into the tubes. The mucus can clump together and form "plugs" that can clog the smaller airways. Specialized allergy and inflammation cells (eosinophils and white blood cells), which accumulate at the site, cause tissue damage. These damaged cells are shed into the airways, thereby contributing to the narrowing. Bronchospasm The muscles around the bronchial tubes tighten during an attack of asthma. This muscle constriction of the airways is called bronchospasm. Bronchospasm causes the airway to narrow further. Chemical mediators and nerves in the bronchial tubes cause the muscles to constrict. Bronchospasm can occur in all humans and can be brought on by inhaling cold or dry air. Hyperreactivity (hypersensitivity) In patients with asthma, the chronically inflamed and constricted airways become highly sensitive, or reactive, to triggers such as allergens, irritants, and infections. Exposure to these triggers may result in progressively more inflammation and narrowing. The combination of these three factors results in difficulty with breathing out, or exhaling. As a result, the air needs to be forcefully exhaled to overcome the narrowing, thereby causing the typical "wheezing" sound. People with asthma also frequently "cough" in an attempt to expel the thick mucus plugs. Reducing the flow of air may result in less oxygen passing into the bloodstream, and if very severe, carbon dioxide may dangerously accumulate in the blood.
Acute asthma attack
An acute, or sudden, asthma attack is usually caused by an exposure to allergens or an upperrespiratory-tract infection. The severity of the attack depends on how well your underlying asthma is being controlled (reflecting how well the airway inflammation is being controlled). An acute attack is potentially life-threatening because it may continue despite the use of your usual quickrelief medications (inhaled bronchodilators). Asthma that is unresponsive to treatment with an inhaler should prompt you to seek medical attention at the closest hospital emergency room or your asthma specialist office, depending on the circumstances and time of day. Asthma attacks do not stop on their own without treatment. If you ignore the early warning signs, you put yourself at risk of developing status asthmaticus.
Common asthma triggers: Allergens
"seasonal" pollens year-round dust mites, molds, pets, and insect parts
foods, such as fish, egg, peanuts, nuts, cow's milk, and soy additives, such as sulfites work-related agents, such as latex, epoxides, and formaldehyde Allergy fact About 80% of children and 50% of adults with asthma also have allergies. Irritants respiratory infections, such as those caused by viral "colds," bronchitis, and sinusitis drugs, such as aspirin, other NSAIDs (nonsteroidal antiinflammatory drugs), and beta blockers (used to treat blood pressure and other heart conditions) tobacco smoke outdoor factors, such as smog, weather changes, and diesel fumes indoor factors, such as paint, detergents, deodorants, chemicals, and perfumes nighttime GERD (gastroesophageal reflux disorder) exercise, especially under cold dry conditions work-related factors, such as chemicals, dusts, gases, and metals emotional factors, such as laughing, crying, yelling, and distress hormonal factors, such as in premenstrual syndrome
Asthma Dos And Donts - The Key To Living With Asthma
If you keep the asthma dos and donts in mind, you are less likely to face asthma attacks. There are not any sure cures for this illness of the respiratory system. But the key to keeping it in check is to make sure that you make some minor alterations to you lifestyle. A lot of people have benefitted by taking regular medication, doing breathing exercises and avoiding certain triggers. The Donts: Do not eat certain food items like refined flour, milk products and white sugar which cause mucus to form. Mucus blocks the air pathways. Therefore, some minor changes in your diet might be called for. Children should keep away from chocolates. Most people refuse to accept that the breathing disorder they have is asthma. They just brush it aside as breathlessness or some minor breathing problem. It is better to accept and take the necessary medication before it becomes chronic. Do not expose yourself to cold weather. When cold hits the chest, the throat and the back, it can bring on an attack. So keep yourself warm at all times. The air-conditioning system in the house and offices can also aggravate asthmatic symptoms. The vents and filters should be periodically cleaned. Smoking actively or even passively can trigger an asthma attack. Avoid smoking and take care not to expose yourself to smoke. Pets that shed hair should not be kept at home. The hair of these pets and their excretions are also known to trigger asthma.
