Documente Academic
Documente Profesional
Documente Cultură
Abdominal Aortic Aneurysm
Încărcat de
Aria MontgomeryDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Abdominal Aortic Aneurysm
Încărcat de
Aria MontgomeryDrepturi de autor:
Formate disponibile
Abdominal aortic aneurysm An abdominal aortic aneurysm is a weakened and bulging area in the lower part of the aorta,
the major blood vessel that supplies blood to the body. The aorta, about the thickness of a garden hose, runs from your heart through the center of your chest and abdomen. Because the aorta is the body's main supplier of blood, a ruptured abdominal aortic aneurysm can cause life-threatening bleeding. Although you may never have symptoms, finding out you have an abdominal aortic aneurysm can be frightening. Most small and slow-growing abdominal aortic aneurysms don't rupture, but large, fast-growing abdominal aortic aneurysms may. Depending on the size and rate at which the aortic aneurysm is growing, treatment may vary from watchful waiting to emergency surgery. Once an abdominal aortic aneurysm is found, doctors will closely monitor it so that surgery can be planned if it's necessary. Emergency surgery for a ruptured abdominal aneurysm can be risky. Anatomy The abdominal aorta maintains 3 distinct tissue layers, an intima, media, and adventitia. The intima is composed of the classic endothelial layer. The media contains vascular smooth muscle and matrix proteins, elastin, and collagen. The diameter of the aorta decreases in size from its thoracic portion to the abdominal and infrarenal portions. A normal aorta shows a reduction in medial elastin layers from the thoracic area to the abdominal portion. Elastin and collagen content are also reduced. Aneurysms represent a dilatation in all layers of the vessel wall. The shape of the aneurysm can be described as saccular or fusiform, although this description represents a continuum. Aneurysm diameter is an important risk factor for rupture. The important surgical and endovascular anatomic considerations include associated renal and visceral artery involvement (either occlusive disease or involved in the aneurysm process) and the iliac artery (either occlusive disease or aneurysms). The length of the infrarenal aortic neck is important in helping determine the surgical approach (retroperitoneal vs transabdominal) and the location of the aortic cross clamp. Hypogastric artery (internal iliac) outflow is important in planning surgical repair. Loss of blood flow from the hypogastric artery may result in impotence in males and sigmoid colon ischemia with necrosis. Inflammatory aneurysms represent a subsegment of AAA and are characterized by a thick inflammatory peal. These aneurysms are associated with retroperitoneal fibrosis and adhesion of the duodenum and fibrosis (see the image below). What is an aneurysm? An aneurysm is an area of a localized widening (dilation) of a blood vessel. (The word "aneurysm" is borrowed from the Greek "aneurysma" meaning "a widening"). Symptoms Abdominal aortic aneurysms often grow slowly and usually without symptoms, making them difficult to detect. Some aneurysms will never rupture. Many start small and stay small, although many expand over time. Some aortic aneurysms enlarge slowly, increasing less than half an inch (1.2 centimeters) a year. Others expand at a faster rate, which increases the risk of rupture. How quickly an aortic aneurysm may enlarge is difficult to predict. As an aortic aneurysm enlarges, some people may notice: A pulsating feeling near the navel Tenderness or pain in the abdomen or chest Back pain
What is an aneurysm? An aneurysm is an area of a localized widening (dilation) of a blood vessel. (The word "aneurysm" is borrowed from the Greek "aneurysma" meaning "a widening"). What are the thoracic and abdominal aorta? The aorta is first called the thoracic aorta as it leaves the heart, ascends, arches, and descends through the chest until it reaches the diaphragm (the partition between the thorax and abdomen). The aorta is then called the abdominal aorta after it has passed the diaphragm and continues down the abdomen. The abdominal aorta ends where it splits to form the two iliac arteries that go to the legs. Where do aortic aneurysms tend to develop? Aortic aneurysms can develop anywhere along the length of the aorta. The majority, however, are