Documente Academic
Documente Profesional
Documente Cultură
What Is A Subchorionic Hemorrhage
Încărcat de
Budo LataquinDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
What Is A Subchorionic Hemorrhage
Încărcat de
Budo LataquinDrepturi de autor:
Formate disponibile
What is a Subchorionic Hemorrhage? Subchorionic Hemorrhage is bleeding behind the placenta, often caused by a clot.
In most cases, this clot will dissolve away, resolving the problem and allowing the pregnancy to progress normally. It may take several weeks for this clot to dissolve. Treatment for a Subchorionic hemorrhage is typically bed rest. Rarely, the clot dissects between the placenta and the attachment to mother. This may lead to placental abruption. Risk factors that may increase the chance of experiencing this include high blood pressure, smoking and cocaine use. Symptoms may include: contractions that don't stop pain in the uterus tenderness in the abdomen over the uterus vaginal bleeding
http://www.amazingpregnancy.com/pregnancy-articles/191.html What is Diabetes Mellitus Type 2?
Type 2 Diabetes Mellitus is a chronic metabolic syndrome defined by resistance to the hormone insulin. This leads to inappropriate hyperglycaemia(increased blood sugar levels) and deranged metabolism of carbohydrate, fats and proteins. Insulin is a key metabolic hormone secreted by the pancreas. Insulin exerts its actions in the liver and peripheral tissues such as muscle and fat. In type 2 diabetes mellitus, relative insulin deficiency usually occurs because of resistance to the actions of insulin in muscle, fat, and the liver. This abnormality results in decreased glucose transport in muscle, increased liver glucose production, and increased breakdown of fat. Type 2 diabetes mellitus is also known as Non Insulin Dependent Diabetes Mellitus (NIDDM). This name is no longer used as some patients with type 2 diabetes mellitus do require insulin treatment in advanced stages. Risk Factors for Diabetes Mellitus Type 2 In type 2 diabetes, peripheral resistance to the actions of insulin is combined with a pancreatic secretory deficiency of varying severity. Insulin resistance means the body is unable to take glucose (sugar) up into cells. Normally, the body would compensate for this by producing increased amounts of insulin, but in type 2 diabetes mellitus the pancreas cannot respond. This means not enough insulin is produced, and excess sugar remains in the bloodstream (hyperglycemia) instead of being taken up into cells and used for energy. Type 2 diabetes is partly a genetic disease and partly a lifestyle disease. While some people have a genetic predisposition to diabetes, they may not actual develop the disease without 'lifestyle' triggers such as excess fat and sugar intake or inadequate physical exercise. While there is no single cause for developing Type 2 diabetes, there are well-known risk factors. Some of these can be changed (avoidable) and some cannot (unavoidable).
Unavoidable risk factors A family history of diabetes. Identical twins of an affected person have more than 80% chance of developing diabetes, and 25% of patients have an affected first degree relative. Age - people greater than 45 years have higher rates of disease. The risk increases as we get older. Ethnic background - Aboriginal or Torres Strait Islander men, and people with Melanesian, Polynesian, Chinese or Indian background are more likely to develop type 2 diabetes mellitus. Having Polycystic Ovarian Syndrome or a history of gestational diabetes during pregnancy. Low birth weight is thought to predispose to diabetes due to poor beta-cell development and function. Avoidable risk factors Obesity (Click the relevent links to explore possible treatment options to combat obesity: meal replacement programs, lifestyle changes, drugs and surgery). Physical inactivity High blood pressure Diet Cholesterol Smoking Progression of Diabetes Mellitus Type 2 Type 2 diabetes mellitus may have an onset over several months, or be asymptomatic and be detected on a routine blood test. It is generally not recognised and diagnosed until the patient seeks health care for another problem. Some common presenting symptoms of type 2 diabetes mellitus include: Excessive thirst. Increased urine output (polyuria). Hunger. Weight loss or gain. Slow healing or frequent infections. Blurred vision. Dry eyes Headaches. Numbness, tingling or burning of the feet (peripheral neuropathy). Without treatment patients may develop acute complications due to dehydration (HONKC, see below) and long-term complications will develop much more rapidly. The main acute complication is hyperosmolar nonketotic coma (HONKC), sometimes also known as hyperosmolar hyperglycaemic nonketotic coma (HHNC). This is a condition that develops over several days in poorly controlled diabetes involving high blood glucose and potentially lethal secondary dehydration and electrolyte disturbances. Long-term complications include: Microvascular disease: Diabetic retinopathy (eye disease). Diabetic nephropathy (kidney disease). Peripheral neuropathy and autonomic neuropathy (nerve disease). Impotence (difficulty maintaining an erection). Macrovascular disease - i.e. atherosclerosis (hardening of the arteries) causing: Coronary artery disease or heart attack. Cerebrovascular disease (stroke). Peripheral vascular disease - potentially causing gangrene and leading to need for leg or toe amputation. Men are particularly susceptible to diabetic complications and often have higher rates of mortality than females. Symptoms of Diabetes Mellitus Type 2 Diabetes can be easily diagnosed if you present with the classic symptoms of: Thirst. Polyuria- Passing urine often or waking at night several times to pass urine (nocturia). Fatigue.