The Dos: One main culprit that sets off asthma is dust. There should be adequate ventilation in the house to ensure low moisture levels. Dust mites aggravate asthma attacks; therefore the house should be regularly vacuumed. Beddings, pillow cases and quilts should be washed frequently. Bathrooms too, should be well-ventilated. Excess moisture can breed mildew. Constant exposure to mildew is not good for people with breathing ailments. In case of asthma, you should identify the trigger that brings on an attack. Some allergens might cause only minimal reaction whereas other allergens might cause a full-fledged attack. It is better to avoid exposure to these triggers. It is better to eat several light meals a day. There is no need for a particular diet but the daily intake of food should include fresh fruit and vegetables. Whole grain cereals are also considered beneficial. Learn to identify the early warning signs of an attack. Medicines or breathing exercises can then ensure that it does not become a full-blown attack. Many people benefit from this single cue and are able to manage their asthma better. The asthma dos and donts mentioned above will ensure that your problem is kept control and you can live a normal life. Most asthmatics these days are barely dependent on inhalers and other medicines. These points are not only simple to follow but definitely beneficial if followed. So go ahead, and live a life free from asthma.
Asthma Natural Remedies - Natures Alternative To Curing Asthma
Of all the cures that have been discovered to relieve people from this breathing ailment, the more widely accepted are the asthma natural remedies. The main reason for its popularity is that it is natural. The other factor for its success is that there are no side effects. In recent times, more and more people are finding relief in these natural methods. A Few Natural Alternatives Of Asthma Treatment Acupressure: Acupressure has its origins in China. Unlike acupuncture, instead of needles, pressure is applied by the fingers at certain energy points in the body. These energy points, according to the Chinese, hold the key to correcting several body ailments. Ayurveda: Ayurvedic methods of treatment differ from the conventional cure in that ayurveda suggests that asthma is caused due to toxin build-up in the body. This build-up of toxins is attributed to chemical imbalance and improper digestion. Correcting the diet, nutrition, and improving digestion are some of the common methods. Ayurvedic treatment requires the addition of certain herbs in the diet. You might be restricted from consuming dairy products and sugar. Also, cold foods have to be avoided. Yoga: The breathing exercises used in yoga help to clear the lungs and the respiratory passages. Yoga aims at reducing stress and controls your breathing. There are several exercises in yoga that help asthmatic patients. Home Remedies: There are several home remedies that help in combating the effects of asthma. These are the methods that will purely keep the symptoms at bay and are not to be considered as a cure. These are just concoction of things available at home that help to relieve a person from asthmatic symptoms. Eat a ripe banana, warmed on a slow flame, sprinkled with black pepper. Asthmatic pains are known to subside with this. A glass of lime juice with two teaspoons of ginger juice and consumed daily is known to reduce
the frequency of attacks. Drink milk with a teaspoon of honey before sleeping. Honey has asthma controlling properties. Drinking a glass of milk with a teaspoon of turmeric powder, two to three times a day is known as an effective asthma remedy. Another home remedy requires you to boil a glass of water with two teaspoons of fenugreek seeds. This should be reduced to one-third its quantity. Drink this solution to help relieve you. Drinking eight to ten glasses of water a day allows the body to get rid of the accumulated toxins. It will also help keep the secretions loose and therefore can be easily removed. Are These Natural Remedies Safe? As long as these natural remedies in no way interfere with the medications, they are safe to be tried. But you should inform your doctor if you are taking any alternative cure, simply because certain herbs may interfere with the medicines prescribed by your doctor. Most of these asthma natural medicines are not considered to have any adverse side-effects. However, it is always better to be cautious!
TB
What is tuberculosis? Tuberculosis (TB) is an infectious disease caused by bacteria whose scientific name is Mycobacterium tuberculosis. It was first isolated in 1882 by a German physician named Robert Koch who received the Nobel Prize for this discovery. TB most commonly affects the lungs but also can involve almost any organ of the body. Many years ago, this disease was referred to as "consumption" because without effective treatment, these patients often would waste away. Today, of course, tuberculosis usually can be treated successfully with antibiotics. There is also a group of organisms referred to as atypical tuberculosis. These involve other types of bacteria that are in the Mycobacterium family. Often, these organisms do not cause disease and are referred to as "colonizers" because they simply live alongside other bacteria in our bodies without causing damage. At times, these bacteria can cause an infection that is sometimes clinically like typical tuberculosis. When these atypical mycobacteria cause infection, they are often very difficult to cure. Often, drug therapy for these organisms must be administered for one and a half to two years and requires multiple medications.
