Documente Academic
Documente Profesional
Documente Cultură
Dengue Shock Syndrome Case with Pleural Effusion
Încărcat de
Fred CapiliDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Dengue Shock Syndrome Case with Pleural Effusion
Încărcat de
Fred CapiliDrepturi de autor:
Formate disponibile
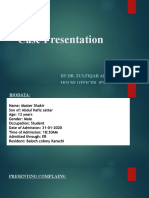
A CASE ON DENGUE SHOCK SYNDROME This is a case of an 8 yr old female born December 6, 2002, from Pililia, Rizal who
came in with a chief complaint of fever. Four days PTA, patient had fever Tmax 39C accompanied by cough dry and watery nasal discharge and headache. Consult was done at Tanay Hospital where impression was unknown and she was given Cefalexin 5 ml TID and Paracetamol. Three days PTA, patient still had fever, intermittent, now accompanied by abdominal pain. No other symptoms were noted and no consult was done. One day PTA, still with fever, intermittent, accompanied by abdominal pain and headache, consult at Tanay General Hospital was done where BP was noted to be 70/40. Patient was admitted and was given PNSS as fast drip for 3 doses. Hypotension persisted and Dopamine and Dobutamine were given until it was increased to 15cc/hr due to persistence of hypotension. CBC showed Hgb 135 Hct 0.40 WBC 5.0 neutrophils 0.55 lymphocytes 0.45 platelet 124. Chext Xray showed pleural effusion. Due to persistence of symptoms, patient was then transferred to our institution. This is the patients 1st hospitalization. She is the second of two children. There are reported cases of dengue in their community and school. They have a family history of asthma. Their family lives in a mountainous area. Water is boiled from the faucet and electricity is from meralco. At the ER, patient was drowsy, in respiratory distress with the ff vital signs: BP unappreciated, CR 123 RR 44 Temp 36.3 with puffy eyelids, petechiae at the upper extremities, symmetrical chest expansion, with retractions, decreased breath sounds at both lower lung fields, adynamic precordium, tachycardic, no murmurs, distended abdomen, liver edge at 3cm BRCM with poor pulses and CRT 3secs. Patient was admitted as a case of Dengue shock syndrome with bilateral pleural effusion. Patient was placed on NPO with O2 face mask at 5lpm. Dopamine and dobutamine were maintained at 15cc/hr and D5LRS at 55cc/hr (MR). Furosemide was started. The ff labs were done: CBC: Hgb 170 hct 0.51 wbc 6.5 neutro 0.66 lympho 0.34 platelet 61 PT 13.9 (12.5) PTT 87.3 (35.2) INR 1.15 Na137 Albumin 20 SGPT 31 SGOT 120 AlkPO4 61 At the ER, patient was then noted to have palpatory BP 70 with weak pulses hence epinephrine drip was started. On the 1st ICU day, patient was afebrile, CR 140-150 RR 40s BP 110-120/70-80. Patient still had tachypnea. Patient was conscious, coherent, in distress. Symmetrical chest expansion, with decreased breath sounds at both lower lungfields. Abdomen is distended, circumference of 59with flank fullness. FFP transfusion was given. Repeat CBC showed Hgb163 Hct 0.49 WBC 14.3 Neutro 0.60 Lymph 0.39 Platelet 40. LDH 689 CKMB 55. 12 L ECG was also done. Dopamine, Dobutamine, and epinephrine drip were continued. Furosemide drip was also continued. On the 2nd ICU day, day 2 afebrile, patient is still tachypneic with RR 40s, subcostal retractions, decreased breath sounds on both lower lung fields. BP was 100-120/60-80 CR 90-120s Abdomen is distended. Pulses were full and equal. Urine output was adequate at 2.4cc/kg/hr. Epinephrine drip was discontinued. Dopamine and dobutamine drip was decreased to 5cc/hr. Albumin transfusion was given. Repeat CBC showed Hgb 140 hct 0.42 WBC 16.4 Neutro 0.71 Lymph 0.29 Platelet 80.
