Documente Academic
Documente Profesional
Documente Cultură
Effects of Pesticides On Male Reproductive Functions
Încărcat de
Dr. Attalla F. El-kottDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Effects of Pesticides On Male Reproductive Functions
Încărcat de
Dr. Attalla F. El-kottDrepturi de autor:
Formate disponibile
IJMS Vol 30, No 4, December 2005
Review Article
Effects of Pesticides on Male Reproductive Functions
J. Srinivasa, P. Maxim , J. Urban, 2 A. DSouza
1
Abstract
Exposure to pesticides could be one of the contributing cause to the falling sperm counts and rising levels of male infertility. Adverse effects of pesticides in the environment first received widespread attention in the 1960s. However, only recently it has been postulated that long term, low exposure of these chemicals are increasingly linked to human health effects such as immuno-suppression, endocrine disruption, reproductive abnormalities and cancer. This article critically reviewed the epidemiological studies of reproductive toxicity of different pesticides in males. According to previous studies it is shown that exposure to pesticides was significantly associated with sperm levels well below the limit for male fertility. No largescale studies assessing pesticide exposure and its relationship to infertility have been done. To overcome the difficulties in interpretation and to reach strong conclusions, future studies on human male reproductive effects of different types of pesticides should consider several methodological problems. So, we conclude integrated studies considering many factors are warranted to draw definite conclusion and also in the view of adverse health effects observed to some extent in workers with few pesticides, it is necessary now to find out ecologically sound alternatives to pesticides and also to educate the workers/farmers about the safe use of these pesticides to reduce reproductive health risk associated with exposure. Iran J Med Sci 2005; 30(4): 153-159.
Keywords pesticides sperm count male reproductive functions Introduction cientists studying the impact of man-made chemicals on human health, claim human males will be infertile by the middle of the next century if present industrial trends are maintained. The culprits are the chemicals which have the ability to mimic hormones, particularly the female sex hormone estrogen-are widespread in society and include pesticides (such as DDT), industrial chemicals (such as PCBs), and environmental pollutants such as dioxin and human therapeutics such as anticancer drugs.1,2 Most, though not all, of the estrogen-mimicking chemicals involve chlorine. Several research studies have indicated that sperm counts have been in decline for decades and scientists say modern lifestyles and contacts with chemicals are a contributing factor.3 Exposure to pesticides is just one of the reasons for this decline. Mothers can absorb these chemicals and pass on their destructive properties through the womb to the unborn
Department of Medical Bioscience, Monash University Malaysia, 46150 Petaling Jaya, Malaysia. 1 Wipro Technologies, Bangalore, India 2 School of Medicine, University Malaysia Sabah, Kota Kinabalu, Sabah, Malaysia Correspondence: Jayachandra Srinivasa MD, Department of Medical Bioscience, Monash University of Malaysia, No 2, Jalan Kolej Bandar Sunway 46150 Petaling Jaya, Malaysia. Tel: +60 3 56360600 Fax: +60 3 56360622 E-mail: sjayacha@monash.edu.my
Iran J Med Sci December 2005; Vol 30 No 4 153
J. Srinivasa, P. Maxim, J. Urban, A. DSouza
child or through breastfeeding to the infant. Although, human is not the unique target which is affected by these agents, many birds and animals in the wild have displayed problems. Birds that refuse to court each other nest or raise their young, female gulls nesting with other females and alligators suffering reproductive problems. Not only have scientists collected evidences that human sperm production has declined over the last half century, but the list of pesticides known to disrupt sperm production or male hormones continue to hamper. So this article aims to review the epidemiological studies of reproductive toxicity induced by different pesticides in males and to suggest possible further research in this field. Declining Sperm Counts In 1992, four Danish scientists published a research study suggesting that sperm counts have declined about 50 percent since 1940 worldwide.4 The study analyzed the results of over 60 studies of sperm counts published between 1938 and 1991 as a statistical analysis that linked results of a large number of independent studies, "meta-analysis".4 Using a model which assumed that sperm counts changes over time in a linear way, the results of the meta-analysis indicated average sperm counts declined from 113 million to 66 million per ml of semen during the half century (Fig 1).1 These studies were reported from different countries around the world.
million per ml between 1977 and 1994.5 Similarly, another study demonstrated that median sperm count among sperm donors had declined about 40 percent in men born in the 1940s in comparison with that born in the late 1960s.6 It was reported that at a sperm bank, mean sperm counts among donors declined by about two percent per year from 1973 to 1992, for a total decline of 32 percent.7 Perhaps of greater concern, these studies found that other measures of sperm quality also showed changes from the normal trend,8 both the volume of semen produced and the vigor of the sperm declined. Carlsen found that semen volume decreased about 20 percent.4 In addition, the proportion of men with sperm counts below 20 million per ml tripled.4 Another study found that both the proportion of abnormal sperm and their mobility decreased during the last 20 years.5 As well, another study had similar, and just as unsettling results.7 Several researchers felt Carlsen's results could be a statistical artifact, or caused by changes in sperm counting equipments. A study pointed out that the data used by Carlsen et al. could be analyzed with different statistical models. The three models that seemed to fit the data best showed a 50 percent decline around 1965, but a constant or slightly increasing sperm count in the years since 1970. In summary, there is a controversy in the scientific world about the decline in human sperm count during the past 50 years based on different studies.9-11 Causes of decline in sperm counts Studies of sperm counts over time leave a critical question unanswered. It is important to know what could account for a precipitous decline in sperm production by otherwise healthy men. Carlsen suggested that environmental causes, particularly those toxins that could affect human hormone systems, were likely.4 Another study developed a more specific hypothesis, and suggested that the decline "is the result of endocrine changes in fetal/ prepubertal life 12 prior to birth or during childhood". In this study, it was hypothesized that this complex system might be disrupted before birth or during childhood by substances acting like natural hormones resulting a permanent impairment of the reproductive system.12 In particular, it was hypothesized that hormone disruption at a sensitive time of development may block the development of Sertoli cells, cells within the testes that "nurse" sperm cells as they develop. The number of Sertoli cells sets a cap on the number of sperm, which a man is able to produce; therefore, a chemical exposure that blocked
Fig 1: Linear regression of mean sperm density reported in 61 publications (represented by circles whose area is proportional to the logarithm of the number of subjects in study), each weighted according to number of subjects, 1 1938 to 1990. Data from Carlsen et al.