How does a person get TB?
A person can become infected with tuberculosis bacteria when he or she inhales minute particles of infected sputum from the air. The bacteria get into the air when someone who has a tuberculosis lung infection coughs, sneezes, shouts, or spits (which is common in some cultures). People who are nearby can then possibly breathe the bacteria into their lungs. You don't get TB by just touching the clothes or shaking the hands of someone who is infected. Tuberculosis is spread (transmitted) primarily from person to person by breathing infected air during close contact. There is a form of atypical tuberculosis, however, that is transmitted by drinking unpasteurized milk. Related bacteria, called Mycobacterium bovis, cause this form of TB. Previously, this type of bacteria was a major cause of TB in children, but it rarely causes TB now since most milk is pasteurized (undergoes a heating process that kills the bacteria). What happens to the body when a person gets TB? When the inhaled tuberculosis bacteria enter the lungs, they can multiply and cause a local lung infection (pneumonia). The local lymph nodes associated with the lungs may also become involved
with the infection and usually become enlarged. The hilar lymph nodes (the lymph nodes adjacent to the heart in the central part of the chest) are often involved. In addition, TB can spread to other parts of the body. The body's immune (defense) system, however, can fight off the infection and stop the bacteria from spreading. The immune system does so ultimately by forming scar tissue around the TB bacteria and isolating it from the rest of the body. Tuberculosis that occurs after initial exposure to the bacteria is often referred to as primary TB. If the body is able to form scar tissue (fibrosis) around the TB bacteria, then the infection is contained in an inactive state. Such an individual typically has no symptoms and cannot spread TB to other people. The scar tissue and lymph nodes may eventually harden, like stone, due to the process of calcification of the scars (deposition of calcium from the bloodstream in the scar tissue). These scars often appear on X-rays and imaging studies like round marbles and are referred to as a granuloma. If these scars do not show any evidence of calcium on X-ray, they can be difficult to distinguish from cancer. Sometimes, however, the body's immune system becomes weakened, and the TB bacteria break through the scar tissue and can cause active disease, referred to as reactivation tuberculosis or secondary TB. For example, the immune system can be weakened by old age, the development of another infection or a cancer, or certain medications such as cortisone, anticancer drugs, or certain medications used to treat arthritis or inflammatory bowel disease. The breakthrough of bacteria can result in a recurrence of the pneumonia and a spread of TB to other locations in the body. The kidneys, bone, and lining of the brain and spinal cord (meninges) are the most common sites affected by the spread of TB beyond the lungs. How common is TB, and who gets it? Over 8 million new cases of TB occur each year worldwide. In the United States, it is estimated that 10-15 million people are infected with the TB bacteria, and 22,000 new cases of TB occur each year. Anyone can get TB, but certain people are at higher risk, including people who live with individuals who have an active TB infection, poor or homeless people, foreign-born people from countries that have a high prevalence of TB, nursing-home residents and prison inmates, alcoholics and intravenous drug users, people with diabetes, certain cancers, and HIV infection (the AIDS virus), health-care workers.
There is no strong evidence for a genetically determined (inherited) susceptibility for TB.
What are the symptoms and signs of tuberculosis?