On the 3rd ICU day, day 3 afebrile. Bp range 90-120/60-80 CR 100-120 RR20-30. Patient had no difficulty of breathing. Symmetrical chest expansion, no retractions, with decreased breath sounds at the left basal lungfields. Abdominal circumference was 57cm, nondistended, soft, non tender. Pulses were full and equal. Urine output was adequate at 3.2cc/kg/hr. Repeat CBC showed Hgb 110 Hct 0.33 WBC 15 Neutro 49 Lympho 51 Platelet 60 PT 12.1(14.1) PTT 51.1(34.1). Dopa-Dobu drip was decreased to 3cc/hr and Furosemide drip was discontinued. IV Furosemide was started q8. IVF was shifted to D5IMB at maintenance rate. On the 4th ICU day, day 4 afebrile. BP range 90-120/60-80 CR 90-110 RR 20s Patient had no subjective complaints. She had symmetrical chest expansion, no retractions with decreased breath sounds at left basal lung fields.Abdomen was flat with normoactive bowel sounds, soft, nontender, no organomegaly.Pulses were full and equal. Urine output was at 4cc/kg/hr. Repeat CBC showed Hgb 106 Hct 0.32 WBC 6.6 neutro 52 Lympho 48 platelet 85. Dopa-dobutamine drip and furosemide drip were discontinued. Patient was then transferred to ward. IV line was shifted to hepline. Patient then discharged home and was advised follow up at General OPD and Cardio OPD.
S-ar putea să vă placă și
- Hospital Case PneumothoraxDocument9 paginiHospital Case PneumothoraxJohn Rendel LopezÎncă nu există evaluări
- Endorsement Week 9Document13 paginiEndorsement Week 9MICHELLE FACTOÎncă nu există evaluări
- Careplan IsbarDocument3 paginiCareplan IsbarAmanda SimpsonÎncă nu există evaluări
- Cor Pulmonale et Causa SOPT Pasca TuberkulosisDocument32 paginiCor Pulmonale et Causa SOPT Pasca TuberkulosisBrinna Anindita SatriaÎncă nu există evaluări
- Polytrauma Patient Death from Sepsis ComplicationsDocument3 paginiPolytrauma Patient Death from Sepsis ComplicationsSiva SankarÎncă nu există evaluări
- Mortality by YvonneDocument25 paginiMortality by YvonneYvonne SiiloÎncă nu există evaluări
- Pedia BAIEDocument49 paginiPedia BAIEDarlene Clarice V. LabacladoÎncă nu există evaluări
- RESIDENTS NOTES LUCEDADocument2 paginiRESIDENTS NOTES LUCEDARizielle MendozaÎncă nu există evaluări
- 'Batangas Medical Center Case Report by PGI Carlos H. AcuñaDocument7 pagini'Batangas Medical Center Case Report by PGI Carlos H. AcuñaCarlos H. AcuñaÎncă nu există evaluări
- Clinico-Pathologic Case Presentation: GroupDocument27 paginiClinico-Pathologic Case Presentation: GroupMichelle Vera GabunÎncă nu există evaluări
- Mock CodeDocument4 paginiMock CodeKrezielDulosEscobarÎncă nu există evaluări
- Staff Round: Ward 32 Prof. N. Gupta UnitDocument22 paginiStaff Round: Ward 32 Prof. N. Gupta UnitSaroj SahooÎncă nu există evaluări
- ER: Perforated Peptic Ulcer Surgery and RecoveryDocument10 paginiER: Perforated Peptic Ulcer Surgery and RecoveryKubendranArikrishnanÎncă nu există evaluări
- 001 ICU Case CoyocaDocument9 pagini001 ICU Case CoyocaMiguel Kelly CataneÎncă nu există evaluări
- Cardiac Failure: Ramon Magsaysay Memorial Medical Center College of Nursing NCM 106Document17 paginiCardiac Failure: Ramon Magsaysay Memorial Medical Center College of Nursing NCM 106pauchanmnlÎncă nu există evaluări
- 14 MR Er Krs RDG ZakDocument15 pagini14 MR Er Krs RDG Zaktriska antonyÎncă nu există evaluări
- Try Out NewDocument19 paginiTry Out NewIke AdrianaÎncă nu există evaluări
- TOACS OneeeeeeeeDocument24 paginiTOACS Oneeeeeeeealiakbar178Încă nu există evaluări
- Aortic dissection CT findings pathophysiologyDocument44 paginiAortic dissection CT findings pathophysiologyRoni ArmandaÎncă nu există evaluări
- 1 Cardiac FailureDocument18 pagini1 Cardiac FailurepauchanmnlÎncă nu există evaluări
- RESIDENTS NOTES GUATLODocument2 paginiRESIDENTS NOTES GUATLORizielle MendozaÎncă nu există evaluări
- PCC CaseDocument9 paginiPCC CaseKaila AbeledaÎncă nu există evaluări
