Documente Academic
Documente Profesional
Documente Cultură
Do We Have The Tools To Prevent Phantom Limb Pain .11
Încărcat de
Noha Gamal El-AassarDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Do We Have The Tools To Prevent Phantom Limb Pain .11
Încărcat de
Noha Gamal El-AassarDrepturi de autor:
Formate disponibile
Do We Have the Tools to Prevent Phantom Limb Pain?
ERSISTENT pain after limb amputation is common, most often taking the form of phantom limb pain or localized pain in the residual portion of the limb (stump pain). The conflicts in Afghanistan and Iraq have brought this to the forefront: in a report1 appearing in 2008, of the 8,058 reported military casualties in US military personnel, 5,684 (70.5%) had major limb injuries; and 423 (7.4%) of patients with major limb injuries underwent amputation. In a recent nationwide survey2 of more than 1,088 amputees in Germany, 14.8% were pain free, 74.5% had phantom limb pain, 45.2% had stump pain, and 35.5% had a combination of both types of pain. This pain led to sleep disorders in most of those affected1 and has been linked with long-term adverse health outcomes, including acceleration in onset of cardiovascular disease, obesity, and chronic joint and low-back pain.3 Not all amputees experience persistent pain, and the reasons for this are unclear. One of the risk factors that seem to be associated with a higher prevalence of persistent pain is severe and poorly controlled pain before surgery,4 raising the possibility that providing good analgesia before amputation may well decrease the risk of developing chronic pain. In this issue of ANESTHESIOLOGY, Karanikolas et al.5 present the results of a small randomized controlled trial in patients undergoing amputation; the results further support the notion that providing for good pain control before amputation may be one of our best hopes of minimizing the risk of persistent pain after amputation. The concept of preemptive analgesia (i.e., the idea that central sensitization might be mitigated or prevented altogether by reducing or eliminating the barrage of nociceptive input reaching the central nervous system and thereby decreasing the degree of central sensitization) arose more than a decade ago.6 Anesthesiologists embraced the concept that establishing neural blockade in the area of surgery before the surgical insult might improve pain treatment. The idea that preoperative epidural blockade could be used preemptively to provide analgesia before amputation and reduce the prevalence of persistent postamputation pain in the first 12 months after surgery was first tested by Bach et al.7 in 1988. In this study, 11 patients received a continuous lumbar epidural block so that they were pain free for 3 days before the operation; however, patients who received epidural analgesia and remained in pain were excluded from the trial, a significant shortcoming in this small study. The control group of 14 patients all had preoperative limb pain. Seven days after the operation, 3 (27%) of 11 patients in the preoperative epidural group and 9 (64%) of 14 patients in the control group had phantom limb pain. After 6 months, all patients in
Accepted for publication January 4, 2011. The authors are not supported by, nor maintain any financial interest in, any commercial activity that may be associated with the topic of this article.
Copyright 2011, the American Society of Anesthesiologists, Inc. Lippincott Williams & Wilkins. Anesthesiology 2011; 114:1021 4
the epidural group were pain free, whereas 5 (36%) of 14 patients in the control group had pain. After 1 yr, all the patients in the epidural group were still pain free; 3 (21%) of 14 patients in the control group had phantom limb pain. Despite these promising early results, numerous studies have ensued and the true benefit of preemptive analgesia in and of itself appears to be limited.8 Nevertheless, severe pain after amputation is clearly associated with a higher prevalence of postamputation pain,9,10 suggesting that aggressive efforts to control pain before surgery may have the potential of decreasing the prevalence of chronic pain. The outcomes in previous trials of preemptive analgesia and phantom limb pain in comparison with the new trial appearing in this issue are shown in Table 1. In the study by Karanikolas et al.,5 which appears in this issue of ANESTHESIOLOGY, 65 patients with severe lower-limb ischemic pain from peripheral vascular disease underwent amputation and were assigned to one of five analgesic regimens, including preoperative, intraoperative, and/or postoperative use of epidural analgesia or intravenous opioids, delivered by a patient-controlled analgesia device to provide adequate pain relief. Small groups of patients receiving these interventions were compared against standard means of providing preoperative analgesia using intermittent nurse-administered doses of intramuscular opioid. The analysis reveals consistent and striking differences between the control group receiving intramuscular opioid and all other treatment groups: the patient groups whose pain was well controlled perioperatively using combinations of intravenous patientcontrolled analgesic opioid and/or epidural analgesia had a dramatically decreased prevalence of phantom limb pain 6 months after amputation compared with the opioid analgesia alone group (15 [28.8%] of 52 patients vs. 9 [75.0%] of 12 patients). In addition to decreasing the prevalence of phantom limb pain, the severity of symptoms in those who did develop phantom limb pain was lower in the groups with better pain control before surgery than in the control group. Therefore, providing good perioperative pain control before and after amputation was enough to dramatically reduce the prevalence and severity of postamputation pain. The means used to control pain preoperatively in the control group in this study deserve special attention. Those receiving conventional preoperative analgesia (i.e., the control group) were given intramuscular meperidine or codeine/acetaminophen orally and had much higher pain scores (of a total 100) before surgery. This group of control
This Editorial View accompanies the following article: Karanikolas M, Aretha D, Tsolakis J, Monantera G, Kiekkas P, Papadoulas S, Swarm RA, Filos KS: Optimized perioperative analgesia reduces chronic phantom limb pain intensity, prevalence, and frequency: A prospective, randomized, clinical trial. ANESTHESIOLOGY 2011; 114:1144 54.