As previously mentioned, TB infection usually occurs initially in the upper part (lobe) of the lungs. The body's immune system, however, can stop the bacteria from continuing to reproduce. Thus, the immune system can make the lung infection inactive (dormant). On the other hand, if the body's immune system cannot contain the TB bacteria, the bacteria will reproduce (become active or reactivate) in the lungs and spread elsewhere in the body. It may take many months from the time the infection initially gets into the lungs until symptoms develop. The usual symptoms that occur with an active TB infection are a generalized tiredness or weakness, weight loss, fever, and night sweats. If the infection in the lung worsens, then further symptoms can include coughing, chest pain, coughing up of sputum (material from the lungs) and/or blood, and shortness of breath. If the infection spreads beyond the lungs, the symptoms will
depend upon the organs involved. Is there a vaccine against tuberculosis? Bacille Calmette Gurin, also known as BCG, is a vaccine given throughout many parts of the world. It is derived from an atypical Mycobacterium but offers some protection from developing active tuberculosis, especially in infants and children. This vaccination is believed to be important in parts of the world where TB is quite common. This is not the case in the United States, and the vaccine is not routinely administered in the U.S. When BCG has been administered, future PPD and Tine skin tests remain positive and can cause some confusion when trying to diagnose TB. It is also important to realize that even with a BCG vaccine in childhood, tuberculosis can still occur in an adult exposed to the tuberculosis bacteria, which calls into question the real utility and effectiveness of this vaccination. A new blood test is now available that can help distinguish between a prior BCG vaccine and a positive PPD due to TB infection (QuantiFERON-TB Gold). This test involves mixing the patient's blood with substances that produce a TB-like immune response. After a period of time, the immune cells, if infected with TB, produce interferon-gamma, a protein produced by the body to defend against an infection. This test, like most, is not perfect, but with the proper clinical information can help distinguish a real TB infection from a positive reaction on the test due to a prior BCG vaccine.
What is the treatment for tuberculosis?
A person with a positive skin test, a normal chest X-ray, and no symptoms most likely has only a few TB germs in an inactive state and is not contagious. Nevertheless, treatment with an antibiotic may be recommended for this person to prevent the TB from turning into an active infection. The antibiotic used for this purpose is called isoniazid (INH). If taken for six to 12 months, it will prevent the TB from becoming active in the future. In fact, if a person with a positive skin test does not take INH, there is a 5%-10% lifelong risk that the TB will become active. Taking isoniazid can be inadvisable (contraindicated) during pregnancy or for those suffering from alcoholism or liver disease. Also, isoniazid can have side effects. The side effects occur infrequently, but a rash can develop, and the individual can feel tired or irritable. Liver damage from isoniazid is a rare occurrence and typically reverses once the drug is stopped. Very rarely, however, especially in older people, the liver damage (INH hepatitis) can even be fatal. It is important therefore, for the doctor to monitor a patient's liver by periodically ordering blood tests called "liver function tests" during the course of INH therapy. Another side effect of INH is a decreased sensation in the extremities referred to as a peripheral neuropathy. This can be avoided by taking vitamin B6 (pyridoxine), and this is often prescribed along with INH. A person with a positive skin test along with an abnormal chest X-ray and sputum evidencing TB bacteria has active TB and is contagious. As already mentioned, active TB usually is accompanied by symptoms, such as a cough, fever, weight loss, and fatigue. Active TB is treated with a combination of medications along with isoniazid. Rifampin (Rifadin), ethambutol (Myambutol), and pyrazinamide are the drugs commonly used to treat active TB in conjunction with isoniazid (INH). Four drugs are often taken for the first two months of therapy to help kill any potentially resistant strains of bacteria. Then the number is usually reduced to two drugs for the remainder of the treatment based on drug-sensitivity testing that is usually available by this time in the course. Streptomycin, a drug that is given by injection, may be used as well, particularly when the disease is extensive and/or the patients do not take their oral medications reliably (termed "poor compliance"). Treatment usually lasts for many months and sometimes for years. Successful treatment of TB is dependent largely on the compliance of the patient. Indeed, the failure of a patient to take the medications as prescribed is the most important cause of failure to cure the TB infection. In some locations, the health department demands direct monitoring of
patient compliance with therapy. Surgery on the lungs may be indicated to help cure TB when medication has failed, but in this day and age, surgery for TB is unusual. Treatment with appropriate antibiotics will usually cure the TB. Without treatment, however, tuberculosis can be a lethal infection. Therefore, early diagnosis is important. Those individuals who have been exposed to a person with TB, or suspect that they have been, should be examined by a doctor for signs of TB and screened with a TB skin test. What is drug-resistant TB? Drug-resistant TB (TB that does not respond to drug treatment) has become a very serious problem in recent years in certain populations. For example, INH-resistant TB is seen among patients from Southeast Asia. The presence of INH-like substances in the cough syrups in that part of the world may play a role in causing the INH resistance. Drug-resistant cases are also often seen in prison populations. However, the major reason for the development of resistance is poorly managed TB care. This can result from poor patient compliance, inappropriate dosing or prescribing of medication, poorly formulated medications, and/or an inadequate supply of medication. Multidrugresistant tuberculosis (MDR-TB) refers to organisms that are resistant to at least two of the first-line drugs, INH and Rifampin. More recently, extensively (extremely) drug-resistant tuberculosis (XDRTB) has emerged. These bacteria are also resistant to three or more of the second-line treatment drugs. XDR-TB is seen throughout the world but is most frequently seen in the countries of the former Soviet Union and Asia. Preventing XDR-TB from spreading is essential. The World Health Organization (WHO) recommends improving basic TB care to prevent emergence of resistance and the development of proper laboratories for detection of resistant cases. When drug-resistant cases are found, prompt, appropriate treatment is required. This will prevent further transmission. Collaboration of HIV and TB care will also help limit the spread of tuberculosis, both sensitive and resistant strains.
