Documente Academic
Documente Profesional
Documente Cultură
32707170
Încărcat de
shahrzad_ghazalDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
32707170
Încărcat de
shahrzad_ghazalDrepturi de autor:
Formate disponibile
European Journal of Sport Science, July 2008; 8(4): 183192
ORIGINAL ARTICLE
Effect of a preventive intervention programme on the prevalence of anterior knee pain in volleyball players
E. CUMPS1, E. A. VERHAGEN2, S. DUERINCK1, A. DEVILLE1, L. DUCHENE1, & 1 R. MEEUSEN
Department of Human Physiology and Sports Medicine, Vrije Universiteit Brussel, Brussels, Belgium, and 2EMGO Institute, VU University Medical Centre, Amsterdam, The Netherlands
1
Abstract Chronic knee disorders, such as patellofemoral pain syndrome and patellar tendinosis, are common injuries in volleyball players. Using a randomized clinical trial, the aim of the present study was to determine the effect of a 4-month in-season intervention programme on the prevalence of anterior knee pain in volleyball players. No significant differences were observed between the intervention and control group for the prevalence of anterior knee pain after the intervention programme (odds ratio 01.58 [95% confidence interval: 0.604.20]). Also, no significant differences were observed for individuals with previously sustained anterior knee pain (OR 00.81 [95% CI: 0.332.20]). It was revealed that the risk for recurrent anterior knee pain is significantly higher than the risk for newly sustained anterior knee pain (OR 05.79 [95% CI: 1.5921.00]). In conclusion, we were unable to confirm any preventive effect of the intervention programme on the prevalence of anterior knee pain. However, a previous study using the same intervention and measuring the effect on the intrinsic risk factors of anterior knee pain showed a positive effect.
Keywords: Anterior knee pain, patellofemoral pain syndrome, patellar tendinosis, prevention
Introduction Knee injuries sustained across various sport disciplines, which account for 1550% of all sports injuries (de Loes, Dahlstedt, & Thomee, 2000), have often been reported on (Backx, Beijer, Bol, & Erich, 1991; Kujala et al., 1995). A high incidence of knee injuries has been observed in volleyball (Aagaard & Jorgensen, 1996; Bahr, Reeser, & Federation Internationale de Volleyball, 2003; Hewett, Stroupe, Nance, & Noyes, 1996; Kujala et al., 1995; Schafle, Requa, Patton, & Garrick, 1990; Verhagen, Van der Beek, Bouter, Bahr, & van Mechelen, 2004), where chronic knee injuries (50 88%) are more common than acute knee injuries (1235%) (Aagaard & Jorgensen, 1996; Aagaard, Scavenius, & Jorgensen, 1997; Bahr et al., 2003; Briner & Benjamin, 1999; Schafle et al., 1990). A common chronic knee disorder in athletic popula-
tions is the patellofemoral pain syndrome (Fairbank, Pynsent, Van Poortvliet, & Phillips, 1984; Kujala et al., 1995; Roush et al., 2000; Thomee, Augustsson, & Karlsson, 1999). Patellofemoral pain syndrome is a term believed to encompass all painrelated problems of the anterior part of the knee excluding intra-articular pathologies, peripatellar tendonitis or bursitis, plica syndromes, Sinding Larsens and Osgood Schlatters disease, neuromas and other rarely occurring pathologies (Thomee, Renstrom, Karlsson, & Grimby, 1995). Patellar tendinosis or jumpers knee is an anterior knee pain pathology most frequently found in volleyball players (Aagaard & Jorgensen, 1996; Bahr et al., 2003; Ferretti, Ippolito, Mariani, & Puddu, 1983; Lian, Engebretsen, & Bahr, 2005; Lian, Engebretsen, Ovrebo, & Bahr, 1996; Schafle et al., 1990), with an incidence of 9% (Bahr et al., 2003) to 64% (Schafle et al., 1990).
Correspondence: R. Meeusen, Department of Human Physiology and Sports Medicine, Vrije Universiteit Brussel, Pleinlaan 2, 1050 Brussels, Belgium. E-mail: rmeeusen@vub.ac.be ISSN 1746-1391 print/ISSN 1536-7290 online # 2008 European College of Sport Science DOI: 10.1080/17461390802067711
184
E. Cumps et al. medialis obliquus (Cowan, Bennell, Hodges, Crossley, & McConnel, 2001; McConnel, 2002; Voight & Wieder, 1991; Witvrouw, Sneyers, Lysens, Victor, & Bellemans, 1996; Witvrouw et al., 2000). Strengthening of the vastus medialis obliquus has been advocated as a treatment for patellofemoral pain syndrome, as weakness of this component of the quadriceps muscle is postulated to contribute to malalignment of the patella (Laprade, Culham, & Brouwer, 1998). Since anterior knee pain especially patellofemoral pain syndrome and patellar tendinosis is a major concern of volleyball players, we aimed at developing an intervention programme to prevent the prevalence of self-reported anterior knee pain. The purpose of this study was to determine the effect of a 4-month intervention programme on the prevalence of anterior knee pain in volleyball players.
