Documente Academic
Documente Profesional
Documente Cultură
Pharmacology Note
Încărcat de
firstrikerDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Pharmacology Note
Încărcat de
firstrikerDrepturi de autor:
Formate disponibile
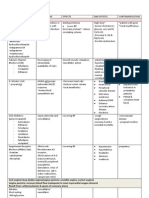
Drugs Affecting ANS Type Cholinergic Agonist Drugs Direct Acting: Acetylcholine Bethanechol Carbachol Pilocarpine Indirect Acting:
Physostigmine Neostigmine Organophosphorous compound Atropine Ipratropium Trimethaphan Vecuronium Tibocuararine Pancuronium Noradrenaline Adrenaline Oxymetazoline Xylometazoline Phenyephrine Dobutamine Salbutamol Dopamin Prazosin Terazosin Propanolol Atenolol Uses/ Functions - Decreases Heart rate and Blood Pressure - Increases GIT motility & secretion - Relaxation of sphincters - Increases respiratory secretion Inhibit cholinesterase enzyme Adverse Effect
Cholinergic Antagonist
Anti-muscarinic Atropine: use in bradycardia and organic phosphate poisoning Ganglion Blocker Neuromuscular blocker
Sympathomimetics
Facilitate/mimic actions of sympathetic nervous system
Anti-adrenergic (sympatholytic)
adrenergic blocker adrenergic blocker
Neuromuscular Blocking Agents Type Competitive, nondepolarising agents Drugs Curare Pancuronium Gallamine Mivacurirum Atracurirum Vecuronium Succinylcholine Suxamethonium Uses/ Functions - Compete with Ach for binding receptor Adverse effects - Muscarinic blocking - Histamine release - Apnea - Hypotension
Non-competitive, depolarising agents
Desensitize receptor for Ach
Bradycardia Hyperkalemia Hypotension Muscle pain Apnea Stroke Cerebral palsy Multiple sclerosis
Direct-acting muscle relaxant
Neostigmine Dantrolene Dantrium Botulinum toxin A
Treatment of Myasthenia Gravis Inhibit muscle release Treatment of Malignant Hyperthermia Inhibit release of Ach from presynaptic nerve Cosmetic use: removal of facial wrinkles
NSAIDs Type Non-selective COX inhibitor Drugs Aspirin Ibuprofen Piroxicam Uses/ functions Aspirin: - Anti-inflammatory (3-6 g/day) - Antipyretic, Analgesia (1 g/day) - Anti-platelet (75-325 mg/day) Analgesic Antipyretic Selectively inhibit COX-2 Adv over non-selective COX inhibitor: Low chance of bleeding, less gastric mucosal damage Inhibit COX-2 but still can inhibit COX-1 Adverse Effects - Peptic ulcer - Decrease renal blood flow - Allergic reaction (leukotrines) - Angioedema - Delay labors - Depletion of glutathione conjugation in children and alcoholic Enhanced CVS risk Salt & water retention Less anti-inflammatory action
Paracetamol
Selective COX-2 inhibitor
Celecoxib Itoricoxib Parecoxib Nimesulide Meloxicam Nabumetone
Refential COX-2 inhibitor
Anti-arrhytmic Drugs Type Class Ia Drugs Quinidine Procainamide Disopyramide Lidocaine Tocainide Flecanide Uses/ functions - Block Na channels with moderate potency - Block K channels - For supra-arrhythmia and ventricular arrhythmia - Block Na channels weakly - only for ventricular arrhythmia, after MI Block Na channels markedly Weakly block Ca channels For supra and ventricular arrhythmia Blocking norepinephrine and epinephrine Slows AV node conduction Inhibit K gates Used in atrial fibrillation and flutter use in bradycardia use in heart block slows AV conduction Adverse effects - Pro-arrhytmic - Visual disturbance - Abdominal pain - Dizziness - Seizure - Drowsiness - Blurred vision - Hallucination - Depression
Class Ib
Class Ic
Class II Class III Non-classified Non-classified
Esmolol Amiodarone Sotalol Digoxin Atropine Adenosine
Pro-arrhytmic Ventricular arrhythmia bradycardia
malaise facial flushing chest pain
Antihypertensive Drugs Type 1-adrenoceptors antagonist Drugs Selective: Prazosin Terazosin Doxazosin Non-selective: Phenoxybenzamine Phentolamine Selective 1: Atenolol Esmolol Acebutolol Metoprolol Non-selective: Timolol Propanolol Vasodilator: Carvedilol Labetolol Pindolol Nebivolol Partial agonist: Acebutolol Pindolol Enalapril Lisinopril Peridopril Uses/ functions - Block 1-adrenergic receptors - Reduces muscular tone of arterioles - Dilatation of veins Adverse effects - Postural hypotension - Nausea
Reflex tachycardia
-adrenergic antagonist
Reduces release of renin from juxtraglomerular cells, thus reducing output of Angiotensin II
Bradycardia
Reduces heart rate and contractility
Asthma Nightmare Bradycardia
Block -adrenergic receptors Release nitric oxide Dilates muscular vessels
Less bradycardia risk
ACE inhibitor
Inhibit ACE Reducing Angiotensin II, aldosterone Increases bradykinin Bring about vasodilatation Reduces total peripheral resistance Reduces sodium retention
Cough Mild hypotension
Type 2-adrenoceptor agonist
Drugs Clonidine Methyldopa
Uses/ Functions - Inhibition of noradrenaline release - Causes vasodilatation
Diuretics
Aldosterone antagonist: Spironolactone Eplerenone Thiazide
Inhibit action of aldosterone
Adverse Effects - Dry mouth - Sedation - Male sexual dysfunction - Tiredness - Depression - Postural hypotension - GIT disturbance - Hyperkalemia - Hyponatremia Hypokalemia hypocalcemia Cough Dizziness Hyperkalemia Flushing Headache Reflex tachycardia Reflex tachycardia except for amlodipine
Angiotensin receptor inhibitor Vasodilators
Irbesartan Telmisartan Valsartan K channels opener: Minoxidil CCB: Amlodipine Nifedipine Diltiazem cGMP activator: Hydralazine Nitrovasodilator: Sodium nitroprusside
Activation of ATP-regulated potassium channels in arterioles Inhibit calcium entry Decrease total peripheral resistance inhibit angiotensin receptor bring about vasodilatation reduce total peripheral resistance Bring about vasodilation
Tachycardia Vomiting Nausea Headache Dizziness Abdominal pain
Treatment of Myocardial Infarction Type Organic nitrates Drugs Nitroglycerine Isosorbide dinitrate Isosorbide mononitrate Dihydropiridines: Amlodipine Nifedipine Verapamil Diltiazem Aspirin Clopidogrel Heparin Warfarin Ranozaline Atenolol Metoprolol Propanolol Timolol Uses/ Functions - Causes vasodilatation - Decreases preload and afterload Vasodilatation Adverse Effects - Headache - Reflex tachycardia - hypotension - Oedema - Wheezing - Hypotension - Headache - Reflex tachycardia - Cause MI if use with beta blocker
Calcium channel blockers
Anti-thrombotic & lipid-lowering drugs
Vasodilatation Decrease myocardial activity Decreases heart rate Prevent thrombosis
Late Na channels blocker -blocker
Decrease intracellular Ca overload in myocardium Decrease heart rate Decrease myocardium contractility
Torsades de pointes Hypotension Cause serious MI if use with verapamil/ diltiazem
Lipid-lowering Intervention Type HMG-CoA inhibitor Fibrates Drugs reductase Atorvastatin Rosvastatin Simvastatin Gemfibrosil Fenofibrate Bezafibrate Nicotinic acid Uses/ functions - Decrease LDLC by 20-55% Adverse effects - Headache - Bowel upset - Muscle tenderness - Myalgia - Hepatitis - Gall stones - Rashes - Skin flushing - Itching - Vomiting - Liver dysfunction
Decrease TGL by 20-50%
Niacin
Decrease TGL by 20-50% Increase HDLC by 20-35%
Ezetimibe
Ezetimibe
Decrease LDLC by 15-20% Use with statin to reduce AE of statin
Treatment of Congestive Heart Failure Type Diurectics Drugs Frusemide Spironolactone Uses/ Functions Adverse effects - Decrease ECF volume - Decrease preload - Block effect of aldosterone from damaging heart, kidney and vessels - Decrease aldosterone effects - Vasodilatation - Decrease cardiac remodelling Venous dilatation
Vasodilators
-blocker
Cardiac glycosides Parental Inotropic drugs
ACE inhibitors: Enalapril Ramipril Lisinopril Nitrovasodilators: Nitroglycerine Isosorbide mononitrate Isosorbide dinitrate Direct vasodilators: Hydralazine Metoprolol Bisoprolol Carvedilol Digoxin Digitoxin & Dopaminergic agonist: Dopamine Dobutamine Phosphodiesterase: Milrinone Inamrinone
Arterial dilatation Decrease myocardium activity Decrease arrhtymia Decrease cardiac remodelling Inhibit Na/K pump SA & AV node inhibiton Inotropic effect Vasodilation For acute heart failure
