Documente Academic
Documente Profesional
Documente Cultură
Dexamethasone
Încărcat de
Mits Valencia KarlssonDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Dexamethasone
Încărcat de
Mits Valencia KarlssonDrepturi de autor:
Formate disponibile
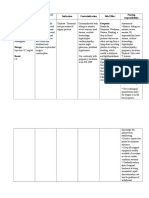
Generic name (brand name) Dexamethasone
Indication
Dosage, Route, frequency Shock: 4 to 8 mg intravenously initially, repeat if necessary to a total dose of 24 mg. Autoimmune diseases and inflammations: longterm therapy with 0.5 to 1.5 mg oral per day. Avoid more than 1.5 mg daily, because serious side effects are more frequently encountered with higher doses. Adjuvant to or part of chemotherapy: individual schedule Diagnostic purposes: special schedule
Mechanism of action Dexamethasone is a synthetic glucocorticoid which decreases inflammation by inhibiting the migration of leukocytes and reversal of increased capillary permeability. It suppresses normal immune response. Onset: As acetate: Prompt. Duration: 72 hr. Absorption: Readily absorbed from the GI tract (Oral). Distribution: Readily crosses the placenta. Protein binding: About 77%. Metabolism: Hepatic. Excretion: Via urine (65% of the dose within 24 hr).
Side effects
Adverse reaction
contraindication
Nursing Responsibility
(decadron)
Classification: Glucocorticoid, Corticosteroid
Pregnancy category: C
Hypercalcemia associated with cancer Short-term management of various inflammatory and allergic disorders, such as rheumatoid arthritis, collagen diseases (SLE), dermatologic diseases (pemphigus), status asthmaticus, and autoimmune disorders Hematologic disorders: Thrombocytopenic purpura, erythroblastopenia Trichinosis with neurologic or myocardial involvement Ulcerative colitis, acute exacerbations of multiple sclerosis, and palliation in some leukemias and
- acne; - anxiety; - black or tarry stool; - cold or infection that lasts a long time; - depression; - dizziness; - easy bruising; - headache; - increased hair growth; - insomnia; - irregular or absent menstrual periods; - muscle weakness; - restlessness; - skin rash; - stomach irritation; - swollen face, lower legs, or ankles; - upset stomach; - vision problems; - vomiting;
If these signs and symptoms will be noted instruct the patient to call or notify the physician immediately. Skin rash Swollen face, legs or ankles (fluid retention) Vision problems ( Dexamethasone may cause cataracts and increased intraocular pressure) Cold or infection that last for a long time Muscle weakness Black or tarry stool (suggestive of peptic ulceration caused by Dexamethasone use)
Contraindicated with infections, especially tuberculosis, fungal infections, amebiasis, vaccinia and varicella, and antibioticresistant infections, allergy to any component of the preparation used. Use cautiously with renal or hepatic disease; hypothyroidism, ulcerative colitis with impending perforation; diverticulitis; active or latent peptic ulcer; inflammatory bowel disease; CHF, hypertension, thromboembolic disorders; osteoporosis; seizure disorders; diabetes mellitus; lactation.
1. Monitor intake and output of patient. 2. Observe the patient for peripheral edema, steady weight gain, rales or crackles or dyspnea. Notify the physician immediately if these clinical manifestations are noted. 3. For patients with cerebral edema, assess then for level of consciousness changes and headache during the therapy. 4. Guaiac-test stools should be carried out. Guaiac-positive stools should be reported to the physician immediately. 5. Administer with meals to minimize GI irritation. 6. For patients with difficulty swallowing, tablets can be crushed and administered with fluids or food. However, capsules should be swallowed whole. 7. Educate the patient to take
Potentially Fatal: Reduced efficacy in
lymphomas Cerebral edema associated with brain tumor, craniotomy, or head injury Testing adrenocortical hyperfunction Unlabeled uses: Antiemetic for cisplatin-induced vomiting, diagnosis of depression Intra-articular or soft-tissue administration: Arthritis, psoriatic plaques Respiratory inhalant: Control of bronchial asthma requiring corticosteroids in conjunction with other therapy Intranasal: Relief of symptoms of seasonal or perennial rhinitis that responds poorly to other treatments
Half-life: About 190 min.
