Documente Academic
Documente Profesional
Documente Cultură
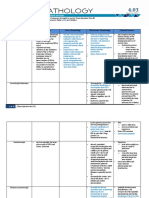
Endocrine Chart
Încărcat de
Niki NikolićDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Endocrine Chart
Încărcat de
Niki NikolićDrepturi de autor:
Formate disponibile
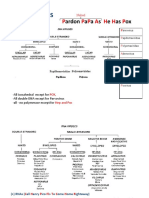
Endocrine/Reproductive Hormones Master List Name CRH Origin Hypoth alamus, and during pregnancy from placenta and
fetus. Synthesis N/A Target Anterior pituitary Function Stimulate the anterior pituitary gland to synthesize and secrete ACTH through a cAMP pathway. Inhibits LH secretion and may mediate inhibitory action of stress on female fertility. Elevated CRH predicts short gestation, and CRH potentiates uterine contracture response to prostaglandins and oxytocin. Stimulates synthesis and secretion of LH and FSH (binds to Gaq to stimulate PLC to make IP3 and DAG to activate PKC). Secretion is pulsatile, frequency and amplitude of pulse will determine the amount of LH and FSH released. + Feedback/ Stimulus Pulsatile secretion stimulated by norepinephrine, serotonin, and acetylcholine; also increased by acute stress, fever, trauma, infection. Fetal cortisol amplifies placental CRH synthesis. Stimulated by norepinephrine and estrogen (ovulatory phase of menstrual cycle for the latter). - Feedback/ Inhibition Inhibited by ACTH, cortisol, GABA, and endorphins. Pathology Tertiary Addisons or Cushings
GnRH
Hypothalam us
N/A
Anterior pituitary gonadotroph cells
Inhibited by inhibin, testosterone, estrogen and progesterone (during follicular and luteal phase of menstrual cycle), dopamine, melatonin, and stress.
Kallmans Syndrome: developmental disorder- aplasia of the olfactory lobes, source of GnRH neurons (so no GnRH production or secretion). Anosmia (no smell) and microphallus.
Emil Fernando
Brett Segel
GHRH
Hypothalam us
N/A
Anterior pituitary somatotroph cells.
Stimulates the secretion of GH.
Stimulated by acetylcholine, alphaadrenergic and dopaminergic stimuli; sleep and stress also stimulate GHRH. Secretion is under serotonergic control. Low levels of T3/T4; secretion occurs in a diurnal rhythm. Stress, infection, temp. and metabolic state can increase TSH stimulation. Starvation? (in ppt slides) .
Inhibits its own release via an ultrashort feedback loop (GHRH inhibits itself); glucose and FFAs also inhibit. N/A
Hypothalamic dwarfism, which can be treated by administering GH.
PRF
Hypothalam us
N/A
Anterior pituitary
Stimulates Prolactin release
N/A
TRH
Hypothalam us
Tripeptide synthesized from prohormone in arcuate nucleus and median eminence neurons; short half life (<5 mins) and low circulating plasma levels.
Anterior pituitary G protein-linked receptors on thyrotroph cells to stimulate TSH.
Stimulates thyrotropin (TSH) synthesis and release. Some prolactin stimulation.
T3/T4 (minor, importance under debate).
TRH can cause a pathological secretion of GH and/or prolactin.
Emil Fernando
Brett Segel
Somatostatin
Hypothalam us and delta cells of the pancreas
N/A
Anterior pituitary and G cells of stomach.
Inhibits GH release from anterior pituitary. Inhibits all other anterior pituitary hormones as well, really. Plays key role in regulating balance of insulin and glucagon. Also inhibits gastrin secretion from G cells. Inhibits secretion of anterior pituitary hormones.
Secretion stimulated by glucose and free fatty acids. Secretion from hypothalamus is induced by somatomedins to shut down GH axis. Important component of many negative feedback pathways. See other hormones.
Secretion inhibited by insulin.
N/A
Dopamine
Hypothalam us
N/A
Anterior pituitary gland
N/A
N/A
ACTH
Corticotroph cells of the anterior pituitary
Synthesized as proopiomelanocortin, which also contains blipotropin and b-MSH opioid peptides.
Binds to receptors on the adrenal cortex.
Promotes growth and Stimulated by activity in the zona CRH through a fasiculata, such as increased cAMP pathway. synthesis of StAR protein Secretion may be (gets cholesterol into diurnal (highest mitochondria) and Cyp450 2-4 hrs before enzymes that are vital for waking and steroid synthesis; stimulates lowest when cortisol production. going to sleep) or cyclic. IL-1 can also cause secretion. Under severe stress, ADH will also stimulate secretion.
Inhibited by cortisol (makes CRH receptors less responsive).
Can have tertiary hypothalamic problem (CRH adenoma) or secondary pituitary problem (Cushings Disease). Will cause hyperpigmentation due to overproduction of MSH and melanin.
Emil Fernando
Brett Segel
Prolactin
Anterior pituitary lactotrophs or mammotrop hs. Numbers increase during pregnancy due to elevated estrogen. They possess dopamine receptors.
N/A
Mammary gland to stimulate milk production.
Causes epithelial cell proliferation and synthesis of milk proteins in mammary glands casein and lactalbumin (breast development and milk production); short loop suppression of gonadotropins (aka, lactationinduced suppression of ovulationbirth control during lactation). Prolactin, cortisol, and insulin are essential for continued milk production.
TRH, Prolactinreleasing peptide (PrRP), or VIP in response to stimuli (stress, suckling, etc.); tonic suppression is dominant mode of regulation of PRL axis. Estrogen effects exerted on the pituitary sensitize it to PRFs (pregnancy)
Inhibited by dopamine.
Hyperprolacti nemia: caused by adenomas of the pituitary. Most common hypothalamichypophyseal disorder. Can be drug induced (by dopamine inhibitors) or virally induced (Herpes zoster stimulates nipples). Primary hypothyroidism with high TRH levels can cause this as well. You will get galactorrhea, be anovulatory, and have amenorrhea in the female. In males, youll have gynecomastia and impotence. Both can have visual impairment and headaches due to tumor size.
Emil Fernando
Brett Segel
GH
Anterior pituitary somatotroph cells
N/A
Acts on the liver, muscle, and adipose tissue, chondrocytes, bone, heart, lung, kidney, pancreas, intestine, skin, and CT to increase growth and development. Liver will also make somatomedins (IGF-1 and 2) to help mediate these effects.
Aids in postnatal somatic growth and development (increases growth of all major organs and linear bone growth at epiphyses). Also sensitizes gonads to LH and FSH at puberty. Helps to maintain normal lean body mass in adults. Increases gluconeogenesis, glycogenolysis, lipolysis, and protein synthesis.
Secretion is stimulated by GHRH.
Secretion is inhibited by somatostatin and through pituitary negative feedback via somatomedins.