Pharmacology of Asthma Type 2-adrenoceptor agonist (bronchodilators) Drugs Salbutamol (short acting) Salmeterol (long acting) Formeterol (long acting) Uses/ Functions Adverse effects - Salbutamol: - Tremor Increase mucus clearance and decrease mediator - tachycardia release - hyperkalemia - Salmeterol, formeterol: In nocturnal asthma - inhibiton of PDE enzyme - narrow margin of safety - prevent degradation of cAMP - nausea - inhibit cell surface of adenosine receptors - vomiting - bring about bronchodilation - tremor - increased mucociliary clearance - insomnia - tachycardia - relax bronchospasm - dry mouth - decreased mucus secretion - competitive antagonist at CysLT receptor - GIT disturbance - inhibit action of leukotrienes - Dry mouth - relaxes bronchial smooth muscle - headache - well tolerated especially for children - depress inflammatory response - dysphonia - inhibit leukotrines - oral thrush - cytokines and prostaglandins formation - systemic penetration inhibit degranulation of mast cell cough transient bronchospasm throat irritation high cost
Methylxanthine (bronchodilators)
Theophylline Thebromine Caffeine
Muscarinic antagonist (bronchodilator) CysLT receptor antagonist (bronchodilator) Glucocorticoids
Ipratropium Tiotropium Montelukast Zafirlukast
Mast cell stabilizers
Beclometasone Budesonide Prednisolone Cromoglycates Cromolyn Nedocromil Omalizumab
Anti-IgE
act by complexing IgE prevent binding of IgE to effector cells
10
Pharmacology of Cough Type Pharyngeal demulcents Drugs Lozenges Cough drops/syrups Glycerine Sodium iodide Potassium iodide Guifenesin Ammonium salts Syrup Ipecac Bromhexine Opioids: Codeine Pholcodeine Non-opiods: Noscapine Dextrometrophan Diphenhydramine Promethazine Chlorpheniramine Benadryl Uses/ functions - Sooth mucus membrane of throat - Reduce afferent impulses from pharyngeal mucosa - Increase bronchial secretion Adverse effects Disadvantages: short-acting inflamed/irritated
Expectorant
Mucolytics Antitussives
Induce thin copious bronchial secretion Reduce viscosity of bronchial secretion Act in CNS to raise threshold of cough centre
Constipation Sedation Addictive
Advantages: no constipation, sedation, no addictive
Antihistaminic
Relieve allergic rhinitis syndrome Relieve itching and swelling
Decongestants
Ephedrine Pseudoephedrine Oxymetzoline Zylometazoline
Vasoconstriction of nose vessels Reduction in oedema and secretion
Sedation Fatigue Dry mouth Fatigue Dizziness Sedation Nausea Headache
11
Haematinics Type Iron supplement Drugs Oral: Ferrous sulphate Ferrous gluconate Ferrous fumarate Parentral: Iron dextrane Iron sucrose Sodium ferric gluconate Cynocobalamine Hydroxycobalamine Folate Uses/ Functions - For iron-deficiency anaemia - Parenteral iron: For oral iron not tolerated Failure to absorb iron due to gastrectomy Chronic bleeding Adverse Effects - Epigastric - Nausea - Staining teeth
B12 supplement Folic acid supplement Erythropoietin
For B12-deficieny anaemia
Erythropoietin
For folic acid deficiency Folic acid deficiency in pregnant causes neural tube defects Essential for erythropoiesis -
Uses of folic acid in B12 deficiency may worsen the condition Never use alone in B12-defeciency
Increases blood viscosity Increase clot formation Hypertension
12
Immunosuppressant Drugs Type Calcineurin inhibitor Drugs Ciclosporin Uses/ Functions - Binds to cyclophilin - Inhibit IL2 production - Inhibit activation of mitogen activated protein kinases Adverse effects - Nephrotoxicity - Hypertension - Fluid retention - Tremor - Headache - Hyperlipidemia - Pleural and pericardial effusion - Cardiomyopathy children Bone marrow suppression Hair loss Vomiting Fever Hypotension GI ulceration Bleeding Diarrhoea Vomiting
Tacrolimus Antiproliferative agents Azathioprine
Binds to FK-binding protein-12 Inhibit IL2 production Metabolized to 6-mercaptopurne Inhibit T-cell DNA synthesis Supressing cell and antibody immune response
Mycophenolate Mofetil
IL2 receptor antibodies
Basiliximab Daclizumab Sirolimus
mTOR inhibitor
Corticosteroids
Cortisol Budesonide
Deprive guanine to lymphocytes by inhibit nucleotide converting enzymes Block IL2 receptor CD4 T-cells no longer can be activated to produce interleukin Binds to FK-binding Protein-12 Inhibits cytoplasmic kinase mTOR Retarding mitogenic protein & DNA synthesis Supress promotion of IL2 expression by calcineurin
13
Drugs affecting Blood Coagulation Type Fibrinolytics Drugs Streptokinase Urokinase Alteplase Injectable: Heparin LMW Heparin (enoxaparin, dalteparin, tinzaparin) Oral route: Warfarin Uses/ Functions - Cleaves plasminogens to plasmin - Plasmin lyses fibrin to fibrin degradation products - For MI and massive pulmonary embolism - Accelerates antithrombin III through IV and subcutaneous - LMWH: selectively inhibit factor Xa less frequency of bleeding lower risk of osteoporosis lower incidence of thrombocytopenia - inhibits Vitamin K reductase - Vitamin K dependant carboxylation of factor II, VII, IX, X cannot occur - 5 days of action onset - Aspirin use because other NSAIDs bind reversibly with platelet - Inhibit COX enzyme in platelets - Selectively inhibit Thromboxane A2 - Inhibit purinergic receptor - Inhibit activation of glycoprotein IIb/IIIa on surface of platelets - Inhibit glycoprotein IIb/IIIa receptors - Inhibit platelets aggregation Adverse effects - Systemic lytic state - Hemorrhage Bleeding Thrombocytopenia osteoporosis
Anti-coagulants
Anti-platelet
Aspirin (75-325mg/day) Clopidogrel Abciximab
Bleeding Teratogenic effect to pregnant mother If overdose: just use blood transfusion GI bleeding GI irritation Haemorrhage Abdominal discomfort Haemorrhage Nausea Vomiting Hypotension Nausea Vomiting Bleeding
Anti-fibrinolytic
-aminocaproic acid tranexaemic acid
Inhibit plasminogen activation Preventing fibrinolysis
14
Treatment for Neoplastic Diseases Type Alkylating agents Antimetabolites Drugs Cyclophosphamide Procarbazine Methotrexate 6-mercaptopurine 5-flurouracil Cystosine arabinoside Topotecan Irinotecan Epiphodophyllotoxins Etoposide Teniposide Vincristine Vinblastine Paclitaxel Doxorubicin Epirubicin Uses/ functions - Cell cycle non specific - Attach to DNA bases and interfere with DNA replication - S phase specific - Inhibit synthesis of DNA bases Adverse effects
Camptothecin analogs
S phase specific Interference with DNA cleavage
Anti-mitotic drug
Anthracycline antibiotics
M phase specific Binding tubulin Inhibit polymerization of microtubules Inhibit transcription Inhibit DNA replication
Cytoxicity
Cytotoxicity
15
Drug Treatment of Acid Peptic Disease Type H2 receptor blockers Drugs Cimetidine Ranitidine Famotidine Nizatidine Uses/ Functions - Decrease 60-70% acid secretion - Decrease basal and stimuli induced secretion - Decrease basal nocturnal secretions - Uses: Duodenal ulcer healing Gastric ulcer healing Prophylaxis of aspiration pneumonia GERD healing Stress ulcer healing Treat Zollinger-Ellison syndrome - Ionize and inhibit H-K-ATPase - Supress 80-90% acid secretion - Uses: Bleeding peptic ulcer Adverse effects - Headache - Dizziness - Bowel upset
Proton pump inhibitor
Omeprazole Lansoprazole Pantoprazole (IV) Rabeprazole (IV)
Prostaglandin analogue
Misoprostol
Antacids
Systemic antacids: Sodium bicarbonate Sodium citrate Non-systemic antacids: Magnesium hydroxide Aluminium hydroxide Magnesium trisilicate Magaldrate
increase mucus secretion increase bicarbonate decreased acid and gastrin increase mucosal blood flow prevents NSAID-induced peptic ulcer Uses: Gastritis Systemic acidosis Alkalize urine Non ulcer dyspepsia Episodes of gastritis
- Nausea - Loose stools - Headache - Abdominal pain - Muscle pain - rashes Disadvantages: - Abdominal cramps - Diarrhoea - Uterine bleeding - 4 times/day dose - Systemic alkalosis
Poorly absorbed insoluble
16
Type Sodium Alginate Sulcralfate
Drugs Sodium Alginate Sulcralfate
Eradication of H. pilori
Omeprazole Lansoprazole Amoxicilin Tinidazole Clarithromycin