In spite of the high incidence of this injury, there are no studies on its prevention. Only the effect of brace application among military recruits to prevent anterior knee pain has been investigated, with the authors reporting a lower incidence of such pain in individuals who wore the brace (Van Tiggelen et al., 2004). A wide variety of treatment options has been proposed, but the conservative treatment protocols have not been properly documented (Visnes, Hoksrud, Cook, & Bahr, 2005). Eccentric training in individuals with patellar tendinosis, which has a very promising effect in the treatment of chronic Achilles tendinosis (Kingma, de Knikker, Wittink, & Takken, 2007), also shows positive results but is inconclusive because of methodological shortcomings of the trials (Visnes & Bahr, 2007). In-depth knowledge of the intrinsic risk factors is also important when designing treatment strategies. Few authors have found an association between muscle tightness and tendinosis (Cook, Kiss, Khan, Purdam, & Webster, 2004; Ekstrand, Gillquist, & Liljedahl, 1983; Witvrouw, Bellemans, Lysens, Danneels, & Cambier, 2001) or patellofemoral pain syndrome (Sommer, 1988; Witvrouw, Lysens, Bellemans, Cambier, & Vanderstraeten, 2000). Decreased flexibility leads to an increase in tendon strain with joint movements and therefore predisposes athletes to tendon overload (Fyfe & Stanish, 1992). Witvrouw et al. (2001) believe that it is crucial to emphasize the use of proper stretching in both the treatment and prevention of patellar tendinosis. Individuals with symptoms of patellofemoral pain syndrome also show lower strength of the quadriceps (Duffey, Martin, Canon, Craven, & Messier, 2000; Messier, Davis, Curl, Lowery, & Pack, 1991; Salsich, Brechter, Farwell, & Powers, 2002; Thomee et al., 1995; Van Tiggelen et al., 2004; Witvrouw et al., 2000), hamstrings (Duffey et al., 2000; Messier et al., 1991), hip abduction and hip external rotation muscles (Ireland, Willson, Ballantyne, & Davis, 2003; Mascal, Landel, & Powers, 2003). One of the compensatory strategies to minimize joint loading and pain is the break phenomenon during quadriceps contraction, which is mainly seen during eccentric contractions (Anderson & Herrington, 2003) and has been described as a saving reflex to prevent further stress. Rehabilitation exercises of the quadriceps in patients with patellofemoral pain syndrome should be chosen with regard to joint loading and range of movement to facilitate quadriceps activation rather than inhibiting it (Anderson & Herrington, 2003). Another phenomenon that has been proposed in the aetiology of the patellofemoral pain syndrome is the imbalance between the activation patterns of the vastus lateralis muscle and vastus
Materials and methods Study design A randomized clinical trial was initiated to measure the effectiveness of an intervention programme on the prevalence of anterior knee pain.
Power analysis Previous research, involving the same participants, revealed that the 1-year prevalence of anterior knee pain, according to the definition outlined below, is 52.2%. An a priori power analysis showed that for a 15% improvement in the prevalence of anterior knee pain, with a 00.05 and b00.90, a sample of 226 individuals is required.
Recruitment During preparation for the 20052006 volleyball season, inclusion criteria for teams to take part in the study and in the randomization procedure were as follows: (1) the members of the team should be Dutch speaking, (2) they should be located within an hours drive from Brussels, and (3) playing in Division 1, Division 2 or National 1. Sixty-nine of 136 teams met the inclusion criteria and were randomized into a control or an intervention group. Of these, 54 initially agreed to participate. Written informed consent was obtained from each player and the study was performed in accordance with the institutional rules for human research and the Declaration of Helsinki for Medical Research involving humans.
Prevention of anterior knee pain Injury registration and injury definition A questionnaire recorded demographic data, information on intrinsic and extrinsic risk factors, and the point-, one-year-, and lifetime-prevalence of anterior knee pain. In the present study, anterior knee pain was defined as an overuse injury that causes physical discomfort in the anterior part of the knee (Thomee et al., 1995), and pain and/or stiffness of the musculoskeletal system, which has an insidious onset and is present during and/or after volleyball activity. Such a complaint has to persist for at least three volleyball active days. Malaise and illness were excluded (Cumps, Verhagen, & Meeusen, 2007). The prevalence of pain used was self-reported anterior knee pain, as per the definition above.
185
Guidelines on how to correct the exercises were also explained. All this information was passed on to each trainer/coach by means of a CD-ROM containing video recordings and a manual with the complete programme and detailed explanation for each individual exercise. Statistical analysis Both groups were compared at baseline for demographic variables using an independent samples t-test (PB0.05) in the case of normal distribution of the variables and with the Mann-Whitney U-test (P B0.05) if the variables were not normally distributed. The Kolmogorov-Smirnov test (P B0.05) was used to determine the distribution of the demographic variables. All statistical analyses were performed using SPSS v. 14.0 (SPSS Inc., Chicago, IL, USA). The effectiveness of the intervention programme, using an intention-to-treat approach, was determined by calculating odds ratios (OR) and their 95% confidence intervals (CI). All participants, including those who did not conform to the intervention throughout the intervention period, were included in the statistical analysis.
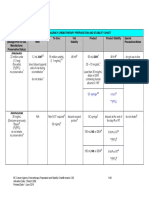
Intervention The intervention programme had to cover a broad spectrum of anterior knee pain disorders, especially patellofemoral pain syndrome and patellar tendinosis, since an exact diagnosis is often hard to establish, especially in self-reported anterior knee pain. The intervention programme is presented in Table I. The intervention programme developed was derived from literature concerning treatment strategies and intrinsic risk factors for anterior knee pain in general and patellofemoral pain syndrome and patellar tendinosis in particular. The intervention programme covered 16 weeks of the 20052006 volleyball season and was performed twice a week during the practice session in addition to the normal training routine of the intervention group. The control group only executed their normal training routine. The effect of injury awareness was minimized by giving both groups exactly the same information on the background and the procedures of the study at baseline. The only difference in information was instruction on the intervention programme, which was withheld from the control group. The main goal of the first month was to train isometric strength using open kinetic chain exercises. During the second month, the programme mainly emphasized isometric strength using closed kinetic chain exercises. Eccentric exercises performed during the third and fourth months also involved sport-specific exercises and jump training or plyometrics, with the emphasis on the quality of landing techniques. After each practice session, passive stretching exercises of the quadriceps, hamstring, iliotibial band, gastrocnemius, soleus, and gluteal muscles were performed. Active hamstring muscle stretching was performed starting in week 3. The coaches received thorough information on the complete programme as well as on all its individual exercises and on how to execute them correctly.
