Documente Academic
Documente Profesional
Documente Cultură
Colonic Inertia Simptoms
Încărcat de
Lindsey MaryanDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Colonic Inertia Simptoms
Încărcat de
Lindsey MaryanDrepturi de autor:
Formate disponibile
Colonic Inertia Symptoms
Arthritis of inflammatory colonic disease are the joint damage that may be peripheral inflammatory and / or axial and which may occur in association with colonic disease (ulcerative colitis / Crohn disease, acute enterocolitis microbial gluten enteropathy, colonic bypass, colitis, collagen, lymphocytic colitis). The possibility that certain food antigens to be absorbed unchanged and to generate immune responses is suggested by clinical observation mainly on breast-fed children, who make colic more frequently when the mother consuming cow's milk. Dietary and socioeconomic factors seem to play an important role in these diseases. Tobacco seems to be protective in ulcerative colitis but also is an aggravating factor in Crohn's disease by immunosuppression effect or influence on the protective mucin colonic mucosa. Both Crohn's disease and ulcerative colitis exist in similar distribution of age (1014 years and 60-70 years), meeting in both sexes but is more common Crohn's disease in women.
One is the involvement of genetic determinants. The genetic factor is the HLA B27 is associated with impaired axial spine.Type I peripheral arthritis is associated with HLA B27, B35 and DR1 and peripheral arthritis associated with HLA type B44 II. Triggers joint inflammation (arthritis) of colonic disease is unknown but most likely involved different germs. In Crohn's disease and mycobacteria were isolated in ulcerative colitis are present signs that a particular approach as ulcerative colitis were found in serum antibodies to Escherichia coli. There have also been involved citomegalovirusuri or Shigella, but not isolated from the colonic wall to determine if the infection is causing or is a superadd. Onset or relapse under emotional stress raised the question of etiologic role of psychological factors but more likely they are secondary.Infection associated with colonicinflammation cauzeza colonic permeability increase for some microbial antigens in the diet lead to loss of tolerance to bacterial flora of their own, forming circulating immune complexes, antigens in the joint and increase storage joint inflammation (arthritis). Crohn's disease have differences in terms of pathology compared with ulcerative colitis. In ulcerative colitis there is inflammation in the colon mucosa (hyperemia, ulcers, bleeding) uniform, continuous and rectum are often interested in Crohn's disease is more frequently affected ileum, which is thickened. Because inflammation occurs after loss of epithelial cells leading to ulceration. Chronic inflammation in Crohn's disease affects all layers of the colonic wall and mesenteric lymph regional interest for including so over time the intestine is thickened, narrow lumen until obstruction. Lesions are staple in Crohn's disease, in approximately 50% of the rectum is not affected. Symptoms Arthritis may be associated with some colonic diseases, pancreatitis, acute hepatitis, chronic active hepatitis, acute enteric infections. Intestine is, on the other hand, often interested in some rheumaticcolonic diseasesuch as Behcet's disease, Reiter syndrome. Extraarticular manifestations in inflammatory bowel disease are found in 25% of cases. Those with severe inflammatory bowel disease presents as joint manifestations: inflammatory arthritis, ankylosing spondylitis and sacroileita. In Crohn's disease are found peripheral arthritis but is recorded and an increased prevalence of ankylosing spondylitis. Arthritis of inflammatory bowel disease usually begins with systemic manifestations, overall influences weight loss, fever, abdominal pain, diarrhea. In ulcerative colitis diarrhea may be bloody, evolution is intermittent in flare-ups or chronic. In Crohn's disease due to the extension variable clinical lesions is diverse - from the appearance of acute sudden onset, fever, abdominal pain suggesting appendicitis chronic forms living dominated compared with the overall digestive signs. This joint manifestations is found in different proportions in inflammatory bowel disease. Peripheral arthritis is seen in 17-20% of patients with HLA B27 is not asocisata.Arthritis Type I occurs