Hunger. Weight loss. However, many patients with diabetes remain assymptomatic for many years but are still subject to the damaging effects of high blood sugars. Unlike type 1 diabetes which tends to present acutely, type 2 diabetes presents gradually over several years. At the time of diagnosis of type 2 diabetes, you may already have several complications of the disease, such as heart or eye problems. You may have noticed blurring of your vision, pins and needles in the feet (due to damage to the nerves) and recurrent infections. Diabetes or impaired glucose tolerance may be detected on routine blood tests as part of a general health check-up or investigation for other symptoms or diseases. If you are obese, suffer from high blood pressure, have a family history of diabetes, have high cholesterol or come from a high risk population (e.g. Aboriginal background) it is important that you get tested for diabetes. Clinical Examination of Diabetes Mellitus Type 2 Your doctor will perform a careful examination mainly looking for the various complications of diabetes. This will include cardiovascular, neurological and retinal (eye) examinations. In the early stages of disease your examination may be completely normal, however as the duration and severity of disease progressed it is likely you will have some end-organ damage. Your doctor will use a special device (called an opthalmoscope) to look at the back of your eye (retina). Here the doctor may see various degrees of diabetic retinopathy which basically represents damage to and leaking from the small vessels at the back of your eyes. Often cataracts (white opacities) may also be found in the lens. These develop because the excess sugar upsets the normal consistency of the lens. You may also have dry eyes. Cardiovascular exam may reveal signs of heart failure due to ischaemic heart disease. You may have an abnormal heart rhythm or crackles at the base of your lungs from accumulated fluid. In addition, your blood pressure will be checked and your doctor may perform an ECG to detect any obvious ischaemic changes. Leg examination may reveal diabetic ulcers (on pressure points in the feet) and peripheral vascular disease (poor peripheral pulses and circualtion), diabetic foot disease and trophic skin changes and skin infections. Your doctor will also test the nerves in your legs. You may have the classic 'glove and stocking' neuropathy which refers to reduced sensation in the distal portions of your limbs (i.e. where gloves and stockings are usually positioned). The neuropathy starts distally and progresses further up the limb as the condition worsens. Your sensations of vibration (tested with a tuning fork placed on the bone) and propioception (recognition of joint space position, tested by wiggling your toe or finger with your eyes closed) tend to be affected first. In advanced cases you may have severe pain and impaired motor function. Finally your doctor may request a urine sample to measure the amount of protein present. This reflects your kidney function as damaged kidneys tend to leak protein. How is Diabetes Mellitus Type 2 Diagnosed? Type 2 diabetes mellitus is diagnosed when any of the following criteria are reached: Symptoms of diabetes are present (increased urination, increased thirst or weight loss) with a random plasma glucose (RPG) level of >11.0mmol/L Fasting plasma glucose (FPG) >7.0mmol/L Oral glucose tolerance test (OGTT) 2 hour plasma glucose >11.1mmol/L Patients who do not reach these criteria may still be classified as having impaired fasting glucose (IFG) or impaired glucose tolerance (IGT) on the basis of fasting blood glucose or oral glucose tolerance test results. These patients are at increased risk of developing type 2 diabetes mellitus. Other tests which may be ordered include: Glycosylated haemoglobin (HbA1c): this test is not used as a diagnostic or screening test for diabetes but may be used in the ongoing monitoring of diabetes. HbA1c reflects blood glucose levels over the past 2-3 months. Results >7% suggest poor blood glucose control and correlate with poor clinical outcomes. When a diagnosis of diabetes mellitus is first made, several tests are often ordered to check for organ function and exclude complications of diabetes. These may include: Full blood count. Urea and electrolytes (potentially showing kidney impairment). Urinalysis to check for infection or protein loss through the kidneys. Liver function tests.
