Documente Academic
Documente Profesional
Documente Cultură
Two Stage Vs One Stage Controversy
Încărcat de
Walaa EL GamalDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Two Stage Vs One Stage Controversy
Încărcat de
Walaa EL GamalDrepturi de autor:
Formate disponibile
Two Stage vs. One Stage Is There Really A Controversy?
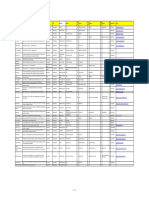
By David A. Garber, DMD, Henry Salama, DMD, and Maurice A. Salama, DMD Introduction The long held injunction setting the two-stage implant approach as the standard surgical modality is derived from the original Branemark protocol developed in the 1960s and 1970s. This protocol was designed as a solution for the totally edentulous patient to support a removable or hybrid type replacement prosthesis. The initial working premise for the two stage approach was that the successful development of osseointegration at the bone implant site during the healing phase. Animal and clinical research conducted over the last ten years, however, have convincingly proven that a one stage protocol can deliver an equal level of predictability to the achievement of osseointegration. Indeed, the present state of knowledge has rendered as moot, any discussions comparing the two or one stage approaches solely based on their ability to achieve oseointegration. Instead, relevant comparisons of the two approaches now focus on their ability to promote clearly defined clinical endpoints such as patient management, esthetics and peri-implant tissue health. Towards that end, therapeutic decision making must emphasize the matching of surgical protocols with the appropriate implant design based on the specific parameters inherent at the receptor site (Table 1). We have identified specific clinical parameters that directly affect the choices made. These parameters are categorized as follows: I. Implant placement is the mature site. Esthetic anterior vs. posterior implant placement A) In posterior or edentulous implant placement a one stage surgical protocol and a one stage implant design, i.e. with a polished collar of 1.5-3mm offers distinct advantages. These advantages include easier and more efficient patient management because there is only one surgical intervention. In addition, optimal management of the peri-implant biological width is enhanced by moving the implant/restorative microgap above the osseous crest. B) In anterior esthetic applications, however, the soft tissue demands create significant challenges that alter decision making. Even proponents of one stage implant systems have proposed altering their surgical protocols in the anterior region to include a two stage protocol of deeper than usual fixture placement which negates the advantages listed earlier for the placement in the posterior region. It is, therefore, clear that soft tissue and esthetic demands will effect the choice of a one or two stage implant protocol as well as a one or two stage implant design.
II. Immediate extraction protocol two or one stage Esthetic concerns determine that a tooth destined for extraction should be evaluated prior to tooth removal to comprehensively evaluate the potential implant receptor site. If it is within the esthetic zone, the necessity of the underlying osseous topography being present to support the soft tissue profiles of the restorative recipient site is essential. Esthetic soft tissue predictability necessitates the presence of interdental osseous peaks of bone within 5mm of the contact point of the potential final restoration. If deficient, soft tissue profiles and the underlying osseous housing may be augmented prior to extraction utilizing orthodontic manipulation of the tooth in an incisal direction. Following an atraumatic extraction, (without raising a flap/incisionless) the residual socket is