located along the abdominal aorta. Most (about 90%) of abdominal aneurysms are located below the level of the renal arteries, the vessels that leave the aorta to go to the kidneys. About two-thirds of abdominal aneurysms are not limited to just the aorta but extend from the aorta into one or both of the iliac arteries. What shape are most aortic aneurysms? Most aortic aneurysms are fusiform. They are shaped like a spindle ("fusus" means spindle in Latin) with widening all around the circumference of the aorta. (Saccular aneurysms just involve a portion of the aortic wall with a localized out pocketing). Who is most likely to have an abdominal aortic aneurysm? Aortic aneurysms are most common after 60 years of age. Males are five times more likely than females to be affected. Approximately 5% of men over age 60 develop an abdominal aortic aneurysm. What are risk factors for aortic aneurysms? Risk factors for aortic aneurysm include: y Cigarette smoking: cigarette smoking not only increases the risk of developing an abdominal aortic aneurysm, the chance of aneurysm rupture (a life-threatening complication of abdominal aneurysm) is also more common among active smokers. High blood pressure High serum cholesterol Diabetes mellitus
y y y
What is the most common cause of aortic aneurysms? The most common cause of aortic aneurysms is "hardening of the arteries" calledarteriosclerosis. At least 80% of aortic aneurysms are from arteriosclerosis. The arteriosclerosis can weaken the aortic wall and the pressure of the blood being pumped through the aorta causes expansion at the site of weakness. What are other causes of aortic aneurysms? Other causes of aortic aneurysms include: y Genetic/hereditary: There is a familial tendency to developing abdominal aortic aneurysms. Individuals with first-degree relatives having abdominal aortic aneurysms have a higher risk of developing abdominal aortic aneurysm than the general population. They also tend to develop the aneurysms at younger ages and have a higher tendency to suffer aneurysm rupture than individuals without family history.
y y y
y y
Genetic disease: There are also rare inheritable genetic diseases of connective tissue (tissue that make up the wall of the aorta) such asEhlers-Danlos syndrome and Marfan's syndrome that can lead to the development of aortic aneurysms. Post-trauma: After physical trauma to the aorta. Arteritis: Inflammation of blood vessels as occurs in Takayasu disease, giant cell arteritis, and relapsing polychondritis. Mycotic (fungal) infection: A mycotic infection that may be associated with immunodeficiency, IV drug abuse, syphilis, and heart valve surgery.
abdomen. Not all aneurysms can be fixed in this manner and there may not be a long-term benefit to this type of surgery. Though the post-operative course is shorter, there is a need for closer follow-up and testing. What is the medical management (non-surgical management) of abdominal aortic aneurysm? For patients who are not surgical candidates (for example for patients with aneurysm smaller than 5 cm); medical treatment to prevent aneurysm expansion and rupture include: y Stopping cigarette smoking y Controlling high blood pressure y Lowering high blood cholesterol y Some doctors may consider medications called beta blockers, like propanolol(Inderal), atenolol (Tenormin), ormetoprolol (Lopressor, Toprol XL), which block adrenaline receptors and lower pressure within the blood vessel. y Close monitoring of the aneurysm size with ultrasound or CT scan every 6 to 12 months (sooner in high risk patients) Abdominal Aortic Aneurysm At A Glance y y y y y y An aneurysm is an abnormal area of localized widening of a blood vessel. The aorta bulges at the site of an aneurysm like a weak spot on a worn tire. Aortic aneurysms are typically spindle-shaped and involve the aorta below the arteries to the kidneys. Five percent of men over 60 develop an abdominal aortic aneurysms. The most common cause of an aneurysm is arteriosclerosis. Abdominal aortic aneurysms often do not cause symptoms. If they do, they may cause deep boring pain in the lower back or abnormally prominent abdominal pulsation. X-rays of the abdomen and other radiologic tests can be used in diagnosing an aneurysm. Rupture of an aortic aneurysm is a catastrophe. Repair of the aneurysm can be done by surgery or endovascular stenting.