Uses/ Functions Adverse Effects - forms thick frothy layer floating on gastric contents preventing acid contact with oesophageal mucosa - sticky gel consistency at pH<4 - constipation - coats ulcer base, - 4 times/day dose - precipitate dietary protein - increase mucus, HCO3 secretion - uses: peptic ulcer stress ulcer gastritis stomatitis - Indirect inhibiton of H. pilori by altering acid environment - Direct inhibiton of H. pilori - Triple drug therapy provides faster ulcer healing and lower relapse rates
17
Treatment of Vomiting Type D2 blockers Drugs Metaclopramide Domperidone Uses/ Functions Adverse effects - Increases Lower Oesophageal Sphincter Metaclopramide: - Relax pyloric sphincter - Diarrohea - Increase peristaltic activity - Sedation - Uses: - Acute muscle dystonia All vomiting except labyrinthine cause - Parkinsonism like symptoms Pregnancy vomiting - Galactorrhoea in long use Dyspepsia Domperidone: GERD - Not crossing BBB, so less Parkinsonism like Duodenal intubation symptoms (adv) Gastric stasis - Still have other adverse effects like metaclopramide Prior emergency surgery - Antagonism of the serotonin receptor in CTZ - Headache - Uses: - Abdominal discomfort All vomiting except labyrinthine cause - Constipation Anticancer drug induced vomiting Post anaesthetic Disease induced vomiting Malignancy associated Radiation sickness Pregnancy vomiting - Inhibiting parasympathetic activities Hyoscine: - Causing relaxation of smooth muscle of GIT - Sedation - Uses: - Dryness of mouth Vomiting due to motion sickness, disease of Dicyclomine: inner ear and ototoxic drugs - Dryness of mouth - Hyoscine: - Constipation Prophylaxis of motion sickness - Blurring vision
5-HT3 blockers
Ondasetron Granisetron
Muscarinic blocker
Hyoscine Dicyclomine Prochlorperazine
18
Type H1 blockers
CB1 agonist Corticosteroids
Drugs Promethazine Diphenhydramine Dimenhydrinate Cyclizine Meclizine Cinnarizine receptor Dronabinol Dexamethasone (IV)
Uses/ Functions - Anti-histamine
Adverse effects - Sedation - Psychomotor in coordination - Dryness of mouth - Constipation after long use
Benzodiazepines Pyridoxine
Uses: Cancer chemotherapy-induced vomiting Uses: Anticancer drug vomiting Uses: Anti-emetic effect uses: anti-emetic effect
Psychological effect Sympathomimetic effects
Amnesia sedation
19
Drugs affecting Intestinal Motility Type Bulk-forming agents Drugs Bran Uses/ functions Bran: - Lignin in bran retains water - Increases luminal volume - Increases peristaltic activity Isphagula: - Undergo fermentation by bacterial flora - Forming short chain of fatty acids - Have pro-kinetic action - Increases bacterial mass that contributes increased stool volume - Lower surface tension of stool - Allows mixing of aqueous and fatty substances - Enhances mucosal secretion - Lubricates hard faecal matter - Easy passage of had faecal mass Adverse effects Limitations: - 2,3 days for effect - Unpalatable (unpleasant taste)
Ispaghula
to 1-3 days Abdominal cramps (AE)
Stool softeners & Docusate sodium emollients Liquid paraffin
Stimulant purgatives
Bisacodyl Sodium picosulfate
Saline laxatives
Magnesium sulphate Magnesium hydroxide Magnesium citrate Sodium phosphate Polyethene glycol
- 1-3 days - Bland to taste - Deficiency of fat soluble vitamins Activated by colonic flora Limitations: Interfere with reabsorption of water intestines - Abdominal cramps Increase intestinal secretions - Electrolyte imbalance Stimulate myentric plexus, increases peristaltic - Colonic atony activity Produce soft, semifluid stools in 6-8 hours Retain water in lumen - Cramps Increase peristalsis - Electrolyte imbalance Complete emptying of bowel Watery stools Action in 1-3 hours Uses: Pre-surgical, pre-endoscopic, pre-radiographic colonic cleansing 20
Type Saline laxatives
Drugs Lactulose
5-HT4 agonists
Mosapride Tegaserod
Enema
Tap water Normal saline Glycerin Treatment of Diarrhoea: 1. treatment of fluid depletion (rehydration) 2. correction of shock and acidosis 3. antimicrobial therapy anti-motility drugs Rehydration IV fluids ORS Anti-motility Loperamide - -receptor agonist drugs - increases segmental activity - decreases peristaltic activity Diphenoxylate - decrease secretion - increase anal sphincter tone Atropine - -receptor blocker - decrease peristalsis Racecadotril - Converted into thiorphan in intestine - Inhibits enkepalinase - Increase cAMP concentration - Decreases intestinal secretion
Uses/functions Adverse effects - Colonic bacteria breakdown lactulose into osmotic Limitations: active products - Flatulence - Uses: chronic constipation - Nausea - Enhance Ach secretion - flatulence - Increase cAMP mediated secretion - Uses: Chronic constipation Irritable bowel syndrome - bowel distension causes evacuation reflex - glycerine: lubricates hard faecal mass
abdominal cramps rashes crosses BBB have CNS adverse effects
Nausea Vomiting Drowsiness flatulence
21
Drugs for Diabetes Mellitus Type Sulfonyurea Drugs Glibenclamide Gliclazide Glipizide Glimepiride Repaglinide Nateglinide Sitaglipin Uses/functions - acts on cells - causes depolarization - increase insulin secretion - also decrease glucagon - short duration - only postprandial insulin secretion - preserve beta cell function longer - inhibit enzyme DPP-4 - inhibit degradation of GLP-1 - prolong actions of insulin release - Insulin sensitizers - Enhances insulin inhibition of gluconeogenesis - Increase glucose uptake in muscle Adverse effect - hypoglycaemia - weight gain
Meglitidines
DPP-4 inhibitor
Biguanides
Metformin
Thiazolidinediones Pioglitazone Rosiglitazone
-glucosidase inhibitor
Acarbose Miglitol
Insulin
Rapid acting: Insulin Lispro Insulin Aspart
Activates Peroxisome proliferator activator receptor on nucleus Activates insulin response genes Increase uptake of muscle glucose Decrease gluconeogenesis in liver by same mechanism Inhibit alpha-glucosidase enzyme Prevent dietary carbohydrates from converting to glucose Reduced postprandial hyperglycemia Duration: 3-5 hrs Best control of postprandial sugar Less hypoglycaemia risk
inflammation of nasal mucosa Urinary tract infection Diarrhoea Abdominal discomfort Nausea anorexia metallic taste lactic acidosis Hepatoxicity Weight gain Oedema Anaemia
Abdominal bloating Flatulence Diarrhoea
22
Type Insulin
Drugs Short acting: Regular insulin Intermediate acting: NPH (Isophane) insulin Lente insulin Slow acting: Insulin detemir Insulin glargine
Uses/functions Duration: 6-8 hrs Duration: 20-24 hrs
Adverse effects
Duration: 14 hrs 24 hrs
23
Antithyroid Drugs Types Anti-thyroid agents (Thioamodes group) Drugs Prophylthiouracil Methimazole Carbamizole Uses/Functions - to prevent hormone synthesis - inhibit thyroid peroxidase enzyme - prevent incorporation of iodine into tyrosyl residue - block iodine organification - inhibit coupling of iodotyrosyl groups Prophythiouracil: - inhibit peripheral deiodination of T4 -> T3 Uses: - to control disorder in anticipation of a spontaneous remission - immediately after radioactive iodine to control hypersecretion - control disorder in preparation for surgery - block iodide uptake by gland - Perchlorates competers Na-I-symporters - high concentration if iodide inhibits organification and hormone release - Uses: Preoperative operation before thyroid surgery Thyroid storm use along propranolol and thioamide agent Protect thyroid gland from radioactive agent Adverse Effects - maculopupular pruritic rash - urticarial rash - vasculitis - arthralgia - agranulocytosis
Ionic inhibitor Iodides
Thiocynates Perchlorates Iodides
Perchlorates causes aplastic anaemia hyperthyroidism Swelling of lips, eye lids Angioedema of larynx Joint pain Fever Petechial haemorrhage Iodism Acneiform rash Swollen salivary gland Ulceration of mucosa Rhinorrhea Metallic taste Drug fever
24
Type Radioactive iodine
Drugs I131
I123
Uses/Functions - Emits and particles - Orally administered (80-120 Ci/gm of tissue) - Trapped, incorporated into iodotyrosine - Deposited into colloid - rays ionizing effect leads follicular cell necrosis, disruption and fibrosis without damaging surrounding tissue - rays only - no ionizing effect - for diagnostic scanning