Anesthesiology, V 114 No 5
1021
May 2011
Editorial Views
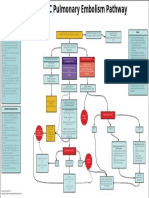
Table 1. Studies Examining the Rate of PLP after Perioperative Treatment with Epidural Analgesia or Continuous Perineural Infusion of a Local Anesthetic
Rate of PLP at 6 Months, % Rate of PLP at 1 yr, % Level of Significance, Study Control P Group Group Level of Significance, LTFU, P %
No. of Patients Study Group Anesthetic Control Group Analgesic
Source Studies Comparing Opioids on Demand with Epidural Analgesia Bach et al.,7 1988 Jahangiri et al.,11 1994 Nikolajsen et al.,12 1997 Nikolajsen et al.,13 1998 Studies Comparing Other Analgesic Regimens Fisher and Meller,14 1991 Lambert et al.,15 2001 Nikolajsen et al.,16 2006 Wilson et al.,17 2008 Borghi et al.,18 2010 Current Study Karanikolas et al.,5 2011
Type
Mode
Study Control Study Control Group Group Group Group
PCC PCC
BUP, M, or BUP/M BUP/DM/C
EPID EPID
Various analgesics Opioids on demand Opioids on demand Opioids on demand
11 13
14 11
0 8
28 73
0.05 0.002
0 8
27 73
0.20 0.002
24.0 0.0
RCT
BUP/M
EPID
29
30
81
55
NS
75
69
NS
52.5
RCT
BUP/M
EPID
23
22
79
59
NS
31.1
POC/HS BUP
PN
Opioids on demand Opioids on demand BUPI (EPID)
11
20
28.8
RCT RCT
RCT POC
BUP/DM EPID vs. vs. BUP PN GABAPENT PO BUP (EPID) KETA/BUP EPID BUP PN
14 23
16 23
63 58
88 50
NS NS
38
50
NS
10.7 28.3
BUP No control group Nurseadministered opioids on demand
24 71
29
40 17
19
NS
50 17
40
NS
43.3 12.7
RCT
EPID/EPID/ EPID PCA/EPID/ EPID PCA/EPID/ PCA PCA/GA/ PCA
EPID and/ or IV PCA
13 13 12 13
12
8 31 58 23
75
0.001 0.027 NS 0.009
11.1*
Adapted with permission from Ypsilantis and Tang.8 * The range was from 0% to 23.1%. Patients lost to follow-up in the study by Karanikolas et al. were as follows: control, 0 (0%) of 12; EPID/EPID/EPID, 3 (23.1%) of 13; PCA/EPID/EPID, 2 (15.4%) of 13; PCA/EPID/PCA, 1 (8.3%) of 12; and PCA/GA/PCA, 1 (7.7%) of 13. BUP bupivacaine; C clonidine; DM diamorphine; EPID epidural; GA general anesthesia; GABAPENT gabapentin; IV intravenous; KETA ketamine; LTFU initial patient population lost to end follow-up; M morphine; NS nonsignificant; PCA patient-controlled analgesia; PCC prospective case-controlled study; PLP phantom limb pain; PN perineural block; PO orally; POC/HS prospective observational cohort study with historical control; RCT randomized controlled trial.
patients had severe and ongoing pain (median pain score, 70) at the end of the 48-h preoperative observation period just before amputation. In comparison, patients receiving either intravenous patient-controlled analgesic opioids or epidural analgesia preoperatively had little or no pain just before amputation (median pain score range, 0 20). Is this really conventional treatment? A brief glance at the baseline pain scores in available published trials (table 2) demonstrates that the baseline pain scores in the current study were not atypical; however, the pain scores in the treatment group once pain treatment had been
Anesthesiology 2011; 114:1021 4 1022
initiated remained higher than would be expected with free access to opioid analgesics on demand. It is unlikely in most developed nations that patients would be allowed to continue for 48 h with reports indicating severe and ongoing pain without more aggressive treatment of some kind. Karanikolas et al.5 note, The high perioperative pain scores in the control group raise the concern that analgesic doses and/or frequency was inadequate. However, unfortunately, analgesia, as provided in the control group, was the norm in our hospital and probably in many other hospitals.