What tests help in the diagnosis of an abdominal aortic aneurysm? In about 90% of the cases, X-rays of the abdomen show calcium deposits in the aneurysm wall. But plain x-rays of the abdomen cannot determine the size and the extent of the aneurysm. Ultrasonography usually gives a clear picture of the size of an aneurysm. Ultrasound has about 98% accuracy in measuring the size of the aneurysm, and is safe and noninvasive. But ultrasound cannot accurately define the extent of the aneurysm and is inadequate for surgical repair planning. Computerized tomography of the abdomen, is highly accurate in determining the size and extent of the aneurysm, and its relation to the renal arteries. However, computerized tomography uses high doses of radiation and for evaluation of blood vessels, requires intravenous dye. This carries some risk including allergic reaction to the dye and irritation of the kidneys. In patients with kidney diseases, the doctor may consider anMRA (magnetic resonance angiography), which is a study of the aorta and the other arteries using MRI scanning. Both computerized tomography and magnetic resonance imaging are effective for diagnosis. An aortogram, where dye is directly injected into the aorta to assess its anatomy, historically was the diagnostic test of choice. Presently, it's indications may be limited to use when surgery or stenting is considered. What are the complications with an abdominal aortic aneurysm? Rupture is a feared problem. Rupture of an abdominal aneurysm is a catastrophe. It is highly lethal and is usually preceded by excruciating pain in the lower abdomen and back, with tenderness of the aneurysm. Rupture of an abdominal aneurysm causes profuse bleeding and leads to shock. Death may rapidly follow. Half of all persons with untreated abdominal aortic aneurysms die of rupture within five years. Abdominal aortic aneurysms are the 13th leading cause of death in the U.S. Peripheral embolization of clot within the aneurysm can occur when a piece of clot comes loose and travels further out in the arterial system. This clot fragment can lodge in a smaller artery and block the flow of blood. Infection of aneurysms can occur from turbulent blood flow from the rough inner surface of the affected aorta. How are abdominal aortic aneurysms repaired? The goal of surgical treatment of abdominal aortic aneurysm is to prevent aneurysm rupture. Traditionally, repair of aortic aneurysms has been surgical. The operation consists of opening the abdomen, finding the aorta and removing (excising) the aneurysm. A synthetic Dacron tube that replaces the removed piece of aorta is sewn into place. A less invasive procedure for aortic aneurysm is endovascular surgery. This minimally invasive procedure that allows the grafts (stent) to be guided within the blood vessel itself to the site of the aneurysm without the need to cut open the
y y y
S-ar putea să vă placă și
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsDe la EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsÎncă nu există evaluări
- Aneurysm PDFDocument20 paginiAneurysm PDFKV100% (1)
- Disseminated Intravascular Coagulation, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandDisseminated Intravascular Coagulation, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- TOF Patient EducationDocument8 paginiTOF Patient EducationMia MiaÎncă nu există evaluări
- Ebstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandEbstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- Congenital Heart DiseaseDocument124 paginiCongenital Heart DiseasemulkanmustafaÎncă nu există evaluări
- Management of Infective EndocarditisDocument14 paginiManagement of Infective Endocarditismhafzam2020Încă nu există evaluări
- Angina PectorisDocument17 paginiAngina PectorisRacel HernandezÎncă nu există evaluări
- Name: Patient X Age: 14 Y/oDocument4 paginiName: Patient X Age: 14 Y/oRyan Jay Patacsil100% (1)
- Ventricular Septal DefectsDocument7 paginiVentricular Septal DefectsMuhammadAldoGiansyahÎncă nu există evaluări