GH is diabetogenic (decreases muscle uptake of glucose and increases insulin resistance in muscle, fat, and liver). Deficiency causes dwarfism. Gigantism if GH overproduction before closure of epiphysis and acromegaly (ossification of bones, bulbous nose, enlarged organs, etc.) if overproduction after closure.
Emil Fernando
Brett Segel
TSH
Anterior pituitary thyrotroph cells
Dimeric glycoprotein synthesized by pituitary thyrotroph cells; -subunit identical to that in FSH, LH and human chorionic gonadotropin (hCG), and subunit confers TSH biological activity N/A
Acts on TSH receptors of the Thyroid gland.
Circulating TSH acts TRH acts on its exclusively on its thyroid G protein-linked gland receptors to produce receptors on iodine organification and thyrotroph cells T4/T3 synthesis from to stimulate TSH thyroglobulin; causes Na, (thyrotropin) I, glucose, and amino acid synthesis and uptake by thyroid gland and release (TRHactivates thyroperoxidases stimulated TSH (along with upregulating secretion is other enzymes and actions pulsatile, with for T3/T4 synthesis). Also small rhythm, increases growth and size of slightly higher at thyroid gland. night) Primarily promotes ovulation and luetinization of the ovary (theca and granulosa cells) and stimulation of the Leydig cell function of the testes (testosterone secretion). Pulsatile secretion of GnRH stimulates LH secretion; estrogen surge prior to ovulation also stimulates LH spike.
Secretion suppressed by plasma T3/T4 levels; dopamine and somatostatin can also inhibit TSH secretion.
Graves disease: auto-antibodies to TSH receptor stimulates overproduction of T3/T4. Will have low serum TSH and a goiter. Can also have hypersecreting thyroid adenomas from constitutively active mutant TSH receptors. Resistant ovarian syndrome: lack of ovarian receptors for LH/FSH; have primordial follicle but no primary follicles. High circulating levels of LH/FSH during this time.
LH
Anterior pituitary gonadotroph s
Leydig cells of the testes and theca and granulosa cells of the ovaries.
Continuous secretion of GnRH inhibits LH secretion; gonadal steroids (testosterone and estrogen) decrease synthesis and number of GnRH receptors on target cells.
Emil Fernando
Brett Segel
FSH
Anterior pituitary gonadotroph s
N/A
FSH acts on the Sertoli cells of the testes and the granulosa cells of the ovaries.
MSH
Anterior pituitary: intermediate lobe
Cleavage products of a larger precursor peptide called proopiomelanocortin (POMC)
Melanocytes
Stimulates follicular development and estradiol secretion in ovary and spermatogenesis in seminiferous tubules. Stimulates biosynthesis of proteins (ABPbinds T), upregulates Sertoli cell testosterone receptors and synthesis of p450aromatase enzymes (converts T to estradiol) and inhibin, and increase synthesis of growth factors for spermatogonia, spermatocytes, spermatids, and their motility. Stimulates melanin (pigment) production.
Pulsatile secretion of GnRH activates FSH secretion, along with Activin (activin ONLY works at the pituitary level).
CRH will stimulate its production.
Continuous secretion of GnRH; gonadal steroids (estrogen, testosterone) decreases synthesis and # of receptors on target cells. Follistatin also inhibits by inhibiting Activin. Inhibin inhibits FSH secretion. N/A
N/A
In Addisons disease, high levels of ACTH production also leads to high MSH levels, which causes hyperpigmentation (abnormal darkening of skin).
Emil Fernando
Brett Segel
ADH (Vasopressin)
Posterior pituitary supraoptic nucleus
N/A
Acts on the distal tubule and collecting duct and thick ascending limb (TAL) of the kidney nephron, as well as systemically on vascular smooth muscle.
Acts to conserve body water (inserts aquaporins into collecting duct and distal tubule with V2 receptor, increases Na reabsorption in the TAL); maintenance of ECF osmolality, blood volume, and blood pressure (constricts vascular smooth muscle at V1 receptor))
Stimulated by increases in plasma osmolality (fluids bathing brain induces water loss from osmoreceptor neurons in hypothalamus); 5-10% decrease in blood volume (barorecptors and atrial stretch receptors, RAA) Mainly neural; stimulated by suckling on nipple and vaginal cervical distension during birth and potentially intercourse. Babys cry can stimulate. Estrogen increases number of Oxytocin receptors in the uterus.
Inhibited by low plasma osmolality and by high blood pressure though inhibitory inputs from baroreceptors.
Central Diabetes insipidus. Too little ADH action causes large volumes of hyposmotic urine (low specific gravitypolyuria) and excessive thirst (polydipsia) Nephrogenic Diabetes Insipidus is a failure of the collecting duct to recognize ADH N/A
Oxytocin
Posterior pituitary paraventricu lar nucleus
N/A
Acts on myoepithelial cells of small ducts/alveoli of mammary glands and smooth muscle of uterine myometrium.
Causes milk ejection as part of the suckling reflex (contracts myoepithelial cells around small ducts and alveoli of the mammary gland and lets down the milk into sinuses and nipples). Also stimulates uterine contraction (target is smooth muscle cell of the uterine myometrium). Also released during intercourse; may aid in sperm transport. This works through a Gaq protein to induce PLC to induce the IP3/DAG pathway.
Inhibited by stress (unless it is a conditioned response).
Emil Fernando
Brett Segel
Melatonin
Pineal gland
Made from serotonin (tryptophan seratonin N acetyl seratonin (via N-acetyl transferase, the regulating enzyme melatonin). Immediately secreted after synthesis not stored; synthesis decreases significantly with age (as much as 50% from teenage years to elderly).
Has high affinity for GPCRs that increase intracellular cAMP and also activates an orphan nuclear receptor (like steroid hormones).
Sleep regulation: large doses can resynchronize, reduce jet lag; small repetitive doses may help in seasonal affective disorder (SAD) and for sleep disturbance during tinnitus. Possible antiaging hormone, countering oxidative stress of aging cells; also considered for adjuvant therapy in pro-inflammatory, prooxidative conditions such as fibromalagia, trauma, thermal injury, etc. Cancer: oncostatic in some cancer studies; recent evidence for adjuvant therapy in breast cancer.
Circadian rhythm driven by NE release high at night, low in light. Night time NE release on pineal gland induces synthesis and secretion.
Day time lack of norepinephrine on pineal gland reduces synthesis and secretion. Almost no melatonin at noon.
Supplementation may worsen asthma.