Chest x-ray. ECG. Blood lipids (including cholesterol). Prognosis of Diabetes Mellitus Type 2 Diabetes is associated with a significant long-term risk of early mortality and morbidity. Heart disease (heart attacks 3-5 times more likely), peripheral vascular disease (amputation 50 times more likely), and stroke (twice as likely) are the major causes of death in patients over the age of 50. In addition, diabetic eye disease and renal failure due to diabetic nephropathy are important causes of morbidity. In addition, renal failure is potentially fatal. However, several large trials have proven that the risks of longterm complications from diabetes can be reduced with good blood glucose (sugar) control. The acute complication of hyperosmolar non-ketotic coma has a mortality approaching 50% due to the fact that it affects elderly patients with extensive medical problems. Hypoglycaemia due to inappropriate use of insulin or as a side-effect of medications is also potentially fatal.
S-ar putea să vă placă și
- 8 Dayz Hunza and Skardu'Document8 pagini8 Dayz Hunza and Skardu'Hasnain AliÎncă nu există evaluări
- Type 2 Diabetes MellitusDocument6 paginiType 2 Diabetes MellitusJoy NisoladaÎncă nu există evaluări
- Diabetes MellitusDocument11 paginiDiabetes MellitusChristinaRegatilloÎncă nu există evaluări
- Diebetes MellitusDocument16 paginiDiebetes Mellitusbayiyitz0003Încă nu există evaluări
- Diabetes OverviewDocument38 paginiDiabetes OverviewKye GarciaÎncă nu există evaluări
- Case Study in DMDocument34 paginiCase Study in DMKathrina Marie B. BinaraoÎncă nu există evaluări
- Case StudDocument5 paginiCase StudmjbscityÎncă nu există evaluări
- Type 2 DiabetesDocument9 paginiType 2 DiabetesLevi MwendaÎncă nu există evaluări
- Diabetes MellitusDocument8 paginiDiabetes MellitusJaja RamosÎncă nu există evaluări
- Diabetes MellitusDocument8 paginiDiabetes MellitusJaja RamosÎncă nu există evaluări
- Diabetes MellitusDocument8 paginiDiabetes MellitusJaja RamosÎncă nu există evaluări
- Diabetes: Oral Health TopicsDocument9 paginiDiabetes: Oral Health TopicsAndrei StamateÎncă nu există evaluări
- IntroductionDocument13 paginiIntroductionSaadÎncă nu există evaluări
- Type2 Diabetes HandoutDocument1 paginăType2 Diabetes Handouthendra_darmawan_4Încă nu există evaluări
- Signs and SymptDocument14 paginiSigns and SymptVealma sikaÎncă nu există evaluări
- Case Study On Diabetes MellitusDocument12 paginiCase Study On Diabetes Mellitusferdz02Încă nu există evaluări
- What Is Diabetes Mellitus?Document5 paginiWhat Is Diabetes Mellitus?Moħắmẻd ŘắắfatÎncă nu există evaluări
- Type 1 DiabetesDocument11 paginiType 1 DiabetesLyne Paggic PabloÎncă nu există evaluări
- Biology Investigatory Project On Diabetes Mellitus by Mahima MahapatraDocument31 paginiBiology Investigatory Project On Diabetes Mellitus by Mahima Mahapatraalex david100% (14)
- Diabetes Overview: Aerobic Exercise ClassDocument13 paginiDiabetes Overview: Aerobic Exercise Classpak3maÎncă nu există evaluări
- Biologyinvestigatoryprojectondiabetesmellitusbymahimamahapatra 211028153449Document30 paginiBiologyinvestigatoryprojectondiabetesmellitusbymahimamahapatra 211028153449SaadÎncă nu există evaluări
- Jaya's BiochemistryDocument13 paginiJaya's BiochemistryJKKP HPJBÎncă nu există evaluări
- Bka Case FinalDocument26 paginiBka Case FinalJayson SorianoÎncă nu există evaluări
- Diabetes Mellitus, Disorder Of: Institute For BiotechnologyDocument10 paginiDiabetes Mellitus, Disorder Of: Institute For BiotechnologyAndre Jonathan Siàńsàkà IIÎncă nu există evaluări
