Documente Academic
Documente Profesional
Documente Cultură
Ip
Încărcat de
Mohd Ashaf Amat Khainan0 evaluări0% au considerat acest document util (0 voturi)
36 vizualizări7 paginiP ox1:i nxirx1rNsioN is the hemodynamic abnormality associated with the most severe complications of cirrhosis. Variceal bleeding is a medical emergency associated with significant morbidity and mortality. The main fields of discussion of the workshop were definitions, methodology and therapeutic strategies in portal hypertension.
Descriere originală:
Titlu original
ip
Drepturi de autor
© Attribution Non-Commercial (BY-NC)
Formate disponibile
PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentP ox1:i nxirx1rNsioN is the hemodynamic abnormality associated with the most severe complications of cirrhosis. Variceal bleeding is a medical emergency associated with significant morbidity and mortality. The main fields of discussion of the workshop were definitions, methodology and therapeutic strategies in portal hypertension.
Drepturi de autor:
Attribution Non-Commercial (BY-NC)
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
36 vizualizări7 paginiIp
Încărcat de
Mohd Ashaf Amat KhainanP ox1:i nxirx1rNsioN is the hemodynamic abnormality associated with the most severe complications of cirrhosis. Variceal bleeding is a medical emergency associated with significant morbidity and mortality. The main fields of discussion of the workshop were definitions, methodology and therapeutic strategies in portal hypertension.
Drepturi de autor:
Attribution Non-Commercial (BY-NC)
Formate disponibile
Descărcați ca PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 7
Journal of Hepatology 2000; 33: 846852 Copyright C European Association
for the Study of the Liver 2000
Printed in Denmark All rights reserved
Munksgaard Copenhagen
Journal of Hepatology
ISSN 0168-8278
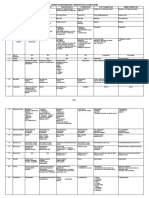
Updating Consensus in Portal Hypertension: Report of the Baveno III
Consensus Workshop on denitions, methodology and therapeutic
strategies in portal hypertension
Roberto de Franchis
Gastroenterology and Gastrointestinal Endoscopy Service, Department of Internal Medicine, University of Milan, and IRCCS Ospedale Maggiore
Policlinico, Milan, Italy
P
o1:i nxir1rNsioN is the hemodynamic abnor-
mality associated with the most severe compli-
cations of cirrhosis, including ascites, hepatic encephal-
opathy and bleeding from gastroesophageal varices.
Since variceal bleeding is a medical emergency associ-
ated with signicant morbidity and mortality, the evalu-
ation of diagnostic tools and the design and conduct of
good clinical trials for the treatment of this condition
have always been difcult. Awareness of these difculties
has led to the organization of a series of meetings aimed
at reaching consensus on the denitions of some key
events related to portal hypertension and variceal
bleeding, and at producing guidelines for the conduct of
trials in this eld. Such meetings took place in Groning-
en, the Netherlands in 1986 (1), in Baveno, Italy in 1990
(Baveno I) (2) and in 1995 (Baveno II) (3,4), in Milan,
Italy in 1992 (5), and in Reston, USA (6), in 1996. All
these meetings were successful and produced consensus
statements on some important points, although several
issues remained unsettled.
To continue the work of the previous meetings, a
Baveno III workshop was held on 1314 April, 2000.
The workshop was attended by many of the experts
responsible for most of the major achievements of re-
cent years in this eld. The majority of them had at-
tended the Groningen, Baveno I, Baveno II and Reston
meetings as well.
The main elds of discussion of the Baveno III
workshop were the same as in Baveno I and II, i.e.
the denitions of key events concerning the bleeding
episode, the diagnostic evaluation of patients, the
Correspondence: Roberto de Franchis, Gastroenterology
and Gastrointestinal Endoscopy Service, Department of
Internal Medicine, University of Milan, and IRCCS Os-
pedale Maggiore Policlinico, Milan, Via Pace 9, 20122 Mi-
lan, Italy. Tel: 39 02 5503 5331/2. Fax: 39 02 5501 5818.
e-mail: gastro/polic.cilea.it
846
therapeutic options in patients with portal hyperten-
sion, and the methodological requirements for future
trials in this eld. For each of these topics, a series of
consensus statements were discussed and agreed upon.
These statements are reported in extenso in the Baveno
III proceedings (7). A summary of the most important
conclusions reached at the workshop is reported here.
Denition of Key Events Regarding the
Bleeding Episode
Active bleeding
Active bleeding at endoscopy (dened as blood ema-
nating from a varix) has prognostic value as a predictor
of failure to control bleeding in the next few days. Fu-
ture studies should ascertain whether the clinical or
prognostic signicance of active bleeding is the same
with or without drug therapy, and whether active
bleeding is related to mortality.
Failure to control bleeding
At Baveno II (3,4), the denition of failure to control
bleeding was divided into 2 time frames:
1) Within 6 h: any of the following factors: a) trans-
fusion of 4 units of blood or more, and inability to
achieve an increase in systolic blood pressure of 20
mmHg or to 70 mmHg or more, and/or b) pulse
reduction to less than 100/min or a reduction of 20/
min from baseline pulse rate.
2) After 6 h: any of the following factors: a) the occur-
rence of hematemesis, b) reduction in blood press-
ure of more than 20 mmHg from the 6-h point, and/
or c) increase of pulse rate of more than 20/min
from the 6-h point on 2 consecutive readings 1 h
apart, d) transfusion of 2 units of blood or more
(over and above the previous transfusions) required
to increase the Hct to above 27% or Hb to above 9
g/dl.