In this line, three other studies have found similar declines in sperm counts in smaller groups of men. It is found that sperm count among sperm donors had declined about 10
154 Iran J Med Sci December 2005; Vol 30 No 4
Effects of pesticides on male reproductive functions
hormone involved with Sertoli cell development would irreversibly limit sperm production.12 Sharpe et al. thought that FSH and estrogen are important in determining adult sperm production.12 Their relevance to sperm production is that FSH in juvenile mammals promotes multiplication of the Sertoli cells. Without enough FSH, fewer Sertoli cells are produced. Levels of FSH are regulated by estrogens; higher levels of estrogen result in lower levels of FSH. Therefore, it was hypothesized that synthetic chemicals acting like estrogen might lower the level of FSH, resulting in fewer Sertoli cells and permanently decrease the sperm production.12 A study concerned mother rats that drank water contaminated with two synthetic chemicals, such as octyl phenol and butyl benzyl phethalate, which are known to act like estrogen.12 The rats used in the study were pregnant or nursing; the study spanned the interval when their male offspring would be developing Sertoli cells. The results fit the mentioned hypothesis perfectly to say that sperm production was reduced (10 to 20 percent) in the offspring of the rats drinking contaminated water and the number of Sertoli cells (as estimated by testes size) was reduced.12 Furthermore, one should consider that the development and growth of the male reproductive system is obviously a complex process and it is therefore not surprising that synthetic chemicals might affect male fertility in more than one way. Pesticides linked with Male Infertility The two chemicals discussed above are found in pesticide products regularly. Octyl phenol and butyl benzyl phthalate are both used as "inert" ingredients, used in most pesticide products to make them more efficient or easier to use. Based on Colborn et al. (Table 1) pesticides are often classified according to the organism specific target, e.g. as fungicides, herbicides, insecticides, nematocides etc.13 Chlordecone In 1975, a worker from a chemical factory visited his family physician for help with persistent headaches, tremors and irritability. Further investigations showed that he and his fellow workers were contaminated with chlordecone, and surprisingly only 25% of workers at the plant had normal sperm counts.14 The sperm produced by
these workers also did not swim like normal sperms. The workers' sperm counts increased over the next five years as medications removed chlordecone from their body tissues.14 1,2-Dibromo-3-chloropropane (DBCP) DBCP was used in the past as a soil fumigant and nematocide on crops; it is no longer used except as an intermediate in chemical synthesis. Its spermatotoxic effects in rats were discovered in the early 60s, but its effects on human spermatogenesis were discovered only in 1977. It was noted that there was paucity of children among the workers in a DBCP plant, after they had started to work in DBCP production.15 They have also reported in the subsequent study that occupational exposure to DBCP caused a reduction in the sperm concentration in ejaculates from a median 79 million cells/ml in unexposed men to 46 million cells/ml in exposed workers.16 Potashnik et al. have studied on six workers exposed to DBCP in a pesticide factory, who underwent testicular biopsy and reported complete atrophy of the somniferous epithelium in these exposed workers.17 Seventeen years follow-up study of 15 workers exposed to DBCP revealed that sperm count recovery was evident within 36 to 45 months in three of the nine azoospermic and in three of the six oligozoospermic men with no improvement thereafter.18 Glass et al. reported studies of male DBCP applicators and determined that the effects of the agent were limited to individuals in certain situations, such as applicators involved in irrigation set-up work and in the calibration of equipment. Once released from these situations, the sperm counts of these individuals returned to normal.19 Later Kahn and Whorton reanalyzed these data and showed that all applicator groups had reduction in sperm counts in a dose related manner and that reversibility was not a certainty.20 Studies of Ychromosome non disjunction, DBCP-exposed workers had a higher average YFF frequency compared to non exposed individuals. An agent that increases Y-Chromosomal no disjunction might be anticipated to result in increased pregnancy wastage.21 In 1997, another study by Multigner et al. showed testicular dysfunction among factory and field workers who were exposed to DBCP.22 In another study on the male workers involved in manu-
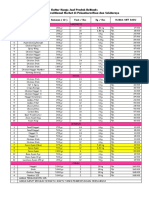
Table 1: Classification of Pesticides Classification Pesticides Herbicides 2,4-D; 2,4,5-T; Alachlor; Amitrole; Atrazine; Metribuzin; Nitrofen; Trifluralin; Paraquat Fungicides Benomyl; Hexachlorobenzene; Mancozeb; Maneb; Metiram-complex; Tributyl tin; Zineb; Ziram -HCH; Carbaryl; Chlordane; Chlordecone; Dicofol; Dieldrin; DDT and metbolites; Endosulfan; HeptaInsecticides chlor and H-epoxide; Lindane; Methomyl; Methoxychlor; Mirax; Oxychlordane; Synthetic pyrethroids; Toxaphene; Transnonachlor Nematocides Aldicarb; DBCP
Iran J Med Sci December 2005; Vol 30 No 4 155
J. Srinivasa, P. Maxim, J. Urban, A. DSouza
facturing of DBCP have reported to have a high level of LH and FSH in their serum and a reduced sperm counts.23 Carbaryl Carbaryl is an insecticide used on a variety of crops. Acute (short-term) and chronic (long-term) occupational human exposure to carbaryl has been observed to cause cholinesterase inhibition, and reduced levels of this enzyme in the blood caused neurological effects. Two studies at a carbaryl manufacturing factory have shown that carbaryl exposure affects the quantity and quality of sperm produced by the workers. One study found that frequent exposure of workers to this chemical induced very low sperm counts as compared to a control group of unexposed workers.24 This result was proved to be significant based on one statistical analysis, but has been criticized because of a second statistical test proving only a closer significance. A second study of the same sperm samples found that the number of sperm abnormalities was increased in workers who were being exposed to carbaryl.25 