Adverse effects - Delayed hypothyroidism - Contraindicated in young and pregnant woman - Long latent period (3-6 months)
25
Adrenocorticoids Major effects of corticosteroids Glucocorticoids - immunological
Anti-inflammatory
Carbohydrate metabolism
Fat metabolism Protein metabolism
Cardiovascular
Central nervous system Anterior hypothalamus pituitary Mineralcorticoids - Kidney
Effects - Decrease production of T and B lymphocytes and macrophages - Decrease function of T and B lymphocytes - Reduced responsiveness to cytokines - Inhibition of complement system - Reduced production of acute inflammatory mediators - Decrease activity of macrophages and fibroblasts - Reducing numbers and activity of circulating immunocompetent cells, neutrophils and macrophages - Increase gluconeogenesis - Decrease cellular uptake and utilization of glucose - Increase storage of glycogen in liver - Redistribution of lipid from steroid-sensitive stores to steroid resistant stors - Increased catabolism - Decrease anabolism - Protein degradation - Increased sensitivity of vascular system to catecholamines - Reduced capillary permeability leading to raised blood glucose - High levels can cause mood changes or psychotic state and - Reduced endogenous secretion of endogenous glucocorticoids
Increased permeability of apical membrane of cells in distal renal tubule to sodium Stimulation of Na/K ATPase pump leading to reabsorption of Na and loss of K in urine Water retention, leading to increased BP
26
Type Glucocorticoids
Drugs Hydrocortisone (cortisol) Prednisolone Deflazacort Betamethasone Dexamethasone Beclometasone Triamcinolone
Mineralcorticoids
Fludrocortisone
Uses/Functions - Orally for adrenal replacement therapy - Intravenously in status asthmaticus and anaphylactic shock - Orally for allergy and inflammatory disease - Orally for allergy and inflammatory disease - Orally and intravenously - Supress inflammation and allergy - Reduce cerebral oedema - Used as aerosol for asthma - Used as cream and ointment in eczema (anti-inflammatory) - Used in severe asthma - Administered by intra-articular for rheumatoid arthritis - Administered orally with glucocorticoid - Replacement therapy
Adverse effects - Central obesity - Moon face - Hyperglycemia - Osteoporosis - Loss of skin structure - Easy bruising - Muscle weakness - Muscle wasting - Suppression of growth children - Cushings syndromes
in
27
Drugs acting on Kidney Type Loop Diuretics Drugs Frusemide Torasemide Uses/Functions - Inhibition of Na-K-2Cl symport - Decrease Na, K, Cl, H - Increase renal blood flow - Increase venous capacitance acute effect (IV) - Uses: Acute pulmonary oedema Chronic CHF Oedema due to nephrotic syndrome, chronic renal insufficiency Hepatic oedema Acute renal insufficiency Forced diuresis - Inhibit Na-Cl symport - Decrease Na, K, Cl, Mg, H - Increase Ca - Slowly decrease BP - Uses: Hypertension Oedema Renal calcium stone - Increase aldosterone level - Uses: Hypertension Oedema Hepatic cirrhosis Primary hyperaldosteronism - Inhibit renal epithelial Na channels - Uses: Hypertension Oedema Adverse effects - Fluid and electrolyte imbalance - Alkalosis - Ototoxicity - Dyslipidaemia - Hyperglycaemia - Hyperuricemia - Skin rash - Photosensitivity - Diarrhoea
Thiazide diuretics
Hydrochlorothiazide Polythiazide Chlorthalidone Indapamide
Potassium sparing Spironolactone diuretics Eplerenone (Aldosterone antagonist)
Triamterene Amiloride
- Electrolyte imbalance - Uricemia - Glycemia - Dyslipidaemia - Sexual dysfunction - Diarrhoea - Hypersensitivity - Photosensitivity Toxicities: Hyperkalemia Peptic ulcer Sexual characteristic altered Drowsiness Skin rashes Toxicities: Hyperkalemia Diarrhoea Megaloblastic anaemia in cirrhosis Photosensitivity 28
Type
Drugs
Osmotic diuretics
Mannitol
Carbonic Anhydrase Inhibitor
Acetazolamide Dorzolamide
Uses/Functions Potassium sparing diuretics always use with frusemide and thiazides to decrease K loss. Hypokalemia can lead to arrhythmia - Only by intravenous - Increase osmolarity of plasma and tubular fluid - Increase plasma volume - Increase GFR - Uses: Acute renal failure Cerebral oedema Glaucoma - Decrease Na, K, Cl, HCO3 - Uses: Glaucoma Altitude sickness
Adverse effects
Contraindication: Oedema Cerebral haemorrhage
Toxicities: - Allergic - Bone marrow depression - Drowsiness
29
Oral contraceptives Type Oestrogen Drugs Natural oestrogen: 17-estradiol Estrone Estriol Equilin Synthetic oestrogen: Ethinyl estradiol Mestranol Diethylstilbestrol (DES) Dienestrol Uses/ functions Actions: - Development and maturation of female internal and external genitalia - Growth of breasts - Bone growth - Closure of epiphyses - Growth of myometrium and development of endothelium lining - Distribution of subcutaneous fat - Pubic and axillary hair - Ovarian follicular development - Regulation of menstrual cycle Uses: - Hypogonadism - Menstrual abnormalities - Menopausal therapy - Oral contraception - Androgen-dependant prostatic tumour by DES - Bind competitively to oestrogen receptor - Uses: Clomiphene treat infertility in cases of anovulation in women with intact hypothalamic-pituitary axis Fulvestrant treat women with progressive breast cancer after tamoxifen + - Suppress secretion of gonadotrophin of - Follicular secretion, follicular maturation, oestrogen surge, LH surge, and ovulation do not take place - Taken for 21 days with a 7 days of break to induce withdrawal bleed - If taken delay greater than 12 hours, effect may be lost Adverse effects - Nausea - Headaches - Cholestasis - Increased risk of endometrial cancer - Postmenopausal bleeding -
Anti-oestrogen
Clomiphene Fulvestrant Tamoxifen Toremifene
Ovarian enlargement Hot flashes Nausea Vomiting
Combined oral Ethinylestradiol contraceptives analogue progesterone
Nausea Vomiting Headache Weight gain Breast tenderness Impaired liver function Impaired glucose tolerance 30
Type Progesterone-only (minipill)
Drugs Low-dose progesterone
Uses/ functions of Causes thickening of cervical mucus preventing penetration Causes suppression of gonadotrophin secretion Taken orally Taken daily Causes thickening of mucus Causes suppression of gonadotrophin secretion Medroxyprogesterone administered intramuscularly Etonogestrel-releasing implant placed subdermally
Adverse effects sperm Menstrual irregularities Nausea Vomiting Headache Weight gain Breast tenderness
Depotprogesterone
Medroxyprogesterone acetate Etonogestrelreleasing implant Levonorgestrel -
Post-coital pill
Progesterone agonists
Progesterone Medroxyprogesterone Dydrogesterone Hydroxyprogesterone Norethisterone
Progesterone antagonist
Mifepristone
High doses of a progesterone Prevent implantation of fertilized Induced contraction of smooth muscle Accelerate movement of fertilized egg into unprepared uterine endometrium mimics endogenous progesterone taken orally/transdermal patches/subcutaneous implants uses: premenstrual symptoms severe dysmenorrhoea menorrhagia endometriosis contraception hormone replacement therapy Bind to progesterone receptors but did not bring about any effect Sensitize uterus to prostaglandin, for termination of pregnancy Taken orally
Menstrual irregularities Nausea Vomiting Headache dizziness Menstrual irregularities Nausea Vomiting Headache Weight gain Breast tenderness
Vaginal bleeding Faintness Nausea Vomiting
31
Pharmacology of Parkinsons Disease Type Drugs Levodopa Uses/ Functions - Precursor of dopamine - Decarboxylated to dopamine - Bradykinesia and rigidity quickly respond to levodopa - Reduction in tremor - Less effective in eliminating postural instability and shuffling gait - Directly act at striatal dopamine receptors - Use in fairly advanced Parkinson disease Adverse effects - Anorexia - Nausea - Vomiting - Hypertension - Tachycardia - Arrhythmia - Anxiety - Confusion - Delusions - Hallucination - Brownish discolouration of saliva, urine
Dopamine receptor agonist
Pergolide Bromocriptine
Monoaminooxidase inhibitor Antiviral
Selegiline
Amantidine