now evaluated to ascertain if it is intact or if there is compromise in the labial or lingual osseous plate which may take the form of either a dehiscence or a fenestration. The advent of wide platform fixtures dramatically altered the immediate implant technique. The matching diameter of the implant body and that of the socket eliminated the need for a membrane over the top of the socket to allow for G.B.R. in the gap between the fixture and the socket in the coronal portion. If these wide bodied fixtures were directed somewhat lingual to the original socket, they could often be placed in the native bone with primary stability while obliterating the access to the socket thereby not requiring a membrane and G.B.R. (This eliminated the need for a definitive two stage procedure and a healing abutment could then be used in the conventional one stage approach.) If the site is intact, the sequential drilling ostectomies are preformed and the site once again evaluated for perforation of the bony housing. If none exists, the implant may be placed in a one stage nonsubmerged approach. (Fig. A and B 135, 139) Perforation of the socket during the sequential drilling ostectomies for cylindrical traditional implants can often be eliminated by using a fixture design that decreases in diameter towards the apical region to accommodate the labial concavity in the premaxilla no osseous compromise facilitates a one stage approach and expedites the process. However, if either following extraction or the drilling ostectomies the integrity of osseous housing has been compromised a flap may now need to be raised. In our opinion, if the osseous compromise is a dehiscence the two stage approach becomes necessary. In these cases, the bone is invariably lost on the labial surface and following implant placement, primary stability is evident but threads may be exposed thru the osseous housing. In these cases membrane guided bone regeneration may be utilized in conjunction with some form of grafting material to maintain space below the membrane. A two stage implant design is generally easier to use in these cases as the reduced profile facilitates complete flap closure. The tissue must now be advanced coronally
S-ar putea să vă placă și
- Tissue ManagementDocument16 paginiTissue ManagementSaleh AlsadiÎncă nu există evaluări
- 2005 Rojas VizcayaDocument14 pagini2005 Rojas Vizcayacasto.carpetasmiaÎncă nu există evaluări
- Treatment of The Severely Atrophic Fully Edentulous Maxilla: The Zygoma Implant OptionDocument16 paginiTreatment of The Severely Atrophic Fully Edentulous Maxilla: The Zygoma Implant Optioncmfvaldesr7Încă nu există evaluări
- Site Preservation Decision TreeDocument8 paginiSite Preservation Decision TreeHaoWangÎncă nu există evaluări
- Tissue Preservation and Maintenance of Optimum Esthetics: A Clinical ReportDocument7 paginiTissue Preservation and Maintenance of Optimum Esthetics: A Clinical ReportBagis Emre GulÎncă nu există evaluări
- Decision Making With Zygomatic and Pterygoid Dental Implants - 2022 - DentistrDocument5 paginiDecision Making With Zygomatic and Pterygoid Dental Implants - 2022 - DentistrHien TruongÎncă nu există evaluări
- Implant-Retained Cantilever Fixed Prosthesis: Where and WhenDocument4 paginiImplant-Retained Cantilever Fixed Prosthesis: Where and WhenSitiKhadijahÎncă nu există evaluări
- Zitz Mann 1999Document9 paginiZitz Mann 1999Camilo SestoÎncă nu există evaluări
- Immedite Placement Makkahnew PDFDocument30 paginiImmedite Placement Makkahnew PDFaymanÎncă nu există evaluări
- Screw-Versus Cement-Retained Implant RestorationsDocument8 paginiScrew-Versus Cement-Retained Implant RestorationsMia V. UckrmnnÎncă nu există evaluări
- All On 4Document50 paginiAll On 4Juan Jose Stuven RodriguezÎncă nu există evaluări