combination with ephedrine, cholestyramine, phenytoin, phenobarbital and rifampicin.
missed doses as soon as remembered, unless almost time for the next dose skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one. 8. Instruct patient to avoid people with known infection and contagious illnesses as corticosteroids causes immunosuppression and may mask symptoms of infection. For systemic administration, do not give drug to nursing mothers; drug is secreted in breast milk.
Give daily doses before 9 AM to mimic normal peak corticosteroid blood levels.
Increase dosage when patient is subject to stress.
Dermatologic preparations: Relief of inflammatory and pruritic manifestations of dermatoses that are steroid-responsive Ophthalmic preparations: Inflammation of the lid, conjunctiva, cornea, and globe
Taper doses when discontinuing high-dose or long-term therapy.
Do not give live virus vaccines with immunosuppressive doses of corticosteroids.
For respiratory inhalant, intranasal preparation, do not use respiratory inhalant during an acute asthmatic attack or to manage status asthmaticus.
Do not use intranasal product with untreated local nasal infections, epistaxis, nasal trauma, septal ulcers, or recent nasal surgery.
Taper systemic steroids carefully during transfer to inhalational steroids; adrenal insufficiency deaths have occurred.
For topical dermatologic preparations, use caution when occlusive dressings, tight diapers cover affected area; these can increase systemic absorption.
Avoid prolonged use near the eyes, in genital and rectal areas, and in skin creases
S-ar putea să vă placă și
- Vii. Drug Study Drug Indication Action Side/Adverse Effects Nursing Consideration Date Ordered: Generic Name: SpecificDocument1 paginăVii. Drug Study Drug Indication Action Side/Adverse Effects Nursing Consideration Date Ordered: Generic Name: SpecificnuraÎncă nu există evaluări
- Drug Study - DexamethasoneDocument2 paginiDrug Study - DexamethasoneCarla Tongson Maravilla100% (2)
- Dexamethasone (Drug Study)Document4 paginiDexamethasone (Drug Study)Franz.thenurse688871% (7)
- Nalbuphine (Nubain)Document2 paginiNalbuphine (Nubain)Adrianne Bazo100% (1)
- Drug Routes Side Effects Co4Ntraindications Nursing Responsibility Brand Name: Inhalation: CoughDocument2 paginiDrug Routes Side Effects Co4Ntraindications Nursing Responsibility Brand Name: Inhalation: CoughChristianne Janella PagadorÎncă nu există evaluări
- Hydrocortisone - Drug StudyDocument2 paginiHydrocortisone - Drug StudyKevin H. Milanes100% (2)
- Hydrocortisone Drug StudyDocument3 paginiHydrocortisone Drug StudyJesrel DelotaÎncă nu există evaluări
- Atracurium BesylateDocument4 paginiAtracurium BesylateStill DollÎncă nu există evaluări
- Drug Study (Aspirin, in Enalapril Maleate, Tramadol, AmlodipineDocument10 paginiDrug Study (Aspirin, in Enalapril Maleate, Tramadol, AmlodipineFlauros Ryu Jabien100% (1)
- Clindamycin Drug StudyDocument2 paginiClindamycin Drug StudyAlex MarieÎncă nu există evaluări
- Drug Study - HYDROCORTISONE, DIAZEPAM, DIGOXIN EtcDocument6 paginiDrug Study - HYDROCORTISONE, DIAZEPAM, DIGOXIN Etc'jmark FranciaÎncă nu există evaluări