- 06.disorder of Carbohydrate MetabolismDocument47 pagini06.disorder of Carbohydrate MetabolismRizka NizarÎncă nu există evaluări
- Diabetes For Dentists: DR Jackie Elliott Clinical Lecturer in DiabetesDocument37 paginiDiabetes For Dentists: DR Jackie Elliott Clinical Lecturer in DiabetesKevalChavdaÎncă nu există evaluări
- DiabetesDocument34 paginiDiabetesqurat-ul-ain.sonÎncă nu există evaluări
- Definition and Diagnostic Criteria For Diabetes Mellitus and Other Categories of Glucose IntoleranceDocument4 paginiDefinition and Diagnostic Criteria For Diabetes Mellitus and Other Categories of Glucose Intolerancevai2Încă nu există evaluări
- 10 High Blood Sugar Symptoms, Signs, Causes, and TreatmentDocument8 pagini10 High Blood Sugar Symptoms, Signs, Causes, and Treatmentranjit__kayalaÎncă nu există evaluări
- Diabetes MellitusDocument13 paginiDiabetes Mellitusdreneavalentinstefan100% (1)
- Diabetes WfaDocument14 paginiDiabetes Wfaapi-611702624Încă nu există evaluări
- DIABETES CorrectedDocument16 paginiDIABETES CorrectedBlaise PascalÎncă nu există evaluări
- Type 2 DiabetesDocument5 paginiType 2 DiabetesNuno Sa PunsoÎncă nu există evaluări
- DiabetesDocument14 paginiDiabetesBocah JomloÎncă nu există evaluări
- Diabetes Diabetes InformationDocument15 paginiDiabetes Diabetes InformationbalatnplÎncă nu există evaluări
- Diabetes Types: Aseel Saleh Al-OmariDocument11 paginiDiabetes Types: Aseel Saleh Al-OmariHasan AlomariÎncă nu există evaluări
- Diabetes and ExerciseDocument23 paginiDiabetes and ExerciseApurba MukherjeeÎncă nu există evaluări
- Diabetes Mellitus IIDocument20 paginiDiabetes Mellitus IIMa R Dy100% (1)
- DiabetesDocument4 paginiDiabetesTuTitÎncă nu există evaluări
- What Is Diabetes Mellitus?Document9 paginiWhat Is Diabetes Mellitus?Nhoel RsÎncă nu există evaluări
- DM Case StudyDocument39 paginiDM Case StudyShella Mae Usquisa100% (1)
- Diabetes MellitusDocument34 paginiDiabetes MellitusKobby AmoahÎncă nu există evaluări
- Type 2 Diabetes: Learn The Warning Signs: Nov 2010 - From: (Free PDF - Manajemen Modern Dan Kesehatan Masyarakat)Document6 paginiType 2 Diabetes: Learn The Warning Signs: Nov 2010 - From: (Free PDF - Manajemen Modern Dan Kesehatan Masyarakat)Deka VeritasÎncă nu există evaluări
- 3 Case Study On DM p.35 1Document44 pagini3 Case Study On DM p.35 1Nina Fatima AllamÎncă nu există evaluări
- Makalah Penyakit DiabetesDocument6 paginiMakalah Penyakit DiabetesTaju'al Taju'alÎncă nu există evaluări
- DM PresentationDocument28 paginiDM PresentationmymommywowÎncă nu există evaluări
- Classification: LiverDocument20 paginiClassification: LivertermskipopÎncă nu există evaluări
- Diabetes MellitusDocument24 paginiDiabetes MellitusAnsh Gaurav KumarÎncă nu există evaluări
- Diabetes MellitusDocument11 paginiDiabetes MellitusSallieÎncă nu există evaluări
- Definition of Diabetes Mellitus (DM)Document12 paginiDefinition of Diabetes Mellitus (DM)Romarc Owen CorpuzÎncă nu există evaluări
- Diabetes Mellitus: Signs and SymptomsDocument2 paginiDiabetes Mellitus: Signs and SymptomsJosbel Alejandro RodríguezÎncă nu există evaluări
- About Diabetes: Type 1 Diabetes Is Sometimes Called Insulin-Dependent, Immune-Mediated orDocument5 paginiAbout Diabetes: Type 1 Diabetes Is Sometimes Called Insulin-Dependent, Immune-Mediated oredysutiarsoÎncă nu există evaluări
- DP DP DPDocument23 paginiDP DP DPAkshay VenkyÎncă nu există evaluări
- DiabetesDocument10 paginiDiabetesFatima El HassouniÎncă nu există evaluări
- Grp.10 DiabetesDocument15 paginiGrp.10 DiabetesVanessa JanneÎncă nu există evaluări
- Smallseotools 1597128331Document3 paginiSmallseotools 1597128331Muhammad RazaÎncă nu există evaluări