Results Participants and drop-out The flow chart of the selection procedures and the number of participants is presented in Figure 1. From the 54 teams that initially agreed to participate, 30 completed the pre- and post-measurements properly, resulting in 167 participants with complete data. Teams and players dropped out because they were not able to attend the post-measurement, suffered from injuries, quit playing volleyball, transferred to another team or withdrawal of the entire team. Table II presents the demographic variables for both the intervention and control groups and those who dropped out. There were no significant differences (independent samples t-test: P B0.05) between the control and intervention group, or between those who dropped out and those who completed the intervention. Effectiveness Inclusion of individuals with symptoms of anterior knee pain at baseline. At baseline, the prevalence of anterior knee pain was higher in the intervention group than in the control group, but no significant differences were observed for the prevalence of anterior knee pain, for the total sample (OR 01.51 [95% CI: 0.703.26), the women only (OR 00.69 [95% CI: 0.202.41]) or the men only (OR 02.05
186
Table I. The intervention programme developed based on a literature review concerning the rehabilitation of patellar tendinosis and patellofemoral pain syndrome
E. Cumps et al.
Month 1 Isometric strength in OKC Week 1 Q-ceps setting 3 )10 (7 s) Oscillating exercise Q-ceps with tubing with knee angle 1208 3 )20 s SLR lifting up and down 3 )10 Week 2 Q-ceps setting 3 )10 (7 s) Co-contraction with knee angle 1208 3 )10 (7 s) SLR lifting inside and outside 3 )10 Q-ceps setting 3 )10 (7 s) Oscillating exercise Q-ceps with tubing with knee angle 1208 3 )20 s SLR in abduction lying on the side 3 )10 Q-ceps setting 3 )10 (7 s) Oscillating exercise Q-ceps with tubing with knee angle 1208 3 )20 s Co-contraction with knee angle 908 3 )10 (7 s)
Month 2 Isometric strength in CKC Oscillating bilateral squat back against wall, knee angle max. 1208 3)20 s SLR circles clockwise and not clockwise 3)10 Oscillating exercise H prone with tubing 3)20 s Q-ceps setting 3)10 (7 s) Oscillating exercise Q-ceps with tubing with knee angle 1208 Oscillating lunge with knee angle 1208 3)20 s Co-contraction with knee angle 1208 3)10 (7 s) Oscillating lunge with knee angle 1208 3)20 s Oscillating exercise H prone with tubing 3)20 s SLR in abduction lying on the side 3)10 Oscillating bilateral squat back against wall, knee angle max. 1208 3)20 s Oscillating lunge with knee angle 1208 3)20 s
Month 3 Sports specific skills and plyometrics
Month 4 Eccentric load exercise
Oscillating bilateral squat back 1/3 (01208 knee angle) unilateral against wall, knee angle max. 1208 squat 3)20 s 3 )10 Oscillating exercise H prone with tubing Lateral step up & down 3)20 s 3 )10 1/3 (01208 knee angle) bilateral squat 3)10 1/3 (01208 knee angle) bilateral squat with tubing 3)10 Oscillating lunge with knee angle until 1208 3)20 s Lateral step up & down 3)10 Dropsquat knee angle until 908 3)10 Frontal step up & down 3)10 Lunge knee angle until 1208 3)10 SLR in abduction lying on the side 3)10 Oscillating jump lunge with knee angle until 1008 3 )20 s Dropsquat knee angle until 908 3 )12 Sliding/shuffle sideways with knee angle around 1008 3 )20 Jump and reach 3 )15 Jump lunge knee angle until 908 3 )10 Oscillating drop jump knee angle until 908 3 )30 s 1/3 (01208 knee angle) bilateral squat with tubing 3 )20 Oscillating drop jump knee angle until 908 4 )30 s Frontal step up & down 3 )10
Week 3
Week 4
1/3 (01208 knee angle) bilateral squat against wall 3)10 Sliding/shuffle sideways with knee angle 1/2 (0908 knee angle) unilateral around 1008 squat against wall 3)20 3 )10
Note: OKC0open kinetic chain; CKC0closed kinetic chain; Q-ceps0quadriceps; SLR0straight leg raise; H0hamstring; oscillating0small repetitive swinging movements within a range of 58; tubing 0exercise with elastic bands.
Prevention of anterior knee pain
187
Figure 1. Flow chart of selection procedures and the number of players and teams nally participating in the study. AKP0anterior knee pain, IG 0intervention group, CG 0control group.
[95% CI: 0.686.20]). Figure 2 shows the percentage of participants with anterior knee pain after the 4-month intervention period with the associated odds ratio (95% confidence interval). No significant differences in prevalence of anterior knee pain were found between the control and intervention group as a result of the intervention programme. The prevalence of anterior knee pain did not decrease significantly baseline and post-intervention, either in the intervention group (OR 00.86 [95% CI: 0.461.60]) or in the control group (OR 00.91 [95% CI: 0.382.17]). Exclusion of individuals with symptoms of anterior knee pain at baseline. There was no significant difference
between the intervention and control group after the 4-month intervention. Figure 3 presents odds ratios (95% confidence intervals) and the percentages of players with anterior knee pain. In the control group, 60.4% of the participants had presented with anterior knee pain in the past, whereas 59.2% of the intervention group had experienced such pain before. Again no significant differences were observed after the intervention between the intervention and control group for the occurrence of new anterior knee pain (OR 01.21 [95% CI: 0.314.76]) or recurrent anterior knee pain (OR 00.81 [95% CI: 0.332.20]). Figure 4 presents the percentages of new and recurrent anterior knee pain for both groups. In the control