- Rifampicin Drug StudyDocument3 paginiRifampicin Drug StudyNicole Louize CaloraÎncă nu există evaluări
- Clindamycin (Drug Study)Document4 paginiClindamycin (Drug Study)Franz.thenurse6888100% (1)
- College of Nursing: Pharmacological ManagementDocument3 paginiCollege of Nursing: Pharmacological ManagementAnika PleñosÎncă nu există evaluări
- Drug Study - BisacodylDocument4 paginiDrug Study - BisacodylKyla CastroÎncă nu există evaluări
- DRUG STUDY - DexamethasoneDocument26 paginiDRUG STUDY - DexamethasoneChristel Santos100% (5)
- VancomycinDocument1 paginăVancomycinE100% (2)
- LevofloxacinDocument2 paginiLevofloxacinMuhammad ArsalanÎncă nu există evaluări
- DRUG STUDY LevetiracetamDocument3 paginiDRUG STUDY LevetiracetamMaria Althea NajorraÎncă nu există evaluări
- Beclomethasone Dipropionate (Drug Study)Document2 paginiBeclomethasone Dipropionate (Drug Study)Franz.thenurse6888100% (1)
- Drug Stidy TramadolDocument2 paginiDrug Stidy TramadolRez ApegoÎncă nu există evaluări
- Drug Name Mecahnism of Action Indication Side Effects Generic NameDocument2 paginiDrug Name Mecahnism of Action Indication Side Effects Generic NamehahahaÎncă nu există evaluări
- VancomycinDocument3 paginiVancomycinGwyn Rosales100% (3)
- Drug StudyDocument9 paginiDrug Studywarlocke100% (2)
- AMIKACINDocument2 paginiAMIKACINJesrel DelotaÎncă nu există evaluări
- Drug Study in GentamicinDocument2 paginiDrug Study in Gentamicinanthony_alviar100% (1)
- 1 Drug Study - DexamethasoneDocument6 pagini1 Drug Study - DexamethasoneJohn100% (1)
- PhenobarbitalDocument1 paginăPhenobarbitalSherwin LauronÎncă nu există evaluări
- Drug StudyDocument6 paginiDrug StudyGeleen Margaret Atienza100% (1)
- Vit K Drug StudyDocument2 paginiVit K Drug StudyPrisHee YhaRz SalvadorÎncă nu există evaluări
- Enalapril MaleateDocument4 paginiEnalapril Maleateapi-3797941Încă nu există evaluări
- Drug StudyDocument3 paginiDrug StudyRae Marie AquinoÎncă nu există evaluări
- Amiodarone (PACERONE)Document1 paginăAmiodarone (PACERONE)Amanda CoadÎncă nu există evaluări
- Generic Name: Brand Name:: ClassificationsDocument2 paginiGeneric Name: Brand Name:: ClassificationsbillyktoubattsÎncă nu există evaluări
- DRug Study PhenytoinDocument1 paginăDRug Study Phenytoinmichelle marquezÎncă nu există evaluări
- OmeprazoleDocument2 paginiOmeprazoleLyka Ngayan0% (1)
- Drug Study DexamethasoneDocument4 paginiDrug Study Dexamethasoneamal abdulrahmanÎncă nu există evaluări
- Drug Study MetronidazoleDocument2 paginiDrug Study MetronidazoleJha NetÎncă nu există evaluări
- Drug Study NubainDocument2 paginiDrug Study NubainNylia Atibi100% (1)
- Co TrimoxazoleDocument2 paginiCo TrimoxazoleGrace Donato100% (1)
- Name of Drug FinalDocument7 paginiName of Drug FinalJaessa FelicianoÎncă nu există evaluări
- Hyperthermia NCPDocument2 paginiHyperthermia NCPMatthew Emmanuel M. Martinez0% (1)
- Generic Name: Amikacin SulfateDocument2 paginiGeneric Name: Amikacin Sulfateichiro017100% (7)
- Gentamycin Drug StudyDocument2 paginiGentamycin Drug StudyShin Guevara100% (3)