Emil Fernando
Brett Segel
T4/T3
Thyroid gland follicles
Thyroglobulin is T3/T4 is made from amino carried in acids and glucose plasma bound in the ER. Then it to TBG gets shipped to (mainly T4), the follicular albumin lumen. There, (mainly T3), thyroperoxidases and TBPA. organify it to T4 is major oxidized iodine circulating (will get T3, T4, form. T4 is and mono and dideiodinated iodo tyrosines by 5attached to deiodinase in thyroglobulin). the target Then it is taken cells to back into the cell become active through T3. T3 binds psuedopods. Then to proteases will act intracellular on it to release T3/ receptors in T4 (these will go many into the blood) different and mono and ditarget cells; idodotyrosines; the receptors mono and diheterodimerize iodinases will with retinoic then strip off the acid (RXX) iodines from the receptors and tyrosines so they go to the can be recycled. nucleus to act Antithyroid drugs as (propylthiouracil; transcription
T3 is a catabolic hormone. It will increase basal metabolic rate, cardiac output (decreased peripheral vascular resistance with increased myocardial contractility), ventilation, food intake, mobilization of endogenous carbs, fats, and proteins, increase CO2 and urea, decrease muscle mass and adipose tissue, increase kidney function, increase thermogenesis, and causes sweating and insensible water loss. It increases mitochondrial activity, respiratory enzymes, Na/K pump, and ramps up other proteins as well. T3 will also increase activity of cytochrome oxidases, glucose transporters, betaadrenergic receptors, Gs proteins, growth hormone, alkaline phosphatases, ADH, osteocalcin, and sexsteroid binding globulin. It will decrease T3 receptors, total and LDL cholesterol, Gi proteins, T3, myosin heavy chain, and creatine
Synthesis and secretion stimulated by TSH binding to its receptor on the thyroid follicle cells.
Inhibited by high T3/T4 levels. Very high levels of iodine will suppress T3/ T4 synthesis and secretion (WolffChaikoff effect). Lithium will inhibit iodine uptake by thyroid gland, which will result in decreased T3/ T4 synthesis and excretion.
Congenital defects in thyroid hormone synthesis (iodidetrapping enzymes, peroxidases, and deiodinases and coupling enzymes deficiencies). Hyperthyroidism (commonly due to Graves disease [stimulatory autoantibodies to TSH receptor], thyroiditis) should have low TSH levels and goiter. Can lead to thyrotoxicosis and thyroid storm. Hypothyroidism (iodine deficiency, Hashimotos [antibodies against thyroid gland that destroy the tissue]) Can have high TSH levels if primary problem and low TSH levels if secondary/
Emil Fernando
Brett Segel
PTH
Parathyroid glands
PTU) for hyperthyroidism inhibit thyroperoxidase and related steps, blocking T4/T3 production. rT3 is inactive form, T4 is prohormone, and T3 is active hormone. N/A
factors. Unbound T3/ RXR heterodimers are repressor TFs and bound T3/ RXR heterodimers are activating TFs. Acts on the kidney (activates D3), and bone.
kinase. Very important in the developing child for bone and growth development, and especially for mental development.
tertiary problem. Both hyper and hypothyroidism can yield a goiter.
Increases Ca reabsorption and decreases phosphate reabsorption (increases excretion) from kidney; increases Ca and phosphate resorption from bone; no known effect on intestine; increases bone formation when released intermittently, increases bone resorption when released continuously; promotes activation of Vit D in the kidney. Works through G-protein linked membrane receptors in kidney and bone PKA ( cAMP) and PLC ( IP3) (urinary cAMP levels are basic assays in PTH stimulation tests).
Low levels of circulating calcium.
Inhibited by high levels of Ca via GPCR Calciumsensing receptor (CaSR), inhibited by active vit. D (negative feedback) via VDR.
Some cancers (notably squamous cell lung cancer and breast cancer) secrete ectopic PTH or PTHrelated protein (PTHrP), from a gene different than PTH, that promotes bone resorption and hypercalcemia during the disease by stimulating PTH receptors and perhaps its own receptors in bone and kidney.
Emil Fernando
Brett Segel
Calcitonin
C-cells surrounding thyroid follicles (ccells derived from neural crest cells); also CNS and ENS C-Cells (differential processing of calcitonin gene, in CNS CGRP
N/A
G-Protein coupled receptors high in bone and kidney.
No known effect on intestine; weakly decreases calcium and phosphate reabsorption from kidney; decreases calcium reabsorption from bone and increases calcium mineralization in bone.
Gastrin after eating; increased plasma Ca.
Normal or low levels of serum calcium inhibit secretion of Calcitonin.
Calcitonin is not really essential for human life no known related diseaseshyper secretion is a good marker for thyroid adenomagood for short term treatment of osteoperosis in post-menapausal women, but not good for chronic treatment due to down-regulation of receptors
Emil Fernando
Brett Segel
Calcitriol (1,25 Vit. D)
Exogenous from diet or endogenous via skin production by sun (UV) light.
UV light converts cholesterol to D3 in skin. In the liver, 25hydroxylase (a Cyp450 enzyme) takes it to 25-OHD3 (highest one in plasma). In the kidney, it is converted to either 24,25 D3 (inactive storage form) or 1,25 D3 (active form) by another Cyp450 enzyme (1 -hydroxylase).
Transcalciferi 1,25 Vit. D is the active n is the form. It causes increased globulin that active transcellular binds and absorption of Ca and transports all phosphate in the intestine; Vit. D forms causes increased calcium in the plasma. and phosphate reabsorption Vitamin D in the kidney and increased receptor Ca and phosphate (VDR) resorption from bone expressed in (increases serum Ca brain, and phosphate). In GI pancreas, enterocytes, it increases pituitary, synthesis of calbindin to skin, blood more effectively pick up vessels, lung, and bind more Ca. Vit. and 20 other D is also pleiotropic and tissues. VDR can reduce cancer risk and is a nuclear increase bone density. Vit. receptor that D is also anti-proliferative heterodimerize (promotes tumor cell s with the apoptosis and maintains RXR receptor normal cell proliferation). It to become a also boosts innate immunity transcription and suppresses acquired factor (similar immune responses. to T3 receptor).
Conversion from 25-OH D3 to 1,25 D3 is due mainly to kidney stimulation by PTH. High PTH is due to low serum Ca, Vit. D deficiency, and low serum phosphate.
Inhibited by normal/ high levels of calcium and normal/ high levels of phosphate in the serum, as well as vit. D sufficiency.
Vitamin D deficiency is primary contributor to rickets in children and osteomalacia in adults. Deficiency can also cause susceptibility to certain cancers, hypertension, osteoporosis, diabetes, multiple sclerosis, viral respiratory infections, and decreased host antimicrobial activity.
Emil Fernando
Brett Segel
Somatomedin s (IGF-1 and 2)
Liver synthesizes these after stimulation from GH.
Homologous structure to proinsulin.
The somatomedins act on chondrocytes, bone, heart, lung, kidney, pancreas, intestine, skin, CT, anterior pituitary, and hypothalamus.