Irreversible inhibitor of MAO-B Retards breakdown of dopamine Enhances and prolong dopamine effect Use as initial therapy for mild PD
Muscarinic antagonist
Benztropine Trihexiphenidyl Diphenhydramine Biperidin
Use in early PD Drug of choice in drug-induced Parkinsonism: Reserpine Anti-psychotic drugs
Lethargy Dizziness Sleep disturbances Nausea Vomiting Dry mouth Anorexia Urinary retention Drowsiness Mental confusion Restlessness Dryness of mouth Blurred vision Urinary retention Constipation
32
Type COMT Inhibitors
Drugs Tolcapone Entacapone
Uses/ Functions - Increases duration of effect of levodopa - Should be taken with carbidopa/ levodopa - Can reduce dose, thus reduce AE
Adverse effects
33
Sedatives and Hypnotics Type Drugs Benzodiazepines Ultra-short acting (<6hrs) : Triazolam Midazolam Short acting (10-12hrs) : Lorazepam Oxazepam Temazepam Intermediate acting (1218hrs): Alprazolam Nitrazepam Longer acting (12-24hrs): Diazepam Flurazepam Clonazepam Chlordiazepoxide Uses/ functions - Increases frequency of openings of GABAergic channels - Advantages over barbiturates: Lower neuronal depression Wider margin of safety Do not effect REM sleeps Little effect on cardiovascular and respiratory system Flumazenil used for overdosage of BZD - Treating anxiety states: Alprazolam Lorazepam Oxazepam Diazepam Chlordiazepoxide - Treating insomnia: i. Transient insomnia Triazolam temazepam ii. Short term insomnia Temazepam Flurazepam iii. Chronic insomnia Flurazepam Nitrazepam - Pre-anaesthetic and induction of anaesthesia: Diazepam Lorazepam Midazolam - Skeletal muscle relaxation Diazepam Adverse effects - Sedation - CNS depression - Irritability - Excitement - Rage - Ataxia - Confusion - Tolerance and dependence on prolonged use and withdrawal symptoms on stoppage
34
Type Drugs Benzodiazepines
NonZolpidem benzodiazepines Zaleplon hypnotics Zopiclone
blocker
Propanolol
Anti-histamine Anti-depressant Anti-psychotic (neuroleptics) Anxiolytic
Promethazine
Uses/functions - Anticonvulsant: Diazepam Lorazepam Clonazepam (absent seizure) - Alcohol withdrawal Diazepam Oxazepam chlordiazepoxide - Act on BZ1 receptor - Minimal muscle relaxing effect - Minimal anti convulsant effect - Increase slow wave sleep, no effect on REM - Zolpidem and Zaleplon for transient insomnia - Zopiclone for short term insomnia - Uses: Palpitation Tremor GIT upset Hypertension Helps in decrease anxiety - Used in children - Depressed patients improvement of mood - Improve sleep - Promote sleep in resistant insomnia Used for General Anxiety Disorder Partial agonist at 5-HT1A receptor Inhibit serotonin release Induction of anaesthesia Anticonvulsant Epilepsy
Adverse effects
Buspirone
Barbiturates
Thiopental Methohexital Phenobarbital
35
Opiods Analgesic Type agonist Drugs Morphine Uses/ functions - Tranquillity - Euphoria - Decrease fear, anxiety, restlessness - Depress cough - Uses: Cancer pain Fracture pain Post-operative pain Biliary colic MI Left ventricular failure Balanced anaesthesia - Better oral efficacy - Less respiratory depression - Less constipation - Abuse potential unclear - Uses: Musculoskeletal pain Post-operative pain - Uses: Labor pain - High lipid solubility - Quick onset of action by IV route - Short acting - Less respiratory depression by epidural route - Better CV stability - Uses: Labor pain, During surgery, Postoperative pain, cancer pain Adverse effects - Constipation - Physical and psychological tolerance - Nausea - Vomiting - Increase biliary tract pressure - Urinary retention - Hypotension - Pruritus - Drowsiness - Mental clouding - Respiratory depression
Tramodol
Pethidine Fentanyl Sufentanyl
36
Type agonist
Drugs Methadone
Uses/ functions - Uses: As analgesic Treating heroin opioid addicts - Better oral bioavailability - Mild withdrawal reactions
Adverse effects
Opioid antagonist
Naloxone Naltrexone
Morphine congener
Codeine
partial Buprenophrine agonist
agonist
Pentazocine
Intravenous For opioid poisoning Oral Prevent relapse of heroin abuse and alcohol abuse Depress cough centre Uses: Dry cough Musculoskeletal pain Highly lipid soluble Longer duration Uses: Post-operative pain Cancer pain Treating heroin addicts Ceiling effects for analgesia
Constipation Drowsiness
Nalbuphine
Ceiling effects for analgesia
Produce dysphoria Increase BP and heart rate due to sympathetic stimulation Produce dysphoria
37
Pharmacodynamics Pharmacodynamics: study of effects of drugs on body and their mode of actions Drug: chemical substances used for treatment, cure, prevention or diagnosis in human/animal Receptor: specific macromolecular protein which is capable to bind with specific physiological ligand or drug Affinity: ability of a ligand molecule to bind to receptor Efficacy (intrinsic factor): ability of ligand to induce functional change in receptor and trigger response Agonist: has affinity and efficacy Antagonist: Has affinity, lack efficacy Prevent binding of ligand to receptor, prevent physiological action No action from antagonist itself Reversible antagonism: increasing concentration of agonist will overcome antagonism completely (Atropine overcome by Neostigmine) Irreversible antagonism: increasing concentration of agonist will not overcome antagonism
Receptor regulation: Continued receptor stimulation causes decreased availability of receptors, causes desensitization of receptors thus bring about less effectiveness of agonist Continued presence of receptor also causes increased availability of receptors and increased transducer mechanism, causes increase sensitization of receptor, increasing action of agonist and causes withdrawal reaction when drug stop taken.
38
Functional/ Physiological antagonism: Endogenous ligands act at its own receptors which bring about opposite effect E.g adrenaline produce broncodilatation, histamine brings about broncoconstriction
Pharmacological/ receptor antagonism: Drug act as antagonist at receptor
Drug dosage: Def: appropriate amount of drug needed to produce certain degree of response in patient Dosage = amount + dosage form + frequency + duration Regulated dose: dose adjusted by repeat measurement of affected body function E.g antihypertensive, anti-diabetic Target level dose: response to drug not easily measureable. Response expected with certain range of plasma concentration E.g: anti-depressant, anti-epileptic, lithium Titrated dose: maximal dose achieved by titrating with acceptable level of adverse effect E.g: anti-cancer drug, corticosteroids
Drug potency: Amount of drug needed to produce response Higher potency doesnt confer superiority
Drug efficacy: Maximal response of a drug can elicit
39
Drug A is more potent that Drug B Drug C shows lowest potency and lowest efficacy Drug A and B have same efficacy Drug A and B have same efficacy Drug A is more potent than B Drug C and D have same efficacy Drug D is more potent than C C and D is have less efficacy than A and B
40
Safety Margin of a drug: Dose of drug need to be increased to obtain maximum beneficial effects until the dosage that gives toxic effect Therapeutic/Safety range is bound by dose that which minimal therapeutic effect and dose that produce maximal acceptable toxic effect Wider the safety margin, safer the drug
Therapeutic Index: TD50/ED50 TD50: dose that produce toxic effect in 50% of human ED50: dose that produce desired effect in 50% of population
41
Treatment of Malaria Type 4-aminoquinolines Drugs Chloroquine Amodiaquine Uses/Functions - Treatment of P. vivax, ovale and malariae - Does not produce radical cure - Interferes with parasite haem detoxification - Dosage: tablets of 100mg or 150mg - Amodiaquinie: ACT for chloroquine resistrant Falciparum Adverse effects - Nausea - Vomiting - Skin rashes - Itching - Headache - Visual disturbance - Prolonged administration may cause irreversible retinopathy as in treatment of rheumatoid arthritis cinchonism hypoglycaemia hypotension large doses can cause hypotension, cardiac arrhythmia and AV block
Quinoline methanol Cinchona alkaloid
Mefloquine Quinine Quinidine