- Cardio Case StudentDocument5 paginiCardio Case StudentReynald Ddc ShiroÎncă nu există evaluări
- Candy MIDocument40 paginiCandy MICandy Paraiso AgustinÎncă nu există evaluări
- Morning Report: STEMI Patient Chest PainDocument11 paginiMorning Report: STEMI Patient Chest PainSri Lestari FajerinÎncă nu există evaluări
- RESIDENTS NOTES SEGUBREDocument2 paginiRESIDENTS NOTES SEGUBRERizielle MendozaÎncă nu există evaluări
- Case Scenario Critical CareDocument1 paginăCase Scenario Critical Careapi-236445988Încă nu există evaluări
- Case Study Ws I Perki 2019Document70 paginiCase Study Ws I Perki 2019Luh Leni AriniÎncă nu există evaluări
- CPC Protocol 2022Document4 paginiCPC Protocol 2022Brian AtencionÎncă nu există evaluări
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document26 paginiP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)hendra2darmawan0% (1)
- Sunday, June 26'th 2011Document11 paginiSunday, June 26'th 2011chiquitaputriÎncă nu există evaluări
- Case Report Kardiologi TamponadeDocument13 paginiCase Report Kardiologi TamponadeMuhammad HidayatÎncă nu există evaluări
- Course Task Week 7 NCMB 312Document6 paginiCourse Task Week 7 NCMB 312Angie BaylonÎncă nu există evaluări
- Internal MedicineDocument146 paginiInternal MedicineSh. RamÎncă nu există evaluări
- TBL CasesDocument11 paginiTBL CasesSheng Qian YewÎncă nu există evaluări
- 49-Year-Old Male Admitted with Decreased SensoriumDocument8 pagini49-Year-Old Male Admitted with Decreased SensoriumJan Crizza Dale R. FrancoÎncă nu există evaluări
- PracticeExam 2 QsDocument24 paginiPracticeExam 2 QsBehrouz YariÎncă nu există evaluări
- Nurse Handover: Patient Admitted for Hypertension, HeadacheDocument3 paginiNurse Handover: Patient Admitted for Hypertension, HeadacheAC SantosÎncă nu există evaluări
- Mesenteric Ischemia in Dilated CardiomyopathyDocument30 paginiMesenteric Ischemia in Dilated CardiomyopathyJo AnneÎncă nu există evaluări
- A Case of Ruptured Ectopic Pregnency With Severe Anaemia.: Dr. Shamim Dr. Sarfaraz Dr. ShadabDocument25 paginiA Case of Ruptured Ectopic Pregnency With Severe Anaemia.: Dr. Shamim Dr. Sarfaraz Dr. ShadabShadab KamalÎncă nu există evaluări
- RESIDENTS NOTES LUMBAODocument3 paginiRESIDENTS NOTES LUMBAORizielle MendozaÎncă nu există evaluări
- Anafilactic ShockDocument2 paginiAnafilactic ShockprayogarathaÎncă nu există evaluări
- Paroxysmal Cold Hemoglobinuria Case AnalysisDocument5 paginiParoxysmal Cold Hemoglobinuria Case AnalysisKD NudoÎncă nu există evaluări
- Respiratory System Diseases Case StudyDocument9 paginiRespiratory System Diseases Case Studykuyetjoy20Încă nu există evaluări
- The Era of Modern Medical Sciences A Great Share of Knowledge by ZKDocument47 paginiThe Era of Modern Medical Sciences A Great Share of Knowledge by ZKSyed Abul HasanÎncă nu există evaluări
- Lung Cancer Case ReportDocument65 paginiLung Cancer Case ReportGlennie33% (3)
- Soal Juni Beserta KunciDocument76 paginiSoal Juni Beserta Kuncirsiamb100% (1)
- Morning Report Sunday Morning, March 8th 2020: Syt/Slr/Sth/SwiDocument25 paginiMorning Report Sunday Morning, March 8th 2020: Syt/Slr/Sth/SwimuhammadrikiÎncă nu există evaluări
- Protocol pES PDFDocument4 paginiProtocol pES PDFPaola Gracielle CabreraÎncă nu există evaluări
- Laporan Kasus TB MDRDocument12 paginiLaporan Kasus TB MDRRiyantono PutraÎncă nu există evaluări
- Step 2 CK - NBME 7 Answers UncompleteDocument16 paginiStep 2 CK - NBME 7 Answers UncompleteDuke83% (12)
- Severe PET, TPROM and GDM case scenariosDocument7 paginiSevere PET, TPROM and GDM case scenariosIvy DanÎncă nu există evaluări
- KROK 2 1 профиль (315 Q 2004-2005)Document54 paginiKROK 2 1 профиль (315 Q 2004-2005)Ali ZeeshanÎncă nu există evaluări
- 132 Emergency MedicineDocument14 pagini132 Emergency MedicineVania NandaÎncă nu există evaluări