- Esthetics and Implant DentistryDocument18 paginiEsthetics and Implant DentistryVikas Aggarwal0% (1)
- 10-Grafting Alveolar DefectDocument10 pagini10-Grafting Alveolar DefectAhmed BastawissiÎncă nu există evaluări
- Immediateimplantplacementbeckeretalperio2k2008 PDFDocument11 paginiImmediateimplantplacementbeckeretalperio2k2008 PDFNiaz AhammedÎncă nu există evaluări
- Restoration of Edentulous Mandibles With Fixed ProsthesesDocument41 paginiRestoration of Edentulous Mandibles With Fixed ProsthesesCostina BolboriciÎncă nu există evaluări
- 1 s2.0 S0011853220300823 MainDocument11 pagini1 s2.0 S0011853220300823 Mainctbmfhcpf3Încă nu există evaluări
- Maintenance of Gingival Form Following Implant PlacementDocument4 paginiMaintenance of Gingival Form Following Implant PlacementRomina BitaÎncă nu există evaluări
- Clin Implant Dent Rel Res - 2021 - Alexopoulou - Immediate Implant in The Posterior Region Combined With Alveolar RidgeDocument12 paginiClin Implant Dent Rel Res - 2021 - Alexopoulou - Immediate Implant in The Posterior Region Combined With Alveolar Ridgecr.bustamantes3481Încă nu există evaluări
- Bedrossian Treatment Planning The Maxilla PDFDocument11 paginiBedrossian Treatment Planning The Maxilla PDFSitiKhadijahÎncă nu există evaluări
- The Single-Tooth Dental Implant: Practical Guidelines For Hard Tissue AugmentationDocument16 paginiThe Single-Tooth Dental Implant: Practical Guidelines For Hard Tissue Augmentation歐亦焜100% (1)
- The Palatal Advanced Flap: A Pedicle Flap For Primary Coverage of Immediately Placed ImplantsDocument7 paginiThe Palatal Advanced Flap: A Pedicle Flap For Primary Coverage of Immediately Placed ImplantsMárcia ChatelieÎncă nu există evaluări
- 6 IntroductionDocument6 pagini6 IntroductionDrsaumyaÎncă nu există evaluări
- Cap 10087Document13 paginiCap 10087snkidÎncă nu există evaluări
- Ridge Preservation Techniques For Implant Therapy: JO M I 2009 24 :260-271Document12 paginiRidge Preservation Techniques For Implant Therapy: JO M I 2009 24 :260-271Viorel FaneaÎncă nu există evaluări
- Dental ImplantsDocument9 paginiDental ImplantsPati Villalobos AntibiloÎncă nu există evaluări
- Inward-Inclined Implant Platform For The Amplified Platform-Switching Concept: 18-Month Follow-Up Report of A Prospective Randomized Matched-Pair Controlled TrialDocument9 paginiInward-Inclined Implant Platform For The Amplified Platform-Switching Concept: 18-Month Follow-Up Report of A Prospective Randomized Matched-Pair Controlled TrialdivyaÎncă nu există evaluări
- Use of Implants in The Pterygoid RegionDocument4 paginiUse of Implants in The Pterygoid RegionManjulika TysgiÎncă nu există evaluări
- Use of Implants in The Pterygoid Region For Prosthodontic TreatmentDocument4 paginiUse of Implants in The Pterygoid Region For Prosthodontic TreatmentSidhartha KumarÎncă nu există evaluări
- Grizas 2018Document16 paginiGrizas 2018Dome CárdenasÎncă nu există evaluări
- Prosthetic SurgeryDocument14 paginiProsthetic SurgeryCristina CArrera100% (1)
- Marginal Bone Loss and Immediate DentureDocument14 paginiMarginal Bone Loss and Immediate DentureSupriya ShuklaÎncă nu există evaluări
- Immediate Implant Placement PDFDocument11 paginiImmediate Implant Placement PDFFerdinan PasaribuÎncă nu există evaluări
- Anterior Implant EstheticsDocument9 paginiAnterior Implant EstheticsRatih Cynthia100% (1)
- Os SEO IntegrationDocument7 paginiOs SEO IntegrationAkshay GajakoshÎncă nu există evaluări
- Implant Placement in Ridge SplitDocument10 paginiImplant Placement in Ridge SplitQuang Bui100% (1)
- Bone and Tissue LevelDocument3 paginiBone and Tissue LevelSaleh AlsadiÎncă nu există evaluări
- Aumento de Reborde Con Tejido BlandoDocument8 paginiAumento de Reborde Con Tejido BlandoSilvia SolisÎncă nu există evaluări