Updating consensus in portal hypertension
These denitions were conrmed at Reston (6). At
Baveno III it was felt that some of the above criteria
could be misleading. There was consensus that the Ba-
veno II (3,4) and Reston (6) criteria should be re-evalu-
ated, in particular the use of hemodynamic criteria
without evidence of clinical bleeding.
Failure of secondary prevention
Failure to prevent rebleeding was dened as a single
episode of clinically signicant rebleeding from portal
hypertensive sources, according to the Baveno II (3,4)
criteria: [transfusion requirement of 2 units of blood
or more within 24 h of time zero the time of admis-
sion of a patient to the rst hospital he is taken to
(2), together with a systolic blood pressure 100
mmHg or a postural change of 20 mmHg and/or
pulse rate 100/min at time zero].
New information to be obtained in future studies
More information is needed on the relationship of in-
fection to failure to control bleeding and mortality. Tri-
als of salvage therapy following failure to prevent early
rebleeding should be performed.
Diagnosis of Portal Hypertension
Denition of clinically signicant portal hypertension
(CSPH)
An increase in portal pressure gradient to a threshold
above approximately 10 mm Hg. The presence of var-
ices, variceal hemorrhage and/or ascites is indicative of
the presence of CSPH.
Diagnostic tools to assess portal hypertension
The reliability of both the hepatic vein pressure gradi-
ent (HVPG) measurement and endoscopic assessment
of esophageal varices for the diagnosis of CSPH is sat-
isfactory. However, specic, simple guidelines might
further improve reliability. The accuracy of non-invas-
ive tests such as Doppler ultrasound and variceal press-
ure measurement for the diagnosis of CSPH should be
further assessed before their use can be recommended
in clinical practice.
Screening for the presence of CSPH and follow-up
a) All cirrhotic patients should be screened for the
presence of varices at the time of the initial diagnosis
of cirrhosis.
b) In compensated patients without varices, endo-
scopy should be repeated at 23-year intervals to evalu-
ate the development of varices
c) In compensated patients with small varices, endo-
scopy should be repeated at 12-year intervals to evalu-
ate progression of varices.
847
d) There is no indication for subsequent evaluations
once large varices are detected.
The suggested intervals for follow-up endoscopy were
prolonged in comparison to those agreed upon at Bav-
eno II (3,4) and Reston (5), as dictated by the current evi-
dence in the literature. However, the available infor-
mation on this matter is scanty. Further studies of the
natural course of cirrhosis should better clarify the inci-
dence of esophago-gastric varices and the progression of
variceal size fromsmall to large, in order to better dene
the interval between endoscopic evaluations.
Treatment monitoring
HVPG is the only parameter presently suitable to
monitor pharmacological treatment. Variceal pressure
measurement and Doppler-ultrasound seem promising
but, due to inter-equipment and inter-observer vari-
ability, their use in clinical practice cannot be rec-
ommended. The efcacy of treatment adjustments
based on monitoring should be further investigated.
Diagnosis of portal hypertensive gastropathy (PHG)
and gastric antral vascular ectasia (GAVE)
1) Based on current data of natural history (8), PHG
should be classied as:
a) Mild: when mosaic-like pattern (MLP) of mild
degree (without redness of the areola) is present;
b) Severe: when the MLP is superimposed by red
signs or if any other red sign is present.
The lesions may change over time (uctuate, worsen
or improve).
2) GAVE is a distinct clinical, endoscopic and histo-
pathologic entity endoscopically characterized by
aggregates of red spots arranged in linear pattern
or diffused lesion, if conrmed by biopsy, in the an-
trum of the stomach. GAVE can be seen in con-
ditions other than portal hypertension.
Diagnosis of gastric varices
The classication of Sarin et al. (9) should be used. In
addition, for fundal varices, the presence of red signs,
large size and Child class B or C should be considered
as risk factors for bleeding.
Fundal gastric varices (GOV2 and IGV1) are at the
highest risk of bleeding.
Therapeutic Options in Patients with Portal
Hypertension
Pre-primary prophylaxis (prevention of the formation/
growth of varices)
Every patient with cirrhosis without complications of
portal hypertension ideally needs HVPG measure-
ments in order to be included in a trial of pre-primary
R. de Franchis
prevention. The sequence portal hypertensioncol-
lateralsvarices is an accepted one; collaterals can be
diagnosed before the development of varices.
Portal pressure is predictive of varices formation,
while the clinical importance of collaterals as predic-
tors of more severe portal hypertensive complications
should be further investigated.
Low risk varices are small-sized varices without
red color signs. The risk of bleeding within 2 years of
these varices is 10%. The risk of bleeding between
two consecutive endoscopies performed at yearly inter-
vals in patients with cirrhosis undergoing surveillance
for low-risk varices is 5%. The reproducibility of a
diagnosis of low-risk varices by endoscopy is variable
and inuenced by expertise. Spontaneous regression of
small varices is a rare event. Regression is related to
improvement in liver status, particularly after alcohol
abstinence in alcoholic cirrhosis.
More data are needed before a conclusion can be
drawn on the usefulness of starting prophylaxis of vari-
ceal bleeding in patients with low-risk varices.