J. P. Rathmell and H. Kehlet
EDITORIAL VIEWS
Table 2. Comparison of Baseline Pain Scores in Studies Examining the Rate of Limb Pain (PLP) after Perioperative Treatment with Epidural Analgesia or Continuous Perineural Infusion of a Local Anesthetic
Scores after Analgesic Treatment (before Amputation)* Study Group 0 (00) Control Group 31 (2151) Rate of PLP at 6 Months, % Level of Significance, P NS
Baseline Pain Scores* Study Group Anesthetic Control Group Analgesic Opioids on demand Opioids on demand BUP Study Group 51 (2478) Control Group 44 (2568)
No. of Patients
Source Nikolajsen et al.,12 1997 Nikolajsen et al.,13 1998 Wilson et al.,17 2008 Lambert et al.,15 2001 Nikolajsen et al.,16 2006 Karanikolas et al.,5 2011
Type
Mode EPID
Study Control Study Control Group Group Group Group 27 29 81 55
RCT BUP/M
RCT BUP/M
EPID
62
31
46
29
0 (031)
29 (080)
23
22
79
59
NS
RCT KETA/BUP
EPID
50 (4050)
70 (5083)
NR
NR
24
29
40
19
NS
RCT BUP/DM vs. BUP
EPID vs. PN
Opioids on demand BUP (EPID)
60 (1080)
50 (090)
NR
NR
14
16
63
88
NS
RCT GABAPENT PO BUP (EPID) RCT EPID/EPID/ EPID or EPID IV PCA PCA/EPID/ EPID PCA/EPID/ PCA PCA/GA/ PCA
80 (20100)
80 (10100)
NR
NR
23
23
58
50
NS
Nurse90 (70100) administered opioids on 82 (25100) demand 90 (70100) 80 (50100)
70 (70100)
0 (030) 20 (030) 20 (030) 10 (035)
60 (2080)
13 13 12 13
12
8 31 58 23
75
0.001 0.027 NS 0.009
Only those studies that reported baseline pain scores and/or pain scores after analgesic treatment but before amputation were included. * Data are given as median (range) visual analog scale score unless otherwise indicated. The possible score was from 0 to 100. Data are given as mean SD. BUP bupivacaine; DM diamorphine; EPID epidural; GA general anesthesia; GABAPENT gabapentin; IV intravenous; KETA ketamine; M morphine; NS nonsignificant; NR not reported; PCA patient-controlled analgesia; PLP phantom limb pain; PN perineural block; PO orally; RCT randomized controlled trial.
The current study is plagued by the same limitations apparent in previous trials; the most worrisome of these limitations is the small sample size in the groups. Because of the few patients in each treatment group, it is difficult to interpret the results between the treatment subgroups receiving different intraoperative and postoperative analgesic regimens (i.e., the relative role of epidural vs. patientcontrolled analgesia). Nevertheless, the conclusions of this and many previous studies seem to be similar. Simply providing good pain control in the hours leading up to limb amputation and continued postoperatively with whatever means are available might well decrease the probability and severity of phantom limb pain. Sadly, poor control of pain before amputation likely remains more the rule than the exception. We can do better with the simple tools that are readily available to us today. What once passed for conventional perioperative analgesia should no longer be acceptable practice: the long-term well-being of our patients undergoing limb amputation is in our hands.
James P. Rathmell, M.D.,* Henrik Kehlet, M.D., Ph.D. *Division of Pain Medicine, Department of Anesthesia, Critical Care and Pain Medicine, Massachusetts General Hospital, and Harvard Medical School, Boston, Massachusetts. jrathmell@partners.org. Division of Surgical Pathophysiology, Rigshospitalet, Copenhagen University, Copenhagen, Denmark.