in 5% of patients and reflect colonic inflammation activity.This condition may be oligoarticular, monoarticulara, acute, asymmetrical, migratory. Usually large joints are affected leg (often knee), appears early and is associated with erythema nodosum and uveitis. Arthritis Type II is found in 3-4% of patients, polyarticular, symmetrical. This type of arthritis cause joint deformities, affecting the metacarpophalangeal joints frequently.Large joints are rarely involved knees, ankles, elbows, shoulders, fists, proximal interphalangeal joints and metatarsophalangeal. Joint damage is present in both types of arthritis, inflammation bowel disease reflects not. Sacroileita (inflammation of the sacroiliac joints) occurs in 4-8% of asymptomatic cases and about 1-26% ankylosing spondylitis. Arthritis acute colonic parallel flashes, occurred early in the course of inflammatory bowel disease, is limited in scope and is manifested by swelling, redness, local heat and cause destruction and osteoarticular deformities. Both Crohn's disease and ulcerative colitis are frequently associated with spondilartrita. Spondylitis in inflammatory bowel
disease do not differ from idiopathic in terms of onset and clinical evolution. Frequent association with arthritis and scapulohumeral coxofemurala is increased in patients with ankylosing spondylitis. Other possible joint manifestations are common among digital clubbing in Crohn's disease and that disappears after surgical treatment of disease through inactivity osteoporosis, malabsorption and / or after treatment with corticosteroids, osteomalacia in malabsorption. Extraarticular manifestations in inflammatory bowel disease are: - Eye damage - often acute anterior uveitis is present, which is unilateral, usually transient and recurrent. Anterior uveitis is frequently associated with severe axial and HLA B27. - Skin and mucosal lesions - erythema nodosum is seen in those with severe type I peroferica - Amyloidosis - rare, about 1% of patients, 25% were found postmortem. Tests Blood tests conducted reveals inflammatory syndrome (elevated ESR, positive C-reactive protein), anemia characteristic of chronic disease, leukocytosis, thrombocytosis (700000-1000000/mm3). Synovial fluid analysis often highlights an increased number of leukocytes (1500-5000/mm3) with predominant polymorphonuclear. Immunological exploration highlights the absence of RF and antinuclear antibodies (ANA) and the presence of HLA B27. Radiological examination emphasizes the inflammatory axial (spine damage), sacroileita symmetric (inflammation of the sacroiliac joints) bilateral and present sindesmofitelor typical spine (column layout is the "column of bamboo"). The peripheral arthritis of the joints involved radiological examination rarely reveals destructive arthropathy of the hip and small joints of the hands and feet, sometimes entezita. Diagnosis and Treatment Diagnosis of rheumatic manifestations and their framing raise special problems when inflammatory bowel disease is unknown. Positive diagnosis is established after history and laboratory explorations. This arthritis must first great migration of rheumatic fever. If monoarticulare damage (affecting a single joint) to make problems of differential diagnosis of gout, pseudogout, Reiter's syndrome and reactive arthritis onset diarrhea. In chronic forms of arthritis with joint deformities that accompany inflammatory bowel colonic disease with rheumatoid arthritis differential diagnosis is difficult, especially when joint manifestations does not correlate with the bowel or sometimes when rheumatoid arthritis is seronegative. Treatment Specific treatment is with anti-inflammatory, used for axial and peripheral joint pains.Sometimes anti-inflammatory drugs can exacerbate especially colonic symptoms, such as in some cases be used only if symptoms and signs of inflammatory bowel disease do not occur or worsen. Intra-articular corticosteroid therapy may be administered intravenously and in some cases, especially for digestive distress in the form of enema. Remission treatment including joint pain is sulphasalazine (mesalazine, olsalazina), azathioprine or 6mercaptopurine, methotrexate, cyclosporin A, anti-TNF biological therapy. For Type II joint damage and impaired biological axial anti TNF therapy is recommended: etanercept and infliximab. The axial impairment and physical therapy is beneficial.