Prevention of the rst bleeding episode
The conclusions reached at Baveno II (3,4) and Reston
(5) (i. e. that beta-blockers are the rst-line treatment
for preventing the rst bleeding episode, that endo-
scopic sclerotherapy is not indicated, and that endo-
scopic band ligation as an alternative to beta-blockers
in this clinical setting should be further investigated)
were not challenged. The attention of the experts fo-
cused on the following points:
Monitoring beta-blockade. Increasing the dose of beta-
blockers to achieve a 25% reduction in resting heart
rate or down to 55 b.p.m. or development of symptoms
are the most commonly used approaches for adjusting
the dose of beta-blockers in cirrhotic patients. Some,
but not all, patients treated with beta-blockers achiev-
ing these targets will be protected from variceal
bleeding. However, there is no relationship between re-
duction in portal pressure or protection from variceal
bleeding and the degree of beta-blockade, as assessed
by the reduction in resting heart rate.
A reduction in HVPG below 12 mmHg or more
than 20% from baseline is the only tested parameter
to detect those patients treated with beta-blockers who
are protected from variceal bleeding. However, since
about 60% of patients treated with beta-blockers who
do not achieve these targets will not bleed (for 2 years)
(10), in primary prophylaxis it is not mandatory to
check the HVPG response.
Treatment of patients with contra-indications or intol-
erance to beta-blockers, or non-compliant. There is no
consensus about howwe should treat patients with large
848
esophageal varices (more than 5 mm in size) who have
contraindications or intolerance to beta-blockers. There
are no published studies specically addressing this
issue. However, preliminary data suggest that isosor-
bide-5-mononitrate may not be a good alternative. Pre-
liminary data with prophylactic endoscopic band lig-
ation are encouraging in high-risk patients, but more
studies are needed in patients with contraindications.
There is no consensus on how to treat non-com-
pliant patients.
Combination of treatments. Available evidence is in-
sufcient to support the use of combination therapy
with beta-blockers and nitro-vasodilators in the pre-
vention of the rst variceal bleed. The combination of
endoscopic treatment and pharmacologic therapy can-
not be recommended at present because there are no
data to support its use.
Indications for treatment and follow-up. Based on
available data, there is no indication to treat patients
with small varices. All patients with large varices
should be treated. Additional endoscopic signs do not
inuence the indication for therapy. There is no need
for follow-up endoscopy in patients on pharmacologic
therapy.
Future studies. Trials of prophylactic band ligation
in high-risk patients with contraindications or intoler-
ance to beta-blockers are encouraged. In the absence
of specic data, randomized controlled trials should be
performed in patients with gastric varices.
Treatment of acute bleeding from esophageal varices
Timing of endoscopy. Endoscopy should be performed
as soon as possible after admission (within 12 h), espe-
cially in patients with clinically signicant bleeding or
in patients with features suggesting cirrhosis. In mild
bleeds, neither causing hemodynamic changes nor re-
quiring blood volume restitution, endoscopy can be
done electively.
Blood volume restitution. Blood volume restitution
should be done cautiously and conservatively, using
packed red cells to maintain the hematocrit between
2530%, and plasma expanders to maintain hemody-
namic stability.
Further data are required on the need for treating
coagulopathy and thrombocytopenia.
Use of antibiotics for preventing bacterial infections/
spontaneous bacterial peritonitis. The presence of infec-
tion should be considered in all patients. Antibiotic
prophylaxis is an integral part of therapy and should
be instituted from admission. Randomized controlled
trials of oral non-absorbable vs. systemic antibiotics
are needed.
Prevention of hepatic encephalopathy. Lactulose
Updating consensus in portal hypertension
should be given by mouth, naso-gastric tube, or enema
to prevent hepatic encephalopathy.
Assessment of prognosis. The Child-Pugh classi-
cation is not sufcient to assess individual risk and
prognosis, and the additional utility of other prognos-
tic indicators should be assessed. The effect of other
chronic diseases, renal failure, bacterial infections,
HCC and active bleeding at endoscopy should be
evaluated. Portal pressure monitoring should be
further investigated.
Use of balloon tamponade. Balloon tamponade
should only be used in massive bleeding as a temporary
bridge until denitive treatment can be instituted.
Pharmacologic treatment. In suspected variceal
bleeding, vasoactive drugs should be started as soon as
possible, before diagnostic endoscopy. Even if there is no
active bleeding at endoscopy, it is recommended to per-
form endoscopic therapy, especially in high-risk pa-
tients. Drug therapy may be maintained for up to 5 days
to prevent early rebleeding. Randomized controlled tri-
als should be done to determine the optimal duration.
Endoscopic treatment. In acute bleeding either lig-
ation or endoscopic sclerotherapy can be used. For
subsequent treatment, endoscopic banding ligation is
replacing injection sclerotherapy as rst-line endo-
scopic treatment for bleeding esophageal varices.
Endoscopic treatments are best used in association
with pharmacological therapy, which preferably should
be started before endoscopy.
Treatment of bleeding from portal hypertensive
gastropathy (PHG)
The incidence of acute PHG bleeding is low (less than
3% at 3 years); for chronic bleeding, it is around 10
15% at 3 years (9).
Treatment of acute bleeding. Vasoactive drugs are an-
ecdotally used with a high success rate (70100%) in un-
controlled studies. Emergency transjugular intrahepatic
porto-systemic shunt (TIPS) or shunt surgery should be
regarded as rescue treatments in failures of vasoactive
drugs for PHG lesions likely to respond to a portal
pressure decrease (excluding GAVE). The utility of Ar-
gon plasma coagulators should be evaluated.
Treatment of chronic bleeding. b-blockers, and if
needed iron, are the rst-choice treatment. Combined
b-blockers and isosorbide-5-mononitrate, as well as
other medical treatments (i.e. long-acting somatostatin
analogues), should be evaluated. Treatment should be
continued indenitely.