Multiple pesticide exposure A study conducted by Rope et al. among male workers who were exposed to various mixtures of pesticides such as DDT, BHC, endosulfan; and organophosphorus pesticides i.e. malathion, methyl-parathion, dimethote, monocrotophos, phosphamidon and quinalphos; synthetic pyrethroids such as fenvelrate and cypermethrin during mixing and spraying showed male mediated adverse reproductive outcome such as abortion, stillbirths, neonatal deaths, congenital defects, etc. It is not possible to say any particular pesticide caused the reproductive toxicity on the basis of these results, as there may be cumulative effects of a number of pesticides.26 This can be explained based on another study in which an "in culture" bioassay was used to assess the estrogenicity of several estrogenic pesticides such as DDT and chlordecone which cause deleterious reproductive effects. The E-screen test revealed that estrogenic chemicals may act cumulatively; when mixed together they induce estrogenic responses at concentrations lower than those required when each compound is administered separately.27 Abell et al. studied the testicular function of greenhouse workers exposed to pesticides and reported that male fecundity may be at risk from exposure to pesticides in the manual handling of cultures in green houses.28
Dichlorodiphenyltrichloroethane (DDT) and Polychlorinated biphenyls (PCBs) Studies of males exposed to DDT have found decrements in serum bioavailable testosterone levels,29 reduced semen volume on ejaculation and reduced sperm counts.30 In a recent retrospective study, information obtained from 2,033 workers on the reproductive history of the malaria control program workers in the Pacific region revealed an increased risk of birth defects among those most exposed to DDT, without a clear dose response, and a small, non statistically significant, difference in the risk of spontaneous abortion. No change in the sex ratio of newborns was associated with exposure.31 PCBs and p, p-DDE, the most stable metabolite of DDT, are persistent, lipophilic chemicals that are suspected endocrine disruptors. DDT was widely used as an insecticide, whereas PCBs were used in cutting oils, lubricants, and as electrical insulators. In human studies, Bush et al. analyzed 170 semen samples for PCBs and p,p-DDE from fertile men, men with idiopathic oligospermia, and men after vasectomy.32 The mean of the total PCBs (sum of all congeners) in the semen samples was 5.80.8 ng/g.33 The authors stated that these concentrations were minimal and consistent with the levels seen in the general population; the semen sample PCB concentrations were of comparable to the concentration of residues in human blood. Bush et al. also stated that in samples with a sperm count less than 20 million cells/ml, there was a significant inverse relationship between sperm motility and the concentration of PCB congeners 153, 138, and 118 (2,4,5,2,4,5- and 2,4,5,2,3,4-hexachlorobiphenyl and 2,4, 33 5,3,4-pentachlorobiphenyl) respectively. These three congeners are the major components of Aroclor 1254 and 1260. The magnitude of their effects on motility was large; ranging from 46% to 100%, therefore the maximum of their concentrations the three congeners would produce complete lack of motility. Bush et al. concluded that the relationship between specific PCB congeners and motility is both significant and biologically important.33 Their findings are intriguing and disturbing because the three congeners that found to be inversely predictive of sperm motility are ubiquitous in the human population.33 Further evidence of a possible relationship between PCBs and semen quality is presented in a study in rats which suggests that PCB exposure affected the ability of sperm to fertilize eggs.34 In a cross-sectional study of 212 male partners of subfertile couples who presented to the Massachusetts General Hospital Andrology Laboratory, Boston, USA their semen sam-
156 Iran J Med Sci December 2005; Vol 30 No 4
Effects of pesticides on male reproductive functions
ples were analyzed to determine whether environmental levels of PCBs and p,p'-DDE are associated with altered semen parameters in adult men.35 Semen parameters were analyzed as both a continuous measure and dichotomized based on World Health Organization reference values for sperm concentration (< 20 million/ml), motility (< 50% motile), and Kruger strict criteria for morphology (< 4% normal). The comparison group for the dichotomized analysis was men with all the three semen parameters above the reference values. In serum, 57 PCB congeners and p,p'-DDE were measured by congener-specific analysis using gas chromatography with electron capture detection. The results revealed an inverse doseresponse relationship between PCB-138 and sperm concentration, motility, and morphology.35 Whereas, there was limited confirmation of inverse relationships between the sum of PCBs, as well as those PCBs classified as cytochrome P450 enzyme inducers, with sperm motility and sperm morphology, and inverse association between p,p'-DDE and sperm motility.35 The lack of a consistent relationship between semen parameters, individual and grouping congeners of PCB may indicate a difference in spermatotoxicity between congeners.35 Lindane Pages and colleagues in recent study have clearly demonstrated a relatively high level of lindane metabolites in marine environment. Lindane has been directly linked with both reproductive and carcinogenic properties. It is shown that chronic administration of lindane results in endocrine disruption in birds as well as in mammals. Treatment with 1-40 mg of lindane/kg body weight disrupted testicular morphology, decreased spermatogenesis, inhibited testicular steroidogenesis, reduced plasma androgen concentrations and impaired reproductive performances in males.36 Endosulfan A recent study suggests that endosulfan exposure may delay sexual maturity and interfere 37,38 with hormone synthesis in male children. 2,4-Dichlorophenoxy acetic acid (2,4-D) In a study performed on reproductive functions of 32 male farm sprayers exposed to 2,4D, and after four days of sexual inactivity the results of their sperm analysis, compared with unexposed workers, showed a significantly high levels of asthenospermia, necrospermia and teratospermia. Over time, asthenospermia and necrospermia diminished but the abnormal 39 spermatozoa (teratospermia) continued.