The somatomedins act on chondrocytes, bone, heart, lung, kidney, pancreas, intestine, skin, and CT to increase growth and development. Will also act on the anterior pituitary to inhibit GH secretion directly and on the hypothalamus to release somatostatin to inhibit GH release
Stimulated by GH acting on the liver.
N/A
Dwarfism can be caused by a defective somatomedin response/action.
Emil Fernando
Brett Segel
Cortisol
Zona fasciculata of the adrenal cortex
StAR protein transports cholesterol into mitochondria; Cyp450SCC converts it to pregnenelone (rate-limiting step); that goes to ER and becomes 11-deoxycortisol; that goes back to mitochondria and is formed into Cortisol by Cyp450C11. 11-HSD2 (kidney and other mineralocorticoid target cells) converts cortisol to cortisone. 11-HSD1 (glucocorticoid target cells) converts cortisone to cortisol.
Transported in serum bound to transcortin (CBG; 80%) and albumin (15%) with 5% free serum cortisol. It binds to intracellular receptors that form homodimers and travel to nucleus to +/- regulate transcription.
Key contra-insulin hormone ACTH binding (decreases sensitivity of to GPCR on insulin) that is essential adrenal cortex for life. Stimulates liver stimulates gluconeogenesis, fat secretion lipolysis, and protein (pulsatile catabolism (breaks down bursts), as does muscle) while inducing physiological liver gluconeogenic enzyme and pathological levels over the long term. It stressors also blocks insulins action (surgery, trauma, on substrate storage and etc.). Highest promotes liver glycogen level of serum synthesis (paradoxical cortisol is around action). It is a permissive 8 am (exhibits hormone that maximizes a circadian the actions of epinephrine rhythm). and glucagon. It also has potent anti-inflammatory and anti-immune effects (induces inhibitory proteins). It also decreases CT and bone formation, increases GFR, maintains cardiac output, and helps fetus to mature. Can act like aldosterone if there is an 11-HSD2 deficiency (works on same receptor). During pregnancy for the fetus, cortisol causes fetal lung maturation (increased pulmonary surfactant),
Pretreatment with glucocorticoid analog will inhibit ACTH and, subsequently cortisol secretion.
CAH: deficiency of 21 hydroxylase cortisol deficiency increased ACTH production steroidogenesis increased androgen production (masculinization in female and high serum ACTH). Cushings syndrome: excess cortisol production from adrenal cortex. Cushings disease: excess cortisol production from increased ACTH secretion by anterior pituitary. Addisons disease: reduced cortisol secretion from adrenocortical failure.
Emil Fernando
Brett Segel
Aldosterone
Zona glomerulosa of the adrenal cortex
Same pathway and intracellular locations as cortisol production (starts with cholesterol), but different Cyp450 enzymes will convert the to aldosterone. Has an aldehyde group that allows it to cyclize in serum as a hemiacetal.
Travels in the serum in its hemiacetal (cyclical) form with 60% bound to albumin; shorter halflife than cortisol. Forms homodimers with its nuclear receptor in target cells.
increased liver glycogen, liver gluconeogenesis, intestinal transport and digestion, and closure of the ductus arteriosus. Part of the RAA system. Acts on the distal tubule of the nephron through the Na/K ATPase to increase Na reabsorption and K excretion; this will increase serum Na (and lower serum K) in order to retain fluid and maintain total body water. Often brought into play during hemorrhage, Na deprivation, an upright posture, and congestive heart failure (latter is a pathologic role).
High ACTH levels can stimulate aldosterone secretion, but main trigger is angiotensin II binding to its receptor in the zona glomerulosa. Hyperkalemia, hyponatremia, serotonin, ACh, and VIP also stimulate.
Normal plasma osmolarity, Na, and K concentrations, as well as dopamine and ANP (aldosterone escape phenomenon) inhibit aldosterone release.
Hyperaldoster onism (Conns disease): clinically characterized by hypertension, hypokalemia, and hypernatremia; is diagnosed by high plasma/urinary aldosterone. Essential hypertension (inappropriate activation of RAA system) causes edema and swelling.
Emil Fernando
Brett Segel
Weak Androgens
Zona Same pathway reticularis of and intracellular the adrenal locations as cortex cortisol production (starts with cholesterol), but different Cyp450 enzymes will convert the products to DHEA and androstenedione.
Conversion into testosterone in fat, muscle is significant T source in females. Can also be converted to estrogen as well by liver and fat.
Conversion into strong androgens and/or estrogen is usually minimal (significant in female and in CAH). See Testosterone and Estrogen for details on these hormone actions.
ACTH can stimulate production.
N/A
Adrenogenital syndrome (synonymous with congenital adrenal hyperplasiasee above).
Emil Fernando
Brett Segel
Insulin
Pancreatic beta cells
Insulin is synthesized as a large (86 amino acids) single polypeptide chain precursor called proinsulin. Proinsulin is converted to insulin by peptidases within the secretory granules (C chain is released; C chain is what is measured to detect serum insulin levels).
Insulin binds to its receptor (a protein tyrosine kinase). Receptor autophosp horylation ensues, which activates the receptor to phosphorylate multitudes of proteins to initiate transcription factors. The insulin receptor is then internalized and degraded.
Storage of fuel substrates (liver, muscle, adipose tissue). In liver, it promotes glycogenesis, increases synthesis of triglycerides, cholesterol and VLDL, increases protein synthesis, promotes glycolysis, inhibits glycogenolysis, inhibits ketogenesis, and inhibits gluconeogenesis. In muscle, it promotes protein synthesis (increases amino acid transport, stimulates ribosomal protein synthesis) and glycogen synthesis (increases glucose transport, enhances activity of glycogen synthase, inhibits activity of glycogen phosphorylase). In adipose tissue, it promotes triacylglyceride storage (Induces lipoprotein lipase, making fatty acids available for absorption into fat cells, increases glucose transport into fat cells, thus increasing availability of a-glycerol phosphate for triglyceride synthesis, inhibits intracellular
Glucose in serum activates secretion: glucose enters through GLUT2 receptors in cells oxidized to ATP ATP shuts off ATPsensitive K channel (sulfonylurea drugs work at this step!) membrane depolarization opening of Ca channels and increased intracellular Ca release of insulincontaining vesicles. Glucogenic amino acids increase the secretion of insulin.