Biguanide Diaminopyrimidines 8-Aminoquinoline
Proguanil Pyrimethamine Primaquine
Effective blood schizonticide Act on mature trophozoite stage Also kills sexual stages of P.vivax, malariae,and ovale but not mature gametocytes of falciparum Preparation: i) tablets of quinine hydrochloride, quinine dihydrochloride, quinine sulphate and quinine bisulfate ii) injections of quinine hydrochloride, quinine dihydrochlorie, and quinine sulphate Prophylaxis of malaria with choloroquine Inhibit dihydrofolate reducatase of Plasmodium Used with sulfadoxine effective against intrahepatic forms of all types of malaria parasite used to provide radical cure of P. vivax and P. ovale preparations: tablets of 5 mg, 7.5 mg, 15 mg primaquine diphosphate
Megaloblastic anaemia Folate deficiency haemolytic anaemia in G6PD deficiency patient abdominal pain leucocytosis leukopenia agranulocytosis GI symptoms
Sulfonamides, Sulfones
Sulfadoxine Dapsone
Produce sequential block in folate and inhibits synthesis of purines and pyrimidines 42
Types Tetracyclines Sesquiterpine lactones
Drugs Tetracycline Doxycycline Artesunate Artemether Arteether
Amino alcohols
Halofantrine Lumifantrine
Naphthoquinone
Atovaquone
Uses/functions - Short term prophylaxis in areas with multiresistant strains of Plasmodia - Attack from young rings to schizont - Active against all Plasmodium species - Also kills falciparum gametocytes - Inhibit essential calcium adenosine triphosphate - Artemether preparations: i) Capsule of 40mg arthemether ii) Tablet of 50 mg iii) 80mg injection iv) 20mg of arthemether with 120mg lumefantrine - Artesunate preparation: i) Artesunic acid + sodium bicarbonate = sodium artesunate right before injection ii) Also by oral(50mg/200mg), rectal(100mg/400mg) or IM - Artheether i) IM injection of 150mg of artemotil in 2ml of injectable solution Halofantrine - Blood schizonticide - Active against Falciparum Lumifantrine - Long acting erythrocytic schizonticide - Inhibit heme polymerization and inhibition of protein and nucleic acid synthesis - Used only in combination with artemether - Inhibit electron transport to reduce membrane potential of mitochondria - Admin with proguanil - Treatment and prophylaxis of Falciparum
Adverse effects
GI disturbance Dizziness Tinnitus Reticulocytopenia Neutropenia ECG abnormalities
GI disturbance Headache Rash
43
Beta lactam antibiotics & cell wall inhibitor antibiotics Types Natural penicillin Drug Penicillin G Uses/functions - B-lactamase sensitive - For gram positive cocci: streptococcus pyogenes, s. pneumonia, s. viridans, s. faecalis - For gram positive bacilli: c. tetani, c. perfringes, c. diptherie, B. anthrasis, Listeria monocytogenes - Prophylactic: rheumatic fever, bacterial endocarditis Adverse effects - Allergy - Superinfections by Candida - Diarrhoea - Haemolysis - Nephritis - Neurotoxicity - Jarisch-Herxheimer reaction
Acid resistant penicillin
Penicillinase resistant penicillin
Aminopenicillin
Procain penicillin Benzathin penicillin Phenoxy methyl - Acid stable penicillin - For minor infections - Effective against anaerobic organisms - Prophylaxis of rheumatic carditis Methicillin - Used in infections by penicillinase-producing Oxacillin staphylococci Cloxacillin - Used in skin and soft tissue infection Dicloxacillin Nafcillin Flucloxacillin Ampicillin Ampicillin Becampicillin - Broad spectrum: effective against Gram Talampicillin positive bacilli and gram negative bacilli Amoxicillin - Uses: bite wound infection, enterococci endocarditis, intra-abdominal/ skin/soft tissue infections, meningitis
44
Types Carboxypenicillin Ureidopenicillin
Drugs Carbenicillin Indanyl carbenicillin Mezlocillin Ticarcillin Piperacillin
Uses/ functions
Adverse effects
First generation cephalosporins
Cephazolin Cephalexin Cephadroxyl
Second generation cephalosporins
Cefotixin Cefaclor Cefuroxime axetil Cefuroxime
Effective against Pseudomonas aeruginosa Effective against gram negative bacilli except Klebsiella Uses: intra-abdominal/skin/soft tissue infection, nosocomial pneumonia Effective against gram positive cocci e.g Proteus mirabilis, E. coli, Klebsiella pneumonia Uses: skin infection of staphylococci or streptococci UTI due to E. coli Cephazolin used to prevent invection of staphylococci and aerobic enteric bacilli during surgery Active against S. aureus, S. pyrogens, S. pneumonae, Haemophilus influenza, Enterobacter aerogenes, Neisseria species, Proteus mirabilis, E. coli, Klebsiella pneumonie, Serratia marcescens Uses: Cefotixin: diverticulitis, pelvic inflammatory disease, prevention of infections during surgical procedure Cefuroxime(oral): Respiratory tract, skin infections and UTI Cefuroxime(parenteral): community acquired pneumonia, pneumonia due to H. influenza or Pneumococci
Haemolytic anaemia Thrombocytopenia Interstitial nephritis Abnormal liver function test
45
Types Third generation cephalosporins
Drugs Cefixime Cefotaxime Ceftriaxone
Fourth generation cephalosporins
Cefipime Cefpirome
Monobactams
Aztreonam
Carbapenems
Imipenem Meropenem Ertapenem
Uses/functions - Gram negative action - Can cross BBB - Activity against pseudomonas Uses: - Cefixime gonorrhoea, otitis media - Cefotaxime and Ceftriaxone septicaemia, pneumonia, gonorrhoea, intra-abdominal infections, osteomyelitis, otitis media, skin infections, soft tissue infections, UTI - Ceftazidime Pseudomonas aeruginosa infections - Activity against both gram positive and negative bacteria - Used to treat infections due to multi drug resistant organisms in hospital - Active against Gram negative rods e.g Klebsiella, Pseudomonas and Serratia - Used in penicillin allergic patients, renal insufficiency and patient that cant tolerate amino glycosides - Drug of choice for initial empirical therapy in severe infections - Uses: - Infections due to multidrug resistant gram negatives bacilli, drug of choice for ennterobacter, intra-abdominal infections, pelvic, skin, soft tissue, bone, joint, urinary, respiratory and nosocomial infections - Imipenem combined with cilastatin - Meropenem and ertapenem have less renal and CNS toxicity
Adverse effects - Opportunistic infection with resistant bacteria or candida albicans or C. difficile diarrhoea - Cholethiasis (ceftriaxone)
Occasional GI upset
GI upset Allergic reactions CNS effect convulsion)
(confusion,
46
Type Cell wall synthesis inhibitor
Drugs Vancomycin
Teicoplanin Daptomycin Bacitracin
Uses/ functions Adverse effects - Inhibit gram positive bacterial cell wall - Redmans syndrome synthesis - Used for MRSA and infections due to IV catheters, pseudomembranous colitis (used with metronidazole) - Same as vancomycin Topical antibiotic Combined with neomycin, polymyxin B and corticosteroids Demonstrates synergistic activity against enterococci, MRSA when combined with cephalosporins, aminoglycosides and others
Fosfomycin
47
Macrolides and protein synthesis inhibitor Type Macrolides Drugs Erythromycin Uses/functions - Effective against Gram positive bacteria and spirochaetes - Not effective against Gram negative except for Neisseria gonorrhoeae and H. influenza Adverse effects - GI upset - Rashes - Fever - Transient hearing disturbance - Cholestatic jaundice - Epigastric pain - Thrombophlebitis - Opportunistic infection of GI/ vagina
Azithromycin
Clarithromycin
Ketolides Telithromycin Lincosamides Clindamycin -
Effective against Gram postitive Bacteria More effective against H. influenza More active against Legionella Excellent action against Toxoplasma gondii Twice more affective against H. influenza compared to erythromycin Effective against Mycobacterium avium-intercellulare Useful in leprosy and against H. pylori Macrolides are drug of choice for M. pneumonae infections, Legionnaires pneumonia, Chlamydial infection, Diphtheria, Pertussis, Alternative drugs in tetanus, streptococcal tonsillitis, pharyngitis, pneumonia, mild staphylococcal infection Prophylactic drug in rheumatic fever after surgery of valvular lesion to prevent endocarditis Have increased activity against erythromycin resistant gram positive cocci such as S. pneumonia Effective against H. influenza, C. pneumonia, M. catarrhalis, Bordetella pertussis, and Legionella pneumophila Effective against Gram-positive cocci Inhibit protein synthesis Used in infection by Bacteroides organisms and Staphylococcal infection of bones and joints