- Diabetus MellitusDocument4 paginiDiabetus Mellitusგიორგი ანთაძეÎncă nu există evaluări
- Diabetes PPT FianlDocument31 paginiDiabetes PPT FianlUqba MishalÎncă nu există evaluări
- Diabetes Mellitus HospitalDocument29 paginiDiabetes Mellitus HospitalgegeÎncă nu există evaluări
- Single ResultDocument2 paginiSingle ResultHibaBsharatÎncă nu există evaluări
- Tips On Surviving Floor RotationsDocument22 paginiTips On Surviving Floor RotationsYucheng TangÎncă nu există evaluări
- Case Study Presentation On Diabetic Foot UlcerDocument61 paginiCase Study Presentation On Diabetic Foot UlcerBindu GC100% (1)
- Management of Anesthesia: Diabetes MellitusDocument29 paginiManagement of Anesthesia: Diabetes MellitusHari PrasadÎncă nu există evaluări
- GESTASIONAL DIABETES MELLITUS SimposiumDocument18 paginiGESTASIONAL DIABETES MELLITUS SimposiumHabiby Habibaty QolbiÎncă nu există evaluări
- Nursing Drug StudyDocument5 paginiNursing Drug StudyArah Mae Dasal ArricivitaÎncă nu există evaluări
- Human Biology (Biologi Manuasia) : Prof Madya Dr. Mohamad Aziz DollahDocument29 paginiHuman Biology (Biologi Manuasia) : Prof Madya Dr. Mohamad Aziz DollahQisNani NorainiÎncă nu există evaluări
- Personal Fat ThresholdDocument6 paginiPersonal Fat ThresholdPROJETO PRI E GABIÎncă nu există evaluări
- Nursing Care PlanDocument26 paginiNursing Care PlanDinda MaretaÎncă nu există evaluări
- Chapter 9 - Nancy NG - Gestational DiabetesDocument6 paginiChapter 9 - Nancy NG - Gestational DiabetesEunice Cortés100% (1)
- Oral Diabetic MedicationDocument26 paginiOral Diabetic MedicationTaimoor BaigÎncă nu există evaluări
- A Review of The Ef Ficacy and Safety of Banaba (Lagerstroemia Speciosa L.) and Corosolic AcidDocument8 paginiA Review of The Ef Ficacy and Safety of Banaba (Lagerstroemia Speciosa L.) and Corosolic AcidLyka MahrÎncă nu există evaluări
- Quinolizidine Alkaloids Isolated From Lupinus Species Enhance Insulin SecretionDocument4 paginiQuinolizidine Alkaloids Isolated From Lupinus Species Enhance Insulin SecretionLeonardo C.Încă nu există evaluări
- Diabetic Emergencies in Small AnimalsDocument17 paginiDiabetic Emergencies in Small Animalsdia_dianneÎncă nu există evaluări
- Sandler - Diet Prevents PolioDocument69 paginiSandler - Diet Prevents PolioIyemhetepÎncă nu există evaluări
- Liver, Bile, & Pancreatic Physiology PDFDocument6 paginiLiver, Bile, & Pancreatic Physiology PDFAdvin BurkeÎncă nu există evaluări
- A To Z PharmacologyDocument41 paginiA To Z PharmacologyMaddy Huseynl100% (1)
- Hospital Training Report Part-I (BP509P) B.Pharm 5 Semester Session 2021-22Document39 paginiHospital Training Report Part-I (BP509P) B.Pharm 5 Semester Session 2021-22Prakash Kori83% (18)
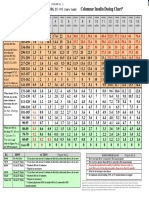
- Columnar Insulin Dosing Chart : (1 ML 1 Unit)Document1 paginăColumnar Insulin Dosing Chart : (1 ML 1 Unit)Philippe KinnaerÎncă nu există evaluări
- Aspiration PneumoniaDocument46 paginiAspiration Pneumoniayasmine abdelkarimÎncă nu există evaluări
- Mahogany Seeds For Health BenefitsDocument14 paginiMahogany Seeds For Health BenefitsGreg PalmaÎncă nu există evaluări
- Clinical Chemistry Notes With BlanksDocument34 paginiClinical Chemistry Notes With Blanksepson printerÎncă nu există evaluări
- Acm 20072Document16 paginiAcm 20072numbnessÎncă nu există evaluări
- Book Lab Tests in India - Find Diagnostic Centers Near Your Place - MedlifeDocument1 paginăBook Lab Tests in India - Find Diagnostic Centers Near Your Place - Medlifegunjali daveÎncă nu există evaluări
- Case QuestionsDocument6 paginiCase Questionsapi-353723892Încă nu există evaluări