Epinephrine Type 2 diabetes and (insulin Norepinephrine resistance): genetic inhibit the disposition, release of excessive food insulin in the intake, inadequate immediate exercise (leading point. to obesity and Glucagon, insulin resistance), cortisol, and and compensatory GH are also hyperinsulinemia contra-insulin can lead to beta hormones. cell decomposition Fasting and (inflammatory exercise will mechanism) and also decrease diabetes (adultinsulin levels. onset, nonIncreased ketogenic, nonserum fatty insulin dependent). acids (obesity) Treat with weight leads to insulin loss and insulininsensitivity in releasing drugs. muscle. Type I diabetes (insulin dependent): Genetic disposition, beta cytotrophic viruses and chemical toxins, and islet antibodies lead to beta cell injury and diabetes. Juvenile, Brett Segel
Emil Fernando
lipolysis). Insulin will increase protein synthesis. Insulin is also important for transporting K+ into cells. Glucagon Pancreatic alpha cells The alpha cells make glucagon and the intestinal enterocytes make Glycentin and GLP-1 and GLP2 in response to a meal. Glucagon receptor is found mainly in the liver; it has 7transmembr ane domains that interact with Gs and Gq proteins to increase cAMP and Ca. Mobilization of fuel substrates (liver). It increases gluconeogenesis and glycogenolysis, increases lipolysis and subsequent beta-oxidation of fatty acids and ketone body formation. It decreases glycolysis and glycogen synthesis. It also promotes amino acid (gluconeogenic) conversion into glucose. Serum glucose, free fatty acids, (glucogenic aa: and ketone Ala, Ser, Gly, body levels Cys, Thr), CCK, will inhibit the release gastrin, cortisol, of glucagon. exercise, Insulin and infections, somatostatin other stresses, will also inhibit a-Adrenergic glucagon stimulators, secretion. and ACh will increase glucagon secretion. Amino acids
ketosis-prone, and insulin-dependent. Treat with insulin injections, diet, and exercise. Glucagonomaglucagon-secreting tumor of the pancreatic alpha cells. Very rare.
Emil Fernando
Brett Segel
Epinephrine
Chromaffin Synthesis: cells in tyrosine dopa adrenal (via tyrosine medulla hydroxylase [TH]) most DA NE (via are EPIDA Hydroxylase secreting [DBH]) (80Epi (via phenylethano 85%); CA lamine N release by exocytosis methyl-transferase [PMNT]). involves Ca Peripheral dependent cholinergic nerves fusion of synapsing on granules chromaffin cells with inner induce TH and membrane DBH levels/ and release activities, causing of granule exocytosis contents Cortisol perfusing into medulla from ECS and cortex induces bloodstr DBH and eam: EPI especially PNMT, and/or NE thus sustaining with ATP, EPI synthesis and endorphins, secretion. enkephalins Path in medulla and same as in brain dopamine-hydroxylase and symp neurons. Stops at DA in enzyme. DA neurons.
Beta receptors are greater than alpha.
Epinephrine promotes muscle glycogenolysis (providing glucose for energy metabolism and lactate for liver gluconeogenesis); also liver glycogenolysisnot as potent as glucagon but just as rapid and still important. Liver gluconeogenesisbut less potent than cortisol; potent stimulator of triglyceride lipolysis via hormonesensitive lipase in adipose tissue, providing fatty acids & glycerol for the liver. Inhibits insulin secretion, potentiating its direct effects above on carbohydrates and lipids; increases muscle K+ secretion; increases cardiac contractility and heart rate; vasodilation (decreases BP) especially of muscle arterioles; venous constriction increasing venous return; causes urinary, bronchial, and gastrointestinal muscle relaxation decreasing gastric motility and
Secretion stimulated by trauma, pain, hypovolemia, anoxia, hypotension, asphyxia, heat, cold, hypoglycemia, and exercise.
Epi is Excretion of reuptaken VMA and into cells, metanephrines: with some useful clinical re-storage in assays for several sympathetic catecholaminenerves. related Metabolized pathological by MAO and conditions. COMT with Pheochromocytom help from a (10% tumor): AidDh mainly (Lecture 82 nonmalignant slide 8) chromaffin cell 2 pathways: tumor secreting excess EPI and Epi COMT often NE that metanephrin can underlie MAO + hypertension. AldDH Other signs: Vanillylmandel ic acid (VMA) tremor, sweating, anxiety, OR pulmonary edema, Epi MAO occasionally +AldDH part of Multiple Dihydroxym Endocrine andelic acid Neoplasia (MEN COMT Vanillylmandel 2A and MEN 2B) ic acid (VMA). Primary autonomic dysfunction: severe adrenomedullary deficiency Brett Segel
Emil Fernando
Stops at NE at noradrenergic neurons.
increasing O2/CO2 exchange, increases liver ketogenesis, and increases glucagon secretion.
or defect in neural reflex arc secondary to disease; causes orthostatic hypotension, impaired sweating, bladder problems. Trauma, pain, hypovolemia, anoxia, hypotension, asphyxia, heat, cold, hypoglycemia, exercise, cytokine release in response to injury, CRH (Cortisol and NE work synergistically). Metabolism by MAO and COMT w/ help from AidDh 2 pathways: NE COMT normetaneph rin MAO + AldDH Vanillylmandel ic acid (VMA) OR NE MAO +AldDH Dihydroxym andelic acid COMT Vanillylmandel ic acid (VMA). Same pathologies as for epinephrine.
Norepinephri ne
Adrenal medulla (chromaffin cells: 1520%), but mostly from noradrenerg ic brain and peripheral postganglionic sympathetic neurons.
Refer to epinephrine pathway and just stop at NE.
Alpha receptors are greater than beta.
Increases gluconeogenesis and glycogenolysis; decreases insulin secretion; increases cardiac contractility; causes vascoconstriction of splanchnic, renal, genital, and skin vasculature; GI and urinary sphincter constriction; increases sweating, dilation of pupils, and platelet aggregation; works synergistically with T4 to produce heat in BAT (brown adipose tissue) via Gs protein cAMP Mitochondrial ETC uncoupling.
Emil Fernando
Brett Segel
Testosterone (also dihydrotestos terone DHT, potent form).
Primarily in Cholesterol the Leydig converted to cells of pregnenolone the testes within the upon LH mitochondria, stimulation, then taken to but also in testosterone. 5 brain, skin, alpha reductase and adipose converts T to DHT tissue (more potent), (conversion and aromatase from weak converts T to androgens). estradiol. Also from Theca cells of the ovary.