GI disturbance Pseudomembranous colitis
48
Type Oxazolidinones
Drugs Linezolid
Streptogramins Quinupristin Dalfopristin -
Uses/functions Active against wide variety of Gram-postive bactria Used in treatment of MRSA, penicillin-resistant Streptococcus pneumonia and vancomycin-resistant enterococci To treat pneumonia, septicaemia, skin and soft tissue infections Inhibit bacterial protein synthesis by binding to a site on 50s ribosomal subunit individually exhibit bacteriostatic activity combined together as IV injection, they are active against Gram-positive bacteria effective against MRSA and vancomycin-resistant Enterococcal faecium
Adverse effects - Thrombocytopenia - Diarrhoea - Nausea - Rash - dizziness
infusion site inflammation pain arthralgia myalgia nausea vomiting diarrhoea
49
Fluoroquinolones and Aminoglycosides Type Quinolone Drugs Nalidixic acid 1st Generation: Norfloxacin (oral) 2nd Generation: Ciprofloxacin (oral, topical, IV) Ofloxacin Pefloxacin 3rd Generation: Levofloxacin Lemofloxacin Gatifloxacin Moxifloxacin 4th Generation Trovafloxacin Streptomycin Tobramycin Kanamycin Neomycin Soframycin Gentamicin Amikacin Netilmicin Uses/ Functions - Inhibit bacterial DNA gyrase - Prevent supercoiling of DNA - Inhibit topoisomerase IV in gram positive bacteria - Bactericidal in nature - 1st and 2nd generation highly effective against gram negative organisms - 3rd generation effective against streptococci and anaerobes - 4th generation effective against gram positive and anaerobes - Uses: UTI, gonorrhoea, Thyphoid, septicemias, meningitis Nalidixic acid for chronic UTI and diarrhoea bind to 30S ribosomal subunit inhibit protein synthesis bactericidal active against aerobic gram negative bacilli, staphylococci, mycobacteria combined with penicillin G/ampicillin/vancomycin for enterococci uses: gentamicin for enterococci septicaemia streptomycin for tuberculosis neomycin and framycetin for ear and eye infection Adverse effects - GI upset - Allergic reaction - Dizziness - Headache - Confusion - arthropathy
Aminoglycosides
Ototoxicity Tinnitus Headache Dizziness Nausea Nephrotoxicity Neuromuscular block
50
Broad spectrum antibioticss Types Chloramphenicol Drugs Chloramphenicol Uses/functions - Binds to 50s subunit respectively - Inhibit transpeptidation - Block binding of aminoacyl moiety of tRNA to mRNA complex - Inhibited by hepatic glucoronosyltransferase - Uses: Bacteriostatic Bactericidal for H. influenza, N. meningitides, Bacteroides Treatment of pneumococcal and meningococcal meningitis in beta-lactam-sensitive person Used in infections where tetracycline is contraindicated Used in combination with metronidazole for treatment of abscess Brucellosis where tetracycline is contraindicated Short acting (6-12 hrs): - Bind to 30S Tetracycline - Blocks Chlortetracycline - Impaired by food and multivalent cations Oxytetracycline - Uses: Against gram positive and negative M. pneumoniae (tetracycline) Intermediate acting Chlamydia (12-16hrs): Granuloma inguinale Demeclocycline Rickettsia Long acting (16Vibrio cholera 24hrs): Acne Doxycycline GI ulcers by H. pylori Minocycline Amoebiasis Lyme disease Adverse effects - GI disturbances - Candidiasis - Anaemia - Leukopenia - Thrombocytopenia - Gray baby syndrome
Tetracycline
GI disturbances Candidiasis Tooth enamel dysplasia Irregularities in bone growth Hepatic toxicity Fanconis syndrome Photosensitivity (Demeclocycline) Vestibular toxicity
51
Types Cotrimoxazole
Drugs Cotrimoxazole
Uses/functions - Bacteriostatic - Produce sequential blocks - Uses: Lower UTI Respiratory tract infections Bacterial diarrhoeas Typhoid fever P. carinii infections Meliodosis Chancroid
Adverse effects - Skin rashes - GI disturbances - Exfoliative dermatitis - Nausea - Vomiting - Megaloblastic anaemia
52
Anti-Tubercular Drug
Type
Drugs Pyrazinamide
Ethambutol
Rifampicin
Uses/ functions - Weak bactericidal - Active in acidic - Lethal to intracellular Uses: Multiagents short-term therapy of uncomplicated pulmonary tuberculosis - Bacteriostatic - Inhibit cell wall synthesis - Supresses growth of INH & streptomycin-resistant tubercle bacilli - Bactericidal to M. tuberculosis - Effective against all subpopulation of mycobacteria - Active against extra&intracellular organisms Bactericidal Effective against intra & extracellular bacilli Active in acidic and alkaline media Bactericidal Effective only against extracellular bacilli Only as IM injection
Isoniazid
Streptomycin
Adverse effects - Liver damage - Hyperuricemia - Gout - Rashes - Arthralgia - Optic neuritis - Red-green colour blindness - C/I: children <6 y.old - Hepatitis - Body secretion become reddish orange - Leprosy - Hepatic injury - Peripheral neuritis - Urinary retention - Insomnia - VIII cranial nerve damage - Problem with hearing and balance - Nephrotoxicity
53
S-ar putea să vă placă și
- DrugsDocument7 paginiDrugsCaine ReganÎncă nu există evaluări
- List of Opioids in The UDocument3 paginiList of Opioids in The UmchalftzÎncă nu există evaluări
- Article Tainted Money PDFDocument18 paginiArticle Tainted Money PDFMuhammad Arif HasbullahÎncă nu există evaluări
- Freak's Scoring Essentials: Principle 1: Efficiency Is KeyDocument6 paginiFreak's Scoring Essentials: Principle 1: Efficiency Is KeyVlad TincuÎncă nu există evaluări
- What Is ScamDocument1 paginăWhat Is Scamniraj4uall1947Încă nu există evaluări
- Balance ExercisesDocument1 paginăBalance Exercisesteam_moÎncă nu există evaluări
- Surefire Ways To Get Taken by Identity ThievesDocument3 paginiSurefire Ways To Get Taken by Identity ThievesvietrossÎncă nu există evaluări
- Poison & Antidote Chart IWK Regional Poison Cen PDFDocument1 paginăPoison & Antidote Chart IWK Regional Poison Cen PDFdeeptiÎncă nu există evaluări
- Low BP - Decreased Cardiac Output - Improved Renal Blood FlowDocument2 paginiLow BP - Decreased Cardiac Output - Improved Renal Blood Flowtantalizin marieÎncă nu există evaluări
- 筆記 下肢神經Document1 pagină筆記 下肢神經屏頂大Încă nu există evaluări
- How To Attack Effectively - Roy Saunders Sep 2007Document5 paginiHow To Attack Effectively - Roy Saunders Sep 2007Juan Pablo Varela de la ColinaÎncă nu există evaluări
- Football Speed and Agility Training ProgramDocument24 paginiFootball Speed and Agility Training ProgramAdolfo Enciso EsquivelÎncă nu există evaluări
- Endurance For BowlingDocument3 paginiEndurance For BowlingEzaim DweomermasterÎncă nu există evaluări
- Speed & Agility InformationDocument10 paginiSpeed & Agility InformationFioravanti AlessandroÎncă nu există evaluări
- Semester 2 Drug ListDocument7 paginiSemester 2 Drug ListNam_Pham_6481Încă nu există evaluări
- Congestive Heart Failure: CardiacDocument36 paginiCongestive Heart Failure: CardiacHUZAIFA YAMAANÎncă nu există evaluări
- Drugs ClassificationDocument24 paginiDrugs ClassificationManda HoÎncă nu există evaluări
- Pharmacological Management of Ischaemic Heart Disease and Acute Myocardial InfarctionDocument50 paginiPharmacological Management of Ischaemic Heart Disease and Acute Myocardial InfarctionMuh Akbar BaharÎncă nu există evaluări
- Antihypertensive DrugsDocument7 paginiAntihypertensive Drugshamadadodo7Încă nu există evaluări
- Cardiotonic DrugsDocument67 paginiCardiotonic DrugsLady Mae Ramos100% (1)
- Heart Failure and Its Drug ClassificationDocument37 paginiHeart Failure and Its Drug ClassificationMaham AzmatÎncă nu există evaluări
- PharmacologyDocument23 paginiPharmacologyAbhisek ChatterjeeÎncă nu există evaluări
- Cholinergic System: e CarbamatesDocument26 paginiCholinergic System: e CarbamatesAcai BoncaiÎncă nu există evaluări
- Cardiovascular PharmacologyDocument61 paginiCardiovascular PharmacologyTeeOne920% (1)