- Glucose HomeostasisDocument37 paginiGlucose HomeostasisBryan DocallasÎncă nu există evaluări
- Metformin Ameliorates Diabetes With Metabolic Syndrome Induced Changes in Experimental RatsDocument11 paginiMetformin Ameliorates Diabetes With Metabolic Syndrome Induced Changes in Experimental RatsGuadalupe Hernandez EquihuaÎncă nu există evaluări
- Brochure Ionogramme Easylyte Marque - MedicaDocument6 paginiBrochure Ionogramme Easylyte Marque - MedicaFayssal BenfoddaÎncă nu există evaluări
- Abstrac 2222Document19 paginiAbstrac 2222josephmainam9Încă nu există evaluări
- Neonatal Hyperglycemia1Document17 paginiNeonatal Hyperglycemia1Abhinav Mitra VatsÎncă nu există evaluări
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 4 din 5 stele4/5 (6)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe la EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsÎncă nu există evaluări
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeEvaluare: 2 din 5 stele2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (24)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe la EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe la EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisEvaluare: 4.5 din 5 stele4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedEvaluare: 5 din 5 stele5/5 (80)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDe la EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDEvaluare: 5 din 5 stele5/5 (1)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!De la EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Evaluare: 5 din 5 stele5/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDe la EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsEvaluare: 5 din 5 stele5/5 (1)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDe la EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisEvaluare: 4 din 5 stele4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.De la EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Evaluare: 4.5 din 5 stele4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerDe la EverandGut: the new and revised Sunday Times bestsellerEvaluare: 4 din 5 stele4/5 (392)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe la EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityEvaluare: 4 din 5 stele4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDe la EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsEvaluare: 4.5 din 5 stele4.5/5 (169)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDe la EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryEvaluare: 4 din 5 stele4/5 (44)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDe la EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessEvaluare: 4.5 din 5 stele4.5/5 (328)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe la EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsEvaluare: 3.5 din 5 stele3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDe la EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisEvaluare: 3.5 din 5 stele3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningDe la EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningEvaluare: 4 din 5 stele4/5 (3)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)De la EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Evaluare: 4 din 5 stele4/5 (378)
- To Explain the World: The Discovery of Modern ScienceDe la EverandTo Explain the World: The Discovery of Modern ScienceEvaluare: 3.5 din 5 stele3.5/5 (51)
- The Marshmallow Test: Mastering Self-ControlDe la EverandThe Marshmallow Test: Mastering Self-ControlEvaluare: 4.5 din 5 stele4.5/5 (58)