What's in the future for TB?
Conceivably, TB could have been eliminated by effective treatment, vaccinations, and public-health measures by the year 2000. However, the emergence of HIV changed the whole picture. Because of HIV, a tremendous increase in the frequency (incidence) of TB occurred in the '80s and throughout the '90s. This increase in TB happened because suppression of the body's immune (defense) system by HIV allowed TB to occur as a so-called opportunistic infection. With the increasing HIV epidemic in Africa, serious concerns are being raised about the development of MDR-TB and XDRTB in this population. Hopefully, control of HIV in the future will check this resurgence of tuberculosis. The epidemic of HIV and TB has been a deadly combination especially on the African continent. A recent study comparing prophylactic regimens for prevention of active TB in HIV-infected individuals has shown effectiveness, however, the distribution of medication for both of these disease in the third world remains problematic. EVS
S-ar putea să vă placă și
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Quiz RespiratoryDocument123 paginiQuiz RespiratoryMedShare100% (23)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- CKD NCPDocument4 paginiCKD NCPArlene Macatangay100% (1)
- Community Acquired Pneumonia. FinalDocument48 paginiCommunity Acquired Pneumonia. FinalHampson Malekano100% (2)
- PaediatricsDocument363 paginiPaediatricsWani FarkhandaÎncă nu există evaluări
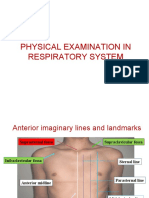
- Physical Examination in Respiratory SystemDocument58 paginiPhysical Examination in Respiratory SystemMarian0% (1)
- 15 Respiratory AcidosisDocument40 pagini15 Respiratory AcidosisJoel Topf100% (8)
- Pcap C CaseDocument81 paginiPcap C CaseAyaBasilio70% (10)
- OET-Preparation-Book - Reading-Sub-Test - Volume-1-Anna-HartfordDocument57 paginiOET-Preparation-Book - Reading-Sub-Test - Volume-1-Anna-HartfordGeorgianNeagu100% (1)
- Assessing and Managing Ineffective Airway ClearanceDocument3 paginiAssessing and Managing Ineffective Airway ClearanceNelle Agni100% (1)
- Cardiovascular & Respiratory System Immunology - PPT (Compatibility Mode)Document64 paginiCardiovascular & Respiratory System Immunology - PPT (Compatibility Mode)Mwanja MosesÎncă nu există evaluări
- Dr. S.K. Haldar's Lectures On Industrial Health For AFIH Students - Occu. Lung Dis Asbestosis Silicosis ByssinosisDocument26 paginiDr. S.K. Haldar's Lectures On Industrial Health For AFIH Students - Occu. Lung Dis Asbestosis Silicosis ByssinosisDr. Prakash Kulkarni100% (2)
- 7th Class Respiratory SystemDocument14 pagini7th Class Respiratory SystemCas Tan100% (1)
- Warren BuffetDocument1 paginăWarren BuffetDipen VyasÎncă nu există evaluări
- Warren BuffetDocument1 paginăWarren BuffetDipen VyasÎncă nu există evaluări
- Dabur SWOT AnalysisDocument5 paginiDabur SWOT AnalysisDipen VyasÎncă nu există evaluări
- Dabur SWOT AnalysisDocument5 paginiDabur SWOT AnalysisDipen VyasÎncă nu există evaluări
- Dabur SWOT AnalysisDocument5 paginiDabur SWOT AnalysisDipen VyasÎncă nu există evaluări
- Lifebuoy HardDocument6 paginiLifebuoy HardDipen VyasÎncă nu există evaluări