Anesthesiology 2011; 114:1021 4 1023
References
1. Stansbury LG, Lalliss SJ, Branstetter JG, Bagg MR, Holcomb JB: Amputations in U.S. military personnel in the current conflicts in Afghanistan and Iraq. J Orthop Trauma 2008; 22: 43 6 2. Kern U, Busch V, Rockland M, Kohl M, Birklein F: Prevalence and risk factors of phantom limb pain and phantom limb sensations in Germany: A nationwide field survey. Schmerz 2009; 23:479 88 3. Robbins CB, Vreeman DJ, Sothmann MS, Wilson SL, Oldridge NB: A review of the long-term health outcomes associated with war-related amputation. Mil Med 2009; 174:588 92 4. Kehlet H, Jensen TS, Woolf CJ: Persistent postsurgical pain: Risk factors and prevention. Lancet 2006; 367:1618 25 5. Karanikolas M, Aretha D, Tsolakis I, Monantera G, Kiekkas P, Papadoulas S, Swarm RA, Filos KS: Optimized perioperative analgesia reduces chronic phantom limb pain intensity, prevalence, and frequency: A prospective, randomized, clinical trial. ANESTHESIOLOGY 2011; 114:1144 54 6. Woolf CJ, Chong MS: Preemptive analgesia: Treating postoperative pain by preventing the establishment of central sensitization. Anesth Analg 1993; 77:36279 7. Bach S, Noreng MF, Tjellden NU: Phantom limb pain in amputees during the first 12 months following limb amputation, after preoperative lumbar epidural blockade. Pain 1988; 33:297301 8. Ypsilantis E, Tang TY: Pre-emptive analgesia for chronic limb pain after amputation for peripheral vascular disease: A systematic review. Ann Vasc Surg 2010; 24:1139 46 9. Jensen TS, Krebs B, Nielsen J, Rasmussen P: Immediate and J. P. Rathmell and H. Kehlet
Editorial Views
10.
11.
12.
13.
14.
long-term phantom limb pain in amputees: Incidence, clinical characteristics and relationship to pre-amputation limb pain. Pain 1985; 21:26778 Nikolajsen L, Ilkjaer S, Kroner K, Christensen JH, Jensen TS: The influence of preamputation pain on postamputation stump and phantom pain. Pain 1997; 72:393 405 Jahangiri M, Jayatunga AP, Bradley JW, Dark CH: Prevention of phantom pain after major lower limb amputation by epidural infusion of diamorphine, clonidine and bupivacaine. Ann R Coll Surg Engl 1994; 76:324 6 Nikolajsen L, Ilkjaer S, Christensen JH, Krner K, Jensen TS: Randomised trial of epidural bupivacaine and morphine in prevention of stump and phantom pain in lower-limb amputation. Lancet 1997; 350:13537 Nikolajsen L, Ilkjaer S, Jensen TS: Effect of preoperative extradural bupivacaine and morphine on stump sensation in lower limb amputees. Br J Anaesth 1998; 81: 348 54 Fisher A, Meller Y: Continuous postoperative regional anal-
15.
16.
17.
18.
gesia by nerve sheath block for amputation surgery: A pilot study. Anesth Analg 1991; 72:300 3 Lambert AW, Dashfield AK, Cosgrove C, Wilkins DC, Walker AJ, Ashley S: Randomized prospective study comparing preoperative epidural and intraoperative perineural analgesia for the prevention of postoperative stump and phantom limb pain following major amputation. Reg Anesth Pain Med 2001; 26:316 21 Nikolajsen L, Finnerup NB, Kramp S, Vimtrup AS, Keller J, Jensen TS: A randomized study of the effects of gabapentin on postamputation pain. ANESTHESIOLOGY 2006; 105: 1008 15 Wilson JA, Nimmo AF, Fleetwood-Walker SM, Colvin LA: A randomised double blind trial of the effect of pre-emptive epidural ketamine on persistent pain after lower limb amputation. Pain 2008; 135:108 18 Borghi B, DAddabbo M, White PF, Gallerani P, Toccaceli L, Raffaeli W, Tognu A, Fabbri N, Mercuri M: The use of pro` longed peripheral neural blockade after lower extremity amputation: The effect on symptoms associated with phantom limb syndrome. Anesth Analg 2010; 111:1308 15
Anesthesiology 2011; 114:1021 4
1024
J. P. Rathmell and H. Kehlet
S-ar putea să vă placă și
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- A Manual of Organic Materia Medica and PharacognosyDocument534 paginiA Manual of Organic Materia Medica and PharacognosyPeggy BarouniÎncă nu există evaluări