188
E. Cumps et al.
Table II. Demographic variables for the intervention and control groups for effectiveness with inclusion and exclusion of participants with symptoms of anterior knee pain before the intervention period Effectivenessa Number (n) Height (m) Weight (kg) BMI (kg m (2) Age (years) Number (n) Height (cm) Effectivenessb Weight (kg) BMI (kg m (2) Age (years)
Female Male Total Female Male Total Female Male Total Female Male Total
38 64 102 39 28 67 20 7 27 17 8 25
1.73 (0.06) 1.87 (0.07) 1.82 (0.10)
Intervention group 64.6 (9.4) 21.6 (2.4) 23.3 (6.2) 33 1.73 (0.06) 64.2 (9.8) 21.4 (2.4) 23.4 (6.5) 82.7 (11.4) 23.6 (2.5) 26.8 (5.7) 43 1.87 (0.07) 82.5 (11.1) 23.5 (2.5) 26.9 (5.8) 76.0 (13.8) 22.8 (2.6) 25.5 (6.1) 76 1.81 (0.10) 74.5 (13.9) 22.6 (2.6) 25.4 (6.3) 1.73 (0.06) 64.5 (6.6) 21.6 (1.7) 23.9 (6.2) 1.88 (0.07) 82.7 (10.5) 23.4 (2.7) 26.4 (7.4) 1.79 (0.09) 72.0 (12.3) 22.4 (2.3) 24.9 (5.7)
Control group 1.73 (0.06) 65.8 (7.5) 22.1 (2.1) 24.4 (5.9) 32 1.088 (0.06) 84.0 (9.9) 23.7 (2.7) 26.5 (6.5) 21 1.79 (0.09) 73.4 (12.4) 22.8 (2.5) 25.3 (8.5) 53 1.75 (0.06) 1.86 (0.07) 1.83 (0.08) 1.75 (0.05) 1.89 (0.08) 1.80 (0.09)
Intervention group (drop-out) 67.8 (5.25) 22.2 (1.5) 26.2 (6.1) 5 1.75 (0.06) 62.0 (7.1) 20.3 (0.8) 24.1 (6.9) 80.2 (9.8) 23.1 (2.2) 26.2 (7.7) 21 1.87 (0.08) 83.3 (12.2) 23.8 (2.6) 26.7 (5.7) 76.9 (10.4) 22.9 (2.1) 26.2 (6.9) 26 1.86 (0.09) 81.4 (13.2) 23.5 (2.7) 26.5 (5.7) Control group (drop-out) 67.2 (7.5) 21.9 (2.9) 23.3 (6.7) 7 1.88 (0.09) 89.3 (4.6) 25.3 (2.0) 27.0 (5.6) 84.8 (13.7) 23.8 (3.9) 25.8 (5.7) 7 1.73 (0.04) 71.4 (9.4) 24.0 (2.8) 26.5 (4.6) 73.0 (12.9) 22.6 (3.3) 24.1 (6.4) 14 1.79 (0.10) 78.8 (11.9) 24.5 (2.5) 26.7 (5.2)
b
Note: a Participants with symptoms of anterior knee pain during the PRE measurements are included; anterior knee pain during the PRE measurements are excluded.
Participants with symptoms of
group, the risk for recurrent anterior knee pain was significantly higher than the risk for new anterior knee pain (OR 05.79 [95% CI: 1.5921.00]). Exclusion of individuals without symptoms of anterior knee pain at baseline. Before the intervention, 25.5% of the intervention group and 20.9% of the control group reported anterior knee pain. The number of participants with anterior knee pain pre-intervention diminished, with 34.6% in the intervention group and 14.3% in the control group. There was no significant decrease in the number of participants with anterior knee pain in the intervention compared
with the control group (OR 00.41 [95% CI: 0.07 2.18]).
Discussion The main purpose of this study was to develop a preventive intervention programme to cover a broad range of pathologies, defined as anterior knee pain, in volleyball players. This approach appeared necessary, since patellofemoral pain syndrome is difficult to define and diagnose, as patients experience a variety of symptoms from the patellofemoral joint with different levels of pain and physical impairment
Figure 2. The percentages of players with anterior knee pain (AKP) post-intervention are presented. Participants with symptoms of anterior knee pain during the pre-measurements were included. IG 0intervention group, CG0control group.
Figure 3. The percentages of players with anterior knee pain (AKP) post-intervention are presented. Participants with symptoms of anterior knee pain during the pre-measurements were excluded. IG0intervention group, CG0control group.
Prevention of anterior knee pain
189
Figure 4. The percentages of players with recurrent and new anterior knee pain (AKP) post-intervention are presented. Participants with symptoms of anterior knee pain during the premeasurements are excluded. IG 0intervention group, CG 0 control group.
(Thomee et al., 1999). The term patellofemoral is appropriate, as it is hard to pinpoint which specific structure is affected and pain is the symptom that all patients experience (Thomee et al., 1999). Many treatment options have been proposed, ranging from conservative rehabilitation programmes to eccentric training programmes (Visnes et al., 2005; Visnes & Bahr, 2007), yet the results are inconclusive due to poorly documented protocols and methodological shortcomings of the studies respectively.
Intervention programme Decreased strength of the quadriceps (Duffey et al., 2000; Messier et al., 1991; Salsich et al., 2002; Thomee et al., 1995; Van Tiggelen et al., 2004; Witvrouw et al., 2000), hamstrings (Duffey et al., 2000; Messier et al., 1991), hip adduction and hip external rotation muscles (Ireland et al., 2003; Mascal et al., 2003) have been observed in individuals with symptoms of patellofemoral pain syndrome. The imbalance in activation pattern of the vastus medialis obliquus and vastus lateralis has been found to be an important factor in patients with patellofemoral pain syndrome (Cowan et al., 2001; McConnel, 2002; Voight & Wieder, 1991; Witvrouw et al., 1996, 2000). It has been implied that reduced motor unit activity of the vastus medialis obliquus relative to the vastus lateralis could be the cause of lateral patellar subluxation and dislocation (Sakai, Luo, Rand, & An, 2000). This is why re-education of the vastus medialis obliquus is considered an essential component of a non-operative approach to patellofemoral pain (LaBrier & ONeill, 1993; Souza & Gross, 1991). The vastus medialis obliquus is believed to be stimulated most during isometric quadriceps contractions in combination with adduc-
tion and internal rotation of the hip (Gyf & Man, 1996), although some authors did not report preferential activation of this muscle with associated hip adduction (Cerny, 1995; Coqueiro et al., 2005; Davlin, Holcomb, & Guadagnoli, 1999). Bilateral semi-squats together with hip adduction do reveal an increase in vastus medialis obliquus and vastus lateralis activation patterns (Cerny, 1995; Coqueiro et al., 2005; Dursun, Dursun, & Kilic, 2001; Heitkamp, Horstmann, Mayer, Weller, & Dickhuth, 2001; Hertel, Eral, Tsang, & Miller, 2004). In our intervention programme, strengthening of the quadriceps and hamstrings was achieved by starting with an emphasis on isometric strength in an open kinetic chain evolving to isometric strength in a closed kinetic chain in the second month, starting with eccentric exercises in a closed kinetic chain in the third month, and introducing sport-specific exercises and jump alignment training during month 4. Both open and closed kinetic chain exercises were integrated in the intervention programme, because Cohen et al. (2001) revealed that throughout the entire flexion