Treatment of bleeding gastric varices
The following hypotheses need to be tested by appro-
priate randomized controlled trials:
849
Acrylate glue injection is effective for acute gastric
varices (GV) bleed.
Endoscopic variceal sclerotherapy (EVS) (EtOH,
ethanolamine oleate) is an alternative.
Vasoactive drugs could be used in combination with
other treatments.
Banding needs evaluation.
TIPS and surgery are indicated as rescue therapy.
Prevention of rebleeding from esophageal varices
First-line treatments. Either beta-blockade or band lig-
ation is the rst-line treatment method for prevention
of recurrent variceal hemorrhage. Patients with ad-
vanced liver disease should be evaluated for liver trans-
plantation. Combinations of endoscopic and drug
treatments should be further investigated.
Treatment of patients with contra-indications to beta-
blockers. Band ligation is the preferred treatment to
prevent recurrent variceal hemorrhage in patients who
have a contraindication to beta-blocker therapy or who
have bled while on beta-blockers.
Treatment for patients who fail rst-line therapy. Sur-
gical shunt or TIPS is the recommended treatment for
good-risk patients who fail rst-line treatments (beta-
blockers/banding) for prevention of recurrent bleeding.
TIPS is the recommended treatment for selected high-
risk patients who fail the preferred rst-line treatments
(beta-blockers/banding) for prevention of recurrent
bleeding. These patients should be considered for liver
transplantation.
Future studies. Future trials for secondary prophy-
laxis should include two or more of the following treat-
ment arms: a) Beta-blockersNitrates; b) Band
ligationdrug therapy; c) TIPS; d) Distal spleno-renal
shunt; e) Small diameter shunts; f) Other portal hypo-
tensive drugs Beta-blockers g) Combination of treat-
ments.
Cost and quality of life evaluations should be done
in future trials.
Prevention of rebleeding from gastric varices
The following treatment options need to be tested by
appropriate randomized controlled trials: long-term
glue injection, TIPS, surgical shunt (for good-risk pa-
tients), drug therapy.
Complications of Treatments for Portal
Hypertension
Complications of pharmacological treatments
The following denitions were agreed upon:
Fatigue. Inability to perform regular physical activi-
ties carried out before treatment.
Abdominal cramps. Abdominal pain starting after
R. de Franchis
treatment that persists for more than 4 h after other
major causes of abdominal pain (i.e. bacterial perito-
nitis) have been ruled out.
Severe bradycardia. Reduction of heart rate to a
value below 50 b.p.m. during treatment, in the presence
of symptoms.
Arterial hypertension. Systolic blood pressure 170
mmHg and/or diastolic blood pressure 95 mmHg
during treatment in a non-hypertensive patient.
Arterial hypotension. Reduction in mean arterial
pressure of 25% or greater with respect to baseline
values with a nal value of 70 mmHg.
Headache. Appearance of headache or worsening of
pre-existing headache not responsive to usual analgesic
drugs.
Complications of endoscopic treatments
Esophageal ulcers. Large, conuent esophageal ulcers
2 weeks or more after the last session of endoscopic
treatment, in the presence of symptoms.
Bleeding from esophageal ulcers. Upper GI bleeding
with one of the following: a) active bleeding at the ul-
cer site; b) adherent clot at the ulcer site; or c) absence
of other potentially bleeding lesions at upper GI endo-
scopy.
Dysphagia. Dysphagia 1 week or more after treat-
ment.
Esophageal stricture. Persistent narrowing of the eso-
phageal lumen, as diagnosed by esophagogram or
endoscopy, associated with dysphagia 2 weeks or more
after treatment.
Chest pain. Non-cardiac chest pain requiring anal-
gesics after treatment, persisting for more than 48 h.
Complications of TIPS
TIPS dysfunction. There was agreement on the use of
angiography and/or pressure measurements when there
are clinical signs of TIPS dysfunction, such as re-
appearance of esophageal varices or ascites.
There was no agreement on whether or not TIPS
dysfunction should be assessed in patients not develop-
ing esophageal varices or ascites and which technique
should be used.
Hepatic encephalopathy post-TIPS. In patients with-
out hepatic encephalopathy before TIPS: development
of clinical episodes of encephalopathy. In patients with
hepatic encephalopathy before TIPS: increase in the fre-
quency and/or intensity of episodes of encephalopathy.
Methodological Requirements for Future Trials
in Portal Hypertension
Randomized controlled trials in portal hypertension
should: a) include a sufcient number of patients,
850
based on appropriate sample size calculation; b) pref-
erably be multicenter; c) preferably use stratied ran-
domization/minimization; d) preferably report quality
of life; e) preferably report health economics.
Prognostic stratication (progstrat)
Consensus statements of previous meetings:
Groningen, 1986. Progstrat at randomization needed
at least for description of patients.
Baveno, 1990. Progstrat in randomization and
analysis.
Baveno, 1995. RCTs results in major prognostic sub-
groups should be reported.
Reston, 1996. RCTs results in major prognostic sub-
groups should be reported. Therapeutic benet and
harm should be interpreted according to baseline
risk.
Baveno III consensus statements. Knowledge of differ-
ent treatment effect according to the patient character-
istics may be clinically important. Stratication of pa-
tients according to a few important prognostic vari-
ables allows proper evaluation of different subgroup
treatment effects in meta-analyses if single RCTs do
not reach adequate power. Stratied analysis is justied
a) if a prior hypothesis is made in planning the study;
b) to validate hypotheses from previous studies; c) if it
is made explicit that it is a post-hoc analysis.