- Anemia Differential Diagnosis : Microcytic Normocytic MacrocyticDocument1 paginăAnemia Differential Diagnosis : Microcytic Normocytic Macrocyticمحمد عقيلي100% (1)
- InfertilityDocument55 paginiInfertilityFedlu SirajÎncă nu există evaluări
- Fractional RF Machine: Use InstructionDocument21 paginiFractional RF Machine: Use Instructionjuras500Încă nu există evaluări
- 10 12 15hematoo Edit 1Document10 pagini10 12 15hematoo Edit 1Anonymous 18GsyXbÎncă nu există evaluări
- Imaging of Intracranial InfectionsDocument12 paginiImaging of Intracranial Infectionsrafael rocha novaesÎncă nu există evaluări
- Hiperpigmentasi Paska InflamasiDocument18 paginiHiperpigmentasi Paska InflamasiNoventyChristiÎncă nu există evaluări
- EMCrit Lae Pulmonary FlowDocument1 paginăEMCrit Lae Pulmonary FlowhmsptrÎncă nu există evaluări
- A Bad Case of StripesDocument2 paginiA Bad Case of StripesRadhika RathoreÎncă nu există evaluări
- Utsmidterms PDFDocument10 paginiUtsmidterms PDFJazzie SorianoÎncă nu există evaluări
- Long Term Follow Up After Admin Human GT Products - Jan - 2020Document37 paginiLong Term Follow Up After Admin Human GT Products - Jan - 2020DÎncă nu există evaluări
- Quick Energy Boost Yoga PosesDocument5 paginiQuick Energy Boost Yoga PosesTai CheeÎncă nu există evaluări
- Request For Cashless Hospitalisation For Health Insurance Policy PART C (Revised)Document4 paginiRequest For Cashless Hospitalisation For Health Insurance Policy PART C (Revised)Abhishek MkÎncă nu există evaluări
- En Abbott Realtime Sars-Cov-2: For Use Under An Emergency Use Authorization (Eua) OnlyDocument12 paginiEn Abbott Realtime Sars-Cov-2: For Use Under An Emergency Use Authorization (Eua) OnlyDevi OktaviannyÎncă nu există evaluări
- Impaction in Dairy Animals: Ashwani KumarDocument6 paginiImpaction in Dairy Animals: Ashwani KumarGiriÎncă nu există evaluări
- Tromso. Norway Orders Drug-Free Treatment in PsychiatryDocument21 paginiTromso. Norway Orders Drug-Free Treatment in PsychiatryMarcelo Astorga VelosoÎncă nu există evaluări
- Ectopic PregnancyDocument1 paginăEctopic PregnancyBheru Lal50% (2)
- RRL LocalinternationalDocument11 paginiRRL LocalinternationalkdfhjfhfÎncă nu există evaluări
- Unpaywall ArticleDocument2 paginiUnpaywall ArticleChristian HdezÎncă nu există evaluări
- Unit 2 - Innovations in Health and Medicine (Paragraphs)Document1 paginăUnit 2 - Innovations in Health and Medicine (Paragraphs)April ThunÎncă nu există evaluări
- Msds ChosunDocument6 paginiMsds ChosunDheeraj E MohananÎncă nu există evaluări
- Apraxia of Speech and Grammatical Language Impairment in Children With Autism Procedural Deficit HypothesisDocument6 paginiApraxia of Speech and Grammatical Language Impairment in Children With Autism Procedural Deficit HypothesisEditor IJTSRDÎncă nu există evaluări
- Giardia M.SC PDFDocument18 paginiGiardia M.SC PDFRahul ChaudharyÎncă nu există evaluări
- Kidney DiseasesDocument22 paginiKidney Diseasesphoto copyhemnÎncă nu există evaluări
- Amniotic MembraneDocument8 paginiAmniotic Membraneapi-481789048Încă nu există evaluări
- The Importance of Mineral Elements For Humans, Domestic Animals and Plants: A ReviewDocument3 paginiThe Importance of Mineral Elements For Humans, Domestic Animals and Plants: A ReviewMaricel Canlas MacatoÎncă nu există evaluări
- The SPLENOMEGALY Power Point Dr. CosmescuDocument29 paginiThe SPLENOMEGALY Power Point Dr. CosmescuNisha PillaiÎncă nu există evaluări
- Osteosarcoma PDFDocument3 paginiOsteosarcoma PDFkc andrea torresÎncă nu există evaluări
- 04-15-21 Covid-19 Vaccine TrackerDocument52 pagini04-15-21 Covid-19 Vaccine TrackerJohn Michael JetiganÎncă nu există evaluări
- Extensive Reading - AVK44CDocument42 paginiExtensive Reading - AVK44CNinh Nhat Thao Vy K189Încă nu există evaluări