range, open kinetic chain stresses are neither supra-physiological nor significantly greater than closed kinetic chain exercise stresses. Instructions on jump-landing techniques were incorporated in the intervention programme due to the recent surge of lower extremity injury prevention programmes (Hewett et al., 1996), which produced promising results in reducing knee injuries among young female athletes who took part in a jumplanding instructional programme (Onate et al., 2005). Although these jump-landing techniques have focused on the prevention of ACL injuries, it is known that a knee valgus and an internally rotated knee position are unfavourable for the development of patellofemoral pain syndrome (Sommer, 1988). Each session of the intervention programme ended with stretching exercises because muscle tightness is often associated with patellofemoral pain syndrome (Duffey et al., 2000; Ireland et al., 2003; Mascal et al., 2003; Messier et al., 1991; Salsich et al., 2002; Thomee et al., 1995; Van Tiggelen et al., 2004; Witvrouw et al., 2000). Because the intervention programme needs to be cost-beneficial and easy to implement during practice sessions, treatment options such as taping, bracing, isokinetic strength training, electro-stimulation, ultrasound therapy, and biofeedback training were excluded. Effectiveness The main aim of the present study was to assess the effectiveness of a preventive intervention programme on the prevalence of anterior knee pain in volleyball players. We found no effect of the 4-month
190
E. Cumps et al. As a result, the programme can be seen as being too long on top of the normal training routine. Whether the programme should be performed in-season or pre-season and how long it should last remains to be determined. Terminology for anterior knee pain Another factor that could have resulted in the noneffectiveness of the programme is the purpose it was developed for. Anterior knee pain is a wide-ranging complaint that involves many different pathologies and encompasses a diverse terminology (Thomee et al., 1999). The fact that the symptoms of patellofemoral pain syndrome and patellar tendinosis are similar complicates the establishment of an exact diagnosis. In other words, there is a discrepancy since on the one hand the intervention programme should cover both pathologies because there is often no exact diagnosis, but on the other a more specific approach would probably result in better results regarding prevalence and symptoms. Conclusion Patellofemoral pain syndrome and patellar tendinosis are of major concern among volleyball players (Aagaard & Jorgensen, 1996; Bahr et al., 2003; Ferretti et al., 1983; Lian et al., 1996, 2005; Schafle et al., 1990). There are conflicting results regarding the intrinsic risk factors and treatment options proposed for these knee disorders. This is probably a consequence of the varying terminology used in the literature (Thomee et al., 1999). The lack of preventive studies of anterior knee pain is probably a result of these inconsistencies. A research question for the future is whether the prevention of anterior knee pain should be reached using a general approach covering both patellofemoral pain syndrome and patellar tendinosis, or if it should concentrate on a single pathology, with the inherent difficulties and costs in establishing the diagnosis. Although the present study was unable to determine the effectiveness of the intervention programme, a previous study showed a positive effect on the intrinsic risk factors associated with patellofemoral pain syndrome and patellar tendinosis (Cumps et al., 2007). This lack of effectiveness can be ascribed to the power of the sample or to the broad approach, which included both patellofemoral pain syndrome and patellar tendinosis.
intervention on the prevalence of anterior knee pain in the intervention group, for the total sample, for the women alone or men alone. There were also no significant differences in recurrent and new cases of anterior knee pain. An a priori power analysis revealed that to achieve a 15% improvement in the prevalence of anterior knee pain (a 00.05; b 00.90), a sample of 226 would be necessary. Initially, 54 teams (232 players) agreed to participate and were randomized into a control or intervention group. There was a drop-out rate of 27.2%, reducing the total number of participants to 169. Of those 169 participants, 40 dropped out of the study because of anterior knee pain at the inception of the intervention programme. So, one possible reason for the ineffectiveness of the programme can be attributed to the insufficient observed power of the study, which was 69.5% (a 00.05; b 00.70). We aimed to keep injury awareness as low as possible by providing both groups with exactly the same information on the study at baseline, except for the intervention programme, which was kept from the control group. Nevertheless, a higher prevalence of anterior knee pain was seen in the intervention group after the intervention, although this was not significant. This phenomenon can be attributed to the higher prevalence of anterior knee pain in the intervention group during the inception of the intervention on the one hand, and by the so-called medical student syndrome on the other. This syndrome is a form of hypochondria frequently seen in medical students, in which they perceive themselves to be experiencing the symptoms of whatever disease they are studying. These persons figure that they are victim of a certain disease, whereas in reality no medical condition is present (Morrison & Bennet, 2006). Compliance In the intervention group, 22 participants (including players with anterior knee pain) and 8 participants (excluding players with anterior knee pain) admitted that they had not performed the intervention programme. This resulted in a drop-out rate of 21.6% and 11.9% respectively. The players did not perform the intervention programme because of a lack of interest or time, according to the trainer/coach. Towards the end of the 20052006 season, some teams approached promotion or degradation periods. As a result, the intervention programme was sometimes performed inaccurately or was skipped altogether. As mentioned by the participants, the intervention programme lasted 20 min per session. This can be considered quite a long time, since the majority of the teams only train twice a week for 2 h.
References
Aagaard, H., & Jorgensen, U. (1996). Injuries in elite volleyball. Scandinavian Journal of Medicine and Science in Sports, 6, 228 232.