Table 2: List of pesticide(s) causing male reproductive toxicity. pesticide(s) References 1 Chlordecone 14 2 di-bromochloropropane 15-23 3 Carbaryl 24,25 4 Multiple pesticide exposure 26,28 4 DDT and PCBs 29-35 6 Lindane 36 7 Endosulfan 37,38 8 2,4-dichlorophenoxyacetic acid 39 9 Paraquat 40
Conclusion Exposure to pesticides lowers sperm levels well below the limit for male fertility. Over 50 currently used pesticides are shown to induce adverse effects on male fertility based on animal or human studies. Although, it is proved that pesticide exposure is associated with infertility, there are not large-scale studies assessing their relationships to human infertility. To overcome the difficulties in the interpretation and to reach strong conclusions, future studies on the effects different types of pesticides on the human male reproductive system should consider several methodological problems, such as the standardization of analytical procedures with strict quality controls within and between laboratories, adoption of well defined terms of the outcome to be measured, the use of concurrent control subjects, analysis of semen with respect to the time variables, the adoption of standardized criteria for information and motivation of the participants, and exposure assessment. It is also important to study large cohorts to evaluate, possible effects at different pesticide concentrations, the currently encountered in occupationally exposed populations and to design such studies to characterize the doseresponse relation and evaluate change of values over time. This will also enable establishment of a no effect level of the chemical and proper biological limit values. The question of the indicator of exposure should also be clarified, taking into account that possible indicators such as seminal pesticide concentrations may be more useful in fertility studies than the indicators of recent exposure. It should be underlined that interactions with other occupational and nonoccupational exposures must be considered and every possible confounding factor should be controlled. In this respect, integrated studies should be promoted which will evaluate not only seminal and endocrine end points, but also other aspects such as the time of pregnancy and also in the view of adverse health effects observed to some extent in work-
Iran J Med Sci December 2005; Vol 30 No 4 157
J. Srinivasa, P. Maxim, J. Urban, A. DSouza
ers/applicators with few pesticides. It is also necessary to find out ecologically sound alternatives to pesticides and to educate the workers / farmers about the safe use of these pesticides to reduce reproductive health risk associated with their exposures. References 1 D'Souza UJ. Effect of tamoxifen on spermatogenesis and tubular morphology in rats. Asian J Androl 2004; 6: 223-6. D'Souza UJ. Tamoxifen induced multinucleated cells (symplasts) and distortion of seminiferous tubules in rat testis. Asian J Androl 2003; 5: 217-20. Jayachandra S, Pinto M, U JA DSouza. Alternative Testing MethodsReproductive toxicity. Tr J of Med Sci 2004; 34: 419. Carlsen E, Giwereman A, Keiding N, et al. Evidence for decreasing quality of semen during the past 50 years. BMJ 1992; 305: 609-13. Van Waeleghem K, Declercq N, Vermeulen L, et al. Deterioration of sperm quality in young Belgian men during recent decades. Human Reprod 1994; 9: 73. Irvine DS. Falling sperm quality. BMJ 1994; 309: 476. Auger J, Kutmann JM, Czglik F, et al. Decline in semen quality among fertile men in Paris during the past 20 years. N Engl J Med 1995; 332: 281-5. Leto S, Frensilli FJ. Changing parameters of donor semen. Fertil Steril 1981; 36: 766-70. Olsen GW, Bodner KM, Ramlow JM, et al. Have sperm counts been reduced 50 percent in 50 years? A statistical model revisited. Fertil Steril 1995; 63: 887-93. Itoh N, Kayama F, Tatsuki TJ, Tsukamoto T. Have sperm counts deteriorated over the past 20 years in healthy young japanese men? Results from the Sapporo area. J Androl 2000; 22: 40-4. D'Souza UJ, D'Souza VM, Narayana K. Is today's male population really less fertile? Declining semen quality-a global phenomenon? Indian J Med Sci 2004; 58: 305-6. Sharpe RM, Skakkebask NE. Are oestrogens involved in falling sperm counts and disorders of the male reproductive tract? Lancet 1993; 341: 1392-95. Colborn T, vom Saal FS, Soto AM. Developmental Effects of Endocrine Disrupting Chemicals in Wildlife and Humans. Environ Health Perspect 1993; 101: 378-84. Guzelian PS. Comparative toxicology of chlordecone (Kepone) in humans and experimental animals. Annu Rev Pharmacol Toxicol 1982; 22: 89-113.