- Cyclobenzaprine Hydrochloride (Drug Study)Document1 paginăCyclobenzaprine Hydrochloride (Drug Study)Franz.thenurse6888Încă nu există evaluări
- Metronidazole 500mg/tab 1 Tab 3xadayDocument4 paginiMetronidazole 500mg/tab 1 Tab 3xadayCrisyl LipawenÎncă nu există evaluări
- Amikacin Drug StudyDocument4 paginiAmikacin Drug StudyMark Angelo LorzanoÎncă nu există evaluări
- Bearse Tablet InsertDocument2 paginiBearse Tablet InsertLeonard ByunÎncă nu există evaluări
- Nrn101 and Nrn102 Drug Card: Zithromax, Zmax, Z-PakDocument2 paginiNrn101 and Nrn102 Drug Card: Zithromax, Zmax, Z-PakJanet Sheldon50% (2)
- SERETIDEDocument3 paginiSERETIDETempoÎncă nu există evaluări
- Name of Drugs Kaligen 8Document2 paginiName of Drugs Kaligen 8mellany100% (1)
- IsoketDocument2 paginiIsoketJaessa FelicianoÎncă nu există evaluări
- DrugsDocument2 paginiDrugsgailannreyesÎncă nu există evaluări
- DrugsDocument2 paginiDrugsgailannreyesÎncă nu există evaluări
- Docetaxel - 40mg/ml Injection: InstructionDocument11 paginiDocetaxel - 40mg/ml Injection: InstructionywÎncă nu există evaluări
- Drug Cefaclor IsoxsuprineDocument6 paginiDrug Cefaclor IsoxsuprineJelly Ong 王金玉Încă nu există evaluări
- Drug StudyDocument6 paginiDrug StudyFloramae Celine BosqueÎncă nu există evaluări
- Drug Analysis: Submitted By: GALICINAO, Gretta Shalou GDocument9 paginiDrug Analysis: Submitted By: GALICINAO, Gretta Shalou GggalicinaoÎncă nu există evaluări
- HydrocortisoneDocument2 paginiHydrocortisoneMaggieÎncă nu există evaluări
- Drug StudyDocument9 paginiDrug StudyAlexander Chavez Alto100% (1)
- Topical Route of Drug Administration and Dosage Forms: Dr. Mansij Biswas, FYRDocument74 paginiTopical Route of Drug Administration and Dosage Forms: Dr. Mansij Biswas, FYRknotstmÎncă nu există evaluări
- Intranasal Midazolam Versus Intravenous Diazepam For The Treatment of Acute Seizures in Paediatric PatientsDocument5 paginiIntranasal Midazolam Versus Intravenous Diazepam For The Treatment of Acute Seizures in Paediatric PatientsArif KusumawidjayaÎncă nu există evaluări
- Introduction To Novel Drug Delivery SystDocument5 paginiIntroduction To Novel Drug Delivery SystshreeharilxrÎncă nu există evaluări
- UKMi QA Allergic-Rhinitis-Pregnancy 2020 FINALDocument7 paginiUKMi QA Allergic-Rhinitis-Pregnancy 2020 FINALChristian AriÎncă nu există evaluări
- LohiaDocument11 paginiLohiastanleyÎncă nu există evaluări
- Trazissin® VASOPRESSIN INJECTION USP 20IU Per 1ml Solution For Injection Package Leaflet - Taj PharmaDocument1 paginăTrazissin® VASOPRESSIN INJECTION USP 20IU Per 1ml Solution For Injection Package Leaflet - Taj PharmaTAJ PHARMA — A Health Care ProviderÎncă nu există evaluări
- Desmopressin: Drug InformationDocument12 paginiDesmopressin: Drug InformationKeny StefanusÎncă nu există evaluări
- Nasal and Pulmonary Drug Delivery SystemDocument71 paginiNasal and Pulmonary Drug Delivery SystemDRx Sonali TareiÎncă nu există evaluări
- Pharmacology - Technology TrendsDocument2 paginiPharmacology - Technology TrendsGiselleÎncă nu există evaluări
- Intranasal Liposomes: An Approach For Drug Delivery To BrainDocument13 paginiIntranasal Liposomes: An Approach For Drug Delivery To BrainMaruf Momin100% (1)