- List of Drugs Pharmacology 2Document13 paginiList of Drugs Pharmacology 2Maisarah Ab SamadÎncă nu există evaluări
- Anti-Hypertensive DrugsDocument56 paginiAnti-Hypertensive Drugsapi-3815243Încă nu există evaluări
- Pharmacology: Teratogenic CarcinogenicDocument13 paginiPharmacology: Teratogenic CarcinogenicSherlock HolmesÎncă nu există evaluări
- MS2 USMLE Pharm ReviewDocument25 paginiMS2 USMLE Pharm ReviewAnna ArtyÎncă nu există evaluări
- Review Handouts For Medical Pharmacology: Terriann Crisp, PH.DDocument28 paginiReview Handouts For Medical Pharmacology: Terriann Crisp, PH.Dmus zaharaÎncă nu există evaluări
- Angina Pharmacology YeahDocument16 paginiAngina Pharmacology YeahMuhammad AfifuddinÎncă nu există evaluări
- PantoprazoleDocument10 paginiPantoprazoleTheresa AbrilloÎncă nu există evaluări
- Pharmacology: Unit VIIIDocument92 paginiPharmacology: Unit VIIIChristian Laraya AlayonÎncă nu există evaluări
- Department of Clinical Pharmacology: Pharmacotherapy of Chronic Ischemic Heart DiseaseDocument84 paginiDepartment of Clinical Pharmacology: Pharmacotherapy of Chronic Ischemic Heart DiseasePatty ReyesÎncă nu există evaluări
- Drug ListsDocument10 paginiDrug ListsAmber Merritt100% (1)
- Rug Therapy For Heart Failure: Dr. Santhosh RamakrishnaDocument40 paginiRug Therapy For Heart Failure: Dr. Santhosh RamakrishnaNiteesh Kumar SharmaÎncă nu există evaluări
- Alpha Blockers PharmacologyDocument23 paginiAlpha Blockers PharmacologyHesbon MomanyiÎncă nu există evaluări
- CardiotonicsDocument21 paginiCardiotonicsmohsen mirdamadiÎncă nu există evaluări
- Anti Hypertensive 20191211Document35 paginiAnti Hypertensive 20191211helloitsmenadÎncă nu există evaluări
- Meds #1 NotesDocument4 paginiMeds #1 NotesAnh TrinhÎncă nu există evaluări
- MC Ii Unit IiiDocument38 paginiMC Ii Unit IiinallamillipavithraÎncă nu există evaluări
- CVPR Prototype Drugs TableDocument27 paginiCVPR Prototype Drugs TablethommyvaÎncă nu există evaluări
- PharmaDocument11 paginiPharmaGohar KamranÎncă nu există evaluări
- CVD and HTNDocument60 paginiCVD and HTNZsazsa100% (1)
- Cardiovascular Pharmacology OutlineDocument11 paginiCardiovascular Pharmacology OutlineLhay de OcampoÎncă nu există evaluări
- Pharm - Pure & SimpleDocument33 paginiPharm - Pure & SimpleBlake FarberÎncă nu există evaluări
- Obat Gagal Jantung N Anti AnginaDocument42 paginiObat Gagal Jantung N Anti AnginaAyu Devi YantiÎncă nu există evaluări
- Cardio Winter BreakDocument13 paginiCardio Winter Breakmadhungry34Încă nu există evaluări
- Pharmacology Mnemonics.Document16 paginiPharmacology Mnemonics.Shan Shani67% (3)
- 17 Cardiac DrugsDocument6 pagini17 Cardiac DrugshiwaralelataÎncă nu există evaluări
- Beta Blockers and Calcium Channel BlockersDocument34 paginiBeta Blockers and Calcium Channel Blockersnevena.stankovic986Încă nu există evaluări
- Pharm MnemonicsDocument33 paginiPharm MnemonicsThomson George75% (4)
- Antianginal Drugs Are Used Primarily To Restore The Balance Between The Oxygen SupplyDocument8 paginiAntianginal Drugs Are Used Primarily To Restore The Balance Between The Oxygen SupplyUzma KhanÎncă nu există evaluări
- Awhai April 2023Document11 paginiAwhai April 2023Mac Gerald CuetoÎncă nu există evaluări
- Anti Anginal DrugsDocument60 paginiAnti Anginal DrugsPranish SawantÎncă nu există evaluări
- Drugs Used in The Treatment of Cardiac Failure: Assoc. Prof. Iv. Lambev WWW - Medpharm-Sofia - EuDocument38 paginiDrugs Used in The Treatment of Cardiac Failure: Assoc. Prof. Iv. Lambev WWW - Medpharm-Sofia - EuYeshaa MiraniÎncă nu există evaluări
- Cardio Lab MedsDocument11 paginiCardio Lab MedsDianne Erika MeguinesÎncă nu există evaluări
- Pharmacology Important Things To RememberDocument5 paginiPharmacology Important Things To RememberHydie100% (1)
- Smooth MuscleDocument7 paginiSmooth MusclewanichysonlyÎncă nu există evaluări
- 10-11 Treatment of HypertensionDocument11 pagini10-11 Treatment of HypertensionHanif GandohÎncă nu există evaluări
- Delinda Marti (1800010) - (2) Antihipertensi - Farmakologi 1Document35 paginiDelinda Marti (1800010) - (2) Antihipertensi - Farmakologi 1Devi Septiani D3-2019Încă nu există evaluări
- Nursing Care Plan: Nikolai P. Funcion, FSUU-SNDocument5 paginiNursing Care Plan: Nikolai P. Funcion, FSUU-SNNikolai FuncionÎncă nu există evaluări
- Chinese General Hospital College of Nursing Nursing Care PlanDocument2 paginiChinese General Hospital College of Nursing Nursing Care PlanKenji ToleroÎncă nu există evaluări
- Health 7 1st Quiz #02 Health Concerns and Health AppraisalDocument2 paginiHealth 7 1st Quiz #02 Health Concerns and Health Appraisalryan bersaminÎncă nu există evaluări
- Bio CrystalDocument32 paginiBio CrystalMarija PapaÎncă nu există evaluări
- Manual FFHH Oaci (Ingles)Document335 paginiManual FFHH Oaci (Ingles)Pran Antonio EscobarÎncă nu există evaluări
- Sleep: Dr. John BergmanDocument42 paginiSleep: Dr. John BergmanAndrew FongÎncă nu există evaluări
- Thesis Statement On Sleep DisordersDocument7 paginiThesis Statement On Sleep Disordersafkoliddh100% (2)
- Argumentative EssayDocument7 paginiArgumentative EssayHoang Thi Huyen DieuÎncă nu există evaluări
- LACOSAMIDE TABLETSMedGuideDocument5 paginiLACOSAMIDE TABLETSMedGuideEko YuliantoÎncă nu există evaluări
- Barnes 2019Document7 paginiBarnes 2019José VitorÎncă nu există evaluări
- Final Research Paper Group 4Document64 paginiFinal Research Paper Group 4Airey Alasan EconarÎncă nu există evaluări
- Buteyko Meets DR MewDocument176 paginiButeyko Meets DR MewAnonymous hndaj8zCA100% (1)
- Assessment Diagnosis Background Planning Implementation Rationale Evaluation Short Term GoalsDocument2 paginiAssessment Diagnosis Background Planning Implementation Rationale Evaluation Short Term GoalsKenneth Gabriel Catulin50% (2)
- Stress and Health - 2020 - Benham - Stress and Sleep in College Students Prior To and During The COVID 19 PandemicDocument12 paginiStress and Health - 2020 - Benham - Stress and Sleep in College Students Prior To and During The COVID 19 PandemicchatarinaÎncă nu există evaluări
- Anxiolytic, Sedative-Hypnotic DrugsDocument39 paginiAnxiolytic, Sedative-Hypnotic DrugsNina100% (1)
- Management of Stress Induced Insomnia Through AyurvedaDocument5 paginiManagement of Stress Induced Insomnia Through AyurvedaIJAR JOURNALÎncă nu există evaluări
- Test Bank For Stress Management For Life A Research Based Experiential Approach 5th Edition Michael Olpin Margie HessonDocument36 paginiTest Bank For Stress Management For Life A Research Based Experiential Approach 5th Edition Michael Olpin Margie Hessonjocosevannerh98oj100% (41)
- LACOSAMIDE ORAL SOLUTIONMed GuideDocument4 paginiLACOSAMIDE ORAL SOLUTIONMed GuideEko YuliantoÎncă nu există evaluări
- STRFTT Dod Blog: Street FoodDocument6 paginiSTRFTT Dod Blog: Street FoodOlgaÎncă nu există evaluări
- Post Traumatic Stress DisorderDocument23 paginiPost Traumatic Stress Disorderapi-379794175% (4)
- 4-6 SL PsychostimulantsDocument35 pagini4-6 SL PsychostimulantsMichiko MeritasariÎncă nu există evaluări
- LitCharts: Nearing Forty by Derek WalcottDocument12 paginiLitCharts: Nearing Forty by Derek Walcottreya100% (1)
- A Case of Chronic Insomnia Cured by HomoeopathyDocument6 paginiA Case of Chronic Insomnia Cured by HomoeopathyHomoeopathic Pulse100% (2)
- Blueprint 5 Workbook Answer KeyDocument52 paginiBlueprint 5 Workbook Answer KeyAngelo Mejia100% (2)
- Class 9 EnglishDocument11 paginiClass 9 EnglishAS empireÎncă nu există evaluări
- Sleep Wake DisordersDocument5 paginiSleep Wake DisordersIsabel CastilloÎncă nu există evaluări
- How To Fall AsleepDocument10 paginiHow To Fall AsleepmidowakilÎncă nu există evaluări
- Flurazepam Prescribing InformationDocument2 paginiFlurazepam Prescribing InformationMohammed Shamiul ShahidÎncă nu există evaluări
- Geriatrics Board Review: October 9,2009Document95 paginiGeriatrics Board Review: October 9,2009Charis Paroginog100% (2)
- Sleeping ProblemsDocument24 paginiSleeping ProblemsMariam MatchavarianiÎncă nu există evaluări