3 4
6 7
8 9
10
11
12
13
14
15 Whorton D, Krauss RM, Marshall S, Milby TH. Infertility in male pesticide worker. Lancet 1977; 11: 1259-61. 16 Whorton D, Milby TH, Krauss RM, Stubbs HA. esticular function in DBCB exposed pesticide workers. J Occup Med 1979; 21: 161-6. 17 Potashnik G, Ben Aderet N, Israeli R, et al. Suppressive effect of 1, 2dibromo-3chloropropane on human spermatogenesis. Fertil Steril 1978; 30: 444-7. 18 Potashnik G, Porath A. Dibromochloropropane (DBCP): A 17-year reassessment of testicular function and reproductive performance. J Occup Environ Med 1995; 37: 1287-92. 19 Glass RI, Lyness RN, Mengle DC, et al. Sperm count depression in pesticide applicators exposed to dibromochloropropane. Am J Epidemiol 1979; 109: 346-51. 20 Kahn E, Whorton D. Re "sperm count depression in pesticide applicators exposed to dibromochloropropane". Am J Epidemiol 1980; 112: 161-5. 21 Kapp RW, Picciano DJ, Jacobson CB. Ychromosomal nondisjunction in dibromochloropropane-exposed workmen. Mutat Res 1979; 64: 47-51. 22 Multigner L, Spira A. The epidemiology of male reproduction In: Barratt C, de Jonge C, Mortimer D, Parinaud J, eds: Genetics of human male fertility; 1997. p. 43-65. 23 .Mattison DR, Plowchlk DR, Eadows MJ, et al. Reproductive toxicity: Male and female reproductive systems as target for chemical injury. Med Clin North Am 1990; 74: 391-411. 24 Whorton MD, Milby TH, Stubbs HA, et al. Testicular function among carbaryl-exposed exployees. J Toxicol Environ Health 1979; 5: 929-41. 25 Wyrobek AJ, Watchmaker G, Gordon L, et al. Sperm shape abnormalities in carbaryl-exposed employees. Environ Health Perspect 1981; 40: 255-65. 26 Rupa DS, Reddy PP, Reddi OS. Reproductive performance in population exposed to pesticides in cotton fields in India. Environ Res 1991; 55: 123-8. 27 Soto AM, Chung KL, Sonnenschein C. The pesticides endosulfan, toxaphene, and dieldrin have estrogenic effects on human estrogen-sensitive cells. Environ Health Perspect 1994; 102: 380-3. 28 Abell A, Ernst E, Bonde JP. Semen quality and sexual hormones in greenhouse workers. Scand J Work Environ Health 2000; 26: 492-500. 29 Martin S, Harlow SD, Sowers MF, et al. DDT metabolite and androgens in African-
158 Iran J Med Sci December 2005; Vol 30 No 4
Effects of pesticides on male reproductive functions
30
31
32
33
34
American farmers. Epidemiology 2002; 13: 454-8. Ayotte P, Giroux S, Dewailly E, et al. DDT spraying for malaria control and reproductive function in Mexican men. Epidemiology 2001; 12: 366-7. Salazar-Garcia F, Gallardo-Diaz E, CeronMireles P, et al. Reproductive effects of occupational DDT exposure among male malaria control workers. Environ Health Perspect 2004; 112: 542-7. Bush B, Bennett AH, Snow JT. Polychlorobiphenyl congeners, p,p'-DDE, and sperm function in humans. Arch Environ Contam Toxicol 1986; 15: 333-41. Bush B, Snow J, Kobiintz R. Polychlorobiphenyi (PCB) congeners, p,p'-DDE, and hexachlorobenzene in maternal and fetal cord blood from mothers in upstate New York. Arch Environ Contam Toxicol 1984; 13: 517. Sager DB, Girard D, Nelson D. Early postnatal exposure to PCBs: sperm function in rats. Environ Toxicol Chem 1991; 10: 737-46.
35 Hauser R, Chen Z, Pothier L, et al. The relationship between human semen parameters and environmental exposure to polychlorinated biphenyls and p,p'-DDE. Environ Health Perspect 2003; 111: 1505-11. 36 Pages N, Sauviat MP, Bouvet S, GoudeyPerriere F. Reproductive toxicity of lindane. J Soc Biol 2002; 196: 325-38. 37 Saiyed H, Dewan A, Bhatnagar V, et al. Effect of Endosulfan on Male Reproductive Development. Environ Health Perspect 2003; 111: 1958-62. 38 Narayana K, Narayan P, D'Souza UJ. Is our drinking water a slow poison? Indian J Med Sci 2004; 58: 528-30. 39 Lerda D, Rizzi R. Study of reproductive function in persons occupationally exposed to 2,4-dichlorophenoxyacetic acid (2,4-D). Mutat Res 1991; 262: 47-50. 40 D'Souza UJ, Zain A, Raju S. Genotoxic and cytotoxic effects in the bone marrow of rats exposed to a low dose of paraquat via the dermal route. Mutat Res 2005; 581: 187-90.