Post-hoc subgroup analyses may be considered only
explorative of plausible hypotheses. Subgroup effects
should be replicated in other studies and/or conrmed
by meta-analysis before being accepted for clinical
practice.
Quality of life evaluation
In patients with portal hypertension, both the disease
and its treatment are likely to have a signicant impact
on quality of life. Future studies on portal hyperten-
sion should, thus, measure Health-Related Quality of
Life as one of the (major) outcomes.
At present, there is no disease-specic instrument for
patients with portal hypertension that has all the essen-
tial properties for measurement of HRQOL (validity,
reliability, responsiveness/sensitivity, and coverage).
While instruments to measure HRQOL are being de-
veloped and validated for patients with portal hyper-
tension, generic and chronic liver disease specic in-
struments may be used in trials.
Health economics evaluation
Higher survival and effectiveness are the primary rea-
sons for choosing a treatment for portal hypertension.
Future RCTs on portal hypertension should be
planned to record at least the event-based basic details
Updating consensus in portal hypertension
about the cost of therapy. The adequacy of the time
horizon, sample size and the protocol-driven costs
should be clearly stated.
The methodology for health economic assessment in
portal hypertension should be a topic on a future con-
sensus conference.
Conclusions
The purpose of the consensus denitions about the
variceal bleeding episode and complications of treat-
ments is to use them in trials and other studies on por-
tal hypertension. This does not mean that authors can-
not use their own denitions, but they are encouraged
to use and evaluate in parallel these Baveno III consen-
sus denitions. This should result in some measure of
standardization and increased ease of interpretation
among different studies. Equally important, if there are
uniformly dened end-points, meta-analyses will be
based on more homogeneous studies, which is an es-
sential pre-requisite of this methodology. It is desirable
that future studies be reported using these denitions
as part of the evaluation. Change or renement can
then take place, as they have at Baveno III with respect
to Baveno II and Reston, to ensure that the consensus
denitions do have clinical relevance and are easily ap-
plied in practice. Several denitions agreed upon in Ba-
veno I (2) and II (3,4) were taken for granted and not
discussed in Baveno III. Interested readers can refer to
the Baveno I and II reports (24).
As far as the statements concerning diagnostic algo-
rithms, natural history and treatment strategies are
concerned, they are based on the evidence emerging
from the recent literature; where such evidence is weak
or nonexistent, the statements reect the prevailing
current opinion among the experts.
The suggestions about the topic of future studies
also reect the opinions of the experts about the areas
where new information is most needed.
As long as new diagnostic tools and new treatments
appear, they will have to be assessed in comparison
with present-day standards.
Acknowledgement
The Baveno III workshop was endorsed and supported
in part by an unrestricted educational grant of the
European Association for the Study of the Liver
(EASL).
References
1. Burroughs AK, editor. Methodology and Review of Clinical Tri-
als in Portal Hypertension. Excerpta Medical Congress Service
No. 763. Amsterdam, New York, Oxford: 1987.
2. de Franchis R, Pascal JP, Ancona E, Burroughs AK, Henderson
JM, Fleig W, et al. Denitions, methodology and therapeutic
851
strategies in portal hypertension. A consensus development
workshop. J Hepatol 1992; 15: 25661.
3. de Franchis R. Developing consensus in portal hypertension. J
Hepatol 1996; 25: 3904.
4. de Franchis R, editor. Portal Hypertension II. Proceedings of the
Second Baveno International Consensus Workshop on De-
nitions, Methodology and Therapeutic Strategies. Oxford;
Blackwell Science; 1996.
5. Spina GP, Arcidiacono R, Bosch J, Pagliaro L, Burroughs AK,
Santambrogio R, et al. Gastric endoscopic features in portal hy-
pertension: nal report of a consensus conference. J Hepatol
1994; 21: 4617.
6. Grace ND, Groszmann RJ, Garcia-Tsao G, Burroughs AK, Pag-
liaro L, Makuch RW, et al. Portal hypertension and variceal
bleeding: an AASLD single topic symposium. Hepatology 1998;
28: 86880.
7. de Franchis R, editor. Portal Hypertension III. Proceedings of
the Third Baveno International Consensus Workshop on De-
nitions, Methodology and Therapeutic Strategies. Oxford:
Blackwell Science; 2000 (in press).
8. Primignani M, Carpinelli L, Preatoni P, Battaglia G, Carta A,
Prada A, et al. Natural history of portal hypertensive gastropa-
thy in patients with liver cirrhosis. Gastroenterology 2000; 119:
1817.
9. Sarin SK, Lahoti D, Saxena SP, Murthi NS, Makwane UK.
Prevalence, classication and natural history of gastric varices:
long-term follow-up study in 568 patients with portal hyperten-
sion. Hepatology 1992; 16: 13439.
10. Feu F, Garcia Paga`n JC, Bosch J, Luca A, Teres J, Escorsell A,
et al. Relation between portal pressure response to pharmaco-
therapy and risk of recurrent variceal haemorrhage in patients
with cirrhosis. Lancet 1995; 346: 10569.
Participants
The following chaired sessions or gave review lectures
during the Workshop:
Jaime Bosch, M.D., Barcelona, Spain; Andrew K. Bur-
roughs, M.D., London, U.K.; Gennaro DAmico,
M.D., Palermo, Italy; Juan Carlos Garcia-Paga`n,
M.D., Barcelona, Spain; Guadalupe Garcia-Tsao,
M.D., New Haven, CT, U.S.A.; Pere Gine`s, M.D., Bar-
celona, Spain; Christian Gluud, M.D., Copenhagen,
Denmark; Norman D. Grace, M.D., Boston, Mass.