Acts on Intracellular T binds to hypothalamus androgen receptor (or made to inhibit to DHT and binds receptor); GnRH it is a nuclear receptor that secretion becomes a TF. and anterior Essential for sperm pituitary maturation; held near to inhibit semimiferous tubules by LH (main ABP (androgen binding regulator of protein) that is made by LH!) 45% Sertoli cells. Stimulates is bound to Sertoli cells (along with SHBG (sex FSH) to make ABP, p450hormone aromatase and inhibin. binding DHT will negatively globulin), feedback inhibit GnRH 55% bound to from hypothalamus and albumin and pituitary gonadotrophs. corticosteroid- Testosterone is essential for binding development of the male globulin (causes development of (CBG), and Wolffian ducts), bone 2% is free growth, adipose growth, biologically RBC growth, increased active and muscle mass, increased may diffuse VLDLs and LDLs into cells. (decreased HDL), and development of larynx. DHT causes beard and prostrate growth, sebum formation, pubertal development, intrauterine differentiation of male sex
Stimulated by LH acting on the Leydig cells. Also positive feedback from Sertoli cells (they make inhibin, which causes testosterone secretion, which causes Sertoli cells to make more inhibin)
Secretion inhibited by activin and estradiol release from the Sertoli cells. Secretion indirectly inhibited by prolactin (prolactin suppresses gonadotropin secretion)
Hypergondadotrop ic Hypogonadism (lots of LH/FSH with low T/DHT; primary problem) Hypogonadotroph ic Hypogonadism (low LH/FSH with low T/DHT; secondary/tertiary problem) Androgen resistance/ insensitivity causes male pseudohermaphroditism. Androgens are involved in prostatic cancer and benign prostratic hypertrophy (too much DHT, so give 5alpha reductase inhibitors [finestride] for prostatic hyperplasia).
Emil Fernando
Brett Segel
organs, and sperm production.
Emil Fernando
Brett Segel
Estrogen (really Estradiol E2)
Theca cells Dominant estrogen Estradiol in During the follicular phase, of the ovary, is Estradiol (E2), serum via estrogen negativelyplacenta with Estrone (E1) SHBG [sex feedback inhibits GnRH and corpus and Estriol (E3, hormone from hypothalamus and LH/ luteum dominant estrogen binding FSH from anterior in pregnancy and globulin]. pituitary; it also increases marker for fetal Estradiol also follicular development health) much increases while decreasing sensitivity weaker SHBG. of FSH-secreting cells. Cholesterol is This can be Estradiol levels continue to precursor from useful for rise until they reach diet or acetate ameliorating threshold in the ovulatory Rate limiting step: androgen phase; then it switches to cholesterol excess. positive feedback on pregnenolone Progesterone hypothalamic GnRH and Importance via CBG pituitary to cause a huge of Aromatase [corticosteroid surge of LH and ovulation. reaction binding Rupture of follicle (testosterone globulin] decrease in E2 decrease to estradiol; in + feedback decrease increased in LH. Follicle then aromatase activity becomes corpus luteum in in the dominant the luteal phase and makes follicle.) more E2 with progesterone; Liver conversion switch back to negative of both estradiol feedback of E2 on LH. and estrone to Loss of LH causes estriol. degradation of corpus Major progestins luteum unless rescued by progesterone pregnancy. Estradiol also and 17ainhibits the growth of hydroxyprogestero cohort follicles, alters ne cervical mucus to enhance
Synthesis and secretion by the ovaries is stimulated by LH and FSH.
Degradation of the corpus luteum results in vastly decreased synthesis and excretion of estrogen.
Low estrogen levels (as with 17a-hydroxylase deficiency) primordial follicles do not develop into primary follicles. Postmenopausal hormone therapy is currently recommended short-term for the management of moderate-tosevere vasomotor flushes. Long-term use for prevention of disease is no longer recommended (increased risk of osteoporosis, breast and colon cancer).
The RATIO of estrogen to progesterone is important in pregnancy. Estrogen >> progesterone plays an essential role in parturition.
Emil Fernando
Brett Segel
sperm transport, causes fallopian tube to favor transport of ovum and zygote, and prepares uterine lining for progesterone to evoke secretory response (proliferative phase of endometrium). During pregnancy, it stimulates mammogenesis (promotes growth of ductal system of breast), causes continuous growth of myometrium, preparing for its role in labor, softens pelvic ligaments and symphysis pubis (in concert with Relaxin), and causes enlargement of external genitalia. In late gestation it is involved in parturition.
Emil Fernando
Brett Segel
Progesterone
Corpus Luteum
Cholesterol Pregnenolone Progesterone either estradiol, testosterone, cortisol, Androstenedione, DHEA, aldosteroneetc.
All over main focus = hypothalamus and endometrium.
Inhibits pulse generator at hypothalamus, decreasing FSH and LH production. Converts endometrium to prepare uterus for implantation (secretory phase). If no pregnancy, progesterone levels will decrease, leading to menstruation. During pregnancy, it is directly responsible for establishment and sustenance of the fetus, inhibits uterine contractions, inhibits prostaglandin production (keeps uterus in quiescent state), decreases sensitivity to oxytocin (decreases OT receptors), upregulates b-adrenergic receptors that promote myometrial relaxation, inhibits maternal immune response to antigenic fetus, suppresses T-cell activation and macrophage function, reduces number of leukocytes, and causes 50% increase in maternal blood volume in 2nd trimester.
Stimulated by FSH. The RATIO of estrogen to progesterone is important in pregnancy. Progesterone >> estrogen maintains uterine quiescence and sustenance of the fetus.
N/A
N/A
Emil Fernando
Brett Segel
Activin
Sertoli cells of the testes and granulosa cells of the ovaries Sertoli cells of the testes and granulosa cells of the ovaries.
Always composed of 2 beta subunits (Beta A and B, 2 beta As, or 2 beta Bs).
Inhibin
Always has an Alpha. AlphabetaA (Inhibin A, corpus luteum) or alpha-betaB (Inhibin B, dominant follicle). N/A
Follistatin
Released by testes and ovaries.
Acts on the anterior pituitary gland gonadotrophs and Leydig cells of the testes. Acts on anterior pituitary gonadotrophs, Leydig cells of the testes, and the hypothalamus. Blocks activin.
Promotes mammogenesis stimulates alveolar pouches of mammary glands increase in their capacity to secrete milk. Ant. Pit. To increase FSH synth and secretion, inhibits testosterone from Leydig cells
Stimulated by FSH action on testes.
Inhibited by follistatin
N/A
Inhibits FSH secretion, enhances testosterone secretion from Leydig cells. May cause hypothalamus to increase secretion of GnRH. Inhibin B augments androgen production by the Theca cells. Inhibits activin, resulting in inhibition of FSH secretion from anterior pituitary (synergistic function with inhibin).
Stimulated by FSH action on testes.
N/A
N/A
Stimulated by FSH.
N/A
N/A
Emil Fernando
Brett Segel
Relaxin
Produced by both corpus luteum, placenta, and decidua.
N/A
Uterus
Inhibits myometrial contractions (ensure uterine quiescence in early pregnancy). Relaxes pelvic bones and ligaments and softens cervix (may play a role in parturition).