Iran J Med Sci December 2005; Vol 30 No 4 159
S-ar putea să vă placă și
- Endocrine Disrupting Chemicals PDFDocument12 paginiEndocrine Disrupting Chemicals PDFRocco LamponeÎncă nu există evaluări
- Endocrine Effects of Prenatal Exposure PCBS, Dioxins, and Other Xenobiotics: Implications For Policy and Future ResearchDocument4 paginiEndocrine Effects of Prenatal Exposure PCBS, Dioxins, and Other Xenobiotics: Implications For Policy and Future ResearchAgent Orange LegacyÎncă nu există evaluări
- Effects of XenoDocument8 paginiEffects of XenoPadmaja NamballaÎncă nu există evaluări
- Hormones and Embryonic Development: Advances in the BiosciencesDe la EverandHormones and Embryonic Development: Advances in the BiosciencesG. RaspéÎncă nu există evaluări
- Effects of Male Age On Semen Quality and Fertility: A Review of The LiteratureDocument12 paginiEffects of Male Age On Semen Quality and Fertility: A Review of The LiteraturethunderdomeÎncă nu există evaluări
- Endocrine Disruptors 508Document4 paginiEndocrine Disruptors 508isaco1531012Încă nu există evaluări
- Male ReproductionDocument88 paginiMale ReproductionBlackHerbalsÎncă nu există evaluări
- Male InfertilityDocument5 paginiMale InfertilityAleksandra BozinovskaÎncă nu există evaluări
- Reproductive Toxicology in Occupational Settings: An Update: ReviewDocument10 paginiReproductive Toxicology in Occupational Settings: An Update: ReviewGhilea AlinaÎncă nu există evaluări
- Cigarette Smoking's Effects on Male FertilityDocument7 paginiCigarette Smoking's Effects on Male FertilityEka PriyantiÎncă nu există evaluări
- Alexandria Bulletin: El Samra Et Al. 165Document11 paginiAlexandria Bulletin: El Samra Et Al. 165rahman_alfarisiÎncă nu există evaluări
- Disruptores EndocrinosDocument16 paginiDisruptores EndocrinospalomitadanceÎncă nu există evaluări
- Infertilidad MasculinaDocument22 paginiInfertilidad MasculinaAnaÎncă nu există evaluări
- Artikel Penelitian Sistem EndokrinDocument9 paginiArtikel Penelitian Sistem EndokrinMusyamuÎncă nu există evaluări
- 50 Percent Fertility Reduction Because of These Household ChemicalsDocument5 pagini50 Percent Fertility Reduction Because of These Household ChemicalsDivyajyoti DevaÎncă nu există evaluări
- Argumentos en Contra Del Uso de Animales de ExperimentaciónDocument5 paginiArgumentos en Contra Del Uso de Animales de ExperimentaciónJuan David RejónÎncă nu există evaluări
- Fendo 13 1107903Document3 paginiFendo 13 1107903puspitaÎncă nu există evaluări
- Grade 3 Varicocele in Fertile MenDocument6 paginiGrade 3 Varicocele in Fertile MenMuhammad AndilaÎncă nu există evaluări
- Transgenic Monkeys Produced in Japan: Bautista Hernández Jorge Luis Ingles III Cuarto SemestreDocument3 paginiTransgenic Monkeys Produced in Japan: Bautista Hernández Jorge Luis Ingles III Cuarto SemestreJorge Luis BautistaÎncă nu există evaluări
- EndosulfanDocument6 paginiEndosulfanAshraf MambalamÎncă nu există evaluări
- Barlow 1999Document11 paginiBarlow 1999asdsffggeettrgbfbfbftggrg ergrtertererefrerrÎncă nu există evaluări
- PDF CJMB 37Document6 paginiPDF CJMB 37shahan lodhiÎncă nu există evaluări
- Epigenetic SDocument8 paginiEpigenetic Smaria dulce100% (1)
- Lifestyle and Fertility: The Influence of Stress and Quality of Life On Male FertilityDocument11 paginiLifestyle and Fertility: The Influence of Stress and Quality of Life On Male FertilitySantiago CeliÎncă nu există evaluări
- New Chapter in Old Story: Endocrine Disruptors and Male Reproductive SystemDocument10 paginiNew Chapter in Old Story: Endocrine Disruptors and Male Reproductive SystemDania KumalasariÎncă nu există evaluări
- Implement The Zero Garbage System at Domestic LevelDocument5 paginiImplement The Zero Garbage System at Domestic Levelsamar karemoreÎncă nu există evaluări
- Contribution of Environmental Factors To The Risk of Male InfertilityDocument9 paginiContribution of Environmental Factors To The Risk of Male Infertilitya.itatahineÎncă nu există evaluări
- Édi PDFDocument16 paginiÉdi PDFCamii CvÎncă nu există evaluări
- A Prospective, Single Centre, Observational Study For The Impact of Lifestyle Modifications On Semen Parameters in Patiens Diagnosed With Abnormal Semen AnalysisDocument7 paginiA Prospective, Single Centre, Observational Study For The Impact of Lifestyle Modifications On Semen Parameters in Patiens Diagnosed With Abnormal Semen AnalysisEditor IJTSRDÎncă nu există evaluări
- The Effect of Paternal Age On Assisted Reproduction Outcome: Modern TrendsDocument8 paginiThe Effect of Paternal Age On Assisted Reproduction Outcome: Modern TrendsFedrik Monte Kristo LimbongÎncă nu există evaluări