- ZavzpretDocument21 paginiZavzpretNeethu Anna StephenÎncă nu există evaluări
- Nasya Karma in Relation To Anidra W.S.R To InsomniaDocument4 paginiNasya Karma in Relation To Anidra W.S.R To InsomniaEditor IJTSRDÎncă nu există evaluări
- Translated From Original Russian Instructions by Extrapharmacy Online StoreDocument1 paginăTranslated From Original Russian Instructions by Extrapharmacy Online StoreFaiz AmriÎncă nu există evaluări
- Nasal Drug Delivery System: By: Samer Khalid AliDocument36 paginiNasal Drug Delivery System: By: Samer Khalid AliPh SamerÎncă nu există evaluări
- Yashwant V. Pathak, Hemant K. S. Yadav - Nasal Drug Delivery - Formulations, Developments, Challenges, and Solutions-Springer (2023)Document426 paginiYashwant V. Pathak, Hemant K. S. Yadav - Nasal Drug Delivery - Formulations, Developments, Challenges, and Solutions-Springer (2023)Putri RamadhaniÎncă nu există evaluări
- Zeteo Biomedical Introduces ZEOx1 Orion (TM) Nasal Vaccine and Drug Delivery SystemsDocument2 paginiZeteo Biomedical Introduces ZEOx1 Orion (TM) Nasal Vaccine and Drug Delivery SystemsPR.comÎncă nu există evaluări
- PosiSep PosiSepX FlyerDocument2 paginiPosiSep PosiSepX FlyerpkfosteriusÎncă nu există evaluări
- When To Pick The Nose: Out-of-Hospital and Emergency Department Intranasal Administration of MedicationsDocument9 paginiWhen To Pick The Nose: Out-of-Hospital and Emergency Department Intranasal Administration of MedicationsepraetorianÎncă nu există evaluări
- 2.intra Nasal Drug Delivery SystemDocument62 pagini2.intra Nasal Drug Delivery SystemSakshi SinghÎncă nu există evaluări
- Allergic PDFDocument17 paginiAllergic PDFSiska HarapanÎncă nu există evaluări
- Cyclic Vomiting Syndrome - UpToDateDocument38 paginiCyclic Vomiting Syndrome - UpToDateAlvaro HuidobroÎncă nu există evaluări
- Triamcinolone Clinical - PREA PDFDocument62 paginiTriamcinolone Clinical - PREA PDFnephylymÎncă nu există evaluări
- NaloxonaDocument12 paginiNaloxonaApuntes espacioÎncă nu există evaluări
- 10 1016@j Jconrel 2017 09 001Document88 pagini10 1016@j Jconrel 2017 09 001ummi isnainiÎncă nu există evaluări
- The Role of Himsradya Taila Nasya in Primary HypothyroidismDocument4 paginiThe Role of Himsradya Taila Nasya in Primary HypothyroidismResearch ParkÎncă nu există evaluări
- Aria Pharm PGDocument14 paginiAria Pharm PGBlack3Fox56Încă nu există evaluări
- ASCIA Allergic Rhinitis Treatment Plan 2020Document1 paginăASCIA Allergic Rhinitis Treatment Plan 2020BigPharma HealtcareÎncă nu există evaluări
- Pathophysiology and Management of Gustatory Rhinitis: Literature ReviewDocument8 paginiPathophysiology and Management of Gustatory Rhinitis: Literature ReviewmiraÎncă nu există evaluări
- Optimization of Curcumin Nanocrystals As Promising Strategy For Nose-to-Brain Delivery ApplicationDocument27 paginiOptimization of Curcumin Nanocrystals As Promising Strategy For Nose-to-Brain Delivery ApplicationJohn CoucÎncă nu există evaluări
- Beclomethasone Dipropionate (Drug Study)Document2 paginiBeclomethasone Dipropionate (Drug Study)Franz.thenurse6888100% (1)