- Acute and Chronic Pancreatitis ShirleyDocument6 paginiAcute and Chronic Pancreatitis ShirleyVictor AladejanaÎncă nu există evaluări
- Pulmonary Function TestsDocument2 paginiPulmonary Function TestsSafuan Sudin100% (1)
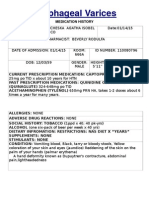
- Esophageal Varices: Medication HistoryDocument4 paginiEsophageal Varices: Medication HistoryNeil Patrick PasuquinÎncă nu există evaluări
- Cardiac TamponadeDocument10 paginiCardiac TamponadeRahmi Fatma SariÎncă nu există evaluări
- Welcome To The Case Study Presentation:-: Prostate CancerDocument22 paginiWelcome To The Case Study Presentation:-: Prostate CancerDengo ChapatieeÎncă nu există evaluări
- Congestive Heart Failure: Dr. J. SaravananDocument31 paginiCongestive Heart Failure: Dr. J. Saravananpetervazhayil100% (1)
- Right Sided Heart FailureDocument33 paginiRight Sided Heart FailurePaulÎncă nu există evaluări
- Anatomy and PhysiologyDocument3 paginiAnatomy and PhysiologyKobe ManuelÎncă nu există evaluări
- Acute Renal Failure: Dr. Bobi Ahmad S, S.KPDocument62 paginiAcute Renal Failure: Dr. Bobi Ahmad S, S.KPdr.Bobi Ahmad Sahid, S.KepÎncă nu există evaluări
- Nstemi: How To Risk Stratify?Document32 paginiNstemi: How To Risk Stratify?dhannibernadetÎncă nu există evaluări
- Pulmonary EdemaDocument14 paginiPulmonary EdemaRizzamwah Catague100% (1)
- Tracheostomy Care: PhysiologyDocument2 paginiTracheostomy Care: PhysiologyrajirajeshÎncă nu există evaluări
- 403 Full PDFDocument10 pagini403 Full PDFKuroto YoshikiÎncă nu există evaluări
- Heart FailureDocument4 paginiHeart FailureDane WrightÎncă nu există evaluări
- Complete Guide To ECGDocument78 paginiComplete Guide To ECGAnas YahyaÎncă nu există evaluări
- Generic Name Therapeutic Classification Pharmacologic ClassificationDocument3 paginiGeneric Name Therapeutic Classification Pharmacologic ClassificationAnselle CasilÎncă nu există evaluări
- Nursing Care PlanDocument19 paginiNursing Care PlanChic Dian UsmanÎncă nu există evaluări
- Angina PectorisDocument33 paginiAngina PectorisRosse Del MundoÎncă nu există evaluări
- Basilar Skull FractureDocument16 paginiBasilar Skull FractureRindahMDÎncă nu există evaluări
- Cardiac ArrestDocument54 paginiCardiac ArrestIdha FitriyaniÎncă nu există evaluări
- Deep Vein ThrombosisDocument9 paginiDeep Vein ThrombosisGladys YaresÎncă nu există evaluări
- Rheumatic Heart DiseaseDocument13 paginiRheumatic Heart Diseasedy15Încă nu există evaluări
- Jade R. Dinolan BSN-4: Diagnosi SDocument5 paginiJade R. Dinolan BSN-4: Diagnosi SJhade Relleta100% (1)
- Abdominal Aortic AneurysmDocument37 paginiAbdominal Aortic Aneurysmannu300Încă nu există evaluări
- Chest TraumaDocument14 paginiChest TraumaMary Rose BatagaÎncă nu există evaluări
- Cardiac Tamponade and ManagementDocument42 paginiCardiac Tamponade and Managementأم حمدÎncă nu există evaluări
- Nursing Management: Nursing Management: Acute Kidney Injury and Chronic Kidney DiseaseDocument22 paginiNursing Management: Nursing Management: Acute Kidney Injury and Chronic Kidney Diseasedian rachmat saputroÎncă nu există evaluări
- Aortic RegurgitationDocument19 paginiAortic RegurgitationsunilgenextÎncă nu există evaluări
- How Stroke Affects Speech and LanguageDocument5 paginiHow Stroke Affects Speech and Languagemino songÎncă nu există evaluări
- Non-St Segment Elevation Myocardial Infarction (Nstemi)Document24 paginiNon-St Segment Elevation Myocardial Infarction (Nstemi)MHIEMHOIÎncă nu există evaluări
- Heart FailureDocument10 paginiHeart Failureurmila prajapatiÎncă nu există evaluări
- Atrial Septal DefectDocument12 paginiAtrial Septal DefectNurruhaizi Aizi100% (1)
- Esophageal Varices Week 4 T2T3Document37 paginiEsophageal Varices Week 4 T2T3liewhuilianÎncă nu există evaluări
- 19 Cardiac DisordersDocument51 pagini19 Cardiac DisordersChessie Garcia100% (1)
- Nursing Case Presentation For A Patient With CABG: Subject: Medical Surgical Nursing-IIDocument10 paginiNursing Case Presentation For A Patient With CABG: Subject: Medical Surgical Nursing-IIanamika sharmaÎncă nu există evaluări
- Cardiac MonitorDocument5 paginiCardiac MonitorhumbertolgeÎncă nu există evaluări