- Própolis e FertilidadeDocument7 paginiPrópolis e FertilidadeMonica Lopes Assunção FerreiraÎncă nu există evaluări
- Glutathione in The Human Male: Prostate ProblemsDocument11 paginiGlutathione in The Human Male: Prostate Problemsapi-26034055Încă nu există evaluări
- Male Infertility Thesis PDFDocument7 paginiMale Infertility Thesis PDFlizharriskansascity100% (2)
- Effect of Emerging Water ContaminantsDocument5 paginiEffect of Emerging Water ContaminantsMadhur Bain SinghÎncă nu există evaluări
- NIH Public Access: Author ManuscriptDocument21 paginiNIH Public Access: Author ManuscriptgiannidietÎncă nu există evaluări
- CREDO Project NewsletterDocument20 paginiCREDO Project NewsletterKarolina PendovskaÎncă nu există evaluări
- Female Reproductive Tract and Mammary Disorders Caused by Endocrine DisruptorsDocument4 paginiFemale Reproductive Tract and Mammary Disorders Caused by Endocrine DisruptorsNur AnindyaÎncă nu există evaluări
- Expression of Estrogen Receptors Aandbin Paratesticular Tissues in Boys Operated On For Unilateral Cryptorchidism Between The 1 and 4 Years of LifeDocument5 paginiExpression of Estrogen Receptors Aandbin Paratesticular Tissues in Boys Operated On For Unilateral Cryptorchidism Between The 1 and 4 Years of LifeHamdan Yuwafi NaimÎncă nu există evaluări
- 2016 S FM Myers Our StolenDocument2 pagini2016 S FM Myers Our StolenShanica Paul-RichardsÎncă nu există evaluări
- Research Bisphenol A (BPA) Causes 100x More Harm Than Previously ImaginedDocument5 paginiResearch Bisphenol A (BPA) Causes 100x More Harm Than Previously ImaginedThavam RatnaÎncă nu există evaluări
- Trend of Fertility Potentials With Increasing Age in Pakistani MalesDocument5 paginiTrend of Fertility Potentials With Increasing Age in Pakistani MalesmominamalikÎncă nu există evaluări
- Dgab 034Document12 paginiDgab 034Nofianti anggia putriÎncă nu există evaluări
- Clinical Urologic Endocrinology: Principles for Men’s HealthDe la EverandClinical Urologic Endocrinology: Principles for Men’s HealthParviz K. KavoussiÎncă nu există evaluări
- Danis 2019Document8 paginiDanis 2019周保亨Încă nu există evaluări
- Natural compounds may treat male infertilityDocument13 paginiNatural compounds may treat male infertilitynajib fahmiÎncă nu există evaluări
- Ehp 119 713Document6 paginiEhp 119 713Brianza CentraleÎncă nu există evaluări
- Case Study WrittenDocument35 paginiCase Study Writtenkritikas9977Încă nu există evaluări
- Chemotherapies and Male InfertilityDocument4 paginiChemotherapies and Male Infertilitymiguel saba sabaÎncă nu există evaluări
- FeeeDocument8 paginiFeeeRoxana MariaÎncă nu există evaluări
- Aspartame Is An Excitoneurotoxic Carcinogenic DrugDocument9 paginiAspartame Is An Excitoneurotoxic Carcinogenic DrugThorsteinn ThorsteinssonÎncă nu există evaluări
- Effect of Workstress and Smoking Towards Sperm Quality Among Infertile MaleDocument8 paginiEffect of Workstress and Smoking Towards Sperm Quality Among Infertile MalececeÎncă nu există evaluări
- Biol Sex Differ 2020 11 1 15Document10 paginiBiol Sex Differ 2020 11 1 15Fernando SousaÎncă nu există evaluări
- Corporate Espionage The Seralini AffairDocument46 paginiCorporate Espionage The Seralini AffairMarcelo SarlingoÎncă nu există evaluări
- Erkek Infertilitesi Makale-2Document9 paginiErkek Infertilitesi Makale-2Dr.Serkan SenerÎncă nu există evaluări
- Science Magazine 5696 2004-10-22Document120 paginiScience Magazine 5696 2004-10-22WillimSmithÎncă nu există evaluări
- Hormones and Reproduction of Vertebrates, Volume 1: FishesDe la EverandHormones and Reproduction of Vertebrates, Volume 1: FishesÎncă nu există evaluări
- Are Urinary Bisphenol A Levels in Men Related To Semen Quali 2014 FertilityDocument12 paginiAre Urinary Bisphenol A Levels in Men Related To Semen Quali 2014 Fertilitycuongduong172839Încă nu există evaluări
- Jurnal VarikokelDocument19 paginiJurnal VarikokelMahdi SegafÎncă nu există evaluări
- Relationship Between Sperm Quality and Male Reproductive Hormones Among Male Partners With Fertility Complications: Attending CHUBDocument13 paginiRelationship Between Sperm Quality and Male Reproductive Hormones Among Male Partners With Fertility Complications: Attending CHUBabd.m.midanyÎncă nu există evaluări
- Human TissueDocument29 paginiHuman TissueSudeep ShahÎncă nu există evaluări
- 2014 Effects of Dietary Thyme (Thymus Vulgaris) and Fish OilDocument7 pagini2014 Effects of Dietary Thyme (Thymus Vulgaris) and Fish OilDr. Attalla F. El-kottÎncă nu există evaluări
- Instructions For Authors Molecular & Cellular ToxicologyDocument7 paginiInstructions For Authors Molecular & Cellular ToxicologyDr. Attalla F. El-kottÎncă nu există evaluări