- DRMC Grand Rounds: Case of Myxedema ComaDocument9 paginiDRMC Grand Rounds: Case of Myxedema ComaKristiannlae DanoÎncă nu există evaluări
- Block 1Document24 paginiBlock 1AbAÎncă nu există evaluări
- Pneumonia QuestionsDocument2 paginiPneumonia Questionsjana.alngÎncă nu există evaluări
- CPC-Patho Version 6Document20 paginiCPC-Patho Version 6Bea SamonteÎncă nu există evaluări
- TBL PaedsDocument10 paginiTBL PaedsHo Yong WaiÎncă nu există evaluări
- Internal Audit ChecklistDocument18 paginiInternal Audit ChecklistAkhilesh Kumar75% (4)
- Ancient MesopotamiaDocument69 paginiAncient MesopotamiaAlma CayapÎncă nu există evaluări
- The Apu Trilogy - Robin Wood PDFDocument48 paginiThe Apu Trilogy - Robin Wood PDFSamkush100% (1)
- Virchow TriadDocument6 paginiVirchow Triadarif 2006Încă nu există evaluări
- Lesson Plan: Lesson: Projectiles Without Air ResistanceDocument4 paginiLesson Plan: Lesson: Projectiles Without Air ResistanceeltytanÎncă nu există evaluări
- 1"a Study On Employee Retention in Amara Raja Power Systems LTDDocument81 pagini1"a Study On Employee Retention in Amara Raja Power Systems LTDJerome Samuel100% (1)
- WL 318 PDFDocument199 paginiWL 318 PDFBeckty Ahmad100% (1)
- Chap 2 Debussy - LifejacketsDocument7 paginiChap 2 Debussy - LifejacketsMc LiviuÎncă nu există evaluări
- Problem SolutionsDocument5 paginiProblem SolutionskkappaÎncă nu există evaluări
- EP - EngineDocument4 paginiEP - EngineAkhmad HasimÎncă nu există evaluări
- LKC CS Assignment2Document18 paginiLKC CS Assignment2Jackie LeongÎncă nu există evaluări
- 11bg USB AdapterDocument30 pagini11bg USB AdapterruddyhackerÎncă nu există evaluări
- Smart Grid Standards GuideDocument11 paginiSmart Grid Standards GuideKeyboardMan19600% (1)
- 2 - Elements of Interior DesignDocument4 pagini2 - Elements of Interior DesignYathaarth RastogiÎncă nu există evaluări
- Religion in Space Science FictionDocument23 paginiReligion in Space Science FictionjasonbattÎncă nu există evaluări
- Flood FillDocument1 paginăFlood FillshubhamÎncă nu există evaluări
- Compare Blocks - ResultsDocument19 paginiCompare Blocks - ResultsBramantika Aji PriambodoÎncă nu există evaluări
- Home Brewing Log Sheet PDFDocument2 paginiHome Brewing Log Sheet PDFStefanita0% (1)
- Flexibility Personal ProjectDocument34 paginiFlexibility Personal Projectapi-267428952100% (1)
- Sattvik Brochure - Web VersionDocument4 paginiSattvik Brochure - Web Versionudiptya_papai2007Încă nu există evaluări
- Features Integration of Differential Binomial: DX BX A X P N MDocument4 paginiFeatures Integration of Differential Binomial: DX BX A X P N Mابو سامرÎncă nu există evaluări
- Essentials For Professionals: Road Surveys Using SmartphonesDocument25 paginiEssentials For Professionals: Road Surveys Using SmartphonesDoly ManurungÎncă nu există evaluări
- Xii Neet Chemistry Mcqs PDFDocument30 paginiXii Neet Chemistry Mcqs PDFMarcus Rashford100% (3)
- Material and Energy Balance: PN Husna Binti ZulkiflyDocument108 paginiMaterial and Energy Balance: PN Husna Binti ZulkiflyFiras 01Încă nu există evaluări
- A Compilation of Thread Size InformationDocument9 paginiA Compilation of Thread Size Informationdim059100% (2)
- SB Z Audio2Document2 paginiSB Z Audio2api-151773256Încă nu există evaluări
- Elements of ClimateDocument18 paginiElements of Climateእኔ እስጥፍÎncă nu există evaluări
- Lesson 2 Socio Anthropological View of The SelfDocument12 paginiLesson 2 Socio Anthropological View of The SelfAilyn RamosÎncă nu există evaluări
- IS 4991 (1968) - Criteria For Blast Resistant Design of Structures For Explosions Above Ground-TableDocument1 paginăIS 4991 (1968) - Criteria For Blast Resistant Design of Structures For Explosions Above Ground-TableRenieÎncă nu există evaluări
- Innovative Food Science and Emerging TechnologiesDocument6 paginiInnovative Food Science and Emerging TechnologiesAnyelo MurilloÎncă nu există evaluări