- Myocardial InfractionDocument16 paginiMyocardial InfractionYAMINIPRIYANÎncă nu există evaluări
- Chronic Kidney Disease OverviewDocument15 paginiChronic Kidney Disease Overviewjames100% (1)
- UGIBDocument5 paginiUGIBdwyane0033100% (1)
- Myocardial InfarctionDocument2 paginiMyocardial InfarctionnkosisiphileÎncă nu există evaluări
- OsteomalaciaDocument6 paginiOsteomalaciaapi-3801039Încă nu există evaluări
- Pulmonaryembolism 150329161109 Conversion Gate01Document60 paginiPulmonaryembolism 150329161109 Conversion Gate01Rafika RaraÎncă nu există evaluări
- Care of Patient With TPM Slide PresentationDocument16 paginiCare of Patient With TPM Slide PresentationirzehronÎncă nu există evaluări
- Men in NursingDocument2 paginiMen in NursingMark JosephÎncă nu există evaluări
- Compartment SyndromeDocument3 paginiCompartment SyndromeTantyo Adi P100% (2)
- Heart FailureDocument43 paginiHeart FailuresimonjosanÎncă nu există evaluări
- Coronary Artery DiseaseDocument3 paginiCoronary Artery Diseasetrew_wertÎncă nu există evaluări
- Case StudyDocument6 paginiCase StudyApoorv Jain100% (1)
- Heart TransplantationDocument10 paginiHeart TransplantationNajmi Leila SepyanisaÎncă nu există evaluări
- Cardiomyopathy My LectureDocument33 paginiCardiomyopathy My LectureAbraha HailuÎncă nu există evaluări
- 7 200320 HWCDocument56 pagini7 200320 HWCParmar JigneshÎncă nu există evaluări
- Health Benefits of Bicycle RidingDocument3 paginiHealth Benefits of Bicycle RidingPeter JohnsonÎncă nu există evaluări
- Vanjaarsveld MelodyM 1111992 PatientReportDocument2 paginiVanjaarsveld MelodyM 1111992 PatientReportmelodyvanjaasveldÎncă nu există evaluări
- Insulin, Regular (Humulin R)Document1 paginăInsulin, Regular (Humulin R)EÎncă nu există evaluări
- ExamView - Chapter - 33 PDFDocument8 paginiExamView - Chapter - 33 PDFChizua OkoyeÎncă nu există evaluări
- NCPDocument7 paginiNCPJo Chiko FlorendoÎncă nu există evaluări
- Methylene Blue For Refractory Shock in Pediatric PatientsDocument16 paginiMethylene Blue For Refractory Shock in Pediatric Patientsandi rahmatÎncă nu există evaluări
- Kertas Kerja Program Sayangkan KitaDocument5 paginiKertas Kerja Program Sayangkan Kitaaknb2702Încă nu există evaluări
- HSV1 HSV2 R-Gene & VZV R-GeneDocument2 paginiHSV1 HSV2 R-Gene & VZV R-GeneSachinÎncă nu există evaluări
- Musculoskeletal System (20000 Series) : A) 20205 B) 20206 C) 20225 D) 27324Document8 paginiMusculoskeletal System (20000 Series) : A) 20205 B) 20206 C) 20225 D) 27324JJKÎncă nu există evaluări
- Analise Dinamica Sorriso - Mudanças Com A IdadeDocument2 paginiAnalise Dinamica Sorriso - Mudanças Com A IdadeCatia Sofia A PÎncă nu există evaluări
- Hallux Valgus PDFDocument26 paginiHallux Valgus PDFDeny EvanderÎncă nu există evaluări
- Depression in Older AdultsDocument9 paginiDepression in Older Adultsapi-509881562Încă nu există evaluări
- Universal PrecutionsDocument30 paginiUniversal PrecutionsShirmi BamunusingheÎncă nu există evaluări
- Understanding The Different Routes of Drug AdministrationDocument3 paginiUnderstanding The Different Routes of Drug AdministrationMark Russel Sean LealÎncă nu există evaluări
- First AID For The USMLE Public HealthDocument20 paginiFirst AID For The USMLE Public HealthLilit M-yanÎncă nu există evaluări
- The Human Eye PowerPointDocument69 paginiThe Human Eye PowerPointKemoy Francis100% (1)
- Nodular Goiter Concept MapDocument5 paginiNodular Goiter Concept MapAllene PaderangaÎncă nu există evaluări
- Neonatal InfectionDocument9 paginiNeonatal InfectionnishaÎncă nu există evaluări
- Clinical Genetics: General Aspects and Laboratory DiagnosticsDocument14 paginiClinical Genetics: General Aspects and Laboratory DiagnosticsKinga-Borbála GagyiÎncă nu există evaluări
- (B-0270) Day Surgery Procedure UnitDocument22 pagini(B-0270) Day Surgery Procedure UnitAhmad Gamal Elden MAhanyÎncă nu există evaluări
- Faculty List2019Document6 paginiFaculty List2019suyashsahu2505Încă nu există evaluări
- VermiphobiaDocument2 paginiVermiphobiaKenPedresoÎncă nu există evaluări
- A. Knowledge-WPS OfficeDocument9 paginiA. Knowledge-WPS Officeannabelle castanedaÎncă nu există evaluări