- Editor BoardDocument7 paginiEditor BoardDr. Attalla F. El-kottÎncă nu există evaluări
- Chronic Toxicity (Or Exposure) in Vitro Toxicity Data: AmitrazDocument2 paginiChronic Toxicity (Or Exposure) in Vitro Toxicity Data: AmitrazDr. Attalla F. El-kottÎncă nu există evaluări
- 7Document7 pagini7Dr. Attalla F. El-kottÎncă nu există evaluări
- Copyright Form IJRRDocument3 paginiCopyright Form IJRRDr. Attalla F. El-kottÎncă nu există evaluări
- Diabetes Mellitus: Overview and TreatmentsDocument36 paginiDiabetes Mellitus: Overview and TreatmentsGlenn Nadine N. Masicampo100% (1)
- AmitrazDocument8 paginiAmitrazGamal SolimanÎncă nu există evaluări
- Amitraz MetabolismDocument28 paginiAmitraz MetabolismDr. Attalla F. El-kottÎncă nu există evaluări
- Elephant 97Document3 paginiElephant 97Arslan Farooq0% (4)
- General Introduction of NeonateDocument42 paginiGeneral Introduction of Neonateapi-19916399Încă nu există evaluări
- The Shape of Grief: Thwop Goes The Top and She IsDocument2 paginiThe Shape of Grief: Thwop Goes The Top and She Ispranati putrevuÎncă nu există evaluări
- Anatomy Test - QuestionsDocument5 paginiAnatomy Test - QuestionsNom NomÎncă nu există evaluări
- PM 286 BDocument2 paginiPM 286 Bnasreen95035Încă nu există evaluări
- Derek Walcott - The Castaway and Other PoemsDocument62 paginiDerek Walcott - The Castaway and Other PoemsSequeTon Enlo60% (5)
- Communicating Spirit: The White Wind Birth ChartDocument35 paginiCommunicating Spirit: The White Wind Birth ChartYannis KaratsÎncă nu există evaluări
- JPMR TITLEDocument5 paginiJPMR TITLEsharmila janaki100% (1)
- otoRhinoLaRynGoLogic Exam ChecklistDocument5 paginiotoRhinoLaRynGoLogic Exam ChecklistSulabh ShresthaÎncă nu există evaluări
- Evolution and Biodiversity Test ReviewDocument15 paginiEvolution and Biodiversity Test ReviewSanaa SamkoÎncă nu există evaluări
- A Busy Mom's Guide To Daily Meal Preparation: I Just Wanted To Expound That What I Usually Do IsDocument8 paginiA Busy Mom's Guide To Daily Meal Preparation: I Just Wanted To Expound That What I Usually Do IsCarina TanÎncă nu există evaluări
- Name: - Score: - Subject Teacher: - DateDocument3 paginiName: - Score: - Subject Teacher: - DateJaideHizoleSapulÎncă nu există evaluări
- Grade 9 CardioDocument16 paginiGrade 9 CardioJamoi Ray VedastoÎncă nu există evaluări
- Daftar Harga Jual Produk Belfoods Untuk Grosir, Traditional Market Di Pekanbaru-Riau Dan SekitarnyaDocument2 paginiDaftar Harga Jual Produk Belfoods Untuk Grosir, Traditional Market Di Pekanbaru-Riau Dan SekitarnyaDwi Mahendra SubhiÎncă nu există evaluări
- 2018 BortoDocument26 pagini2018 BortoBortoÎncă nu există evaluări
- Q2 W3 SCI 5-Methods of Reproduction (ANIMALs)Document32 paginiQ2 W3 SCI 5-Methods of Reproduction (ANIMALs)Buena Rosario100% (1)
- This That These Those Grammar Drills 44826Document2 paginiThis That These Those Grammar Drills 44826Nicolás RuizÎncă nu există evaluări
- HOOTER by Nicky Epstein PDFDocument3 paginiHOOTER by Nicky Epstein PDFAnneita100% (1)
- Singular and Plural NounsDocument6 paginiSingular and Plural NounsDarlene Daguno CabridoÎncă nu există evaluări
- Hematology Reference RangesDocument9 paginiHematology Reference Rangesdrafq2000Încă nu există evaluări
- Pathophysiology of Type 2 Diabetes MellitusDocument7 paginiPathophysiology of Type 2 Diabetes MellitusarbyjamesÎncă nu există evaluări
- Umberto BERNABUCCIDocument9 paginiUmberto BERNABUCCIbermudez_eduard8792Încă nu există evaluări
- Physicians Committee For Responsible MedicineDocument10 paginiPhysicians Committee For Responsible MedicinePeter M. HeimlichÎncă nu există evaluări
- Movie Script - The Lord of The Rings - The Two TowersDocument101 paginiMovie Script - The Lord of The Rings - The Two TowersMarc RitzÎncă nu există evaluări
- Cryptic Film TitlesDocument2 paginiCryptic Film TitlesChay HallÎncă nu există evaluări
- MiletskiDocument281 paginiMiletskiCanisLupusZeta100% (2)
- Rabies Control Program by DohDocument11 paginiRabies Control Program by DohSabrina Porquiado Magañan SNÎncă nu există evaluări
- TSR 9125 - UK5 - Eye of The Serpent PDFDocument38 paginiTSR 9125 - UK5 - Eye of The Serpent PDFRobert Bailey100% (3)
- What Is PuppetDocument7 paginiWhat Is PuppetsylviannitaÎncă nu există evaluări
- Pemerintah Kabupaten Cianjur Dinas Pendidikan Dan Kebudayaan Naskah Soal Penilaian Akhir Tahun Kurikulum 2013 TAHUN PELAJARAN 2020/2021Document15 paginiPemerintah Kabupaten Cianjur Dinas Pendidikan Dan Kebudayaan Naskah Soal Penilaian Akhir Tahun Kurikulum 2013 TAHUN PELAJARAN 2020/2021wahanaajaranÎncă nu există evaluări