Secreted in response to hCG
N/A
N/A
Emil Fernando
Brett Segel
S-ar putea să vă placă și
- ENDOCRINE PATHOLOGY WebpathDocument35 paginiENDOCRINE PATHOLOGY Webpathapi-3766657Încă nu există evaluări
- Endocrine Gland Hormone(s) Secreted Stimulus Effect of Hormone Inhibition PathologyDocument3 paginiEndocrine Gland Hormone(s) Secreted Stimulus Effect of Hormone Inhibition PathologySamuelÎncă nu există evaluări
- Breast CancerDocument6 paginiBreast Cancersarguss14Încă nu există evaluări
- AtelectasisDocument3 paginiAtelectasisLouis FortunatoÎncă nu există evaluări
- Haematology-Summary My NotesDocument24 paginiHaematology-Summary My NotesToria053Încă nu există evaluări
- Adrenergic PharmacologyDocument6 paginiAdrenergic Pharmacologyjess6001Încă nu există evaluări
- USMLE Step 1 DrugsDocument36 paginiUSMLE Step 1 DrugscougardiverÎncă nu există evaluări
- Reproductive Physiology and Sexual DifferentiationDocument11 paginiReproductive Physiology and Sexual DifferentiationAbeebs SalahouÎncă nu există evaluări
- Cell Adaptation and Necrosis: Hypertrophy, Atrophy, MetaplasiaDocument8 paginiCell Adaptation and Necrosis: Hypertrophy, Atrophy, MetaplasiaivankcurryÎncă nu există evaluări
- Diseases - BiochemDocument4 paginiDiseases - BiochemJay FeldmanÎncă nu există evaluări
- Respi PhysioDocument7 paginiRespi PhysioAmal JohnsonÎncă nu există evaluări
- Cardiology Arteritis ChartDocument3 paginiCardiology Arteritis ChartM PatelÎncă nu există evaluări
- Genetic Disorders-Www - Qworld.co - inDocument13 paginiGenetic Disorders-Www - Qworld.co - inQworld100% (1)
- Clinical Medicine - Lecture: - Topic: - DateDocument3 paginiClinical Medicine - Lecture: - Topic: - DateqselmmÎncă nu există evaluări
- 7sgdfgf PDFDocument438 pagini7sgdfgf PDFPratik JadhavÎncă nu există evaluări
- Approximate Equivalents:: 0.100 Gmn. 1.00 GMDocument8 paginiApproximate Equivalents:: 0.100 Gmn. 1.00 GMakane ryuÎncă nu există evaluări
- UW (Step 1) Biochemistry - Educational ObjectivesDocument41 paginiUW (Step 1) Biochemistry - Educational ObjectivesUsama BilalÎncă nu există evaluări
- Concise SEO-Optimized Title for Clotting DocumentDocument3 paginiConcise SEO-Optimized Title for Clotting DocumentRyan TurnerÎncă nu există evaluări
- Pancreatic Hormones and Antidiabetic AgentsDocument3 paginiPancreatic Hormones and Antidiabetic AgentsChristian DeeÎncă nu există evaluări
- Heart Failure - Notes From "Cardiology" (Timmis Et Al) : Main CausesDocument3 paginiHeart Failure - Notes From "Cardiology" (Timmis Et Al) : Main CausesPrarthana Thiagarajan100% (3)
- Inflammatory Response and Vascular Permeability ChangesDocument20 paginiInflammatory Response and Vascular Permeability Changesjeffaguilar100% (2)
- General Pathology 4.03 Endocrine System Super SummaryDocument15 paginiGeneral Pathology 4.03 Endocrine System Super SummaryJade MonrealÎncă nu există evaluări
- Physio B 1.2 Renal Physiology Pt. 4 (Dr. Vila) : Because of Increase Water ReabsorptionDocument5 paginiPhysio B 1.2 Renal Physiology Pt. 4 (Dr. Vila) : Because of Increase Water ReabsorptionAnny AlvrzÎncă nu există evaluări
- Pharmacology of EthanolDocument5 paginiPharmacology of EthanolJoshua RemonÎncă nu există evaluări
- Anti FungalsDocument5 paginiAnti FungalskakuÎncă nu există evaluări
- Hematology & Oncology. Anatomy 56Document60 paginiHematology & Oncology. Anatomy 56Heran TeferiÎncă nu există evaluări
- Table of 12 Cranials and TractusDocument5 paginiTable of 12 Cranials and TractusjuwitavalenÎncă nu există evaluări
- Table of Genetic Disorders: Download A Copy of This Study GuideDocument11 paginiTable of Genetic Disorders: Download A Copy of This Study Guideerica perezÎncă nu există evaluări
- 2 Renal Buzzword ChartDocument6 pagini2 Renal Buzzword ChartTyler KingÎncă nu există evaluări
- Dr. A. Samy TAG Bone Diseases - 1Document2 paginiDr. A. Samy TAG Bone Diseases - 1Herato MenaÎncă nu există evaluări
- Kidney NewDocument4 paginiKidney NewParth BhayanaÎncă nu există evaluări
- Cellular Injury, Adaptation and Cell DeathDocument8 paginiCellular Injury, Adaptation and Cell DeathJessica Febrina Wuisan100% (1)
- Anat 6.3 GSA Appendix - EsguerraDocument4 paginiAnat 6.3 GSA Appendix - Esguerralovelots1234Încă nu există evaluări
- Pharmacology: Teratogenic CarcinogenicDocument13 paginiPharmacology: Teratogenic CarcinogenicSherlock HolmesÎncă nu există evaluări
- Liver Function Tests Diagnostic GuideDocument2 paginiLiver Function Tests Diagnostic GuideostarburstoÎncă nu există evaluări
- 4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangDocument4 pagini4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangMiel Raphael AranillaÎncă nu există evaluări
- Respi - PathDocument19 paginiRespi - PathKimberly KanemitsuÎncă nu există evaluări
- Renal SystemDocument76 paginiRenal SystemDaNy ChiriacÎncă nu există evaluări
- By DR - Mohammad Z. Abu Sheikha@: +pigmented Stones (Black Stone - Non Infected) (Brown Stone - Infected)Document11 paginiBy DR - Mohammad Z. Abu Sheikha@: +pigmented Stones (Black Stone - Non Infected) (Brown Stone - Infected)Nisreen Al-shareÎncă nu există evaluări
- DNA Viruses: P P P A H H PDocument2 paginiDNA Viruses: P P P A H H PKimberly KanemitsuÎncă nu există evaluări
- Cardiac Murmurs and Maneuvers GuideDocument1 paginăCardiac Murmurs and Maneuvers GuidePkernÎncă nu există evaluări
- Pediatric Hematooncology Alarm SymptomsDocument22 paginiPediatric Hematooncology Alarm SymptomsMuhammad ArifÎncă nu există evaluări
- Clinical correlations by Dr. Irfan MirDocument55 paginiClinical correlations by Dr. Irfan MirsammieahemdÎncă nu există evaluări
- Spinal Cord LesionsDocument1 paginăSpinal Cord Lesionsnpatelmd14Încă nu există evaluări