http://colonic-inertia.blogspot.com/
S-ar putea să vă placă și
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- CAT 320D2: Hydraulic ExcavatorDocument5 paginiCAT 320D2: Hydraulic Excavatorhydeer 13Încă nu există evaluări
- Linguistics Is Descriptive, Not Prescriptive.: Prescriptive Grammar. Prescriptive Rules Tell You HowDocument2 paginiLinguistics Is Descriptive, Not Prescriptive.: Prescriptive Grammar. Prescriptive Rules Tell You HowMonette Rivera Villanueva100% (1)
- Arens - Auditing and Assurance Services 15e-2Document17 paginiArens - Auditing and Assurance Services 15e-2Magdaline ChuaÎncă nu există evaluări
- Introduction-: Microprocessor 68000Document13 paginiIntroduction-: Microprocessor 68000margyaÎncă nu există evaluări
- Technology Management 1Document38 paginiTechnology Management 1Anu NileshÎncă nu există evaluări
- 70 Valves SolenoidDocument105 pagini70 Valves SolenoidrizalÎncă nu există evaluări
- AIA1800 Operator ManualDocument184 paginiAIA1800 Operator ManualZain Sa'adehÎncă nu există evaluări
- Movie Piracy in Ethiopian CinemaDocument22 paginiMovie Piracy in Ethiopian CinemaBehailu Shiferaw MihireteÎncă nu există evaluări
- Powerpoint Speaker NotesDocument4 paginiPowerpoint Speaker Notesapi-273554555Încă nu există evaluări
- HirePro Video Proctored Online-Instruction Sheet - Bain IndiaDocument1 paginăHirePro Video Proctored Online-Instruction Sheet - Bain Indiaapoorv sharmaÎncă nu există evaluări
- Chronic Kidney DiseaseDocument15 paginiChronic Kidney Diseaseapi-270623039Încă nu există evaluări
- Carob-Tree As CO2 Sink in The Carbon MarketDocument5 paginiCarob-Tree As CO2 Sink in The Carbon MarketFayssal KartobiÎncă nu există evaluări
- DP 2 Human IngenuityDocument8 paginiDP 2 Human Ingenuityamacodoudiouf02Încă nu există evaluări
- PM CH 14Document24 paginiPM CH 14phani chowdaryÎncă nu există evaluări
- Report Card Grade 1 2Document3 paginiReport Card Grade 1 2Mely DelacruzÎncă nu există evaluări
- GT-N7100-Full Schematic PDFDocument67 paginiGT-N7100-Full Schematic PDFprncha86% (7)
- Evaluation TemplateDocument3 paginiEvaluation Templateapi-308795752Încă nu există evaluări
- SMR 13 Math 201 SyllabusDocument2 paginiSMR 13 Math 201 SyllabusFurkan ErisÎncă nu există evaluări
- Bana LingaDocument9 paginiBana LingaNimai Pandita Raja DasaÎncă nu există evaluări
- Dtu Placement BrouchureDocument25 paginiDtu Placement BrouchureAbhishek KumarÎncă nu există evaluări
- Unit 16 - Monitoring, Review and Audit by Allan WatsonDocument29 paginiUnit 16 - Monitoring, Review and Audit by Allan WatsonLuqman OsmanÎncă nu există evaluări
- History of The Sikhs by Major Henry Cour PDFDocument338 paginiHistory of The Sikhs by Major Henry Cour PDFDr. Kamalroop SinghÎncă nu există evaluări
- Read While Being Blind.. Braille's Alphabet: Be Aware and Active !Document3 paginiRead While Being Blind.. Braille's Alphabet: Be Aware and Active !bitermanÎncă nu există evaluări
- Emea 119948060Document31 paginiEmea 119948060ASHUTOSH MISHRAÎncă nu există evaluări
- Vendor Information Sheet - LFPR-F-002b Rev. 04Document6 paginiVendor Information Sheet - LFPR-F-002b Rev. 04Chelsea EsparagozaÎncă nu există evaluări
- Organizational ConflictDocument22 paginiOrganizational ConflictTannya AlexandraÎncă nu există evaluări
- 13 Adsorption of Congo Red A Basic Dye by ZnFe-CO3Document10 pagini13 Adsorption of Congo Red A Basic Dye by ZnFe-CO3Jorellie PetalverÎncă nu există evaluări
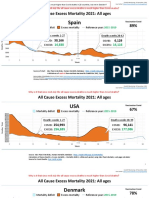
- Countries EXCESS DEATHS All Ages - 15nov2021Document21 paginiCountries EXCESS DEATHS All Ages - 15nov2021robaksÎncă nu există evaluări
- Appendix - Pcmc2Document8 paginiAppendix - Pcmc2Siva PÎncă nu există evaluări
- Psychological Contract Rousseau PDFDocument9 paginiPsychological Contract Rousseau PDFSandy KhanÎncă nu există evaluări