Prevention of anterior knee pain
Aagaard, H., Scavenius, M., & Jorgensen, U. (1997). An epidemiological analysis of the injury pattern in indoor and beach volleyball. International Journal of Sports Medicine, 18, 217221. Anderson, G., & Herrington, L. (2003). A comparison of eccentric isokinetic torque production and velocity of knee exion angle during step down in patellofemoral pain syndrome patients. Clinical Biomechanics, 18, 500504. Backx, F. J., Beijer, H. J., Bol, E., & Erich, W. B. (1991). Injuries in high-risk persons and high-risk sports: A longitudinal study of 1818 school children. American Journal of Sports Medicine, 19, 124130. Bahr, R., Reeser, J. C., & Federation Internationale de Volleyball (2003). Injuries among world-class professional beach volleyball players. American Journal of Sports Medicine, 31, 119125. Briner, W. W., & Benjamin, H. (1999). Volleyball injuries: Managing acute and overuse disorders. The Physician and Sportsmedicine, 27, 4860. Cerny, K. (1995). Vastus medialis oblique/vastus lateralis muscle activity ratios for selected exercises in person with and without patellofemoral pain syndrome. Physical Therapy, 75, 672683. Cohen, Z. A., Roglic, H., Grelsamer, R. P., Henry, J. H., Levine, W. N., Mow, V. C., et al. (2001). Patellofemoral stresses during open and closed kinetic chain exercises: An analysis using computer simulation. American Journal of Sports Medicine, 29, 480487. Cook, J. L., Kiss, Z. S., Khan, K. M., Purdam, C. R., & Webster, K. (2004). Anthropometry, physical performance, and ultrasound patellar tendon abnormality in elite junior basketball players: A cross-sectional study. British Journal of Sports Medicine, 38, 206209. Coqueiro, K. R., Bevilaqua-Grossi, D., Berzin, F., Soares, A. D., Candolo, C., & Monteiro-Perdro, V. (2005). Analyses on the activation of the VMO and VLL muscles during semi-squat exercises with and without hip adduction in individuals with patellofemoral pain syndrome. Journal of Electromyography and Kinesiology, 15, 596603. Cowan, S. M., Bennell, K. L., Hodges, P. W., Crossley, K. M., & McConnel, J. (2001). Delayed onset of electromyographic activity of vastus medialis obliquus relative to vastus lateralis in subjects with patellofemoral pain syndrome. Archives of Physical Medicine and Rehabilitation, 82, 183189. Cumps, E. (2007). Effect of an exercise programme on intrinsic risk factors of anterior knee pain. In Sports injuries in Flanders: From general epidemiology to prevention strategies in basketball and volleyball (pp. 147165). Doctoral dissertation, Department of Human Physiology and Sports Medicine, Vrije Universiteit Brussel. Cumps, E., Verhagen, E., & Meeusen, R. (2007). Prospective epidemiological study of basketball injuries during one competitive season: Ankle sprains and overuse knee injuries. Journal of Sports Science and Medicine, 6, 204211. Davlin, C. D., Holcomb, W. R., & Guadagnoli, M. A. (1999). The effect of hip position and electromyographic biofeedback training on the vastus medialis oblique/vastus lateralis ratio. Journal of Athletic Training, 34, 342349. de Loes, M., Dahlstedt, L. J., & Thomee, R. R. (2000). A 7-year study on risks and costs of knee injuries in male and female youth participants in 12 sports. Scandinavian Journal of Medicine and Science in Sports, 10, 9097. Duffey, M. J., Martin, D. F., Canon, D. W., Craven, T., & Messier, S. P. (2000). Etiologic factors associated with anterior knee pain in distance runners. Medicine and Science in Sports and Exercise, 32, 18251832. Dursun, N., Dursun, E., & Kilic, Z. (2001). Electromyographic biofeedback-controlled exercise versus conservative care for patellofemoral pain syndrome. Archives of Physical Medicine and Rehabilitation, 82, 16921695.
191
Ekstrand, J., Gillquist, J., & Liljedahl, S. O. (1983). Prevention of soccer injuries: Supervision by doctor and physiotherapist. American Journal of Sports Medicine, 11, 116120. Fairbank, J. C., Pynsent, P. B., Van Poortvliet, J. A., & Phillips, H. (1984). Mechanical factors in the incidence of knee pain in adolescents and young adults. Journal of Bone and Joint Surgery B, 66, 685693. Ferretti, A., Ippolito, E., Mariani, P., & Puddu, G. (1983). Jumpers knee. American Journal of Sports Medicine, 11, 5862. Fyfe, I., & Stanish, W. D. (1992). The use of eccentric training and stretching in the treatment and prevention of tendon injuries. Clinics in Sports Medicine, 11, 601624. Gyf, N. G., & Man, V. Y. (1996). EMG analysis of vastus medialis obliquus and vastus laterlais during static knee extension with different hip and ankle positions. New Zealand Journal of Physiotherapy, 24, 710. Heitkamp, H. C., Horstmann, T., Mayer, F., Weller, J., & Dickhuth, H. H. (2001). Gain in strength and muscular balance after balance training. International Journal of Sports Medicine, 22, 285290. Hertel, J., Eral, J. E., Tsang, K. K., & Miller, S. J. (2004). Combining isometric knee extension exercises with hip adduction does not increase quadriceps EMG activity. British Journal of Sports Medicine, 38, 210213. Hewett, T. E., Stroupe, A. L., Nance, T. A., & Noyes, F. R. (1996). Plyometric training in female athletes: Decreased impact forces and increased hamstring torques. American Journal of Sports Medicine, 24, 765773. Ireland, M. L., Willson, J. D., Ballantyne, B. T., & Davis, I. M. (2003). Hip strength in females with and without patellofemoral pain. Journal of Orthopaedic and Sports Physical Therapy, 33, 671676. Kingma, J. J., de Knikker, R., Wittink, H. W., & Takken, T. (2007). Eccentric overload training in patients with chronic Achilles tendinopathy: A systematic review. British Journal of Sports Medicine, 41, e3. Kujala, U. M., Taimela, S., Antti-Poika, I., Orava, S., Tuominen, R., & Myllynen, D. (1995). Acute injuries in soccer, ice hockey, volleyball, basketball, judo, and karate. British Medical Journal, 311, 14651468. LaBrier, K., & ONeill, D. B. (1993). Patellofemoral stress syndrome: Current concepts. Sports Medicine, 16, 449459. Laprade, J., Culham, E., & Brouwer, B. (1998). Comparison of ve isometric exercises in the recruitment of the vastus medialis oblique in persons with and without patellofemoral pain syndrome. Journal of Orthopaedic and Sports Physical Therapy, 27, 197204. Lian, . B., Engebretsen, L., & Bahr, R. (2005). Prevalence of jumpers knee among elite athletes from different sports: A cross-sectional study. American Journal of Sports Medicine, 33, 561567. Lian, ., Engebretsen, L., Ovrebo, R. V., & Bahr, R. (1996). Characteristics of the leg extensors in male volleyball players with jumpers knee. American Journal of Sports Medicine, 24, 380385. Mascal, C. L., Landel, R., & Powers, C. (2003). Management of patellofemoral pain targeting hip, pelvis, and trunk muscle function: 2 case reports. Journal of Orthopaedic and Sports Physical Therapy, 33, 647660. McConnel, J. (2002). Management of patellofemoral problems. Clinics in Sports Medicine, 21, 363367. Messier, S. P., Davis, S. E., Curl, W. W., Lowery, R. B., & Pack, R. J. (1991). Etiologic factors associated with patellofemoral pain in runners. Medicine and Science in Sports and Exercise, 29, 10081015. Morrison, V., & Bennett, P. (2006). An introduction to health psychology. Harlow, UK: Pearson Prentice Hall.