- RBC Disorder BcqsDocument68 paginiRBC Disorder BcqsMukhtiar AhmedÎncă nu există evaluări
- OPTOMED-HW2-Diabetic Retinopathy PDFDocument3 paginiOPTOMED-HW2-Diabetic Retinopathy PDFDanalie SalvadorÎncă nu există evaluări
- Clinical SignsDocument26 paginiClinical SignswiraandiniÎncă nu există evaluări
- Chart - WBC DisordersDocument1 paginăChart - WBC DisordersSamuel RothschildÎncă nu există evaluări
- Blueprints - Radiology PDFDocument134 paginiBlueprints - Radiology PDFBenny KMÎncă nu există evaluări
- Causes, Types and Morphology of Cell Injury and DeathDocument18 paginiCauses, Types and Morphology of Cell Injury and DeathYoja GarzonÎncă nu există evaluări
- Epilepsy: Causes of Seizures (Non-Epileptic)Document5 paginiEpilepsy: Causes of Seizures (Non-Epileptic)humdingerÎncă nu există evaluări
- Pathology B - Gastrointestinal Tract (Esguerra, 2015)Document18 paginiPathology B - Gastrointestinal Tract (Esguerra, 2015)Ars MoriendiÎncă nu există evaluări
- NEUROLOGY Goljan FootnotesDocument10 paginiNEUROLOGY Goljan FootnotesPrince DuÎncă nu există evaluări
- General pathology reviewDocument93 paginiGeneral pathology reviewPrarthanaÎncă nu există evaluări
- Casts inDocument1 paginăCasts ingregoryvoÎncă nu există evaluări
- Epithelial TissueDocument7 paginiEpithelial TissueJoan PaulineÎncă nu există evaluări
- Disorders of Cho MetabolismDocument4 paginiDisorders of Cho MetabolismJohn Christopher LucesÎncă nu există evaluări
- Chapter 3 Genetic VariationDocument21 paginiChapter 3 Genetic VariationAbdulkarimÎncă nu există evaluări
- Problem-based Approach to Gastroenterology and HepatologyDe la EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisÎncă nu există evaluări
- Anterior Pituitary HormonesDocument46 paginiAnterior Pituitary Hormonespramod bhaleraoÎncă nu există evaluări
- Infertility ACOGDocument8 paginiInfertility ACOGRifdaÎncă nu există evaluări
- Hormones in Human Reproduction: Group 1Document36 paginiHormones in Human Reproduction: Group 1Accel YcoÎncă nu există evaluări
- Draft Ventilation Control For White Leg Horn PoultryDocument6 paginiDraft Ventilation Control For White Leg Horn PoultryHope Ladyline EspanolaÎncă nu există evaluări
- StetDocument34 paginiStetCameron FoxÎncă nu există evaluări
- 06 - 213the Pathophysiology and Treatment of Polycystic Ovarian Syndrome-A Systematic ReviewDocument4 pagini06 - 213the Pathophysiology and Treatment of Polycystic Ovarian Syndrome-A Systematic ReviewAnni SholihahÎncă nu există evaluări
- Chemical Coordination and Integration Chemical Coordination and IntegrationDocument7 paginiChemical Coordination and Integration Chemical Coordination and IntegrationAkash AbbarapuÎncă nu există evaluări
- Evaluation and Management of Primary Amenorrhea - UpToDateDocument15 paginiEvaluation and Management of Primary Amenorrhea - UpToDateGaby GarridoÎncă nu există evaluări
- Company Introduction Marketing Plan OfHCG & HMGDocument29 paginiCompany Introduction Marketing Plan OfHCG & HMGwk babar100% (2)
- A Case Study About Cervical PolypsDocument8 paginiA Case Study About Cervical PolypsJisel-Apple BulanÎncă nu există evaluări
- Menstrual Cycle Lecture MidwiferyDocument45 paginiMenstrual Cycle Lecture MidwiferyAldrinÎncă nu există evaluări
- Pure GonDocument24 paginiPure Gonulfa primadhaniÎncă nu există evaluări
- Maternal and Child Nursing Care 3rd Edition London Test BankDocument11 paginiMaternal and Child Nursing Care 3rd Edition London Test BankSerenaÎncă nu există evaluări
- Previous IB Exam QuestionsDocument12 paginiPrevious IB Exam QuestionsJohn OsborneÎncă nu există evaluări
- Male and Female Reproductive Parts and Functions and Hormones On ReproductionDocument99 paginiMale and Female Reproductive Parts and Functions and Hormones On ReproductionThird WillowÎncă nu există evaluări
- Mercury Contamination in Water & Its Impact On Public HealthDocument8 paginiMercury Contamination in Water & Its Impact On Public HealthHerman KarimÎncă nu există evaluări
- The Ncuk International Foundation Year IFYBI002 Biology 2017-18 Mark SchemeDocument16 paginiThe Ncuk International Foundation Year IFYBI002 Biology 2017-18 Mark SchemeFran cÎncă nu există evaluări
- Short Note Biology Form 5-Chapter 4 Reproduction and GrowthDocument7 paginiShort Note Biology Form 5-Chapter 4 Reproduction and Growthsalamah_sabri50% (2)
- Gynecology and Obstetrics Abbreviations GuideDocument1 paginăGynecology and Obstetrics Abbreviations Guidejcachica21Încă nu există evaluări
- Precocious PubertyDocument30 paginiPrecocious PubertyAjoritsedere Eric AkonuÎncă nu există evaluări
- GynecologyDocument50 paginiGynecologyPhilips55100% (4)
- Hormones in Reproduction: Presented To: Dr. Akhtar Rasool Presented By: M Tayyab 2012-VA-300Document17 paginiHormones in Reproduction: Presented To: Dr. Akhtar Rasool Presented By: M Tayyab 2012-VA-300javeria choudharyÎncă nu există evaluări
- Adult-2, Unit 1, Metabolic and EndocrineDocument157 paginiAdult-2, Unit 1, Metabolic and EndocrineBav VAansoqnuaetzÎncă nu există evaluări
- Evidence Based Fertility Investigations Final 2018 2Document43 paginiEvidence Based Fertility Investigations Final 2018 2Sagie NaiduÎncă nu există evaluări
- Armando Menstrual CycleDocument2 paginiArmando Menstrual CycleMatthew PinedaÎncă nu există evaluări
- 0610 s18 Ms 42 PDFDocument11 pagini0610 s18 Ms 42 PDFTheNether ManiacÎncă nu există evaluări
- Sexuality in AyurvedaDocument9 paginiSexuality in AyurvedaRamanasarmaÎncă nu există evaluări
- Human reproduction overviewDocument30 paginiHuman reproduction overviewfirstclassÎncă nu există evaluări
- Lecture Notes AnatomyDocument18 paginiLecture Notes AnatomyFau Fau DheoboÎncă nu există evaluări
- Activity 7Document2 paginiActivity 7kristine dagohoyÎncă nu există evaluări