U.S.A.; Roberto Groszmann, M.D., New Haven CT,
U.S.A.; Loren Laine, M.D., Los Angeles, Ca, U.S.A.;
Didier Lebrec, M.D., Clichy, France; Carlo Merkel,
M.D., Padua, Italy; Massimo Primignani, M.D., Mil-
an, Italy; Massimo Pinzani, M.D., Florence, Italy;
Juan Rode`s, M.D., Barcelona, Spain; Shiv K. Sarin,
New Delhi, India; Detlef Schuppan, M.D., Erlangen,
Germany; Thorkild I.A. Srensen, M.D., Copenhagen,
Denmark; Gregory van Stiegmann, Denver, Col.,
U.S.A.
The following participated in the presentations and the
discussion as panellists:
Belgium: F. Nevens, M.D., Leuven; Canada: N. Mar-
con, M.D., Toronto; France: P. Cale`s, M.D., Angers;
R. Moreau, M.D., Clichy; C. Silvain, M.D., Poitiers;
JP Vinel, M.D., Toulouse; Germany: M. Rssle, M.D.,
Freiburg; T. Sauerbruch, M.D., Bonn; Italy: G. Bald-
R. de Franchis
ucci, M.D., Rome; G. Battaglia, M.D., Padua; M. Bol-
ognesi, M.D., Padua; GC Caletti, M. D., Bologna; R.
Cestari, M.D., Brescia; F. Cosentino, M.D., Milan; M.
Merli, M.D., Rome; O. Riggio, M.D., Rome; D. Sacer-
doti, M.D., Padua; F. Salerno, M.D., Milan; GP Spina,
M.D., Milan; M. Zoli, M.D., Bologna; Spain: A. Es-
corsell, M. D., Barcelona; J Pique`, M.D., Barcelona;
852
C. Villanueva, M.D., Barcelona; Switzerland: C Sieber,
M.D., Basel; Taiwan: FY Lee, M.D. Taipei; HC Lin,
M.D., Taipei; The Netherlands: H. van Buuren, M.D.,
Rotterdam; United Kingdom: D. Patch, M.D., London;
U.S.A. : T. Boyer, M.D., Atlanta, GA; JM Henderson,
M.D. Cleveland, OH; P Kamath, M.D., Rochester,
MN.
S-ar putea să vă placă și
- Consenso Baveno V PDFDocument7 paginiConsenso Baveno V PDFTatiana CostaÎncă nu există evaluări
- Baveno IVDocument10 paginiBaveno IVdepe_cutzÎncă nu există evaluări
- Expanding Consensus in Portal HypertensionDocument10 paginiExpanding Consensus in Portal HypertensionRuben VergaraÎncă nu există evaluări
- Expanding Consensus in Portal HypertensionDocument10 paginiExpanding Consensus in Portal HypertensionJudith MedinaÎncă nu există evaluări
- Expanding Consensus in Portal HypertensionDocument10 paginiExpanding Consensus in Portal HypertensionMarcelo Soares PiresÎncă nu există evaluări
- Baveno 6Document29 paginiBaveno 6José Pepo Apey Reinoso100% (1)
- Baveno VI Consensus Workshop 2015 PDFDocument10 paginiBaveno VI Consensus Workshop 2015 PDFMadalina StoicescuÎncă nu există evaluări
- Approaches To The Diagnosis of Portal HipertensionDocument12 paginiApproaches To The Diagnosis of Portal HipertensionValentina IorgaÎncă nu există evaluări
- Hemodynamic Response To Pharmacological Treatment of Portal Hypertension and Long-Term Prognosis of CirrhosisDocument7 paginiHemodynamic Response To Pharmacological Treatment of Portal Hypertension and Long-Term Prognosis of CirrhosisBarbara Sakura RiawanÎncă nu există evaluări
- GI Bleeding (Text)Document11 paginiGI Bleeding (Text)Hart ElettÎncă nu există evaluări
- Consenso Baveno V PDFDocument7 paginiConsenso Baveno V PDFPerla PradoÎncă nu există evaluări
- The Role of Elastography in ClinicallyDocument11 paginiThe Role of Elastography in ClinicallyValentina IorgaÎncă nu există evaluări
- Baveno DR SilvaDocument6 paginiBaveno DR SilvacarlosarutaÎncă nu există evaluări
- Report of The Baveno VI Consensus Workshop: Liver News ElsewhereDocument2 paginiReport of The Baveno VI Consensus Workshop: Liver News ElsewhereHariana SolorzanoÎncă nu există evaluări
- Gastro Colopatia HTPDocument18 paginiGastro Colopatia HTPHernan Del CarpioÎncă nu există evaluări
- Outcome of Conservative Therapy in COVID-19 in Pts Presenting With GI BleedingDocument7 paginiOutcome of Conservative Therapy in COVID-19 in Pts Presenting With GI BleedingTAUSEEFA JANÎncă nu există evaluări
- Peptic 20 Ulcer 20 BleedingDocument11 paginiPeptic 20 Ulcer 20 Bleedingmsyamsul bachriÎncă nu există evaluări
- Prevencion de Sangrado VaricealDocument5 paginiPrevencion de Sangrado VaricealMayra BeltranÎncă nu există evaluări
- DM31 03 706032Document8 paginiDM31 03 706032oki harisandiÎncă nu există evaluări
- HP94 04 PredictingDocument8 paginiHP94 04 PredictingSa 'ng WijayaÎncă nu există evaluări
- Management of Suspected Anastomotic Leak After Bariatric Laparoscopic Roux-en-Y Gastric BypassDocument7 paginiManagement of Suspected Anastomotic Leak After Bariatric Laparoscopic Roux-en-Y Gastric BypassJOTACEÎncă nu există evaluări