- Exim BobDocument8 paginiExim BobDipen VyasÎncă nu există evaluări
- Focus MKTDocument1 paginăFocus MKTDipen VyasÎncă nu există evaluări
- How To Become An IASDocument18 paginiHow To Become An IASDipen VyasÎncă nu există evaluări
- The Export Promotion Councils WordDocument4 paginiThe Export Promotion Councils Wordshahbhaumik_er1949Încă nu există evaluări
- How To Become An IASDocument18 paginiHow To Become An IASDipen VyasÎncă nu există evaluări
- Cystic Fibrosis Signs and Symptoms ExplainedDocument3 paginiCystic Fibrosis Signs and Symptoms ExplainedsakthiprimeÎncă nu există evaluări
- QB U10 Update2020 EngDocument11 paginiQB U10 Update2020 EngAlex FungÎncă nu există evaluări
- Penyakit Paru Obstruktif Kronik (PPOK) : Fakultas Kedokteran Universitas Sultan Khairun (Unkhair)Document53 paginiPenyakit Paru Obstruktif Kronik (PPOK) : Fakultas Kedokteran Universitas Sultan Khairun (Unkhair)WahyunitadotokaÎncă nu există evaluări
- Test Pitanja Iz Respiratornog Sistema Sa PrevodomDocument10 paginiTest Pitanja Iz Respiratornog Sistema Sa PrevodomzerohajdukÎncă nu există evaluări
- Anatomy and Physiology of The Respiratory SystemDocument14 paginiAnatomy and Physiology of The Respiratory SystemAmore BuenafeÎncă nu există evaluări
- NURS1108 Lecture 14 - Respiratory System PART 1 of 2Document62 paginiNURS1108 Lecture 14 - Respiratory System PART 1 of 2Jacia’s SpaceshipÎncă nu există evaluări
- Material - Engleza - Medicina Anul 1, Sem 2Document58 paginiMaterial - Engleza - Medicina Anul 1, Sem 2Gabriella CoadaÎncă nu există evaluări
- Micro - Respiratory SystemDocument3 paginiMicro - Respiratory SystemKaren ValdezÎncă nu există evaluări
- Physiology Haq 2nd EdDocument19 paginiPhysiology Haq 2nd Edsathvikamothe0103Încă nu există evaluări
- Anatomy Final Exam Notes PDFDocument45 paginiAnatomy Final Exam Notes PDFLydia LalalandÎncă nu există evaluări
- National Tracheostomy Care Guidelines 2023Document43 paginiNational Tracheostomy Care Guidelines 2023nurulÎncă nu există evaluări
- Ineffective Airway Clearance Nursing Care PlanDocument2 paginiIneffective Airway Clearance Nursing Care Planrois romaÎncă nu există evaluări
- Case Study 5 (Respiratory) - COPDDocument6 paginiCase Study 5 (Respiratory) - COPDSamantha AquinoÎncă nu există evaluări
- 4 - Batteries Material Safety Data SheetDocument6 pagini4 - Batteries Material Safety Data Sheethafed baccoucheÎncă nu există evaluări
- Bronchial AsthmaDocument7 paginiBronchial AsthmaKarolien Faye DongaÎncă nu există evaluări
- NURSING INTERVENTIONS FOR INEFFECTIVE BREATHING PATTERNDocument7 paginiNURSING INTERVENTIONS FOR INEFFECTIVE BREATHING PATTERNDanica Kate GalleonÎncă nu există evaluări
- Nursing Process Care Plan For Ineffective Breathing Pattern Assessment Diagnosis Planning Implementation EvaluationDocument19 paginiNursing Process Care Plan For Ineffective Breathing Pattern Assessment Diagnosis Planning Implementation EvaluationZIANAH JOY FAMYÎncă nu există evaluări
- Capitol University College of Nursing: in Partial Fulfillment in Related Learning Experince (RLE8)Document16 paginiCapitol University College of Nursing: in Partial Fulfillment in Related Learning Experince (RLE8)Jongjong Efondo RamosoÎncă nu există evaluări