- Screw Retained Vs Cement Retained Implant-Supported Fixed Dental ProsthesisDocument11 paginiScrew Retained Vs Cement Retained Implant-Supported Fixed Dental ProsthesisMario Troncoso AndersennÎncă nu există evaluări
- Implant ResearchDocument8 paginiImplant ResearchFBI LUC1FeRÎncă nu există evaluări
- A Classification System of DefectsDocument12 paginiA Classification System of DefectsPrana SkyaÎncă nu există evaluări
- AJDSM Volume 22 Issue 3 Pages 247-251Document5 paginiAJDSM Volume 22 Issue 3 Pages 247-251MarisbebelaÎncă nu există evaluări
- Abutment Options For The Restoration of The Malalinged Implant 2016 PDFDocument5 paginiAbutment Options For The Restoration of The Malalinged Implant 2016 PDFmarwa100% (1)
- GholamiDocument4 paginiGholamiLalaÎncă nu există evaluări
- Articol Pentru Teme 14-18Document9 paginiArticol Pentru Teme 14-18Diamanta Yalomit CirsteaÎncă nu există evaluări
- Prosthodontic Perspective To All-On-4 Concept For Dental ImplantsDocument4 paginiProsthodontic Perspective To All-On-4 Concept For Dental Implantsprostho booksÎncă nu există evaluări
- A Review of The Surgical Protocol For Reconstruction of Alveolar Ridge DeficiencyDocument21 paginiA Review of The Surgical Protocol For Reconstruction of Alveolar Ridge DeficiencyAymen Elatrash100% (1)
- АльвеолопластикаDocument12 paginiАльвеолопластикаIrinaBorodulinaÎncă nu există evaluări
- Restoration of Edentulous Maxillae With OverdenturesDocument29 paginiRestoration of Edentulous Maxillae With OverdenturesCostina BolboriciÎncă nu există evaluări
- I S M B M o L A: CDocument7 paginiI S M B M o L A: CAshraf KamalÎncă nu există evaluări
- Orthognathic Surgery Seminars 2017Document4 paginiOrthognathic Surgery Seminars 2017Tony SantosÎncă nu există evaluări
- Australian Dental Journal - 2018 - RuljancichDocument8 paginiAustralian Dental Journal - 2018 - RuljancichISAI FLORES PÉREZÎncă nu există evaluări
- Aumento de Reborde 1Document4 paginiAumento de Reborde 1valeriaÎncă nu există evaluări
- Selection of Attachment PresentationDocument44 paginiSelection of Attachment PresentationIbrahim Ahmed Dahab100% (1)
- Allon4 ProtesisDocument5 paginiAllon4 Protesis6mp57dy74sÎncă nu există evaluări
- Screw Retained Vs Cement Retained Implant-Supported FDP, Closed-Tray Vs Open-Tray Dental Implant ImpressionDocument5 paginiScrew Retained Vs Cement Retained Implant-Supported FDP, Closed-Tray Vs Open-Tray Dental Implant ImpressionMazen T. ShembeshÎncă nu există evaluări
- BDJ Volume 201 Issue 6 2006 (Doi 10.1038/sj - bdj.4814041) Chee, W Jivraj, S - Treatment Planning of The Edentulous MandibleDocument9 paginiBDJ Volume 201 Issue 6 2006 (Doi 10.1038/sj - bdj.4814041) Chee, W Jivraj, S - Treatment Planning of The Edentulous MandibleahmadÎncă nu există evaluări
- Short ImplantsDe la EverandShort ImplantsBoyd J. TomasettiÎncă nu există evaluări
- Treatment Planning Single Maxillary Anterior Implants for DentistsDe la EverandTreatment Planning Single Maxillary Anterior Implants for DentistsÎncă nu există evaluări
- Zygomatic Implants: Optimization and InnovationDe la EverandZygomatic Implants: Optimization and InnovationJames ChowÎncă nu există evaluări
- Dental Implants and Dentures: Open Access: Computer Guided Implantology: For Optimal Implant PlanningDocument4 paginiDental Implants and Dentures: Open Access: Computer Guided Implantology: For Optimal Implant PlanningFiru LgsÎncă nu există evaluări
- Seminar 6 Preventive Prosthodontics in CD WordDocument29 paginiSeminar 6 Preventive Prosthodontics in CD Wordketaki kunteÎncă nu există evaluări
- Zygomatic Implants PDFDocument18 paginiZygomatic Implants PDFgirl33Încă nu există evaluări
- J Esthet Restor Dent - 2018 - Tezulas - Clinical Procedures Designs and Survival Rates of All Ceramic Resin Bonded FixedDocument12 paginiJ Esthet Restor Dent - 2018 - Tezulas - Clinical Procedures Designs and Survival Rates of All Ceramic Resin Bonded FixedFrederico RovedaÎncă nu există evaluări