- Annals of HepatologyDocument6 paginiAnnals of HepatologyMishel Vega CoralÎncă nu există evaluări
- 249 13017 2018 Article 169Document6 pagini249 13017 2018 Article 169Rs93Încă nu există evaluări
- Baveno VDocument7 paginiBaveno VMiguel Angel100% (1)
- Gastric Varices Management 2020Document14 paginiGastric Varices Management 2020Oscar ArdilaÎncă nu există evaluări
- Marcadores en Cirrosis HepaticaDocument11 paginiMarcadores en Cirrosis HepaticaBelmonte FerÎncă nu există evaluări
- Aasld 2016Document59 paginiAasld 2016Matias JiménezÎncă nu există evaluări
- TP en Cirrosis2021Document12 paginiTP en Cirrosis2021Daniela OrtizÎncă nu există evaluări
- Acute Variceal HemorrhageDocument48 paginiAcute Variceal HemorrhagePRATAPSAGAR TIWARIÎncă nu există evaluări
- Variceal and Non-Variceal Upper Gastrointestinal Bleeding. Analysis of 249 Hospitalized PatientsDocument7 paginiVariceal and Non-Variceal Upper Gastrointestinal Bleeding. Analysis of 249 Hospitalized PatientsWendy MichelÎncă nu există evaluări
- Esophageal Varices: Pathophysiology, Approach, and Clinical DilemmasDocument2 paginiEsophageal Varices: Pathophysiology, Approach, and Clinical Dilemmaskaychi zÎncă nu există evaluări
- Portal Vein Thrombosis, Risk Factors, Clinical Presentation, and TreatmentDocument6 paginiPortal Vein Thrombosis, Risk Factors, Clinical Presentation, and TreatmentAdiÎncă nu există evaluări
- Determining Severe GI BleedDocument8 paginiDetermining Severe GI BleedDanny SilvaÎncă nu există evaluări
- 2014 Article 639Document8 pagini2014 Article 639Anida HasnaÎncă nu există evaluări
- Clinical StudyDocument6 paginiClinical StudyyrtewdqsfeÎncă nu există evaluări
- Transfusion - 2002 - Pereira - A Model of The Health and Economic Impact of Posttransfusion Hepatitis C Application ToDocument10 paginiTransfusion - 2002 - Pereira - A Model of The Health and Economic Impact of Posttransfusion Hepatitis C Application ToromapechaÎncă nu există evaluări
- Manejo Del ResangradoDocument13 paginiManejo Del ResangradoRudy J CoradoÎncă nu există evaluări
- Ruling Out Esophageal Varices in NAFLD Cirrhosis: Can We Do Without Endoscopy?Document3 paginiRuling Out Esophageal Varices in NAFLD Cirrhosis: Can We Do Without Endoscopy?Marcel DocÎncă nu există evaluări
- Prevalence of Variceal Bleeding in ALD PatientsDocument5 paginiPrevalence of Variceal Bleeding in ALD PatientsvarishÎncă nu există evaluări
- Snowdon 2012Document8 paginiSnowdon 2012Israel BlancoÎncă nu există evaluări
- Guidelines For The Management of Upper Gastrointestinal BleedingDocument4 paginiGuidelines For The Management of Upper Gastrointestinal BleedingDanny Dwi JuniarkoÎncă nu există evaluări
- Ibi JurnalDocument9 paginiIbi JurnalRiski Pradika 2017Încă nu există evaluări
- c1 PDFDocument11 paginic1 PDFirene chanÎncă nu există evaluări
- Evaluation and Management of Suspected Sepsis and Septic Shock in AdultsDocument48 paginiEvaluation and Management of Suspected Sepsis and Septic Shock in AdultsIsmael IbrahimÎncă nu există evaluări
- BUN CR HTDADocument5 paginiBUN CR HTDACecilio MartínÎncă nu există evaluări
- 2014 06 Manejo de Las Varices GastricasDocument11 pagini2014 06 Manejo de Las Varices GastricasrafodocÎncă nu există evaluări
- Kring JournalDocument3 paginiKring JournalcbanguisÎncă nu există evaluări
- Pan 23Document11 paginiPan 23Asad KakarÎncă nu există evaluări
- Non-Invasive Tools For Compensate D Advance D Chronic Liver Disease and Portal Hypertension After Baveno VII - An UpdateDocument10 paginiNon-Invasive Tools For Compensate D Advance D Chronic Liver Disease and Portal Hypertension After Baveno VII - An UpdateValentina IorgaÎncă nu există evaluări
- 18 BudimirDocument8 pagini18 BudimirJain KasparÎncă nu există evaluări
- Endoscopic Band Ligation Is Safe Despite Low Platelet Count and HighDocument10 paginiEndoscopic Band Ligation Is Safe Despite Low Platelet Count and HighGustavo FernándezÎncă nu există evaluări
- Massive Gastrointestinal HemorrhageDocument19 paginiMassive Gastrointestinal HemorrhageVikrantÎncă nu există evaluări
- Research ArticleDocument8 paginiResearch ArticleHuda Al-AnabrÎncă nu există evaluări
- Febrile NeutropeniaDocument18 paginiFebrile Neutropeniajames njengaÎncă nu există evaluări
- Practical Trends in Anesthesia and Intensive Care 2018De la EverandPractical Trends in Anesthesia and Intensive Care 2018Încă nu există evaluări