192
E. Cumps et al.
prevention of anterior knee pain a prospective randomised study. Knee Surgery and Sports Traumatology Arthroscopy, 12, 434439. Verhagen, E. A., Van der Beek, A. J., Bouter, L. M., Bahr, R. M., & van Mechelen, W. (2004). A one season prospective cohort study of volleyball injuries. British Journal of Sports Medicine, 38, 477481. Visnes, H., & Bahr, R. (2007). The evolution of eccentric training as treatment for patellar tendinopathy (jumpers knee) a critical review of exercise programmes. British Journal of Sports Medicine, 41, 217223. Visnes, H., Hoksrud, A., Cook, J., & Bahr, R. (2005). No effect of eccentric training on jumpers knee in volleyball players during the competitive season: A randomised clinical trial. Clinical Journal of Sport Medicine, 15, 227234. Voight, M. L., & Wieder, D. L. (1991). Comparative reex response times of the vastus medialis and the vastus lateralis in normal subjects and subjects with extensormechanism dysfunction. American Journal of Sports Medicine, 10, 131137. Witvrouw, E., Bellemans, J., Lysens, R., Danneels, L., & Cambier, D. (2001). Intrinsic risk factors for the development of patellar tendinitis in an athletic population: A two-year prospective study. American Journal of Sports Medicine, 29, 190 195. Witvrouw, E., Lysens, R., Bellemans, J., Cambier, D., & Vanderstraeten, S. (2000). Intrinsic risk factors for the development of anterior knee pain in an athletic population: A twoyear prospective study. American Journal of Sports Medicine, 28, 480489. Witvrouw, E., Sneyers, C., Lysens, R., Victor, J., & Bellemans, J. (1996). Reex response times of the vastus medialis oblique and vastus lateralis in normal subjects and in subjects with patellofemoral pain syndrome. Journal of Orthopaedic and Sports Physical Therapy, 24, 160165.
Onate, J. A., Guskiewicz, K. M., Marshall, S. W., Giuliani, C., Yu, B., & Garrett, W. E. (2005). Instruction of jump-landing technique using videotape feedback: Altering lower extremity motion patterns. American Journal of Sports Medicine, 33, 831 842. Roush, M. B., Sevier, T. L., Wilson, J. K., Jenkinson, D. M., Helfst, R. H., Gehlsen, G. M., et al. (2000). Anterior knee pain: A clinical comparison of rehabilitation methods. Clinical Journal of Sport Medicine, 10, 2228. Sakai, N., Luo, Z. P., Rand, J.A., & An, K. N. (2000). The inuence of weakness in the vastus medialis oblique muscle on the patellofemoral joint: An in vitro biomechanical study. Clinical Biomechanics, 15, 335339. Salsich, G. B., Brechter, J. H., Farwell, D., & Powers, C. M. (2002). The effects of patellar taping on knee kinematics, and vastus lateralis muscle activity during stair ambulation in individuals with patellofemoral pain. Journal of Orthopaedic and Sports Physical Therapy, 32, 310. Schae, M. D., Requa, R. K., Patton, W. L., & Garrick, J. G. (1990). Injuries in the 1987 national amateur volleyball tournament. American Journal of Sports Medicine, 18, 624631. Sommer, H. M. (1988). Patellar chondropathy and apicitis, and muscle imbalances of the lower extremities in competitive sports. Sports Medicine, 5, 386394. Souza, D. R., & Gross, M. T. (1991). Comparison of vastus medialis obliquus: vastus lateralis muscle integrated electromyographic ratios between healthy subjects and patients with patellofemoral pain. Physical Therapy, 71, 310320. Thomee, R., Augustsson, J., & Karlsson, J. (1999). Patellofemoral pain syndrome: A review of current issues. Sports Medicine, 28, 245262. Thomee, R., Renstrom, P., Karlsson, J., & Grimby, G. (1995). Patellofemoral pain syndrome in young women. Scandinavian Journal of Medicine and Science in Sports, 5, 237251. Van Tiggelen, D., Witvrouw, E., Roget, P., Cambier, D., Danneels, L., & Verdonk, R. (2004). Effect of bracing on the
S-ar putea să vă placă și
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- 32707167Document8 pagini32707167shahrzad_ghazalÎncă nu există evaluări
- 32707167Document8 pagini32707167shahrzad_ghazalÎncă nu există evaluări
- Fighting The Blues: Author Web Site: Journal Web SiteDocument3 paginiFighting The Blues: Author Web Site: Journal Web Siteshahrzad_ghazalÎncă nu există evaluări
- 32707171Document10 pagini32707171shahrzad_ghazalÎncă nu există evaluări
- Sensorimotor Impairments and Strategies in Adults With Intellectual DisabilitiesDocument15 paginiSensorimotor Impairments and Strategies in Adults With Intellectual Disabilitiesshahrzad_ghazalÎncă nu există evaluări
- Behavior, 32,: Assessing "Short" and "Core" FlowDocument3 paginiBehavior, 32,: Assessing "Short" and "Core" Flowshahrzad_ghazalÎncă nu există evaluări
- How Spreading The Forefeet Apart Influences Upright Standing ControlDocument14 paginiHow Spreading The Forefeet Apart Influences Upright Standing Controlshahrzad_ghazalÎncă nu există evaluări