- Significance of 4D Printing For Dentistry: Materials, Process, and PotentialsDocument9 paginiSignificance of 4D Printing For Dentistry: Materials, Process, and PotentialsMohamed FaizalÎncă nu există evaluări
- Overview of Nanoparticle Coating of Dental Implants For Enhanced Osseointegration and Antimicrobial PurposesDocument13 paginiOverview of Nanoparticle Coating of Dental Implants For Enhanced Osseointegration and Antimicrobial Purposesmichelle alvarracinÎncă nu există evaluări
- Introducing Dental ImplantsDocument13 paginiIntroducing Dental ImplantsKeyser SozeÎncă nu există evaluări
- Diagnosis and Treatment Planning in FPDDocument109 paginiDiagnosis and Treatment Planning in FPDaziz2007Încă nu există evaluări
- Classification and Impression Techniques of ImplantsDocument72 paginiClassification and Impression Techniques of ImplantsGoutham Sunil100% (5)
- Name Clinic/Hosp/Med Name &address Area City Speciality SEWA01 Disc 01 SEWA02 DIS C02 SEWA03 Disc 03 SEWA04 DIS C04 Contact No. EmailDocument8 paginiName Clinic/Hosp/Med Name &address Area City Speciality SEWA01 Disc 01 SEWA02 DIS C02 SEWA03 Disc 03 SEWA04 DIS C04 Contact No. EmailshrutiÎncă nu există evaluări
- Step-By-Step Instructions On The: Straumann TibrushDocument4 paginiStep-By-Step Instructions On The: Straumann Tibrushadambear213Încă nu există evaluări
- Thesis ImplantDocument194 paginiThesis ImplantKaushik keth100% (1)
- Implant BiomaterialsDocument18 paginiImplant BiomaterialsPadma GnanamÎncă nu există evaluări
- Lecture 1, Introduction To Complete Dentures (Script)Document17 paginiLecture 1, Introduction To Complete Dentures (Script)JustDen09100% (2)
- Impacts of Orthodontic Treatment On PeriDocument10 paginiImpacts of Orthodontic Treatment On PeriCatia Sofia A PÎncă nu există evaluări
- Mock Exam 11Document11 paginiMock Exam 11Abhay Khanna100% (2)
- Implant ComplicationsDocument15 paginiImplant ComplicationsDhanasriÎncă nu există evaluări
- Abutment Options For The Restoration of The Malalinged Implant 2016 PDFDocument5 paginiAbutment Options For The Restoration of The Malalinged Implant 2016 PDFmarwa100% (1)
- Complications, Failures and Maintainence of Dental Implant: Presented By: DR Tarun Sharma Mds Iind YearDocument58 paginiComplications, Failures and Maintainence of Dental Implant: Presented By: DR Tarun Sharma Mds Iind YearHimanshuGoyalÎncă nu există evaluări
- Jurnal 3Document5 paginiJurnal 3ayu augustineÎncă nu există evaluări
- Socket Shield Otto Zuhr Hurzeler PDFDocument12 paginiSocket Shield Otto Zuhr Hurzeler PDFLozovan GregoryÎncă nu există evaluări
- Biokompatibilitas PhilipDocument23 paginiBiokompatibilitas PhilipKrisna MertaÎncă nu există evaluări
- Mandible Vertical Height Correction Using LingualDocument5 paginiMandible Vertical Height Correction Using LingualNguyễn Thái AnÎncă nu există evaluări
- VersahDocument1 paginăVersahNehas HassanÎncă nu există evaluări
- JADA 2012 Balevi 1011 2Document3 paginiJADA 2012 Balevi 1011 2Linda RodriguezÎncă nu există evaluări
- Masticatory Force Measurement in Natural Dentition: Himmlova@seznam - CZ WWW - Vus.czDocument1 paginăMasticatory Force Measurement in Natural Dentition: Himmlova@seznam - CZ WWW - Vus.czHadil AltilbaniÎncă nu există evaluări
- Immediate Loading of Dental Implants PDFDocument15 paginiImmediate Loading of Dental Implants PDFAmar Bimavarapu100% (2)
- Scientic Rationale For Dental Implant DesignDocument34 paginiScientic Rationale For Dental Implant DesignvikramÎncă nu există evaluări
- Ora Aid Dental DressingDocument30 paginiOra Aid Dental Dressingahmed amerÎncă nu există evaluări
- Advanced Restorative Dentistry A Problem For The ElderlyDocument8 paginiAdvanced Restorative Dentistry A Problem For The ElderlyAli Faridi100% (1)