- Secondary HypertensionDe la EverandSecondary HypertensionAlberto MorgantiÎncă nu există evaluări
- Variceal HemorrhageDe la EverandVariceal HemorrhageRoberto de FranchisÎncă nu există evaluări
- Home Blood Pressure MonitoringDe la EverandHome Blood Pressure MonitoringGeorge S. StergiouÎncă nu există evaluări
- Stretching SportDocument6 paginiStretching Sportscott105Încă nu există evaluări
- Valplast: Flexible, Esthetic Partial DenturesDocument4 paginiValplast: Flexible, Esthetic Partial Denturesአነኬ ቹህቺዶሃሠኪቺጆቺÎncă nu există evaluări
- Post MenopauseDocument59 paginiPost Menopausemayuri zanwar100% (1)
- Prostaglandins, Angiotensin and Bradikinin-Dr - Jibachha Sah, M.V.SC, LecturerDocument27 paginiProstaglandins, Angiotensin and Bradikinin-Dr - Jibachha Sah, M.V.SC, Lecturerjibachha sahÎncă nu există evaluări
- Constant SystemsDocument16 paginiConstant SystemsWanderley PedrosoÎncă nu există evaluări
- Verticillium WiltsDocument561 paginiVerticillium Wiltsmohammadi100% (1)
- Beginning Molecular Biology Laboratory Manual-UMBC.2003 (Por Trisquelion)Document52 paginiBeginning Molecular Biology Laboratory Manual-UMBC.2003 (Por Trisquelion)Sivan AndiÎncă nu există evaluări
- Emergencies in UrologyDocument112 paginiEmergencies in UrologySusiyadiÎncă nu există evaluări
- Mekanisme Fertilisasi PDFDocument9 paginiMekanisme Fertilisasi PDFmaulaalfarisiÎncă nu există evaluări
- FISA Club Training ProgrammeDocument40 paginiFISA Club Training Programmemendes67Încă nu există evaluări
- Pathophysiology of AppendicitisDocument2 paginiPathophysiology of AppendicitisDivine Jane Purcia67% (3)
- Geron Sas 15Document8 paginiGeron Sas 15SSA CommissionÎncă nu există evaluări
- Nutritional and Anti-Nutritional Composition of Bridelia Ferruginea Benth (Euphorbiaceae) Stem Bark SampleDocument13 paginiNutritional and Anti-Nutritional Composition of Bridelia Ferruginea Benth (Euphorbiaceae) Stem Bark SampleAmin MojiriÎncă nu există evaluări
- Nobel Prize in Physiology or Medicine WinnersDocument19 paginiNobel Prize in Physiology or Medicine WinnersNelly Bling BaileyÎncă nu există evaluări
- The Science Behind Peak Metabolic Health DR Inigo San Millan The Proof Podcast - YouTubeDocument50 paginiThe Science Behind Peak Metabolic Health DR Inigo San Millan The Proof Podcast - YouTubeDavid RodriguezÎncă nu există evaluări
- The Real EveDocument2 paginiThe Real EveKangMaru_025Încă nu există evaluări
- CH 22 Chemical Coordination and IntegrationDocument4 paginiCH 22 Chemical Coordination and IntegrationRohankanani007100% (1)
- Insomnia-Diagnosis and Treatment PDF (Apr 27, 2010) - (1420080792) - (CRC Press)Document497 paginiInsomnia-Diagnosis and Treatment PDF (Apr 27, 2010) - (1420080792) - (CRC Press)bogdasusÎncă nu există evaluări
- Dream Yoga SyllabusDocument2 paginiDream Yoga SyllabusmichaÎncă nu există evaluări
- History of Psychosomatic Medicine BlumenfeldDocument20 paginiHistory of Psychosomatic Medicine Blumenfeldtatih meilaniÎncă nu există evaluări
- Human Placental LactogenDocument2 paginiHuman Placental Lactogenvici911Încă nu există evaluări
- 08 Scorpion Sting UpdateDocument10 pagini08 Scorpion Sting Updatejoaoalmeida_1955Încă nu există evaluări
- GS Activity (OCT-DEC 2019) Rev. 1-1Document3 paginiGS Activity (OCT-DEC 2019) Rev. 1-1Reyof Al HarthiÎncă nu există evaluări
- Revised Rguhs M FinalDocument205 paginiRevised Rguhs M FinalNishaÎncă nu există evaluări
- Lower Invertebrates Comparative CharactersDocument5 paginiLower Invertebrates Comparative CharactersShadab HanafiÎncă nu există evaluări
- Ardio Ulmonary EsucitationDocument24 paginiArdio Ulmonary EsucitationfaizasaleemsameÎncă nu există evaluări
- Metabolic Reprogramming Due To Hypoxia in Pancreatic Can - 2021 - BiomedicineDocument14 paginiMetabolic Reprogramming Due To Hypoxia in Pancreatic Can - 2021 - BiomedicineAkhmad BajuriÎncă nu există evaluări
- Culture Media Used in Microbiology: Salman Tausif Senior Technologist Clinical MicrobiologyDocument36 paginiCulture Media Used in Microbiology: Salman Tausif Senior Technologist Clinical MicrobiologyZeeshan YousufÎncă nu există evaluări
- Sepsis Case StudiesDocument5 paginiSepsis Case StudiesRia Arcane0% (2)
- Biotex FlyerDocument2 paginiBiotex FlyerNadim NikÎncă nu există evaluări