- Diabetes and The Nutrition and Diets For Its PreveDocument16 paginiDiabetes and The Nutrition and Diets For Its PreveRam MÎncă nu există evaluări
- Bayabas: Instructions For GuavaDocument2 paginiBayabas: Instructions For GuavadorothypearlÎncă nu există evaluări
- Aloe Vera DoajDocument8 paginiAloe Vera DoajNur AiniÎncă nu există evaluări
- Pulpotomy Pediatric Prevention Diagnosis Treatment PlanningDocument122 paginiPulpotomy Pediatric Prevention Diagnosis Treatment PlanningTamara Nitya ArianiÎncă nu există evaluări
- Sedatives, Hypnotics & Anxiolytics (Antianxiety Drugs) Ms. S.R.DhandeDocument347 paginiSedatives, Hypnotics & Anxiolytics (Antianxiety Drugs) Ms. S.R.DhandeEsha pantÎncă nu există evaluări
- Management of Anembryonic Pregnancy Loss: An Observational StudyDocument6 paginiManagement of Anembryonic Pregnancy Loss: An Observational StudyAnonymous ORleRrÎncă nu există evaluări
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (32)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDe la EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDEvaluare: 5 din 5 stele5/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedEvaluare: 4.5 din 5 stele4.5/5 (82)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)De la EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Evaluare: 3 din 5 stele3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDe la EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionEvaluare: 4 din 5 stele4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe la EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsÎncă nu există evaluări
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe la EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaEvaluare: 4.5 din 5 stele4.5/5 (266)
- To Explain the World: The Discovery of Modern ScienceDe la EverandTo Explain the World: The Discovery of Modern ScienceEvaluare: 3.5 din 5 stele3.5/5 (51)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeEvaluare: 2 din 5 stele2/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe la EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsEvaluare: 4 din 5 stele4/5 (4)
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeDe la EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeEvaluare: 4.5 din 5 stele4.5/5 (2)
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 4 din 5 stele4/5 (6)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe la EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisEvaluare: 4.5 din 5 stele4.5/5 (44)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.De la EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Evaluare: 4.5 din 5 stele4.5/5 (110)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesDe la EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesEvaluare: 4.5 din 5 stele4.5/5 (1412)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDe la EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsEvaluare: 5 din 5 stele5/5 (1)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsDe la EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsEvaluare: 4.5 din 5 stele4.5/5 (39)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDe la EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeEvaluare: 4.5 din 5 stele4.5/5 (254)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDe la EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsEvaluare: 4.5 din 5 stele4.5/5 (170)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDe la EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryEvaluare: 4 din 5 stele4/5 (46)
- The Marshmallow Test: Mastering Self-ControlDe la EverandThe Marshmallow Test: Mastering Self-ControlEvaluare: 4.5 din 5 stele4.5/5 (60)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsDe la EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsÎncă nu există evaluări
- Hearts of Darkness: Serial Killers, The Behavioral Science Unit, and My Life as a Woman in the FBIDe la EverandHearts of Darkness: Serial Killers, The Behavioral Science Unit, and My Life as a Woman in the FBIEvaluare: 4 din 5 stele4/5 (20)