- Football in The Reconstruction of The Gender Order in Japan: Soccer & SocietyDocument16 paginiFootball in The Reconstruction of The Gender Order in Japan: Soccer & Societyshahrzad_ghazalÎncă nu există evaluări
- Nutrition, The Brain and Prolonged Exercise: Phil WatsonDocument12 paginiNutrition, The Brain and Prolonged Exercise: Phil Watsonshahrzad_ghazalÎncă nu există evaluări
- Football in The Reconstruction of The Gender Order in Japan: Soccer & SocietyDocument16 paginiFootball in The Reconstruction of The Gender Order in Japan: Soccer & Societyshahrzad_ghazalÎncă nu există evaluări
- Analysis of Goalkeepers' Defence in The World Cup in Korea and Japan in 2002Document10 paginiAnalysis of Goalkeepers' Defence in The World Cup in Korea and Japan in 2002shahrzad_ghazalÎncă nu există evaluări
- Call For Papers: ISSN 1477-5085 (Print) /ISSN 1029-5399 (Online) # 2008 Taylor & Francis DOI: 10.1080/14775080802208526Document2 paginiCall For Papers: ISSN 1477-5085 (Print) /ISSN 1029-5399 (Online) # 2008 Taylor & Francis DOI: 10.1080/14775080802208526shahrzad_ghazalÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Pumpkin TakoshiDocument22 paginiPumpkin TakoshiSudhanshu NoddyÎncă nu există evaluări
- Preterm Prelabour Rupture of MembranesDocument12 paginiPreterm Prelabour Rupture of MembranesSeptiany Indahsari DjanÎncă nu există evaluări
- Polysaccaride Krestin (PSK)Document5 paginiPolysaccaride Krestin (PSK)Andromeda AbrahamÎncă nu există evaluări
- Advanced Handbook of Systemic Lupus ErythematosusDocument179 paginiAdvanced Handbook of Systemic Lupus ErythematosusCésar CuadraÎncă nu există evaluări
- U.S. Fund For UNICEF Annual Report 2010Document44 paginiU.S. Fund For UNICEF Annual Report 2010U.S. Fund for UNICEF100% (1)
- 24 Bio Fertilization of BananaDocument6 pagini24 Bio Fertilization of Bananamiceli57Încă nu există evaluări
- Pulmonary Hypertension: Dya Andryan MD Sumedang General HospitalDocument32 paginiPulmonary Hypertension: Dya Andryan MD Sumedang General HospitalDya AndryanÎncă nu există evaluări
- 1 To 3Document49 pagini1 To 3Vikki NandeshwarÎncă nu există evaluări
- Chemo Stability Chart AtoK 1jun2016Document46 paginiChemo Stability Chart AtoK 1jun2016arfitaaaaÎncă nu există evaluări
- Cytogenetics - Prelim TransesDocument15 paginiCytogenetics - Prelim TransesLOUISSE ANNE MONIQUE L. CAYLOÎncă nu există evaluări
- Sino-Nasal Outcome Test (SNOT-22) Questionnaire: Patient's Name Date DOBDocument2 paginiSino-Nasal Outcome Test (SNOT-22) Questionnaire: Patient's Name Date DOBIchsanJuliansyahÎncă nu există evaluări
- PrioritizationDocument4 paginiPrioritizationJhennie EyescandieÎncă nu există evaluări
- SNB Exam Sample Question Paper 2Document19 paginiSNB Exam Sample Question Paper 2Ketheesaran LingamÎncă nu există evaluări
- Escala de Apatia de StarksteinDocument6 paginiEscala de Apatia de StarksteinVanessa HernandezÎncă nu există evaluări
- Malawi Clinical HIV Guidelines 2019 Addendumversion 8.1Document28 paginiMalawi Clinical HIV Guidelines 2019 Addendumversion 8.1INNOCENT KHULIWAÎncă nu există evaluări
- Nail Disorder and DiseasesDocument33 paginiNail Disorder and Diseasesleny90941Încă nu există evaluări
- Roadmap For TelemedicineDocument48 paginiRoadmap For TelemedicinePradip Gupta100% (2)
- THE CLAT POST March 2020Document30 paginiTHE CLAT POST March 2020Mukund GargÎncă nu există evaluări
- HEX PG SyllabusDocument124 paginiHEX PG SyllabusJegadeesan MuniandiÎncă nu există evaluări
- CHN - 1Document23 paginiCHN - 1Raagul SaravanaKumarÎncă nu există evaluări
- Egger & Angold, 2006 Disorders - DiscussionDocument25 paginiEgger & Angold, 2006 Disorders - DiscussionAlkistis MarinakiÎncă nu există evaluări
- The Analysis and Reflection On That Sugar FilmDocument2 paginiThe Analysis and Reflection On That Sugar FilmkkkkÎncă nu există evaluări
- Hypnosis For Irritable Bowel SyndromeDocument3 paginiHypnosis For Irritable Bowel SyndromeImam Abidin0% (1)
- Tamiflu and ADHDDocument10 paginiTamiflu and ADHDlaboewe100% (2)
- Music Therapy in Nursing HomesDocument7 paginiMusic Therapy in Nursing Homesapi-300510538Încă nu există evaluări
- Formulation and Evaluation of Herbal Lip Rouge.: Research ArticleDocument5 paginiFormulation and Evaluation of Herbal Lip Rouge.: Research ArticleTynÎncă nu există evaluări
- Program Implementation With The Health Team: Packages of Essential Services For Primary HealthcareDocument1 paginăProgram Implementation With The Health Team: Packages of Essential Services For Primary Healthcare2A - Nicole Marrie HonradoÎncă nu există evaluări
- Beauty Care 1st Summative TestDocument4 paginiBeauty Care 1st Summative TestLlemor Soled SeyerÎncă nu există evaluări
- Deadly Deception - Robert WillnerDocument303 paginiDeadly Deception - Robert Willnerleocarvalho001_60197100% (5)
- Complications and Failures of ImplantsDocument35 paginiComplications and Failures of ImplantssavÎncă nu există evaluări